Abstract
Background: Wrist immobilization is a common clinical intervention for wrist injuries; however, its repercussions on gait parameters and plantar support have not been extensively investigated. Objectives: The purpose of the study was to determine whether wrist immobilization causes alterations in foot pressure and center of gravity, considering hand dominance and visual conditions (eyes open or closed). Methods: The research experiment was conducted using the PodoPrint S4 platform. Basic descriptive statistics were calculated to summarize the variables. Additionally, in the mixed linear model (t-tests use Satterthwaite’s method) an analysis of variance for repeated measures (ANOVA-RM) was conducted for the determination of the objectives of the study. Results: This study included a total of 44 participants (29 females and 15 males), with an average age of 36.5 years (SD = 17.5). Immobilization, independent of eye condition, resulted in significant alterations in antero-posterior oscillation and in a larger plantar support area. In addition, the results suggest that the eye state significantly influences plantar support, independent of limb immobilization or dominance. Conclusions: Our findings reveal significant alterations in antero-posterior oscillation and plantar support due to immobilization, suggesting a dynamic interplay between wrist function and lower limb biomechanics.
1. Introduction
Wrist injuries, encompassing distal radius fracture (DRF), triangular fibrocartilage complex injury, instability, scaphoid fracture, and various orthopedic conditions, are commonplace in clinical practice [,]. Joint restriction constrains the ability to flexibly coordinate the joints and might lead to reduced balance stability when people perform different tasks or activities []. To promote wrist stability and facilitate the healing process, healthcare providers often employ wrist immobilization devices, such as casts or splints [,,]. The potential secondary effects of this intervention on other aspects of an individual’s biomechanics and functional mobility have received limited attention in the scientific literature.
One of the most immediate reactions to upper limb immobilization is an altered gait pattern [] to compensate for the loss of upper limb function and maintain equilibrium []. When the wrist is immobilized, there is a shift in the body’s center of mass. To counteract this shift and prevent falls, individuals may adjust their body posture and engage their core and lower limbs more actively. This adaptive response helps in stabilizing the body’s center of mass during walking [].
Ford MP et al. [] confirmed that constraining one arm resulted in an adaptation in trunk and inter-limb coordination when walking at higher velocities in healthy adults, but no specific upper limb extremity movement disorders participants have been included, and studies did not evaluate possible changes in plantar pressure distribution when there is immobilization and consequently no use of the upper limb. This potential alteration in statics could cause postural changes during daily activities that do not involve walking or any form of displacement. Arm swing is a natural component of walking that aids in balance and stability []. When upper limb function is compromised due to immobilization, there may be a compensatory reduction or modification in arm swing. Steven H. Collins et al. [] conducted a series of simulations and human subject experiments with the goal of elucidating the role of arm swinging and its underlying mechanisms in human gait.
Other investigations [,,,] have concluded that normal arm swing indeed leads to a reduced vertical angular momentum when compared to walking without arm swing. These studies emphasized the imperative to identify alterations in plantar support following wrist or hand immobilization and how these changes may impact not only the movement of the upper limbs but also plantar support. This, in turn, can affect gait cadence and balance, potentially causing challenges or modifications in movement patterns during everyday activities.
Despite the presence of various factors that may affect plantar support following wrist or hand injuries requiring immobilization, such as fear of movement, pain, or catastrophizing, the specific influence of immobilization itself on plantar support remains inconclusive, leaving the potential impact on overall functional recovery uncertain.
The first aim of the present study was to analyze the intra-subject variability in antero-posterior oscillation (APO) and plantar pressure parameters in healthy subjects during the bipedal standing test under wrist–hand dominant and non-dominant immobilization, with both open-eye (OE) and closed-eye (CE) conditions. Based on this aim, we hypothesize that (1) wrist immobilization, regardless of hand dominance, will cause significant alterations in antero-posterior oscillation and plantar pressure distribution when compared to the non-immobilized condition, (2) the effects of wrist immobilization on these parameters will vary depending on hand dominance, and (3) visual conditions (eyes open vs. closed) will significantly influence plantar pressure parameters and postural stability, regardless of wrist immobilization or hand dominance.
