Journal Description
Société Internationale d’Urologie Journal
Société Internationale d’Urologie Journal
(SIUJ) is an international, peer-reviewed, open access journal that covers all aspects of urology and related fields. The journal is owned by the Société Internationale d’Urologie (SIU) and is published bimonthly online by MDPI (since Volume 5, Issue 1 - 2024).
- Open Access— free for readers and authors (diamond open access), with article processing charges (APC) paid by the Société Internationale d’Urologie.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 39.9 days after submission; acceptance to publication is undertaken in 50.3 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
subject
Imprint Information
Open Access
ISSN: 2563-6499
Latest Articles
Abstracts of the 45th Congress of the Société Internationale d’Urologie
Soc. Int. Urol. J. 2025, 6(5), 67; https://doi.org/10.3390/siuj6050067 - 21 Oct 2025
Abstract
The SIU wishes to extend its gratitude to the urologists who contributed their time to review abstract submissions for the 45th SIU Congress:Refaat Abusamra, Libya;Sanjai Addla, India;Kinju Adhikari, India;Neeraj Agarwal, United States;Madhu Agrawal, India;Sachin Agrawal, United Kingdom;Thomas Ahlering, United States;Shusuke Akamatsu, Japan;Peter
[...] Read more.
The SIU wishes to extend its gratitude to the urologists who contributed their time to review abstract submissions for the 45th SIU Congress:Refaat Abusamra, Libya;Sanjai Addla, India;Kinju Adhikari, India;Neeraj Agarwal, United States;Madhu Agrawal, India;Sachin Agrawal, United Kingdom;Thomas Ahlering, United States;Shusuke Akamatsu, Japan;Peter Albers, Germany;Salah Albuheissi, United Kingdom;Naif Alhathal, Saudi Arabia;Bedeir Ali-El-Dein, Egypt;Murtadha Almusafer, Iraq;Anastasios Anastasiadis, Greece;Mohamed Arafa, Qatar;Amandeep Arora, India;Zeeshan Aslam, United Kingdom;Hammad Ather, Pakistan;Widi Atmoko, Indonesia;Melanie Aubé-Peterkin, QC;Riccardo Autorino, United States;Ben Ayres, United Kingdom;Puskal Kumar Bagchi, India;Ganesh Bakshi, India;Mevlana Derya Balbay, Turkey;Neil Barber, United Kingdom;John Barry, United States;Jens Bedke, Germany;Elisa Berdondini, Italy;Gajanan Bhat, India;Amit Bhattu, United States;Naeem Bhojani, Canada;N I Bhuiyan, Bangladesh;Marta Bizic, Serbia;Damien Bolton, Australia;Vincenzo Borgna, Chile;Muhammad Bulbul, Lebanon;Gian Maria Busetto, Italy;Ana Gabriela Caballero Garcia, Mexico;Adam Calaway, United States;Amparo Camacho, United States;Kevin Campbell, United States;Francesco Capelan, Switzerland;Manuel Castanheira de Oliveira, Portugal;Christine Joy Castillo, Philippines;David Castro-Diaz, Spain;Arun Chawla, India;Manohar ChikkaMoga Siddaiah, India;Archil Chkhotua, Georgia;Sung Yong Cho, Korea, Rep [...]
Full article
Open AccessArticle
Long-Term Patient-Reported Outcomes of Hyperbaric Oxygen Therapy for Haematuria Due to Radiation Cystitis Secondary to External Beam Radiotherapy for Pelvic Malignancy
by
Thomas Milton, Darcy Noll, Peter Stapleton, Henry Shaw, Joseph Hewitt, Marcus Kha, Troy Pudney, Hien Le, Adrian Winsor and Rajinder Singh-Rai
Soc. Int. Urol. J. 2025, 6(5), 66; https://doi.org/10.3390/siuj6050066 - 21 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: To determine long-term patient-reported outcomes for patients undergoing hyperbaric oxygen therapy (HBO2) following external beam radiotherapy. Methods: A retrospective cohort study of all consecutive patients who underwent HBO2 for radiation cystitis in South Australia from September 2017 to March 2023
[...] Read more.
Background/Objectives: To determine long-term patient-reported outcomes for patients undergoing hyperbaric oxygen therapy (HBO2) following external beam radiotherapy. Methods: A retrospective cohort study of all consecutive patients who underwent HBO2 for radiation cystitis in South Australia from September 2017 to March 2023 was performed. Patient-reported symptom severity, anxiety, healthcare use and transfusion requirements pre- and post-treatment were collected through telephone interview. Readmission data and procedural data was collected through both telephone interview and a state-wide electronic medical record. Jamovi was used to perform paired sample t-tests for statistical analysis. Results: There were 89 patients who underwent HBO2 for radiation cystitis with 54 completing the questionnaire. There were 85% of patients alive at the time of follow-up, with 61% of the total cohort and 74% of survivors completing the questionnaire. For those completing the questionnaire, 96% were male with all of them having prostate cancer. Median age was 74 (interquartile range [IQR] 69–78). The mean reduction in patients’ perceived symptom severity after HBO2 on a scale out of 10 was 7.9 to 2 with a difference of 5.9 (95% confidence interval [CI] 5.1–6.7, p < 0.001) and the mean reduction in perceived anxiety was 6.9 to 2.1 with a difference of 4.7 (95% CI 3.6–5.8 p < 0.001). Patients reported a reduction in family doctor visits from 2.7 to 0.76 with a mean reduction of 2 (95% CI 0.8 to 3.2, p = 0.003), emergency department presentations from 3.3 to 0.57 with a mean reduction of 2.7 (95% CI 1.4–4.1, p ≤ 0.001) and blood transfusions from 0.67 to 0.31 with a mean reduction of 0.34 (95% CI −0.44 to 1.1, p = 0.017). Ongoing haematuria was reported in 21 of the 54 patients (39%). Further treatment was required for 20 patients (25%). No patients reported any severe or ongoing adverse effects from HBO2 via the questionnaire. Conclusions: HBO2 is a safe option for recurrent haematuria due to radiation cystitis with high patient satisfaction and reduction in patient-perceived symptom severity, anxiety and healthcare utilisation. Level of evidence: 4.
