Abstract
Background: Improving food and nutrition literacy is fundamental to tackling the Middle East and North Africa (MENA) region’s enormous challenges, including malnutrition and food insecurity. To direct initiatives, it is crucial to assess the region’s food and nutrition literacy. Thus, we aimed to review studies on food/nutrition literacy status in the MENA countries and illuminate the region’s research gaps in these areas, in terms of assessment, policy, and program implementation. Methods: PubMed and Google Scholar databases were searched between 18 December and 8 May 2022, to identify relevant articles published up to 2022 in the MENA region. Results: Twelve studies were included in this review. Lebanon, Palestine, and Iran are the only three MENA countries where nutrition and/or food literacy were assessed. People in these countries mostly had inadequate food and/or nutrition literacy levels, especially in the skills rather than the cognitive domain. Food and/or nutrition literacy showed associations with food habits, food-label use, food-consumption patterns, school performance, food security, dietary diversity, and nutrient adequacy. The MENA countries developed no policies or programs to address food and nutrition literacy. Conclusion: This review is a wake-up call for researchers and policymakers to develop a robust approach to combat food and nutrition literacy concerns in the MENA region.
Keywords:
food literacy; nutrition literacy; MENA; malnutrition; food insecurity; researchers; policymakers 1. Introduction
1.1. Malnutrition and Food Insecurity Burden in the MENA Region
The triple burden of malnutrition and anemia along with the coexistence of food insecurity are tremendous challenges in the MENA region []. With ongoing conflicts, political instability, and the COVID-19 pandemic, the region is witnessing an unprecedented increase in food insecurity, a decline in dietary diversity [], the adoption of unhealthy eating patterns, and changes in food literacy []. In addition, the ongoing conflict in Ukraine, since February 2022, is compounding the impacts of two long years of the COVID-19 pandemic on economies, food insecurity, poverty, and malnutrition in the MENA region []. It is expected that the number of people affected by hunger in the region will surpass 75 million by 2030 []. Recent estimates show that more than 7 million children in the region suffer from chronic malnutrition, manifested as stunting []. Besides, 3.7 million children have acute malnutrition, of which 1.6 million are severely wasted []. The average prevalence of overweight and obesity was 27% and 24% in adults and 16.5% and 4.8% in school-aged children, respectively []. Besides, anemia prevalence in the region ranged between 22.6% and 63% amongst pregnant women, 27% and 69.6% amongst women of reproductive age, and 23.8% and 83.5% amongst under-five children []. Added to these, MENA’s share of the world’s acutely food-insecure people was 20%, which is considered high for its 6% share of the population []. Hence, to overcome these challenges, the MENA countries should re-prioritize and reform inefficacious practices and food-related policies towards “high-return nutrition investment” that amplifies the availability of and the access to nutritious foods []. Furthermore, the reform of incompetent food-related practices and policies offers resources that can be used to ramp-up well-targeted educational, social, behavioral, nutritional, and health-related outcomes []. These outcomes are needed to transform and enhance the resilience of the region’s food systems, to increase the capacity to ensure safe, healthy, and sustainable diets []. To achieve Zero Hunger by 2030, it is crucial to transform Arab food systems to end hunger and malnutrition []. Thus, some various elements should be the focus of intervention. These include nutrition knowledge and attitudes, food and cooking skills, food environment, food preferences, and food literacy []. Being food literate is crucial to help people make healthy food choices that ensure nutritional needs are met []. “Food literacy is particularly important in the early years, when children are developing the eating patterns and skills that they will carry into adulthood and pass on to future generations” [].
1.2. Existing Definitions of Food Literacy and Nutrition Literacy
The term “food literacy” has gained momentum in recent years, being evolved from the broader concept of health literacy []. Researchers will continue to debate the definition of food literacy for many years until it becomes a rich study area []. Food literacy is defined as the ability to make appropriate food decisions to support individual health and a sustainable food system, considering environmental, social, economic, cultural, and political contexts []. Food and nutrition knowledge, food skills, self-efficacy and confidence, food decisions, and multiple environmental factors, particularly the food system, are all food literacy attributes, according to the Food Literacy Framework for Healthy Eating []. Widener, P. and Karides, M. (2014) [] further suggested the term “system food literacy”, implying that food literacy entails a thorough understanding of the food system and its social and economic issues. Besides, the components of functional (comprehend and understand information), interactive (share and exchange information and interact with others), and critical (evaluate and judge information) literacy presented by Nutbeam’s tripartite model [] are reflected in worldwide food-literacy definitions.
Similar to food literacy, nutrition literacy is under the umbrella of health literacy []. It is considered “a health literacy applied to the field of nutrition” []. The nutritionally literate individual is one who can obtain, process, and understand basic nutrition information necessary for making appropriate nutrition decisions []; however, food literacy is incorporated into a broader spectrum of theoretical and practical knowledge and skills []. In other words, the skills incorporated in nutrition literacy are prerequisites for food-literacy competencies []. Nevertheless, they do not represent the whole spectrum of skills and competencies needed to perform well in making healthy and right food decisions []. Food and nutrition literacy are distinct but complementary concepts, as they are not debated as freestanding terms []. Food-literacy and nutrition-literacy definitions have not been originated by Arab authors yet, indicating that these topics are undervalued in the region. The definitions of food literacy and nutrition literacy over the years are summarized in Table 1.

Table 1.
Summary of definitions of food literacy and nutrition literacy over the years.
1.3. Food and Nutrition Literacy and Nutrition Outcomes
Promoting food and nutrition literacy is a determinant factor in leading to healthy food choices and the adoption of healthy diets by children and adolescents, in particular []. Plenty of evidence shows that adequate levels of food and nutrition literacy are positively associated with food selection, food preparation, eating habits, and diet quality []. For instance, a higher level of food and nutrition literacy has been associated with increased consumption of fruits and vegetables [], preference for healthy food [], and decreased consumption of prepacked or processed food []. Besides, having limited food skills was shown to be associated with increased consumption of ultra-processed foods []. Above these, inadequate food literacy had exacerbated food insecurity by impeding adequate food utilization []. Though evidence demonstrating the relationship between nutrition outcomes and food and nutrition literacy is still developing, the foregoing findings suggest that food- and nutrition-literacy-based interventions in the MENA region are extremely promising.
1.4. Rationale of the Study and Study Objectives
As outlined above, in order to address the region’s emerging challenges, it is necessary to adopt a package of intervention measures, focused on improving food and nutrition literacy and guided by a thorough analysis of the region’s nutrition situation, especially in the critical stages of life, such as childhood and adolescence. In fact, inadequate nutrition in childhood and adolescence can potentially retard growth []. Equipping people with adequate nutrition knowledge and food skills is one promising approach to reducing MENA’s malnutrition and food-insecurity burden [,,]. In light of this, and in order to direct initiatives, additional information about the state of food literacy and nutrition literacy in the MENA region is needed. Therefore, in this paper, we aimed to:
- Review studies on the food-literacy and nutrition-literacy status in the MENA countries.
