Abstract
For long-term successful use of ceramic materials in dental procedures, it is necessary to ensure reliable bonding of restorations to dental substrates. This can be achieved by the application of a proper luting cement and through additional surface conditioning. The present systematic review summarizes the most up-to-date evidence on the use of different surface modification methods to enhance the bond strength of dental ceramics to the hard tissues of the teeth. The authors of the review searched the Web of Science, Scopus, and MEDLINE databases to identify relevant articles published between 1 January 2010 and 1 January 2020. A total of 4892 records were identified, and after screening, the full text of 159 articles was evaluated, which finally resulted in the inclusion of 19 studies. The available reports were found to be heterogeneous in terms of materials and methodology, and therefore, only within-studies comparison was performed instead of comparison between studies. A statistically significant difference in the bond strength between the samples treated with different methods of surface conditioning, or between conditioned and nonconditioned samples, was revealed by most of the studies. Predominantly, the studies showed that a combination of mechanical and chemical methods was the most effective way of enhancing bond strength. Artificial aging and luting cement were also identified as the factors significantly influencing bond strength.
1. Introduction
Due to growing esthetic demand and the development of computer-aided design/computer-aided manufacturing (CAD/CAM) systems in recent years, ceramics have become a very popular material for the manufacturing of fixed dental prosthetics, ranging from veneers, inlays, and onlays to full-crown restorations and bridges. This popularity is mainly attributed to their properties, such as biocompatibility, excellent esthetic effect, and chemical and volumetric stability [1,2,3,4]. However, the clinical success of a ceramic restoration also depends on good marginal adaptation as well as strong and reliable adhesion of the ceramic surface to the tooth tissues. Adhesive bond strength, calculated by dividing the failing load by the bond area, could be determined using various tests (shear, tensile, microtensile or pull-out test). Reliable adhesion could be achieved by using a proper luting cement providing attachment of dental restoration to the prepared teeth (including conventional cements, such as zinc phosphate or glass-ionomer, and contemporary cements, such as resin and resin-modified glass-ionomer) and through additional surface conditioning. This will not only increase the retention of the restoration but also minimize microleakage, improve marginal adaptation, and increase the fracture resistance, thereby ensuring durability and long life of the prosthetic reconstruction [5,6,7].
The successful bonding of ceramic restorations is strongly associated with proper chemical and mechanical interactions of the ceramic surface with luting cement and the hard tissues of the teeth [5,8,9,10]. For this purpose, various methods of surface treatment are applied to increase the adhesion of the ceramic material to the luting cement and the dental substrates [11,12,13]. Micromechanical retention, which results in increased surface roughness, could be facilitated by methods such as acid etching, airborne particle abrasion (APA), tribochemical silica coating, and laser irradiation [12]. On the other hand, chemical conditioning can be performed using bifunctional silane agents that enhance the wettability of the ceramic surface and improve the penetration of the resin cement into microscopic porosities created in the conditioned surface [13,14]. A frequently studied alternative is the universal adhesive system which is based on phosphate monomers (10-methacryloyloxydecyl dihydrogen phosphate, MDP) [10,11,12,13]. The 10-MDP, incorporated into dental adhesive systems as a functional monomer, promotes chemical interaction with dental substrates, enhancing adhesion forces. Through the formation of MDP-calcium salts it promotes also the protection of collagen fibers [15].
The proper choice of surface conditioning method is of huge importance for the clinical utility of ceramic restorations. The selection of this method is dependent on the chemical and physical properties of the material. Silica-based ceramics, such as leucite, lithium disilicate, or feldspathic porcelain, are easier to work with because their glassy phase can be more easily chemically treated than high-strength zircon dioxide [3,4,5]. On the other hand, zirconia has favorable mechanical properties such as high flexural strength, relatively low elastic modulus, and high fracture toughness [16]. This material is also characterized by good chemical and dimensional stability [5,6]. However, the adhesion of zirconium to the dental substrates is unstable and poor which attracts the attention of many research groups attempting to achieve optimum bond strength without altering the strength of the ceramic itself [5,6,7,8,9]. Due to their crystalline structure, zirconium materials are acid-resistant. Therefore, the first modification of their surface mainly involves a mechanical process and the creation of a layer containing a glassy phase that can be modified chemically in a much simpler way. For this purpose, APA, silica coating, or porcelain glazing was performed [3,5,9,10].
