Decreased Sound Tolerance in Tinnitus Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Interview
2.2. Audiological Evaluation
2.3. Questionnaires
2.3.1. Hyperacusis Questionnaire
2.3.2. Visual Analogue Scales
2.3.3. Tinnitus Handicap Inventory
2.4. Statistical Analysis
2.5. Participants
3. Results
3.1. Audiological Tests
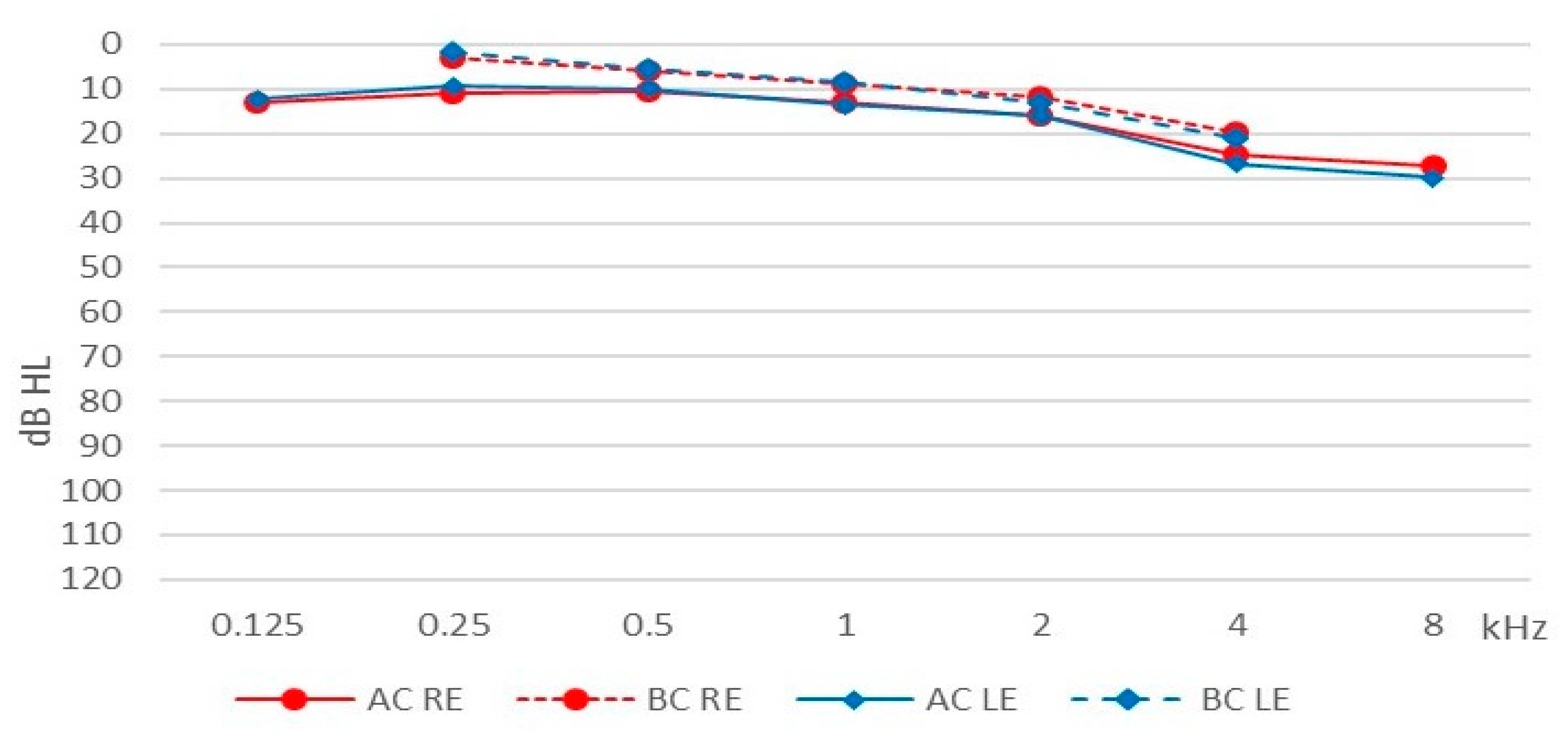
3.1.1. Pure Tone Audiometry
3.1.2. Uncomfortable Loudness Levels
3.1.3. Impedance Audiometry
3.2. Decreased Sound Tolerance Assessment
3.2.1. Interview
3.2.2. Visual Analogue Scales
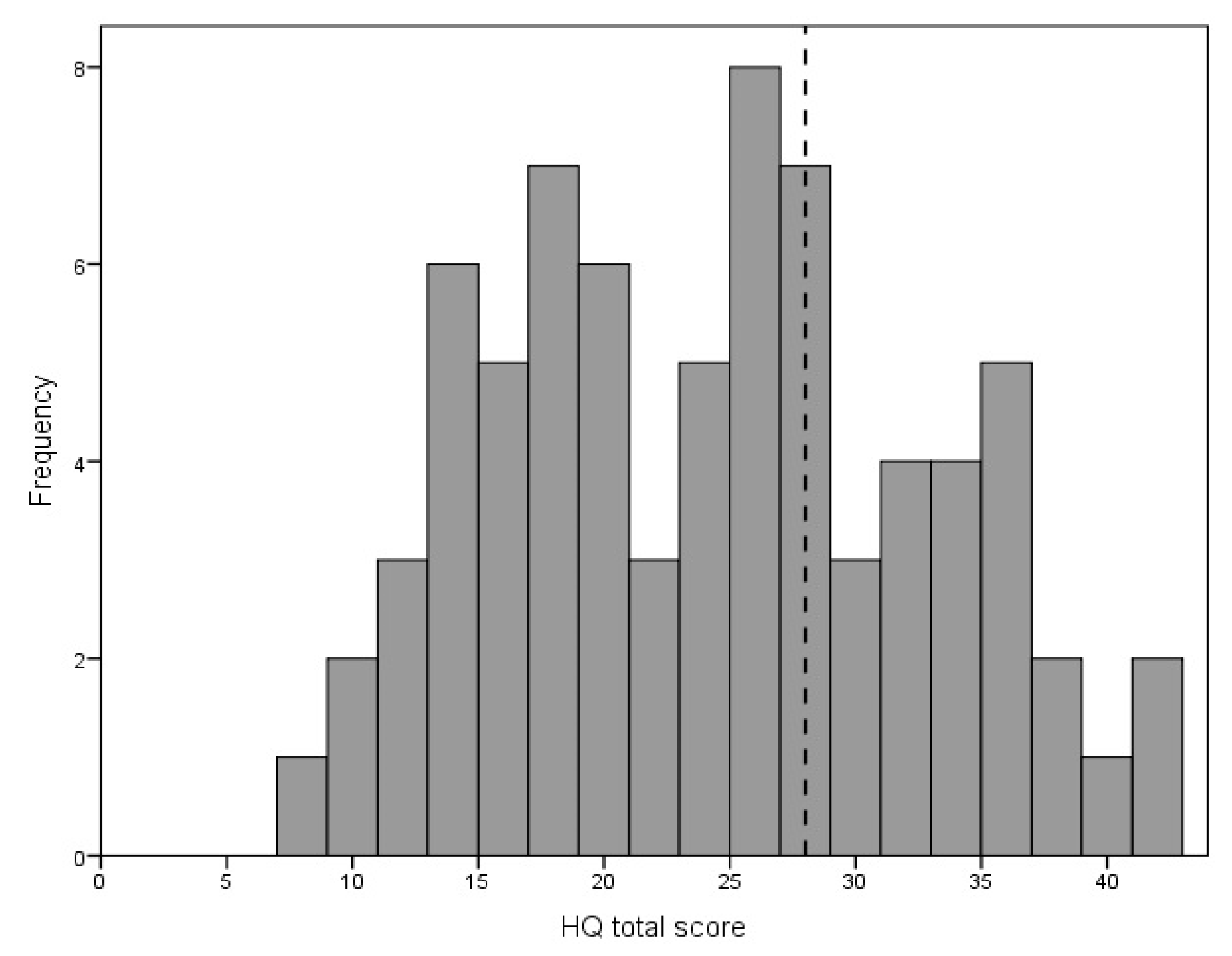
3.2.3. Hyperacusis Questionnaire
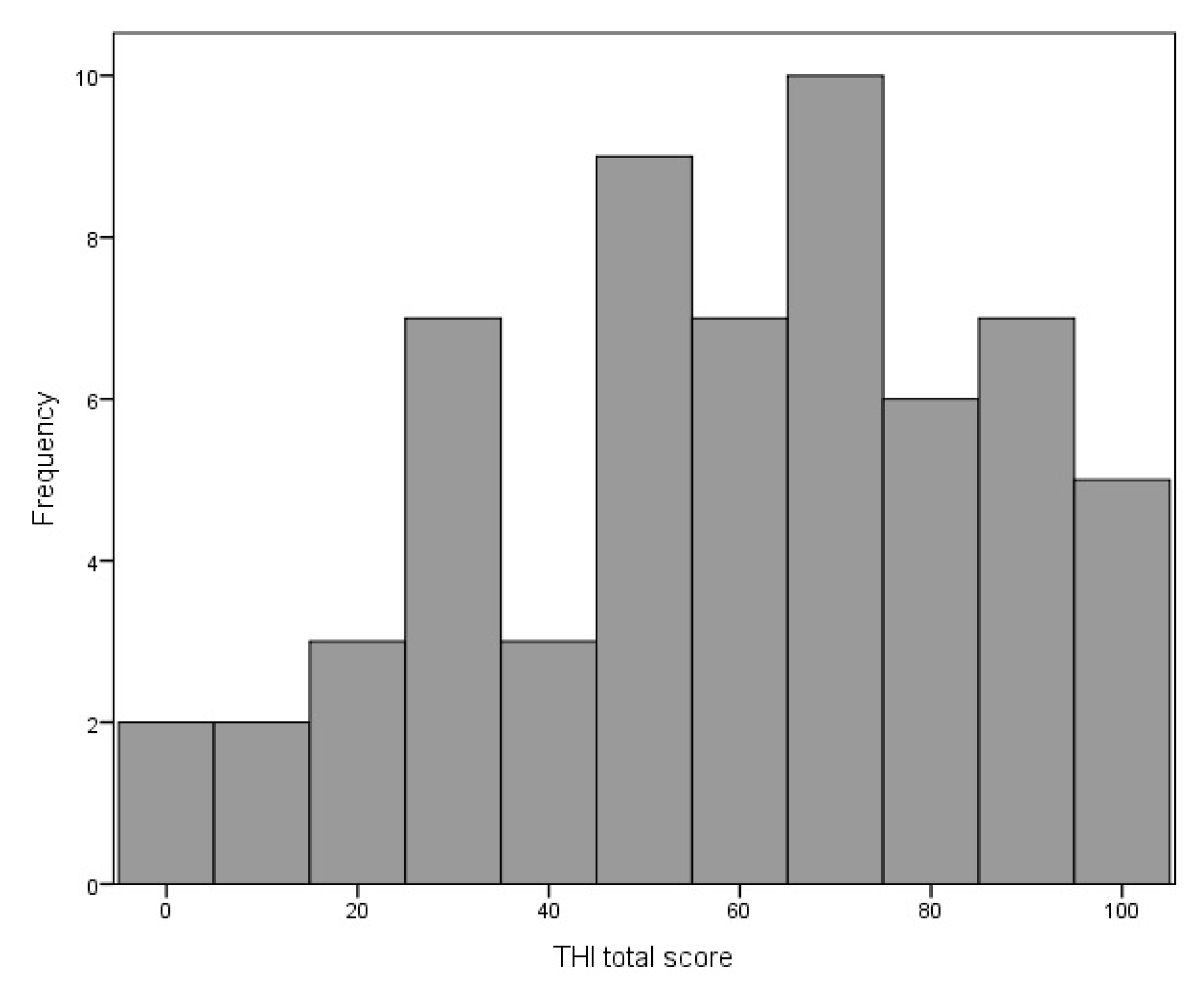
3.3. Tinnitus Assessment
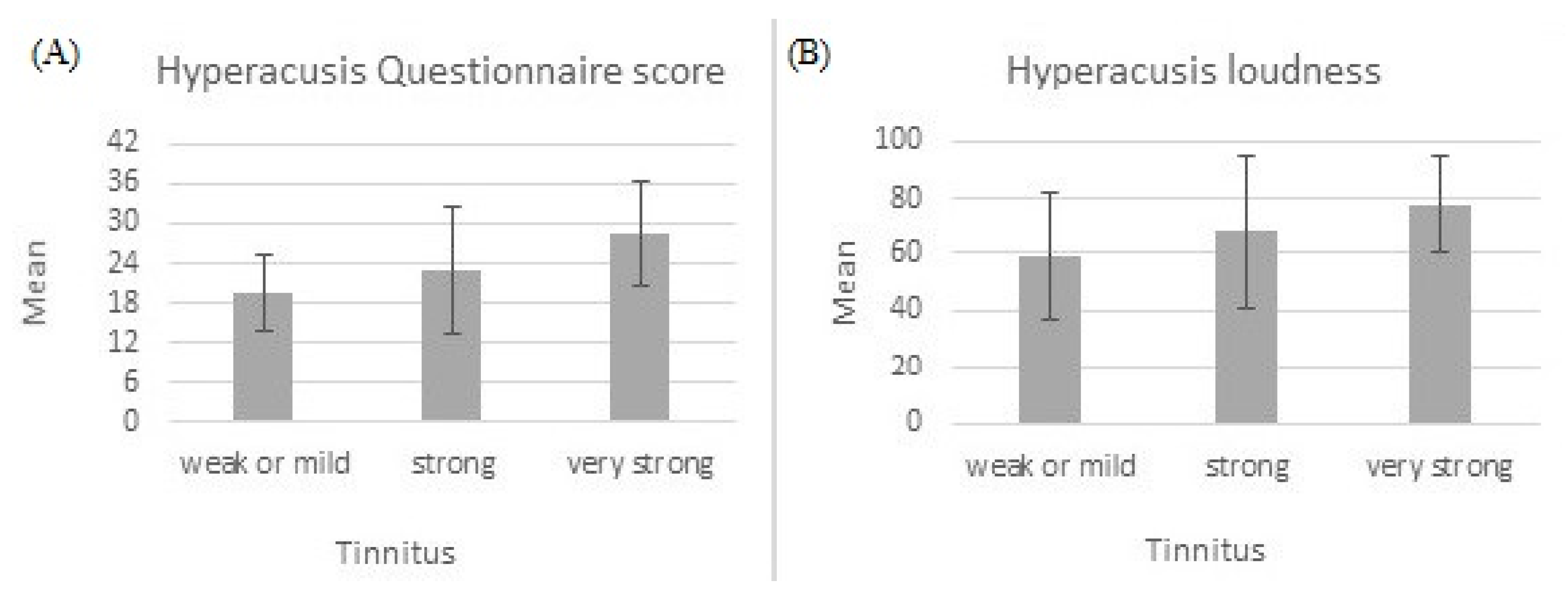
3.4. Relationship between Hyperacusis and Tinnitus
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Jastreboff, P.J.; Jastreboff, M. Decreased sound tolerance. In Tinnitus: Theory and Management; BC Decker, Inc.: Hamilton, ON, Canada, 2004; pp. 8–15. [Google Scholar]
- Jastreboff, P.J.; Jastreboff, M. Using TRT to Treat Hyperacusis, Misophonia and Phonophobia. ENT Audiol. News 2013, 21, 88–90. [Google Scholar]
- Jastreboff, P.J.; Jastreboff, M. Decreased sound tolerance: Hyperacusis, misophonia, diplacousis, and polyacousis. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2015; pp. 375–387. [Google Scholar]
- Theodoroff, S.M.; Reavis, K.M.; Griest, S.E.; Carlson, K.F.; Hammill, T.L.; Henry, J.A. Decreased Sound Tolerance Associated with Blast Exposure. Sci. Rep. 2019, 9, 10204. [Google Scholar] [CrossRef] [PubMed]
