Abstract
During the last ten years the use of robotic-assisted rehabilitation has increased significantly. Compared with traditional care, robotic rehabilitation has several potential advantages. Platform-based robotic rehabilitation can help patients recover from musculoskeletal and neurological conditions. Evidence on how platform-based robotic technologies can positively impact on disability recovery is still lacking, and it is unclear which intervention is most effective in individual cases. This systematic review aims to evaluate the effectiveness of platform-based robotic rehabilitation for individuals with musculoskeletal or neurological injuries. Thirty-eight studies met the inclusion criteria and evaluated the efficacy of platform-based rehabilitation robots. Our findings showed that rehabilitation with platform-based robots produced some encouraging results. Among the platform-based robots studied, the VR-based Rutgers Ankle and the Hunova were found to be the most effective robots for the rehabilitation of patients with neurological conditions (stroke, spinal cord injury, Parkinson’s disease) and various musculoskeletal ankle injuries. Our results were drawn mainly from studies with low-level evidence, and we think that our conclusions should be taken with caution to some extent and that further studies are needed to better evaluate the effectiveness of platform-based robotic rehabilitation devices.
1. Introduction
In the last several years, the use of robotic-assisted rehabilitation has increased significantly [1,2]. Compared with traditional care, robotic rehabilitation can be better performed at high intensity and frequency, and can continuously monitor exercise performance so that the level of treatment can be better adapted to the patient’s needs [3], and can generate more appropriate movements and forces during training [4,5].
Two major types of robotic rehabilitation devices are available. The first one consists of wearable devices: robotic orthoses [6] and exoskeletons [7] for correcting the gait pattern of patients and improving ankle performance during walking. The second one includes platform-based devices that are designed solely to improve ankle performance [8,9]. These technologies have a fixed platform and a movable footplate that can be used with a single degree of freedom (DOF) [10] or multiple degrees of freedom (DOFs) [11,12]. Platform-based robotic rehabilitation allows for complex and specialized spatial movements [11,12,13,14]. Their architectures provide the device with high stiffness, balanced force distribution, and improved adaptability to the mechanical properties of human ankle joints [13]. The utilization of platform-based robotic rehabilitation can help the patients recovering from neurological conditions (e.g., stroke, brain injury, spinal cord injury, and cerebral palsy) and musculoskeletal disorders (e.g., post-traumatic lower-limb disorders).
Recently, systematic reviews (SRs) have examined the effectiveness of wearable robotic technologies: exoskeletons and orthoses for upper limbs [15]; exoskeletons for lower limbs in neuromuscular impairments [16]; and individuals with cerebral palsy [17]. However, evidence on how platform-based robotic technologies can positively impact disability recovery is still lacking, and it is unclear which intervention is most effective in individual cases. Therefore, we performed this systematic review with the main aim of first providing a comprehensive evaluation of the evidence-based effectiveness of platform-based rehabilitation robotics for people with musculoskeletal or neurological injuries. Secondly, we aim to show the current state of platform-based rehabilitation robotics technology. Finally, these results should enable physiotherapists to safely use platform-based robots in rehabilitation settings.
2. Materials and Methods
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [18].
2.1. Search Strategy
A literature search was performed in the following electronic databases: PubMed, Excerpta Medical Database (EMBASE), Cochrane Database of Systematic Reviews (CDSR), and Scopus. The medical subject headings (MeSH) used were ”robotics” and ”rehabilitation”, “robotics” and “rehabilitate*” or “treat*” and “effectiveness of robotics.” In addition, we performed a free search on Google Scholar by using keywords (such as ”platform-based robotics” and “robotic rehabilitation effectiveness”) and reviewed key references in relevant publications to make our search as systematic and complete as possible. We also used a snowball search strategy, which means the reference lists of selected and published systematic review articles were manually searched to identify other possible eligible studies. The snowball search was limited to articles published between January 2016 and August 2021. The Movendo technology website was also searched for the clinical trials [19].
2.2. Inclusion and Exclusion Criteria
We included all the studies that examined the clinical outcomes of platform-based robotic rehabilitation training. Both male and female participants (all ages) were included to allow for the generalization of the results. We considered studies with at least one ill subject in the intervention group rehabilitated with a platform-based robot and articles in English and Italian published (as of August 2021) in peer-reviewed journals or as conference papers (national and international), abstracts, or as gray literature. Studies that included only healthy subjects and/or evaluated outcomes with another type of robotic rehabilitation technology were excluded.
2.3. Selection Criteria
Based on the titles, a screening of the articles was performed by two independent reviewers (M.R. and R.R.) to identify relevant studies. One reviewer (M.R.) evaluated all article abstracts for eligibility after the screening of titles was completed. Abstracts that met the inclusion criteria were included in the full review. Otherwise, they were excluded. Studies which one reviewer (M.R.) was unsure whether to include were discussed by two reviewers (M.R., R.R.). Disagreements between the two reviewers were resolved by the inclusion of the third reviewer (A.B.P.) and discussion between these three reviewers. The full texts of the included articles were examined for the typology of platform-based technological rehabilitation robot studied, and the duration of training in the intervention group.
2.4. Assessment of Methodological Quality
The quality of all included studies was evaluated by two independent reviewers (M.R., A.B.P.) by using the Joanna Briggs Institute (JBI) critical appraisal tool [20]. The JBI critical appraisal tool is used to assess the methodological quality of studies. It consists of items (13 items for RCT, 11 for cohort studies, 8 for case studies) that address the internal validity and risk of bias of the studies, particularly confounding, selection, and information bias, as well as the importance of clear reporting. Disagreements between the two reviewers were resolved through the involvement of a third reviewer (K.V.) and discussions among the three reviewers. A high risk of bias was determined when positive responses were ≤49%; moderate risk of bias was assumed when risk of bias was between 50% and 69%; a low risk of bias was determined when positive responses were greater than 70%.
