Telehealth Needs and Concerns of Stakeholders in Pediatric Palliative Home Care
Abstract
1. Introduction
- information about PPHC for new patients;
- care network coordination;
- support services [17].
2. Materials and Methods
2.1. Study I: PPHC Teams
2.1.1. Participants
2.1.2. Materials and Procedure
2.2. Study II: Families
2.2.1. Participants
2.2.2. Materials and Procedure
2.3. Study I & Study II: Qualitative Analysis
2.4. Study III: Other Stakeholders
2.5. Study I-III: Quantitative Analysis
3. Results
3.1. Recruited Stakeholders
3.2. Needs
- data transmission;
- video consultation;
- access to the patient records.
- 4.
- symptom questionnaires;
- 5.
- communication support;
- 6.
- shared calendar;
- 7.
- informational materials;
- 8.
- electronic stethoscope.
3.3. Basic Needs
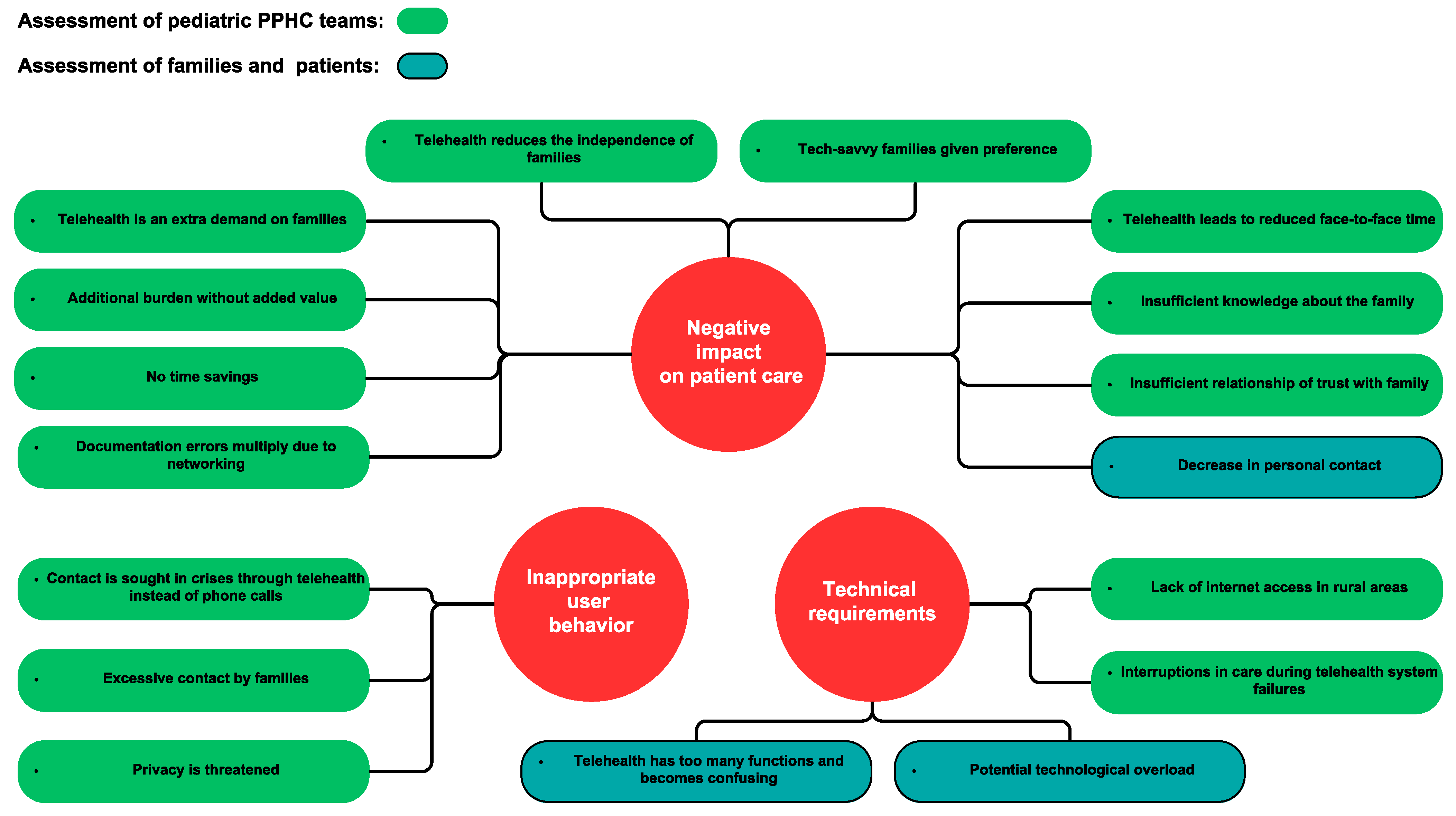
3.4. Concerns
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Content | |
|---|---|
| Phase 1 | Address of welcome |
| Phase 2 | Participants fill out the written consent forms |
| Phase 3 | Introduction: (5–10 min)
|
| Phase 4 | Warming up: Flash light (state first name for transcript): “If you could quit doing one task in your job, what one task would you like to give up?”