- Tyler, R.S.; Pienkowski, M.; Roncancio, E.R.; Jun, H.J.; Brozoski, T.; Dauman, N.; Dauman, N.; Andersson, G.; Keiner, A.J.; Cacace, A.T.; et al. A Review of Hyperacusis and Future Directions: Part I. Definitions and Manifestations. Am. J. Audiol. 2014, 23, 402–419. [Google Scholar] [CrossRef]
- Edelstein, M.; Brang, D.; Rouw, R.; Ramachandran, V.S. Misophonia: Physiological Investigations and Case Descriptions. Front. Hum. Neurosci. 2013, 7, 296. [Google Scholar] [CrossRef] [PubMed]
- Schröder, A.; Vulink, N.; Denys, D. Misophonia: Diagnostic Criteria for a New Psychiatric Disorder. PLoS ONE 2013, 8, e54706. [Google Scholar] [CrossRef]
- McKay, D.; Kim, S.-K.; Mancusi, L.; Storch, E.A.; Spankovich, C. Profile Analysis of Psychological Symptoms Associated With Misophonia: A Community Sample. Behav. Ther. 2018, 49, 286–294. [Google Scholar] [CrossRef]
- Rouw, R.; Erfanian, M. A Large-Scale Study of Misophonia. J. Clin. Psychol. 2018, 74, 453–479. [Google Scholar] [CrossRef]
- Fabijańska, A.; Rogowski, M.; Bartnik, G.; Skarzynski, H. Epidemiology of Tinnitus and Hyperacusis in Poland; The Tinnitus and Hyperacusis Centre: London, UK, 1999; pp. 569–571. [Google Scholar]
- Fabijńska, A.; Rgowski, M.; Bartnik, G.; Skarzynski, H. Program Badań Epidemiologicznych Nad Występowaniem Szumów i Nadwrażliwości Słuchowej w Polsce. Nowa Audiofonologia 1999, 13, 261–266. [Google Scholar]
- Andersson, G.; Lindvall, N.; Hursti, T.; Carlbring, P. Hypersensitivity to Sound (Hyperacusis): A Prevalence Study Conducted via the Internet and Post. Int. J. Audiol. 2002, 41, 545–554. [Google Scholar] [CrossRef]
