Novel Anthropometric Indices: An Allometric Perspective
Abstract
1. Introduction
2. Methods
2.1. Selection of Anthropometric Indices
2.2. Units and Transformations of Indices
2.3. Correlations and Mortality Risk Associations
3. Results
3.1. Index Characteristics
3.2. Correlations Between Indices
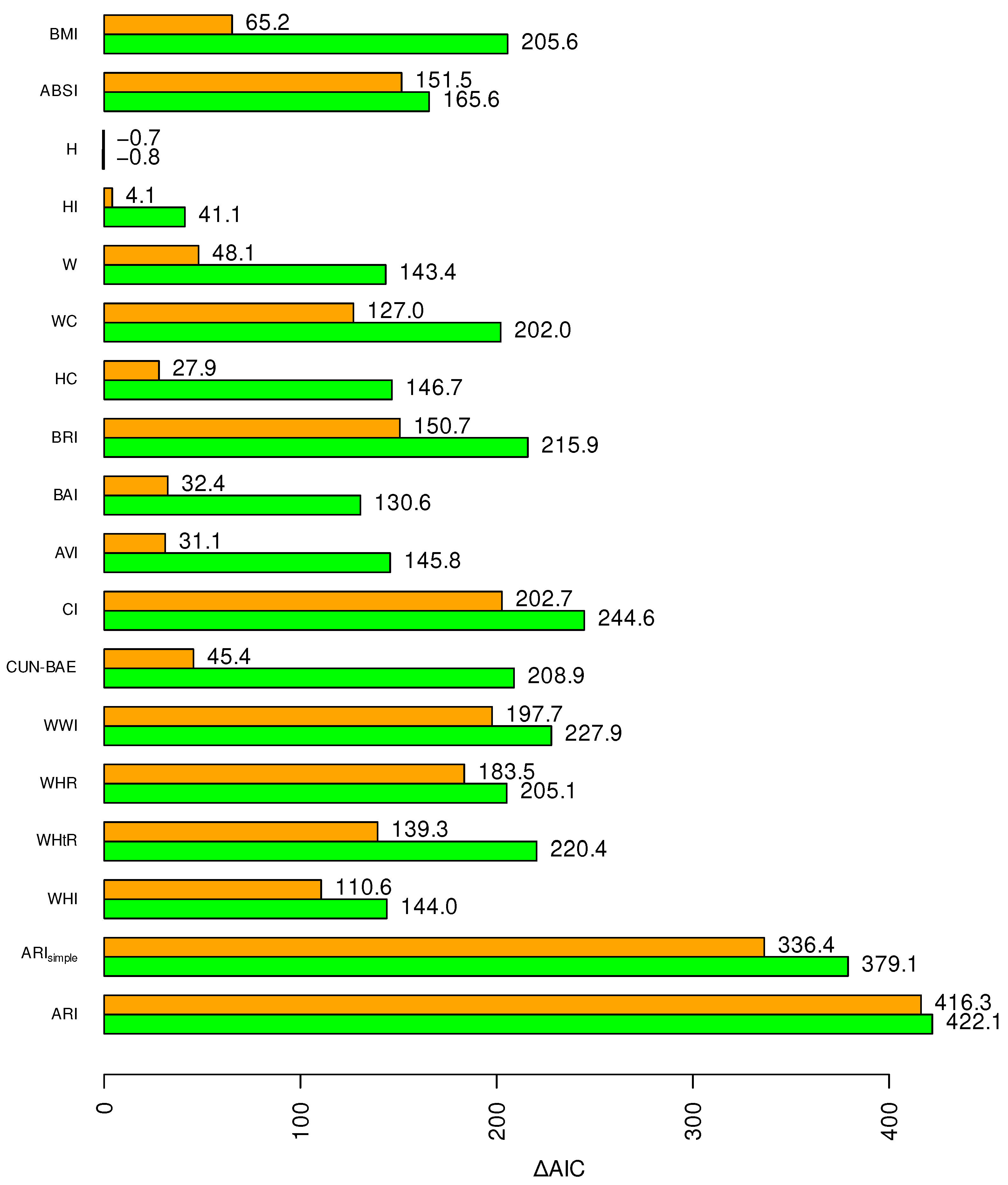
3.3. Associations with Mortality Hazard
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Correction Statement
References
- Schulz, L.O. Obese, overweight, desirable, ideal: Where to draw the line in 1986? J. Am. Diet. Assoc. 1986, 86, 1702–1704. [Google Scholar] [CrossRef]
- NHLBI. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report; Technical Report 98-4083; National Heart Lung and Blood Institute, National Institutes of Health: Bethesda, MD, USA, 1998. [Google Scholar]
- WHO. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks; Technical Report; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Flegal, K.M. Use and misuse of BMI categories. AMA J. Ethics 2023, 25, E550–E558. [Google Scholar] [CrossRef] [PubMed]
- Ashwell, M.; Cole, T.J.; Dixon, A.K. Obesity: New insight into the anthropometric classification of fat distribution shown by computed tomography. BMJ 1985, 290, 1692–1694. [Google Scholar] [CrossRef]
- Snijder, M.; van Dam, R.; Visser, M.; Seidell, J. What aspects of body fat are particularly hazardous and how do we measure them? Int. J. Epidemiol. 2006, 35, 83. [Google Scholar] [CrossRef]
- Vazquez, G.; Duval, S.; Jacobs, D.R., Jr.; Silventoinen, K. Comparison of body mass index, waist circumference, and waist/hip ratio in predicting incident diabetes: A meta-analysis. Epidemiol. Rev. 2007, 29, 115–128. [Google Scholar] [CrossRef]
- Huxley, R.; Mendis, S.; Zheleznyakov, E.; Reddy, S.; Chan, J. Body mass index, waist circumference and waist:hip ratio as predictors of cardiovascular risk–a review of the literature. Eur. J. Clin. Nutr. 2009, 64, 16. [Google Scholar] [CrossRef]
- Jayedi, A.; Soltani, S.; Zargar, M.S.; Khan, T.A.; Shab-Bidar, S. Central fatness and risk of all cause mortality: Systematic review and dose-response meta-analysis of 72 prospective cohort studies. BMJ 2020, m3324. [Google Scholar] [CrossRef]
- Ndumele, C.E.; Rangaswami, J.; Chow, S.L.; Neeland, I.J.; Tuttle, K.R.; Khan, S.S.; Coresh, J.; Mathew, R.O.; Baker-Smith, C.M.; Carnethon, M.R.; et al. Cardiovascular-kidney-metabolic health: A presidential advisory from the American Heart Association. Circulation 2023, 148, 1606–1635. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, R.; Ostrominski, J.W.; Vaduganathan, M. Prevalence of cardiovascular-kidney-metabolic syndrome atages in US adults, 2011–2020. JAMA 2024, 331, 1858. [Google Scholar] [CrossRef] [PubMed]
- Kengne, A.P.; Beulens, J.W.; Peelen, L.M.; Moons, K.G.; van der Schouw, Y.T.; Schulze, M.B.; Spijkerman, A.M.; Griffin, S.J.; Grobbee, D.E.; Palla, L.; et al. Non-invasive risk scores for prediction of type 2 diabetes (EPIC-InterAct): A validation of existing models. Lancet Diabetes Endocrinol. 2014, 2, 19–29. [Google Scholar] [CrossRef]