- Illuminate the region’s current research gaps in these areas, in terms of assessment, policy, and program implementation.
2. Methods
Search Strategy and Data Extraction
We conducted an extensive review of the literature on studies on the assessment of food literacy and nutrition literacy in the MENA countries published up to 2022 using the online databases: PubMed and Google Scholar. We also hand-searched for the relevant literature using snowballing by accessing reference lists to identify additional papers. The following search terms were used: “food literacy”; “nutrition literacy”; “MENA region”; “MENA countries” “Lebanon”; “Egypt”; “Saudi Arabia”; “United Arab Emirates”; “Qatar”; “Morocco”; “Jordan”; “Bahrain”; “Oman”; “Tunisia”; “Kuwait”; “Palestine”; “Iraq”; “Syria”; “Libya”;” Algeria”; “Iran”; “Yemen”. These keywords were chosen by referring to the latest classification of the MENA countries according to the Office of the United States Trade Representative (USTR) [], which are presently the 18 countries listed above. The keywords were used in various combinations to find relevant articles. This search was performed between 18 December and 8 May 2022. Filters and limits included (in PubMed database) the English language and the human species to avoid irrelevant searches. The reviewers screened the title and abstract of the citations to highlight the suitable articles relevant to the objective of the review for further inclusion. Eligible studies included those that assessed food literacy and/or nutrition literacy in any MENA country, used a cross-sectional design, and included healthy participants of any age. For those articles that appeared relevant, the full-text study report was obtained and data were extracted, to be documented in an Excel spreadsheet using a prepared template including the following information: study title, authors’ names, year of publication, country, study objectives, sample size, age group, study instruments, and relevant findings. The detailed search strategy and identification process of included articles are shown in Figure 1.
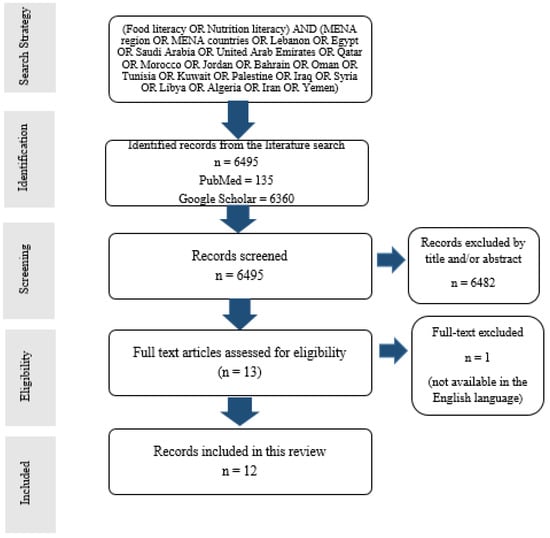
Figure 1.
The flow diagram of the search and identification process for the 12 studies included in this review.
The review findings on the status of food and/or nutrition literacy were compared with that obtained outside the MENA region to allow for comparison and discussion. Besides, we reviewed food literacy and nutrition literacy policies and programs with the countries of their implementation, to identify if any have been implemented in the MENA region.
3. Results and Discussion
Overall, 12 studies were included in this review. Table 2 presents the data extracted from each study. Among them, five were published in the year 2021 [,,,,]; four in 2020 [,,,]; one in 2019 []; and two in 2018 [,]. Regarding the country of origin of the studies, one study was conducted in Lebanon [], two studies were conducted in Palestine [,], and the nine remaining were performed in Iran [,,,,,,,,]. In addition, eight of the studies were assessing food and/or nutrition literacy among adolescents [,,,,,,,], while the remaining studies included adult participants [,,,]. Adolescents were considered as individuals aged between 10–19 years old, according to the recommended criteria of the World Health Organization (WHO) []. Besides, the sample size in the reviewed studies ranged between 101 and 803 participants. All in all, five studies assessed both the food literacy and nutrition literacy of the participants [,,,,], whereas the remaining seven studies assessed nutrition literacy alone [,,,,,,]. However, no studies solely addressed the food-literacy concept.

Table 2.
Summary of studies assessing food and/or nutrition literacy in the MENA region.
3.1. Assessment Tools
To assess food and nutrition literacy in the MENA countries, the Food and Nutrition Literacy Assessment Tool (FNLAT) and the Food and Nutrition Literacy Tool (FNLIT) were used on the reviewed studies. FNLAT was used on only one study [], while FNLIT was used on five studies [,,,,]. For nutrition-literacy assessment, six different tools were used: the Nutrition Literacy Assessment Instrument (NLAI) []; Newest Vital Sign (NVS) []; Nutrition Literacy Scale []; NLQ-20 []; Nutrition Literacy Instrument, developed in Turkey []; Evaluation Instrument of Nutrition Literacy on Adults (EINLA) [].
Multiple tools with different psychometric properties also exist and were used outside the MENA boundaries; these include the Food Literacy Assessment Tool for Healthy, Joyful, and Sustainable Diet in South Korea [], Food and Nutrition Literacy Questionnaire for Chinese School-age Children (FNLQ-SC) [], a food literacy instrument for school children in a Danish context [], Food Literacy Assessment Tool (FLitT) in the United States (U.S.) [], Thai-Nutrition Literacy Assessment Tool for Adolescents (Thailand) [], preschool-FLAT for Italian children [], Tool for Food Literacy Assessment in Children (TFLAC) in U.S. [], Critical Nutrition Literacy Scale (CNL-E) (Norway) [], Menu Board Literacy, and Self-Efficacy Scale for Children in the U.S. [], the dietary behavior scale and the self-efficacy in science scale (Norway) [], Food Label Literacy for Applied Nutrition Knowledge (FLLANK) Questionnaire in the U.S. [], Adolescent Nutrition Literacy Scale (ANLS) in Turkey [,,,], 19-item food literacy measurement tool in Korea [], Nutrition Literacy Scale-Greek (NLS-Gr) [], Your PEL—Promote and Empower for Health Literacy (with a food-literacy scale) in Portugal [], NLit-P in the U.S. [], Spanish Nutrition Literacy Scale [], Electronic-Nutrition Literacy Tool (eNutLit) [], Short Food Literacy Questionnaire (SFLQ) [], and Italian Food Literacy Survey (IT-FLS) [].
3.2. Food and/or Nutrition-Literacy Status in the MENA Countries
Taleb, S. and Itani, L. (2021) [] assessed the nutrition literacy among 189 Lebanese adolescents aged 14–19 years old and the association of nutrition literacy with adolescents’ BMI status and food habits. Lebanese adolescents had adequate nutrition literacy on the nutrition and health, macronutrients, and food-groups literacy components of the NLAI scale; however, marginal nutrition literacy was observed for household-food measures and food-label reading []. In contrast, Natour, N. et al. (2021) [] reported that about one quarter (29%) of Palestinian adult participants appeared to have adequate nutrition literacy. Tell et al. (2021) [] further found that the mean of functional nutrition literacy (FNL) was 2.8 ± 0.5 (over 7), 3.3 ± 0.5 (over 8) for interactive nutrition literacy (INL), and 3.6 ± 0.5 (over 11) for critical nutrition literacy (CNL), indicating literacy insufficiency at all sublevels among Palestinian adults.