- Hannula, S.; Bloigu, R.; Majamaa, K.; Sorri, M.; Mäki-Torkko, E. Self-Reported Hearing Problems among Older Adults: Prevalence and Comparison to Measured Hearing Impairment. J. Am. Acad. Audiol. 2011, 22, 550–559. [Google Scholar] [CrossRef]
- Paulin, J.; Andersson, L.; Nordin, S. Characteristics of Hyperacusis in the General Population. Noise Health 2016, 18, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Khalfa, S.; Dubal, S.; Veuillet, E.; Perez-Diaz, F.; Jouvent, R.; Collet, L. Psychometric Normalization of a Hyperacusis Questionnaire. ORL J. Otorhinolaryngol. Relat. Spec. 2002, 64, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Sherlock, L.P.; Formby, C. Estimates of Loudness, Loudness Discomfort, and the Auditory Dynamic Range: Normative Estimates, Comparison of Procedures, and Test-Retest Reliability. J. Am. Acad. Audiol. 2005, 16, 85–100. [Google Scholar] [CrossRef] [PubMed]
- Davis, A.; Refaie, A. Epidemiology of tinnitus. In Tinnitus Handbook; Singular Publishing Group: San Diego, CA, USA, 2000; pp. 1–23. [Google Scholar]
- Dobbie, R. Overview: Suffering from tinnitus. In Tinnitus: Theory and Management; BC Decker Inc.: Lewiston, NY, USA, 2004; pp. 1–7. [Google Scholar]
- Dauman, R.; Tyler, R.S. Some Considerations on the Classification of Tinnitus. In Tinnitus 91, Proceedings of the Fourth International Tinnitus Seminar, Amsterdam, The Netherlands, 1992; Aran, J.M., Dauman, R., Eds.; Kugler & Ghedini Publications: Amsterdam, The Netherlands, 1992; pp. 225–229. [Google Scholar]
- Tyler, R.S.; Conrad-Armes, D. The Determination of Tinnitus Loudness Considering the Effects of Recruitment. J. Speech Lang. Hear. Res. 1983, 26, 59–72. [Google Scholar] [CrossRef] [PubMed]