- Dhana, K.; Ikram, M.A.; Hofman, A.; Franco, O.H.; Kavousi, M. Anthropometric measures in cardiovascular disease prediction: Comparison of laboratory-based versus non-laboratory-based model. Heart 2015, 101, 377–383. [Google Scholar] [CrossRef]
- Krakauer, N.Y.; Krakauer, J.C. Association of x-ray absorptiometry body composition measurements with basic anthropometrics and mortality hazard. Int. J. Environ. Res. Public Health 2021, 18, 7927. [Google Scholar] [CrossRef]
- Krakauer, N.Y.; Krakauer, J.C. Expansion of waist circumference in medical literature: Potential clinical application of a body shape index. J. Obes. Weight Loss Ther. 2014, 4, 216. [Google Scholar] [CrossRef]
- Arcidiacono, B.; Chiefari, E.; Foryst-Ludwig, A.; Currò, G.; Navarra, G.; Brunetti, F.S.; Mirabelli, M.; Corigliano, D.M.; Kintscher, U.; Britti, D.; et al. Obesity-related hypoxia via miR-128 decreases insulin-receptor expression in human and mouse adipose tissue promoting systemic insulin resistance. eBioMedicine 2020, 59, 102912. [Google Scholar] [CrossRef] [PubMed]
- Mirabelli, M.; Tocci, V.; Donnici, A.; Giuliano, S.; Sarnelli, P.; Salatino, A.; Greco, M.; Puccio, L.; Chiefari, E.; Foti, D.P.; et al. Maternal preconception body mass index overtakes age as a risk factor for gestational diabetes mellitus. J. Clin. Med. 2023, 12, 2830. [Google Scholar] [CrossRef] [PubMed]
- Nevill, A.M.; Stewart, A.D.; Olds, T.; Holder, R. Relationship between adiposity and body size reveals limitations of BMI. Am. J. Phys. Anthropol. 2006, 129, 151–156. [Google Scholar] [CrossRef]
- Ahima, R.S.; Lazar, M.A. The health risk of obesity—Better metrics imperative. Science 2013, 341, 856–858. [Google Scholar] [CrossRef]
- Alser, M.; Naja, K.; Elrayess, M.A. Mechanisms of body fat distribution and gluteal-femoral fat protection against metabolic disorders. Front. Nutr. 2024, 11, 1368966. [Google Scholar] [CrossRef]
- Nilsson, G.; Hedberg, P.; Öhrvik, J. Survival of the fattest: Unexpected findings about hyperglycaemia and obesity in a population based study of 75-year-olds. BMJ Open 2011, 1, e000012. [Google Scholar] [CrossRef]
- Cepeda-Valery, B.; Pressman, G.S.; Figueredo, V.M.; Romero-Corral, A. Impact of obesity on total and cardiovascular mortality—Fat or fiction? Nat. Rev. Cardiol. 2011, 8, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; De Schutter, A.; Patel, D.A.; Romero-Corral, A.; Artham, S.M.; Milani, R.V. Body composition and survival in stable coronary heart disease. J. Am. Coll. Cardiol. 2012, 60, 1374–1380. [Google Scholar] [CrossRef] [PubMed]
- Elagizi, A.; Kachur, S.; Lavie, C.J.; Carbone, S.; Pandey, A.; Ortega, F.B.; Milani, R.V. An overview and update on obesity and the obesity paradox in cardiovascular diseases. Prog. Cardiovasc. Dis. 2018, 61, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Clark, A.L.; Fonarow, G.C.; Horwich, T.B. Waist circumference, body mass index, and survival in systolic heart failure: The obesity paradox revisited. J. Card. Fail. 2011, 17, 374–380. [Google Scholar] [CrossRef]
