Effectiveness of Platform-Based Robot-Assisted Rehabilitation for Musculoskeletal or Neurologic Injuries: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Selection Criteria
2.4. Assessment of Methodological Quality
2.5. Data Extraction
3. Results
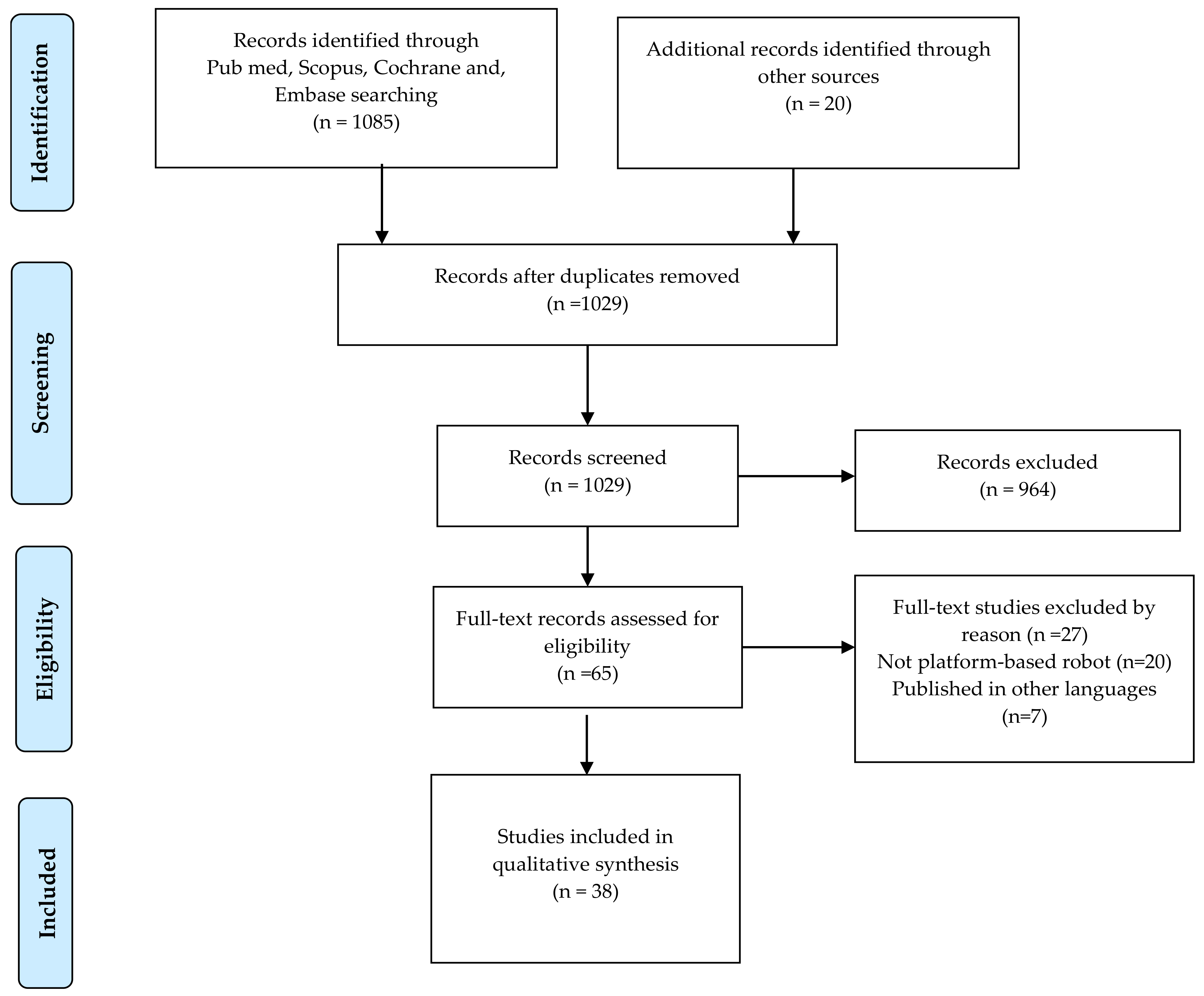
3.1. Study Selection
3.2. Study Characteristics
3.3. Effectiveness of Platform-Based Rehabilitation Robots
3.3.1. Rutgers Ankle Rehabilitation System
3.3.2. Ankle Stretching Robotic Rehabilitation System
3.3.3. Other Typology of Ankle Robotic Rehabilitation Devices
3.3.4. ARBOT Rehabilitation Robot
3.3.5. Hunova Robotic Rehabilitation System
- Geriatric rehabilitation
- ii.
- Neurorehabilitation
- iii.