- Anari, M.; Axelsson, A.; Eliasson, A.; Magnusson, L. Hypersensitivity to Sound--Questionnaire Data, Audiometry and Classification. Scand. Audiol. 1999, 28, 219–230. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.S.; Lewin, A.B.; Murphy, T.K.; Storch, E.A. Misophonia: Incidence, Phenomenology, and Clinical Correlates in an Undergraduate Student Sample. J. Clin. Psychol. 2014, 70, 994–1007. [Google Scholar] [CrossRef]
- Zhou, X.; Wu, M.S.; Storch, E.A. Misophonia Symptoms among Chinese University Students: Incidence, Associated Impairment, and Clinical Correlates. J. Obs.-Compuls. Relat. Disord. 2017, 14, 7–12. [Google Scholar] [CrossRef]
- Newman, C.W.; Jacobson, G.P.; Spitzer, J.B. Development of the Tinnitus Handicap Inventory. Arch. Otolaryngol. Head Neck Surg. 1996, 122, 143–148. [Google Scholar] [CrossRef]
- Cima, R.F.F.; Mazurek, B.; Haider, H.; Kikidis, D.; Lapira, A.; Noreña, A.; Hoare, D.J. A Multidisciplinary European Guideline for Tinnitus: Diagnostics, Assessment, and Treatment. HNO 2019, 67, 10–42. [Google Scholar] [CrossRef]
- Skarżyński, P.H.; Rajchel, J.J.; Gos, E.; Dziendziel, B.; Kutyba, J.; Bieńkowska, K.; Świerniak, W.; Gocel, M.; Raj-Koziak, D.; Włodarczyk, E.A.; et al. A Revised Grading System for the Tinnitus Handicap Inventory Based on a Large Clinical Population. Int. J. Audiol. 2020, 59, 61–67. [Google Scholar] [CrossRef]
- Sheldrake, J.; Diehl, P.U.; Schaette, R. Audiometric Characteristics of Hyperacusis Patients. Front. Neurol. 2015, 6, 105. [Google Scholar] [CrossRef] [PubMed]