Full article
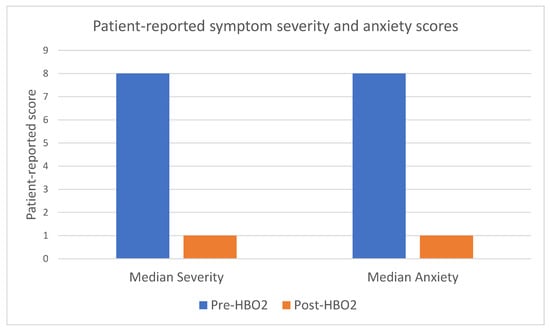
Figure 1
Open AccessSystematic Review
Spontaneous Stone Passage Rates of Ureteric Stones After Stenting for Acute Renal Colic: A Systematic Review
by
Sean Lim, Patrick Gordon, Daryl Thompson, Damien Bolton, Oneel Patel and Joseph Ischia
Soc. Int. Urol. J. 2025, 6(5), 65; https://doi.org/10.3390/siuj6050065 - 21 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: Renal colic poses a significant burden on patients and healthcare systems. Negative ureteroscopy in the setting of stented patients is reported at up to 14%, resulting in unnecessary surgeries and inefficiencies. While ureteral stents have demonstrated efficacy in relieving obstruction, their exact
[...] Read more.
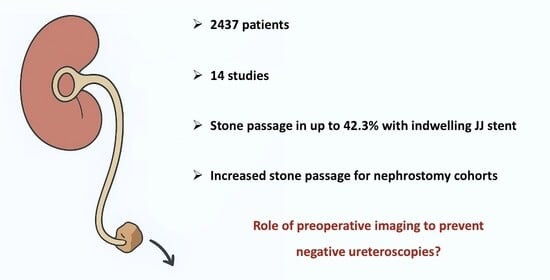
Background/Objectives: Renal colic poses a significant burden on patients and healthcare systems. Negative ureteroscopy in the setting of stented patients is reported at up to 14%, resulting in unnecessary surgeries and inefficiencies. While ureteral stents have demonstrated efficacy in relieving obstruction, their exact effect on spontaneous stone passage (SSP) is unclear. Hence, a systematic evaluation of the literature was performed to identify the impact of ureteral stents on spontaneous stone passage rates. Methods: A systematic search was conducted in MEDLINE, Embase, and PubMed (January 1989–February 2025) to identify studies investigating indwelling ureteric stents and SSP. Two independent reviewers screened the abstracts and full texts, with a third resolving conflicts. Quality assessment was conducted using The Risk Of Bias In Non-randomized Studies—of Interventions (ROBINS-I) and Cochrane Risk of Bias 2 (RoB-2) tools. Results: A total of 2437 patients in 14 studies investigating SSP in stented patients were included. One included study was a randomised controlled trial, but the rest were observational (n = 13). Three studies compared stented and control groups, whereas 11 studies only investigated patients with stents. Mean/median overall stone sizes ranged from 4.7 to 7.8 mm in diameter. Overall, SSP rates with stents varied significantly, ranging from 1.7 to 42.3%, in the setting of variable stone size, location, duration of follow-up, and method of stone passage detection. When comparing stented and non-stented patients, two studies demonstrated impaired SSP rates in stented patients (13.9% vs. 26.8% and 14% vs. 20%), but only one of these differences was statistically significant. Three studies comparing patients with retrograde ureteral stents and nephrostomies found increased SSP rates in nephrostomy cohorts (p < 0.001). Conclusions: Stone passage rates with stents vary widely due to heterogeneity in study design, patient characteristics, and follow-up. Some studies suggest that stents may impair passage; however, evidence remains inconclusive due to the limited availability of high-quality comparative data. This study underscores the need for larger prospective trials to clarify the actual impact of stenting on stone passage.
Full article
Graphical abstract
Open AccessInteresting Images
Nutcracker Syndrome as an Uncommon Cause of Isolated Hematuria in Adults
by
Oleksandr Boiko, Soledad Larburu and David Lecumberri
Soc. Int. Urol. J. 2025, 6(5), 64; https://doi.org/10.3390/siuj6050064 - 21 Oct 2025
Abstract
►▼
Show Figures
Compression of the left renal vein between the abdominal aorta and superior mesenteric artery, known as nutcracker syndrome, can present with subtle, nonspecific symptoms that often delay diagnosis, posing a clinical challenge in daily urology practice and necessitating targeted imaging for accurate identification.
[...] Read more.
Compression of the left renal vein between the abdominal aorta and superior mesenteric artery, known as nutcracker syndrome, can present with subtle, nonspecific symptoms that often delay diagnosis, posing a clinical challenge in daily urology practice and necessitating targeted imaging for accurate identification. We report the case of a 39-year-old patient who presented with isolated hematuria and long-standing pelvic pain and was ultimately diagnosed with nutcracker syndrome. Following the failure of endovascular therapy, the patient underwent renal autotransplantation, resulting in complete resolution of symptoms at follow-up.