- Orthopedic rehabilitation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Loureiro, R.C.V.; Harwin, W.S.; Nagai, K. Advances in upper limb stroke rehabilitation: A technology push. Med. Biol. Eng. Comput. 2011, 49, 1103–1118. [Google Scholar] [CrossRef]
- Péter, O.; Fazekas, G.; Zsiga, K. Robot-mediated upper limb physiotherapy: Review and recommendations for future clinical trials. Int. J. Rehabil. Res. 2011, 34, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Volpe, B.T.; Krebs, H.I.; Hogan, N. Robot-aided sensorimotor training in stroke rehabilitation. Curr. Opin. Neurol. 2001, 14, 745–752. [Google Scholar] [CrossRef]
- Bosecker, C.; Dipietro, L.; Volpe, B. Kinematic Robot-Based Evaluation Scales and Clinical Counterparts to Measure Upper Limb Motor Performance in Patients with Chronic Stroke. Neurorehabil. Neural. Repair. 2010, 24, 62–69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krebs, H.; Hogan, N.; Aisen, M. Robot-Aided Neurorehabilitation. IEEE Trans. Rehabil. Eng. 1998, 6, 75–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, Y.L.; Chen, B.R.; Pérez-Arancibia, N.O. Design and control of a bio-inspired soft wearable robotic device for ankle-foot rehabilitation. Bioinspir. Biomim. 2014, 9, 016007. [Google Scholar] [CrossRef]
- Roy, A.; Krebs, H.; Williams, D. Robot-Aided Neurorehabilitation: A Novel Robot for Ankle Rehabilitation. IEEE Trans. Neural. Syst. Rehabil. Eng. 2009, 25, 569–582. [Google Scholar] [CrossRef]
- Mohammed, S.; Amirat, Y.; Rifai, H. Lower-limb movement assistance through wearable robots: State of the art and challenges. Adv. Robot. 2012, 26, 1–22. [Google Scholar] [CrossRef]
- Senanayake, C.; Senanayake, S.M.N.A. Emerging robotics devices for therapeutic rehabilitation of the lower extremity. In Proceedings of the 2009 IEEE/ASME International Conference on Advanced Intelligent Mechatronics, Singapore, 14–17 July 2009; pp. 1142–1147. [Google Scholar] [CrossRef]
- Zhang, L.Q.; Chung, G.; Bai, Z. Intelligent stretching of ankle joints with contracture/spasticity. IEEE Trans. Neural. Syst. Rehabil. Eng. 2002, 10, 149–157. [Google Scholar] [CrossRef]
- Saglia, J.A.; Tsagarakis, N.G.; Dai, J.S. Control strategies for patient-assisted training using the ankle rehabilitation robot (ARBOT). IEEE/ASME Trans Mechatron. 2013, 18, 1799–1808. [Google Scholar] [CrossRef]
- Saglia, J.A.; De Luca, A.; Squeri, V. Design and development of a novel core, balance and lower limb rehabilitation robot: Hunova. In Proceedings of the 2019 IEEE 16th International Conference on Rehabilitation Robotics (ICORR), Toronto, ON, Canada, 24–28 June 2019; pp. 417–422. [Google Scholar] [CrossRef]
- Alvarez-Perez, M.G.; Garcia-Murillo, M.A.; Cervantes-Sánchez, J.J. Robot-assisted ankle rehabilitation: A review. Disabil. Rehabil. Assist. Technol. 2019, 15, 394–408. [Google Scholar] [CrossRef] [PubMed]
- Miao, Q.; Zhang, M.; Wang, C. Towards optimal platform-based robot design for ankle rehabilitation: The state of the art and future prospects. J. Healthc. Eng. 2018, 2018, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Gandolla, M.; Antonietti, A.; Longatelli, V. The Effectiveness of Wearable Upper Limb Assistive Devices in Degenerative Neuromuscular Diseases: A Systematic Review and Meta-Analysis. Front. Bioeng. Biotechnol. 2020, 7, 450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernández, A.R.; Prat, J.L.; Llagunes, J.M.F. Systematic review on wearable lower-limb exoskeletons for gait training in neuromuscular impairments. J. Neuroeng. Rehabil. 2021, 18, 22. [Google Scholar] [CrossRef] [PubMed]
- Bunge, L.R.; Davidson, A.J.; Helmore, B.R. Effectiveness of powered exoskeleton use on gait in individuals with cerebral palsy: A systematic review. PLoS ONE 2021, 16, e0252193. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, 332–336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Movendo Technology. Available online: https://www.movendo.technology/en/ (accessed on 1 August 2021).
- JBI’s Critical Appraisal Tools. Available online: https://jbi.global/critical-appraisal-tools (accessed on 5 December 2021).
- Clinical Studies: Movendo Technology. Available online: https://www.movendo.technology/en/clinical-studies/ (accessed on 1 August 2021).
- Wu, Y.N.; Hwang, M.; Ren, Y. Combined passive stretching and active movement rehabilitation of lower-limb impairments in children with cerebral palsy using a portable robot. Neurorehabil. Neural. Repair. 2011, 25, 378–385. [Google Scholar] [CrossRef]
- Cioi, D.; Kale, A.; Burdea, G. Ankle control and strength training for children with cerebral palsy using the Rutgers Ankle CP. In Proceedings of the 2011 IEEE International Conference on Rehabilitation Robotics, Zurich, Switzerland, 9 June–1 July 2011; pp. 654–659. [Google Scholar] [CrossRef]
- Homma, K.; Usuba, M. Development of ankle dorsiflexion/plantarflexion exercise device with passive mechanical joint. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 13–15 June 2007; pp. 292–297. [Google Scholar] [CrossRef]
- Boian, R.F.; Deutsch, J.E.; Lee, C.S. Haptic effects for virtual reality-based post-stroke rehabilitation. In Proceedings of the 11th Symposium on Haptic Interfaces for Virtual Environment and Teleoperator Systems, HAPTICS 2003, Los Angeles, CA, USA, 22–23 March 2003; pp. 247–253. [Google Scholar] [CrossRef]
- Girone, M.; Burdea, G.; Bouzit, M. Orthopedic rehabilitation using the ‘rutgers ankle’ interface. Stud. Health Technol. Inform. 2000, 70, 89–95. [Google Scholar] [CrossRef]
- Deutsch, J.; Latonio, J.; Burdea, G. Rehabilitation of musculoskeletal injuries using the Rutgers ankle haptic interface: Three case reports. In Proceedings of the Eurohaptics Conference, Birmingham, UK, 1–4 July 2001; The University of Birmingham: Birmingham, UK, 2001; pp. 11–16. Available online: https://apps.dtic.mil/sti/pdfs/ADA393363.pdf (accessed on 1 February 2022).