- Aazh, H.; Moore, B.C.J. Factors Related to Uncomfortable Loudness Levels for Patients Seen in a Tinnitus and Hyperacusis Clinic. Int. J. Audiol. 2017, 56, 793–800. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, T.G.; Moraes, F.; Casseb, J.; Cota, J.; Freire, K.; Roberts, L.E. Tinnitus Is Associated with Reduced Sound Level Tolerance in Adolescents with Normal Audiograms and Otoacoustic Emissions. Sci. Rep. 2016, 6, 27109. [Google Scholar] [CrossRef] [PubMed]
- Fackrell, K.; Fearnley, C.; Hoare, D.J.; Sereda, M. Hyperacusis Questionnaire as a Tool for Measuring Hypersensitivity to Sound in a Tinnitus Research Population. Biomed. Res. Int. 2015, 2015, 290425. [Google Scholar] [CrossRef] [PubMed]
- Raj-Koziak, D.; Gos, E.; Swierniak, W.; Rajchel, J.J.; Karpiesz, L.; Niedzialek, I.; Wlodarczyk, E.; Skarzynski, H.; Skarzynski, P.H. Visual Analogue Scales as a Tool for Initial Assessment of Tinnitus Severity: Psychometric Evaluation in a Clinical Population. Audiol Neurootol 2018, 23, 229–237. [Google Scholar] [CrossRef]
- Schecklmann, M.; Lehner, A.; Schlee, W.; Vielsmeier, V.; Landgrebe, M.; Langguth, B. Validation of Screening Questions for Hyperacusis in Chronic Tinnitus. Biomed Res Int 2015, 2015, 191479. [Google Scholar] [CrossRef]
- Gilles, A.; Goelen, S.; Van de Heyning, P. Tinnitus: A Cross-Sectional Study on the Audiologic Characteristics. Otol. Neurotol. 2014, 35, 401–406. [Google Scholar] [CrossRef]
- Cederroth, C.R.; Lugo, A.; Edvall, N.K.; Lazar, A.; Lopez-Escamez, J.-A.; Bulla, J.; Uhlen, I.; Hoare, D.J.; Baguley, D.M.; Canlon, B.; et al. Association between Hyperacusis and Tinnitus. J. Clin. Med. 2020, 9, 2412. [Google Scholar] [CrossRef]