The food and nutrition literacy has been widely addressed in Iran more than any other country in the MENA region. Ashoori, M. et al. (2021) [] explored that Iranian senior-high-school students (17–18 years old) had inadequate levels of food and nutrition literacy, with a mean ± SD of the total food and nutrition literacy (FNL) score equal to 52.1 ± 10.96 (a score of 60 is considered acceptable) []. Among 803 Iranian student participants (10–12 years old), 68.8% of them had high food and nutrition scores in the cognitive domains (understanding food and nutrition information); nevertheless, at least one out of four students (25%) had low score values in the skill domain (including food label literacy, food choice literacy) []. Moreover, the study findings by Doustmohammadian et al. (2020) [] reemphasized the latter, by showing that 25% of school-age Iranian students had low scores in the skill domain, and the majority (97.4%) scored moderate-to-high in the cognitive domain of the food and nutrition literacy. Similar findings were also reported in a 2019 published paper [], which explored that even though most Iranian adolescents had adequate food and nutrition literacy, more than half (69%) had the highest score in the cognitive domain, while only few (15%) scored highly in the skills domain. Khorramrouz, F. et al. (2020) [] demonstrated that 14% of 315 Iranian students had inadequate food and nutrition literacy, and only 23.2% had high food- and nutrition-literacy scores. Mehri et al. (2020) [] also reported that most Iranian adolescents had poor food and nutrition literacy (62% of males and 58.1% of females). As well, the nutrition literacy score in elementary school teachers in Yasuj, Iran was 27.14 ± 3.2, revealing that 22.7% of participants were nutritionally illiterate []. Added to these, the mean ± SD of total nutrition literacy was 52.98 ± 7.15, an indication of inadequacy in literacy levels among Iranian young adolescents (13–15 years old) []. On the contrary, about half of Iranian medical students (48.1%) showed adequate nutrition literacy, and, interestingly, only 1% had poor nutrition-literacy scores [].
Therefore, food literacy and nutrition literacy have been inadequately addressed in the MENA countries, with the most data available in Iran. Moreover, where assessed, the data seem distressing, with critical deficits in skills rather than cognitive areas, such as food-label reading, food selection, and cooking. Nonetheless, food literacy and nutrition literacy were shown to be of better status in multiple countries outside the MENA region, even among adolescent participants. This was evident in recent studies conducted in China [], Turkey [,,], the U.S. [], and Ghana [], with all emphasizing adequate nutrition literacy in the sampled population, showing good competencies in most or even all food-literacy and nutrition-literacy components. Besides, good nutrition-literacy levels and basic food literacy were recorded in Greece [] and Canada [], respectively. The disparity between the MENA countries and other nations’ findings may be attributed by the latter’s investment in food and nutrition education. For instance, in the U.S., the percentage of schools providing nutrition education and instructions was 74.1% in 2014 []. Besides, it is encouraging to note that Nigeria has decided to increase investment in school food and nutrition []. Evidence suggests that people can change their behaviors to improve their nutrition outcomes, particularly when they are in supportive environments []. Thus, in a region such as the MENA that is plagued by numerous conflicts, the people, especially children and youth, need opportunities to develop nutrition and food literacy through food and nutrition education, standards, and policies. In addition to national governments, activists and advocates have a role to play in bringing about change. This is in line with the call for systemic change made by Agenda 2030 and the emphasis placed on food systems in the outcome documents of the Second International Conference on Nutrition (ICN2).
Most of the reviewed studies in the MENA region included adolescent participants, with all reporting dismal literacy levels in this vulnerable age group. This observation is crucial because adolescence encompasses critical stages of development and rapid growth, mainly the pubertal growth stage, during which nutrient requirements increase []. Accordingly, nutrition-related problems have been observed among adolescents having inadequate levels of nutrition literacy []. Therefore, it is essential to promote healthy eating habits during this unique life stage, by having interventions be delivered continuously, with a specific emphasis on school-based food and nutrition education. Besides, the review presently reveals that skill-based literacy, mainly food-label use, is more problematic than cognitive-based literacy, with lower use of food labels among food/nutrition-illiterate participants [,,,,]. Based on many pieces of evidence, food-label reading is one pivotal step to improving food choices and dietary habits []. One possible explanation for observing such findings in the MENA countries is that this concept and its application have neither been entered into school curricula and textbooks nor in education programs, to empower individuals in basing their food choices according to nutrition- and safety-related considerations. One recent study showed that Lebanese shoppers expressed poor nutrition-label-related knowledge, and more than half the population either read nutrition labels occasionally or did not look at the food label at all []. Emirati consumers reported looking mostly at the expiration date of the products rather than the information related to the food-storage and -handling instructions and the biotechnology as well, which are key components of being food literate []. Similarly, only 42% of Bahraini consumers read the food label, with the common practice being reading the basic label information related to production and expiry dates []. Food-literacy interventions focusing on consumer’ skills to read food labels should be prioritized in such regions, where nutrition inadequacy and malnutrition are not uncommon. Thereupon, Hoteit M. and colleagues (2022) [] provided data on this topic, “the first steps in the Nutri-Score roadmap”, to serve as an initiative to motivate the national implementation of food-labeling approaches in Lebanon such as the Nutri-Score front-of-pack label.
3.3. Correlates of Food and/or Nutrition Literacy in the MENA Countries
This review found associations between food and/or nutrition literacy and critical factors and correlates. The nutrition literacy of Lebanese adolescents was associated with their food habits; nevertheless, an unusual finding is that participants with higher nutrition literacy scores had poorer food habits (higher fat intake, higher sweets intake, and lower intake of fruits and vegetables) as compared to other participants with low nutrition-literacy scores []. Related to this, Taleb, S. and Itani, L. debated that nutrition literacy alone, if not coupled with essential behavior capabilities and environmental support, may not guarantee behavior change []. What is also worth mentioning is that the body mass index (BMI) of Lebanese adolescents did not correlate with their nutrition literacy []. However, higher nutrition-literacy levels among Palestinian adults predicted better use of the food labels as well as checking the health benefits on the label and, in consequence, higher consumption of low-calorie products []. In addition, the food and nutrition literacy were correlated with the use of food labels and looking, in particular, over the ingredients part of the label []. Adding cheese and mayonnaise to meals was less common in participants with adequate critical food and nutrition literacy []. Participants with better FNL seemed to rely on health professionals and scientific books rather than unreliable online sources to seek nutrition information [].