|
| Phase 5 | Main part Consider occupational group differences: -relationship -affinity for technology -hierarchy. Topic block A:
1. Question: What properties should the app have to do its job as well as possible?
|
| Phase 6 | End: conclusion and thank you |
| Characteristics (n = 15) | Total (n = 15) | Ongoing PPHC 1 (n = 9) | Patient Deceased (n = 3) | Self-Reporting Patients (n = 3) | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Gender | ||||||||
| Female | 2 | 13.3% | 2 | 22.2% | 0 | 0.0% | 0 | 0.0% |
| Male | 13 | 86.7% | 7 | 77.8% | 3 | 100% | 3 | 100% |
| Age | ||||||||
| 0–1 month | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| 2–11 months | 5 | 33.3% | 4 | 44.4% | 1 | 33.3% | 0 | 0.0% |
| 1–9 years | 5 | 33.3% | 4 | 44.4% | 1 | 33.3% | 0 | 0.0% |
| 10–18 years | 2 | 13.3% | 1 | 11.1% | 1 | 33.3% | 0 | 0.0% |
| Older than 18 years | 3 | 20 % | 0 | 0.0% | 0 | 0.0% | 3 | 100% |
| Migration background | 5 | 33.3% | 5 | 55.6% | 0 | 0.0% | 0 | 0.0% |
| Living conditions | ||||||||
| With both parents | 14 | 93.3% | 8 | 88.9% | 3 | 100% | 3 | 100% |
| With only one parent | 1 | 6.7% | 1 | 11.1% | 0 | 0.00% | 0 | 0.0% |
| Siblings with life-limiting illness | 2 | 13.3% | 2 | 22.2% | 0 | 0.0% | 0 | 0.0% |
| Assistance | ||||||||
| Friends and family | 5 | 33.3% | 3 | 33.3% | 0 | 0.0% | 2 | 66.7% |
| Pediatrician in private practice | 9 | 60% | 5 | 55.6% | 2 | 66.7% | 2 | 66.7% |
| Naturopathy | 3 | 20% | 3 | 33.3% | 0 | 0.0% | 0 | 0.0% |
| Social Service | 1 | 6.7% | 0 | 0.0% | 0 | 0.0% | 1 | 33.3% |
| Family support | 1 | 6.7% | 1 | 11,1% | 0 | 0.0% | 0 | 0.0% |
| Outpatient hospice services | 9 | 60% | 6 | 66.7% | 1 | 33.3% | 2 | 66.7% |
| Psychological support | 6 | 40% | 4 | 44.4% | 2 | 66.7% | 0 | 0.0% |
| Grief counseling | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Religious support | 2 | 13.3% | 2 | 22.2% | 0 | 0.0% | 0 | 0.0% |
| Diagnoses (n = 15) | n | % | Comparative Study (n = 75 1) % |
|---|---|---|---|
| Neuromuscular diseases | 4 | 26.67 | 37.0 |
| Neurodegenerative diseases | 1 | 6.67 | 12.0 |
| Metabolic disorders | 3 | 20 | / |
| Heart disease | 3 | 20 | 8.0 |
| Chromosomal changes | 1 | 6.67 | 8.0 |
| Oncological diseases | 3 | 20 | 28.1 |
| comprising: | |||
| Solid tumor | 1 | 6.67 | 14.7 |
| Brain tumor | 1 | 6.67 | 10.7 |
| Leukemia | 1 | 6.67 | 2.7 |
| Other | / | / | 4.0 |
| Prioritization of Needs from Interviews with Patients and Family Members | Prioritization of Needs from Focus Groups of PPHC 1 Teams | |
|---|---|---|
| Very high | Positive and/or somewhat positive evaluation in at least 2/3 of the cases, no negative assessment | Positive and/or somewhat positive evaluation in more than 2/3 of the cases, no negative assessment |