- Jastreboff, P.; Jastreboff, M. Decreased Sound Tolerance and Tinnitus Retraining Therapy (TRT). Aust. N. Z. J. Audiol. 2002, 24, 74–84. [Google Scholar] [CrossRef]
| Hz | Min | Max | M | SD | |
|---|---|---|---|---|---|
| 1000 | 20 | 105 | 74.04 | 18.55 | |
| Right ear | 2000 | 25 | 110 | 73.75 | 18.25 |
| 4000 | 25 | 120 | 76.91 | 19.83 | |
| 1000 | 25 | 120 | 74.85 | 18.87 | |
| Left ear | 2000 | 20 | 115 | 73.82 | 18.55 |
| 4000 | 25 | 120 | 76.54 | 19.67 |
| VAS | Min | Max | M | SD |
|---|---|---|---|---|
| Loudness | 10 | 100 | 69.99 | 23.11 |
| Pain | 0 | 100 | 47.59 | 32.43 |
| Fear | 4 | 100 | 64.00 | 28.79 |
| Misophonia | 0 | 100 | 38.55 | 34.28 |
| Item | Item Content | Frequency of Responses for Items (%) | M | SD | |||
|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | ||||
| 1 | Use earplugs/earmuffs to reduce noise perception | 28.8 | 37.0 | 12.3 | 21.9 | 1.27 | 1.11 |
| 2 | Harder to ignore sounds | 11.0 | 39.7 | 28.8 | 20.5 | 1.59 | 0.94 |
| 3 | Trouble reading in noise | 4.1 | 25.7 | 27.0 | 43.2 | 2.09 | 0.92 |
| 4 | Trouble concentrating in noise | 2.7 | 18.9 | 37.8 | 40.5 | 2.16 | 0.83 |
| 5 | Difficulty listening to conversation in noise | 6.8 | 23.3 | 30.1 | 39.7 | 2.03 | 0.96 |
| 6 | Has anyone told you that you tolerate noise badly | 31.5 | 41.1 | 12.3 | 15.1 | 1.11 | 1.02 |
| 7 | Particularly sensitive to street noise | 16.2 | 32.4 | 21.6 | 29.7 | 1.65 | 1.08 |
| 8 | Noise unpleasant in certain situations | 6.8 | 21.6 | 23.0 | 48.6 | 2.14 | 0.98 |
| 9 | Anticipate noise before going out | 27.0 | 31.1 | 10.8 | 31.1 | 1.46 | 1.20 |
| 10 | Turn down invitation because of noise | 27.0 | 44.6 | 9.5 | 18.9 | 1.20 | 1.05 |
