Abstract
Culture, tradition, structural violence, and mental health-related stigma play a major role in global mental health for refugees. Our aim was to understand what factors determine the success or failure of community-based psychotherapy for trauma-affected refugees and discuss implications for primary health care programs. Using a systematic realist-informed approach, we searched five databases from 2000 to 2018. Two reviewers independently selected RCTs for inclusion, and we contacted authors to obtain therapy training manuals. Fifteen articles and 11 training manuals met our inclusion criteria. Factors that improved symptoms of depression, anxiety, and PTSD included providing culturally adapted care in a migrant-sensitive setting, giving a role to other clinical staff (task-shifting), and intervention intensity. Precarious asylum status, constraining program monitoring requirements, and diverse socio-cultural and gender needs within a setting may reduce the effectiveness of the program. Primary care programs may enable community based mental health care and may reduce mental health-related stigma for refugees and other migrants. More research is needed on the cultural constructs of distress, programs delivered in primary care, and the role of cultural and language interpretation services in mental health care.
1. Introduction
There are 25.9 million refugees in the world [1]. As refugees integrate, more community clinicians are providing global mental health care. Exposure to violence and forced migration increases the risk for common mental health disorders, chronic pain, and other somatic complaints [2]. Global mental health research considers disease prevalence, traditional beliefs, idioms of distress and stigma [3]. Pharmacotherapy may also play an important role in common mental health disorders [2]; however, this study focuses on community-based psychotherapy and trauma-informed care programs (see Table 1).

Table 1.
Principles of trauma-informed programs and care (Adapted from Purkey et al. [4]).
Refugees do not easily engage in psychotherapeutic relationships [4,5]. Front line physicians are however frequently consulted [6,7]. Refugees prefer community-based care, as opposed to specialist/in hospital care, but are less likely to accept mental health services compared to non-migrant populations [8,9]. Culture impacts patterns of coping, help seeking, adherence to treatment, emotional expression as well as relationships with clinicians [10]. Culture and language interpreters are integral to help clinicians understand the patient’s context [11].
Primary health care clinics can be referred to as the “patient’s medical home”. This “medical home” is a community based interdisciplinary clinic in which patients can access primary healthcare services on a regular basis [12]. While refugee patients visit their “medical home” for medical needs, they often consult for psychosocial needs. For example, refugees are often faced with social issues such as housing or food insecurity [13], and will visit their “medical home” for assistance. These visits for social assistance also allow the primary care clinician further insight into the struggles their patients may be facing, which allows them the opportunity to screen for mental health concerns [2]. These “medical homes” become a trusted space for refugee patients and integration into these “homes”, we argue, is an important element of health settlement and global mental health care. Given this, primary care clinicians may be well positioned to screen, diagnose, and treat common mental health conditions in refugee patients [2].
Interest in community-based psychotherapies for refugees continues to grow [14]. Community based mental health interventions, however, are culturally complex, multi-faceted and dynamic in nature. Consequently, we conducted a realist-informed systematic review to address the following research question: What factors determine the success or failure of community-based psychotherapy for trauma-affected refugees?
2. Materials and Methods
We conducted a realist-informed review to better understand community-based psychotherapies for refugee mental health programs. A traditional realist synthesis is a resource intensive [15], theory-driven approach that seeks to unpack the mechanism of how programs work in particular contexts and settings [15,16]. Several groups have developed pragmatic “realist-informed” reviews. We adopted the approach by Greenhalgh et al. [17], which used a realist lens to analyze rigorous randomized controlled trials. We report our findings according to the RAMESES (Realist and Meta-narrative Evidence Syntheses: Evolving Standards) publication standards (see Supplementary S1) [18].
2.1. Research Team and Initial Scoping of the Literature
We assembled a research team consisting of three primary care clinicians specializing in refugee health, one medical student, one international medical graduate, and one research methodologist experienced in reviews of refugee health. We scoped published medical literature for reviews and trials of psychotherapies. Within the team, we discussed these interventions’ reach, effectiveness, adoption, implementation, and maintenance [19]. Through discussion, we applied a realist lens and developed an evaluation matrix that considered participant, provider and intervention characteristics, process details, historical context, and effectiveness outcomes. This matrix informed our subsequent search strategy, data extraction, and analysis.
2.2. Search Strategy and Selection Criteria
We included any randomized controlled trial whose population included refugees or asylum seekers with experience of trauma in any geographic context. By trauma, we mean the result of “an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or threatening and that has lasting adverse effects on the individual’s functioning and physical, social, emotional, or spiritual well-being” [20]. In the case of refugees, this is often the result of war and/or persecution. We focused exclusively on randomized controlled trials because they are designed around a clear hypothesis; their design minimizes the risk of confounding, and their effectiveness findings are likely to be closer to the true effect than the findings generated by other research methods [21]. We included male or female populations over the age of 18 years who participated in a psychotherapy delivered in any clinical or community setting. We excluded studies focused on children or adolescents and group therapies. We considered any type of comparator (such as waitlist-control or an alternative intervention) and included mental health outcomes of interest: PTSD, depression, or anxiety symptomatology (see Supplementary S2 for full inclusion and exclusion criteria).
We developed a systematic search using relevant keywords and MeSH terms for relevant published randomized controlled trials. Keywords included “refugee”, “asylum seeker”, “trauma”, “PTSD” and “psychotherapy” (see Supplementary S3 for search strategy). We searched MEDLINE, EMBASE, PsycINFO, CENTRAL and PILOTS from 1 January, 2000, to 26 September, 2018. There were no language restrictions. We manually searched reference lists of identified systematic reviews for relevant citations and cross-referenced it against our original search results. Any additional potentially relevant citations were screened. We contacted the authors of all included studies to obtain intervention training manuals or protocols. These training manuals and protocols were included in our review to better understand the theoretical underpinnings and implementation considerations of each identified psychotherapy.