Ashoori, M. et al. [] found that high food and nutrition literacy scores predicted better school performance among high school students. Participants who had a family member having a nutrition-related disease scored higher on the food-label-reading skill of the food and nutrition literacy []. Better food and nutrition literacy anticipated everyday intake of breakfast, lunch, and dinner compared to those who used to skip meals []. Participants having higher food- and nutrition-literacy scores reported lower consumption of sausages, hamburgers, and sweets []. Further, food and nutrition literacy were a barrier to dietary diversity and nutrient adequacy in school-age children in Iran []. A low level of functional food and nutrition literacy (FFNL) was significantly associated with a lower intake of fruits and meat products []. Likewise, inadequate food-label literacy predicted significantly lower consumption of dairy and meat products []. It was also found that poor food and nutrition literacy was significantly associated with a low level of nutrition adequacy ratio (NAR) of protein, calcium, vitamin B3, vitamin B6, and vitamin B9 and the probability of a lower-level mean adequacy ratio (MAR) []. Adolescents who were in contact with healthcare providers had better food- and nutrition-literacy scores []. Moreover, an increase in total nutrition literacy (T-NL), INL, and CNL enhance diet quality []. An increase in FNL was associated with lower sugar intake and better energy balance in male participants []. Further, higher education level was also a significant correlate with the nutrition literacy []. Nutritional literacy had a significant correlation with the field of study, residence, and body mass index (p < 0.05) []. Food and nutrition literacy and food insecurity have also been associated, and food-insecure participants were about three times more likely to have low food and nutrition literacy scores compared to the food-secure participants (OR = 2.86, 95% CI 1.35, 6.05; p = 0.006) [].
The review findings of food literacy and nutrition literacy correlate with those reported by studies outside the MENA boundaries, with significant associations with a myriad of nutrition outcomes. Costarelli, V. et al. (2021) [] debated that better parental nutrition literacy was significantly associated with the feeding practices of their children, including healthy-eating guidance and monitoring practices. Moreover, better food literacy was found to have a negative association with fast food consumption and alcohol abuse among secondary students (16–21 years old) in Portugal []. The relationship between food literacy and food security has been also addressed in Australia, showing that food-insecure participants were 1.4 times less likely to base their food choices on looking over the nutrition information panel []. Furthermore, food-label use was higher among Turkish adolescents having adequate nutrition literacy, who also experienced lower consumption of fast food and reliance on reliable sources to search for and access nutrition information [], which were also emphasized by the findings reported by Ayer, Ç. and Ergin, A. (2021) [] and Koca, B. and Arkan, G. (2020) []. Besides, there was a significant positive relationship between food literacy and students’ dietary behavior in Ghana []. Moreover, multiple studies reported a positive association between food literacy and adolescents’ dietary intake; adolescents with greater food knowledge and frequent food preparation behaviors had healthier dietary practices []. Taken together, improving communities’ food and nutrition literacy could refigure the nutrition situation in many countries, pushing them closer to or even attaining Goal 2 of the 2030 Agenda of Sustainable Development, which is to end all forms of malnutrition.
3.4. Existing Food Literacy and Nutrition Literacy Policies and Programs
The published literature reveals that the MENA countries have not adopted any food-literacy or nutrition-literacy policies and programs yet, despite the need and the evident effectiveness of the existing ones. On the other hand, many countries have taken the initiative to formulate and adopt school-based programs and policies to promote food and nutrition knowledge and skills among children, and in certain circumstances, those of their parents and other community members. According to Hawkes and colleagues [], there are four mechanisms by which a policy can influence food preferences and support healthy-eating patterns: (1) policy provides an enabling environment for healthy-preference learning; (2) policy overcomes barriers to the expression of healthy preferences; (3) policy encourages people to reassess existing unhealthy preferences; and (4) policy stimulates a food-system response. Table 3 lists a collection of food-literacy and nutrition-literacy programs and policies, along with the countries in which they were implemented, the target group, a brief description of the program/policy, the theory they are based on, the effectiveness, and the evaluation tools. Countries such as Australia and the United States appear to have made the most efforts in developing effective programs to improve the food literacy and nutrition knowledge of intervened participants. Refer to Table 3 for more details about the existing policies and programs.

Table 3.
Policies and programs have been implemented to improve food and/or nutrition literacy.
3.5. Limitations and Strengths of This Review
This review has some limitations. There is the potential for missing studies because only a few databases were searched. Nonetheless, the strength of this review is crystallized, contributing to the literature by highlighting the MENA’s undervaluation of the food-literacy and nutrition-literacy concepts in terms of original definitions, assessment, policies, and programs. Our findings can be used to inform researchers and policymakers to start taking incremental steps to improve the state of food literacy and nutrition literacy in the region.
4. Conclusions
Food and nutrition literacy is one of many factors contributing to the prevalence rates of malnutrition and health outcomes. This review emphasized that there is a current dearth of data, policies, and programs regarding food literacy and nutrition literacy in the MENA region. The authors present this review data to spur additional research efforts into these topics in such a region plagued by high rates of malnutrition and nutrition-related disorders. This review is a wake-up call for researchers and policymakers to develop a robust approach to address and combat food literacy and nutrition literacy concerns in the MENA region.
Recommendations and Future Perspectives
The MENA countries should start taking steps to create a supportive environment that boosts the food literacy and nutrition literacy of people in the region. Nutrition education and food and nutrition programs and policies are indispensable to providing an enabling environment for healthy dietary behaviors and stimulating a food system response. The existing policies need to be evaluated and monitored formally to assess the extent of implementation and whether they are applicable in the MENA region, having the same promising short-term and long-term effective outcomes. Nutrition and food education in child care and school settings is one of many steps that can be initiated to pave the way to come near to achieving the sustainable development goals (SDGs) by 2030. Regional researchers should prioritize conducting sufficient studies on food and nutrition literacy as well, to serve as baseline data for stakeholders and policymakers for taking an action. It is the researchers’ responsibility to point out when and where to act, as it is the vulnerable population that benefits the most from intervention, and the best ways to develop, monitor, and evaluate food-literacy and nutrition-literacy programs.
Author Contributions
H.M. and M.H.: conceptualization, data curation, formal analysis, investigation, methodology, project administration, supervision, validation, writing―original draft preparation; Y.S.: project administration, writing―review and editing; L.H.-W.: project administration, supervision, writing―review and editing; M.H.: data curation, methodology, project administration, supervision, validation, writing―review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All the study data are reported in this paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- UNICEF. Nutrition. Middle East and North Africa. 2022. Available online: https://www.unicef.org/mena/nutrition (accessed on 15 May 2022).