| 11 | Noise bothers more in a quiet place | 7.2 | 46.4 | 23.2 | 23.2 | 1.62 | 0.93 |
| 12 | Stress reduces ability to concentrate in noise | 10.8 | 28.4 | 27.0 | 33.8 | 1.84 | 1.02 |
| 13 | Less able to concentrate in noise at end of the day | 12.2 | 37.8 | 20.3 | 29.7 | 1.68 | 1.04 |
| 14 | Noise causes stress | 2.7 | 28.4 | 24.3 | 44.6 | 2.11 | 0.92 |
| VAS-L | VAS-P | VAS-F | VAS-M | THI | ULL RE | ULL LE | |
|---|---|---|---|---|---|---|---|
| HQ | 0.52 ** | 0.36 ** | 0.58 ** | 0.18 | 0.44 ** | −0.13 | −0.16 |
| VAS-L | 0.37 ** | 0.57 ** | 0.09 | 0.34 ** | −0.06 | −0.06 | |
| VAS-P | 0.39 ** | −0.06 | 0.04 | −0.04 | −0.02 | ||
| VAS-F | 0.18 | 0.37 ** | 0.06 | 0.04 | |||
| VAS-M | 0.06 | 0.10 | 0.09 | ||||
| THI | −0.24 | −0.28 * | |||||
| ULL RE | 0.81 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raj-Koziak, D.; Gos, E.; Kutyba, J.; Skarzynski, H.; Skarzynski, P.H. Decreased Sound Tolerance in Tinnitus Patients. Life 2021, 11, 87. https://doi.org/10.3390/life11020087
Raj-Koziak D, Gos E, Kutyba J, Skarzynski H, Skarzynski PH. Decreased Sound Tolerance in Tinnitus Patients. Life. 2021; 11(2):87. https://doi.org/10.3390/life11020087
Chicago/Turabian StyleRaj-Koziak, Danuta, Elżbieta Gos, Justyna Kutyba, Henryk Skarzynski, and Piotr H. Skarzynski. 2021. "Decreased Sound Tolerance in Tinnitus Patients" Life 11, no. 2: 87. https://doi.org/10.3390/life11020087
APA StyleRaj-Koziak, D., Gos, E., Kutyba, J., Skarzynski, H., & Skarzynski, P. H. (2021). Decreased Sound Tolerance in Tinnitus Patients. Life, 11(2), 87. https://doi.org/10.3390/life11020087







