Abstract
Compression of the left renal vein between the abdominal aorta and superior mesenteric artery, known as nutcracker syndrome, can present with subtle, nonspecific symptoms that often delay diagnosis, posing a clinical challenge in daily urology practice and necessitating targeted imaging for accurate identification. We report the case of a 39-year-old patient who presented with isolated hematuria and long-standing pelvic pain and was ultimately diagnosed with nutcracker syndrome. Following the failure of endovascular therapy, the patient underwent renal autotransplantation, resulting in complete resolution of symptoms at follow-up.
Case Presentation
A 39-year-old patient presented with a 1-month history of isolated hematuria. Past history included chronic pelvic pain of 8 years’ duration without identifiable organic cause. There was no personal or family history of genitourinary malformations, malignancy, or infection. Physical examination, laboratory tests, cystoscopy, and initial imaging were unremarkable. Computed tomography revealed compression of the left renal vein (LRV) between the abdominal aorta and superior mesenteric artery (SMA), with prestenotic dilatation and an aortomesenteric angle reduced to 14° (Figure 1 and Figure 2). Magnetic resonance imaging showed dilated left pelvic veins (Figure 3).

Figure 1.
Axial computed tomography of a 39-year-old woman with nutcracker syndrome. There is compression of the left renal vein between the aorta and the superior mesenteric artery, with significant dilation of the left renal vein proximal to the stenosis (white arrow).

Figure 2.
Sagittal computed tomography. The aortomesenteric angle is reduced to 14° (black arrow).
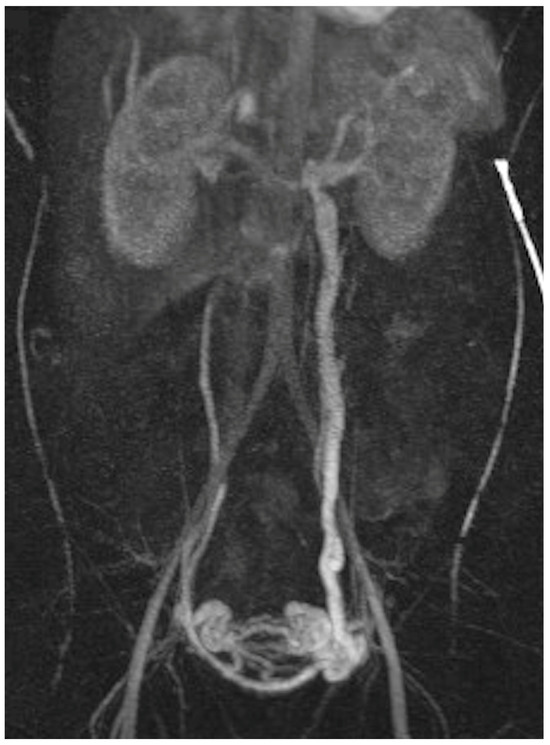
Figure 3.
Magnetic resonance imaging, coronal plane. Dilated pelvic veins on the left side.
Based on clinical and imaging findings, the diagnosis of nutcracker syndrome was established. Initial embolization of the left gonadal vein failed to provide symptom relief. Subsequently, renal autotransplantation involving laparoscopic nephrectomy and reimplantation into the right iliac fossa was performed. Recovery was uneventful, with complete resolution of symptoms at 12-month follow-up.
Nutcracker syndrome is a rare vascular disorder that may present with chronic pelvic pain, hematuria, and, in males, varicocele. It is more commonly observed in young, slender women and represents an important cause of otherwise unexplained hematuria [1]. The underlying mechanism is compression of the LRV between the aorta and SMA, particularly when the aortomesenteric angle is reduced to less than 35° [2]. This leads to elevated venous pressure and the development of collateral circulation, and contributes to hematuria through pressure-induced vascular disruption. Diagnosis remains challenging because radiologic findings are often subtle and nonspecific, frequently delaying recognition in daily urologic practice. Endovascular interventions are considered the first-line therapeutic option; however, in refractory cases, surgical approaches—including renal autotransplantation—may be required [3].
Author Contributions
Conceptualization, O.B. and D.L.; methodology, O.B.; software, O.B. and S.L.; validation, O.B., S.L. and D.L.; formal analysis, O.B.; investigation, O.B.; resources, O.B. and S.L.; data curation, O.B. and S.L.; writing—original draft preparation, O.B.; writing—review and editing, O.B., S.L. and D.L.; visualization, software, O.B. and S.L.; supervision, D.L.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained and archived from the patient for the use of imaging, video recording, and subsequent publication.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Erben, Y.; Gloviczki, P.; Kalra, M.; Bjarnason, H.; Reed, N.R.; Duncan, A.A.; Oderich, G.S.; Bower, T.C. Treatment of Nutcracker Syndrome with Open and Endovascular Interventions. J. Vasc. Surg. Venous Lymphat. Disord. 2015, 3, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Ananthan, K.; Onida, S.; Davies, A.H. Nutcracker Syndrome: An Update on Current Diagnostic Criteria and Management Guidelines. Eur. J. Vasc. Endovasc. Surg. 2017, 53, 886–894. [Google Scholar] [CrossRef] [PubMed]
- Li, K.D.; Bowman, M.S.; Yang, H.; Sui, W.; Freise, C.; Stoller, M. Case Presentation and Review of Renal Autotransplantation for Nutcracker Syndrome. Urol. Case Rep. 2024, 54, 102717. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Société Internationale d’Urologie. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).