2. Materials and Methods
2.1. Study Design and Participants
The study was performed in the Faculty of Health Science of the University of Málaga. The study was approved by the local ethics committee with the number CEUMA: 97-2022-H and was carried out according to the Helsinki Declaration on ethical principles for research involving human subjects []. A convenience sample of 44 participants was selected during November 2022 and December 2023. Informed consent was obtained from all participants before their inclusion in the study.
The inclusion criteria were age ≥ 18 years. The exclusion criteria included cognitive or neurological impairments that could interfere with the instructions, any previously diagnosed musculoskeletal disorders, recent acute injuries (<1 year) in any limb, immobilization within the previous 6 months, and balance problems.
2.2. Procedure
Participants were recruited through an open call via social media posts to ensure a diverse and representative sample within the study’s eligibility criteria. Volunteers who expressed interest were invited to participate, provided they met the predefined inclusion criteria outlined in the study protocol. Additionally, all participants received detailed information about the study’s objectives and procedures before providing their informed consent.
Firstly, a questionnaire (designed by the authors) was provided to the participants to obtain the demographic variables, such as age, sex, occupation, physical activity, and hand dominance. The platform pressure data were collected by a researcher who was familiar with the instrument and software, and all measurements were taken by the same evaluator to avoid discrepancies.
The baropodometric measurements were carried out using a baropodometric platform called PodoPrint® S4, a reliable tool for evaluating the distribution of plantar pressures in the dynamic study of the barefoot gait of healthy individuals. The ICCs showed moderate to good repeatability (greater than 0.81 and less than 0.93) []. The dimensions of this platform are 57 cm × 57 cm × 9 mm, and it has 1600 sensors. The data were sent digitally to a computer and then processed using software that shows the parameters of plantar pressure, center of pressure, and postural sway. All measurements were taken twice to make data more precise and eliminate possible bias. Assessment was performed in a soundproof room with absolute silence and with no visual distractions. Each participant had to take off any ornaments on their wrists or objects that they had in their pockets, and they had to be barefoot (with no socks). A foot positioning template was used to position the feet at an angle of 30°, with a separation of 2 cm between heels. For every measurement, the participant had to be standing, with resting arms along the body and looking straight ahead at a color signal that was previously placed on the wall. In this position, the following data were obtained for each subject: total foot support surface, measured in cm2; average foot pressure in static support, measured in gr/cm2; body sway length and body sway area, both in static support; and center of pressures on the X-axis (COP X) and Y-axis (COP Y), which represent the position of the center of foot pressure compared to the theoretical one.
At first, a quiet stance test was performed for each subject with open eyes (OEs), followed by a second measurement with the same procedure but with closed eyes (CEs). Secondly, a posture–stabilometric test was also performed with OEs and CEs. This procedure was repeated in the same order, immobilizing the wrist of the dominant arm and then immobilizing the other wrist. Dominance was determined by asking the patient which hand they use for writing. We immobilized the wrist with a thermoplastic splint that put the wrist in a neutral position [,]. Also, the splint did not cover any fingers or elbow. If the participant coughed, sneezed, turned his/her head, talked, or performed a sudden movement, the measurements were repeated to avoid possible bias.
2.3. Data Analysis
The data were processed with R version 4.3.2 for statistical study []. The validity conditions (sphericity and normality) were checked. Mauchly tests for sphericity and Greenhouse–Geisser and Huynh–Feldt corrections for departure from sphericity. The Shapiro–Wilk test for normality was used. A mixed linear model (t-tests use Satterthwaite’s method) and an analysis of variance for repeated measures (ANOVA-RM) were conducted for the determination of the objectives of the study. Post hoc comparisons with Holm methods were used. For all statistical analyses, the significance level was set at 5%.