Although numerous studies have been carried out on ceramic surface conditioning, there is still no consensus on the optimal protocol that would enable the best bonding between a ceramic restoration and the dental tissue to be obtained. The aim of this systematic review was to summarize the most up-to-date available evidence on the use of different surface conditioning methods to enhance the bond strength of dental ceramics to the hard tissues of the teeth. The authors of the review focused on the critical revision of the technical details concerning the materials and techniques applied in the most recent experimental research, which could allow the identification of the strengths and weaknesses of the available reports. Additionally, the review is intended to determine the significance of the other factors influencing the bond strength values, such as artificial aging and luting cement, in order to identify the most effective surface conditioning methods that would contribute to increasing the clinical utility of modern dental materials.
2. Results
2.1. Study Selection
Three authors (A.M., S.O. and W.F.) were involved in the literature identification and record screening procedure. The selection process is detailed in the PRISMA flow diagram in Figure 1. A total of 4892 records were found in the databases: 2035 in Web of Science, 1724 in Scopus, and 1133 in MEDLINE. In addition, two records were added after screening the reference lists of the qualified studies. After removing the duplicates from the studies identified from the different databases, a total of 4070 records remained. Then, three authors screened the titles and abstracts of these remaining records based on the inclusion and exclusion criteria, after which 3911 articles were excluded. Afterward, two authors (A.M. and W.F.) independently assessed the full text of 159 selected articles for the final evaluation of eligibility. Their assessment was critically revised by another author (J.W.). Finally, 19 articles were included in this systematic review.
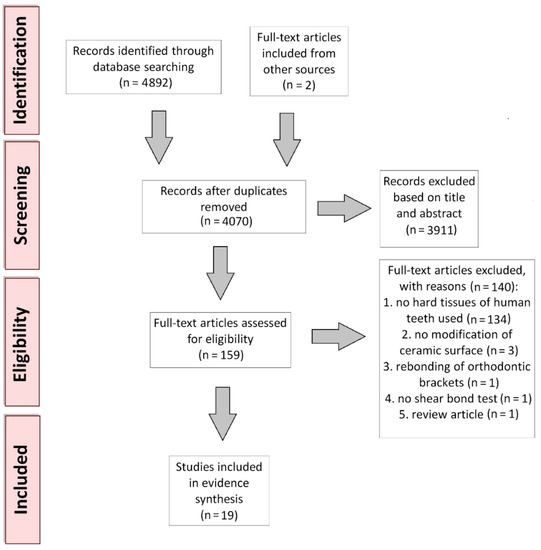
Figure 1.
PRISMA flow diagram of the systematic review protocol.
2.2. Material Characterization and Specimen Preparation
All the qualified papers investigated the bond strength of dental ceramics to dental hard tissues. Fifteen of these studies described ceramics luted to human dentin [7,16,17,18,19,20,21,22,23,24,25,26,27,28,29], two described ceramics luted to human enamel [30,31] and one described ceramics luted to the dentin of bovine teeth [32]. Saker et al. performed a comparative study on two human dental tissues: dentin and enamel [33].
The types of ceramic materials and dental cements used in the included studies for specimen preparation are summarized in Table 1. Most of the selected studies focused on yttria-stabilized tetragonal zirconia polycrystals (Y-TZP) [16,18,19,20,21,22,24,26,31,32,33]. Furthermore, lithium disilicate glass-ceramic was investigated by Madina et al. [17], feldspathic ceramic by Jetti et al. [25], and monolithic zirconia by Reddy et al. [20], Feng et al. [23], Butler et al. [29], and Zandparsa et al. [30], while Park et al. evaluated resin nanoceramics [7]. Different types of dental ceramics were compared by Kara et al. [27] (feldspathic ceramic, leucite-reinforced hot-pressed ceramic, hot-pressed lithium disilicate ceramic, and zirconia) and Gamal et al. [28] (lithium disilicate and zirconia).

Table 1.
Characteristics of the materials used in the studies included in the systematic review, presented in chronological order.
The included papers also differed in terms of the dental cement used to lute the ceramic to the tooth tissue. In many studies, Panavia F2.0, a self-etching, MDP-containing dual-polymerizing resin cement, was either used separately [17,19,30,33] or compared with adhesive self-curing resin cement (Superbond C and B [31]) or dual-polymerizing resin cement (Variolink N [26]). Other self-adhesive materials evaluated were Multilink Speed, a self-curing composite resin cement, which can be light-cured if desired [20], and Clearfil Esthetic Cement [27]. Some studies also investigated the dual-polymerizing adhesive cements, including Multilink Automix [16], Variolink II [25], RelyX Ultimate [28], and Duo-link [29]. Shahin et al. compared the various groups of cements, namely zinc phosphate cement (Hoffmann quick setting), glass-ionomer cement (Ketac Cem Maxi Cap), and adhesive resin cement (Panavia 21) [18]. Alves et al. compared an adhesive resin cement (RelyX ARC) with a self-adhesive resin cement (RelyX U200) [24], while De Castro et al. compared an adhesive resin cement (RelyX ARC) with a self-adhesive (RelyX U100) and a dual-polymerizing resin cement (Panavia F) [21]. Menani et al. [32] also separately studied Panavia F as well as comparing this cement with self-adhesive dual-polymerizing resin cements (Clearfil SA Cement [22], RelyX Unicem [23]). One study focused on a cement material described as “RelyX,” but it is not very informative [7].