We uploaded search results to Rayyan reference manager software to facilitate the study selection process [22]. Two review authors independently assessed each study for inclusion by title, abstract and full text. Disagreements were resolved through discussion with a third reviewer.
2.3. Data Analysis
We developed a standardized data extraction template which included study design, setting, participant characteristics, intervention, provider, language, process details, study history, outcomes, mechanisms, and conclusions. We extracted data in duplicate and resolved disagreements through discussion. We assessed the methodological rigor of included studies using the Cochrane Risk of Bias tool in duplicate [23]. The review team discussed the relevancy of each included article to the purpose of the review. An appraisal deemed “low” was used for articles that did not include any information or discussion of mechanism or contextual factors. A rating of “medium” was given to studies that provided information on either contextual or mechanism variables. A rating of “high” was given to studies that provided information on both mechanism and contextual variables. We did not exclude any articles based on our critical appraisal (see Supplementary S4). We followed a realist analysis approach (see Table 2). Chains of inference and hypothesis formulation were developed iteratively through discussion with the entire review team. We discussed preliminary conclusions and synthesized key findings using a narrative and interpretive approach.

Table 2.
Realist-informed analysis.
3. Results
Our systematic search identified 647 citations. After the removal of duplicates, two reviewers independently assessed 383 articles by title, abstract, and full-text review. Of the 123 articles assessed at full-text, 15 articles met the eligibility criteria. We contacted the authors of the 15 articles and included 11 additional training documents in our realist analysis (see Figure 1: PRISMA).
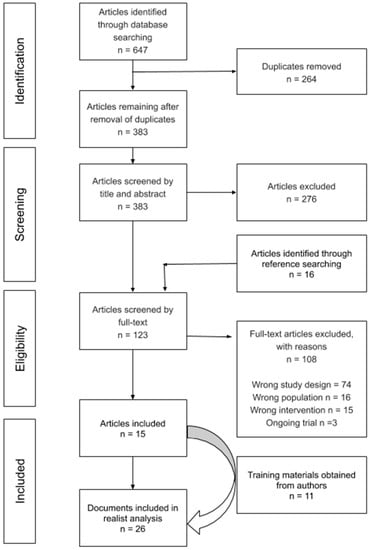
Figure 1.
PRISMA flow diagram.
Our 15 included articles captured findings from 14 randomized controlled trials conducted in Denmark (1), Egypt (1), Germany (3), Norway (1), Sweden (1), Thailand (1), Uganda (2), and the United States (4). All studies were conducted among refugees or asylum seekers with experience of trauma. Interventions included Narrative Exposure Therapy (NET), Common Elements Treatment Approach (CETA), Stress Management (SM), Cognitive Behavioral Therapy (CBT), and Interpersonal Therapy (IPT). We obtained training materials for all interventions in the form of books, training manuals, and peer-reviewed articles. See Table 3 for additional study characteristics.

Table 3.
Characteristics of Included Studies.
We tabulated the effectiveness of individual psychotherapies on participant attrition, anxiety, depression, and PTSD symptomology in Supplementary S5. In summary, all included psychotherapies (CBT, CETA, IPT, NET, and SM) had statistically significant positive effects on symptoms of PTSD. Findings on depression and anxiety outcomes varied across studies. For example, four studies on CBT consistently demonstrated improved symptoms of anxiety and depression when compared with a wait-list control [37,40,41] or exposure therapy [49]. In contrast, NET reduced symptoms of depression in three studies [26,36,50] but had no impact on depression in two other studies [35,46]. Researchers highlighted that refugees with a secure legal status reported less depression across all time points [50]. NET was reported to be equivalent to supportive counselling and psychoeducation according to indicators of depression and anxiety [48]. CETA was effective in reducing symptoms of depression and anxiety, and these results were not dependent on the gender of the participant or severity of trauma [29].
Our systematic search and realist-informed analysis of randomized controlled trials provided data which we then applied to a context-mechanism-outcome configuration to evaluate the success of community-based psychotherapy for trauma-affected refugees. The context within which most refugees seek care is generally in migrant-sensitive healthcare settings and community-based practices [2]. These practices improve access, lessen transportation and financial and migration status needs, and reduce mental health treatment related stigma with interdisciplinary primary care teams. Literature suggests that the way in which care is delivered, or the mechanisms of delivery, are fundamental to successful outcomes. In this study we found that the management of refugee mental health can be tasked-shifted from specialty care (e.g., psychiatry) to primary care [29,42,47,48]. Primary care may include physicians, nurse practitioners, nurses, social workers, settlement workers, and sometimes cultural navigators and even shared mental health care teams. Mental health programs and clinicians can adopt a trauma-informed approach and deliver culturally appropriate psychotherapy to refugees with common mental health conditions. Existing psychotherapeutic approaches, such as CBT, have been culturally adapted with success [40,41].
Programs and clinicians need to be aware of socio-cultural preferences and global mental health presentations in refugee patients. Provision of programs, mentorship, advocacy, and psychotherapy of sufficient intensity can empower and enhance self-efficacy, emotional regulation, and social support, thereby improving mental health outcomes.
The theories underpinning the success or failure of community-based psychotherapy for trauma-affected refugees is explored below.