3. Results
This study included a total of 44 participants, composed of 29 females and 15 males, with an average age of 36.5 years (SD = 17.5). An initial exploration of the data revealed that the antero-posterior oscillation (APO) varies significantly with the state of the eyes (open vs. closed), as illustrated in Figure 1.
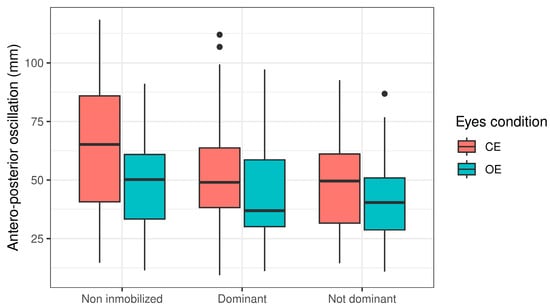
Figure 1.
Antero-posterior oscillation associated with state of eyes (open vs. closed).
Notably, immobilization alone, independent of eye condition, resulted in significant alterations in APO (p < 0.001), as detailed in Table 1.

Table 1.
Summary of the statistical significance of APO alterations due to immobilization alone.
Further analysis using an interaction model to assess the effects of eye condition (open vs. closed) separately revealed that immobilization impacts APO irrespective of eye condition (p < 0.001), without significant differences between immobilization of the dominant or non-dominant limb (Figure 2a).
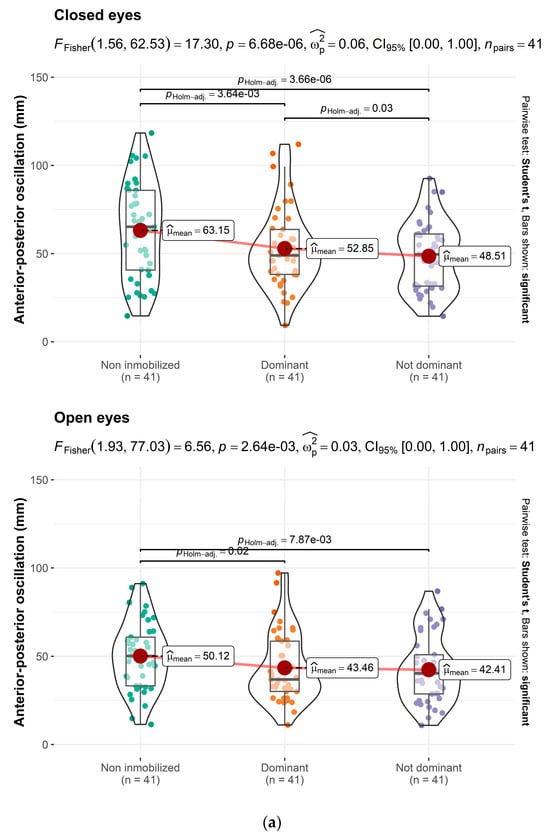
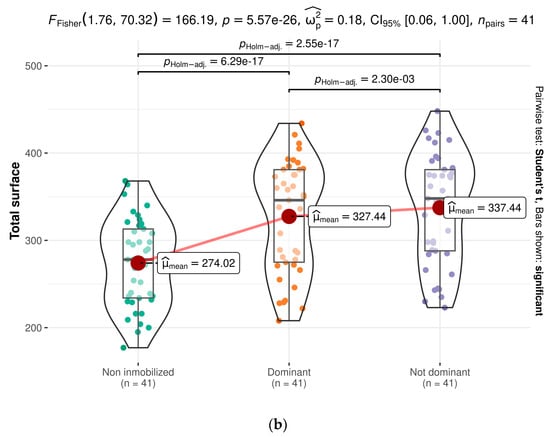
Figure 2.
(a) Immobilization impacts APO irrespective of eye condition. (b). Differences between dominant and non-dominant sides.