| High | Positive or somewhat positive evaluation in at least 2/3 of the cases | Positive or somewhat positive evaluation, no negative assessment |
| Medium | Positive and/or somewhat positive evaluation in more than 1/3 of the cases | More positive than negative assessments |
| Low | Positive and/or rather positive evaluation in 1/3 of the cases or less | Predominantly negative assessments |
| Messenger | Transmission of Vital Signs Monitor Signal | Shared Calendar | |
|---|---|---|---|
| Further member check feedback | Clear communication rules necessary | Association with curative care feared Not necessary in PPHC 1 | Highly desired by staff who schedule home visits, other team members neutral as it is less relevant to their own tasks |
| Expected likelihood of future use | |||
| Average feedback | ++ | - | +/− |
| comprising: | |||
| Strongly agree | 7 | 2 | 1 |
| Agree | - | - | - |
| Undecided | - | - | 2 |
| Disagree | - | - | 1 |
| Strongly disagree | - | 4 | 1 |
| Need | Mention in the Focus Groups | Evaluation of the PPHC 1 Teams in the Focus Groups. | Priority Focus Groups 2,3 | Family Mentions | Evaluation of the Families | Priority of Families 2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ++ | + | +/- | - | -- | ++ | + | +/- | - | -- | |||||
| Data transmission | 3/3 focus groups | 3 | 0 | 0 | 0 | 0 | Very high | 10/15 families | 9 | 1 | 0 | 0 | 0 | Very high |
| Video consultation | 3/3 focus groups | 3 | 0 | 0 | 0 | 0 | Very high | 14/15 families | 12 | 1 | 0 | 1 | 0 | High |
| Access to patient record | 3/3 focus groups | 2 | 1 | 0 | 0 | 0 | Very high | 10/15 families | 6 | 3 | 0 | 1 | 0 | Medium |
| Symptom questionnaires | 2/3 focus groups | 2 | 0 | 0 | 0 | 0 | High | 13/ 15 families | 10 | 2 | 0 | 0 | 1 | High |
| Communication support | 2/3 focus groups | 2 | 0 | 0 | 0 | 0 | High | 3/3 families 4 | 1 | 1 | 0 | 0 | 1 | High |
| Shared calendar | 2/3 focus groups | 1 | 1 | 0 | 0 | 0 | High | 6/15 families | 5 | 0 | 1 | 0 | 0 | Low |
| Information materials | 3/3 focus groups | 2 | 0 | 0 | 1 | 0 | Medium | 12/15 families | 9 | 2 | 0 | 0 | 1 | High |
| Electronic stethoscope | 3/3 focus groups | 0 | 2 | 0 | 1 | 0 | Medium | 12/15 families | 9 | 2 | 0 | 1 | 0 | High |
| Messenger | 1/3 focus groups | 0 | 0 | 0 | 1 | 0 | Low | 7/15 families | 3 | 4 | 0 | 0 | 0 | Medium |
| Caregivers with Ongoing PPHC 1 Relative Frequencies of Agreement | Bereaved Caregivers Relative Frequencies of Agreement | Self-Reporting Patient Relative Frequencies of Agreement | |
|---|---|---|---|
| (n = 9) | (n = 3) | (n = 3) | |
| Messenger | |||
| chat with… | |||
| …other patients | 11.1% | 0% | 33.3% |
| …other parents | 44.4% | 33.3% | 33.3% |
| …PPHC 1 team | 88.9% | 66.7% | 100% |
| …other service providers | 44.4% | 0% | 33.3% |
| Information materials | |||