3.1. Theories That Explain Why Community-Based Mental Health Services for Refugees Work
3.1.1. Practice: Migrant-Sensitive Healthcare Settings
Whether caused by social, structural or financial barriers, evidence suggests that refugees do not access health services effectively, ultimately impacting health outcomes [29,35,42,46,47]. Refugee patients possess complex medical issues and require special considerations to meet their mental health needs, beginning with the setting of care. Ten studies from high resource settings administered mental health interventions in an outpatient setting [26,29,31,35,37,40,41,46,50,51]. In low resource settings, researchers made use of participants’ homes or quiet places nearby [47], straw huts or under trees [48], and church or community center [36]. In the majority of studies, the setting of care was specialized for general refugee populations [26,35] or a specific ethnic or cultural group such as a Burmese-run clinic for Burmese refugees in Thailand [29] or a Sudanese-founded NGO in Egypt [42]. In such cases, the clinical practice setting addressed social determinants of health and offered migrant-sensitive services including language interpretation, culturally tailored support programs, and community-based cultural support staff.
3.1.2. Provider: Task-Shifting
Task shifting holds promise for improving mental health care delivery in primary care settings. It entails the shifting of tasks, typically from more to less highly trained individuals, to make efficient use of resources. Several included studies showed that some therapies could be adopted by other traditionally non-medical personnel including social workers, lay counselors, teachers, and even former refugees with the appropriate training [29,42,47,48]. However, the majority of psychotherapies were delivered by psychiatrists, clinical psychologists and experienced mental health workers in high income countries [26,31,35,36,37,40,41,46,49,50]. Qualifications for laypersons recruitment included language fluency (English and mother tongue); educational attainment (attended primary school and/or secondary school); interest in mental health/counseling; and shared cultural, religious, and political experience [29,42,47,48]. Of note, none of the studies looked at primary care clinicians delivering these psychotherapies. However, successful task-shifting to non-medical personnel suggests that primary health care clinicians could equally deliver the therapy, and this would likely lead to better health outcomes, where primary care practitioners are already educated on the diagnosis and management of mental health disorders.
3.1.3. Psychotherapy: Cultural Adaptations for Refugee Mental Health
Culture influences how mental health conditions are generated, experienced, and treated. This highlights the need for an effective and inexpensive process that is both easy to administer and culturally sensitive. Cultural adaptation is the “systematic modification of evidence-based treatment to account for language, culture, and context that is consistent with the client’s cultural patterns, meanings, and values” [38]. In addition, culture may influence the acceptability of psychotherapy interventions. For example, cultures that value oral tradition and history telling may find narrative approaches such as NET socially acceptable, thereby, potentially countering the stigma associated with traditional mental health services [36]. Similarly, investigators suggested that CBT was particularly useful for Southeast Asian refugees owing to the similarity of Buddhist principles to core aspects of CBT (e.g., mindfulness) [40] and the ability to incorporate culturally appropriate visualization, such as a lotus bloom [41]. Furthermore, practitioners of CETA tailored skills to the individual and familial needs of their clients, as well as to the cultural needs of the community, by using culturally relevant folktales, personal anecdotes, and local expressions or adages to convey key principles [29]. Cultural modifications also included building on existing strengths (e.g., support of family and community) and existing coping strategies (e.g., meditation, singing songs, having tea with friends) to increase daily functioning [29].
3.1.4. Psychotherapy: Intensity
Primary health care typically has a limited early focus on mental health. The majority of our included studies achieved positive expected outcomes by observing the recommended intensity of psychotherapies according to the treatment manuals. However, three trials adopted a more brief version of psychotherapies [36,42,48]. Two studies on NET conducted three treatment sessions of 90 to 120 min duration [36,48]. The standard version of NET is a median of 9–10 treatment sessions with 120 min duration [46]. One study provided 6 biweekly sessions of IPT compared to the traditional version of 12–16 individual weekly sessions [42]. In studies offering brief interventions, weaker symptom improvement was due to the limited dose of treatment sessions, coupled with the relatively severe and often long-standing trauma symptoms in the sample [36]. In contrast, the high intensity (16–20 sessions, 120 min in length) of CBT and exposure therapy was reported as a factor contributing to these psychotherapies’ positive significant results [49]. If a considerably lesser amount of, and shorter sessions, had been used, the clinical impression is that both exposure therapy and CBT would not have resulted in significant improvements in the patients [49]. In cases where the refugee patient does not speak the local language, the presence of an interpreter also has implications for psychotherapy intensity: Not only must the patient trust the interpreter enough to allow them to participate in the treatment, but the treatment itself must proceed at a considerably slower pace and be long enough so that adequate time is allotted to all aspects of the treatment [49]. Indeed, variable outcomes may reflect the limitations of short-term psychosocial interventions [48].
3.2. Theories of Why Community-Based Mental Health Services for Refugees Do Not Work
3.2.1. Clinician: Diverse Socio-Cultural Differences
Social and cultural factors influence how patients from a given culture express and manifest their symptoms, their style of coping, their family and community support, and their willingness to seek treatment. Importantly, the current Diagnostic and Statistical Manual of Mental Disorders (DSM) PTSD criteria may not represent the full spectrum of response to trauma across different cultural contexts, and culture-specific reactions to trauma need to be elucidated. Thus, there is not always content equivalence in the symptomatology of trauma-related disorders in different cultural groups [40]. As such, clinicians should consider socio-cultural factors when selecting interventions. For example, a study on Stress Inoculation Training (SIT) found no reduction in PTSD symptoms among asylum seekers in Germany [35]. This may be due to differences in participant education and other sociocultural factors. SIT may be more successful with more highly educated patients because it requires an understanding of abstract concepts (i.e., the distinction between thoughts, feelings, and behavior). Moreover, it is possible that some of the treatment components of SIT were outside of the cultural norms of the participants because it has been developed according to the Western understanding of human experiences and behavior [35].