Table 2 presents the effects of wrist and hand immobilization on the total plantar support area. The findings indicate a larger plantar support area during immobilization compared to non-immobilization, regardless of the dominance of the immobilized limb (p < 0.001), with discernible differences between the dominant and non-dominant sides (Figure 2b).

Table 2.
Data on the impact of wrist and hand immobilization on total plantar support area.
Additionally, when disregarding immobilization and limb dominance, the impact of eye state (open vs. closed) on plantar support was evaluated. The results suggest that the eye state significantly influences plantar support, independent of limb immobilization or dominance (Table 3).

Table 3.
Exploring the effect of eye state on plantar support, disregarding immobilization and limb.
4. Discussion
Despite the importance of proprioception in long-term functional outcomes after wrist–hand immobilization [], no previous studies have examined the effect that wrist or hand immobilization may have on plantar support and, consequently, on the disruptions in the development of daily activities. Our study aimed to investigate the impact of wrist immobilization on postural control, specifically examining antero-posterior oscillation and plantar pressure distribution, while also considering the roles of hand dominance and visual conditions. In line with our hypotheses, the results revealed that wrist immobilization, regardless of hand dominance, led to significant changes in both postural sway and plantar pressure parameters when compared to the non-immobilized condition. These findings suggest that even distal upper limb constraints can influence body balance.
There are several plantar pressure measurement systems, such as Footscan® [], TekScan® [], Emed® [], Pedar® [], WalkinSense® [], and Medicapteurs S-Plate® [], among others. There have been some foot-related research studies that have used the PodoPrint® platform [,]. Reliability and repeatability of the PodoPrint® system have been demonstrated, and normal values of plantar foot pressure have also been identified in a healthy population [].
We already knew that the immobilization of the wrist or hand had consequences on the shoulder [], and increased time of immobilization of the wrist was associated with an increase in shoulder pain in patients after wrist fracture. However, we were unaware of the potential effects that immobilizing the wrist or hand could have on plantar support, gait development, balance, and consequently, on the sensation of movement and agility during locomotion. The results of this study could have clinical implications in patients with conditions involving wrist immobilization, highlighting the importance of a global rehabilitation approach. Specifically, the findings elucidated on the relationship between wrist immobilization and various postural parameters revealed not only the dynamic interplay between upper limb function and lower limb biomechanics but also the influence of wrist–hand immobilization on these parameters []. Our results indicate that wrist immobilization alone induces changes in antero-posterior oscillation (APO), regardless of whether the immobilized hand is dominant or non-dominant and independent of visual conditions (eyes open or closed). However, when the eyes are closed, the length of APO increases, likely due to the involvement of the vestibular system [].
Previous studies concluded that plantar pressure parameters can be modulated in response to different visual inputs [,]. Effects of visual stimuli on plantar pressure parameters were also reported in open-eye (OE) condition by Fullin et al. []. Similarly, P. De Blasiis et al. [] investigated the impact of visual stimuli on postural stability and plantar pressure parameters in a healthy population, analyzing changes under both OE and closed-eye (CE) conditions. Their results confirm that the coefficient of variation was lower than 20% in CEs and OEs across all parameters, except for the right arch index, which suggests a greater dynamic role of the dominant foot with respect to the postural adaptations occurring with closed eyes. Also, Hébert-Losier, K et al. [,] concluded that plantar pressure parameters do not seem to be affected by the different visual conditions. These studies partially differ from our results, as we observed differences in participants depending on whether their eyes were open or closed. This discrepancy may be attributed to wrist immobilization, a variable not considered in previous studies. Our findings suggest that eye condition (open vs. closed) significantly impacts the distribution of plantar load, regardless of limb immobilization or dominance. Nevertheless, it is important to emphasize that irrespective of the eye condition or dominance, it is the immobilization itself that induces effects on both antero-posterior oscillation and the area of plantar support.