| necessary topics: | |||
| Medical | 88.9% | 33.3% | 33.3% |
| Nursing | 88.9% | 66.7% | 66.7% |
| Naturopathy | 66.7% | 0% | 0% |
| Social law | 100% | 66.7% | 33.3% |
| Children’s hospices | 88.9% | 66.7% | 33.3% |
| Psychological Coping strategies | 44.4% | 66.7% | 33.3% |
| Bidding farewell | 44.4% | 66.7% | 33.3% |
| Last wishes | 33.3% | 66.7% | 33.3% |
| Recognizing the dying process | 44.4% | 100% | - |
| Actions in case of death | 33.3% | 100% | - |
| Patient record | |||
| access to: | |||
| View entries | 77.8% | 33.3% | 66.7% |
| Create tasks | 44.4% | 33.3% | 66.7% |
| Update contact details | 55.6% | 33.3% | 33.3% |
| Drug chart/Discharge letters | 88.9% | 66.7% | 100% |
| Common calendar | 55.6% | 66.7% | 66.7% |
| Video consultation | |||
| for contacts… | |||
| …in crisis situations | 77.8% | 100% | 33.3% |
| …in routine care | 66.7% | 66.7% | 66.7% |
| …for psychological counselling | 22.2% | 0% | 33.3% |
| Data transmission | |||
| of: | |||
| Electronic stethoscope | 66.7% | 66.7% | 33.3% |
| Vital signs monitor signal | 66.7% | 100% | 66.7% |
| Medical event Documentation/symptom Questionnaire | 88.9% | 100% | 100% |
| Pictures, videos, documents | 77.8% | 66.7% | 66.7% |
References
- Marcus, K.L.; Santos, G.; Ciapponi, A.; Comandé, D.; Bilodeau, M.; Wolfe, J.; Dussel, V. Impact of Specialized Pediatric Palliative Care: A Systematic Review. J. Pain Symptom Manag. 2020, 59, 339–364.e10. [Google Scholar] [CrossRef]
- Kaye, E.C.; Rubenstein, J.; Levine, D.; Baker, J.N.; Dabbs, D.; Friebert, S.E. Pediatric palliative care in the community. CA Cancer J. Clin. 2015, 65, 316–333. [Google Scholar] [CrossRef]
- Higginson, I.J.; Hart, S.; Koffman, J.; Selman, L.; Harding, R. Needs assessments in palliative care: An appraisal of definitions and approaches used. J. Pain Symptom Manag. 2007, 33, 500–505. [Google Scholar] [CrossRef]
- Phillips, J.L.; Davidson, P.M.; Newton, P.J.; Digiacomo, M. Supporting patients and their caregivers after-hours at the end of life: The role of telephone support. J. Pain Symptom Manag. 2008, 36, 11–21. [Google Scholar] [CrossRef]
- Holmen, H.; Riiser, K.; Winger, A. Home-Based Pediatric Palliative Care and Electronic Health: Systematic Mixed Methods Review. J. Med. Internet Res. 2020, 22, e16248. [Google Scholar] [CrossRef]
- May, S.; Bruch, D.; Gehlhaar, A.; Linderkamp, F.; Stahlhut, K.; Heinze, M.; Allsop, M.; Muehlensiepen, F. Digital technologies in routine palliative care delivery: An exploratory qualitative study with health care professionals in Germany. BMC Health Serv. Res. 2022, 22, 1516. [Google Scholar] [CrossRef]
- Burke, B.L.; Hall, R.W. Telemedicine: Pediatric Applications. Pediatrics 2015, 136, e293–e308. [Google Scholar] [CrossRef]