Socio-cultural factors, such as gender roles, may influence the selection of the clinician. In the literature, female patients withdrew from interventions because they did not want a male therapist [49] or because their husbands “forbade them to continue” [42]. Evidence indicated that mixed gender pairing between patient and clinician may require the presence of another clinician during the encounter [30], highlighting the need for gender-sensitive approaches to care.
3.2.2. Clinician: (Lack of) Mentorship and Advocacy
Mentorship is an important aspect within medicine and among psychotherapists. Physicians often work in a team-based approach and turn to colleagues for mentorship, consult on clinical cases, and share knowledge from clinical experience. High-quality training, supervision, and emotional and technical support are paramount to the success of psychotherapy implementation in primary health care settings (see Supplementary File S6). For example, the CETA trial employed levels of outside (i.e., USA-based) monitoring and supervision that may not be feasible in other settings like low resource clinics. High levels of mentoring were necessary to ensure that CETA was delivered with fidelity by newly trained providers [29]. Notably, this intervention also adopted a task-shifting approach; however, it was recommended that counsellors and supervisors meet weekly to go over the details of each case [30], a level of mentorship that may not be feasible within every practice.
Further, psychotherapy sessions have the potential to be an avenue for advocacy, which is rarely recognized. For example, at the end of NET treatment, patients obtain a written version of their narrative [52]. This hard copy of their biography can then be used for advocacy, including court proceedings and the refugee determination process as well as a testimony to the atrocities lived by the refugee. Many patients submitted their narratives to the court of human rights as proof of the violations of human rights occurring in their countries [46,48]. This is an opportunity for patients to feel fulfilled by their therapeutic experience and is also an opportunity for primary care clinicians in high-income countries to contribute to advocacy for refugees.
3.2.3. Psychotherapy: Risk for Vicarious Trauma
Vicarious trauma is the secondary trauma encountered by mental health clinicians when working with patients with a history of trauma or PTSD. It is a process of internalizing the patient’s experiences through empathetic engagement and can lead to transformations within the clinician resulting in symptoms similar to that of the patient [53]. Given this risk, some psychotherapies may be better suited for non-professionals. For example, IPT does not involve detailed recounts of traumatic memories, thus reducing the risk of vicarious trauma compared to exposure therapies. In this respect, IPT may have a broader safety margin for delivery by lay therapists and providers in post-conflict communities [42].
3.2.4. Patient: Insecure Asylum Status
Precarious political status limits access to basic services, including primary care and mental health services. Insecure asylum status can lead to an ongoing sense of insecurity and injustice, further exacerbating symptoms of PTSD for patients with experience of trauma. Such insecurities can lead to fear and limited engagement with mental health interventions. For example, in a study examining the effectiveness of NET vs SIT (a form of Stress Management (SM)), the majority of patients were in a continuous state of fear of being deported and one participant went into hiding for fear of deportation [35]. Under such conditions of “continuous trauma”, SIT may not be an effective treatment. Transfer of the newly taught stress-reducing exercises to everyday stressful situations may not work where there is a serious ongoing threat [35]. In a trial of CETA, few mental health services were available to Burmese refugees in Thailand except counselling at the Burmese-run Mae Tao Clinic. Many Burmese refugees were reluctant to go to the clinic or other places due to fear of deportation by Thai authorities [29]. One study associated high patient dropout rate with forced repatriation and migration resettlement programs [47]. Finally, there is a possibility that being a refugee in a country that one perceives as responsible for one’s victimization generates conflicted feelings and resentment that might exacerbate the original trauma and hinder successful emotional processing of it [36].
4. Discussion
Mental health interventions are often embedded in social systems, and how they work is shaped by this socio-cultural context [54]. To our knowledge, this is the first realist-informed review to explore contextual factors that influence psychotherapy for refugees. Our findings recognize the integral role that culture plays in the presentation, identification, and treatment of trauma. Mental health consequences of trauma may be effectively addressed by a primary care program within the “medical home” and using a trauma-informed approach. A program may deliver a culturally adapted psychotherapy with sufficient intensity in a migrant-friendly environment. Meeting such program requirements necessitates a commitment to building clinician capacity, interdisciplinary human resource allocation, mentorship, and advocacy. Given that primary care clinicians are often the first point of contact for refugee patients, we argue that this program is best placed within primary care.
Several systematic reviews have examined the effectiveness of psychotherapies for refugees. NET and CBT have the most robust evidence base for refugee populations [55,56,57]. Interestingly, effect sizes for the effectiveness of NET are substantially larger when delivered by refugee community counselors as opposed to clinical practitioners [58]. However, the mechanisms by which this larger effect occurs remain unknown. Our realist synthesis suggests that a shared lived experience of trauma or shared culture between practitioners and patients may reduce stigma and improve understanding. Existing reviews also report that asylum seekers and displaced persons face the uncertainty of protection and fear of return to danger [59], and that insecure residence status increases the risk of mental health problems. As such, empirical evidence suggests that programs that are effective for PTSD in the general population may not completely overlap with those that are appropriate for PTSD in asylum seekers and refugees [57]. While trauma-focused therapies for refugees reduce symptoms of PTSD and depression, more research is needed on the role of cultural factors and programs in the treatment of refugee populations [60].