Upper extremity limitations impact gait, balance, and overall functionality [,]. This redistribution of plantar pressure may be indicative of an attempt to redistribute body weight in response to compromised upper limb function. Our study also revealed significant changes in plantar pressure distribution in individuals due to wrist immobilization. It is conceivable that individuals with wrist immobilization, either consciously or subconsciously, engage their lower limbs to a greater extent to compensate for reduced upper limb functionality during walking, as interlimb neural coupling influences muscle recruitment []. It is not the first time that some investigators reported the correlation between the hand and the foot; for example, Slobounov, S et al. reported referred differences between the parameters of hand strength and plantar pressure distribution [,]. Other studies that have focused on postural control have shown the right hemisphere’s pivotal role on balance control and body posture in healthy subjects [,]. In the same line, Rosario Emanuele Bonaventura et al. [] investigated the effect of prismatic adaptation (PA) on handgrip strength and plantar pressure. They concluded that the PA effects on body posture are probably related to modulation of body representation.
Focus on body representation, and in concordance with our results, there are many results that converge on the conclusion that maintaining an upright posture requires the nervous system to integrate information from the somatosensory, visual, and vestibular systems. Therefore, any external factor that may influence this perception (such as wrist immobilization in our study) could impact the motor and sensory systems, leading to a series of mechanical and proprioceptive adjustments that are crucial for effective rehabilitation. These objective findings, which highlight the correlation between wrist immobilization and plantar support, could be the way for new research focused on clinical applications for upper limb injury rehabilitation.
However, our results are based on a healthy population; consequently, the impact of factors, such as kinesiophobia or post-injury wrist pain, on plantar support remains unknown. Moreover, a potential limitation of this study is the possibility of evaluator bias, as the evaluator was aware of the conditions being tested. Although efforts were made to ensure objective assessments, the lack of blinding may have introduced an unintended source of bias. Future research should address this limitation by implementing a double-blind design to enhance the reliability of the findings. Future research should integrate clinical assessments to strengthen the interpretation and clinical relevance of our findings. Additionally, further studies should explore the impact of various factors influencing plantar support following wrist immobilization, identifying both predictive and confounding variables, as well as potential changes occurring throughout the progression of the pathology.
5. Conclusions
Wrist–hand immobilization alone, independent of eye status (open or closed), resulted in significant alterations in antero-posterior oscillation and plantar pressure, with discernible differences between the dominant and non-dominant sides. The eye state significantly influenced plantar support, independent of limb immobilization or dominance.
Author Contributions
