Artificial Intelligence in Urology—A Survey of Urology Healthcare Providers
Abstract
1. Introduction
2. Materials and Methods
2.1. Survey Content/Design
2.2. Data Collection/Analysis
3. Results
3.1. Actual and Perceived Use of AI in Urological Practice
3.2. Attitudes and Beliefs Towards AI in Urological Care
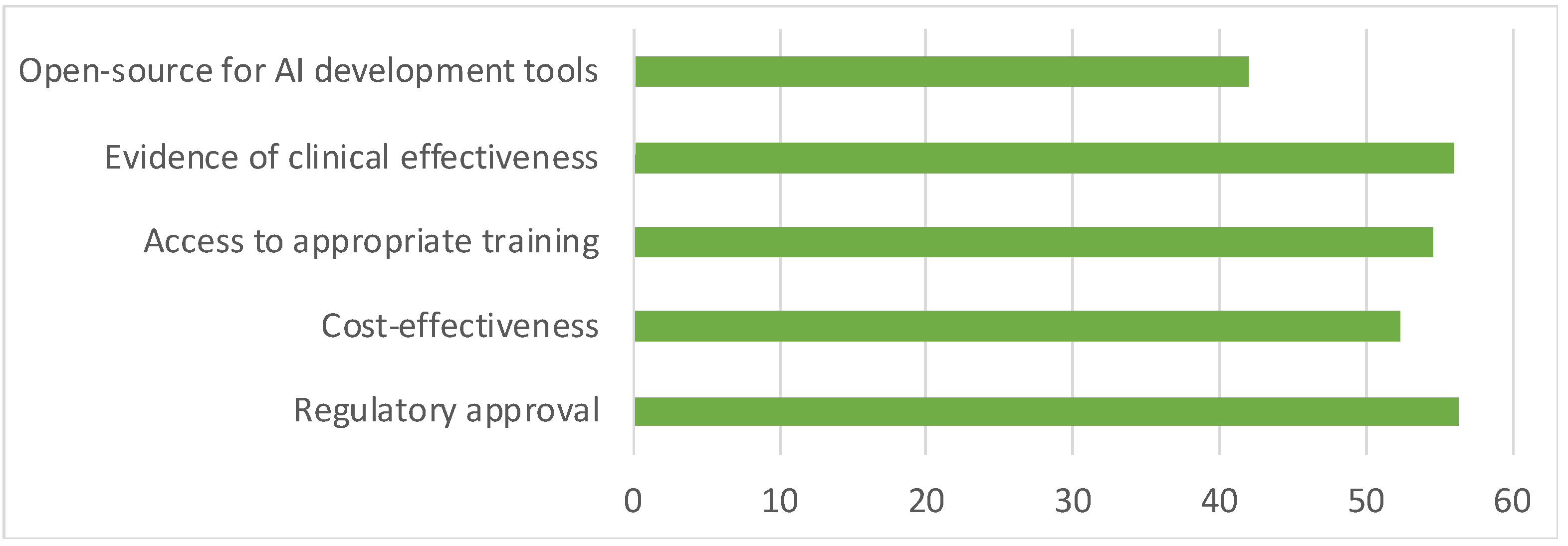
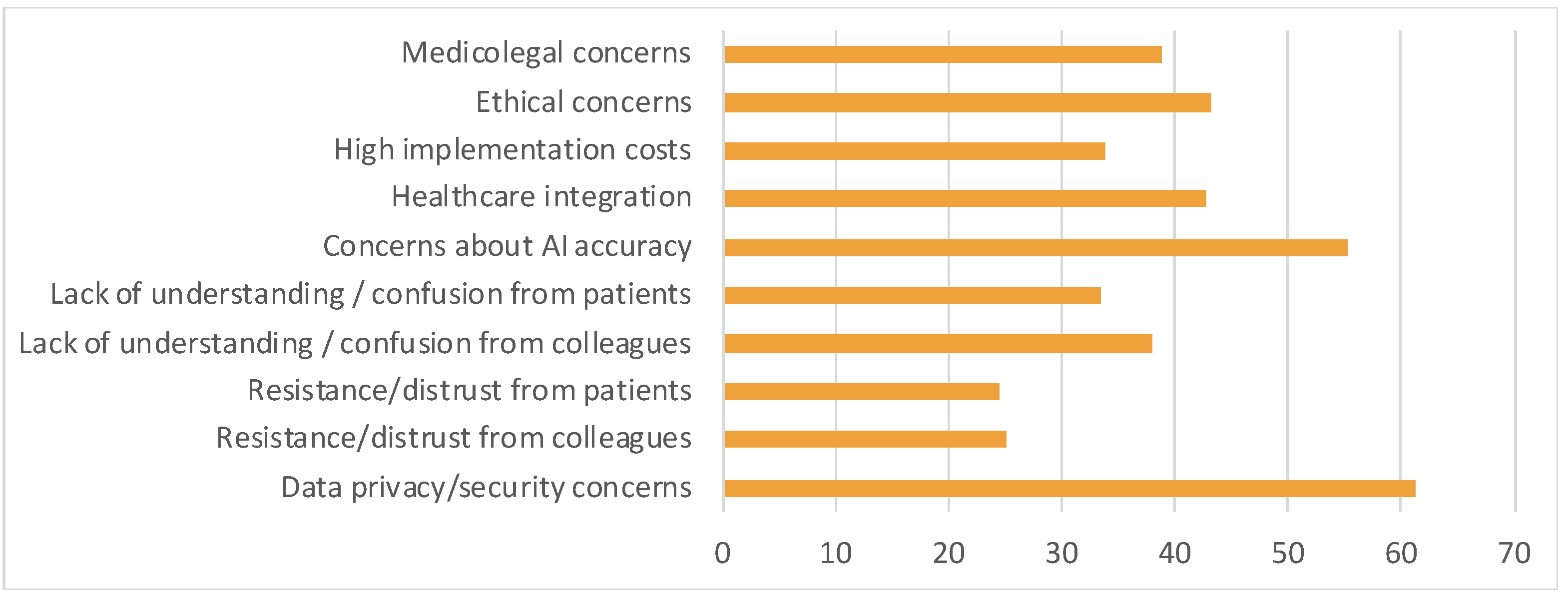
3.3. Perceived Enablers and Barriers for AI Use
3.4. Ordinal Logistic Regression
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AI | Artificial intelligence: technology that allows computers or machines to simulate human behaviours such as learning, comprehension, decision making, problem solving and creativity |
| EMR | Electronic medical records: the electronic medical system that records patient data and information |
| UAA | Urological Association of Asia: the professional urological organisation in Asia, to promote and improve care of urology patients in the region. |
| IP | Internet Protocol |
| CI | Confidence Interval |
| JMO | Junior Medical Officer |
| SIUJ | Société Internationale d’Urologie Journal |
| AUA | American Urological Association |
| CUA | Canadian Urological Association |
| EAU | European Association of Urology |
References
- Shah, M.; Naik, N.; Somani, B.K.; Hameed, B.M.Z. Artificial intelligence (AI) in urology-Current use and future directions: An iTRUE study. Turk. J. Urol. 2020, 46 (Suppl. S1), S27–S39. [Google Scholar] [PubMed]
- Beam, A.L.; Kohane, I.S. Big Data and Machine Learning in Health Care. JAMA 2018, 319, 1317–1318. [Google Scholar] [CrossRef] [PubMed]
- Amisha Malik, P.; Pathania, M.; Rathaur, V.K. Overview of artificial intelligence in medicine. J. Family Med. Prim. Care 2019, 8, 2328–2331. [Google Scholar] [CrossRef]
- Grand View Research. AI in Healthcare Market Size, Share & Trends Analysis Report by Component (Hardware, Services), by Application, by End-use, by Technology, by Region, and Segment Forecasts, 2024–2030. 2024, pp. 1–150. Available online: https://www.grandviewresearch.com/industry-analysis/artificial-intelligence-ai-healthcare-market (accessed on 20 September 2024).