Full article

Figure 1
Open AccessArticle
Effectiveness of Transurethral Bulkamid Injections as an Adjunct to the AdVance XP Sling for Male Patients with Post-Prostatectomy Incontinence
by
Sophie Plagakis, Joshua Makary, Thomas King, Vincent Tse and Lewis Chan
Soc. Int. Urol. J. 2025, 6(5), 63; https://doi.org/10.3390/siuj6050063 - 21 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: Bulkamid® (Axonics, Irvine, CA, USA) is a non-particulate polyacrylamide hydrogel used in the treatment of urinary incontinence. While its effectiveness is well-documented in female stress urinary incontinence (SUI), there is limited data on its role in male stress urinary incontinence, particularly
[...] Read more.
Background/Objectives: Bulkamid® (Axonics, Irvine, CA, USA) is a non-particulate polyacrylamide hydrogel used in the treatment of urinary incontinence. While its effectiveness is well-documented in female stress urinary incontinence (SUI), there is limited data on its role in male stress urinary incontinence, particularly post-prostatectomy incontinence (PPI). This study evaluates the efficacy of Bulkamid as a primary or adjunctive treatment for male PPI. Methods: A retrospective chart review was conducted on male patients who developed PPI and underwent Bulkamid injections between 2016 and 2021. Data collected included pre- and post-procedure pad usage, the volume of Bulkamid injected, prior and subsequent incontinence treatments, and patient-reported satisfaction. Bulkamid was injected transurethrally in four quadrants near the vesicourethral anastomosis using a rigid cystoscope. Results: Twenty-one men with a history of radical prostatectomy (six open and fifteen robotic), including four who received adjuvant radiotherapy, were included. Fifteen underwent Bulkamid injection as a primary treatment, with five (33%) requiring repeat injections due to initial improvement. Eight (54%) subsequently underwent an AdVance XP® sling placement, while two (13%) required no further treatment. Six patients received Bulkamid as an adjunct to prior incontinence surgery, with 80% of post-sling patients reporting improved continence. Bulkamid was less effective in men with detrusor overactivity or prior radiation. Conclusions: Bulkamid demonstrated a higher success rate as an adjunct to the AdVance XP sling, with 80% of men experiencing improved continence. As a primary treatment for PPI, success was modest, with only 33% achieving improvement, often requiring repeat injections or conversion to a sling. Bulkamid presents a low-risk option for select male PPI patients, particularly those with prior sling placement, but durability and long-term effectiveness remain concerns.
Full article
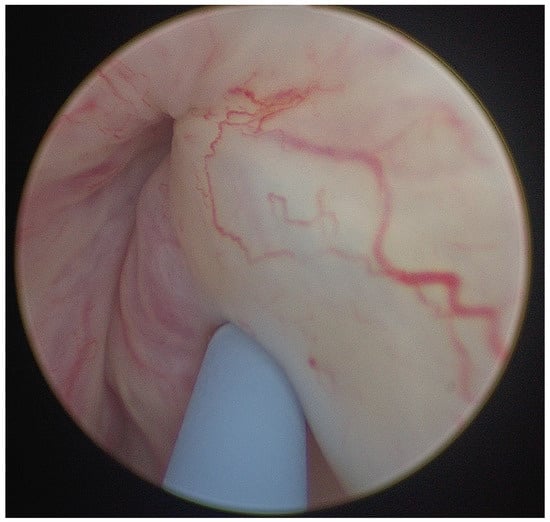
Figure 1
Open AccessArticle
Renal Decompression for Malignant Ureteric Obstruction: A Tertiary Hospital Cohort Analysis
by
Alex Buckby, Rowan David and Arman Kahokehr
Soc. Int. Urol. J. 2025, 6(5), 62; https://doi.org/10.3390/siuj6050062 - 21 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: Malignant ureteric obstruction is an increasingly common problem; however, its treatment remains challenging due to associated poor survival and quality of life outcomes. There is a lack of consensus on how to best manage these patients. We provide a description of
[...] Read more.
Background/Objectives: Malignant ureteric obstruction is an increasingly common problem; however, its treatment remains challenging due to associated poor survival and quality of life outcomes. There is a lack of consensus on how to best manage these patients. We provide a description of the survival outcomes, renal function outcomes, complications, and prognostic factors associated with the treatment of malignant ureteric obstruction in a cohort of patients at our tertiary Urology unit. Methods: A retrospective review of prospectively identified patients treated for malignant ureteric obstruction at our tertiary Urology unit was performed. Obstruction was relieved with either retrograde insertion of a ureteric stent or percutaneous nephrostomy between the 1st of January 2018, and 31st of December 2023. Renal function, complications, and survival data were recorded. Subgroup analysis and survival analysis were performed to determine prognostic factors. Results: Eighty-four patients underwent treatment for malignant ureteric obstruction with a median survival of 197 days (3–1549 days). A total of 51% percent of patients had a stent-related complication requiring hospitalisation, resulting in a total of 966 additional days in hospital. A total of 78% of patients had improved renal function at 12 months. Factors associated with worse survival included emergency treatment of malignant ureteric obstruction, having no further oncological treatment, receiving no oncological-specific treatment for malignancy, bilateral obstruction, female gender, and poor Primary site, Laterality, serum Creatinine level, and Treatment for primary site (PLaCT) prognosis group (p =< 0.01). Conclusions: Patients with malignant ureteric obstruction have a poor prognosis despite intervention. Treatment is often futile and associated with a significant burden of complications related to ureteric stents and percutaneous nephrostomies.