- Shirahama, Y.; Tabata, N.; Sakamoto, K.; Sato, R.; Yamanaga, K.; Fujisue, K.; Sueta, D.; Araki, S.; Takashio, S.; Arima, Y.; et al. Validation of the obesity paradox by body mass index and waist circumference in patients undergoing percutaneous coronary intervention. Int. J. Obes. 2022, 46, 1840–1848. [Google Scholar] [CrossRef]
- Rubino, F.; Cummings, D.E.; Eckel, R.H.; Cohen, R.V.; Wilding, J.P.H.; Brown, W.A.; Stanford, F.C.; Batterham, R.L.; Farooqi, I.S.; Farpour-Lambert, N.J.; et al. Definition and diagnostic criteria of clinical obesity. Lancet Diabetes Endocrinol. 2025, 13, 221–262. [Google Scholar] [CrossRef]
- The Lancet Diabetes & Endocrinology. Redefining obesity: Advancing care for better lives. Lancet Diabetes Endocrinol. 2025, 13, 75. [Google Scholar] [CrossRef]
- Keys, A.; Fidanza, F.; Karvonen, M.J.; Kimura, N.; Taylor, H.L. Indices of relative weight and obesity. J. Chronic Dis. 1972, 25, 329–343. [Google Scholar] [CrossRef]
- Gayon, J. History of the concept of allometry. Am. Zool. 2000, 40, 748–758. [Google Scholar] [CrossRef]
- Krakauer, N.Y.; Krakauer, J.C. A new body shape index predicts mortality hazard independently of body mass index. PLoS ONE 2012, 7, e39504. [Google Scholar] [CrossRef] [PubMed]
- Krakauer, N.Y.; Krakauer, J.C. An Anthropometric Risk Index based on combining height, weight, waist, and hip measurements. J. Obes. 2016, 2016, 8094275. [Google Scholar] [CrossRef]
- Krakauer, N.Y.; Krakauer, J.C. Untangling waist circumference and hip circumference from body mass index with a body shape index, hip index, and anthropometric risk indicator. Metab. Syndr. Relat. Disord. 2018, 16, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Krakauer, N.Y.; Krakauer, J.C. The new anthropometrics and abdominal obesity: A body shape index, hip index, and anthropometric risk index. In Nutrition in the Prevention and Treatment of Abdominal Obesity, 2nd ed.; Watson, R.R., Ed.; Academic Press: Cambridge, MA, USA, 2019; Chapter 2; pp. 19–27. [Google Scholar] [CrossRef]
- Ji, M.; Zhang, S.; An, R. Effectiveness of A Body Shape Index (ABSI) in predicting chronic diseases and mortality: A systematic review and meta-analysis. Obes. Rev. 2018, 19, 737–759. [Google Scholar] [CrossRef] [PubMed]
- Bawadi, H.; Abouwatfa, M.; Alsaeed, S.; Kerkadi, A.; Shi, Z. Body Shape Index is a stronger predictor of diabetes. Nutrients 2019, 11, 1018. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Chen, L.; Hu, W.; He, L. Association between a body shape index and subclinical carotid atherosclerosis in population free of cardiovascular and cerebrovascular diseases. J. Atheroscler. Thromb. 2021, 29, 1140–1152. [Google Scholar] [CrossRef]
- Ikeue, K.; Kusakabe, T.; Yamakage, H.; Ishii, K.; Satoh-Asahara, N. A Body Shape Index is useful for BMI-independently identifying Japanese patients with obesity at high risk of cardiovascular disease. Nutr. Metab. Cardiovasc. Dis. 2023, 34, 387–394. [Google Scholar] [CrossRef]
- Krakauer, N.Y.; Krakauer, J.C. Dynamic association of mortality hazard with body shape. PLoS ONE 2014, 9, e88793. [Google Scholar] [CrossRef]