2.3. Methodology of the Selected Studies: Surface Treatment, Artificial Aging, and Bond Strength Evaluation
The methods used for surface conditioning and artificial aging in the included studies are presented in Table 2.

Table 2.
Characteristics of the surface treatment and artificial aging methods, and primary and secondary outcomes of the studies included in the systematic review, presented in chronological order. HF acid = hydrofluoric acid; APA = airborne particle abrasion; SBS = shear bond strength.
The included studies investigated the techniques of both micromechanical and chemical bonding of ceramics to dental hard tissues. Among the methods applied to achieve micromechanical bonding, there were different kinds of mechanical treatments such as APA [7,16,17,18,20,21,23,26,27,28,29,30,31,33], tribochemical silica coating [7,16,17,19,21,22,23,24,26,30,33], laser irradiation [26,27,28], and wet hand grinding [16]. The second approach utilized for micromechanical bonding was a chemical-based one which involved the use of various acid solutions to etch the conditioned surface [7,16,17,20,22,25,27,28,30,31,32,33]. On the other hand, different methods applied to achieve chemical bonding were also evaluated. These included the use of porcelain glaze [22,33] and coupling agents such as primers and silanes [7,16,17,19,20,22,23,24,25,28,29,30,32,33]. A nontreated control was used in 12 of the 19 included studies [16,18,19,20,23,24,26,27,29,31,32,33]. In the rest of the studies, different methods of surface conditioning were compared with each other [7,17,21,22,25,28,30].
Additionally, in 10 of the 19 selected studies, artificial aging was performed [16,18,21,22,24,26,27,30,31,33]. The parameters of aging differ significantly. In the studies, the specimens were subjected to prolonged storage in distilled water at 37 °C for different periods of time [18,21,24] or subjected to different numbers of thermal cycles between 5 °C and 55 °C with different dwell times [21,22,26,27,30,31,33]. Both prolonged water storage and thermal cycles were performed in the study conducted by Qeblawi et al., [16]. In a study carried out by Shahin et al., water storage and thermocycling were followed by masticatory simulation [18].
To investigate the bond strength between dental ceramics and dental hard tissues, most of the researchers used shear bond strength test with a shear crosshead speed of 1.0 mm/min [16,20,24,25,26,28,31] or 0.5 mm/min [19,22,29,30]. The other methods used for evaluating bond strength were the pull-out test of retentive strength [17,18], extrusion shear test [32], tensile test [33], and microtensile strength test [7,21,23,27].
2.4. Outcomes
The primary and secondary outcomes of the selected studies are described in Table 2.
As a primary outcome, a statistically significant difference in bond strength between the samples treated with different surface conditioning methods, or between the conditioned and nonconditioned samples, was revealed in most of the studies [7,16,18,19,20,21,23,24,25,26,27,28,29,30,31,32,33]. Only two studies showed no statistically significant difference between the compared experimental groups [17,22]. However, in these studies, there were no nontreated control groups, but different surface conditioning methods were compared to each other (hydrofluoric (HF) acid + silane vs. APA + tribochemical silica coating + silane [17] or low-fusing porcelain glaze + HF acid + silane vs. tribochemical silica coating [22]). Kara et al. found no significant differences in bond strength in one out of four evaluated ceramic groups that were treated with different methods [27]. All the studies conducted using a nontreated control group concluded that the bond strength of the nontreated specimens was significantly lower than that of the specimens subjected to surface modification [16,18,19,20,23,24,26,27,29,31,32,33]. Many studies suggested that a combination of mechanical and chemical methods, such as silica coating + silane [16], silica coating + primer or HF acid + glaze [33], APA + primer [30], APA + silica coating + silane [23], and APA + universal adhesive [7], was the most effective way of enhancing bond strength.
The impact of the other studied factors on bond strength between ceramics and teeth was investigated as a secondary outcome in 10 of the 19 selected papers. Artificial aging [16,18,21,22,31] and luting cement [18,21,23,26] were identified as the factors significantly influencing the obtained values of bond strength. Furthermore, Saker et al. demonstrated that substrate type (enamel vs. dentin) also had a significant influence on bond strength [33].