Full article
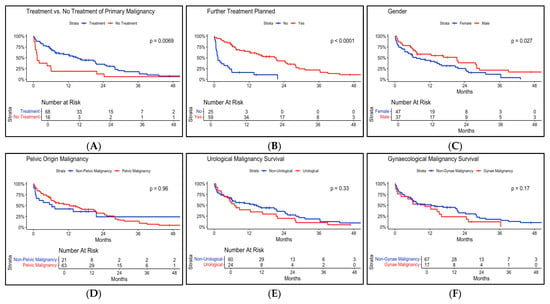
Figure 1
Open AccessInteresting Images
When Bladder Cancer Treatment Strikes Back: Mycotic Aneurysms After Intravesical BCG Therapy
by
Sarah Blackwell, Kevin Yinkit Zhuo, Andrew Jensen and Balasubramanian Indrajit
Soc. Int. Urol. J. 2025, 6(5), 61; https://doi.org/10.3390/siuj6050061 - 20 Oct 2025
Abstract
►▼
Show Figures
Intravesical Bacillus Calmette-Guerin (BCG) remains the gold standard adjuvant therapy for intermediate and high-risk non-muscle invasive bladder cancer (NMIBC) [...]
Full article

Figure 1
Open AccessArticle
The Impact of Patient Navigators on Overactive Bladder Care: Real-World Practice Patterns from a US National Database
by
Ekene Enemchukwu, Jennifer Miles-Thomas, Nitya Abraham, Diane K. Newman, Marc Schwartz, Kimberly Becker Ifantides, Mariana Nelson and Raveen Syan
Soc. Int. Urol. J. 2025, 6(5), 60; https://doi.org/10.3390/siuj6050060 - 20 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: We here describe the impact of navigated care on utilization patterns of pharmacologic and minimally invasive overactive bladder therapies. Methods: This retrospective observational cohort study used electronic medical record data from the Precision Point Specialty Analytics Portal in the United States. Eligible
[...] Read more.
Background/Objectives: We here describe the impact of navigated care on utilization patterns of pharmacologic and minimally invasive overactive bladder therapies. Methods: This retrospective observational cohort study used electronic medical record data from the Precision Point Specialty Analytics Portal in the United States. Eligible patients were adults (≥18 years) newly diagnosed and treated for non-neurogenic overactive bladder (1 January 2015 to 31 December 2019). Categorical endpoints were analyzed by chi-square test or Fisher exact test. Of 170,000 eligible patients, 8982 (≈5%) were randomly selected and stratified by navigation status (navigated: 1150 [12.8%]; non-navigated: 7832 [87.2%]). Results: Overall, 60.0% of patients were female, 69.9% were White, and 42.7% had Medicare coverage. Navigated care was more common among women, Black patients, and those covered by Medicaid/Medicare. Initial pharmacologic treatment rates were similar between navigated and non-navigated groups (anticholinergic: 57.0% vs. 57.4%; beta-3 agonist: 43.0% vs. 42.6%). Greater percentages of navigated versus non-navigated patients received minimally invasive therapy (23.8% vs. 10.8%, respectively; p < 0.0001). Discontinuation rates were lower for navigated versus non-navigated patients undergoing pharmacologic treatment (62.5% vs. 71.3%; p < 0.0001). Conclusions: Patient navigation for overactive bladder may help increase access to minimally invasive therapies and may be a tool to address treatment disparities.
Full article

Graphical abstract
Open AccessArticle
The Clinical Integration of ChatGPT Through an Augmented Patient Encounter in a Real-World Urological Cohort: A Feasibility Study
by
Shane Qin, Emre Alpay, Bodie Chislett, Joseph Ischia, Luke Gibson, Damien Bolton and Dixon T. S. Woon
Soc. Int. Urol. J. 2025, 6(5), 59; https://doi.org/10.3390/siuj6050059 - 20 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: To evaluate the viability of using ChatGPT in a real clinical environment for patient education during informed consent for flexible cystoscopy, assessing its practicality, patient perceptions, and clinician evaluations within a urological cohort. Methods: A prospective feasibility study was conducted at a
[...] Read more.
Background/Objectives: To evaluate the viability of using ChatGPT in a real clinical environment for patient education during informed consent for flexible cystoscopy, assessing its practicality, patient perceptions, and clinician evaluations within a urological cohort. Methods: A prospective feasibility study was conducted at a single institution involving patients with haematuria who attended an in-person clinic review with access to ChatGPT-4o mini. Using predetermined prompts regarding haematuria, we evaluated the accuracy, consistency, and suitability of the ChatGPT information. Responses were appraised for errors, omission of key information, and suitability for patient education. The functionality, usability, and quality of ChatGPT for patient education were assessed by three urologists using the Patient Education Materials Assessment Tool (PEMAT) and DISCERN tools. Readability was assessed using the Flesch–Kincaid tests. Further clinician questionnaires evaluated ChatGPT’s accuracy, reproducibility, and integration potential. Results: Ten patients were recruited, but one patient was excluded because he refused to use ChatGPT due to language barriers. All patients found ChatGPT to be useful, but most believed it could not entirely replace the doctor, especially for obtaining informed consent. There were no significant errors. The mean PEMAT score for understandability was 77.8%, and actionability was 63.8%. The mean DISCERN score was 57.7, corresponding to a ‘good’ quality score. The Flesch Reading Ease score was 30.2, with the writing level comparable to US grade level 13. Conclusions: ChatGPT offers valuable support for patient education, delivering accurate and comprehensive information. However, challenges with readability, contextual understanding, and actionability highlight the need for development and careful integration. Generative artificial intelligence (AI) should augment, not replace, clinician–patient interactions, emphasising ethical considerations and patient trust. This study provides a basis for further exploration of AI’s role in healthcare.