- Liu, X.; Shi, J.; Li, Z.; Huang, Y.; Zhang, Z.; Zhang, C. The Present and Future of Artificial Intelligence in Urological Cancer. J. Clin. Med. 2023, 12, 4955. [Google Scholar] [CrossRef]
- Pinar, U.; Pradere, B.; Roupret, M. Artificial intelligence in bladder cancer prognosis: A pathway for personalized medicine. Curr. Opin. Urol. 2021, 31, 404–408. [Google Scholar] [CrossRef]
- Ananthapadmanabhan, S.; Wang, H.; Shanmugasundaram, R.; Khadra, M.; Thangasamy, I. Artificial intelligence in urology: A technology with transformative potential. Trends Urol. Men’s Health 2024, 15, 3–6. [Google Scholar] [CrossRef]
- Lee, G.; Jeong, C.W. Unleashing the potential: Artificial intelligence in urology for enhanced diagnosis, treatment, and personalized care. Investig. Clin. Urol. 2023, 64, 307–309. [Google Scholar] [CrossRef]
- Knudsen, J.E.; Ghaffar, U.; Ma, R.; Hung, A.J. Clinical applications of artificial intelligence in robotic surgery. J. Robot. Surg. 2024, 18, 102. [Google Scholar] [CrossRef] [PubMed]
- Guo, A.A.; Razi, B.; Kim, P.; Canagasingham, A.; Vass, J.; Chalasani, V.; Rasiah, K.; Chung, A. The Role of Artificial Intelligence in Patient Education: A Bladder Cancer Consultation with ChatGPT. Société Int. D’urologie J. 2024, 5, 214–224. [Google Scholar] [CrossRef]
- Liao, J.; Li, X.; Gan, Y.; Han, S.; Rong, P.; Wang, W.; Li, W.; Zhou, L. Artificial intelligence assists precision medicine in cancer treatment. Front. Oncol. 2022, 12, 998222. [Google Scholar] [CrossRef]
- Teoh, J.Y.C.; Ong, W.L.K.; Gonzalez-Padilla, D.; Castellani, D.; Dubin, J.M.; Esperto, F.; Campi, R.; Gudaru, K.; Talwar, R.; Okhunov, Z.; et al. A Global Survey on the Impact of COVID-19 on Urological Services. Eur. Urol. 2020, 78, 265–275. [Google Scholar] [CrossRef]
- Nasa, P.; Jain, R.; Juneja, D. Delphi methodology in healthcare research: How to decide its appropriateness. World J. Methodol. 2021, 11, 116–129. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.-J.; Zhao, K.; Fils-Aime, F. Response rates of online surveys in published research: A meta-analysis. Comput. Hum. Behav. Rep. 2022, 7, 100206. [Google Scholar] [CrossRef]
- Canady, B.E.; Larzo, M. Overconfidence in Managing Health Concerns: The Dunning-Kruger Effect and Health Literacy. J. Clin. Psychol. Med. Settings 2023, 30, 460–468. [Google Scholar] [CrossRef]
- Yelne, S.; Chaudhary, M.; Dod, K.; Sayyad, A.; Sharma, R. Harnessing the Power of AI: A Comprehensive Review of Its Impact and Challenges in Nursing Science and Healthcare. Cureus 2023, 15, e49252. [Google Scholar] [CrossRef]
- Zhu, X.H.; Wu, C.L.; Zu, X.B.; Lu, J. Editorial: The application of artificial intelligence in diagnosis, treatment and prognosis in urologic oncology. Front. Oncol. 2022, 12, 1118442. [Google Scholar] [CrossRef] [PubMed]
- Brodie, A.; Dai, N.; Teoh, J.Y.; Decaestecker, K.; Dasgupta, P.; Vasdev, N. Artificial intelligence in urological oncology: An update and future applications. Urol. Oncol. 2021, 39, 379–399. [Google Scholar] [CrossRef]