2.5. Evidence Synthesis
The quality of the evidence presented in the studies, with overall GRADE (Grading of Recommendations Assessment, Development and Evaluation) scores for primary and secondary outcomes, is shown in Table 3. The number of samples in each experimental group used in the included studies ranged from 3 [21] to 30 [7]. Most of the included studies (17 out of 19) revealed the significant influence of the surface conditioning methods on the bond strength of dental ceramics to dental hard tissues. A significant effect of the other studied factors (e.g., luting cement and artificial aging) was demonstrated in 8 out of 10 studies.

Table 3.
Summary findings for the primary and secondary outcomes.
The quality of the evidence presented in most of the included studies was scored as +++− (moderate), ++++ (high), or ++− (low). The common causes of score reduction included imprecision and risk of bias.
3. Discussion
Due to their huge clinical importance, the methods that promote reliable bonding of ceramic restorations to the dental hard tissues are of interest to many research groups. Several interesting reviews of the research concerning surface conditioning methods applied to increase the bond strength between ceramics and teeth have been published in recent years. The conducted analyses drew the conclusion that a combination of mechanical and chemical treatments is essential for good adhesion. However, they revealed that currently there is a lack of evidence to support a universal adhesion protocol [34,35,36].
This systematic review focused primarily on the influence of surface modification methods on the bond strength between ceramics and dental substrates. The vast majority of the selected articles performed the modification of zirconia to achieve long-term, durable bonding of this material. In one study, a lithium disilicate glass-ceramic [17] and feldspathic ceramic [25] were investigated. One research paper was based on resin nanoceramic [7], which is a relatively new material, used mainly for minor restorations. Different types of dental ceramics were compared in the studies by Kara et al. (feldspathic ceramic, leucite-reinforced hot-pressed ceramic, hot-pressed lithium disilicate ceramic, and zirconia) [27] and Gamal et al. (lithium disilicate and zirconia) [28]. These studies demonstrated that different types of ceramics required different methods of surface conditioning for strong bonding to dental substrates [27,28].
The present systematic review revealed that different mechanical treatments (APA, tribochemical silica coating, laser irradiation, and wet hand grinding) and chemical treatments (acid etching) were investigated to achieve micromechanical bonding. Other methods of chemical bonding such as the use of porcelain glaze and coupling agents (primers and silanes) were also evaluated. A statistically significant difference in bond strength between the samples treated with different surface conditioning methods, or between conditioned and nonconditioned samples, was revealed in most of the studies. Predominantly, the studies showed that a combination of mechanical and chemical methods, such as silica coating + silane [16], silica coating + primer or HF acid + glaze [33], APA + primer [30], APA + silica coating + silane [23], and APA + universal adhesive [7], was the most effective way of enhancing bond strength. Three studies investigated the effectiveness of laser irradiation as an alternative technique for treating ceramic surfaces prior to bonding resin cements. They revealed increased shear bond strength between zirconia and dentin after irradiation with YbPL laser [26], Nd:YAG laser [27], and CO2 laser [28] compared with nonirradiated ceramic surfaces.
Apart from evaluating the effectiveness of surface conditioning methods in the present review, attention was also paid to the significance of the effects of artificial aging performance and the selection of luting agent on bond strength. Artificial aging was performed in 10 out of 19 selected studies [16,18,21,22,24,26,27,30,31,33]. The parameters of aging differ significantly—in the selected studies, the specimens were stored in distilled water at 37 °C for different periods of time or were subjected to different numbers of thermal cycles between 5 °C and 55 °C. One study combined prolonged water storage and thermocycling [16], while another study additionally performed masticatory simulation after water storage and thermocycling [18]. Only 5 out of 10 studies that used artificial aging compared the results for aged and nonaged samples. All of them reported a statistically significant decrease in the bond strength of specimens after artificial aging [16,18,21,22,31].
In total, 6 out of 19 studies compared the bond strength values achieved using different luting agents. Shahin et al. compared various groups of cements—zinc phosphate cement (Hoffmann quick setting), glass-ionomer cement (Ketac Cem Maxi Cap), and adhesive resin cement (Panavia 21), and demonstrated that the adhesive resin cement (Panavia 21) provided significantly higher retention than the conventional cements [18]. Most of the other studies also revealed a statistically significant difference in bond strength between the groups luted with different cements [21,22,23,26]. Application of the adhesive resin cement Panavia F resulted in a significantly higher bond strength compared to several self-adhesive cements (RelyX U100 [21], Clearfil SA [22], RelyX Unicem [23]). Unal et al. showed a higher bond strength after cementation with adhesive MDP-containing Panavia F 2.0 compared to Bis-GMA-containing Variolink N cement [26]. Only one study did not show any statistically significant difference between the compared adhesive resin cement (RelyX ARC) and self-adhesive resin cement (RelyX U200), and thus did not confirm the influence of the type of cement on bond strength [24].