Full article

Figure 1
Open AccessComment
Navigating the Future of Robotic Urological Surgery: The Hinotori System Joins the Expanding Armamentarium. Comment on Ong et al. Early Clinical Outcomes of the Novel Hinotori Robotic System in Urological Surgery—A Review of Existing Literature. Soc. Int. Urol. J. 2025, 6, 56
by
Kevin Lu, Yung-Shun Juan and Wen-Jeng Wu
Soc. Int. Urol. J. 2025, 6(4), 58; https://doi.org/10.3390/siuj6040058 - 21 Aug 2025
Abstract
Over the past two decades, robotic-assisted surgery has revolutionized the field of urology, offering remarkable advancements in surgical precision, reduced perioperative morbidity, and enhanced postoperative recovery [...]
Full article
Open AccessEditorial
Pathways for Innovation in Urology
by
Peter C. Black
Soc. Int. Urol. J. 2025, 6(4), 57; https://doi.org/10.3390/siuj6040057 - 20 Aug 2025
Abstract
The pages of this month’s Société Internationale d’Urologie Journal (SIUJ) feature important contributions addressing the clinical implementation of innovation and technology in Urology [...]
Full article
Open AccessReview
Early Clinical Outcomes of the Novel Hinotori Robotic System in Urological Surgery—A Review of Existing Literature
by
Simone Meiqi Ong, Hong Min Peng, Wei Zheng So and Ho Yee Tiong
Soc. Int. Urol. J. 2025, 6(4), 56; https://doi.org/10.3390/siuj6040056 - 19 Aug 2025
Abstract
►▼
Show Figures
Robotic-assisted surgery has gradually established its role in uro-oncological cases that demand a high level of precision, optimising surgeon ergonomics and decreasing fatigue whilst maintaining optimal clinical outcomes. With the novel Hinotori surgical robot (Medicaroid Corporation (Kobe, Hyogo, Japan)) launched in Japan back
[...] Read more.
Robotic-assisted surgery has gradually established its role in uro-oncological cases that demand a high level of precision, optimising surgeon ergonomics and decreasing fatigue whilst maintaining optimal clinical outcomes. With the novel Hinotori surgical robot (Medicaroid Corporation (Kobe, Hyogo, Japan)) launched in Japan back in 2019, it has now demonstrated its use case across various clinical series of different surgeries. We sought to narratively synthesise the initial feasibility of the Hinotori robotic system in urology. A systematic, comprehensive literature search was conducted across various databases from September 2024 to October 2024. Relevant keywords within the scope of this study were generated for a more accurate search. After exclusion and removal of duplicates, a total of nine articles were included for review. Among the included studies, one study reported data solely on radical prostatectomy for prostate cancer, two studies reported on robotic-assisted nephroureterectomy for renal tumours, two studies reported on partial nephrectomy performed for renal masses, two studies reported on radical nephrectomy carried out for renal malignancies and one study reported on robotic-assisted adrenalectomy for adrenal cancer. Lastly, one study collectively reported on outcomes pertaining to partial nephrectomy, partial nephrectomy, vesicourethral anastomosis and pelvic lymph node dissection in a porcine model, as well as partial nephrectomy, radical prostatectomy and pelvic lymph node dissection in cadavers. The current literature supports its non-inferiority to the well-established Da Vinci system, with no major drawbacks or concerns identified when comparing parameters such as intraoperative time, estimated blood loss (EBL), perioperative events (transfusions, conversion to open surgery), length of hospital stay and major postoperative complications. Future studies involving larger cohorts and more complex surgical cases are essential to further evaluate the efficacy and safety of the Hinotori system. The new Hinotori robotic system offers unique three-dimensional features as a non-inferior robotic platform alternative that has proven clinically safe thus far in its use. Larger scale studies and randomised trials are eagerly awaited to assess and validate more holistically its clinical utility.
Full article
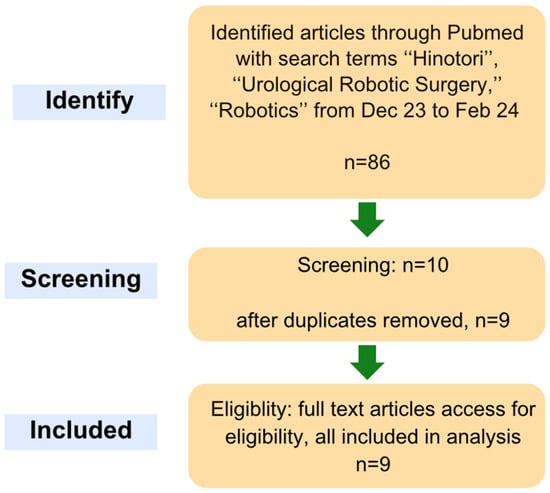
Figure 1
Open AccessArticle
The “Footprint” Sign in Voiding Cystourethrography Indicates Poor Renal Function in Vesicoureteral Reflux: Is It a Pop-Off Mechanism?
by
Hooman Kamran, Negar Mohammadi Ganjaroudi, Nooshin Tafazoli, Mehrzad Mehdizadeh and Abdol-Mohammad Kajbafzadeh
Soc. Int. Urol. J. 2025, 6(4), 55; https://doi.org/10.3390/siuj6040055 - 19 Aug 2025
Abstract
►▼
Show Figures
Background/Objectives: To assess the “footprint” sign in voiding cystourethrogram (VCUG) for its diagnostic and prognostic significance in indicating a “pop-off” mechanism that may reduce pressure on the contralateral kidney. Methods: A retrospective analysis included patients with a “footprint” sign or high-grade vesicoureteral reflux
[...] Read more.