- Kosugi, T.; Eriguchi, M.; Yoshida, H.; Tamaki, H.; Uemura, T.; Tasaki, H.; Furuyama, R.; Nishimoto, M.; Matsui, M.; Samejima, K.; et al. Association of body indices with mortality in older population: Japan Specific Health Checkups (J-SHC) Study. J. Am. Geriatr. Soc. 2024, 73, 150–161. [Google Scholar] [CrossRef]
- Shafran, I.; Krakauer, N.Y.; Krakauer, J.C.; Goshen, A.; Gerber, Y. The predictive ability of ABSI compared to BMI for mortality and frailty among older adults. Front. Nutr. 2024, 11, 5330. [Google Scholar] [CrossRef]
- Christakoudi, S.; Tsilidis, K.K.; Evangelou, E.; Riboli, E. A Body Shape Index (ABSI), hip index, and risk of cancer in the UK Biobank cohort. Cancer Med. 2021, 10, 5614–5628. [Google Scholar] [CrossRef]
- Christakoudi, S.; Riboli, E.; Evangelou, E.; Tsilidis, K.K. Associations of body shape index (ABSI) and hip index with liver, metabolic, and inflammatory biomarkers in the UK Biobank cohort. Sci. Rep. 2022, 12, 8812. [Google Scholar] [CrossRef]
- Consalvo, V.; Krakauer, J.C.; Krakauer, N.Y.; Antonio, C.; Romano, M.; Vincenzo, S. ABSI (A Body Shape Index) and ARI (Anthropometric Risk Indicator) in bariatric surgery. First application on a bariatric cohort and possible clinical use. Obes. Surg. 2018, 27, 1966–1973. [Google Scholar] [CrossRef]
- Kuang, M.; Sheng, G.; Hu, C.; Lu, S.; Peng, N.; Zou, Y. The value of combining the simple anthropometric obesity parameters, Body Mass Index (BMI) and a Body Shape Index (ABSI), to assess the risk of non-alcoholic fatty liver disease. Lipids Health Dis. 2022, 21, 104. [Google Scholar] [CrossRef]
- Hewage, N.; Wijesekara, U.; Perera, R. Determining the best method for evaluating obesity and the risk of non-communicable diseases in females of childbearing age by using the body mass index, waist circumference, waist-to-hip ratio, waist-to-height ratio, A Body Shape Index, and hip index. Nutrition 2023, 114, 112135. [Google Scholar] [CrossRef] [PubMed]
- Piqueras, P.; Ballester, A.; Durá-Gil, J.V.; Martinez-Hervas, S.; Redón, J.; Real, J.T. Anthropometric indicators as a tool for diagnosis of obesity and other health risk factors: A literature review. Front. Psychol. 2021, 12, 631179. [Google Scholar] [CrossRef] [PubMed]
- Christakoudi, S.; Evangelou, E.; Riboli, E.; Tsilidis, K.K. GWAS of allometric body-shape indices in UK Biobank identifies loci suggesting associations with morphogenesis, organogenesis, adrenal cell renewal and cancer. Sci. Rep. 2021, 11, 10688. [Google Scholar] [CrossRef] [PubMed]
- Cheung, Y.B. “A Body Shape Index” in middle-age and older Indonesian population: Scaling exponents and association with incident hypertension. PLoS ONE 2014, 9, e85421. [Google Scholar] [CrossRef]
- Dimai, H.P. Use of dual-energy X-ray absorptiometry (DXA) for diagnosis and fracture risk assessment; WHO-criteria, T- and Z-score, and reference databases. Bone 2017, 104, 39–43. [Google Scholar] [CrossRef]
- de Onis, M.; Habicht, J.P. Anthropometric reference data for international use: Recommendations from a World Health Organization Expert Committee. Am. J. Clin. Nutr. 1996, 64, 650–658. [Google Scholar] [CrossRef]