- Hoteit, M.; Mortada, H.; Al-Jawaldeh, A.; Mansour, R.; Yazbeck, B.; AlKhalaf, M.; Bookari, K.; Tayyem, R.; Al-Awwad, N.J.; Sabbah, H.A.; et al. Dietary diversity in the Eastern Mediterranean region before and during the COVID-19 pandemic: Disparities, challenges, and mitigation measures. Front. Nutr. 2022, 9, 813154. [Google Scholar] [CrossRef] [PubMed]
- De Backer, C.; Teunissen, L.; Cuykx, I.; Decorte, P.; Pabian, S.; Gerritsen, S.; Matthys, C.; Sabbah, H.A.; Van Royen, K. The Corona Cooking Survey Study Group. An evaluation of the COVID-19 pandemic and perceived social distancing policies in relation to planning, selecting, and preparing healthy meals: An observational study in 38 countries worldwide. Front. Nutr. 2020, 7, 621726. [Google Scholar] [CrossRef] [PubMed]
- UNICEF. As the War in Ukraine Continues, Millions of Children in the Middle East and North Africa at Increased Risk of Malnutrition Amid Food Price Hikes. 2022. Available online: https://www.unicef.org/mena/press-releases/war-ukraine-continues-millions-children-middle-east-and-north-africa-increased-risk (accessed on 25 June 2022).
- FAO. Regional Overview of Food Security and Nutrition. 2020. Available online: https://www.fao.org/3/cb4902en/cb4902en.pdf (accessed on 22 July 2022).
- UNICEF. TOO Little or Too Much. Available online: https://www.unicef.org/mena/too-little-or-too-much (accessed on 22 July 2022).
- Nasreddine, L.; Ayoub, J.J.; Al Jawaldeh, A. WHO Regional Office for the Eastern Mediterranean. Review of the nutrition situation in the Eastern Mediterranean Region. East. Mediterr. Health J. 2018, 24, 77–91. [Google Scholar] [CrossRef]
- Al-Jawaldeh, A.; Taktouk, M.; Doggui, R.; Abdollahi, Z.; Achakzai, B.; Aguenaou, H.; Al-Halaika, M.; Almamary, S.; Barham, R.; Coulibaly-Zerbo, F.; et al. Are countries of the Eastern Mediterranean region on track towards meeting the World Health Assembly target for anemia? A review of evidence. Int. J. Environ. Res. Public Health 2021, 18, 2449. [Google Scholar] [CrossRef] [PubMed]
- Belhaj, F.; Soliman, A. MENA Has a Food Security Problem, But There Are Ways to Address It. World Bank Group. 2021. Available online: https://www.worldbank.org/en/news/opinion/2021/09/24/mena-has-a-food-security-problem-but-there-are-ways-to-address-it (accessed on 22 July 2022).
- IFPRI. Overcoming the Triple Burden of Malnutrition in the MENA Region. Available online: https://www.ifpri.org/blog/overcoming-triple-burden-malnutrition-mena-region%E2%80%A8 (accessed on 25 June 2022).
- UNICEF. Hunger and Malnutrition in the Arab Region Stand in the Way of Achieving Zero Hunger by 2030, UN Report Warns. Available online: https://www.unicef.org/mena/press-releases/hunger-and-malnutrition-arab-region-stand-way-achieving-zero-hunger-2030-un-report (accessed on 25 June 2022).
- Fingland, D.; Thompson, C.; Vidgen, H. Measuring food literacy: Progressing the development of an International Food Literacy Survey using a content validity study. Int. J. Environ. Res. Public Health 2021, 18, 1141. [Google Scholar] [CrossRef] [PubMed]
- Vaitkeviciute, R.; Ball, L.E.; Harris, N. The relationship between food literacy and dietary intake in adolescents: A systematic review. Public Health Nutr. 2015, 18, 649–658. [Google Scholar] [CrossRef]
- CDC. Food Literacy, Nutritional Literacy & Health Literacy. 2022. Available online: https://www.cdc.gov/healthliteracy/researchevaluate/foodliteracy.html#:~:text=Children%20and%20food%20literacy (accessed on 21 June 2022).
- Cullen, T.; Hatch, J.; Martin, W.; Higgins, J.W.; Sheppard, R. Food Literacy: Definition and Framework for Action. Can. J. Diet. Pract. Res. 2015, 76, 140–145. [Google Scholar] [CrossRef]
- LCDP Healthy Eating Team. Food Literacy: A Framework for Healthy Eating. Locally Driven Collaborative Project Measuring Food Literacy in Public Health. 2018. Available online: https://www.odph.ca/upload/membership/document/2018-11/food-literacy-poster-front-back-final-for-web_1.pdf (accessed on 21 June 2022).
- Widener, P.; Karides, M. Food System Literacy. Food Cult. Soc. 2014, 17, 665–687. [Google Scholar] [CrossRef]
- Yoo, H.L.; bin Jo, E.; Kim, K.; Park, S. Defining food literacy and its application to nutrition interventions: A scoping review. Korean J. Community Nutr. 2021, 26, 77. [Google Scholar] [CrossRef]
- Aihara, Y.; Minai, J. Barriers and catalysts of nutrition literacy among elderly Japanese people. Health Promot. Int. 2011, 26, 421–431. [Google Scholar] [CrossRef]
- Krause, C.; Sommerhalder, K.; Beer-Borst, S.; Abel, T. Just a subtle difference? Findings from a systematic review on definitions of nutrition literacy and food literacy. Health Promot. Int. 2016, 33, 378–389. [Google Scholar] [CrossRef] [PubMed]
- Wickham, C.A.; Carbone, E.T. What’s technology cooking up? A systematic review of the use of technology in adolescent food literacy programs. Appetite 2018, 125, 333–344. [Google Scholar] [CrossRef] [PubMed]
- Truman, E.; Lane, D.; Elliott, C. Defining food literacy: A scoping review. Appetite 2017, 116, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Sustain Ontario. Food Literacy Student Nutrition Programs & Food Literacy. 2013. Available online: https://sustainontario.com/greenhouse/custom/uploads/2016/09/Food-literacy-and-SNPs.pdf (accessed on 25 June 2022).