Background/Objectives: To assess the “footprint” sign in voiding cystourethrogram (VCUG) for its diagnostic and prognostic significance in indicating a “pop-off” mechanism that may reduce pressure on the contralateral kidney. Methods: A retrospective analysis included patients with a “footprint” sign or high-grade vesicoureteral reflux (VUR) in VCUG. They were categorized into two groups: those with (Group A) and those without (Group B) the “footprint” sign. Results: Among 55 patients (median age 18 months), 18 exhibited the “footprint” sign. Group A had predominantly male patients. Bilateral VUR was less common in Group A (38.9%) compared to Group B (51.4%), though not statistically significant (p-value: 0.385). The “footprint” sign was predominantly associated with the left side (77.8% in Group A). The median differential renal function (DRF) was significantly lower in kidneys with the “footprint” sign (11.5%) compared to those without (44.5%, p-value < 0.001). All patients with a DRF under 20% exhibited the “footprint” sign. Conclusions: The “footprint” sign correlates with poor renal function, suggesting a potential pop-off mechanism protecting the contralateral kidney. Management should prioritize the contralateral kidney with normal function. The “footprint” sign alone in VCUG may suffice to indicate compromised renal function, negating the need for further ipsilateral kidney assessment.
Full article

Figure 1
Open AccessArticle
First Multi-Center, Real-World Study on the Temporary Implantable Nitinol Device (iTIND) for the Management of Lower Urinary Tract Symptoms Related to Benign Prostatic Obstruction
by
Roberto Castellucci, Silvia Secco, Alberto Olivero, Feras Al Jaafari, Sinan Khadhouri, Alessio Faieta, Cosimo De Nunzio, Riccardo Lombardo, Simone Morselli, Dean Elterman and Luca Cindolo
Soc. Int. Urol. J. 2025, 6(4), 54; https://doi.org/10.3390/siuj6040054 - 13 Aug 2025
Abstract
Background/Objectives: Lower urinary tract symptoms (LUTSs) due to benign prostatic obstruction (BPO) represent a common condition affecting aging men. Transurethral resection of the prostate represents the gold standard surgical treatment but is not without complications such as retrograde ejaculation, bleeding and urinary retention.
[...] Read more.
Background/Objectives: Lower urinary tract symptoms (LUTSs) due to benign prostatic obstruction (BPO) represent a common condition affecting aging men. Transurethral resection of the prostate represents the gold standard surgical treatment but is not without complications such as retrograde ejaculation, bleeding and urinary retention. The temporary implantable nitinol device (iTIND) is considered a minimally invasive surgical technique, designed to treat LUTS while preserving erectile and ejaculatory function. Herein we report the results of a multi-center, real-world assessment of the iTIND procedure. Methods: Data from five international centers treating LUTS with the iTIND device were collected. We recorded changes through an International Prostatic Symptom Score (IPSS) questionnaire with Quality of Life (QoL), International Index of Erectile Function (IIEF5) questionnaire, antegrade ejaculatory function, maximum flow (QMax), post voiding residual volume (PVR) and freedom from repeat intervention. Results: A total of 74 subjects were enrolled; median follow-up was 12 months. IPSS and QoL changed from a median of 23 and 4 points at baseline to 11 and 2 points, respectively, at the last follow-up. A mean improvement in Qmax and PVR from 9 mL/s and 56 mL at baseline to 13 mL/s and 40 mL was noticed at the last follow-up. Total median operative time was 10 min, and the median time of iTIND indwell time was 7 days. The median device removal time was 5 min. There were no changes in IIEF5 scores and antegrade ejaculation rate. No intraoperative complications were reported, and non-serious postoperative complications occurred in six patients (two urinary retention, two mild haematuria, two urinary tract infection). Finally, four patients underwent reoperation during the follow-up period. All procedures were performed as outpatient day cases. Conclusions: Our results confirms that treatment with the iTIND is effective and safe in terms of improving urinary symptoms and quality of life without impacting sexual function. Longer follow-up is required to better define the durability of this minimally invasive procedure.
Full article
Open AccessArticle
Artificial Intelligence in Urology—A Survey of Urology Healthcare Providers
by
Yam Ting Ho, Rizal Rian Dhalas, Muhammad Zohair, Subrata Deb, Mohammed Shoaib, Sandra Elmer, A. H. M. Imrul Tareq, Tauheed Fareed, Nahid Rahman Zico, Agus Rizal Ardy Hariandy Hamid, Isaac A. Thangasamy and Jeremy Y. C. Teoh
Soc. Int. Urol. J. 2025, 6(4), 53; https://doi.org/10.3390/siuj6040053 - 12 Aug 2025
Cited by 1
Abstract
►▼
Show Figures
Background/Objectives: Artificial intelligence (AI) has been utilised in urological conditions such as urolithiasis, urogynaecology and uro-oncology. The aim of this study is to examine the attitudes and beliefs about AI technology amongst urology healthcare providers. Methods: A structured online questionnaire, created
[...] Read more.