- Westat, Inc. National Health and Nutrition Examination Survey III Body Measurements (Anthropometry); Westat, Inc.: Rockville, MD, USA, 1988. [Google Scholar]
- Ezzati, T.M.; Massey, J.T.; Waksberg, J.; Chu, A.; Maurer, K.R. Sample Design: Third National Health and Nutrition Examination Survey; Vital and Health Statistics. Series 2, Data Evaluation and Methods Research 113; National Center for Health Statistics (US): Washington, DC, USA, 1992.
- Dong, B.; Peng, Y.; Wang, Z.; Adegbija, O.; Hu, J.; Ma, J.; Ma, Y.H. Joint association between body fat and its distribution with all-cause mortality: A data linkage cohort study based on NHANES (1988–2011). PLoS ONE 2018, 13, e0193368. [Google Scholar] [CrossRef]
- National Center for Health Statistics (US). Plan and Operation of the Third National Health and Nutrition Examination Survey, 1988–1994; Number 32 in Vital and Health Statistics, Series 1: Programs and Collection Procedures; National Center for Health Statistics (US): Washington, DC, USA, 1994.
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2024. [Google Scholar]
- Therneau, T.M.; Grambsch, P.M. Modeling Survival Data: Extending the Cox Model; Springer: New York, NY, USA, 2000. [Google Scholar]
- Hartz, A.J.; Rupley, D.C.; Rimm, A.A. The association of girth measurements with disease in 32,856 women. Am. J. Epidemiol. 1984, 119, 71–80. [Google Scholar] [CrossRef]
- Valdez, R. A simple model-based index of abdominal adiposity. J. Clin. Epidemiol. 1991, 44, 955–956. [Google Scholar] [CrossRef]
- Hsieh, S.D.; Yoshinaga, H. Waist/height ratio as a simple and useful predictor of coronary heart disease risk factors in women. Intern. Med. 1995, 34, 1147–1152. [Google Scholar] [CrossRef]
- Guerrero-Romero, F.; Rodr’iguez-Mor’an, M. Abdominal volume index. an anthropometry-based index for estimation of obesity is strongly related to impaired glucose tolerance and type 2 diabetes mellitus. Arch. Med Res. 2003, 34, 428–432. [Google Scholar] [CrossRef] [PubMed]
- Bergman, R.N.; Stefanovski, D.; Buchanan, T.A.; Sumner, A.E.; Reynolds, J.C.; Sebring, N.G.; Xiang, A.H.; Watanabe, R.M. A better index of body adiposity. Obesity 2011, 19, 1083–1089. [Google Scholar] [CrossRef]
- Gómez-Ambrosi, J.; Silva, C.; Galofré, J.; Escalada, J.; Santos, S.; Millán, D.; Vila, N.; Ibañez, P.; Gil, M.; Valentí, V.; et al. Body mass index classification misses subjects with increased cardiometabolic risk factors related to elevated adiposity. Int. J. Obes. 2012, 36, 286–294. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.M.; Bredlau, C.; Bosy-Westphal, A.; Mueller, M.; Shen, W.; Gallagher, D.; Maeda, Y.; McDougall, A.; Peterson, C.M.; Ravussin, E.; et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity 2013, 21, 2264–2271. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.; Kim, N.H.; Kwon, T.Y.; Kim, S.G. A novel adiposity index as an integrated predictor of cardiometabolic disease morbidity and mortality. Sci. Rep. 2018, 8, 16753. [Google Scholar] [CrossRef]
