-
 Psychiatric and Neuroinflammatory Profiles in Cancer Patients with and Without Type 2 Diabetes
Psychiatric and Neuroinflammatory Profiles in Cancer Patients with and Without Type 2 Diabetes -
 T Helper and Cytotoxic T Cells Play an Important Role in Acute Gastric Injury
T Helper and Cytotoxic T Cells Play an Important Role in Acute Gastric Injury -
 Diabetic Ketoacidosis in Young Adults with Type 1 Diabetes: The Impact of the Ketogenic Diet—A Narrative Literature Review
Diabetic Ketoacidosis in Young Adults with Type 1 Diabetes: The Impact of the Ketogenic Diet—A Narrative Literature Review -
 Real-World Challenges in ctDNA NGS Implementation
Real-World Challenges in ctDNA NGS Implementation
Journal Description
Diseases
Diseases
is an international, peer-reviewed, open access, multidisciplinary journal with focus on research on human diseases and conditions, published monthly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within Scopus, ESCI (Web of Science), PubMed, PMC, CAPlus / SciFinder, and other databases.
- Journal Rank: JCR - Q2 (Medicine, Research and Experimental)
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 21 days after submission; acceptance to publication is undertaken in 3.5 days (median values for papers published in this journal in the second half of 2025).
- Recognition of Reviewers: reviewers who provide timely, thorough peer-review reports receive vouchers entitling them to a discount on the APC of their next publication in any MDPI journal, in appreciation of the work done.
- Sections: published in 8 topical sections.
Impact Factor:
3.0 (2024);
5-Year Impact Factor:
3.4 (2024)
Latest Articles
Obesity and Beyond: Lifestyle Patterns and Cardiometabolic Burden in High-Risk Patients with Coronary Artery Disease—Moving Toward Personalized Prevention
Diseases 2026, 14(2), 57; https://doi.org/10.3390/diseases14020057 - 2 Feb 2026
Abstract
►
Show Figures
Background: Obesity substantially increases cardiovascular risk and contributes to the accumulation of cardiometabolic risk factors. Achieving optimal control of body weight and guideline-recommended targets is essential in high-risk patients, particularly in secondary prevention following acute coronary events. This study aimed to evaluate treatment
[...] Read more.
Background: Obesity substantially increases cardiovascular risk and contributes to the accumulation of cardiometabolic risk factors. Achieving optimal control of body weight and guideline-recommended targets is essential in high-risk patients, particularly in secondary prevention following acute coronary events. This study aimed to evaluate treatment strategies and lifestyle modifications undertaken by patients with obesity during long-term follow-up. Methods: This analysis included patients enrolled 6–18 months after acute coronary syndrome or coronary revascularization within the multicentre POLASPIRE II study. Standardized EUROASPIRE methodology was applied to collect clinical, anthropometric, and lifestyle-related data. Results: A total of 788 patients (mean age 65.4 ± 8.9 years; 25.8% women) were included, of whom 40.6% had obesity. No significant association between sex and BMI was observed (β = −0.48; 95% CI −1.30 to 0.31; p = 0.20). Increasing age was associated with lower BMI (β = −0.05; 95% CI −0.09 to −0.0001; p = 0.044), and higher education correlated with lower BMI (β = −1.10; 95% CI −2.00 to −0.22; p = 0.015). With advancing age (OR 1.02; 95% CI 1.002–1.033; p = 0.023) and increasing BMI (OR 1.11; 95% CI 1.076–1.138; p = 0.001), the number of risk factors and comorbidities increased. Higher BMI was associated with poorer control of medical risk factors (OR 1.06; 95% CI 1.03–1.10; p < 0.001), whereas patients with higher BMI demonstrated better control of lifestyle-related risk factors (OR 0.95; 95% CI 0.919–0.983; p = 0.003). Conclusions: Obesity is highly prevalent among high-risk cardiovascular patients and is associated with a greater burden of comorbidities and poorer control of medical risk factors. These findings support the need for strengthened, risk-stratified secondary prevention strategies and more personalized therapeutic approaches in patients with obesity.
Full article
Open AccessArticle
Mitochondrial Resilience in Glaucoma: Targeting NAD+ Metabolism and Oxidative Stress in Retinal Ganglion Cell Degeneration with Nicotinamide Riboside and Berberine: Preliminary Clinical Evidence
by
Federico Visalli, Francesco Cappellani, Giuseppe Gagliano, Alfonso Spinello, Alessandro Avitabile, Ludovica Cannizzaro, Matteo Capobianco, Caterina Gagliano and Marco Zeppieri
Diseases 2026, 14(2), 56; https://doi.org/10.3390/diseases14020056 - 2 Feb 2026
Abstract
►▼
Show Figures
Background: Glaucoma is a chronic neurodegenerative disorder characterized by the selective vulnerability of retinal ganglion cells (RGCs), in which mitochondrial dysfunction, redox imbalance, and impaired bioenergetic signaling play central pathogenetic roles. Mitochondrial homeostasis in RGCs critically depends on maintaining intracellular NAD+ pools,
[...] Read more.