An additional huge advantage of this systematic review is the selection of papers describing research conducted on samples luted to dental hard tissues (dentin or enamel) of humans. This criterion for the method of specimen preparation significantly reduced the number of studies that could be qualified for the review, but it enabled a more precise analysis in terms of the clinical utility of the results obtained. In one study, bovine teeth were used as a substitute for human tissue [32], but the validity of such an approach was confirmed in previous reports [37,38,39,40].
The main limitation of this review is the lack of a meta-analysis, which could not be performed due to the heterogeneity of the available reports on dental ceramic surface modifications, both in terms of materials and protocols. Therefore, the results were compared only within studies but not between studies. The identified risk of bias can be attributed mainly to the lack of information regarding the number of operators performing the experiments and a low sample size which was observed in several studies. Furthermore, some of the reports did not precisely define the full names of the materials used.
One of the sources of heterogeneity was the application of different bond strength tests (shear, pull-out, extrusion, tensile, and microtensile strength tests). Most of the included studies performed a shear bond strength test, which is easy to use, but is characterized by less uniform stress distribution compared to a tensile bond strength test [7,41]. In addition, some previous analyses revealed that microbond tests are more reliable than macrobond tests [42].
Another interesting issue that should be investigated in the future is the limited usefulness of bond strength testing, including shear loading. As they do not fully mimic the real clinical situation with a complex pattern of stress distribution during failure, additional methods should be applied to better predict the clinical behavior of ceramic restorations. Thus, the performance of fatigue tests under cyclic loading, as a way of masticatory simulation, should be considered [43]. The application of degradation protocols (e.g., water or saliva storage and thermal cycling) should also be included to simulate the chemical and thermal conditions that restorations may be subjected to. Due to their low costs, water storage and thermocycling in water are the most common methods of artificial aging. However, many different models could be proposed to evaluate the effect of the oral environment (different pH levels, thermal fluctuations, enzymatic activity, masticatory forces, etc.,) on the degradation of dental materials. Consideration of these factors is strongly recommended for future laboratory research in order to simulate the clinical situation more accurately. Finally, apart from the recommendation for using more comparable methodologies in laboratory studies evaluating the different aspects of bond strength, further clinical trials are needed to provide relevant evidence of successful bonding [34,35].
4. Materials and Methods
This systematic review was accomplished in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines used to collect and report data [44,45]. It was conducted in an attempt to answer the following questions: (1) Does surface conditioning significantly influence the bond strength of dental ceramics to dental tissue? (2) Which surface conditioning method can most effectively improve the bond strength of dental ceramics to dental tissue? (3) What are the other factors (e.g., artificial aging, luting cement) that significantly influence the bond strength of dental ceramics to dental tissue?
4.1. Search Strategy
4.1.1. Data Sources and Searches
The authors searched the Web of Science, Scopus, and MEDLINE databases to identify the relevant articles published in English between 1 January 2010 and 1 January 2020. The literature search was performed combining each of the following keywords: (1) dental ceramic, (2) dental resin cement, (3) dental luting cement, and (4) teeth; with each of the following keywords: (A) surface modification, (B) surface treatment, and (C) surface conditioning; and with each of the following additional keywords: (a) bond strength, (b) durability, and (c) adhesion. The database search was supplemented with a hand search of the bibliographic references of the retrieved articles aimed at the identification of potentially relevant papers [44,45].
Three authors (A.M., S.O. and W.F.) were involved in the literature identification and record-screening procedure. After removing the duplicates from the records identified in different databases, the three authors screened the titles and abstracts of the remaining records based on the inclusion and exclusion criteria. For a final evaluation of eligibility, two authors (A.M. and W.F.) performed an independent assessment of the full text of the selected articles, which was critically revised by another author (J.W.). None of the review authors was blind to the title of the articles, author names, and affiliations.
4.1.2. Eligibility Criteria for Initial Study Selection
During the database search, the authors aimed to select studies that quantitatively investigated the effects of different surface treatment methods on the bond strength of dental ceramics luted with resin cements to the hard tissues of the tooth.
The authors added filters to identify only English language and full-text articles published between 1 January 2010 and 1 January 2020. Inclusion and exclusion criteria were defined according to the PICOS (Population, Intervention, Comparison, Outcomes and Study Design) approach and are listed in Table 4.

Table 4.
Inclusion and exclusion criteria.
4.2. Data Extraction
After the inclusion of final studies, two reviewers (A.M. and W.F.) carried out data extraction independently. Then, the third author (J.W.) checked the validity of the extracted data. The data extraction process included retrieval of information regarding the type of specimen, type and name of ceramics, type and name of the resin cement, number of samples, methods of surface treatment, methods of artificial aging, methods of bond strength evaluation, and primary and secondary outcomes.