- Petersson, L.; Larsson, I.; Nygren, J.M.; Nilsen, P.; Neher, M.; Reed, J.E.; Tyskbo, D.; Svedberg, P. Challenges to implementing artificial intelligence in healthcare: A qualitative interview study with healthcare leaders in Sweden. BMC Health Serv. Res. 2022, 22, 850. [Google Scholar] [CrossRef]
- Kamel Rahimi, A.; Pienaar, O.; Ghadimi, M.; Canfell, O.J.; Pole, J.D.; Shrapnel, S.; van der Vegt, A.H.; Sullivan, C. Implementing AI in Hospitals to Achieve a Learning Health System: Systematic Review of Current Enablers and Barriers. J. Med. Internet Res. 2024, 26, e49655. [Google Scholar] [CrossRef]
- Yu, K.-H.; Beam, A.L.; Kohane, I.S. Artificial intelligence in healthcare. Nat. Biomed. Eng. 2018, 2, 719–731. [Google Scholar] [CrossRef]
- Fritsch, S.J.; Blankenheim, A.; Wahl, A.; Hetfeld, P.; Maassen, O.; Deffge, S.; Kunze, J.; Rossaint, R.; Riedel, M.; Marx, G.; et al. Attitudes and perception of artificial intelligence in healthcare: A cross-sectional survey among patients. Digit. Health 2022, 8, 20552076221116772. [Google Scholar] [CrossRef] [PubMed]
- Akinrinmade, A.O.; Adebile, T.M.; Ezuma-Ebong, C.; Bolaji, K.; Ajufo, A.; Adigun, A.O.; Mohammad, M.; Dike, J.C.; Okobi, O.E. Artificial Intelligence in Healthcare: Perception and Reality. Cureus 2023, 15, e45594. [Google Scholar] [CrossRef]
- Ganapathi, S.; Duggal, S. Exploring the experiences and views of doctors working with Artificial Intelligence in English healthcare; a qualitative study. PLoS ONE 2023, 18, e0282415. [Google Scholar] [CrossRef]
- Eltawil, F.A.; Atalla, M.; Boulos, E.; Amirabadi, A.; Tyrrell, P.N. Analyzing Barriers and Enablers for the Acceptance of Artificial Intelligence Innovations into Radiology Practice: A Scoping Review. Tomography 2023, 9, 1443–1455. [Google Scholar] [CrossRef]
- Eppler, M.; Ganjavi, C.; Ramacciotti, L.S.; Piazza, P.; Rodler, S.; Checcucci, E.; Rivas, J.G.; Kowalewski, K.F.; Belenchón, I.R.; Puliatti, S.; et al. Awareness and Use of ChatGPT and Large Language Models: A Prospective Cross-sectional Global Survey in Urology. Eur. Urol. 2024, 85, 146–153. [Google Scholar] [CrossRef]
- Mennella, C.; Maniscalco, U.; De Pietro, G.; Esposito, M. Ethical and regulatory challenges of AI technologies in healthcare: A narrative review. Heliyon 2024, 10, e26297. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, R. Legal and human rights issues of AI: Gaps, challenges and vulnerabilities. J. Responsible Technol. 2020, 4, 100005. [Google Scholar] [CrossRef]
- Ahmed, M.I.; Spooner, B.; Isherwood, J.; Lane, M.; Orrock, E.; Dennison, A. A Systematic Review of the Barriers to the Implementation of Artificial Intelligence in Healthcare. Cureus 2023, 15, e46454. [Google Scholar] [CrossRef]
- Cacciamani, G.E.; Chen, A.; Gill, I.S.; Hung, A.J. Artificial intelligence and urology: Ethical considerations for urologists and patients. Nat. Rev. Urol. 2024, 21, 50–59. [Google Scholar] [CrossRef]


| Characteristics | n (N = 464) | % |
|---|---|---|
| Gender | ||
| Male | 403 | 86.85 |
| Female | 61 | 13.15 |
| Age group (years) | ||
| <30 | 90 | 19.4 |
| 30–39 | 215 | 46.34 |
| 40–49 | 104 | 22.41 |
| 50–59 | 36 | 7.76 |
| ≥60 | 19 | 4.09 |
| Continent | ||
| Africa | 1 | 0.22 |
| Asia | 389 | 83.84 |
| Oceania | 44 | 9.48 |
| Europe | 5 | 1.08 |
| North America | 20 | 4.31 |
| South America | 5 | 1.08 |
| Institution | ||
| Teaching hospital/academic institution | 312 | 67.24 |
| Nonacademic public hospital | 67 | 14.44 |
| Private practice | 37 | 7.97 |
| Mixed (public/private) | 48 | 10.34 |
| Occupation | ||
| Urology Consultant/Specialist | 272 | 58.62 |
| Urology Nurse/Nursing Consultant | 2 | 0.43 |
| Urology Resident/Trainee/Registrar | 151 | 32.54 |
| General Practitioner | 31 | 6.68 |
| Hospital staff/JMO/Others | 8 | 1.72 |
| Response to Question “Willing to Use AI in Future Clinical Practice” | Age Groups, n (%) | |
|---|---|---|
| <50 years old | ≥50 years old | |
| Agree | 353 (76.1) | 47 (10.1) |
| Urology Consultant/Specialist | 193 (41.6) | 46 (9.9) |
| Urology Nurse/Nursing Consultant | 1 (0.2) | 1 (0.2) |
| Urology Resident/Trainee/Registrar | 125 (26.9) | - |
| General Practitioner | 27 (5.8) | - |
| Hospital staff/JMO/Others | 7 (1.5) | - |
| Neutral | 46 (9.9) | 8 (1.7) |
| Urology Consultant/Specialist | 21 (4.5) | 8 (1.7) |
| Urology Resident/Trainee/Registrar | 20 (4.3) | - |
| General Practitioner | 4 (0.9) | - |
| Hospital staff/JMO/Others | 1 (0.2) | - |
| Disagree | 10 (2.2) | - |
| Urology Consultant/Specialist | 4 (0.9) | - |
| Urology Resident/Trainee/Registrar | 6 (1.3) | - |
| Total | 409 (88.2) | 55 (11.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Société Internationale d’Urologie. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ho, Y.T.; Dhalas, R.R.; Zohair, M.; Deb, S.; Shoaib, M.; Elmer, S.; Tareq, A.H.M.I.; Fareed, T.; Zico, N.R.; Hamid, A.R.A.H.; et al. Artificial Intelligence in Urology—A Survey of Urology Healthcare Providers. Soc. Int. Urol. J. 2025, 6, 53. https://doi.org/10.3390/siuj6040053
Ho YT, Dhalas RR, Zohair M, Deb S, Shoaib M, Elmer S, Tareq AHMI, Fareed T, Zico NR, Hamid ARAH, et al. Artificial Intelligence in Urology—A Survey of Urology Healthcare Providers. Société Internationale d’Urologie Journal. 2025; 6(4):53. https://doi.org/10.3390/siuj6040053
Chicago/Turabian StyleHo, Yam Ting, Rizal Rian Dhalas, Muhammad Zohair, Subrata Deb, Mohammed Shoaib, Sandra Elmer, A. H. M. Imrul Tareq, Tauheed Fareed, Nahid Rahman Zico, Agus Rizal Ardy Hariandy Hamid, and et al. 2025. "Artificial Intelligence in Urology—A Survey of Urology Healthcare Providers" Société Internationale d’Urologie Journal 6, no. 4: 53. https://doi.org/10.3390/siuj6040053
APA StyleHo, Y. T., Dhalas, R. R., Zohair, M., Deb, S., Shoaib, M., Elmer, S., Tareq, A. H. M. I., Fareed, T., Zico, N. R., Hamid, A. R. A. H., Thangasamy, I. A., & Teoh, J. Y. C. (2025). Artificial Intelligence in Urology—A Survey of Urology Healthcare Providers. Société Internationale d’Urologie Journal, 6(4), 53. https://doi.org/10.3390/siuj6040053