- Waldman, G.; Yang, C.Y.; Ren, Y. Effects of robot-guided passive stretching and active movement training of ankle and mobility impairments in stroke. NeuroRehabilitation 2013, 32, 625–634. [Google Scholar] [CrossRef]
- Deutsch, J.E.; Lewis, J.A.; Burdea, G. Technical and patient performance using a virtual reality-integrated Telerehabilitation system: Preliminary finding. IEEE Trans. Neural. Syst. Rehabil. Eng. 2007, 15, 30–35. [Google Scholar] [CrossRef]
- Boian, R.; Lee, C.; Deutsch, J. Virtual reality-based system for ankle rehabilitation post stroke. In Proceedings of the 1st International Workshop on Virtual Reality Rehabil (Mental Health, Neurological, Physical, Vocational) VRMHR 2002, Lausanne, Switzerland; pp. 77–86. Available online: http://www.ti.rutgers.edu/publications/papers/2002_vrmhr_boian.pdf (accessed on 1 February 2022).
- Taglione, E.; De Marco, E.; Pasqualetti, F. Ankle Rehabilitation Using the High-Performance Robotic Device ARBOT: Results from a Randomised Controlled Trial. 2015. Available online: https://www.movendo.technology/clinical-studies/ (accessed on 1 February 2022).
- Zhou, Z.; Zhou, Y.; Wang, N. A proprioceptive neuromuscular facilitation integrated robotic ankle-foot system for post stroke rehabilitation. Rob. Auton. Syst. 2015, 73, 111–122. [Google Scholar] [CrossRef]
- Cella, A.; De Luca, A.; Squeri, V. Robotic balance assessment in community-dwelling older people with different grades of impairment of physical performance. Aging Clin. Exp. Res. 2020, 32, 491–503. [Google Scholar] [CrossRef] [PubMed]
- Cella, A.; De Luca, A.; Squeri, V. Development and validation of a robotic multifactorial fall-risk predictive model: A one-year prospective study in community-dwelling older adults. PLoS ONE 2020, 15, e0234904. [Google Scholar] [CrossRef] [PubMed]
- Vallone, F.; Cella, A.; De Luca, A. Effect of a Robotic Training Focused on Balance and Core Stability in Parkinson’s Disease: A Pilot Study. 2019. Available online: https://www.movendo.technology/wp-content/uploads/2021/04/Movendo-Clinical-Studies_DEF_web.pdf (accessed on 1 February 2022).
- Spina, S.; Facciorusso, S.; Cinone, N. Effectiveness of robotic balance training on postural instability in patients with mild parkinson’s disease: A pilot, single-blind, randomized controlled trial. J. Rehabil. Med. 2021, 53, 2753. [Google Scholar] [CrossRef]
- Pendolino, L.; Veneziano, G.; Salvato, E. Treatment of Advanced Stage Parkinson Disease with Hunova: A Case Study. 2019. Available online: https://www.movendo.technology/en/case-studies/treatment-of-advanced-stage-parkinson-disease-with-hunova/ (accessed on 1 February 2022).
- Marchesi, G.; Casadio, M.; Ballardini, G. Robot-based assessment of sitting and standing balance: Preliminary results in Parkinson’s disease. In Proceedings of the 2019 IEEE 16th International Conference on Rehabilitation Robotics (ICORR), Toronto, ON, Canada, 24–28 June 2019; pp. 570–576. [Google Scholar] [CrossRef]
- De Luca, A.; Squeri, V.; Barone, L.M. Dynamic Stability and Trunk Control Improvements Following Robotic Balance and Core Stability Training in Chronic Stroke Survivors: A Pilot Study. Front. Neurol. 2020, 11, 494. [Google Scholar] [CrossRef]
- Marchesi, G.; Ricaldone, E.; De Luca, A. A robot-based assessment of trunk control in Spinal Cord Injured athletes. In Proceedings of the 2020 8th IEEE RAS/EMBS International Conference for Biomedical Robotics and Biomechatronics (BioRob), New York, NY, USA, 29 November–1 December 2020; pp. 497–502. [Google Scholar] [CrossRef]
- Leo, A.; Bertazzoni, L.; Zarbo, M. The Role of Hunova in Rehabilitative Treatment of Functional Balance in a Patient with Complete Spinal Cord Injury (SCI). 2019. Available online: https://www.movendo.technology/en/case-studies/the-role-of-hunova-in-rehabilitative-treatment-of-functional-balance-in-a-patient-with-complete-spinal-cord-injury-sci-2/ (accessed on 1 February 2022).
- Leo, A.; Zarbo, M.; Cassinis, A. The Use of the Robotic Device Hunova as Rehabilitation and Evaluation Tool for Functional Balance in Individuals with Spinal Cord Injury. 12th ISPRM World Congress–ISPRM 2018 (08–12 July 2018, Paris). 2018. Available online: https://www.movendo.technology/wp-content/uploads/2021/04/Movendo-Clinical-Studies_DEF_web.pdf (accessed on 1 February 2022).
- Escelsior, M.; Fochi, A.; Zolezzi, D. Balance Assessment and Training in an Elderly Neurological Patient: A Case Study. 2020. Available online: https://www.movendo.technology/casestudies/balance-assessment-and-training-in-an-elderly-neurological-patient-a-case-study/ (accessed on 1 February 2022).
- Nguyen, U.; Truman, J. The Role of Hunova in the Treatment of Patient with a Cavernous Malformation and Hypertrophic Olivary Degeneration. 2021. Available online: https://www.movendo.technology/en/case-studies/cavernous-malformation-and-hypertrophic-olivary-degeneration/ (accessed on 1 February 2022).
- Burlando, M.; Bollo, B. Use of Hunova for Rehabilitation Following Severe Acquired Brain Injury (ABI): A Case Study. 2019. Available online: https://www.movendo.technology/en/case-studies/use-of-hunova-for-rehabilitation-following-severe-acquired-brain-injury-abi-a-case-study-2/ (accessed on 1 February 2022).
- Taglione, E.; Graziano, A.; D’Angelo, M. Proprioceptive and Motor Training Using the High-Performance Robotic Device Hunova: Preliminary Results of a Randomized, Controlled Trial in Patients with Lower Limb Post-Traumatic Conditions. 2018. Available online: https://www.movendo.technology/wp-content/uploads/2021/04/Movendo-Clinical-Studies_DEF_web.pdf (accessed on 1 February 2022).
- Vallone, F.; Damiani, G.; D’Angelo, M.L.; De Luca, A.; Squeri, V.; De Michieli, L.; Saglia, J.A.; Sanfilippo, C.; Corrieri, N.; Giorgini, C. Evaluation and Rehabilitation Training with Hunova Robotic System for the Recovery of Dynamic Postural Stability: Open Randomized Interventional Protocol, on Patients after ACL Surgical Reconstruction. 2018. Available online: http://www.congressonazionalesimfer.it/wp-content/uploads/2019/01/SIMFER-2018-Abstract-Book-Versione-2.pdf (accessed on 1 February 2022).
- Di Matteo, A.; Bonazzi, F.; Maschi, E. Hunova as a Tool in Rehabilitation Following Robotic Knee Arthroplasty. 2019. Available online: https://www.movendo.technology/casestudies/hunova-as-a-tool-in-rehabilitation-following-robotic-knee-arthroplasty/ (accessed on 1 February 2022).
- Pieve, V.D.; Tanco, E.; Rossi, F. Rehabilitative Treatment of Fracture-Dislocation of the Ankle with Hunova: A Case Study. 2019. Available online: https://www.movendo.technology/en/case-studies/rehabilitative-treatment-of-fracture-dislocation-of-the-ankle-with-hunova-2/ (accessed on 1 February 2022).
- Barbero, P.; Zolezzi, D. Hunova for Performance Optimization of the Soccer Player: A Case Study. 2020. Available online: https://www.movendo.technology/en/case-studies/hunova-for-performance-optimization-of-the-football-player-a-case-study-3/ (accessed on 1 February 2022).
- Risicato, G.; Puntoni, C.; Agli, S.D. Hunova for Evaluation and Treatment of Chronic Ankle Instability Using Performance Index. 2020. Available online: https://www.movendo.technology/casestudies/hunova-for-evaluation-and-treatment-of-chronic-ankle-instability-using-performance-index/ (accessed on 1 February 2022).
- Mirelman, A.; Bonato, P.; Deutsch, J.E. Effects of training with a robot-virtual reality system compared with a robot alone on the gait of individuals after stroke. Stroke 2008, 40, 169–174. [Google Scholar] [CrossRef]
- Deutsch, J.E.; Paserchia, C.; Vecchione, C. Improved gait and elevation speed of individuals post-stroke after lower extremity training in virtual environments. Neurol. Phys. Ther. 2004, 28, 185–186. [Google Scholar] [CrossRef]
- Cordo, P.; Lutsep, H.; Cordo, L. (AMES): Coupling Motor and Sensory to Remediate. Neurorehabil. Neural. Repair. 2009, 23, 67–77. [Google Scholar] [CrossRef] [Green Version]
- Selles, R.W.; Li, X.; Lin, F. Feedback-controlled and programmed stretching of the ankle plantarflexors and dorsiflexors in stroke: Effects of a 4-week intervention program. Arch. Phys. Med. Rehabil. 2005, 86, 2330–2336. [Google Scholar] [CrossRef]
- Deutsch, J.E.; Latonio, J.; Burdea, G.C. Post-stroke rehabilitation with the Rutgers Ankle system: A case study. Presence Teleoperators Virtual Environ. 2001, 10, 416–430. [Google Scholar] [CrossRef]
- Burdea, G.C.; Cioi, D.; Kale, A. Robotics and gaming to improve ankle strength, motor control, and function in children with cerebral palsy—A case study series. IEEE Trans. Neural. Syst. Rehabil. Eng. 2013, 21, 165–173. [Google Scholar] [CrossRef] [Green Version]
- Maggio, M.G.; Naro, A.; Calatozzo, P. Rehabilitation of somatoparaphrenia with misoplegia: Insights from a single case-pilot study. J. Integr. Neurosci. 2021, 20, 439–447. [Google Scholar] [CrossRef]
- Bessler, J.; Prange-Lasonder, G.B.; Schulte, R.V.; Schaake, L.; Prinsen, E.C.; Buurke, J.H. Occurrence and Type of Adverse Events during the Use of Stationary Gait Robots-A Systematic Literature Review. Front. Robot. AI 2020, 7, 557606. [Google Scholar] [CrossRef] [PubMed]
- Bessler, J.; Prange-Lasonder, G.B.; Schaake, L.; Saenz, J.F.; Bidard, C.; Fassi, I.; Valori, M.; Lassen, A.B.; Buurke, J.H. Safety Assessment of Rehabilitation Robots: A Review Identifying Safety Skills and Current Knowledge Gaps. Front. Robot. AI 2021, 8, 602878. [Google Scholar] [CrossRef] [PubMed]
- Krebs, H.I.; Palazzolo, J.J.; Dipietro, L.; Ferraro, M.; Krol, J.; Rannekleiv, K.; Volpe, B.T.; Hogan, N. Rehabilitation robotics: Performance-based progressive robot-assisted therapy. Auton. Robot. 2003, 15, 7–20. [Google Scholar] [CrossRef]
- Stefano, M.; Patrizia, P.; Mario, A. Robotic upper limb rehabilitation after acute stroke by NeReBot: Evaluation of treatment costs. BioMed Res. Int. 2014, 2014, 265634. [Google Scholar] [CrossRef] [PubMed]
- Hesse, S.; Heß, A.; Werner, C.C. Effect on arm function and cost of robot-assisted group therapy in subacute patients with stroke and a moderately to severely affected arm: A randomized controlled trial. Clin. Rehabil. 2014, 28, 637–647. [Google Scholar] [CrossRef]
- Wagner, T.H.; Lo, A.C.; Peduzzi, P. An Economic Analysis of Robot-Assisted Therapy for Long-Term Upper-Limb Impairment After Stroke. N. Engl. J. Med. 2011, 42, 2630–2632. [Google Scholar] [CrossRef] [Green Version]
- Stephenson, A.; Stephens, J. An exploration of physiotherapists’ experiences of robotic therapy in upper limb rehabilitation within a stroke rehabilitation centre. Disabil. Rehabil. Assist. Technol. 2018, 13, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Tyson, S.; Weightman, A. Professionals’ Views and Experiences of Using Rehabilitation Robotics with Stroke Survivors: A Mixed Methods Survey. Front. Med. Technol. 2021, 3, 780090. [Google Scholar] [CrossRef]
- Zhang, M.; Davies, T.C.; Xie, S. Effectiveness of robot-assisted therapy on ankle rehabilitation—A systematic review. J. Neuroeng. Rehabil. 2013, 10, 30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| N | Title | Study | Study Type | Clinical Field | Sample Size and Patient Characteristics | Intervention | Measures | Outcomes and Conclusions |
|---|---|---|---|---|---|---|---|---|
| 1 | Development and validation of a robotic multifactorial fall-risk predictive model: A one-year prospective study in community-dwelling older adults | A. Cella, 2020 | Longitudinal prospective | Geriatrics | 96 subjects (62 females & 34 males); community-dwelling subjects aged ≥65 years | Evaluation of balance components by using the Hunova robot | Model performance (clinical and robotic parameters): Limit of stability (LOS) test, balance test, five times sit-to-stand (FTSS) test. | A multifactorial fall-risk assessment (that includes clinical and Hunova robotic variables) significantly improves the accuracy of predicting the risk of falling in community-dwelling older people. |
| 2 | Robotic balance assessment in community-dwelling older people with different grades of impairment of physical performance | A. Cella, 2019 | Longitudinal prospective | Geriatrics | 96 subjects | Balance parameters assessed by using the Hunova robot in static and dynamic (unstable and perturbating) conditions, in both standing and seated positions and with the eyes open/closed | Balance parameters (sway area, sway path, anterior–posterior and mediolateral range of oscillation of the CoP and the trunk, trunk variability | The multidimensional balance parameters (as detected by the Hunova robotic system) were significantly correlated with SPPB functional performances in community-dwelling older subjects. |
| 3 | Effect of a robotic training focused on balance and core stability in Parkinson’s disease: a pilot study | F. Vallone, 2019 | Study in clinical practice | Neurology | 10 patients with Parkinson’s disease | Traditional and robotic rehabilitation and exercises with Hunova (20 sessions, 2/week) | Balance; limits of stability; mobility (ankle and pelvis) and ankle force; lower limbs strengthening; trunk control; core strengthening | Improvement in the TUG test, to greater pelvis mobility and stability with an improvement in managing the load in sitting position, besides the maintenance of the improvements achieved with traditional treatments on balance, walking speed, stability limits and trunk mobility |
| 4 | Effectiveness of robotic balance training on postural instability in patients with mild Parkinson’s disease: A pilot, single-blinded, randomized controlled trial | S. Spina, 2021 | A pilot, single-blinded, randomized controlled trial | Neurology | 22 subjects | Robotic balance training with Hunova; 20 treatments (45 min/session, 5 times/week) | Primary outcome measures: Mini BEST test (balance impairments), and Berg Balance Scale (static and dynamic balance impairments); secondary outcome measures: 10-meter walk test, FTSS, and Parkinson’s disease questionnaire | Robotic balance training mat have the same effect as conventional balance training on postural stability. Moreover, robotic training could have additional effects in retaining benefit, reducing risk of falls, and improving QoL. |
| 5 | Treatment of advanced stage Parkinson disease with hunova: a case study | L. Pendolino, 2019 | Single case | Neurology | One patient (70-year-old female) with Parkinson’s disease (IV Hoen and Yahr score) | Ten 1-h sessions with Hunova robot | Sitting postural control; balance in sitting position in static and dynamic conditions; trunk range of motion and control; pelvis range of motion and control; reaching tasks; limits of stability. | Dynamic balance and gait speed functional areas improved; the gait speed increased after the treatment (50% of improvement). |
| 6 | Robot-based assessment of sitting and standing balance: preliminary results in Parkinson’s disease | G. Marchesi, 2019 | Study in clinical practice | Neurology | Ten people with idiopathic PD (72 + 7 std years old; 2 females) and ten age matched healthy subjects (age: 69 + 8; 4 females) without any history of neurological disease | Performance evaluation by using the Hunova robot (while maintaining upright posture in unperturbed, perturbed, and unstable conditions) | Center of pressure displacement; trunk acceleration with a sensor placed on the sternum | Differences in postural control; bigger trunk oscillations coupled with a sharper increase of the CoP backward displacement was seen at the end of the study. |
| 7 | Dynamic Stability and Trunk Control Improvements Following Robotic Balance and Core Stability Training in Chronic Stroke Survivors: A Pilot Study | A. De Luca, 2020 | Open randomized controlled clinical trial | Neurology | 30 patients; The experimental group (N = 15, mean age 58.53 ± 1.87 SE years, 9 females). The control group (N = 15, mean age 63.46 ± 2.51 SE years, 5 females) | Rehabilitative protocol performed with Hunova robot | Balance performance | Experimental group showed greater improvements in proprioceptive control, reactive balance, and postural control in unstable conditions, compared to the control group, showing an improved trunk control with reduced compensatory strategies at the end of the training. |
| 8 | A robot-based assessment of trunk control in Spinal Cord Injured athletes | G. Marchesi, 2020 | Study in clinical practice | Neurology | 10 subjects (8 healthy subjects and 2 expert sit-ski athletes affected by paraplegia after SCI) | Proposed exercises in the protocol performed with Hunova robot | Trunk control | Differences in motor performance was observed at the end of the study |
| 9 | The use of the robotic device hunova as rehabilitation and evaluation tool for functional balance in individuals with spinal cord injury | A. Leo, 2018 | Study in clinical practice | Neurology | 8 subjects (5 M 3 F, mean time from disease 12 ± 5.74, mean age 46 ± 10.6 years) in chronic condition | Evaluation and training sessions performed with Hunova robot | Balance, trunk control, dual motor task with movements of the upper limbs, strengthening, core stability | The subjects showed improvements in trunk control measured both by clinical scales and by Hunova robot during active control tasks and balance tasks in seated position. |
| 10 | The role of hunova in rehabilitative treatment of functional balance in a patient with complete spinal cord injury (SCI) | A. Leo, 2019 | Single case | Neurology | One patient (46-year-old male) with complete neurological loss | 20 sessions (2 sessions per week, 10 weeks) with Hunova | Balance; trunk control; dual-motor-task with movements of the upper limbs; strengthening; core stability | The score of the sitting balance assessment for spinal cord injury (SBASCI) scale improved (from 29 to 37.5). Improved trunk control both in balancing and perturbating conditions and performing active movements with trunk. |
| 11 | Balance assessment and training in an elderly neurological patient: a case study | M. Escelsior, 2020 | Single case | Neurology | One patient (60-year-old male); retro-ocular frontal aneurysm with hemorrahage | Eleven 1-h sessions, twice a week with Hunova | Trunk compensations; trunk oscillations; balance; functional lower extremity strength | Dynamic balance and gait speed functional areas improved at the end of the training program; the gait speed increases after the treatment (50% of improvement). |
| 12 | The role of Hunova in the treatment of patient with a cavernous malformation and hypertrophic olivary degeneration | U. Nguyen, 2021 | Single case | Neurology | One patient; 59-year-old male, former professional hockey player (with a cavernous malformation and hypertrophic olivary degeneration) | 7 customized Hunova training | Monopodalic equilibrium, bipodalic equilibrium | Clinical scales showed improved gait pattern, balance, gait endurance. The improvements obtained in the robotic tests showed increased balance in static and dynamic situations also. |
| 13 | Rehabilitation of somatoparaphrenia with misoplegia: insights from a single case-pilot study | M.G. Maggio, 2021 | Single case | Neurology | One case | Novel multidisciplinary treatment (motor rehabilitation training, traditional physiotherapy and robotic rehabilitation using the Hunova robot and psychological counselling) | Neuropsychological evaluation focused on body representation (BR), cognitive and linguistic functions | The integrated psychological and motor approach may effectively rehabilitate patients with SP, even in the presence of misoplegia. |
| 14 | Use of hunova for rehabilitation following severe acquired brain injury (ABI): a case study | M. Burlando, 2019 | Single case | Neurology | One patient (20-year-old woman) with chronic ABI | 10 sessions (2 sessions per week, 5 weeks) with Hunova. | Bipodalic equilibrium; monopodalic equilibrium; ankle range of motion; balance; core stability | Subject improved her performance in terms of gait speed (20%) and ankle range of motion (46%) assessed by physiotherapists and control of balance in robotic tests. |
| 15 | Proprioceptive and motor training using the high-performance robotic device hunova: preliminary results of a randomized, controlled trial in patients with lower limb post-traumatic conditions | E. Taglione, 2018 | Open randomized controlled clinical trial | Orthopedics | 44 subjects (mean age 45.34 ± 10.41 years): 22 subjects (19 M, 3 F, mean age 45.86 ± 10.93, 10 with proximal and 12 with distal injury) were in experimental group, 22 subjects (16 M, 6 F, mean age 44.81 ± 10.09, 9 with proximal and 13 with distal injury) | A rehabilitation training with Hunova (for 3 weeks) robot. | Balance; limits of stability; endurance proprioceptive; lower extremity | The performance of the experimental group in proprioceptive tests improved significantly compared to the control group (decrease in figural errors in the drawing task, p = 0.03; increase in the number of targets in the grasping test, p = 0.02). Hunova allows one to measure significant parameters of static and dynamic stability and can centralize a complex progression of exercises to recover trunk control and reactive balance after traumatic injuries. Training with Hunova robot was as effective as traditional treatment. |
| 16 | Evaluation and rehabilitation training with hunova robotic system for the recovery of dynamic postural stability: open randomized interventional protocol, on patients after ACL surgical reconstruction | F. Vallone, 2018 | Open randomized controlled clinical trial | Orthopedics | 10 subjects | A rehabilitation training with Hunova (for 8 weeks) robot | Reinforcement; balancing; proprioceptive and core stability | Hunova robot has proven to be safe, easy to use, as effective as conventional treatment, and highly efficient, supporting with its functions all programs of joint mobilization, muscle work, and proprioceptive recovery that were used in the control group. |
| 17 | Hunova as a tool in rehabilitation following robotic knee arthroplasty | A. Di Matteo, 2019 | Case study | Orthopedics | 24 subjects (12 subjects in control group and 12 subjects in experimental group) | 8 sessions (4 sessions per week, for 2 weeks) with Hunova | Weight-bearing sensibilization; proprioception and control; balance; lower-limb strength; core stability and postural passages; BI, KRS, NPRS | Experimental group has better results, compared to control group, in orthostatic stability, postural passages such as sit to stand and in reactive balance at 3-month follow-up. |