The primary outcome of interest was the impact of surface treatment methods on the bond strength of dental ceramics to the tooth structures, while the secondary outcome was the impact of the other studied factors on the mentioned parameter.
4.3. Data Synthesis and Analysis and Quality Assessment
The studies included in this systematic review were very heterogeneous; therefore, it was not possible to perform a meta-analysis, and instead, a narrative and qualitative summary was prepared.
The GRADE approach was used to assess the quality of evidence for the primary and secondary outcomes. For each outcome, the quality of evidence was assigned to one of the following categories: very low, low, moderate, or high [46].
5. Conclusions
Different methods of surface treatment can be applied to achieve strong, durable bonding of different types of ceramics to dental substrates. The present review of laboratory studies revealed a statistically significant difference in bond strength between the samples treated with different surface conditioning methods, or between conditioned and nonconditioned samples. Based on the results analyzed, a combination of mechanical and chemical methods is proposed as the most effective way of enhancing bond strength.
In addition, this review of the available literature highlights the need for standardizing the methodology of surface modification for future investigations. Due to the use of different materials, protocols, and tests by researchers, data comparison is quite difficult. Moreover, standardized protocols should attempt to reproduce clinical conditions by applying different methods of testing, including fatigue tests, as well as through artificial aging of samples. Such an approach will allow better prediction of the real clinical behaviors of the evaluated ceramic materials.
Author Contributions
Conceptualization: J.W. and M.W.; methodology: J.W., A.M., and W.F.; validation: J.W. and M.W.; investigation: A.M., S.O., and W.F.; data curation: A.M. and J.W.; writing—original draft preparation: A.M. and J.W.; writing—review and editing: M.W. and M.Z.; supervision: J.W. and M.W.; funding acquisition: M.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research was partially supported by Funds of Wroclaw Medical University (grant no. SUB.B160.21.061).
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Tanaka, S.; Takaba, M.; Ishiura, Y.; Kamimura, E.; Baba, K. A 3-year follow-up of ceria-stabilized zirconia/alumina nanocomposite (Ce-TZP/A) frameworks for fixed dental prostheses. J. Prosthodont. Res. 2015, 59, 55–61. [Google Scholar] [CrossRef]
- Philipp, A.; Fischer, J.; Hämmerle, C.H.; Sailer, I. Novel ceriastabilized tetragonal zirconia/alumina nanocomposite as framework material for posterior fixed dental prostheses: Preliminary results of a prospective case series at 1 year of function. Quintessence Int. 2010, 41, 313–319. [Google Scholar] [PubMed]
- Blatz, M.B.; Sadan, A.; Kern, M. Resin-ceramic bonding: A review of the literature. J. Prosthet. Dent. 2003, 89, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Blatz, M.B.; Sadan, A.; Arch, G.H.; Lang, B.R. In vitro evaluation of long-term bonding of procera all ceram alumina restorations with modified resin luting agent. J. Prosthet. Dent. 2003, 89, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Lung, C.Y.; Matinlinna, J.P. Aspects of silane coupling agents and surface conditioning in dentistry: An overview. Dent. Mater. 2012, 28, 467–777. [Google Scholar] [CrossRef] [PubMed]
- Bielen, V.; Inokoshi, M.; Munck, J.D.; Zhang, F.; Vanmeensel, K.; Minakuchi, S.; Vleugels, J.; Naert, I.; Van Meerbeek, B. Bonding effectiveness to differently sandblasted dental zirconia. J. Adhes. Dent. 2015, 17, 235–242. [Google Scholar] [PubMed]
- Park, J.H.; Choi, Y.S. Microtensile bond strength and micromorphologic analysis of surface-treated resin nanoceramics. J. Adv. Prosthodont. 2016, 8, 275–284. [Google Scholar] [CrossRef] [PubMed]