L.C.G.: conceptualization, methodology, investigation, and writing—original draft; G.A.G.-N.: validation, formal analysis, and writing—review and editing; S.D.M.: methodology, investigation, and resources; J.B.-L.: formal analysis; C.-T.R.: conceptualization, methodology, formal analysis, writing—review and editing, visualization, and supervision. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the University of Málaga with CEUMA: 97-2022-H.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Acknowledgments
The University of Malaga.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Kim, B.S.; Cho, C.H.; Lee, K.J.; Lee, S.W.; Byun, S.H. Pathomechanism of Triangular Fibrocartilage Complex Injuries in Patients with Distal-Radius Fractures: A Magnetic-Resonance Imaging Study. J. Clin. Med. 2022, 11, 6168. [Google Scholar] [CrossRef] [PubMed]
- Rundgren, J.; Bojan, A.; Mellstrand Navarro, C.; Enocson, A. Epidemiology, Classification, Treatment and Mortality of Distal Radius Fractures in Adults: An Observational Study of 23,394 Fractures from the National Swedish Fracture Register. BMC Musculoskelet. Disord. 2020, 21, 88. [Google Scholar] [CrossRef]
- Hsu, W.L. Adaptive Postural Control for Joint Immobilization during Multitask Performance. PLoS ONE 2014, 9, 108667. [Google Scholar] [CrossRef]
- Rios-Russo, J.L.; Lozada-Bado, L.S.; De Mel, S.; Frontera, W.; Micheo, W. Ulnar-Sided Wrist Pain in the Athlete: Sport-Specific Demands, Clinical Presentation, and Management Options. Curr. Sports Med. Rep. 2021, 20, 312–318. [Google Scholar] [CrossRef]
- Sprouse, R.A.; McLaughlin, A.M.; Harris, G.D. Braces and Splints for Common Musculoskeletal Conditions. Am. Fam. Physician 2018, 98, 570–576. [Google Scholar]
- Howell, D.M.; Bechmann, S.; Underwood, P.J. Wrist Splint. In Interventions, Controls, and Applications in Occupational Ergonomics; CRC Press: Boca Raton, FL, USA, 2023. [Google Scholar] [CrossRef]
- Hong, S.H.; Jung, S.Y.; Oh, H.K.; Lee, S.H.; Woo, Y.K. Effects of the Immobilization of the Upper Extremities on Spatiotemporal Gait Parameters during Walking in Stroke Patients: A Preliminary Study. Biomed. Res. Int. 2020, 2020, 6157231. [Google Scholar] [CrossRef]
- Cooper, J.E.; Shwedyk, E.; Quanbury, A.O.; Miller, J.; Hildebrand, D. Elbow Joint Restriction: Effect on Functional Upper Limb Motion during Performance of Three Feeding Activities. Arch. Phys. Med. Rehabil. 1993, 74, 805–809. [Google Scholar] [CrossRef] [PubMed]
- Boström, K.J.; Dirksen, T.; Zentgraf, K.; Wagner, H. The Contribution of Upper Body Movements to Dynamic Balance Regulation during Challenged Locomotion. Front. Hum. Neurosci. 2018, 12, 8. [Google Scholar] [CrossRef]
- Ford, M.P.; Wagenaar, R.C.; Newell, K.M. Arm Constraint and Walking in Healthy Adults. Gait Posture 2007, 26, 135–141. [Google Scholar] [CrossRef]
- Collins, S.H.; Adamczyk, P.G.; Kuo, A.D. Dynamic Arm Swinging in Human Walking. Proc. Biol. Sci. 2009, 276, 3679–3688. [Google Scholar] [CrossRef]
- Umberger, B.R. Effects of Suppressing Arm Swing on Kinematics, Kinetics, and Energetics of Human Walking. J. Biomech. 2008, 41, 2575–2580. [Google Scholar] [CrossRef]
- Ortega, J.D.; Fehlman, L.A.; Farley, C.T. Effects of Aging and Arm Swing on the Metabolic Cost of Stability in Human Walking. J. Biomech. 2008, 41, 3303–3308. [Google Scholar] [CrossRef] [PubMed]
- De Graaf, M.L.; Hubert, J.; Houdijk, H.; Bruijn, S.M. Influence of Arm Swing on Cost of Transport during Walking. Biol. Open 2019, 8, bio039263. [Google Scholar] [CrossRef]