Background/Objectives: Artificial intelligence (AI) has been utilised in urological conditions such as urolithiasis, urogynaecology and uro-oncology. The aim of this study is to examine the attitudes and beliefs about AI technology amongst urology healthcare providers. Methods: A structured online questionnaire, created from a modified Delphi method with a panel of urologists and urology surgical trainees, was delivered through the Urological Asia Association’s annual congress. The questionnaire, with 25 items of mixed type responses (five-point Likert scale, nominal-polytomous and open-ended), acquired data regarding demographics, perception and attitudes towards general usage of AI in urological care. Results: A total of 464 respondents from 47 different countries were collected. The results showed that 83.4% of participants believed AI will improve efficiency and 18.8% believed they are knowledgeable in AI technology, with ordinal logistic regression showing both urology specialists and trainees are more likely to agree to these responses. Overall, 51.5% believed AI adoption will not replace clinical practice, and regression analysis found those with previous AI training are more likely to agree to this response. We found AI is commonly used in research, patient education and administrative tasks and identified key enablers as regulatory approval, AI clinical effectiveness and access to AI training. Conclusions: Overall attitudes and beliefs towards the use of AI in urology is positive and encouraging. AI training and education and regulatory reform needs to be addressed to allow integration of AI into clinical practice. A limitation of the study lies in its generalisability to global settings due to the demographics of the respondents.
Full article

Figure 1
Open AccessArticle
Trial of Void at Home After Green Light Laser Photosensitive Vaporisation of the Prostate: A Proof of Concept
by
Arjun Guduguntla, Saad Fahd, Andrew Xu, Lauren Chandler, Ken Chow and Dennis Gyomber
Soc. Int. Urol. J. 2025, 6(4), 52; https://doi.org/10.3390/siuj6040052 - 12 Aug 2025
Abstract
►▼
Show Figures
Background/Objectives: Green light laser photosensitive vaporisation of the prostate (GLL-PVP) is a common procedure for bladder outlet obstruction, with a low incidence of post-operative bleeding. At Northern Health, postoperative management involved limited bladder washout with two bags of 2 L saline, spigotting,
[...] Read more.
Background/Objectives: Green light laser photosensitive vaporisation of the prostate (GLL-PVP) is a common procedure for bladder outlet obstruction, with a low incidence of post-operative bleeding. At Northern Health, postoperative management involved limited bladder washout with two bags of 2 L saline, spigotting, and undergoing a trial of void (TOV) the next morning. A new model of care was commenced in which patients were discharged after the two bags of washout, and the TOV occurred at home through the Hospital in the Home service. The aim of this study was to audit patient outcomes, patient satisfaction, and health service benefits of this novel program. Methods: Patients assigned to the program between March 2023 and June 2024 were analysed. Catheter removal occurred the morning after surgery, and the decision on the success of the TOV was made following an afternoon review. Results: A total of 93.3% (28/30) patients passed their TOV at home. There were no readmissions in the first 48 h postoperation, with only three emergency department (ED) presentations in this time. On a five-point rating scale, 25/25 questionnaire respondents were happy with their care, 20/25 rated the service as very good, and 5/25 rated the service as good. An extra AUD 3377.56 in revenue was generated per patient from the freed inpatient beds, which correlated to a net revenue of AUD 83,016.83 generated over the study period. Conclusions: At-home TOV after GLL-PVP is safe and feasible. There is high patient satisfaction and significant benefits to the healthcare system. This framework can additionally be adopted after other urological surgeries.
Full article

Figure 1
Open AccessCommentary
PSMA PET in Favourable Intermediate-Risk Prostate Cancer? Gold Mine or Money Pit
by
Weiwei Shi, Jianliang Liu, Nathan Lawrentschuk and Marlon Perera
Soc. Int. Urol. J. 2025, 6(4), 51; https://doi.org/10.3390/siuj6040051 - 12 Aug 2025
Abstract
Background/Objectives: Since the proPSMA trial, prostate-specific membrane antigen (PSMA) positron emission tomography (PET) scan has primarily replaced conventional imaging for staging newly diagnosed prostate cancer. The objective of this commentary is to summarise the existing literature on the role of PSMA PET
[...] Read more.
Background/Objectives: Since the proPSMA trial, prostate-specific membrane antigen (PSMA) positron emission tomography (PET) scan has primarily replaced conventional imaging for staging newly diagnosed prostate cancer. The objective of this commentary is to summarise the existing literature on the role of PSMA PET in staging favourable intermediate-risk prostate cancer. Methods: A literature search was conducted on Embase and Ovid MEDLINE, and three retrospective cohort studies were identified. Results: Overall, these studies demonstrated a low prevalence of nodal and distant metastases, as well as modest diagnostic performance of PSMA positron emission tomography-computed tomography (PET-CT) in this patient group. Additionally, PSMA PET did not significantly outperform existing nomograms in predicting lymph node involvement. Conclusions: Given its limited sensitivity, low yield, and cost, the routine use of PSMA PET-CT in favourable intermediate-risk prostate cancer patients is not recommended. Further prospective studies and cost-effectiveness analyses are warranted to clarify its role in this population.
Full article
Open AccessArticle
Intraurethral Steroid and Clean Intermittent Self-Dilatation for Lichen Sclerosus Proven Urethral Stricture Disease—A Retrospective Cohort Study
by
Alex Buckby, Ramesh Shanmugasundaram and Arman Kahokehr
Soc. Int. Urol. J. 2025, 6(4), 50; https://doi.org/10.3390/siuj6040050 - 12 Aug 2025
Abstract
►▼
Show Figures
Background/Objectives: Lichen sclerosus is a chronic lymphocyte-mediated inflammatory disorder with a predilection for the anogenital region. It is a common cause of urethral stricture disease in males. The gold standard treatment is considered to be surgical reconstruction; however, there are many patients who
[...] Read more.