| 18 | Rehabilitative treatment of fracture-dislocation of the ankle with hunova: a case study | V. Da Pieve, 2019 | Single case | Orthopedics | One patient (48 years old female) admitted to rehabilitation facility 1 month after surgery for an ankle fracture | 8 sessions (30 min sessions, 2 sessions per week, 1 month) with Hunova | Ankle range of motion; torque; trunk compensations | The left ankle performance improves in terms of ROM and isometric and isokinetic force, and it reaches a good symmetry with the right ankle (<10%). Consequently, balance control increases. |
| 19 | Hunova for performance optimization of the sccocer player: a case study | P. Barbero, 2020 | Single case | Orthopedics | One patient (male, 19 years old, professional youth league U-19 soccer player) | Ten 1-h weekly sessions with Hunova. | Core; ankle range of motion; ankle force; monopodalic equilibrium; bipodalic equilibrium and squat. | The overall performance index score improved from 61% to 76%. The two trained functional areas (core and ROM) reached the average range of performance of the entire team. |
| 20 | Hunova for evaluation and treatment of chronic ankle instability using performance index | G. Risicato, 2020 | Single case | Orthopedics | One patient (24 years old professional basketball player affected by chronic ankle instability) | Eight 1-h sessions, twice a week with Hunova | Ankle range of motion; monopodalic equilibrium; bipodalic equilibrium and squat | The overall performance index score improved from 57% to 74%. The two trained functional areas (core and ROM) reached the average range of performance. In addition, the FAAM score was improved. |
| 21 | Ankle rehabilitation using the high-performance robotic device ARBOT: results from a randomised controlled trial | E. Taglione, 2015 | Randomized controlled clinical trial | Orthopaedics | 32 subjects (31 completed the study) | A rehabilitation training with ARBOT robot | Dorsiflexion ROM; isometric and isokinetic plantar-flexion torque; proprioceptive performance | ARBOT demonstrated to be safe, reliable, and easy to manage. The study showed that the training with ARBOT was totally comparable to traditional methods. |
| 22 | Orthopedic Rehabilitation Using the “Rutgers Ankle” Interface | M. Girone, 2000 | Case study | Orthopedics | 4 subjects (2 patients exhibited hypermobility secondary to chronic ankle instability and the other 2 presented with hypomobility as the sequelae of fractures) | Rutgers ankle prototype | Displacement and torque | The displacement of the uninvolved leg was comparable to normal ROM at the ankle; the maximum torque generated by the uninvolved limb was much larger than that generated by the involved limb. |
| 23 | Rehabilitation of Musculoskeletal Injuries Using the Rutgers Ankle Haptic Interface: Three Case Reports | J. E. Deutsch, 2001 | Single-case series | Orthopedics | 3 subjects; musculoskeletal ankle injuries | Rutgers ankle system with a 3-D piloting of an airplane | ROM; torque generation capacity and ankle mechanical work | Task accuracy improved to 100% for Case 1; a fivefold increase in ankle power output for Case 2 and a three-fold increase for Case 3; both Case 2 and Case 3 reached 100% task accuracy. |
| 24 | Post-stroke rehabilitation with the rutgers ankle system: a case study | J. E. Deutsch, 2001 | Before–after, single case | Neurology | 1 subject; a left cerebral vascular accident | Rutgers ankle system with a 3-D piloting of an airplane | Ankle and foot mobility; force generation; coordination; ability to walk and climb stairs | Strength; endurance; task accuracy; coordination; walking and stair-climbing ability improved over six rehabilitation sessions |
| 25 | Virtual reality-based system for ankle rehabilitation post stroke | R. F. Boian, 2002 | Single case series | Neurology | 3 subjects with post-stroke | Rutgers ankle with two video games | Power and walking endurance | Increase in power generation for all motions and walking endurance increase for one patient |
| 26 | Haptic effects for virtual reality-based post-stroke rehabilitation | R. F. Boian, 2003 | Single case series | Orthopedics | 3 subjects; 2 patients had normal sensation and the third had a decrease with 8/12 on the FM lower extremity sensory score | Second version of VR based ankle rehabilitation system | Muscle strength | Subject 1 increased strength in all four muscle groups, subject 2 in two muscle groups and subject 3 in three muscle groups |
| 27 | Improved gait and elevation speed of individuals post-stroke after lower extremity training in virtual environments | J. E. Deutsch, 2004 | Single case series | Neurology | 6 post-stroke subjects | A robotic device (Rutgers ankle was the input to the virtual environment) | Gait and elevation speed | Gait speed increased 11% (p = 0.08) and elevation time decreased 14% (p = 0.05); gait endurance increased 11%; gait and elevation speed improved from 0 to 44% and 3 to 33% |
| 28 | Ankle control and strength training for children with cerebral palsy using the Rutgers ankle CP: a case study | D. Cioi, 2011 | Single case | Neurology | 1 subject (a child with mild ataxic CP) | Rutgers ankle CP | Impairment, function, and quality of life | Strength, motor control, gait function, overall function, and quality of life improved. |
| 29 | Robotics and Gaming to Improve Ankle Strength, Motor Control, and Function in Children with Cerebral Palsy—A Case Study Series | G. C. Burdea, 2012 | Case study | Neurology | 3 subjects; male children with CP | Rutgers ankle CP | Impairment, function, quality of life and game performance | Strength, motor control, gait function, overall function, quality of life, and game performance improved. |