- Block, L.G.; Grier, S.A.; Childers, T.L.; Davis, B.; Ebert, J.E.J.; Kumanyika, S.; Laczniak, R.N.; Machine, J.E.; Motley, C.M.; Peracchio, L.; et al. From nutrients to nurturance: A conceptual introduction to food well-being. J. Public Policy Mark. 2011, 30, 5–13. [Google Scholar] [CrossRef]
- Kolasa, K.M.; Peery, A.; Harris, N.G.; Shovelin, K. Food literacy partners program: A strategy to increase community food literacy. Top. Clin. Nutr. 2001, 16, 1–10. [Google Scholar] [CrossRef]
- Lee, C.-K.; Liao, L.-L.; Lai, I.-J.; Chang, L.-C. Effects of a healthy-eater self-schema and nutrition literacy on healthy-eating behaviors among Taiwanese college students. Health Promot. Int. 2019, 34, 269–276. [Google Scholar] [CrossRef]
- Silk, K.J.; Sherry, J.; Winn, B.; Keesecker, N.; Horodynski, M.A.; Sayir, A. Increasing nutrition literacy: Testing the effectiveness of print, web site, and game modalities. J. Nutr. Educ. Behav. 2008, 40, 3–10. [Google Scholar] [CrossRef]
- Palumbo, R. Sustainability of well-being through literacy. The effects of food literacy on sustainability of well-being. Agric. Agric. Sci. Procedia 2016, 8, 99–106. [Google Scholar] [CrossRef]
- Burrows, T.L.; Lucas, H.; Morgan, P.J.; Bray, J.; Collins, C.E. Impact evaluation of an after-school cooking skills program in a disadvantaged community: Back to Basics. Can. J. Diet. Pract. Res. 2015, 76, 126–132. [Google Scholar] [CrossRef]
- Hersch, D.; Perdue, L.; Ambroz, T.; Boucher, J.L. The impact of cooking classes on food-related preferences, attitudes, and behaviors of school-aged children: A systematic review of the evidence, 2003–2014. Prev. Chronic Dis. 2014, 11, E193. [Google Scholar] [CrossRef]
- Robson, S.M.; Stough, C.O.; Stark, L.J. The impact of a pilot cooking intervention for parent-child dyads on the consumption of foods prepared away from home. Appetite 2016, 99, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.J.; Oh, K.Y.; Kim, M.Y.; Seo, Y.S.; Shin, J.-H.; Song, Y.R.; Yang, J.-H.; Foxman, B.; Ki, M. Risk factors for group B streptococcus colonization among pregnant women in Korea. Epidemiol. Health 2011, 33, e20110010. [Google Scholar] [CrossRef] [PubMed]
- Khorramrouz, F.; Doustmohammadian, A.; Eslami, O.; Khadem-Rezaiyan, M.; Pourmohammadi, P.; Amini, M.; Khosravi, M. Relationship between household food insecurity and food and nutrition literacy among children of 9–12 years of age: A cross-sectional study in a city of Iran. BMC Res. Notes 2020, 13, 433. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, A.; Butt, A.; Saha, T.K.; Basu, G.; Chattopadhyay, A.; Mukherjee, A. Assessment of malnutrition among adolescents: Can BMI be replaced by MUAC. Indian J. Community Med. 2010, 35, 276. [Google Scholar] [CrossRef] [PubMed]
- López-Hernández, L.; Martínez-Arnau, F.M.; Pérez-Ros, P.; Drehmer, E.; Pablos, A. Improved nutritional knowledge in the obese adult population modifies eating habits and serum and anthropometric markers. Nutrients 2020, 12, 3355. [Google Scholar] [CrossRef]
- Epuru, S.; Al Shammary, M. Nutrition Knowledge and its Impact on Food Choices among the students of Saudi Arabia. IOSR J. Dent. Med. Sci. 2014, 13, 68–74. [Google Scholar] [CrossRef]
- Velpini, B.; Vaccaro, G.; Vettori, V.; Lorini, C.; Bonaccorsi, G. What is the impact of nutrition literacy interventions on children’s food habits and nutrition security? A scoping review of the literature. Int. J. Environ. Res. Public Health 2022, 19, 3839. [Google Scholar] [CrossRef]
- United States Trade Representative. Middle East/North Africa (MENA). 2022. Available online: https://ustr.gov/countries-regions/europe-middle-east/middle-east/north-africa (accessed on 15 May 2022).
- Taleb, S.; Itani, L. Nutrition Literacy among Adolescents and Its Association with Eating Habits and BMI in Tripoli, Lebanon. Diseases 2021, 9, 25. [Google Scholar] [CrossRef]
- Natour, N.; Al-Tell, M.; Ikhdour, O. Nutrition Literacy is Associated with Income and Place of Residence but not with Diet behavior and Food Security in the Palestinian Society. BMC Nutr. 2021, 7, 1–8. [Google Scholar] [CrossRef]
- Tell, M.A.; Natour, N.; Badrasawi, M.; Shawish, E. The relationship between Nutrition Literacy and Nutrition Information seeking attitudes and Healthy Eating Patterns in the Palestinian Society. Res. Sq. 2021, 1–16. [Google Scholar] [CrossRef]
- Ashoori, M.; Omidvar, N.; Eini-Zinab, H.; Shakibazadeh, E.; Doustmohamadian, A.; Abdar-Esfahani, B.; Mazandaranian, M. Food and nutrition literacy status and its correlates in Iranian senior high-school students. BMC Nutr. 2021, 7, 19. [Google Scholar] [CrossRef] [PubMed]
- Doustmohammadinan, A.; Omidvar, N.; Mohammadi, N.K.; Eini-Zinab, H.; Amini, M.; Abdollahi, M.; Esfandyari, S.; Amirhamidi, Z. Food and nutrition literacy (FNLIT) is associated to healthy eating behaviors in children. Nutr. Food Sci. Res. 2021, 8, 37–47. [Google Scholar] [CrossRef]
- Doustmohammadian, A.; Omidvar, N.; Keshavarz-Mohammadi, N.; Eini-Zinab, H.; Amini, M.; Abdollahi, M.; Amirhamidi, Z.; Haidari, H. Low food and nutrition literacy (FNLIT): A barrier to dietary diversity and nutrient adequacy in school age children. BMC Res. Notes 2020, 13, 286. [Google Scholar] [CrossRef] [PubMed]
- Mehri, A.; Jafari, N.; Akbarzadeh, I.; Siri, F.H.; Abbassgholizadeh, N.; Kangavari, H.N.; Barzegar, A.; Mirtorabi, S.D.; Ghadirzadeh, M.R.; Forouzesh, M.; et al. Students’ nutrition literacy and the existence of health care providers in Iranian schools. J. Res. Health Sci. 2020, 20, e00476. [Google Scholar] [CrossRef]
- Bahramfard, T.; Salehi, S.O.; Toori, M.A.; Pourmahmoudi, A.; Jowshan, M.; Parvin, S.; Khosravani, Z.; Malekzadeh, J. Nutritional literacy status and its related factors in students of Yasuj University of Medical Sciences. Nutr. Clín. Diet Hosp. 2020, 40, 55–62. [Google Scholar] [CrossRef]
- Doustmohammadian, A.; Mohammadi, N.K.; Omidvar, N.; Amini, M.; Abdollahi, M.; Eini-Zinab, H.; Amirhamidi, Z.; Esfandiari, S.; Nutbeam, D. Food and nutrition literacy (FNLIT) and its predictors in primary schoolchildren in Iran. Health Promot. Int. 2019, 34, 1002–1013. [Google Scholar] [CrossRef]
- Hemati, M.; Akbartabar Toori, M.; Shams, M.; Behroozpour, A.; Rezaei, A. Measuring Nutritional Literacy in Elementary School Teachers in Yasuj: A Cross-Sectional Study. Armaghane Danesh 2018, 23, 124–133. Available online: http://armaghanj.yums.ac.ir/article-1-1992-en.html (accessed on 15 May 2022).