- Mattiello, R.D.L.; Coelho, T.M.K.; Insaurralde, E.; Coelho, A.A.K.; Terra, G.P.; Kasuya, A.V.B.; Favarao, I.N.; Goncalves, L.S.; Fonseca, R.B. A review of surface treatment methods to improve the adhesive cementation of zirconia-based ceramics. Int. Sch. Res. Not. Biomater. 2013, 2013, 185376. [Google Scholar] [CrossRef]
- Griffin, J.D.; Suh, B.; Chen, L.; Brown, D.J. Surface treatments for zirconia bonding: A clinical perspective. Can. J. Restor. Dent. Prosthodont. 2010, 3, 23–29. [Google Scholar]
- Anami, L.C.; Lima, J.; Valandro, L.F.; Kleverlaan, C.J.; Feilzer, A.J.; Bottino, M.A. Fatigue resistance of Y-TZP/porcelain crowns is not influenced by the conditioning of the intaglio surface. Oper. Dent. 2016, 41, E1–E12. [Google Scholar] [CrossRef]
- Soares, C.J.; Soares, P.V.; Pereira, J.C.; Fonseca, R.B. Surface treatment protocols in the cementation process of ceramic and laboratory-processed composite restorations: A literature review. J. Esthet. Rest. Dent. 2005, 17, 224–235. [Google Scholar] [CrossRef] [PubMed]
- Atsu, S.S.; Kilicarslan, M.A.; Kucukesmen, H.C.; Aka, P.S. Effect of zirconium-oxide ceramic surface treatments on the bond strength to adhesive resin. J. Prosthet. Dent. 2006, 95, 430–436. [Google Scholar] [CrossRef]
- Blatz, M.B.; Chiche, G.; Holst, S.; Sadan, A. Influence of surface treatment and simulated aging on bond strengths of luting agents to zirconia. Quintessence Int. 2007, 38, 745–753. [Google Scholar]
- Lindgren, J.; Smeds, J.; Sjogren, G. Effect of surface treatments and aging in water on bond strength to zirconia. Oper. Dent. 2008, 33, 675–681. [Google Scholar] [CrossRef] [PubMed]
- Carrilho, E.; Cardoso, M.; Marques Ferreira, M.; Marto, C.M.; Paula, A.; Coelho, A.S. 10-MDP Based Dental Adhesives: Adhesive Interface Characterization and Adhesive Stability—A Systematic Review. Materials 2019, 12, 790. [Google Scholar] [CrossRef] [PubMed]
- Qeblawi, D.M.; Munoz, C.A.; Brewer, J.D.; Monaco, E.A. The effect of zirconia surface treatment on flexural strength and shear bond strength to a resin cement. J. Prosthet. Dent. 2010, 103, 210–220. [Google Scholar] [CrossRef]
- Madina, M.M.; Ozcan, M.; Badawi, M.F. Effect of surface conditioning and taper angle on the retention of IPS e.max Press crowns. J. Prosthodont. 2010, 19, 200–204. [Google Scholar] [CrossRef]
- Shahin, R.; Kern, M. Effect of air-abrasion on the retention of zirconia ceramic crowns luted with different cements before and after artificial aging. Dent. Mater. 2010, 26, 922–928. [Google Scholar] [CrossRef]
- Chai, J.; Chu, F.C.; Chow, T.W. Effect of surface treatment on shear bond strength of zirconia to human dentin. J. Prosthodont. 2011, 20, 173–179. [Google Scholar] [CrossRef]
- Reddy, S.M.; Vijitha, D.; Deepak, T.; Balasubramanian, R.; Satish, A. Evaluation of shear bond strength of zirconia bonded to dentin after various surface treatments of zirconia. J. Indian Prosthodont. Soc. 2014, 14, 38–41. [Google Scholar] [CrossRef]
- de Castro, H.L.; Corazza, P.H.; de Paes-Júnior, T.A.; Bona, A.D. Influence of Y-TZP ceramic treatment and different resin cements on bond strength to dentin. Dent. Mater. 2012, 28, 1191–1197. [Google Scholar] [CrossRef] [PubMed]
- Bottino, M.A.; Bergoli, C.; Lima, E.G.; Marocho, S.M.; Souza, R.O.; Valandro, L.F. Bonding of Y-TZP to dentin: Effects of Y-TZP surface conditioning, resin cement type, and aging. Oper. Dent. 2014, 39, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.L.; Liu, R.Y.; Znag, Y.L.; Chen, L.J. Effect of Surface Treatment and Resin Cement on Microtensile Bond Strength of Zirconia to Dentin. Key Eng. Mater. 2014, 602, 602–605. [Google Scholar] [CrossRef]
- Alves, M.; Campos, F.; Bergoli, C.D.; Bottino, M.A.; Özcan, M.; Souza, R. Effect of Adhesive Cementation Strategies on the Bonding of Y-TZP to Human Dentin. Oper. Dent. 2016, 41, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Jetti, R.R.; Balasubramaniam, M.; Chidambaranathan, A.S.; Srinivasan, S. Evaluation of Shear Bond Strength of Feldspathic CAD/CAM Ceramic with Dentin using 2 Bonding Agents and 2 Surface Treatments-An Invitro Study. J. Clin. Diagn. Res. 2015, 9, 36–39. [Google Scholar] [CrossRef] [PubMed]