2.5. Data Extraction
A data extraction sheet was developed to collect data of interest. Three reviewers (M.P., K.V., and A.B.P) read all included articles. One author (A.B.P.) extracted the data from the articles, and later they were double-checked by two other authors (K.V., M.P.). The following information was extracted from each study: title, study design, clinical area, patient characteristics (type of disorder, number of subjects, gender, age), intervention group, outcome measures, and study conclusions. A qualitative synthesis was conducted for the included studies.
3. Results
3.1. Study Selection
We found 1085 entries in Medline (PubMed), Scopus, Cochrane Library, and EMBASE, and 20 additional entries came from Google Scholar and the Movendo technology website [21]. After removing 76 duplicate records, 1029 articles were selected for screening. After reading the title and abstract, 964 records were excluded because they were not relevant to our inclusion criteria. We then screened 65 full-text articles for eligibility. After reading the full text, 27 articles were excluded. Therefore, 38 studies were included in our review. The overall selection process is shown in Figure 1. The studies were conducted to develop, validate, and evaluate the effectiveness of platform-based rehabilitation robots. All the studies met the JBI criteria for the critical appraisal (Appendices 1, 2, and 3) [20]. A summary of quality assessments results is also reported in the Supplementary Materials (Tables S1 and S2). In brief, 25 studies had a low risk of bias with a high percentage of positive responses to the JBI tool questions, 10 studies were classified as having a moderate risk of bias, and the remaining three studies were classified as having a high risk of bias.
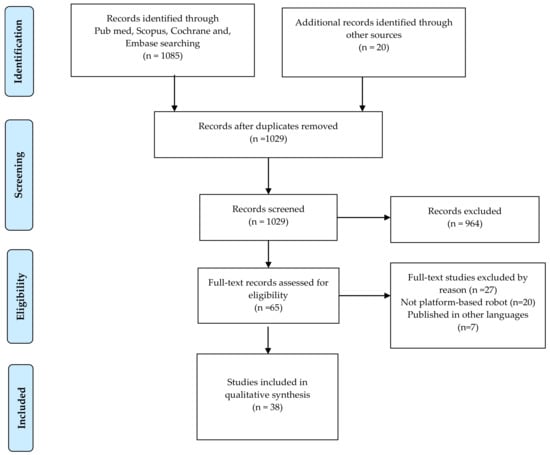
Figure 1.
PRISMA Flow diagram of the records selection process.
3.2. Study Characteristics
Table 1 describes the characteristics of the included studies. The study design included six RCTs with 156 participants, two prospective longitudinal studies, four clinical practice studies, and 26 case studies. Most participants suffered from ankle disabilities, mainly due to musculoskeletal injuries and strokes. In addition, traumatic or nontraumatic brain and spinal cord injuries as well as Parkinson’s disease, knee arthroplasty, and surgical reconstruction of the anterior cruciate ligament (ACL) also played a role in ankle disabilities.

Table 1.
Characteristics of included studies evaluated the effectiveness of Platform-based Robots.
Regarding the outcomes, as they are shown in Table 1, 12 studies investigated ankle-joint performance (e.g., ankle strength, ankle range of motion (ROM), and ankle motor control) [10,22,23,24,25,26,27,28,29,30,31,32]. Nineteen studies examined one or more of the following outcomes: components or parameters of the ankle ROM, trunk parameters (e.g., trunk control, trunk compensations, trunk variability, trunk acceleration, trunk stability), monopodal and bipodal balance, squat, and proprioceptive abilities [33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51]. Two studies examined gait function outcomes [52,53]. Four studies evaluated both ankle performance and gait function to validate the effect of robotic ankle rehabilitation devices [54,55,56,57]. One study [24] also evaluated the device performance by measuring pressure distribution on the footplate. Two studies [26,55] also used participant satisfaction as the main outcome. One study examined neuropsychological assessment with an emphasis on body representation (BR) and cognitive and linguistic functions [58].
3.3. Effectiveness of Platform-Based Rehabilitation Robots
We found the following types of platform-based robotic rehabilitation systems, and their effectiveness is described as follows.
3.3.1. Rutgers Ankle Rehabilitation System
This robotic system has multiple DOF. It operates based on a parallel mechanism (PM) driven by linear actuators, and it is used specifically for ankle rehabilitation in cases of limited mobility [26]. Ten studies have been conducted using the Rutgers Ankle Rehabilitation System (Stewart platform type).
The Virtual Reality System (VR) Rutgers Ankle robot has been investigated in five studies [25,30,52,53,56] and the VR-based telerehabilitation system in one study [29] to rehabilitate individuals after stroke and measure its effects by using various criteria (training focused on gait and climbing speed, ankle and foot mobility, force production, coordination, ability to walk and climb stairs, velocity and distance walked, ankle mechanical strength, and the number of repetitions). The results showed improvements in gait and elevation speed (from 0% to 44% and 3% to 33%, respectively) [53], ankle motion accuracy, exercise duration and training efficiency, ankle mechanical strength, and the number of repetitions [29]. It has been also shown that rehabilitation can help to improve gait and climbing speed [30,53] and ankle muscle strength [25]. However, a robotic virtual reality system produced better results than a robot alone, although the benefits were minor in the gait of post-stroke patients [52].
Two studies investigated the effectiveness of the Rutgers ankle robot in patients with cerebral palsy (CP) [23,57]. Both studies found improvements in ankle strength, motor control, gain function, and patient quality of life [23,57].
Two studies evaluated the effectiveness of the Rutgers ankle haptic interface in patients with musculoskeletal ankle injuries [26,27]. One study showed improvements in range of motion (ROM), ability to generate torque, and mechanical work of the ankle [27]. Another study concluded that the robot can be used for the rehabilitation of patients with hyper-and hypomobile ankles [26].
3.3.2. Ankle Stretching Robotic Rehabilitation System
This type of robotic rehabilitation system usually consists of a single DOF and is usually driven by a rotating motor for a specific application (e.g., ankle stretching). Robotic ankle-stretching devices have been used for rehabilitation in four studies.
Two studies [10,55] investigated an intelligent robotic stretching device in patients with ankle contracture and/or spasticity. Results showed that the treatment was more effective than existing approaches in terms of active and passive ROM, joint stiffness, viscous damping, and reflex excitability [10]. Improvements were noted in muscle strength, walking speed, and subjective sensation [55].
Robotic passive stretching and active training (with biofeedback via motivational games) for ankle rehabilitation has been studied in post-stroke individuals [28] and lower extremity (LE) impairments in children with CP [22]. Results showed improvements in the Modified Ashworth Scale (MAS), the Stroke Rehabilitation Assessment of Movement (STREAM), active dorsiflexion range, dorsiflexor muscle strength, and the Berg Balance Scale (BBS) [28], joint biomechanical properties, motor control performance, and functional capacity in balance and movement [22].
3.3.3. Other Typology of Ankle Robotic Rehabilitation Devices
Homma et al. developed a training robot for ankle dorsiflexion/plantarflexion with a passive mechanical joint. Its effectiveness was evaluated based on pressure distribution on the footplate in a hemiplegic patient. It was unclear in the study whether pressure distribution could be used as an indicator of recovery. Therefore, the study concluded that its relationship to biological data should be further investigated [24].
Cordo et al. tested the efficacy of Assisted Movement with Enhanced Sensation (AMES) by using a robotic ankle device as a treatment for hemiplegia by using strength and joint alignment tests and motor function in post-stroke patients. Results showed improvements in most functional tests within six months [54].
Zhou et al. validated the treatment strategy of proprioceptive neuromuscular facilitation (PNF) with a robotic ankle–foot system in post-stroke patients over six weeks. Results showed improvements in ankle spasticity and/or contracture at the end of the study [32].
3.3.4. ARBOT Rehabilitation Robot
ARBOT is a robotic prototype for ankle rehabilitation. The effectiveness of ARBOT was evaluated on 32 subjects (with ankle and/or hindfoot fractures) comparing conventional and ARBOT-assisted ankle rehabilitation. After a 4-week rehabilitation program, the experimental group showed a significant improvement in the proprioceptive test compared to the control group [31].
3.3.5. Hunova Robotic Rehabilitation System
Hunova is a “platform-based” end-effector robot consisting of two electromechanical platforms with 2 DOF: one is located under the feet and the other under the seat. It is possible to perform exercises both sitting and standing. It allows passive (mobilization), active (with elastic or fluid resistance), proprioceptive, and assistive therapy (i.e., the device intervenes to complete the exercise when the patient needs it). The device can work in both static and dynamic modes. It is used for rehabilitation and evaluation of the sensory-motor function of the lower limbs and torso as well as balance [12]. Twenty studies have been conducted by using the Hunova robot in geriatrics, neurology, and orthopedics. Of these, ten were case studies, four were RCTs, two were prospective longitudinal studies, and four were clinical practice studies.
- Geriatric rehabilitation
Two studies focused on the assessment of balance parameters with Hunova in 96 elderly subjects [33,34]. One study showed that multifactorial fall risk assessment (including clinical and robotic variables) significantly improved the accuracy of fall-risk prediction [34]. Another study showed that balance parameters assessed with this robot were significantly correlated with functional performance in the Short Physical Performance Battery (SPPB) [33].
- ii.
- Neurorehabilitation
Six studies investigated the effectiveness of robotic rehabilitation (training focused on balance and core stability, ankle mobility) in patients with Parkinson’s disease [35,36,37], stroke [39], cavernous malformation and hypertrophic olivary degeneration [44], and severe acquired brain injury [45]. One study focused on the robotic assessment of balance in sitting and standing in patients with Parkinson’s disease [38]. A study investigated multidisciplinary treatment (motor rehabilitation training, traditional physiotherapy and robotic rehabilitation, and psychological counselling) in a patient with somatoparaphrenia (SP) and misoplegia [58]. The results showed improvement in the Timed Up and Go (TUG) test, greater mobility and stability of the pelvis, load management in a seated position [35], dynamic balance, and walking speed [37,44], gait speed and ankle range of motion [45], reactive balance and postural control in an unstable condition, and proprioceptive control in standing and sitting [39]. However, in an RCT (treatment of balance with a robotic platform compared to a conventional rehabilitation), both types of training were found to improve balance, walking, and quality of life [36]. Although differences were noted in postural control, greater trunk sway was noted at the end of the study in association with a greater increase in center of pressure (CoP) backward displacement [38]. Maggio et al. have shown in a case study that an integrated psychological and motor approach can effectively rehabilitate patients with SP, even in the presence of misoplegia [58].
Four studies investigated the effectiveness of robotic assessment and training (focusing on balance, trunk control, dual-motor task with upper limb movements, strengthening, core stability) in individuals with spinal cord injuries (SCI) [40,41,42] and in a patient with retro-ocular frontal aneurysm with hemorrhage [43]. The results showed improvements in trunk control [41,42], dynamic balance and walking speed [43], as well as differences in motor performance at the end of the study [40].
- iii.
- Orthopedic rehabilitation
Three studies investigated Hunova as an aid in rehabilitation, in patients with knee arthroplasty [48], post-traumatic lower limb disorders (to restore motor control and gait performance) [46], and ankle fracture-dislocation [49]. Three studies were performed for evaluation and rehabilitation training in patients after surgical reconstruction of the anterior cruciate ligament (ACL) [47] in a soccer player [50] and in a basketball player with chronic ankle instability [51].