- Joulaei, H.; Keshani, P.; Kaveh, M.H. Nutrition literacy as a determinant for diet quality amongst young adolescents: A cross sectional study. Prog. Nutr. 2018, 20, 455–464. [Google Scholar] [CrossRef]
- World Health Organization. Adolescent Health at a Glance in South-East Asia Region. 1970. Available online: https://apps.who.int/iris/handle/10665/204750 (accessed on 15 May 2022).
- Yoo, H.; Jo, E.; Lee, H.; Park, S. Development of a food literacy assessment tool for healthy, joyful, and sustainable diet in South Korea. Nutrients 2022, 14, 1507. [Google Scholar] [CrossRef]
- Liu, T.; Su, X.; Li, N.; Sun, J.; Ma, G.; Zhu, W. Development and validation of a food and nutrition literacy questionnaire for Chinese school-age children. PLoS ONE 2021, 16, e0244197. [Google Scholar] [CrossRef]
- Stjernqvist, N.W.; Elsborg, P.; Ljungmann, C.K.; Benn, J.; Bonde, A.H. Development and validation of a food literacy instrument for school children in a Danish context. Appetite 2021, 156, 104848. [Google Scholar] [CrossRef] [PubMed]
- Hemmer, A.; Hitchcock, K.; Lim, Y.S.; Butsch Kovacic, M.; Lee, S.-Y. Development of Food Literacy Assessment Tool targeting adults with low income. J. Nutr. Educ. Behav. 2021, 53, 966–976. [Google Scholar] [CrossRef] [PubMed]
- Deesamer, S.; Piaseu, N.; Maneesriwongul, W.; Orathai, P.; Schepp, K.G. Development and psychometric testing of the Thai-nutrition literacy assessment tool for adolescents. PRIJNR 2020, 24, 5–19. Available online: https://he02.tci-thaijo.org/index.php/PRIJNR/article/view/157958 (accessed on 26 June 2022).
- Tabacchi, G.; Battaglia, G.; Messina, G.; Paoli, A.; Palma, A.; Bellafiore, M. Validity and internal consistency of the preschool-FLAT, a new tool for the assessment of food literacy in young children from the Training-to-Health Project. Int. J. Environ. Res. Public Health 2020, 17, 2759. [Google Scholar] [CrossRef] [PubMed]
- Amin, S.A.; Lehnerd, M.; Cash, S.B.; Economos, C.D.; Sacheck, J.M. Development of a Tool for Food Literacy Assessment in Children (TFLAC). J. Nutr. Educ. Behav. 2019, 51, 364–369. [Google Scholar] [CrossRef]
- Naigaga, D.A.; Pettersen, K.S.; Henjum, S.; Guttersrud, Ø. Relating aspects of adolescents’ critical nutrition literacy at the personal level. Nutrire 2022, 47, 1. [Google Scholar] [CrossRef]
- Williams, O.; Quinn, E.L.-H.; Ramirez, M.; Sawyer, V.; Eimicke, J.P.; Teresi, J.A. Development of a menu board literacy and self-efficacy scale for children. J. Nutr. Educ. Behav. 2017, 49, 867–871.e1. [Google Scholar] [CrossRef]
- Guttersrud, Ø.; Petterson, K.S. Young adolescents’ engagement in dietary behaviour—The impact of gender, socio-economic status, self-efficacy and scientific literacy. Methodological aspects of constructing measures in nutrition literacy research using the Rasch model. Public Health Nutr. 2015, 18, 2565–2574. [Google Scholar] [CrossRef]
- Reynolds, J.S.; Treu, J.A.; Njike, V.; Walker, J.; Smith, E.; Katz, C.S.; Katz, D.L. The validation of a food label literacy questionnaire for elementary school children. J. Nutr. Educ. Behav. 2012, 44, 262–266. [Google Scholar] [CrossRef]
- Ayer, Ç.; Ergin, A. Status of nutritional literacy in adolescents in the semi-rural area in Turkey and related factors. Public Health Nutr. 2021, 24, 3870–3878. [Google Scholar] [CrossRef]
- Koca, B.; Arkan, G. The relationship between adolescents’ nutrition literacy and food habits, and affecting factors. Public Health Nutr. 2020, 24, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Yilmazel, G.; Bozdogan, S. Nutrition literacy, dietary habits and food label use among Turkish adolescents. Prog. Nutr. 2021, 23, e2021007-7. [Google Scholar]
- Kalkan, I. The impact of nutrition literacy on the food habits among young adults in Turkey. Nutr. Res. Pract. 2019, 13, 352. [Google Scholar] [CrossRef] [PubMed]
- Park, D.; Choi, M.-K.; Park, Y.K.; Park, C.Y.; Shin, M.-J. Higher food literacy scores are associated with healthier diet quality in children and adolescents: The development and validation of a two-dimensional food literacy measurement tool for children and adolescents. Nutr. Res. Pract. 2022, 16, 272–283. [Google Scholar] [CrossRef] [PubMed]
- Costarelli, V.; Michou, M.; Panagiotakos, D.B.; Lionis, C. Parental health literacy and nutrition literacy affect child feeding practices: A cross-sectional study. Nutr. Health 2022, 28, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, M.; Guiné, R.P.F.; Leitão, A.L.; Duarte, J.; Andrade, J.; Amaral, O. Eating habits and food literacy: Study involving a sample of Portuguese adolescents. Open Agric. 2021, 6, 286–295. [Google Scholar] [CrossRef]
- Gibbs, H.D.; Kennett, A.R.; Kerling, E.H.; Yu, Q.; Gajewski, B.; Ptomey, L.T.; Sullivan, D.K. Assessing the nutrition literacy of parents and its relationship with child diet quality. J. Nutr. Educ. Behav. 2016, 48, 505–509. [Google Scholar] [CrossRef]
- Coffman, M.J.; La-Rocque, S. Development and testing of the Spanish nutrition literacy scale. Hisp. Health Care Int. 2012, 10, 168–174. [Google Scholar] [CrossRef]
- Ringland, E.M.; Gifford, J.A.; Denyer, G.S.; Thai, D.; Franklin, J.L.; Stevenson, M.M.; Prvan, T.; O’Connor, H.T. Evaluation of an electronic tool to assess food label literacy in adult Australians: A pilot study: Electronic tool to assess food label literacy. Nutr. Diet. 2016, 73, 482–489. [Google Scholar] [CrossRef]
- Krause, C.G.; Beer-Borst, S.; Sommerhalder, K.; Hayoz, S.; Abel, T. A short food literacy questionnaire (SFLQ) for adults: Findings from a Swiss validation study. Appetite 2018, 120, 275–280. [Google Scholar] [CrossRef]
- Palumbo, R.; Annarumma, C.; Adinolfi, P.; Vezzosi, S.; Troiano, E.; Catinello, G.; Manna, R. Crafting and applying a tool to assess food literacy: Findings from a pilot study. Trends Food Sci. Technol. 2017, 67, 173–182. [Google Scholar] [CrossRef]
- Zeng, M.; Zhu, Y.; Cai, Z.; Xian, J.; Li, S.; Wang, T.; Shi, Z.; Sharma, M.; Zhao, Y. Nutrition literacy of middle school students and its influencing factors: A cross-sectional study in Chongqing, China. Front. Public Health 2022, 10, 807526. [Google Scholar] [CrossRef]
- Castellanos, D.C.; Holcomb, J. Food insecurity, financial priority, and nutrition literacy of university students at a mid-size private university. J. Am. Coll. Health 2020, 68, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Oti, J.A. Food Literacy and Dietary Behaviour among Day Students of Senior High Schools in Winneba, Central Region of Ghana. J. Food Nutr. Res. 2020, 8, 39–49. Available online: http://www.sciepub.com/journal/jfnr (accessed on 15 May 2022).