- Manzini, J.L. DECLARACIÓN DE HELSINKI: PRINCIPIOS ÉTICOS PARA LA INVESTIGACIÓN MÉDICA SOBRE SUJETOS HUMANOS. Acta Bioethica 2000, 6, 321–334. [Google Scholar] [CrossRef]
- Cobos-Moreno, P.; Astasio-Picado, Á.; Martínez- Nova, A.; Sánchez- Rodríguez, R.; Escamilla-Martínez, E.; Gómez-Martín, B. The Podoprint® Plantar Pressure Platform: Evaluation of Reliability and Repeatability, and Determination of the Normality Parameters. J. Tissue Viability 2022, 31, 619–624. [Google Scholar] [CrossRef] [PubMed]
- Sayudo, I.F.; Sudarman, J.P.; Fernandes, A.; Park, J.Y.; Leibovitch, L.; Machinski, E.; Mahmoud, M.O. Short Versus Regular Periods of Cast Immobilization for Distal Radial Fractures: A Systematic Review and Meta-Analysis. Cureus 2024, 16, e54704. [Google Scholar] [CrossRef] [PubMed]
- de Bruijn, M.A.N.; van Ginkel, L.A.; Boersma, E.Z.; van Silfhout, L.; Tromp, T.N.; van de Krol, E.; Edwards, M.J.R.; Stirler, V.M.A.; Hermans, E. Cast Immobilization Duration for Distal Radius Fractures, a Systematic Review. Eur. J. Trauma. Emerg. Surg. 2024, 50, 1621–1636. [Google Scholar] [CrossRef]
- Patil, I. Visualizations with Statistical Details: The “ggstatsplot” Approach. J. Open Source Softw. 2021, 6, 3167. [Google Scholar] [CrossRef]
- Cantero-Téllez, R. A Global Proprioception Concept after Hand Injury-Patient Report. J. Hand Ther. 2024, 37, 293–295. [Google Scholar] [CrossRef]
- Xu, C.; Wen, X.X.; Huang, L.Y.; Shang, L.; Cheng, X.X.; Yan, Y.B.; Lei, W. Normal Foot Loading Parameters and Repeatability of the Footscan® Platform System. J. Foot Ankle Res. 2017, 10, 30. [Google Scholar] [CrossRef]
- Zammit, G.V.; Menz, H.B.; Munteanu, S.E. Reliability of the TekScan MatScan® System for the Measurement of Plantar Forces and Pressures during Barefoot Level Walking in Healthy Adults. J. Foot Ankle Res. 2010, 3, 11. [Google Scholar] [CrossRef] [PubMed]
- Maetzler, M.; Bochdansky, T.; Abboud, R.J. Normal Pressure Values and Repeatability of the Emed® ST2 System. Gait Posture 2010, 32, 391–394. [Google Scholar] [CrossRef] [PubMed]
- Ramanathan, A.K.; Kiran, P.; Arnold, G.P.; Wang, W.; Abboud, R.J. Repeatability of the Pedar-X® in-Shoe Pressure Measuring System. Foot Ankle Surg. 2010, 16, 70–73. [Google Scholar] [CrossRef]
- Castro, M.P.D.; Meucci, M.; Soares, D.P.; Fonseca, P.; Borgonovo-Santos, M.; Sousa, F.; Machado, L.; Vilas-Boas, J.P. Accuracy and Repeatability of the Gait Analysis by the WalkinSense System. Biomed. Res. Int. 2014, 2014, 348659. [Google Scholar] [CrossRef]
- Izquierdo-Renau, M.; Pérez-Soriano, P.; Ribas-García, V.; Queralt, A. Intra and Intersession Repeatability and Reliability of the S-Plate® Pressure Platform. Gait Posture 2017, 52, 224–226. [Google Scholar] [CrossRef]
- Sánchez-Sáez, J.M.; Palomo-López, P.; Becerro-De-bengoa-vallejo, R.; Calvo-Lobo, C.; Losa-Iglesias, M.E.; López-Del-amo-lorente, A.; López-López, D. Stability of Three Different Sanitary Shoes on Healthcare Workers: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 16, 2126. [Google Scholar] [CrossRef]
- Pereiro-Buceta, H.; Calvo-Lobo, C.; Becerro-De-bengoa-vallejo, R.; Losa-Iglesias, M.E.; Romero-Morales, C.; López-López, D.; Martínez-Jiménez, E.M. Intra and Intersession Repeatability and Reliability of Dynamic Parameters in Pressure Platform Assessments on Subjects with Simulated Leg Length Discrepancy. A Cross-Sectional Research. Sao Paulo Med. J. 2021, 139, 424–434. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, R.B.; Gentile, A.M. Sit-to-Stand: Functional Relationship between Upper Body and Lower Limb Segments. Hum. Mov. Sci. 1994, 13, 817–840. [Google Scholar] [CrossRef]