- Unal, S.M.; Nigiz, R.; Polat, Z.S.; Usumez, A. Effect of ultrashort pulsed laser on bond strength of Y-TZP zirconia ceramic to tooth surfaces. Dent. Mater. J. 2015, 34, 351–357. [Google Scholar] [CrossRef]
- Kara, O.; Ozturk, A. The effect of surface treatments on the bonding strength of ceramic inlays to dentin. J. Adhes. Sci. Technol. 2017, 31, 1–13. [Google Scholar] [CrossRef]
- Gamal, A.E.; Medioni, E.; Rocca, J.P.; Fornaini, C.; Brulat-Bouchard, N. CO2 laser dentin surface treatment most effectively increased ceramic shear bond strength. Laser Ther. 2018, 27, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Butler, S.; Linke, B.; Torrealba, Y. Effect of MDP-Based Primers on the Luting Agent Bond to Y-TZP Ceramic and to Dentin. Biomed. Res. Int. 2018, 16. [Google Scholar] [CrossRef]
- Zandparsa, R.; Talua, N.A.; Finkelman, M.D.; Schaus, S.E. An in vitro comparison of shear bond strength of zirconia to enamel using different surface treatments. J. Prosthodont. 2014, 23, 117–123. [Google Scholar] [CrossRef]
- Lv, P.; Yang, X.; Jiang, T. Influence of Hot-Etching Surface Treatment on Zirconia/Resin Shear Bond Strength. Materials 2015, 8, 8087–8096. [Google Scholar] [CrossRef]
- Menani, L.R.; Farhat, I.A.G.K.M.; Tiossi, R.; Ribeiro, R.F.; Guastaldi, A.C. Effect of surface treatment on the bond strength between yttria partially stabilized zirconia ceramics and resin cement. J. Prosthet. Dent. 2014, 112, 357–364. [Google Scholar] [CrossRef]
- Saker, S.; Ibrahim, F.; Ozcan, M. Effect of different surface treatments on adhesion of In-Ceram Zirconia to enamel and dentin substrates. J. Adhes. Dent. 2013, 15, 369–376. [Google Scholar] [PubMed]
- Russo, D.S.; Cinelli, F.; Sarti, C.; Giachetti, L. Adhesion to Zirconia: A Systematic Review of Current Conditioning Methods and Bonding Materials. Dent. J. 2019, 7, 74. [Google Scholar] [CrossRef] [PubMed]
- Luthra, R.; Kaur, P. An insight into current concepts and techniques in resin bonding to high strength ceramics. Aust. Dent. J. 2016, 61, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Ozcan, M.; Yoshida, K.; Cheng, H.; Sawase, T. Bonding to industrial indirect composite blocks: A systematic review and meta-analysis. Dent. Mater. 2020, 36, 119–134. [Google Scholar] [CrossRef] [PubMed]
- Yassen, G.H.; Platt, J.A.; Hara, A.T. Bovine teeth as substitute for human teeth in dental research: A review of literature. J. Oral Sci. 2011, 53, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Soares, F.Z.; Follak, A.; da Rosa, L.S.; Montagner, A.F.; Lenzi, T.L.; Rocha, R.O. Bovine tooth is a substitute for human tooth on bond strength studies: A systematic review and meta-analysis of in vitro studies. Dent. Mater. 2016, 32, 1385–1393. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho, M.F.F.; Leijôto-Lannes, A.C.N.; Rodrigues, M.C.N.; Nogueira, L.C.; Ferraz, N.K.L.; Moreira, A.N.; Yamauti, M.; Zina, L.G.; Magalhães, C.S. Viability of Bovine Teeth as a Substrate in Bond Strength Tests: A Systematic Review and Meta-analysis. J. Adhes. Dent. 2018, 20, 471–479. [Google Scholar]
- Canbek, K.; Karbach, M.; Gottschalk, F.; Erbe, C.; Wehrbein, H. Evaluation of bovine and human teeth exposed to thermocycling for microleakage under bonded metal brackets. J. Orofac. Orthop. 2013, 74, 102–112. [Google Scholar] [CrossRef]
- Fernandes, V.V.B.; Oliani, M.G.; Nogueira, L.; Silva, J.M.F.; Araujo, R.M. Analysis and Comparison of Different Bond Strength Tests. JSM Dent. 2016, 4, 1076. [Google Scholar]
- Sirisha, K.; Rambabu, T.; Ravishankar, Y.; Ravikumar, P. Validity of bond strength tests: A critical review—Part II. J. Conserv. Dent. 2014, 17, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Rungruanganunt, P.; Kelly, R.J. Insight into “bonding” of all-ceramics influenced by cement, sandblasting and water storage time. Dent. Mater. 2012, 28, 939–944. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; for the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.; Oxman, A.D.; Akl, E.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falk-Ytter, Y.; Glasziou, P.; Debeer, H.; et al. GRADE guidelines 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).