- Nevill, A.M.; Leahy, G.D.; Mayhew, J.; Sandercock, G.R.; Myers, T.; Duncan, M.J. ‘At risk’ waist-to-height ratio cut-off points recently adopted by NICE and US Department of Defense will unfairly penalize shorter adults. What is the solution? Obes. Res. Clin. Pract. 2023, 17, 1–8. [Google Scholar] [CrossRef]
- D’Agostino, R.B., Sr.; Grundy, S.; Sullivan, L.M.; Wilson, P. Validation of the Framingham Coronary Heart Disease Prediction Scores. J. Am. Med Assoc. 2001, 286, 180–187. [Google Scholar] [CrossRef]
- Wang, F.; Chen, Y.; Chang, Y.; Sun, G.; Sun, Y. New anthropometric indices or old ones: Which perform better in estimating cardiovascular risks in Chinese adults. BMC Cardiovasc. Disord. 2018, 18, 14. [Google Scholar] [CrossRef]
- Corbatón Anchuelo, A.; Martínez-Larrad, M.T.; Serrano-García, I.; Fernández Pérez, C.; Serrano-Ríos, M. Body fat anthropometric indexes: Which of those identify better high cardiovascular risk subjects? A comparative study in Spanish population. PLoS ONE 2019, 14, e0216877. [Google Scholar] [CrossRef]
- Hacıağaoğlu, N.; Öner, C.; Çetin, H.; Şimşek, E.E. Body shape index and cardiovascular risk in individuals with obesity. Cureus 2022, 14, e21259. [Google Scholar] [CrossRef]
- Green, B.B.; Anderson, M.L.; Cook, A.J.; Catz, S.; Fishman, P.A.; McClure, J.B.; Reid, R. Using body mass index data in the electronic health record to calculate cardiovascular risk. Am. J. Prev. Med. 2012, 42, 342–347. [Google Scholar] [CrossRef]
- Wang, Q.; Xu, L.; Li, J.; Sun, L.; Qin, W.; Ding, G.; Zhu, J.; Zhang, J.; Yu, Z.; Xie, S. Association of anthropometric indices of obesity with hypertension in Chinese elderly: An analysis of age and gender differences. Int. J. Environ. Res. Public Health 2018, 15, 801. [Google Scholar] [CrossRef]
- Chen, X.; Chen, X.; Shi, F.; Yu, W.; Gao, C.; Gou, S.; Fu, P. Associations between anthropometric indices and biological age acceleration in American adults: Insights from NHANES 2009–2018 data. Sci. Rep. 2025, 15, 22691. [Google Scholar] [CrossRef]
- Chung, W.; Park, J.H.; Ryu, O.H.; Yu, J.M.; Yoo, H.J.; Moon, S. Association of z-score of the log-transformed a body shape index with cardiovascular disease in people who are obese but metabolically healthy: The Korea National Health and Nutrition Examination Survey 2007–2010. J. Obes. Metab. Syndr. 2018, 27, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Parra-Soto, S.; Malcomson, F.C.; Ho, F.K.; Pell, J.P.; Sharp, L.; Mathers, J.C.; Celis-Morales, C. Associations of A Body Shape Index (ABSI) with cancer incidence, all-cause and at 23 sites- Findings from the UK Biobank prospective cohort study. Cancer Epidemiol. Biomark. Prev. 2021, 31, 315–324. [Google Scholar] [CrossRef]
- Kajikawa, M.; Maruhashi, T.; Kishimoto, S.; Yamaji, T.; Harada, T.; Saito, Y.; Mizobuchi, A.; Tanigawa, S.; Nakano, Y.; Chayama, K.; et al. A Body Shape Index as a simple anthropometric marker of abdominal obesity and risk of cardiovascular events. J. Clin. Endocrinol. Metab. 2024, 109, 3272–3281. [Google Scholar] [CrossRef] [PubMed]