- Cantero-Téllez, R.; Orza, S.G.; Bishop, M.D.; Berjano, P.; Villafañe, J.H. Duration of Wrist Immobilization Is Associated with Shoulder Pain in Patients with after Wrist Immobilization: An Observational Study. J. Exerc. Rehabil. 2018, 14, 694–698. [Google Scholar] [CrossRef]
- Nishiike, S.; Okazaki, S.; Watanabe, H.; Akizuki, H.; Imai, T.; Uno, A.; Kitahara, T.; Horii, A.; Takeda, N.; Inohara, H. The Effect of Visual-Vestibulosomatosensory Conflict Induced by Virtual Reality on Postural Stability in Humans. J. Med. Investig. 2013, 60, 236–239. [Google Scholar] [CrossRef]
- Stoffregen, T.A.; Pagulayan, R.J.; Bardy, B.G.; Hettinger, L.J. Modulating Postural Control to Facilitate Visual Performance. Hum. Mov. Sci. 2000, 19, 203–220. [Google Scholar] [CrossRef]
- Fullin, A.; Caravaggi, P.; Picerno, P.; Mosca, M.; Caravelli, S.; De Luca, A.; Lucariello, A.; De Blasiis, P. Variability of Postural Stability and Plantar Pressure Parameters in Healthy Subjects Evaluated by a Novel Pressure Plate. Int. J. Environ. Res. Public Health 2022, 19, 2913. [Google Scholar] [CrossRef]
- De Blasiis, P.; Caravaggi, P.; Fullin, A.; Leardini, A.; Lucariello, A.; Perna, A.; Guerra, G.; De Luca, A. Postural Stability and Plantar Pressure Parameters in Healthy Subjects: Variability, Correlation Analysis and Differences under Open and Closed Eye Conditions. Front. Bioeng. Biotechnol. 2023, 11, 1198120. [Google Scholar] [CrossRef]
- Hébert-Losier, K.; Murray, L. Reliability of Centre of Pressure, Plantar Pressure, and Plantar-Flexion Isometric Strength Measures: A Systematic Review. Gait Posture 2020, 75, 46–62. [Google Scholar] [CrossRef]
- Trehan, S.K.; Wolff, A.L.; Gibbons, M.; Hillstrom, H.J.; Daluiski, A. The Effect of Simulated Elbow Contracture on Temporal and Distance Gait Parameters. Gait Posture 2015, 41, 791–794. [Google Scholar] [CrossRef]
- Leblebici, G.; Tarakcı, E.; Kısa, E.P.; Akalan, E.; Kasapçopur, Ö. The Effects of Improvement in Upper Extremity Function on Gait and Balance in Children with Upper Extremity Affected. Gait Posture 2024, 110, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Slobounov, S.; Hallett, M.; Stanhope, S.; Shibasaki, H. Role of Cerebral Cortex in Human Postural Control: An EEG Study. Clin. Neurophysiol. 2005, 116, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Siemionow, V.; Yue, G.H.; Ranganathan, V.K.; Liu, J.Z.; Sahgal, V. Relationship between Motor Activity-Related Cortical Potential and Voluntary Muscle Activation. Exp. Brain Res. 2000, 133, 303–311. [Google Scholar] [CrossRef]
- Cioncoloni, D.; Rosignoli, D.; Feurra, M.; Rossi, S.; Bonifazi, M.; Rossi, A.; Mazzocchio, R. Role of Brain Hemispheric Dominance in Anticipatory Postural Control Strategies. Exp. Brain Res. 2016, 234, 1997–2005. [Google Scholar] [CrossRef]
- Zhavoronkova, L.A.; Zharikova, A.V.; Kushnir, E.M.; Mikhalkova, A.A. EEG Markers of Upright Posture in Healthy Individuals. Hum. Physiol. 2012, 38, 604–612. [Google Scholar] [CrossRef]
- Bonaventura, R.E.; Giustino, V.; Chiaramonte, G.; Giustiniani, A.; Smirni, D.; Battaglia, G.; Messina, G.; Oliveri, M. Investigating Prismatic Adaptation Effects in Handgrip Strength and in Plantar Pressure in Healthy Subjects. Gait Posture 2020, 76, 264–269. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).