Clinicians have advocated for shifts away from the medicalization of mental health and towards cultural competence in trauma care [61]. Some authors have argued that the DSM V PTSD criteria do not align with presentations and may pathologize normal emotions, including justified anger, and impede the natural recovery of communities and true integration into new societies [56,62]. Furthermore, trauma-focused approaches may not adequately address the needs of refugees with psychosocial stressors such as poverty, changes in support networks due to loss and migration, unsafe living conditions, and poor access to basic resources [60]. Psychotherapies within the context of an interdisciplinary primary care program involving social workers, nurses, and cultural interpreters as well as encompassing different elements of therapy, such as CETA, may be able to target mental health conditions while simultaneously addressing some of the comorbid psychosocial stressors [29]. Increasingly, primary health care is being viewed as the gateway to support the social determinants of health [63,64,65]. Indeed, there is a gap that primary care clinicians can fill to embed global mental health into routine primary health care.
4.1. Strengths and Limitations
Our realist-informed review followed a transparent and systematic methodology [16,66]. This approach allowed us to develop an understanding of what works, for whom, in what circumstances and why. Rather than controlling for real-life events, our realist synthesis provided a framework for working with and untangling the complexity of real-life implementation of psychotherapies for refugees. This allowed for an equal focus on what works, as much as what does not work, in an attempt to learn from failures and maximize learning across policy, disciplinary and organizational boundaries.
Restriction of our inclusion criteria to randomized controlled trials allowed us to assess effectiveness but does not report on rich contextual qualitative factors. Further, no studies were conducted in primary health care, and the majority of studies poorly described their settings of care. We also focused on psychotherapies for individuals only. Primary health care systems are typically oriented to provide services for individuals. Programs must consider the impact of trauma on the whole family as many refugee families share a collective trauma experience, and their healing journey must also be a shared process. Finally, although publication in a language other than English was not an exclusion criterion for studies, we did not search dedicated non-English language databases. Work with refugee populations is relevant across cultures, and we recognize additional evidence in this topic area may exist.
4.2. Implications for Research and Practice
As refugees settle and seek community-based care, they encounter barriers including poor access to mental health specialists. Primary care clinicians are well positioned to screen, diagnose, and manage refugees with complex mental health conditions. At the same time, primary health care clinicians are developing innovative interdisciplinary programs, for example pain management, diabetes, and palliative care. Mental health care of refugees is indeed complex and deserves interdisciplinary programs that can reduce stigma, improve access and adherence, build interdisciplinary care, and develop psychotherapy skills [67,68,69,70]. Links to cultural psychologists and psychiatrists will also improve diagnostics and treatment plans.
Task shifting [71], program composition and management, and refugee community engagement will all need research. Referral to specialized psychological services outside primary care, when access to interpreters and cultural brokers is not guaranteed, will also require community-based research. Community engagement research is needed to study adherence, follow-up, and stigma that can lead to poor mental health outcomes.
5. Conclusions
Our review identified practice, clinician, psychotherapy, and patient factors that contribute to the success and failure of psychotherapy for refugees. Several psychotherapies reduced symptoms and led to improved function and well-being in refugees. Task-shifting to primary care may help ease wait times, reduce mental health stigma, and build a community based “medical home”. However, the implementation of psychotherapy programs in primary care faces numerous logistic, clinical, and remuneration challenges. Empowering primary-care clinicians with the necessary skills, language, and program supports and knowledge may improve refugee care and reduce unnecessary specialist referrals.
Supplementary Materials
The following are available online at https://www.mdpi.com/1660-4601/17/13/4618/s1. Table S1, RAMESES Publication Standards: Realist Synthesis; Table S2, Inclusion and exclusion criteria; Table S3, Search strategy; File S4, Critical appraisal; Table S5, Effectiveness of psychotherapies; Table S6, Key elements and provider training.
Author Contributions
Conceptualization, D.G. and K.P.; methodology, D.G., K.P., L.B., and O.M.; formal analysis, O.M. and L.D.; data curation, D.G., K.P., S.A., L.B., L.D., and O.M.; writing—original draft preparation, O.M., S.A., and D.G.; writing—review and editing, all authors. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
The authors would like to thank Ammar Saad (Bruyère Research Institute, Ottawa, ON K1R 6M1, Canada) and Amanda Hanemaayer (University of Guelph, Guelph, ON N1G 2W1, Canada) for assistance with critical appraisal and creation of tables.
Conflicts of Interest
The authors declare no conflict of interest.
References
- UNHCR. Figures at a Glance; UNCHR: Geneva, Switzerland, 2019.