Background/Objectives: Lichen sclerosus is a chronic lymphocyte-mediated inflammatory disorder with a predilection for the anogenital region. It is a common cause of urethral stricture disease in males. The gold standard treatment is considered to be surgical reconstruction; however, there are many patients who are not suitable or not willing to undergo surgery. Cutaneous lichen sclerosus restricted to the foreskin, prepuce or glans is often response to topical corticosteroids; however, the use of intraurethral corticosteroids for urethral involvement has limited research. Methods: We conducted a retrospective cohort study on 18 patients with histologically confirmed lichen sclerosus and associated urethral stricture disease. They were treated with clean intermittent self catheterisation using a hydrophilic catheter coated with 0.05% betamethasone ointment. International Prostate Symptom Score with Quality of Life scores were measured prior to treatment and at follow-up intervals. Results: There was significant improvement in International Prostate Symptom Score and Quality of Life scores at 3 months, 12 months and 24 months, with only 1 patient ceasing treatment due to intolerance. One patient required a single repeat endoscopic dilatation following a period of non-compliance with treatment. Conclusions: Intraurethral corticosteroids with clean-intermittent self-catheterisation is effective and well tolerated for treating lichen sclerosus-associated urethral stricture disease in the short to intermediate term for patients not willing to undergo urethroplasty.
Full article
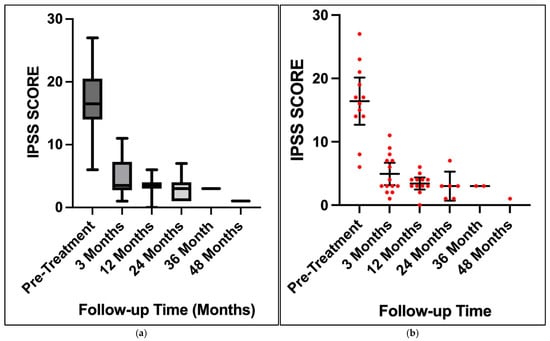
Figure 1
Open AccessReview
Barriers to Introducing New Transformative Surgical Technology in Australian Healthcare: A Comprehensive Review and Guide
by
Matthew Alberto, Jennifer Xu, Oneel Patel, Damien Bolton and Joseph Ischia
Soc. Int. Urol. J. 2025, 6(4), 49; https://doi.org/10.3390/siuj6040049 - 12 Aug 2025
Cited by 2
Abstract
►▼
Show Figures
Background/Objectives: Introducing new transformative surgical technology involves navigating a complex process from design to implementation, often hindered by various barriers that delay the transition into clinical practice. This review critically examines the barriers, proposes a unified guide for medical device implementation in
[...] Read more.
Background/Objectives: Introducing new transformative surgical technology involves navigating a complex process from design to implementation, often hindered by various barriers that delay the transition into clinical practice. This review critically examines the barriers, proposes a unified guide for medical device implementation in the Australian healthcare system utilising the validated Medtech Innovation Guide, and compares regulatory frameworks in Australia, the United Kingdom, and the United States of America. Methods: We conducted a literature review using MEDLINE and EMBASE with MeSH terms or emtree terms and keywords “new OR novel” AND “surgical device OR medical device OR health technology OR surgical technology OR surgical instrument OR transformative technology OR technological innovation OR technological change” AND “implementation OR adoption OR innovation adoption” AND “surgery OR surgical” AND “Australia”. We also assessed governmental websites (gov.au) and documents as well as the Royal Australasian College of Surgeons (RACS) website, policies, and position statements. Furthermore, Australian medical technology start-up companies were asked for any published roadmaps. Results: Four key stakeholder groups were identified: medical professionals, government, hospitals, and patients/consumers. Barriers include surgeon scepticism, regulatory hurdles (e.g., Australian Register of Therapeutic Goods), hospital clearance processes, and meeting patient expectations. To address these challenges, we propose a five-phase system: surgical device development (phase one), compliance with regulatory processes (phase two), research and experimentation (phase three), finalisation for product launch (phase four), and product launch and assessment (phase five). Conclusions: By following our five-phase guide, innovators may better navigate the complexities of integrating transformative surgical technologies into Australian healthcare. Although there are limitations, this approach is based on the validated Medtech Innovation Guide and may help both experienced and inexperienced practitioners better implement innovative technology; however, real-world validation is required.
Full article

Figure 1
Open AccessComment
Is Micro-Ultrasound Ready to Become the New Standard for Prostate Cancer Diagnosis? Comment on Saitta et al. SIU-ICUD: Comprehensive Imaging in Prostate Cancer—A Focus on MRI and Micro-Ultrasound. Soc. Int. Urol. J. 2025, 6, 39
by
Chi-Fai Ng
Soc. Int. Urol. J. 2025, 6(3), 48; https://doi.org/10.3390/siuj6030048 - 17 Jun 2025
Abstract
Prostate cancer remains one of the most prevalent malignancies among men worldwide, with early and accurate diagnosis being critical for improving outcomes [...]
Full article

Journal Menu
► ▼ Journal MenuJournal Browser
► ▼ Journal Browser-
arrow_forward_ios
Forthcoming issue
arrow_forward_ios Current issue - Volumes not published by MDPI
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics