Journal Description
Endocrines
Endocrines
is an international, peer-reviewed, open access journal on endocrinology published quarterly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within ESCI (Web of Science), Scopus, CAPlus / SciFinder, and other databases.
- Journal Rank: CiteScore - Q2 (Medicine (miscellaneous))
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 41.7 days after submission; acceptance to publication is undertaken in 9.7 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
Latest Articles
The Impact of Chronic Autoimmune Thyroiditis During Pregnancy on Maternal and Fetal Outcomes
Endocrines 2025, 6(4), 56; https://doi.org/10.3390/endocrines6040056 - 20 Nov 2025
Abstract
Background/Objectives: Thyroid dysfunction during pregnancy is associated with a range of adverse perinatal outcomes. This study aims to evaluate the effect of maternal thyroid autoimmunity on selected gestational and perinatal outcomes of the newborn in a region with adequate iodine intake. Methods
[...] Read more.
Background/Objectives: Thyroid dysfunction during pregnancy is associated with a range of adverse perinatal outcomes. This study aims to evaluate the effect of maternal thyroid autoimmunity on selected gestational and perinatal outcomes of the newborn in a region with adequate iodine intake. Methods: This retrospective study included 74 full-term singleton pregnancies from women living in the coastal region of Romania. Participants were divided into two groups: group 1—women with chronic autoimmune thyroiditis and euthyroidism; group 2—women without thyroid disorders, serving as the control group. Maternal variables assessed included serum thyroid hormone levels and antithyroid autoantibodies. For newborns, parameters such as birth weight, neonatal TSH levels, and the incidence of gestational and perinatal events were evaluated. Results: The incidence of chronic autoimmune thyroiditis in the study population was 36.4%. Maternal thyroid autoimmunity was associated with an increased incidence of low birth weight, observed in 11% of the autoimmune group compared with 2.1% in the control group (p = 0.099). The incidence of preterm birth was significantly higher in the autoimmune group (18.5% vs. 4.2% in controls, p = 0.043), corresponding to a 4.3-fold increase in relative risk. The most frequent perinatal complication observed in pregnant women with thyroid autoimmunity was spontaneous abortion (11.1%). The median urinary iodine concentrations were within the adequate range in both study groups. Conclusions: Thyroid autoimmunity during pregnancy presents significant clinical challenges, even in areas with adequate iodine intake. Maternal autoimmune thyroiditis constitutes an established risk factor for impaired fetal development and adverse perinatal outcomes. Early assessment of thyroid function prior to conception or during the first trimester is recommended for both diagnostic and preventive purposes.
Full article
(This article belongs to the Section Female Reproductive System and Pregnancy Endocrinology)
Open AccessReview
Diagnosis of Congenital and Acquired Generalized Lipodystrophies—Similarities and Differences
by
Josivan Gomes Lima, Lucas Nobrega Lima, Vitor Yan Bezerra Araujo, Lucia Helena Coelho Nobrega and Julliane Tamara Araújo de Melo Campos
Endocrines 2025, 6(4), 55; https://doi.org/10.3390/endocrines6040055 - 17 Nov 2025
Abstract
Generalized lipodystrophies (GLs) are rare diseases characterized by a lack of body fat. When patients with a GL phenotype are referred with a presumptive diagnosis of congenital generalized lipodystrophy (CGL) but genetic testing for known pathogenic variants is negative, the diagnosis of acquired
[...] Read more.
Generalized lipodystrophies (GLs) are rare diseases characterized by a lack of body fat. When patients with a GL phenotype are referred with a presumptive diagnosis of congenital generalized lipodystrophy (CGL) but genetic testing for known pathogenic variants is negative, the diagnosis of acquired generalized lipodystrophy (AGL) becomes a more likely diagnosis. No single test confirms such a diagnosis, and it is crucial to recognize the similarities and differences between these diseases. We review the literature and report four GL cases from our lipodystrophy outpatient clinic, highlighting the main points for an accurate diagnosis. Similarities: phlebomegaly, umbilical scar protrusion, loss of Bichat’s fat pad, muscle hypertrophy, and hepatomegaly can occur in both. Cirrhosis can also arise, but in AGL, it occurs as a consequence of hepatic steatosis and also due to autoimmune hepatitis. Insulin resistance is frequent, and patients present acanthosis nigricans and acrochordons and may develop difficult-to-control diabetes and its complications, despite very high daily doses of insulin. Low HDL and hypertriglyceridemia are frequent and may progress to acute pancreatitis. Serum leptin levels are typically low and contribute to hyperphagia. Differences: AGL patients’ body fat loss occurs gradually in childhood or adolescence, whereas CGL patients are born with the characteristic phenotype. Evaluating photographs of AGL patients in the first years of life can provide evidence of this selective and gradual fat loss. Some AGL patients may have panniculitis (inflamed and painful subcutaneous nodules), with or without autoimmune diseases. In conclusion, recognizing both similarities and differences is crucial for making an accurate diagnosis and ensuring the most appropriate treatment.
Full article
(This article belongs to the Section Obesity, Diabetes Mellitus and Metabolic Syndrome)
►▼
Show Figures

Figure 1
Open AccessReview
The Role of Follicle-Stimulating Hormone in Bone Loss During Menopause Transition: A Narrative Review
by
Nida Jugulytė and Daiva Bartkevičienė
Endocrines 2025, 6(4), 54; https://doi.org/10.3390/endocrines6040054 - 5 Nov 2025
Abstract
For many years, menopause-related bone loss has been attributed solely to declining estrogen levels. Recently it has been suggested that bone loss accelerates during perimenopause, often preceding declines in estradiol (E2), proposing that follicle-stimulating hormone (FSH), the levels of which are
[...] Read more.
For many years, menopause-related bone loss has been attributed solely to declining estrogen levels. Recently it has been suggested that bone loss accelerates during perimenopause, often preceding declines in estradiol (E2), proposing that follicle-stimulating hormone (FSH), the levels of which are high during late perimenopause, may play a role in skeletal deterioration independently of E2. The aim of this narrative review was to present aspects of bone health throughout the menopause transition with a focus on the relationship between FSH and bone-related outcomes. Epidemiological studies evaluating bone mineral density (BMD) and bone turnover markers (BTMs) were analyzed. Higher FSH levels were associated with reduced BMD, particularly at the spine and hip, as well as enhanced bone remodeling activity. In several longitudinal studies, FSH was found to be a more reliable predictor of bone loss than estrogen. In conclusion, FSH may serve as an early marker of perimenopausal bone health deterioration by identifying women at risk for bone loss and allowing for more personalized prevention strategies; however, further research is needed before its clinical use.
Full article
(This article belongs to the Section Female Reproductive System and Pregnancy Endocrinology)
Open AccessFeature PaperReview
The Mechanisms of Angiogenesis and Apoptosis During the Functional Formation and Regression of the Corpus Luteum in the Ovarian Reproductive Endocrine System
by
Dody Houston Billhaq and Seunghyung Lee
Endocrines 2025, 6(4), 53; https://doi.org/10.3390/endocrines6040053 - 21 Oct 2025
Abstract
The ovarian corpus luteum has functional mechanisms for formation and regression in the reproductive endocrine system. The main functional events of the corpus luteum are angiogenesis and apoptosis mechanisms. The development of the corpus luteum involves homogeneous physiological mechanisms, including cellular functions and
[...] Read more.
The ovarian corpus luteum has functional mechanisms for formation and regression in the reproductive endocrine system. The main functional events of the corpus luteum are angiogenesis and apoptosis mechanisms. The development of the corpus luteum involves homogeneous physiological mechanisms, including cellular functions and reproductive hormones. Angiogenesis is controlled by pro-angiogenic and anti-angiogenic factors. The microenvironment involves various signaling molecules and pathways that may play a potential role in angiogenic response during corpus luteum growth. In luteolysis, the corpus luteum undergoes degeneration, notably induced by reproductive hormones that promote programmed cell death in luteal cells through the apoptosis mechanism. In this sudy, we discuss the mechanisms and functional roles of angiogenesis and apoptosis in the endocrine microenvironment during corpus luteum formation and regression, based on the interrelationship of physiological events in the ovary.
Full article
(This article belongs to the Section Female Reproductive System and Pregnancy Endocrinology)
►▼
Show Figures

Figure 1
Open AccessArticle
Gestational Weight Gain and Adverse Pregnancy Outcomes in Women with Gestational Diabetes Mellitus and Obesity
by
Filipe Dias de Souza, Patrícia Medici Dualib, Martha Camillo Jordão, Micaela Frasson Montero, Maria Carolina Oliveira Abate, Leonardo Luna, Rosiane Mattar and Bianca de Almeida-Pititto
Endocrines 2025, 6(4), 52; https://doi.org/10.3390/endocrines6040052 - 20 Oct 2025
Abstract
Background/Objectives: The association between gestational weight gain (GWG) and adverse outcomes in individuals with gestational diabetes mellitus (GDM) and obesity remains unclear. This study aimed to evaluate the relationship between total GWG and maternal, obstetric, and neonatal outcomes in patients with GDM, stratified
[...] Read more.
Background/Objectives: The association between gestational weight gain (GWG) and adverse outcomes in individuals with gestational diabetes mellitus (GDM) and obesity remains unclear. This study aimed to evaluate the relationship between total GWG and maternal, obstetric, and neonatal outcomes in patients with GDM, stratified by obesity class. Methods: This retrospective cohort included 695 pregnant individuals with GDM treated at a tertiary university hospital in Brazil between 2007 and 2021. GWG was categorized as insufficient, adequate, or excessive per National Academy of Medicine guidelines. Outcomes included maternal, obstetric, and neonatal events. Analyses were conducted for the entire cohort and stratified by obesity class (I and II/III), using multivariate regression models adjusted for maternal age, parity, and pre-pregnancy BMI. Results: The mean age was 33.6 (SD 5.7) years. GWG was insufficient in 33.2%, adequate in 28.2%, and excessive in 37.8%. Excessive GWG was associated with increased odds of cesarean delivery (OR 1.69; 95% CI 1.15–2.48) and large-for-gestational-age newborns (OR 3.29; 95% CI 1.61–6.46). As a continuous variable, GWG was positively associated with cesarean delivery (OR 1.04), LGA (OR 1.10), and birthweight (β = 0.02). Lower GWG was independently associated with reduced preeclampsia risk (OR 1.09 per kg). Insufficient GWG was not linked to increased risk of small-for-gestational-age newborns or other adverse outcomes and was associated with lower insulin requirement. Results remained consistent across obesity subgroups, except for cesarean delivery in class II/III obesity. Conclusions: In individuals with GDM and obesity, insufficient GWG was not associated with increased adverse outcomes, while excessive GWG was consistently linked to unfavorable maternal and neonatal risks. Stricter GWG control may be safe and beneficial in this population.
Full article
(This article belongs to the Section Obesity, Diabetes Mellitus and Metabolic Syndrome)
►▼
Show Figures
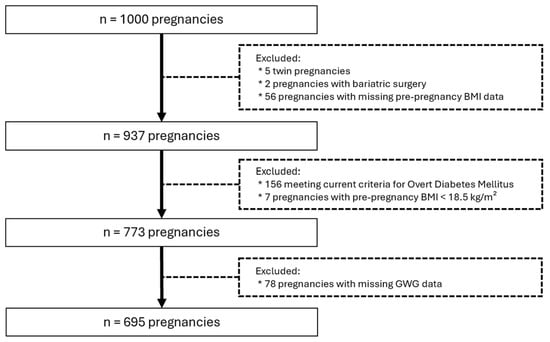
Figure 1
Open AccessArticle
Circulating miR-122 and miR-139-3p: Association with Lipid, Inflammatory, and Glycemic Profile in Adolescents with Insulin-Resistant and Overweight
by
Tanyara Baliani Payolla, Paula Nascimento Brandão-Lima, Gabrielli Barbosa de Carvalho, Flávia Mori Sarti, Regina Mara Fisberg and Marcelo Macedo Rogero
Endocrines 2025, 6(4), 51; https://doi.org/10.3390/endocrines6040051 - 15 Oct 2025
Abstract
Background/Objectives: Insulin resistance (IR) in adolescents contributes to the development of metabolic and immunological alterations. These alterations can lead to chronic, systemic, low-grade inflammation in adulthood. Evidence suggests that alterations in miRNA expression play a significant role in the onset of IR by
[...] Read more.
Background/Objectives: Insulin resistance (IR) in adolescents contributes to the development of metabolic and immunological alterations. These alterations can lead to chronic, systemic, low-grade inflammation in adulthood. Evidence suggests that alterations in miRNA expression play a significant role in the onset of IR by influencing insulin signaling pathways. Therefore, identifying specific miRNAs may aid in the early diagnosis of cardiometabolic risk, particularly during the transition from adolescence to adulthood. Methods: This population-based study aimed to analyze the expression of 21 miRNAs in the plasma of adolescents. We considered IR status, overweight, sex, and age for the analyses. The study measured miRNA expression in plasma samples from 187 adolescents aged 12 to 19 years from the cross-sectional study of the 2015 São Paulo Health Survey (ISA-Nutrition). MiRNA expression was assessed using Exiqon® assays on Fluidigm® technology (Les Ulis, France). Statistical analyses were performed to identify differences in miRNA expression and correlations between variables, using a complex research design to ensure representativeness at the population level. Results: The incidence of IR and overweight was high in adolescents (44% and 33%, respectively). High-sensitivity C-reactive protein (hs-CRP) concentration was higher in overweight adolescents. IR was correlated with higher plasma expression of miR-122 and miR-139-3p. Furthermore, miR-486, miR-363, miR-30d, miR-28, miR-223, miR-21, miR-146, miR-130b, miR-126, miR-122, and miR-139-3p showed specific correlations with individual risk for IR, sex, and adolescent stage. Conclusions: The miRNAs showed differential expression according to sex and adolescent stage, and were correlated with cardiometabolic risk factors, suggesting their potential utility for early screening in adolescents. The study highlights age- and sex-related differences in miRNA levels between adolescents with IR and overweight. The cross-sectional design is a limitation of this study, as we cannot infer causality for the associations observed here.
Full article
(This article belongs to the Section Obesity, Diabetes Mellitus and Metabolic Syndrome)
►▼
Show Figures

Figure 1
Open AccessArticle
Obesity Is Associated with Larger Thyroid Nodules but Not with Malignant Cytology
by
Stefania Giuliano, Giuseppe Seminara, Stefano Iuliano, Stefania Obiso, Eusebio Chiefari, Daniela P. Foti, Maria Mirabelli and Antonio Brunetti
Endocrines 2025, 6(4), 50; https://doi.org/10.3390/endocrines6040050 - 14 Oct 2025
Abstract
Background: Obesity has been proposed as a risk factor for differentiated thyroid carcinoma (DTC), though findings in the literature remain conflicting. While some studies suggest an association between elevated body mass index (BMI) and thyroid malignancy, others attribute this link to diagnostic bias.
[...] Read more.
Background: Obesity has been proposed as a risk factor for differentiated thyroid carcinoma (DTC), though findings in the literature remain conflicting. While some studies suggest an association between elevated body mass index (BMI) and thyroid malignancy, others attribute this link to diagnostic bias. The Calabria region in Southern Italy, historically affected by iodine deficiency and endemic goiter, offers a valuable population for investigating this relationship. Objective: This study aimed to evaluate the association between obesity and clinical, sonographic, and cytological characteristics of thyroid nodules in a Calabrian cohort undergoing fine-needle aspiration biopsy (FNAB). Methods: This retrospective observational study included 1192 patients evaluated at a single endocrine referral center between 2015 and 2024. Patients were stratified by BMI (<30 vs. ≥30 kg/m2). Demographic, biochemical, ultrasound, and cytological data were collected and analyzed. Cytological results were classified according to the SIAPEC 2014 system. Results: Obese patients had significantly larger thyroid nodules in terms of anteroposterior and transverse diameters, as well as overall volume (p < 0.05). However, the distribution of high-risk cytological categories (TIR 3B, TIR 4, and TIR 5) did not differ significantly between obese and non-obese patients (9.4% in both groups). Multivariate analysis confirmed that BMI was not an independent predictor of malignancy risk (OR 0.988; p = 0.723), whereas younger age was inversely associated with malignancy. Conclusions: Obesity appears to influence thyroid nodule size but does not constitute an independent risk factor for cytological malignancy. BMI should not influence indications for FNAB or subsequent treatment decisions. Thyroid nodule management should instead rely on ultrasound risk stratification and cytological findings. Special attention should be given to younger patients as they may carry a higher malignancy risk.
Full article
(This article belongs to the Special Issue Feature Papers in Endocrines 2025)
Open AccessReview
Sleep Deprivation and Its Impact on Insulin Resistance
by
Margarida C. Pinheiro, Henrique E. Costa, Melissa Mariana and Elisa Cairrao
Endocrines 2025, 6(4), 49; https://doi.org/10.3390/endocrines6040049 - 11 Oct 2025
Abstract
►▼
Show Figures
Background/Objectives: Adequate sleep has a fundamental role in human health, mainly in cognitive and physiological functions. However, the daily demands of modern society have led to a constant pursuit of better living conditions, requiring more active hours at the expense of sleeping
[...] Read more.
Background/Objectives: Adequate sleep has a fundamental role in human health, mainly in cognitive and physiological functions. However, the daily demands of modern society have led to a constant pursuit of better living conditions, requiring more active hours at the expense of sleeping hours. This sleep deprivation has been associated with human health deterioration, namely an increase in Diabetes Mellitus incidence. This metabolic disease is a chronic pathology that imposes a big burden on health systems and is associated with the rise in insulin resistance. In this sense, the aim of this review is to analyze the relation between sleep deprivation and insulin resistance, emphasizing the metabolic parameters and hormones that may be involved in the subjacent mechanism. Methods: A literature review of the last 10 years was performed with specific terms related to “sleep deprivation” and “insulin resistance”. Results: Overall, the studies analyzed showed a decrease in insulin sensitivity in cases of sleep deprivation, even with different study protocols. In addition, an association between sleep deprivation and increased non-esterified fatty acids was also noticeable; however, other parameters such as cortisol, metanephrines, and normetanephrines showed no consistent results among the studies. Conclusions: This review allowed us to confirm the relationship between sleep deprivation and insulin resistance; however, despite the difficulties to monitor sleep, more research is needed to understand the related mechanisms that have not yet been clarified.
Full article

Graphical abstract
Open AccessReview
Comparing Glucometer-Based and Laboratory-Based OGTT for Diabetes Diagnosis: A Narrative Review
by
Tanvir Ahmed, Jaimala Kishore, Mensila Onamika, Shuvratithi Goswami, Iffat Rahman Momo, Hanif Sumon and Rodney G. Bowden
Endocrines 2025, 6(3), 48; https://doi.org/10.3390/endocrines6030048 - 18 Sep 2025
Abstract
Background: The oral glucose tolerance test (OGTT) is the gold standard for diagnosing diabetes; however, its use is often limited by the need for laboratory infrastructure, trained personnel, and extended turnaround times. In contrast, glucometer-based OGTT offers a convenient and affordable alternative, especially
[...] Read more.
Background: The oral glucose tolerance test (OGTT) is the gold standard for diagnosing diabetes; however, its use is often limited by the need for laboratory infrastructure, trained personnel, and extended turnaround times. In contrast, glucometer-based OGTT offers a convenient and affordable alternative, especially in resource-limited settings. Objective: This narrative review aims to assess the diagnostic accuracy of glucometer-based OGTT compared to standard laboratory-based OGTT, while also evaluating its feasibility and potential application in diabetes screening programs. Evidence Summary: Studies consistently demonstrate a strong correlation between capillary glucose levels measured by glucometers and venous plasma glucose concentrations obtained through standard laboratory methods. Many studies reported high sensitivity and specificity, often exceeding 90%, particularly when using well-calibrated, newer-generation devices. These findings support the diagnostic utility of glucometer-based OGTT in various populations, although performance may vary by device model and clinical context. Standardization of testing protocols remains essential for consistent results. Conclusions: Glucometer-based OGTT shows promise as a reliable, rapid and cost-effective diagnostic approach, particularly in low-resource and community-based settings. While it is not a complete substitute for laboratory-based OGTT, it offers substantial advantages in accessibility, affordability, and scalability. Continued research with newer-generation glucometers and standardized testing protocols is essential to support broader clinical implementation and public health integration.
Full article
(This article belongs to the Section Obesity, Diabetes Mellitus and Metabolic Syndrome)
Open AccessReview
Diabetes and Sarcopenia: Unraveling the Metabolic Crossroads of Muscle Loss and Glycemic Dysregulation
by
Jose Jorge Ortez Toro
Endocrines 2025, 6(3), 47; https://doi.org/10.3390/endocrines6030047 - 18 Sep 2025
Abstract
The intersection of type 2 diabetes mellitus (T2DM) and sarcopenia, often termed diabetic sarcopenia, represents a critical yet underrecognized comorbidity that significantly impacts the quality of life and functional capacity of older adults. This paper explores the complex interplay between T2DM and sarcopenia,
[...] Read more.
The intersection of type 2 diabetes mellitus (T2DM) and sarcopenia, often termed diabetic sarcopenia, represents a critical yet underrecognized comorbidity that significantly impacts the quality of life and functional capacity of older adults. This paper explores the complex interplay between T2DM and sarcopenia, focusing on the prevalence, risk factors, and underlying mechanisms driving muscle mass and strength decline in this population. Drawing from recent clinical studies, we highlight a prevalence of sarcopenia ranging from 15.36% to 30.2% among elderly T2DM patients, with notable gender disparities (41.3% in men versus 20.1% in women) and regional variations. Key risk factors identified include poor glycemic control (HbA1c ≥8%), longer diabetes duration (>5 years), low body mass index (BMI), and reduced levels of 25-hydroxyvitamin D and insulin-like growth factor-1 (IGF-1). We also recommend a practical screening algorithm for diabetic sarcopenia, integrating tools like the SARC-F questionnaire, dynamometry, and BMI-adjusted calf circumference to facilitate early diagnosis and staging in clinical settings. The review underscores the need for a multidisciplinary approach—encompassing pharmacological optimization, nutritional interventions with high-protein diets, and tailored physical exercise—to mitigate muscle loss and improve metabolic outcomes. Future research directions should focus on validating diagnostic protocols and diagnosis techniques and further exploring specific therapies to effectively address this dual burden.
Full article
(This article belongs to the Section Obesity, Diabetes Mellitus and Metabolic Syndrome)
Open AccessReview
Remnant Cholesterol: From Pathophysiology to Clinical Implications in Type 1 Diabetes
by
Fernando Sebastian-Valles, Álvaro Montes Muñiz and Mónica Marazuela
Endocrines 2025, 6(3), 46; https://doi.org/10.3390/endocrines6030046 - 15 Sep 2025
Cited by 1
Abstract
Remnant cholesterol, contained within triglyceride-rich lipoproteins such as VLDL and IDL, has emerged as an independent risk factor for atherosclerotic cardiovascular disease (ASCVD) in both the general population and individuals with diabetes. Unlike LDL cholesterol, remnant cholesterol has not traditionally been a therapeutic
[...] Read more.
Remnant cholesterol, contained within triglyceride-rich lipoproteins such as VLDL and IDL, has emerged as an independent risk factor for atherosclerotic cardiovascular disease (ASCVD) in both the general population and individuals with diabetes. Unlike LDL cholesterol, remnant cholesterol has not traditionally been a therapeutic target, despite growing evidence of its role in the pathophysiology of atherosclerosis. These particles exhibit high atherogenic and pro-inflammatory potential, and their metabolism is altered in states of insulin resistance and hepatic dysfunction, both common in diabetes. Epidemiological studies have shown its association with ischemic heart disease, peripheral artery disease, progression of nephropathy, and cardiovascular events in type 2 diabetes. In individuals with type 1 diabetes (T1D), the evidence is more recent but relevant: elevated levels of remnant cholesterol have been linked to persistent hyperglycemia, diabetic nephropathy, diabetic foot, subclinical myocardial dysfunction, and carotid atherosclerosis, even when LDL-C levels are within target range. Moreover, lifestyle factors such as physical activity and a healthy diet are associated with lower levels of remnant cholesterol, suggesting opportunities for non-pharmacological interventions. Despite this, treatments targeting remnant cholesterol have shown limited efficacy in reducing clinical events, and individuals with T1D remain underrepresented in clinical trials. Overall, this review highlights the need to incorporate remnant cholesterol into the assessment of residual cardiovascular risk and into personalized therapeutic strategies, especially for vulnerable populations such as those with T1D.
Full article
(This article belongs to the Section Lipid Metabolism and Cardiovascular Endocrinology)
►▼
Show Figures

Figure 1
Open AccessReview
When a Sellar Mass Is Not a Pituitary Adenoma: A Literature Review and Lessons from a Case of Pituicytoma
by
Maria Petersson and Charlotte Höybye
Endocrines 2025, 6(3), 45; https://doi.org/10.3390/endocrines6030045 - 10 Sep 2025
Abstract
Background: Pituicytomas are rare, low-grade gliomas arising from pituicytes in the posterior pituitary or infundibulum. Due to its rarity and nonspecific clinical and radiological characteristics, it is frequently misdiagnosed as pituitary adenomas or other sellar tumors. Aims: To present an overview of pituicytoma,
[...] Read more.
Background: Pituicytomas are rare, low-grade gliomas arising from pituicytes in the posterior pituitary or infundibulum. Due to its rarity and nonspecific clinical and radiological characteristics, it is frequently misdiagnosed as pituitary adenomas or other sellar tumors. Aims: To present an overview of pituicytoma, including clinical presentation, radiological and histopathological characteristics, differential diagnosis and treatment strategies, illustrated by a case report. Methods: A literature review was conducted to contextualize our patient with a sellar tumor, and to highlight key diagnostic and therapeutic considerations. Results/Case report: A 12-year-old boy presented with visual disturbances. MRI revealed a well-defined contrast-enhancing sellar mass, and the patient underwent transsphenoidal surgery. The diagnosis was assumed to be a nonfunctioning pituitary adenoma (NFPA). Two years later a residual tumor was treated with proton irradiation. Six years after the radiotherapy, the patient had epistaxis. Imaging showed a tumor in the sphenoidale sinus, which was surgically resected. The tumor had histopathological features of pituicytoma and immunoreactivity for TTF-1 and S100. The tissue from the first operation was reviewed, showing more characteristics with pituicytoma than NFPA, leading to re-definition of the initial diagnosis. Follow-up has been without any signs of residual tumor. Conclusion: Our case and literature review emphasize the importance of considering pituicytoma in the differential diagnosis among sellar lesions. The diagnosis relies on a combination of preoperative imaging, intraoperative findings and histopathology. Pituitary surgery is the first-line treatment, and the outcome is generally good. Increased awareness of pituicytomas is necessary to improve preoperative diagnostic accuracy and guide appropriate management.
Full article
(This article belongs to the Section Neuroendocrinology and Pituitary Disorders)
Open AccessArticle
Novel Anthropometric Indices: An Allometric Perspective
by
Nir Y. Krakauer and Jesse C. Krakauer
Endocrines 2025, 6(3), 44; https://doi.org/10.3390/endocrines6030044 - 4 Sep 2025
Cited by 2
Abstract
Background/Objectives: Anthropometric indices based on height (H), weight (W), waist circumference (WC) and hip circumference (HC) can identify incident and future health risks. While BMI provides a standard for relative W (adjusted for H), there is no standard for indices using WC
[...] Read more.
Background/Objectives: Anthropometric indices based on height (H), weight (W), waist circumference (WC) and hip circumference (HC) can identify incident and future health risks. While BMI provides a standard for relative W (adjusted for H), there is no standard for indices using WC and HC. A body shape index (ABSI) and hip index (HI) have been proposed to extend to respectively WC and HC the same allometric power-law approach used to derive BMI to be independent of H. Here, we compared the mutually independent allometric set H, BMI, ABSI, HI with other proposed indices. Methods: We examined the formulas and rationales of published indices, and used Third National Health and Nutrition Examination Survey (NHANES III) cohort data to investigate their inter-correlations and association with mortality. Results: Many of the proposed indices are based on geometric (isometric) similarity, which does not match human body variability patterns. Unlike ABSI and HI, most proposed indices showed large correlations with BMI, complicating interpretation when considered together with BMI. Indices’ association with mortality risk were generally consistent with their correlations with BMI and ABSI. Combining the separable mortality risks associated with BMI and ABSI, even in a simplified way, outperformed any single index. Conclusions: With calls for incorporating additional indices incorporating WC and HC to supplement BMI in defining obesity, only ABSI and HI are independent of BMI. Additionally, separate risk estimates from these allometric indices can be readily combined to optimize overall risk assessment.
Full article
(This article belongs to the Special Issue Feature Papers in Endocrines 2025)
►▼
Show Figures

Figure 1
Open AccessReview
Energy Homeostasis and Kisspeptin System, Roles of Exercise and Outcomes with a Focus on Male Reproductive Health
by
Mario Ruggiero, Antonella Vicidomini, Domenico Tafuri, Filomena Mazzeo and Rosaria Meccariello
Endocrines 2025, 6(3), 43; https://doi.org/10.3390/endocrines6030043 - 28 Aug 2025
Abstract
►▼
Show Figures
Background: Obesity is a multisystemic health problem causing chronic diseases like diabetes or cardiovascular diseases, but also reproductive dysfunctions like infertility in adults or altered puberty onset in children. Exercise is a recognized intervention to control or prevent energy imbalance, thus deeply contributing
[...] Read more.
Background: Obesity is a multisystemic health problem causing chronic diseases like diabetes or cardiovascular diseases, but also reproductive dysfunctions like infertility in adults or altered puberty onset in children. Exercise is a recognized intervention to control or prevent energy imbalance, thus deeply contributing to metabolic health in physiological and pathological conditions. The kisspeptin system (KS), the main gatekeeper of reproduction and puberty onset in mammals, is also an upcoming “metabolic sensor”, linking energy homeostasis to reproductive ability both centrally and peripherally. Objectives: This narrative review aims at summarizing recent evidence from animal models and human studies on the role of the KS in energy homeostasis, with a focus on the upcoming role of the KS as a metabolic sensor able to modulate the functionality of the hypothalamus–pituitary–gonad axis in males as an adaptive response to exercise. Methods: PubMed and Scopus search (date: 2015–2025; keywords: kisspeptin and metabolism, male reproduction or exercise; kisspeptin and doping). Results and Conclusions: This review article illustrates the crucial role of the KS in linking energy homeostasis and male reproduction at the central and peripheral levels, and modulation of the KS by exercise in physiological and pathological conditions. Due to the large amount of data from animal models, knowledge gaps occur in the analysis of the relationship among KS, energy homeostasis, male reproduction and exercise in humans, particularly in the case of overtraining. Lastly, kisspeptin inclusion in the doping list is also discussed.
Full article

Figure 1
Open AccessReview
Leptin Signaling in the Hypothalamus: Cellular Insights and Therapeutic Perspectives in Obesity
by
Milen Hristov
Endocrines 2025, 6(3), 42; https://doi.org/10.3390/endocrines6030042 - 28 Aug 2025
Abstract
Leptin, an adipocyte-derived hormone, plays a central role in the regulation of energy homeostasis by acting on distinct hypothalamic nuclei. This review explores recent advances in our understanding of leptin’s region-specific actions within the arcuate nucleus, ventromedial hypothalamus, dorsomedial hypothalamus, and lateral hypothalamus,
[...] Read more.
Leptin, an adipocyte-derived hormone, plays a central role in the regulation of energy homeostasis by acting on distinct hypothalamic nuclei. This review explores recent advances in our understanding of leptin’s region-specific actions within the arcuate nucleus, ventromedial hypothalamus, dorsomedial hypothalamus, and lateral hypothalamus, highlighting their contributions to appetite regulation, energy expenditure, and neuroendocrine function. In the hypothalamic arcuate nucleus, leptin’s differential regulation of pro-opiomelanocortin and agouti-related peptide/neuropeptide Y neurons is now complemented by the identification of novel leptin-responsive neuronal populations—such as those expressing prepronociceptin, basonuclin 2, and Pirt—as well as a growing array of cellular and molecular modulators, including secreted factors like angiopoietin-like growth factor, zinc-α2-glycoprotein, and spexin, intracellular regulators such as Rap1, growth factor receptor-bound protein 10, and spliced X-box binding protein 1. In the ventromedial hypothalamus, leptin integrates with both peripheral (e.g., cholecystokinin) and central (e.g., pituitary adenylate cyclase-activating polypeptide) signals, while epigenetic mechanisms, such as those mediated by Jumonji domain-containing protein D3, regulate leptin receptor expression and sensitivity. The dorsomedial hypothalamus is increasingly recognized for coordinating leptin’s effects on metabolism, circadian rhythms, and respiration through distinct neuronal populations, including a subset of neurons co-expressing GLP-1 receptors that mediate leptin’s metabolic effects. In the lateral hypothalamus, leptin modulates reward-driven feeding via GABAergic neuronal populations—circuits that are particularly susceptible to disruption following early life trauma. Together, these insights reveal a sophisticated neurobiological framework through which leptin orchestrates systemic physiology. Understanding the heterogeneity of leptin signaling opens new avenues for restoring leptin sensitivity and developing personalized therapeutic strategies to combat obesity and related metabolic disorders.
Full article
(This article belongs to the Section Neuroendocrinology and Pituitary Disorders)
►▼
Show Figures

Figure 1
Open AccessReview
Developmental Origin and Functional Diversity of Foxp3+ Regulatory T Cells in Diabetes and Obesity
by
Acelya Yilmazer, Dimitra Maria Zevla and Karsten Kretschmer
Endocrines 2025, 6(3), 41; https://doi.org/10.3390/endocrines6030041 - 21 Aug 2025
Cited by 1
Abstract
Regulatory T (Treg) cells were first identified through the observation that Foxp3 gene mutations in mice and humans can result in their dysfunction, leading to a catastrophic multi-organ autoimmune syndrome. Since then, it has become increasingly evident that Foxp3+ Treg cells serve
[...] Read more.
Regulatory T (Treg) cells were first identified through the observation that Foxp3 gene mutations in mice and humans can result in their dysfunction, leading to a catastrophic multi-organ autoimmune syndrome. Since then, it has become increasingly evident that Foxp3+ Treg cells serve functions extending well beyond dominant tolerance and the mere prevention of autoimmune pathology. Highlighting their pivotal role in metabolic regulation, dysfunction of Treg cells has been implicated in the pathogenesis of both type 1 and type 2 diabetes. Emerging evidence further suggests that Treg cells contribute to tissue homeostasis and regeneration by facilitating repair processes, modulating immune responses to curb excessive inflammation, and supporting stem cell function in key metabolic organs such as muscle, adipose tissue, and the liver. This review aims to highlight recent progress in elucidating the functional specialization of Treg cells in the regulation of metabolic homeostasis. It explores the distinct roles of thymic and peripheral Treg cells in constraining pancreatic β-cell autoimmunity and the inflammation of metabolic organs, while also underscoring the pathogenic potential of Treg cell instability and their dedifferentiation into pathogenic effector cells. Investigating the roles of thymic and peripheral Treg cells in both forms of diabetes is a valuable endeavor, offering insight into their distinct and shared contributions to disease progression, while shedding light on immune dysregulation, metabolic inflammation, and immune–metabolic crosstalk. These insights may provide a foundation for the development of targeted therapeutic approaches directed at specific Treg cell subsets, offering the potential to attenuate disease progression or even entirely prevent its onset.
Full article
(This article belongs to the Special Issue Feature Papers in Endocrines 2025)
►▼
Show Figures

Figure 1
Open AccessReview
Gastric Autonomic Neuropathy in Diabetes
by
Elham Hosseini-Marnani, Jessica A. Marathe, James D. Triplett, Md Kamruzzaman, Kevin Yin, Karen L. Jones, Michael Horowitz and Chinmay S. Marathe
Endocrines 2025, 6(3), 40; https://doi.org/10.3390/endocrines6030040 - 19 Aug 2025
Abstract
Autonomic dysfunction of the stomach typically manifests as delayed gastric emptying or gastroparesis and is seen in individuals with both type 1 and 2 diabetes. However, impaired gastric motility is only modestly associated with the presence of upper gastrointestinal symptoms, and the diagnosis
[...] Read more.
Autonomic dysfunction of the stomach typically manifests as delayed gastric emptying or gastroparesis and is seen in individuals with both type 1 and 2 diabetes. However, impaired gastric motility is only modestly associated with the presence of upper gastrointestinal symptoms, and the diagnosis of gastroparesis essentially requires a formal measurement of gastric emptying, ideally employing a sensitive and precise technique such as scintigraphy. There is a bidirectional relationship between gastric emptying and glycemia: insulin-induced hypoglycemia accelerates, while acute elevations in blood glucose may delay gastric emptying. On the other hand, relatively more rapid emptying is associated with a higher initial rise in postprandial glucose. The management of gastroparesis requires an individualized approach, integrating dietary modifications, nutritional supplementation, pharmacological therapies, and, in severe cases, advanced interventions including gastrojejunostomy and gastric electrical stimulation. This review provides an overview of the pathophysiology and diagnosis of autonomic neuropathy of the diabetic stomach and discusses current clinical management strategies.
Full article
(This article belongs to the Section Obesity, Diabetes Mellitus and Metabolic Syndrome)
►▼
Show Figures

Figure 1
Open AccessArticle
Diagnostic Accuracy of Radiological Bone Age Methods for Assessing Skeletal Maturity in Central Precocious Puberty Girls from the Canary Islands
by
Sebastián Eustaquio Martín Pérez, Isidro Miguel Martín Pérez, Ruth Molina Suárez, Jesús María Vega González and Alfonso Miguel García Hernández
Endocrines 2025, 6(3), 39; https://doi.org/10.3390/endocrines6030039 - 5 Aug 2025
Abstract
Background: Central precocious puberty (CPP), defined as the onset of secondary sexual characteristics before age 8 in girls, is increasingly prevalent worldwide. CPP is often caused by early activation of the HPG axis, leading to accelerated growth and bone maturation. However, the diagnostic
[...] Read more.
Background: Central precocious puberty (CPP), defined as the onset of secondary sexual characteristics before age 8 in girls, is increasingly prevalent worldwide. CPP is often caused by early activation of the HPG axis, leading to accelerated growth and bone maturation. However, the diagnostic accuracy of standard bone age (BA) methods remains uncertain in this context. Objective: To compare the diagnostic accuracy of the Greulich–Pyle atlas (GPA) and Tanner–Whitehouse 3 (TW3) methods in estimating skeletal age in girls with CPP and to assess the predictive value of serum hormone levels for estimating chronological age (CA). Methods: An observational, cross-sectional diagnostic study was conducted, involving n = 109 girls aged 6–12 years with confirmed CPP (Ethics Committee approval: CHUC_2023_86; 13 July 2023). Left posteroanterior hand–wrist (PA–HW) radiographs were assessed using the GPA and TW3 methods. Anthropometric measurements were recorded, and serum concentrations of estradiol, LH, FSH, DHEA-S, cortisol, TSH, and free T4 were obtained. Comparisons between CA and BA estimates were conducted using repeated-measures ANOVA, and ANCOVA was applied to examine the hormonal predictors of CA. Results: Both GPA and TW3 overestimated CA between 7 and 12 years, with the GPA showing larger deviations (up to 4.8 months). The TW3 method provided more accurate estimations, particularly at advanced pubertal stages. Estradiol (η2p = 0.188–0.197), LH (η2p = 0.061–0.068), and FSH (η2p = 0.008–0.023) emerged as the strongest endocrine predictors of CA, significantly enhancing the explanatory power of both radiological methods. Conclusions: The TW3 method demonstrated superior diagnostic accuracy over GPA in girls with CPP, especially between 7 and 12 years. Integrating estradiol, LH, and FSH into BA assessment significantly improved the accuracy, supporting a more individualized and physiologically grounded diagnostic approach.
Full article
(This article belongs to the Section Pediatric Endocrinology and Growth Disorders)
►▼
Show Figures

Figure 1
Open AccessReview
Functional Pancreatic Neuroendocrine Neoplasms: An Overview
by
Ethan A. Mills, Beckey P. DeLucia, Colton D. Wayne, Taylor H. Jacobs, Gail E. Besner and Siddharth Narayanan
Endocrines 2025, 6(3), 38; https://doi.org/10.3390/endocrines6030038 - 1 Aug 2025
Cited by 1
Abstract
►▼
Show Figures
Pancreatic neuroendocrine neoplasms (PNENs) are a diverse group of rare tumor subtypes, representing less than 2% of all pancreatic tumors. Often detected late in the clinical course, they are associated with high rates of morbidity and mortality. Hereditary syndromes such as multiple endocrine
[...] Read more.
Pancreatic neuroendocrine neoplasms (PNENs) are a diverse group of rare tumor subtypes, representing less than 2% of all pancreatic tumors. Often detected late in the clinical course, they are associated with high rates of morbidity and mortality. Hereditary syndromes such as multiple endocrine neoplasia type-1 and von Hippel–Lindau are associated with the development of PNENs, although only a small portion of total tumors have a genetic basis. This review aims to explore the recent advances in laboratory diagnostics, imaging modalities, medical management, and surgical approaches to hormone-producing PNENs (including some common, less common, and some rare subtypes), with the goal of assisting physicians in the integration of evidence-based information into their practice.
Full article

Figure 1
Open AccessReview
Neuroendocrinological Aspects of a Tailored Hormonal Contraception
by
Christian Battipaglia, Anna Szeliga, Veronica Setti, Gregory Bala, Peter Chedraui, Alessandro D. Genazzani and Blazej Meczekalski
Endocrines 2025, 6(3), 37; https://doi.org/10.3390/endocrines6030037 - 31 Jul 2025
Cited by 1
Abstract
Hormonal contraceptives (HCs) are widely used and generally well tolerated; however, their neuroendocrinological effects remain underappreciated in clinical decision-making. Beyond ovulation suppression, HCs influence brain function by modulating key neurotransmitters such as GABA, serotonin, and dopamine, as well as neurosteroids like allopregnanolone and
[...] Read more.
Hormonal contraceptives (HCs) are widely used and generally well tolerated; however, their neuroendocrinological effects remain underappreciated in clinical decision-making. Beyond ovulation suppression, HCs influence brain function by modulating key neurotransmitters such as GABA, serotonin, and dopamine, as well as neurosteroids like allopregnanolone and β-endorphin. These interactions help explain why some users experience mood swings, anxiety, or changes in sexual desire, while others report improvements in well-being. In this narrative review, we explore how different estrogenic and progestin components affect central pathways involved in emotional regulation and cognition. Evidence suggests that estradiol or estetrol-based formulations combined with anti-androgenic progestins like drospirenone or nomegestrol acetate may offer a more favourable neuroendocrine profile, particularly in women with a history of mood disorders or hormonal sensitivity. Understanding these neuroendocrine mechanisms may support more personalized contraceptive choices, particularly in women with mood disorders and hormonal vulnerability.
Full article
(This article belongs to the Section Neuroendocrinology and Pituitary Disorders)
►▼
Show Figures

Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Biomedicines, Diagnostics, Endocrines, JCM, JPM, IJMS
Development of Diagnosis and Treatment Modalities in Obstetrics and Gynecology
Topic Editors: Osamu Hiraike, Fuminori TaniguchiDeadline: 20 March 2026

Conferences
Special Issues
Special Issue in
Endocrines
Feature Papers in Endocrines 2025
Guest Editors: Antonio Brunetti, Maria MirabelliDeadline: 20 December 2025
Special Issue in
Endocrines
Recent Advances in Type 1 Diabetes
Guest Editors: Marina Basina, Daniela FotiDeadline: 31 March 2026