The main results showed improvements in orthostatic stability, postural passages (such as sitting and standing in reactive balance) [48], left ankle performance (in terms of ROM and isometric and isokinetic strength) [49], proprioceptive tests [46], stability index (in dynamic balance tests), joint mobilization, muscle work, and proprioceptive recovery [47]. In two studies, the total performance index improved from 61% to 76% [50] and from 57% to 74%. The two functional areas trained (core and range of motion) [50,51], and the Foot and Ankle Ability Measure (FAAM) score also improved after rehabilitation [51].
4. Discussion
The purpose of our systematic review was to determine the evidence-based effectiveness of platform-based rehabilitation robots for patients with musculoskeletal or neurological disabilities. As a major finding, our study showed that patients with neurological impairments and musculoskeletal injuries can be effectively treated with platform-based robotic rehabilitation devices after their health status is stabilized. With the higher repetitions that robotic devices provide, patients can exercise more, which stimulates neural plasticity in neurological patients in the early stages of their recovery. Once patients can walk better, they can transition to conventional walking to further practice walking on different terrain, improve balance, and correct abnormal gait patterns.
Therefore, we think that platform-based robotic training should be routinely adopted in rehab clinics next to traditional physical therapy. In fact, physiotherapists can use robotic equipment as a multiplier to train more patients. Instead of traditional one-to-one practice, therapists can use robotic devices to treat more patients at the same time. This frees up valuable time for therapists to either train severe patients individually or practice more function-based tasks that require the integration of multiple motor skills. By spending their time on this higher value training activities and letting the robotic devices take over the “heavy” routine tasks, therapists can provide an appropriate level of personalized treatment to their patients and increase their efficiency.
Even though in our study we identified seven types of platform-based robotic rehabilitation systems and reported on their effectiveness [10,12,24,26,31,32,54], we could only draw conclusions for the VR-based Rutgers ankle and Hunova because of the availability of specific literature. In detail, we found that the VR-based Rutgers ankle and Hunova seemed to be the most effective robots for rehabilitation. Ankle rehabilitation using a VR-based Rutgers ankle robot has been shown to be effective in rehabilitating patients after stroke and various musculoskeletal ankle injuries [25,29,30,52,53,56]. We also found that rehabilitation treatment with Hunova is an innovative therapeutic option that can be combined with traditional rehabilitation in patients with Parkinson’s disease [35,36,37], a promising tool for the rehabilitation of stroke patients [39]. For spinal cord injuries (SCI), it can be a useful rehabilitation tool for assessment and training [40,41,42]. In addition, rehabilitation with the Hunova allows measurement of important parameters of static and dynamic stability and can focus on a complex sequence of exercises to restore trunk control and reactive balance after traumatic injury. In the elderly population, the Hunova has the potential to effectively predict fall risk [34]. In patients after traumatic injuries, the Hunova can effectively restore trunk control and reactive balance [40,41,42].
According to our observations and included studies, researchers have studied platform-based robotic rehabilitation in different phases (acute phase, subacute phase, and chronic phase) and at different time points in patients after injuries. Saglia et al. [11], have summarized the rehabilitation protocol for ankle injuries. In the early phase of ankle therapy, the patient can hardly move his foot. Therefore, passive exercises are usually required, during which the movement parameters such as speed, amplitude, and number of repetitions can be determined by the physical therapist. Active exercises can then help the patient regain ROM to move the ankle fully again. Strength training includes both isometric and isotonic exercises. In the final phase of rehabilitation, the patient must perform proprioceptive training (e.g., balance exercises) [11]. Therefore, we believe that an early-stage intervention leads to a faster recovery of the patient than a late-stage intervention. The reason for this is that patients need to do passive exercises in the initial phase. After that, patients need to do active exercises to regain ROM and proprioceptive training (like balance exercises). In contrast, late-stage patients need more exercise sessions to rehabilitate and recover. However, it would be interesting to investigate this in the future through further studies with larger samples.
Bessler et al. reported about 17 adverse events, including tissue-related, musculoskeletal, and physiological adverse events (adverse blood pressure changes) with the use of stationary gait robots (exoskeletons and end-effector) [59,60]. However, for the platform-based robotic devices, we found insufficient literature on adverse events related to long-term use and training. We are not sure and cannot predict what type of adverse events will occur in patients trained with platform-based robots. Future research may provide clues about the adverse effects. This inability to predict adverse events exists because research in the field of robotic rehabilitation is still in its beginning stage.
Robotic rehabilitation was positively evaluated by physiotherapists and occupational therapists. They reported that patients like to use robotic devices for rehabilitation and that they increase accessibility, autonomy, and comfort, and reduce costs [61,62,63,64,65,66]. Therefore, we believe that physiotherapists will have no problems in using the platform-based robotic devices. However, training is required and the amount of training that physiotherapists need depends on how quickly they grasp and understand the functions of the robotic devices. Indeed, the platform-based robots are user-friendly and widely accepted by physiotherapists [12]. Our study has limitations too. Next to fully peer-reviewed articles, we included in our review gray literature, unpublished data, conference papers, and abstracts, and most of the studied literature presented findings with a low level of evidence (mainly from case studies). Therefore, our results were mainly drawn from studies with a low level of evidence, and we think that to some extent, our conclusions should be considered with caution. Most of the included studies presented significant improvements in ankle performance or gait functionality after performing robotic rehabilitation, although they failed in describing how this was achieved. Also, it was difficult to generalize our findings because several platform-based robotic rehabilitation devices have been tested on individuals with different musculoskeletal or neurological injuries, and it was not possible to adopt universal evaluation criteria with effective outcome measures to determine which was the most effective rehabilitation device [67]. Finally, we limited our search strategy to literature in the English and Italian languages; therefore, some studies may have been excluded, leading to a potentially incomplete search. Lastly, we did not analyze the control strategies, safety, and reliability of the investigated platform-based rehabilitation robots, although this was beyond the scope of the study. This could be a further limitation.
5. Conclusions
Our study showed that rehabilitation by using platform-based robots had some encouraging results. The use of robotic rehabilitation allows efficient planning of the rehabilitation process in terms of the duration of sessions, required tools, and availability of a therapist. Therefore, compared to traditional rehabilitation that require combined and intensive efforts of therapists and patients, robotic-assisted rehabilitation should reduce costs because of a shorter hospital stay and greater autonomy at discharge. This highlights the importance of novel rehabilitation techniques that allow therapists to deliver effective treatment interventions while reducing the burden on staff and resources, and related costs. Robotic technology has the potential to transform rehabilitation clinics from labor-intensive to technology-enabled workflows, providing a rich stream of data to help diagnose patients, adjust therapy, and maintain patient records (in a clinic and at home).
Based on our findings, we believe that further studies able to provide results with a higher level of evidence are needed to confirm the effectiveness of platform-based robotic rehabilitation devices. This should primarily include the execution of large sample-size RCTs. These studies should be based on rigorous comparison among the available devices (interventions) and usual care (that is, non-robotic conventional therapies (control)), and should necessarily adopt standardized outcomes to better compare the different models of platform-based rehabilitation robots and to effectively generalize the eventual findings. Therefore, new outcome research is also needed to define universally accepted evaluation criteria able to standardize the devices’ outcomes evaluation. To this end, we also think that wider outcomes should be evaluated, including assessment of comfort, safety, and training performance for the end user.
Despite most studies’ claims that platform-based robots would increase rehabilitation intensity, they allow complex and specialized spatial movements, and the architectures give the robotic device high stiffness, balanced force distribution, and better adaptability to the mechanical properties of human ankles. We believe that this robotic technology can be effectively used by the physiotherapists in the rehabilitation units.
Moreover, in the era of big data and artificial intelligence (AI), computer models can be developed to understand recovery mechanisms, predict the use of different motor control strategies, and ultimately tailor treatment to the patient. We would also like to emphasize that platform-based robotic rehabilitation can only be effective if it would be considered an added value by the patient. Indeed, it is important to consider the perspective of the end user when developing a particular platform-based robotic device to support a specific dysfunction. Such a synergistic effort will certainly lead to effective treatment.
In addition, future research should also focus on the structured and complete recording and dissemination of adverse events related to platform-based robotic rehabilitation to increase knowledge about risks. With this information, appropriate risk mitigation strategies can and should be developed and implemented in platform-based robotic devices to enhance their safety.
Finally, among the platform-based robots studied, the Hunova robot by Movendo technology is commercialized and already available on the market (https://www.movendo.technology/en/) (accessed on 1 August 2021). Therefore, we assume that it has undergone several safety validations before its market launch. In some studies that investigated the Hunova robot, end users also gave positive feedback on training performance and reported that they felt comfortable using the robot for rehabilitation.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/bioengineering9040129/s1, Table S1: Summary of quality assessments using JBI appraisal checklist; Table S2: Summary of quality assessments (Longitudinal Prospective and RCTs) using JBI appraisal checklist.
Author Contributions
Conceptualization, A.B.P., M.R., M.P. and K.V.; methodology, A.B.P., M.R. and M.P.; validation, A.B.P., M.P. and K.V.; formal analysis, A.B.P., R.R., M.R. and M.P.; data curation, A.B.P., M.R. and R.R.; writing—original draft preparation, A.B.P.; writing—review and editing, A.B.P., M.R., R.R., K.V. and M.P.; visualization, A.B.P., K.V. and M.P.; supervision, A.B.P., K.V., M.R. and M.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Loureiro, R.C.V.; Harwin, W.S.; Nagai, K. Advances in upper limb stroke rehabilitation: A technology push. Med. Biol. Eng. Comput. 2011, 49, 1103–1118. [Google Scholar] [CrossRef]
- Péter, O.; Fazekas, G.; Zsiga, K. Robot-mediated upper limb physiotherapy: Review and recommendations for future clinical trials. Int. J. Rehabil. Res. 2011, 34, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Volpe, B.T.; Krebs, H.I.; Hogan, N. Robot-aided sensorimotor training in stroke rehabilitation. Curr. Opin. Neurol. 2001, 14, 745–752. [Google Scholar] [CrossRef]
- Bosecker, C.; Dipietro, L.; Volpe, B. Kinematic Robot-Based Evaluation Scales and Clinical Counterparts to Measure Upper Limb Motor Performance in Patients with Chronic Stroke. Neurorehabil. Neural. Repair. 2010, 24, 62–69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krebs, H.; Hogan, N.; Aisen, M. Robot-Aided Neurorehabilitation. IEEE Trans. Rehabil. Eng. 1998, 6, 75–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, Y.L.; Chen, B.R.; Pérez-Arancibia, N.O. Design and control of a bio-inspired soft wearable robotic device for ankle-foot rehabilitation. Bioinspir. Biomim. 2014, 9, 016007. [Google Scholar] [CrossRef]
- Roy, A.; Krebs, H.; Williams, D. Robot-Aided Neurorehabilitation: A Novel Robot for Ankle Rehabilitation. IEEE Trans. Neural. Syst. Rehabil. Eng. 2009, 25, 569–582. [Google Scholar] [CrossRef]
- Mohammed, S.; Amirat, Y.; Rifai, H. Lower-limb movement assistance through wearable robots: State of the art and challenges. Adv. Robot. 2012, 26, 1–22. [Google Scholar] [CrossRef]
- Senanayake, C.; Senanayake, S.M.N.A. Emerging robotics devices for therapeutic rehabilitation of the lower extremity. In Proceedings of the 2009 IEEE/ASME International Conference on Advanced Intelligent Mechatronics, Singapore, 14–17 July 2009; pp. 1142–1147. [Google Scholar] [CrossRef]
- Zhang, L.Q.; Chung, G.; Bai, Z. Intelligent stretching of ankle joints with contracture/spasticity. IEEE Trans. Neural. Syst. Rehabil. Eng. 2002, 10, 149–157. [Google Scholar] [CrossRef]
- Saglia, J.A.; Tsagarakis, N.G.; Dai, J.S. Control strategies for patient-assisted training using the ankle rehabilitation robot (ARBOT). IEEE/ASME Trans Mechatron. 2013, 18, 1799–1808. [Google Scholar] [CrossRef]
- Saglia, J.A.; De Luca, A.; Squeri, V. Design and development of a novel core, balance and lower limb rehabilitation robot: Hunova. In Proceedings of the 2019 IEEE 16th International Conference on Rehabilitation Robotics (ICORR), Toronto, ON, Canada, 24–28 June 2019; pp. 417–422. [Google Scholar] [CrossRef]
- Alvarez-Perez, M.G.; Garcia-Murillo, M.A.; Cervantes-Sánchez, J.J. Robot-assisted ankle rehabilitation: A review. Disabil. Rehabil. Assist. Technol. 2019, 15, 394–408. [Google Scholar] [CrossRef] [PubMed]
- Miao, Q.; Zhang, M.; Wang, C. Towards optimal platform-based robot design for ankle rehabilitation: The state of the art and future prospects. J. Healthc. Eng. 2018, 2018, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Gandolla, M.; Antonietti, A.; Longatelli, V. The Effectiveness of Wearable Upper Limb Assistive Devices in Degenerative Neuromuscular Diseases: A Systematic Review and Meta-Analysis. Front. Bioeng. Biotechnol. 2020, 7, 450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernández, A.R.; Prat, J.L.; Llagunes, J.M.F. Systematic review on wearable lower-limb exoskeletons for gait training in neuromuscular impairments. J. Neuroeng. Rehabil. 2021, 18, 22. [Google Scholar] [CrossRef] [PubMed]
- Bunge, L.R.; Davidson, A.J.; Helmore, B.R. Effectiveness of powered exoskeleton use on gait in individuals with cerebral palsy: A systematic review. PLoS ONE 2021, 16, e0252193. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, 332–336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Movendo Technology. Available online: https://www.movendo.technology/en/ (accessed on 1 August 2021).
- JBI’s Critical Appraisal Tools. Available online: https://jbi.global/critical-appraisal-tools (accessed on 5 December 2021).
- Clinical Studies: Movendo Technology. Available online: https://www.movendo.technology/en/clinical-studies/ (accessed on 1 August 2021).
- Wu, Y.N.; Hwang, M.; Ren, Y. Combined passive stretching and active movement rehabilitation of lower-limb impairments in children with cerebral palsy using a portable robot. Neurorehabil. Neural. Repair. 2011, 25, 378–385. [Google Scholar] [CrossRef]
- Cioi, D.; Kale, A.; Burdea, G. Ankle control and strength training for children with cerebral palsy using the Rutgers Ankle CP. In Proceedings of the 2011 IEEE International Conference on Rehabilitation Robotics, Zurich, Switzerland, 9 June–1 July 2011; pp. 654–659. [Google Scholar] [CrossRef]
- Homma, K.; Usuba, M. Development of ankle dorsiflexion/plantarflexion exercise device with passive mechanical joint. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 13–15 June 2007; pp. 292–297. [Google Scholar] [CrossRef]
- Boian, R.F.; Deutsch, J.E.; Lee, C.S. Haptic effects for virtual reality-based post-stroke rehabilitation. In Proceedings of the 11th Symposium on Haptic Interfaces for Virtual Environment and Teleoperator Systems, HAPTICS 2003, Los Angeles, CA, USA, 22–23 March 2003; pp. 247–253. [Google Scholar] [CrossRef]
- Girone, M.; Burdea, G.; Bouzit, M. Orthopedic rehabilitation using the ‘rutgers ankle’ interface. Stud. Health Technol. Inform. 2000, 70, 89–95. [Google Scholar] [CrossRef]
- Deutsch, J.; Latonio, J.; Burdea, G. Rehabilitation of musculoskeletal injuries using the Rutgers ankle haptic interface: Three case reports. In Proceedings of the Eurohaptics Conference, Birmingham, UK, 1–4 July 2001; The University of Birmingham: Birmingham, UK, 2001; pp. 11–16. Available online: https://apps.dtic.mil/sti/pdfs/ADA393363.pdf (accessed on 1 February 2022).
- Waldman, G.; Yang, C.Y.; Ren, Y. Effects of robot-guided passive stretching and active movement training of ankle and mobility impairments in stroke. NeuroRehabilitation 2013, 32, 625–634. [Google Scholar] [CrossRef]
- Deutsch, J.E.; Lewis, J.A.; Burdea, G. Technical and patient performance using a virtual reality-integrated Telerehabilitation system: Preliminary finding. IEEE Trans. Neural. Syst. Rehabil. Eng. 2007, 15, 30–35. [Google Scholar] [CrossRef]
- Boian, R.; Lee, C.; Deutsch, J. Virtual reality-based system for ankle rehabilitation post stroke. In Proceedings of the 1st International Workshop on Virtual Reality Rehabil (Mental Health, Neurological, Physical, Vocational) VRMHR 2002, Lausanne, Switzerland; pp. 77–86. Available online: http://www.ti.rutgers.edu/publications/papers/2002_vrmhr_boian.pdf (accessed on 1 February 2022).
- Taglione, E.; De Marco, E.; Pasqualetti, F. Ankle Rehabilitation Using the High-Performance Robotic Device ARBOT: Results from a Randomised Controlled Trial. 2015. Available online: https://www.movendo.technology/clinical-studies/ (accessed on 1 February 2022).
- Zhou, Z.; Zhou, Y.; Wang, N. A proprioceptive neuromuscular facilitation integrated robotic ankle-foot system for post stroke rehabilitation. Rob. Auton. Syst. 2015, 73, 111–122. [Google Scholar] [CrossRef]
- Cella, A.; De Luca, A.; Squeri, V. Robotic balance assessment in community-dwelling older people with different grades of impairment of physical performance. Aging Clin. Exp. Res. 2020, 32, 491–503. [Google Scholar] [CrossRef] [PubMed]
- Cella, A.; De Luca, A.; Squeri, V. Development and validation of a robotic multifactorial fall-risk predictive model: A one-year prospective study in community-dwelling older adults. PLoS ONE 2020, 15, e0234904. [Google Scholar] [CrossRef] [PubMed]
- Vallone, F.; Cella, A.; De Luca, A. Effect of a Robotic Training Focused on Balance and Core Stability in Parkinson’s Disease: A Pilot Study. 2019. Available online: https://www.movendo.technology/wp-content/uploads/2021/04/Movendo-Clinical-Studies_DEF_web.pdf (accessed on 1 February 2022).
- Spina, S.; Facciorusso, S.; Cinone, N. Effectiveness of robotic balance training on postural instability in patients with mild parkinson’s disease: A pilot, single-blind, randomized controlled trial. J. Rehabil. Med. 2021, 53, 2753. [Google Scholar] [CrossRef]
- Pendolino, L.; Veneziano, G.; Salvato, E. Treatment of Advanced Stage Parkinson Disease with Hunova: A Case Study. 2019. Available online: https://www.movendo.technology/en/case-studies/treatment-of-advanced-stage-parkinson-disease-with-hunova/ (accessed on 1 February 2022).
- Marchesi, G.; Casadio, M.; Ballardini, G. Robot-based assessment of sitting and standing balance: Preliminary results in Parkinson’s disease. In Proceedings of the 2019 IEEE 16th International Conference on Rehabilitation Robotics (ICORR), Toronto, ON, Canada, 24–28 June 2019; pp. 570–576. [Google Scholar] [CrossRef]
- De Luca, A.; Squeri, V.; Barone, L.M. Dynamic Stability and Trunk Control Improvements Following Robotic Balance and Core Stability Training in Chronic Stroke Survivors: A Pilot Study. Front. Neurol. 2020, 11, 494. [Google Scholar] [CrossRef]
- Marchesi, G.; Ricaldone, E.; De Luca, A. A robot-based assessment of trunk control in Spinal Cord Injured athletes. In Proceedings of the 2020 8th IEEE RAS/EMBS International Conference for Biomedical Robotics and Biomechatronics (BioRob), New York, NY, USA, 29 November–1 December 2020; pp. 497–502. [Google Scholar] [CrossRef]
- Leo, A.; Bertazzoni, L.; Zarbo, M. The Role of Hunova in Rehabilitative Treatment of Functional Balance in a Patient with Complete Spinal Cord Injury (SCI). 2019. Available online: https://www.movendo.technology/en/case-studies/the-role-of-hunova-in-rehabilitative-treatment-of-functional-balance-in-a-patient-with-complete-spinal-cord-injury-sci-2/ (accessed on 1 February 2022).
- Leo, A.; Zarbo, M.; Cassinis, A. The Use of the Robotic Device Hunova as Rehabilitation and Evaluation Tool for Functional Balance in Individuals with Spinal Cord Injury. 12th ISPRM World Congress–ISPRM 2018 (08–12 July 2018, Paris). 2018. Available online: https://www.movendo.technology/wp-content/uploads/2021/04/Movendo-Clinical-Studies_DEF_web.pdf (accessed on 1 February 2022).
- Escelsior, M.; Fochi, A.; Zolezzi, D. Balance Assessment and Training in an Elderly Neurological Patient: A Case Study. 2020. Available online: https://www.movendo.technology/casestudies/balance-assessment-and-training-in-an-elderly-neurological-patient-a-case-study/ (accessed on 1 February 2022).
- Nguyen, U.; Truman, J. The Role of Hunova in the Treatment of Patient with a Cavernous Malformation and Hypertrophic Olivary Degeneration. 2021. Available online: https://www.movendo.technology/en/case-studies/cavernous-malformation-and-hypertrophic-olivary-degeneration/ (accessed on 1 February 2022).
- Burlando, M.; Bollo, B. Use of Hunova for Rehabilitation Following Severe Acquired Brain Injury (ABI): A Case Study. 2019. Available online: https://www.movendo.technology/en/case-studies/use-of-hunova-for-rehabilitation-following-severe-acquired-brain-injury-abi-a-case-study-2/ (accessed on 1 February 2022).
- Taglione, E.; Graziano, A.; D’Angelo, M. Proprioceptive and Motor Training Using the High-Performance Robotic Device Hunova: Preliminary Results of a Randomized, Controlled Trial in Patients with Lower Limb Post-Traumatic Conditions. 2018. Available online: https://www.movendo.technology/wp-content/uploads/2021/04/Movendo-Clinical-Studies_DEF_web.pdf (accessed on 1 February 2022).
- Vallone, F.; Damiani, G.; D’Angelo, M.L.; De Luca, A.; Squeri, V.; De Michieli, L.; Saglia, J.A.; Sanfilippo, C.; Corrieri, N.; Giorgini, C. Evaluation and Rehabilitation Training with Hunova Robotic System for the Recovery of Dynamic Postural Stability: Open Randomized Interventional Protocol, on Patients after ACL Surgical Reconstruction. 2018. Available online: http://www.congressonazionalesimfer.it/wp-content/uploads/2019/01/SIMFER-2018-Abstract-Book-Versione-2.pdf (accessed on 1 February 2022).
- Di Matteo, A.; Bonazzi, F.; Maschi, E. Hunova as a Tool in Rehabilitation Following Robotic Knee Arthroplasty. 2019. Available online: https://www.movendo.technology/casestudies/hunova-as-a-tool-in-rehabilitation-following-robotic-knee-arthroplasty/ (accessed on 1 February 2022).
- Pieve, V.D.; Tanco, E.; Rossi, F. Rehabilitative Treatment of Fracture-Dislocation of the Ankle with Hunova: A Case Study. 2019. Available online: https://www.movendo.technology/en/case-studies/rehabilitative-treatment-of-fracture-dislocation-of-the-ankle-with-hunova-2/ (accessed on 1 February 2022).
- Barbero, P.; Zolezzi, D. Hunova for Performance Optimization of the Soccer Player: A Case Study. 2020. Available online: https://www.movendo.technology/en/case-studies/hunova-for-performance-optimization-of-the-football-player-a-case-study-3/ (accessed on 1 February 2022).
- Risicato, G.; Puntoni, C.; Agli, S.D. Hunova for Evaluation and Treatment of Chronic Ankle Instability Using Performance Index. 2020. Available online: https://www.movendo.technology/casestudies/hunova-for-evaluation-and-treatment-of-chronic-ankle-instability-using-performance-index/ (accessed on 1 February 2022).
- Mirelman, A.; Bonato, P.; Deutsch, J.E. Effects of training with a robot-virtual reality system compared with a robot alone on the gait of individuals after stroke. Stroke 2008, 40, 169–174. [Google Scholar] [CrossRef]
- Deutsch, J.E.; Paserchia, C.; Vecchione, C. Improved gait and elevation speed of individuals post-stroke after lower extremity training in virtual environments. Neurol. Phys. Ther. 2004, 28, 185–186. [Google Scholar] [CrossRef]
- Cordo, P.; Lutsep, H.; Cordo, L. (AMES): Coupling Motor and Sensory to Remediate. Neurorehabil. Neural. Repair. 2009, 23, 67–77. [Google Scholar] [CrossRef] [Green Version]
- Selles, R.W.; Li, X.; Lin, F. Feedback-controlled and programmed stretching of the ankle plantarflexors and dorsiflexors in stroke: Effects of a 4-week intervention program. Arch. Phys. Med. Rehabil. 2005, 86, 2330–2336. [Google Scholar] [CrossRef]
- Deutsch, J.E.; Latonio, J.; Burdea, G.C. Post-stroke rehabilitation with the Rutgers Ankle system: A case study. Presence Teleoperators Virtual Environ. 2001, 10, 416–430. [Google Scholar] [CrossRef]
- Burdea, G.C.; Cioi, D.; Kale, A. Robotics and gaming to improve ankle strength, motor control, and function in children with cerebral palsy—A case study series. IEEE Trans. Neural. Syst. Rehabil. Eng. 2013, 21, 165–173. [Google Scholar] [CrossRef] [Green Version]
- Maggio, M.G.; Naro, A.; Calatozzo, P. Rehabilitation of somatoparaphrenia with misoplegia: Insights from a single case-pilot study. J. Integr. Neurosci. 2021, 20, 439–447. [Google Scholar] [CrossRef]
- Bessler, J.; Prange-Lasonder, G.B.; Schulte, R.V.; Schaake, L.; Prinsen, E.C.; Buurke, J.H. Occurrence and Type of Adverse Events during the Use of Stationary Gait Robots-A Systematic Literature Review. Front. Robot. AI 2020, 7, 557606. [Google Scholar] [CrossRef] [PubMed]
- Bessler, J.; Prange-Lasonder, G.B.; Schaake, L.; Saenz, J.F.; Bidard, C.; Fassi, I.; Valori, M.; Lassen, A.B.; Buurke, J.H. Safety Assessment of Rehabilitation Robots: A Review Identifying Safety Skills and Current Knowledge Gaps. Front. Robot. AI 2021, 8, 602878. [Google Scholar] [CrossRef] [PubMed]
- Krebs, H.I.; Palazzolo, J.J.; Dipietro, L.; Ferraro, M.; Krol, J.; Rannekleiv, K.; Volpe, B.T.; Hogan, N. Rehabilitation robotics: Performance-based progressive robot-assisted therapy. Auton. Robot. 2003, 15, 7–20. [Google Scholar] [CrossRef]
- Stefano, M.; Patrizia, P.; Mario, A. Robotic upper limb rehabilitation after acute stroke by NeReBot: Evaluation of treatment costs. BioMed Res. Int. 2014, 2014, 265634. [Google Scholar] [CrossRef] [PubMed]
- Hesse, S.; Heß, A.; Werner, C.C. Effect on arm function and cost of robot-assisted group therapy in subacute patients with stroke and a moderately to severely affected arm: A randomized controlled trial. Clin. Rehabil. 2014, 28, 637–647. [Google Scholar] [CrossRef]
- Wagner, T.H.; Lo, A.C.; Peduzzi, P. An Economic Analysis of Robot-Assisted Therapy for Long-Term Upper-Limb Impairment After Stroke. N. Engl. J. Med. 2011, 42, 2630–2632. [Google Scholar] [CrossRef] [Green Version]
- Stephenson, A.; Stephens, J. An exploration of physiotherapists’ experiences of robotic therapy in upper limb rehabilitation within a stroke rehabilitation centre. Disabil. Rehabil. Assist. Technol. 2018, 13, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Tyson, S.; Weightman, A. Professionals’ Views and Experiences of Using Rehabilitation Robotics with Stroke Survivors: A Mixed Methods Survey. Front. Med. Technol. 2021, 3, 780090. [Google Scholar] [CrossRef]
- Zhang, M.; Davies, T.C.; Xie, S. Effectiveness of robot-assisted therapy on ankle rehabilitation—A systematic review. J. Neuroeng. Rehabil. 2013, 10, 30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).