- Preminger, T.J. Telemedicine in pediatric cardiology: Pros and cons. Curr. Opin. Pediatr. 2022, 34, 484–490. [Google Scholar] [CrossRef]
- Lo, M.D.; Gospe, S.M. Telemedicine and Child Neurology. J. Child Neurol. 2019, 34, 22–26. [Google Scholar]
- Da Fonseca, M.H.; Kovaleski, F.; Picinin, C.T.; Pedroso, B.; Rubbo, P. E-Health Practices and Technologies: A Systematic Review from 2014 to 2019. Healthcare 2021, 9, 1192. [Google Scholar] [CrossRef]
- Souza-Junior, V.D.; Mendes, I.A.C.; Mazzo, A.; Godoy, S. Application of telenursing in nursing practice: An integrative literature review. Appl. Nurs. Res. 2016, 29, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Doyen, C.M.; Oreve, M.-J.; Desailly, E.; Goupil, V.; Zarca, K.; L’Hermitte, Y.; Chaste, P.; Bau, M.-O.; Beaujard, D.; Haddadi, S.; et al. Telepsychiatry for Children and Adolescents: A Review of the PROMETTED Project. Telemed. J. E Health 2018, 24, 3–10. [Google Scholar] [CrossRef]
- Nolte-Buchholtz, S.; Zernikow, B.; Wager, J. Pediatric Patients Receiving Specialized Palliative Home Care According to German Law: A Prospective Multicenter Cohort Study. Children 2018, 5, 66. [Google Scholar] [CrossRef]
- German Federal Ministry of Health. Telemedizinische Methoden in der Patientenversorgung—Begriffliche Verortung: Erarbeitet von der AG-Telemedizin und beschlossen vom Vorstand der Bundesärztekammer am 20.03.2015. Available online: https://www.bundesaerztekammer.de/fileadmin/user_upload/_old-files/downloads/pdf-Ordner/Telemedizin_Telematik/Telemedizin/Telemedizinische_Methoden_in_der_Patientenversorgung_Begriffliche_Verortung.pdf (accessed on 1 June 2023).
- Kufel, J.; Bargieł, K.; Koźlik, M.; Czogalik, Ł.; Dudek, P.; Jaworski, A.; Magiera, M.; Bartnikowska, W.; Cebula, M.; Nawrat, Z.; et al. Usability of Mobile Solutions Intended for Diagnostic Images-A Systematic Review. Healthcare 2022, 10, 2040. [Google Scholar] [CrossRef]
- Miller, K.A.; Baird, J.; Lira, J.; Herrera Eguizabal, J.; Fei, S.; Kysh, L.; Lotstein, D. The Use of Telemedicine for Home-Based Palliative Care for Children With Serious Illness: A Scoping Review. J. Pain Symptom Manag. 2021, 62, 619–636. [Google Scholar] [CrossRef]
- Lotstein, D.; Eguizabal, J.H.; Baird, J.; Bemis, H.; Lira, J. Using a Stakeholder Co-Design Framework to Develop a Pediatric Telemedicine Home-Based Palliative Care Model (TH156). J. Pain Symptom Manag. 2022, 63, 798–799. [Google Scholar] [CrossRef]
- Zoom Support. Lokale Zoom-Bereitstellung. Available online: https://support.zoom.us/hc/de/articles/360034064852-Lokale-Zoom-Bereitstellung (accessed on 1 June 2023).
- Mayring, P. Philipp Mayring: Qualitative Content Analysis. Theoretical Foundation, Basic Procedures and Software Solution. Available online: https://nbn-resolving.org/urn:nbn:de:0168-ssoar-395173 (accessed on 1 June 2023).
- Schreier, M. Qualitative Content Analysis in Practice; Sage: London, UK, 2012; ISBN 9781849205931. [Google Scholar]
- Brennan, R.L.; Prediger, D.J. Coefficient Kappa: Some Uses, Misuses, and Alternatives. Educ. Psychol. Meas. 1981, 41, 687–699. [Google Scholar] [CrossRef]
- Ostrowski-Delahanty, S.A.; McNinch, N.L.; Grossoehme, D.H.; Aultman, J.; Spalding, S.; Wagoner, C.; Rush, S. Understanding Drivers of Telemedicine in Pediatric Medical Care. Telemed. J. E Health 2023, 29, 726–737. [Google Scholar] [CrossRef]
- Lundereng, E.D.; Nes, A.A.G.; Holmen, H.; Winger, A.; Thygesen, H.; Jøranson, N.; Borge, C.R.; Dajani, O.; Mariussen, K.L.; Steindal, S.A. Health Care Professionals’ Experiences and Perspectives on Using Telehealth for Home-based Palliative Care: Scoping Review. J. Med. Internet Res. 2023, 25, e43429. [Google Scholar] [CrossRef]
- Harris, N.; Beringer, A.; Fletcher, M. Families’ priorities in life-limiting illness: Improving quality with online empowerment. Arch. Dis. Child. 2016, 101, 247–252. [Google Scholar] [CrossRef]
- Kaplan, B. Revisiting health information technology ethical, legal, and social issues and evaluation: Telehealth/telemedicine and COVID-19. Int. J. Med. Inform. 2020, 143, 104239. [Google Scholar] [CrossRef] [PubMed]
- Bradford, N.K.; Young, J.; Armfield, N.R.; Herbert, A.; Smith, A.C. Home telehealth and paediatric palliative care: Clinician perceptions of what is stopping us? BMC Palliat. Care 2014, 13, 29. [Google Scholar] [CrossRef] [PubMed]
- Collier, A.; Morgan, D.D.; Swetenham, K.; To, T.H.M.; Currow, D.C.; Tieman, J.J. Implementation of a pilot telehealth programme in community palliative care: A qualitative study of clinicians’ perspectives. Palliat. Med. 2016, 30, 409–417. [Google Scholar] [CrossRef] [PubMed]
- Hebert, M.A.; Paquin, M.-J.; Whitten, L.; Cai, P. Analysis of the suitability of ‘video-visits’ for palliative home care: Implications for practice. J. Telemed. Telecare 2007, 13, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Doolittle, G.C.; Whitten, P.; McCartney, M.; Cook, D.; Nazir, N. An empirical chart analysis of the suitability of telemedicine for hospice visits. Telemed. J. E Health 2005, 11, 90–97. [Google Scholar] [CrossRef] [PubMed]

| Need | Definition | Priority | |
|---|---|---|---|
| PPHC 1 Teams | Families | ||
| Data transmission | Uniform, data protection-compliant transfer of files such as audio data, photos, videos or documents | Very high | Very high |
| Video consultation | Sound and image transmission in real time with at least 3 parties | Very high | High |
| Access to patient records | Families and other health care professionals can view and, if necessary, edit parts of the electronic PPHC patient records | Very high | Medium |
| Symptom questionnaires | Families document clinical progress (e.g., vital signs) or symptom scores, using online questionnaires to share with PPHC teams | High | High |
| Communication support | Picture and text material to overcome language barriers | High | High |
| Shared calendar | Shared online calendar to coordinate appointments between families and PPHC teams | High | Low |
| Information materials | PPHC teams provide families with current, relevant, and validated informational materials | Medium | High |
| Electronic stethoscope | Electronic stethoscope transmits auscultation audio signal in real time from family to PPHC teams | Medium | High |
| Messenger | Sending instant messages | Low 2 | Medium |
| Need | Excerpt |
|---|---|
| Data transmission | Father: “In some cases you can’t explain well because of the language and [it] would be good to use the app to send videos and so on so that the doctors there can see and look at the case themselves.” (Family 15, para. 23 1) |
| Video consultation | Nurse: “And especially when it’s the middle of the night, I would like to have a look first and you have a picture [with video consultation], you’re [then] right there, you can watch along and you don’t have to imagine it.” (FG 3, para. 68 1) |