- Kirmayer, L.J.; Narasiah, L.; Munoz, M.; Rashid, M.; Ryder, A.G.; Guzder, J.; Hassan, G.; Rousseau, C.; Pottie, K. Common mental health problems in immigrants and refugees: General approach in primary care. Cmaj 2011, 183, E959–E967. [Google Scholar] [CrossRef] [PubMed]
- Becker, A.E.; Kleinman, A. The history of cultural psychiatry in the last half-century. In Psychiatry Past, Present Prospect; Oxford University Press: Oxford, UK, 2014; pp. 74–95. [Google Scholar]
- Regel, S.; Berliner, P. Current perspectives on assessment and therapy with survivors of torture: The use of a cognitive behavioural approach. Eur. J. Psychother. Couns. 2007, 9, 289–299. [Google Scholar] [CrossRef]
- Kanagaratnam, P.; Pain, C.; McKenzie, K.; Ratnalingam, N.; Toner, B. Recommendations for Canadian mental health practitioners working with war-exposed immigrants and refugees. Can. J. Community Ment. Health 2017, 36, 107–119. [Google Scholar] [CrossRef][Green Version]
- Ivbijaro, G. Report: WONCA working party on mental health. Ment. Health Fam. Med. 2009, 6, 63. [Google Scholar]
- Lesage, A. Prevalence of Mental Illnesses and Related Service Utilization in Canada: An Analysis of The Canadian Community Health Survey; Canadian Collaborative Mental Health Initiative: Hamilton, ON, Canada, 2006. [Google Scholar]
- Durbin, A.; Moineddin, R.; Lin, E.; Steele, L.S.; Glazier, R.H. Mental health service use by recent immigrants from different world regions and by non-immigrants in Ontario, Canada: A cross-sectional study. BMC Health Serv. Res. 2015, 15, 336. [Google Scholar] [CrossRef] [PubMed]
- Aery, A.; McKenzie, K. Primary Care Utilization Trajectories for Immigrants and Refugees in Ontario Compared with Longterm Residents; Wellesley Institute: Toronto, ON, Canada, 2018. [Google Scholar]
- Pumariega, A.J.; Rothe, E.; Pumariega, J.B. Mental health of immigrants and refugees. Community Ment. Health J. 2005, 41, 581–597. [Google Scholar] [CrossRef] [PubMed]
- Butz, A. Use of health diaries in pediatric research. J. Pediatr. Heal. Care 2004, 18, 262–263. [Google Scholar]
- Andrulis, D.P.; Brach, C. Integrating literacy, culture, and language to improve health care quality for diverse populations. Am. J. Health Behav. 2007, 31 (Suppl. S1), S122–S133. [Google Scholar] [CrossRef] [PubMed]
- Wayland, S.V. The Housing Needs of Immigrants and Refugees in Canada; Canadian Housing and Renewal Association Ottawa: Ottawa, ON, Canada, 2007. [Google Scholar]
- Agic, B.; McKenzie, K.; Tuck, A.; Antwi, M. Supporting the Mental Health of Refugees to Canada; Mental Health Commission of Canada: Ottawa, ON, Canada, 2016. [Google Scholar]
- Rycroft-Malone, J.; McCormack, B.; Hutchinson, A.M.; DeCorby, K.; Bucknall, T.K.; Kent, B.; Schultz, A.; Snelgrove-Clarke, E.; Stetler, C.B.; Titler, M.; et al. Realist synthesis: Illustrating the method for implementation research. Implement. Sci. 2012, 7, 33. [Google Scholar] [CrossRef]
- Pawson, R. Realistic Evaluation; SAGE Publications: New York, NY, USA, 1997; p. 256. [Google Scholar]
- Greenhalgh, T.; Kristjansson, E.; Robinson, V. Realist review to understand the efficacy of school feeding programmes. BMJ 2007, 335, 858–861. [Google Scholar] [CrossRef]
- Wong, G.; Greenhalgh, T.; Westhorp, G.; Buckingham, J.; Pawson, R. RAMESES publication standards: Meta-narrative reviews. BMC Med. 2013, 11, 20. [Google Scholar]
- Glasgow, R.E.; Vogt, T.M.; Boles, S.M. Evaluating the public health impact of health promotion interventions: The RE-AIM framework. Am. J. Public Health 1999, 89, 1322–1327. [Google Scholar] [CrossRef] [PubMed]
- Substance Abuse and Mental Health Services Administration. SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach; SAMHSA: Rockville, MD, USA, 2014. [Google Scholar]
- Akobeng, A.K. Understanding randomised controlled trials. Arch. Dis. Child. 2005, 90, 840–844. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G. Assessing risk of bias in included studies. In Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series; John Wiley & Sons: Chichester, UK, 2008; pp. 187–241. [Google Scholar]
- Dalkin, S.M.; Greenhalgh, J.; Jones, D.; Cunningham, B.; Lhussier, M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement. Sci. 2015, 10, 49. [Google Scholar] [CrossRef] [PubMed]
- Westhorp, G. Realist Impact Evaluation: An. Introduction; Overseas Development Institute: London, UK, 2014. [Google Scholar]
- Adenauer, H.; Catani, C.; Gola, H.; Keil, J.; Ruf, M.; Schauer, M.; Neuner, F. Narrative exposure therapy for PTSD increases top-down processing of aversive stimuli-evidence from a randomized controlled treatment trial. BMC Neurosci. 2011, 12, 127. [Google Scholar] [CrossRef]
- Schauer, M.; Neuner, F.; Elbert, T. Narrative exposure therapy for children and adolescents (KIDNET). In Evidence-Based Treatments for Trauma Related Disorders in Children and Adolescents; Springer: Berlin, Germany, 2017; pp. 227–250. [Google Scholar]
- Elbert, T.; Schauer, M.; Neuner, F. Narrative exposure therapy (NET): Reorganizing memories of traumatic stress, fear, and violence. In Evidence Based Treatments for Trauma-Related Psychological Disorders; Springer: Berlin, Germany, 2015; pp. 229–253. [Google Scholar]