| 30 | Technical and patient performance using a virtual reality-integrated telerehabilitation system: preliminary finding | J.E. Deutsch, 2007 | Before–after | Neurology | 6 post-stroke subjects | Rutgers ankle prototype robot with VR | Accuracy of ankle movement; exercise duration; training efficiency; mechanical power of ankle; number of repetitions | All measures improved in the first three weeks and did not decrease during the transition. |
| 31 | Effects of Training with a Robot-Virtual Reality System Compared with a Robot Alone on the Gait of Individuals After Stroke | A. Mirelman, 2008 | Randomized controlled trial | Neurology | 18 chronic hemiparesis after stroke patients | Rutgers Ankle Rehabilitation System coupled with VR | Velocity and distance walked | Greater changes in velocity and distance walked were demonstrated for the group trained with the robotic device coupled with the VR than training with the robot alone. |
| 32 | Intelligent Stretching of Ankle Joints with Contracture/Spasticity | L. Q. Zhang, 2002 | Before–after, Case control | Neurology | 9 subjects (5 healthy subjects and 4 chronic stroke patients with ankle contracture and/or spasticity) | A custom-designed joint-stretching device | ROM; joint stiffness; viscous damping; reflex excitability | The passive and active ROM of the ankle joint increased; joint stiffness and viscosity were reduced; reductions in reflex excitability |
| 33 | Feedback-Controlled and Programmed Stretching of the Ankle Plantarflexors and Dorsiflexors in Stroke: Effects of a 4-Week Intervention Program | R. W. Selles, 2005 | Single-case series | Neurology | 10 spasticity and/or contracture after stroke subjects | Feedback controlled and programmed stretching device | ROM; muscle strength; joint stiffness; joint viscous damping; reflex excitability; walking speed; subjective experiences | Significant improvements were found in the passive ROM, maximum voluntary contraction, ankle stiffness, and comfortable walking speed. |
| 34 | Combined passive stretching and active movement rehabilitation of lower-limb impairments in children with cerebral palsy using a portable robot | Y-N. Wu, 2011 | Before–after | Neurology | 12 children with CP | A portable rehabilitation robot with computer game | PROM, AROM, dorsiflexor and plantar flexor muscle strength; selective control assessment of the lower extremity and functional outcome measures | Improvements in dorsiflexion PROM (p = 0.002), AROM (p = 0.02), and dorsiflexor muscle strength (p = 0.001); spasticity of the ankle musculature was reduced (p = 0.01); selective motor control improved (p = 0.005); functionally, participants improved balance (p = 0.0025) and increased walking distance within 6 min (p = 0.025) |
| 35 | Effects of robot-guided passive stretching and active movement training of ankle and mobility impairments in stroke | G. Waldman, 2013 | Before–after | Neurology | 24 stroke survivors with impaired ankle motor function | 18 sessions (3 times a week over 6 weeks) with portable ankle rehabilitation robot | Active dorsiflexion range; dorsiflexor muscle strength; the average MAS, STREAM, and Berg balance | Dorsiflexion active range motion and dorsiflexor muscle strength, MAS, STREAM, and Berg balance significantly improved in the intervention group. |
| 36 | Development of ankle dorsiflexion/plantarflexion exercise device with passive mechanical joint | K. Homma, 2007 | Case control, Single case | Neurology | 5 subjects (4 healthy subjects and a male with hemiplegia) | A passive exercise device for ankle dorsiflexion and plantarflexion | ROM and pressure distribution | Improvements were within the margin of the measuring error. |
| 37 | Assisted movement with enhanced sensation (AMES): coupling motor and sensory to remediate motor deficits in chronic stroke patients | P. Cordo, 2009 | Before-After | Neurology | 11 post-stroke and severe motor disability of the lower extremity patients | AMES treatment device for ankles | Strength; joint position; motor function | Strength increased 10% in most ankles; joint position improved 10% in all ankles; motor function improved significantly. |
| 38 | A proprioceptive neuromuscular facilitation integrated robotic ankle–foot system for poststroke rehabilitation | Z. Zhou, 2015 | Case-control | Neurology | 10 subjects (five normal subjects-age 27.2 ± 1.8 years; five post stroke patients-age 65.6 ± 9.0 years) | PNF treatment with integrated robotic ankle–foot rehabilitation system carried out for 6 weeks (3 times a week) | Passive and active joint properties | PNF integrated robotic ankle–foot rehabilitation system is effective in improving ankle spasticity and/or contracture. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Payedimarri, A.B.; Ratti, M.; Rescinito, R.; Vanhaecht, K.; Panella, M. Effectiveness of Platform-Based Robot-Assisted Rehabilitation for Musculoskeletal or Neurologic Injuries: A Systematic Review. Bioengineering 2022, 9, 129. https://doi.org/10.3390/bioengineering9040129
Payedimarri AB, Ratti M, Rescinito R, Vanhaecht K, Panella M. Effectiveness of Platform-Based Robot-Assisted Rehabilitation for Musculoskeletal or Neurologic Injuries: A Systematic Review. Bioengineering. 2022; 9(4):129. https://doi.org/10.3390/bioengineering9040129
Chicago/Turabian StylePayedimarri, Anil Babu, Matteo Ratti, Riccardo Rescinito, Kris Vanhaecht, and Massimiliano Panella. 2022. "Effectiveness of Platform-Based Robot-Assisted Rehabilitation for Musculoskeletal or Neurologic Injuries: A Systematic Review" Bioengineering 9, no. 4: 129. https://doi.org/10.3390/bioengineering9040129
APA StylePayedimarri, A. B., Ratti, M., Rescinito, R., Vanhaecht, K., & Panella, M. (2022). Effectiveness of Platform-Based Robot-Assisted Rehabilitation for Musculoskeletal or Neurologic Injuries: A Systematic Review. Bioengineering, 9(4), 129. https://doi.org/10.3390/bioengineering9040129