| Access to patient records | Mother: “Yes, maybe the possibility that you can print out a current medication schedule at short notice or look at it again, that would be great. Maybe also current doctor’s reports, because […] you always have to request it first, phone back and forth and send it back and forth. Something like that would be super practical.” (Family 2, para. 21 1) |
| Symptom questionnaires | Mother: “That’s also quite good, because we were asked to observe and document. (…) So I have everything as a book (…) where I write down, for example, his seizures or abnormalities. So something like that is even better.” (Family 8, para. 41 1) |
| Communication support | Doctor: “There are actually parents or nursing staff with whom you can’t speak a word of German. (…) But if it really were a reliable app and we could translate that one-to-one, that would of course be awesome.” (FG 3, para. 175, P5 1) |
| Shared calendar | Nurse: “Hm, I would wish for: an app that you could use to coordinate the home visit appointments, because we plan a lot about how we should organize the home visits […] and then you make a phone call and find out the physiotherapy appointment is at that time […] and you have to change everything again.” (FG 1, para. 123 1) |
| Information materials | Bereaved mother: “In particular, coping with grief or getting further support, for example, our stay at the rehabilitation center […] which we had to organize ourselves, no one gave us advice. Those would also be helpful points. And also funerals. You don’t know what to do. There could be a small guideline with tick boxes for what to do.” (Family 1, para. 49 1) |
| Electronic stethoscope | Doctor: “Well, I think auscultation is more than the quality of the sound you hear. It’s also everything else you observe: How does he breathe in and out? How does he move? How motivated is he to participate? You would need very good visuals to do that. So I’m not sure if that’s helpful or if I’m actually more likely to initiate a home visit, because auscultation transmission makes me feel more uncertain.” (FG 1, para. 371 1) |
| Messenger | Patient: “We’re not the kind of people who call the doctor about everything and say: Hey, I have this and that, but maybe it would simply be possible to chat with him and say: I’m not doing so well right now […] So if it’s not an emergency, then the doctor can check the message when he has time.” (Family 14, para. 29–31 1) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zimmermann, J.; Heilmann, M.L.; Fisch-Jessen, M.; Hauch, H.; Kruempelmann, S.; Moeller, H.; Nagel, L.; Nathrath, M.; Vaillant, V.; Voelker, T.; et al. Telehealth Needs and Concerns of Stakeholders in Pediatric Palliative Home Care. Children 2023, 10, 1315. https://doi.org/10.3390/children10081315
Zimmermann J, Heilmann ML, Fisch-Jessen M, Hauch H, Kruempelmann S, Moeller H, Nagel L, Nathrath M, Vaillant V, Voelker T, et al. Telehealth Needs and Concerns of Stakeholders in Pediatric Palliative Home Care. Children. 2023; 10(8):1315. https://doi.org/10.3390/children10081315
Chicago/Turabian StyleZimmermann, Jannik, Marie Luise Heilmann, Manuel Fisch-Jessen, Holger Hauch, Sebastian Kruempelmann, Heidi Moeller, Laura Nagel, Michaela Nathrath, Vera Vaillant, Thomas Voelker, and et al. 2023. "Telehealth Needs and Concerns of Stakeholders in Pediatric Palliative Home Care" Children 10, no. 8: 1315. https://doi.org/10.3390/children10081315
APA StyleZimmermann, J., Heilmann, M. L., Fisch-Jessen, M., Hauch, H., Kruempelmann, S., Moeller, H., Nagel, L., Nathrath, M., Vaillant, V., Voelker, T., & Deckers, M. J. (2023). Telehealth Needs and Concerns of Stakeholders in Pediatric Palliative Home Care. Children, 10(8), 1315. https://doi.org/10.3390/children10081315