- Bolton, P.; Lee, C.; Haroz, E.E.; Murray, L.; Dorsey, S.; Robinson, C.; Ugueto, A.M.; Bass, J. A transdiagnostic community-based mental health treatment for comorbid disorders: Development and outcomes of a randomized controlled trial among Burmese refugees in Thailand. PLoS Med. 2014, 11, e1001757. [Google Scholar] [CrossRef]
- Murray, L.K.; Dorsey, S.; Haroz, E.; Lee, C.; Alsiary, M.M.; Haydary, A.; Weiss, W.M.; Bolton, P. A common elements treatment approach for adult mental health problems in low-and middle-income countries. Cogn. Behav. Pract. 2014, 21, 111–123. [Google Scholar] [CrossRef]
- Carlsson, J.; Sonne, C.; Vindbjerg, E.; Mortensen, E.L. Stress management versus cognitive restructuring in trauma-affected refugees—A pragmatic randomised study. Psychiatry Res. 2018, 266, 116–123. [Google Scholar] [CrossRef] [PubMed]
- Vindbjerg, E. Psychotherapy with traumatised refugees—The design of a randomised clinical trial. Torture. J. 2014, 24, 9. [Google Scholar] [CrossRef]
- Lehrer, P.M.; Woolfolk, R.L.; Sime, W.E. Principles and Practice of Stress Management; The Guilford Press: New York, NY, USA, 2008. [Google Scholar]
- Andersen, I. Psykoterapimanual III Individuel Psykoterapi Til Flygtninge Med PTSD og Depression—Manual Baseret på Stress Management; Psykiatrisk Traumeklinik for Flygtninge: Copenhagen, Denmark, 2011. [Google Scholar]
- Hensel-Dittmann, D.; Schauer, M.; Ruf, M.; Catani, C.; Odenwald, M.; Elbert, T.; Neuner, F. Treatment of traumatized victims of war and torture: A randomized controlled comparison of narrative exposure therapy and stress inoculation training. Psychother Psychosom. 2011, 80, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Hijazi, A.M.; Lumley, M.A.; Ziadni, M.S.; Haddad, L.; Rapport, L.J.; Arnetz, B.B. Brief narrative exposure therapy for posttraumatic stress in Iraqi refugees: A preliminary randomized clinical trial. J. Trauma. Stress 2014, 27, 314–322. [Google Scholar] [CrossRef]
- Hinton, D.E.; Hofmann, S.G.; Pollack, M.H.; Otto, M.W. Mechanisms of efficacy of CBT for Cambodian refugees with PTSD: Improvement in emotion regulation and orthostatic blood pressure response. CNS Neurosci. Ther. 2009, 15, 255–263. [Google Scholar] [CrossRef]
- Hinton, D.E.; Patel, A. Cultural adaptations of cognitive behavioral therapy. Psychiatr. Clin. 2017, 40, 701–714. [Google Scholar] [CrossRef] [PubMed]
- Hinton, D.; Jalal, B. Guidelines for the implementation of culturally sensitive cognitive behavioural therapy among refugees and in global contexts. Intervention 2014, 12, 78–93. [Google Scholar] [CrossRef]
- Hinton, D.E.; Chhean, D.; Pich, V.; Safren, S.A.; Hofmann, S.G.; Pollack, M.H. A randomized controlled trial of cognitive-behavior therapy for Cambodian refugees with treatment-resistant PTSD and panic attacks: A cross-over design. J. Trauma. Stress Off. Publ. Int. Soc. Trauma. Stress Stud. 2005, 18, 617–629. [Google Scholar] [CrossRef] [PubMed]
- Hinton, D.E.; Pham, T.; Tran, M.; Safren, S.A.; Otto, M.W.; Pollack, M.H. CBT for Vietnamese refugees with treatment-resistant PTSD and panic attacks: A pilot study. J. Trauma. Stress Off. Publ. Int Soc. Trauma Stress Stud. 2004, 17, 429–433. [Google Scholar] [CrossRef] [PubMed]
- Meffert, S.M.; Abdo, A.O.; Alla, O.A.A.; Elmakki, Y.O.M.; Omer, A.A.; Yousif, S.; Metzler, T.J.; Marmar, C.R. A pilot randomized controlled trial of interpersonal psychotherapy for Sudanese refugees in Cairo, Egypt. Psychol. Trauma. Theory Res. Pract. Policy. 2014, 6, 240. [Google Scholar] [CrossRef]
- Stuart, S. Interpersonal psychotherapy: A guide to the basics. Psychiatr. Ann. 2006, 36. [Google Scholar] [CrossRef]
- Stuart, S. Interpersonal Psychotherapy: A Clinician’s Guide, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2012. [Google Scholar]
- Weissman, M.M.; Markowitz, J.C.; Klerman, G. Comprehensive Guide to Interpersonal Psychotherapy; Basic Books: New York, NY, USA, 2008. [Google Scholar]
- Neuner, F.; Kurreck, S.; Ruf, M.; Odenwald, M.; Elbert, T.; Schauer, M. Can asylum-seekers with posttraumatic stress disorder be successfully treated? A randomized controlled pilot study. Cogn. Behav. Ther. 2010, 39, 81–91. [Google Scholar] [CrossRef]
- Neuner, F.; Onyut, P.L.; Ertl, V.; Odenwald, M.; Schauer, E.; Elbert, T. Treatment of posttraumatic stress disorder by trained lay counselors in an African refugee settlement: A randomized controlled trial. J. Consult. Clin. Psychol. 2008, 76, 686. [Google Scholar] [CrossRef]
- Neuner, F.; Schauer, M.; Klaschik, C.; Karunakara, U.; Elbert, T. A comparison of narrative exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress disorder in an african refugee settlement. J. Consult. Clin. Psychol. 2004, 72, 579. [Google Scholar] [CrossRef] [PubMed]
- Paunovic, N.; Öst, L.-G. Cognitive-behavior therapy vs exposure therapy in the treatment of PTSD in refugees. Behav. Res. Ther. 2001, 39, 1183–1197. [Google Scholar] [CrossRef]