- Fernandez, M.A.; Desroches, S.; Marquis, M.; Lebel, A.; Turcotte, M.; Provencher, V. Which food literacy dimensions are associated with diet quality among Canadian parents? Br. Food J. 2019, 121, 1670–1685. [Google Scholar] [CrossRef]
- CDC. Nutrition Education in US Schools. 2021. Available online: https://www.cdc.gov/healthyschools/nutrition/school_nutrition_education.htm (accessed on 26 June 2022).
- UNSCN. Schools as a System to Improve Nutrition a New Statement for School-Based Food and Nutrition Interventions. 2017. Available online: https://www.unscn.org/uploads/web/news/document/School-Paper-EN-WEB-nov2017.pdf (accessed on 15 May 2022).
- Hawkes, C.; Smith, T.G.; Jewell, J.; Wardle, J.; Hammond, R.A.; Friel, S.; Thow, A.M.; Kain, J. Smart food policies for obesity prevention. Lancet 2015, 385, 2410–2421. Available online: https://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(14)61745-1.pdf (accessed on 26 June 2022). [CrossRef]
- Wojcicki, J.M.; Heyman, M.B. Adolescent nutritional awareness and use of food labels: Results from the National Nutrition Health and Examination Survey. BMC Pediatr. 2012, 12, 55. [Google Scholar] [CrossRef]
- Hoteit, M.; Yazbeck, N.; Al-Jawaldeh, A.; Obeid, C.; Fattah, H.A.; Ghader, M.; Mohsen, H. Assessment of the knowledge, attitudes and practices of Lebanese shoppers towards food labeling: The first steps in the Nutri-score roadmap. F1000Research 2022, 11, 84. [Google Scholar] [CrossRef]
- Basarir, A. Consumers’ awareness of food labeling: A case study of United Arab Emirates. Afr. J. Agric. Res. 2012, 7, 4021–4028. [Google Scholar] [CrossRef]
- Wahab, R.A. Food label use and awareness of nutritional information among consumers in Bahrain: An exploratory study. KnE Life Sci. 2018, 4, 26. [Google Scholar] [CrossRef]
- Begley, A.; Paynter, E.; Butcher, L.M.; Dhaliwal, S.S. Examining the association between food literacy and food insecurity. Nutrients 2019, 11, 445. [Google Scholar] [CrossRef] [PubMed]
- Karpouzis, F.; Lindberg, R.; Walsh, A.; Shah, S.; Abbott, G.; Lai, J.; Berner, A.; Ball, K. Evaluating OzHarvest’s primary-school Food Education and Sustainability Training (FEAST) program in 10–12-year-old children in Australia: Protocol for a pragmatic cluster non-randomized controlled trial. BMC Public Health 2021, 21, 967. [Google Scholar] [CrossRef] [PubMed]
- West, E.G.; Lindberg, R.; Ball, K.; McNaughton, S.A. The role of a food literacy intervention in promoting food security and food literacy-OzHarvest’s NEST program. Nutrients 2020, 12, 2197. [Google Scholar] [CrossRef]
- Begley, A.; Paynter, E.; Butcher, L.M.; Dhaliwal, S.S. Effectiveness of an Adult Food Literacy Program. Nutrients 2019, 11, 797. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6520903/ (accessed on 26 June 2022). [CrossRef]
- Foodbank. Food Sensations® for Schools. Available online: https://www.foodbank.org.au/WA/food-sensations-for-schools/?state=wa (accessed on 26 June 2022).
- Foodbank. Fuel Your Future—A Pilbara Youth Initiative. Available online: https://www.foodbank.org.au/WA/fuel-your-future/?state=wa (accessed on 26 June 2022).
- Foodbank. Food Sensations® for Parents. Available online: https://www.foodbank.org.au/WA/food-sensations-for-parents/?state=wa (accessed on 26 June 2022).
- Rees, J.; Fu, S.C.; Lo, J.; Sambell, R.; Lewis, J.R.; Christophersen, C.T.; Byrne, M.F.; Newton, R.U.; Boyle, S.; Devine, A. How a 7-week food literacy cooking program affects cooking confidence and mental health: Findings of a quasi-experimental controlled intervention trial. Front. Nutr. 2022, 9, 802940. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, L.; Howe, L.; Holland, D.; Brian, K.; Scherr, R. Development of an innovative Food Literacy curriculum focused on agriculture, nutrition, and cooking for high school-aged adolescents. Curr. Dev. Nutr. 2019, 3 (Suppl. S1), nzz050.P16-061-19. [Google Scholar] [CrossRef]
- Scazzocchio, B.; Varì, R.; D’Amore, A.; Chiarotti, F.; Del Papa, S.; Silenzi, A.; Gimigliano, A.; Giovannini, C.; Masella, R. Promoting health and food literacy through nutrition education at schools: The Italian experience with MaestraNatura program. Nutrients 2021, 13, 1547. [Google Scholar] [CrossRef]
- Thomas, H.M.; Irwin, J.D. Cook It Up! A community-based cooking program for at-risk youth: Overview of a food literacy intervention. BMC Res. Notes 2011, 4, 495. [Google Scholar] [CrossRef]
- Elsborg, P.; Thorsen, A.V.; Ravn-Haren, G.; Bonde, A.H.; Andersen, S.G.; Vermund, M.C.; Klinker, C.D.; Stjernqvist, N.W. Improved food literacy among schoolchildren as an effect of a food camp intervention: Results of a controlled effectiveness trial. Appetite 2022, 169, 105845. [Google Scholar] [CrossRef]
- Food Tank. Programs Promoting Food Literacy. 2021. Available online: https://foodtank.com/news/2021/09/organizations-promoting-food-literacy-in-schools/ (accessed on 22 June 2022).
- SNACC|New York, NY. SNACC Program. Available online: https://www.snaccprogram.org/#:~:text=Sustainable%20Nutrition%20And%20Community%20Connection&text=SNACC%20is%20a%20hands%2Don (accessed on 21 June 2022).
- Youth Community Agriculture Program. The Food Literacy Project. Available online: https://foodliteracyproject.org/programs/youth-community-agriculture-program/ (accessed on 21 June 2022).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).