- Rontogianni, M.O.; Bouras, E.; Aglago, E.K.; Freisling, H.; Murphy, N.; Cotterchio, M.; Hampe, J.; Lindblom, A.; Pai, R.K.; Pharoah, P.D.P.; et al. Allometric versus traditional body-shape indices and risk of colorectal cancer: A Mendelian randomization analysis. Int. J. Obes. 2024, 48, 709–716. [Google Scholar] [CrossRef] [PubMed]
- Sodero, G.; Rigante, D.; Pane, L.C.; Sessa, L.; Quarta, L.; Candelli, M.; Cipolla, C. Cardiometabolic risk assessment in a cohort of children and adolescents diagnosed with hyperinsulinemia. Diseases 2024, 12, 119. [Google Scholar] [CrossRef]
- Mameli, C.; Krakauer, J.C.; Krakauer, N.Y.; Bosetti, A.; Ferrari, C.M.; Schneider, L.; Borsani, B.; Arrigoni, S.; Pendezza, E.; Zuccotti, G.V. Effects of a multidisciplinary weight loss intervention in overweight and obese children and adolescents: 11 years of experience. PLoS ONE 2017, 12, e0181095. [Google Scholar] [CrossRef]
- Mameli, C.; Krakauer, N.Y.; Krakauer, J.C.; Bosetti, A.; Ferrari, C.M.; Moiana, N.; Schneider, L.; Borsani, B.; Genoni, T.; Zuccotti, G. The association between a body shape index and cardiovascular risk in overweight and obese children and adolescents. PLoS ONE 2018, 13, e0190426. [Google Scholar] [CrossRef] [PubMed]
- Todorova, S.A. Application of a body shape index as an anthropometric predictor of cardiometabolic risks in children and adolescents (systematic review). Mod. Technol. Med. 2024, 16, 1898. [Google Scholar] [CrossRef] [PubMed]
- Hansen, C.; Davison, B.; Singh, G.R. Small for gestational age and anthropometric body composition from early childhood to adulthood: The Aboriginal Birth Cohort study. Front. Public Health 2024, 12, 1349040. [Google Scholar] [CrossRef] [PubMed]

| Name | Abbreviation | Year | Citations | Formula |
|---|---|---|---|---|
| Body mass index | BMI | 1972 [29] | 730,408 | |
| Waist-to-hip ratio | WHR | 1984 [58] | 23,686 | |
| Conicity index | CI | 1991 [59] | 761 | |
| Waist-to-height ratio | WHtR | 1995 [60] | 7541 | |
| Abdominal volume index | AVI | 2003 [61] | 247 | |
| Body adiposity index | BAI | 2011 [62] | 1139 | |
| Clínica Universidad de Navarra—body adiposity estimator | CUN-BAE | 2012 [63] | 123 | |
| A body shape index | ABSI | 2012 [31] | 1269 | |
| Body roundness index | BRI | 2013 [64] | 640 | |
| Hip index | HI | 2016 [32] | 216 | |
| Weight-adjusted-waist index | WWI | 2018 [65] | 376 | |
| Waist-hip index | WHI | 2021 [48] | 109 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krakauer, N.Y.; Krakauer, J.C. Novel Anthropometric Indices: An Allometric Perspective. Endocrines 2025, 6, 44. https://doi.org/10.3390/endocrines6030044
Krakauer NY, Krakauer JC. Novel Anthropometric Indices: An Allometric Perspective. Endocrines. 2025; 6(3):44. https://doi.org/10.3390/endocrines6030044
Chicago/Turabian StyleKrakauer, Nir Y., and Jesse C. Krakauer. 2025. "Novel Anthropometric Indices: An Allometric Perspective" Endocrines 6, no. 3: 44. https://doi.org/10.3390/endocrines6030044
APA StyleKrakauer, N. Y., & Krakauer, J. C. (2025). Novel Anthropometric Indices: An Allometric Perspective. Endocrines, 6(3), 44. https://doi.org/10.3390/endocrines6030044