- Stenmark, H.; Catani, C.; Neuner, F.; Elbert, T.; Holen, A. Treating PTSD in refugees and asylum seekers within the general health care system. A randomized controlled multicenter study. Behav. Res. Ther. 2013, 51, 641–647. [Google Scholar] [CrossRef] [PubMed]
- Halvorsen, J.Ø.; Stenmark, H.; Neuner, F.; Nordahl, H.M. Does dissociation moderate treatment outcomes of narrative exposure therapy for PTSD? A secondary analysis from a randomized controlled clinical trial. Behav. Res. Ther. 2014, 57, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Onyut, L.P.; Neuner, F.; Schauer, E.; Ertl, V.; Odenwald, M.; Schauer, M.; Elbert, T. Narrative exposure therapy as a treatment for child war survivors with posttraumatic stress disorder: Two case reports and a pilot study in an African refugee settlement. BMC Psychiatry 2005, 5, 7. [Google Scholar] [CrossRef] [PubMed]
- Cohen, K.; Collens, P. The impact of trauma work on trauma workers: A metasynthesis on vicarious trauma and vicarious posttraumatic growth. Psychol. Trauma. Theory Res. Pract. Policy. 2013, 5, 570. [Google Scholar] [CrossRef]
- Kleinman, A. Writing at the Margin: Discourse between Anthropology and Medicine; University of California Press: Berkeley, CA, USA, 1995. [Google Scholar]
- Lely, J.C.G.; Smid, G.E.; Jongedijk, R.A.; Knipscheer, J.W.; Kleber, R.J. The effectiveness of narrative exposure therapy: A review, meta-analysis and meta-regression analysis. Eur. J. Psychotraumatol. 2019, 10, 1550344. [Google Scholar] [CrossRef]
- Crumlish, N.; O’Rourke, K. A systematic review of treatments for post-traumatic stress disorder among refugees and asylum-seekers. J. Nerv. Ment. Dis. 2010, 198, 237–251. [Google Scholar] [CrossRef]
- Nosè, M.; Ballette, F.; Bighelli, I.; Turrini, G.; Purgato, M.; Tol, W.; Priebe, S.; Barbui, C. Psychosocial interventions for post-traumatic stress disorder in refugees and asylum seekers resettled in high-income countries: Systematic review and meta-analysis. PLoS ONE 2017, 12, e0171030. [Google Scholar] [CrossRef]
- Gwozdziewycz, N.; Mehl-Madrona, L. Meta-analysis of the use of narrative exposure therapy for the effects of trauma among refugee populations. Perm. J. 2013, 17, 70. [Google Scholar] [PubMed]
- McFarlane, C.A.; Kaplan, I. Evidence-based psychological interventions for adult survivors of torture and trauma: A 30-year review. Transcult. Psychiatry 2012, 49, 539–567. [Google Scholar] [CrossRef] [PubMed]
- Lambert, J.E.; Alhassoon, O.M. Trauma-focused therapy for refugees: Meta-analytic findings. J. Couns. Psychol. 2015, 62, 28. [Google Scholar] [CrossRef]
- Kidron, C.A.; Kirmayer, L.J. Global mental health and idioms of distress: The paradox of culture-sensitive pathologization of distress in Cambodia. Cult. Med. Psychiatry 2019, 43, 211–235. [Google Scholar] [CrossRef]
- Summerfield, D. A critique of seven assumptions behind psychological trauma programmes in war-affected areas. Soc. Sci. Med. 1999, 48, 1449–1462. [Google Scholar] [CrossRef]
- Andermann, A. Screening for social determinants of health in clinical care: Moving from the margins to the mainstream. Public Health Rev. 2018, 39, 19. [Google Scholar] [CrossRef]
- Pinto, A.D.; Bloch, G. Framework for building primary care capacity to address the social determinants of health. Can. Fam. Physician 2017, 63, e476–e482. [Google Scholar]
- Allen, L. Leveraging primary care to address social determinants. Lancet Public Health 2018, 3, e466. [Google Scholar] [CrossRef]
- Pawson, R.; Greenhalgh, T.; Harvey, G.; Walshe, K. Realist review-a new method of systematic review designed for complex policy interventions. J. Health Serv. Res. Policy 2005, 10 (Suppl. S1), 21–34. [Google Scholar] [CrossRef]
- Salami, B.; Salma, J.; Hegadoren, K. Access and utilization of mental health services for immigrants and refugees: Perspectives of immigrant service providers. Int. J. Ment. Health Nurs. 2019, 28, 152–161. [Google Scholar] [CrossRef]
- Wylie, L.; Van Meyel, R.; Harder, H.; Sukhera, J.; Luc, C.; Ganjavi, H.; Elfakhani, M.; Wardrop, N. Assessing trauma in a transcultural context: Challenges in mental health care with immigrants and refugees. Public Health Rev. 2018, 39, 1–19. [Google Scholar] [CrossRef] [PubMed]
- McKeary, M.; Newbold, B. Barriers to care: The challenges for Canadian refugees and their health care providers. J. Refug. Stud. 2010, 23, 523–545. [Google Scholar] [CrossRef]
- Kates, N.; Mazowita, G.; Lemire, F.; Jayabarathan, A.; Bland, R.; Selby, P.; Isomura, T.; Craven, M.; Gervais, M.; Audet, D. The evolution of collaborative mental health care in Canada: A shared vision for the future. Can. J. Psychiatry 2011, 56, I1. [Google Scholar] [CrossRef][Green Version]
- Kohrt, B.A.; Jordans, M.J.D.; Turner, E.L.; Sikkema, K.J.; Luitel, N.P.; Rai, S.; Singla, D.R.; Lamichhane, J.; Lund, C.; Patel, V. Reducing stigma among healthcare providers to improve mental health services (RESHAPE): Protocol for a pilot cluster randomized controlled trial of a stigma reduction intervention for training primary healthcare workers in Nepal. Pilot Feasibility Stud. 2018, 4, 36. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).