Background: Glaucoma is a chronic neurodegenerative disorder characterized by the selective vulnerability of retinal ganglion cells (RGCs), in which mitochondrial dysfunction, redox imbalance, and impaired bioenergetic signaling play central pathogenetic roles. Mitochondrial homeostasis in RGCs critically depends on maintaining intracellular NAD+ pools, which support oxidative phosphorylation, sirtuin-mediated deacetylation, and antioxidant gene expression. Nicotinamide riboside (NR), a potent NAD+ precursor, and berberine (BBR), an AMPK activator derived from Berberis aristata, have recently emerged as synergistic modulators of mitochondrial metabolism and oxidative stress resistance. Methods: This study retrospectively assessed clinical outcomes associated with combined nutraceutical supplementation of nicotinamide riboside (NR) and berberine (BBR) in patients with primary open-angle glaucoma undergoing stable topical hypotensive therapy. We have included a narrative review in the current literature regarding NAD+ biology, AMPK–sirtuin signaling, and oxidative stress responses in retinal ganglion cell (RGC) degeneration. Due to the absence of comparator groups receiving only NR or only berberine in this retrospective cohort, the combined supplementation has been regarded as a biologically complementary strategy, and the potential for synergistic efficacy remains a subject for further investigation. Results: Translationally, a retrospective clinical cohort receiving combined NR and BBR supplementation showed functional stabilization of the visual field and structural preservation of the retinal nerve fiber layer over a six-month follow-up, in line with the proposed mitochondrial protective mechanisms. Conclusions: The clinical trends identified in this retrospective cohort have substantiated the translational significance of NR + BBR supplementation as a potential adjunctive approach in glaucoma management. NAD+ repletion and engagement of the AMPK–SIRT–NRF2 pathway may enhance mitochondrial resilience in RGCs. Collectively, these findings offer initial clinical evidence advocating for additional controlled studies on NR + berberine supplementation, while mechanistic interpretations have been derived from the existing literature and are hypothesis-generating.
Full article
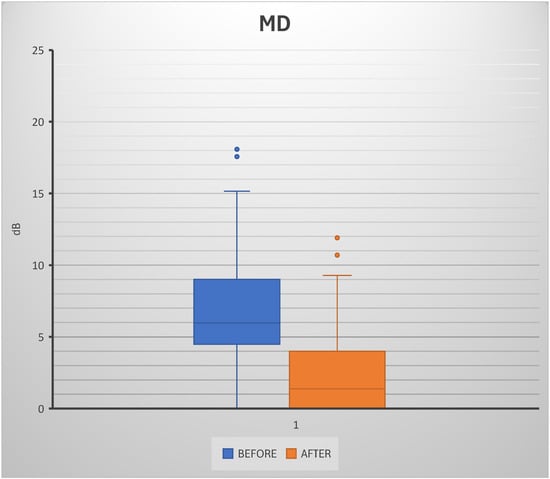
Figure 1
Open AccessArticle
Exploring Factors Associated with Adolescent Tuberculosis in India: Evidence from the National Family Health Survey (2019–21)
by
Ratnakar Singh, Adhin Bhaskar, Jagriti Gupta, Mahalingam Vasantha and Chinnaiyan Ponnuraja
Diseases 2026, 14(2), 55; https://doi.org/10.3390/diseases14020055 - 2 Feb 2026
Abstract
Background: Tuberculosis (TB) in adolescents is distinct from both childhood and adult TB, particularly in terms of risk factors; however, national-level data assessing these factors in adolescents remain limited despite growing attention to the issue. This study aims to identify factors associated with
[...] Read more.
Background: Tuberculosis (TB) in adolescents is distinct from both childhood and adult TB, particularly in terms of risk factors; however, national-level data assessing these factors in adolescents remain limited despite growing attention to the issue. This study aims to identify factors associated with TB among individuals aged 10 to 18 years. Methods: This study leverages data from the National Family Health Survey (NFHS-5) conducted in India during the year 2019–2021. A total of 479,674 adolescents were included. We employ a generalized linear mixed-effects logistic regression model to examine the association between household, environmental, demographic and behavioral factors and self-reported TB status among adolescents. Results: A total of 363 adolescents reported having TB. The results show that adolescents who are male (aOR = 0.735, p < 0.001), living in a nuclear family (aOR = 0.782, p < 0.001), residing in a household without TB cases (aOR = 0.17, p < 0.001), using a traditional mud stove or chullah (aOR = 0.279, p < 0.001), do not have air conditioning or a cooler (aOR = 0.405, p < 0.001), do not use tobacco (aOR = 0.766, p < 0.001), and do not consume alcohol (aOR = 0.912, p < 0.001) have lower odds of TB. Conversely, older age (aOR = 1.136, p < 0.001), absence of a separate kitchen (aOR = 1.395, p < 0.001), belonging to poor (aOR = 2.787, p < 0.005) or middle-income households (aOR = 2.662, p < 0.001), and living in households without cattle (aOR = 1.489, p < 0.001) are associated with higher odds of TB. Conclusions: Using nationally representative NFHS data, this study identifies multiple household, socioeconomic, and behavioral factors associated with TB among adolescents in India. These findings highlight the need for targeted TB prevention strategies that address household conditions, socio-economic disparities, and adolescent health behaviors.
Full article
(This article belongs to the Section Infectious Disease)
►▼
Show Figures

Figure 1
Open AccessArticle
Prospective Bi-Centric Real-World Outcomes of Upadacitinib in Biologic-Experienced Patients with Crohn’s Disease
by
Janina Lüke, Clara Zippel, Phil-Robin Tepasse, Frank Lenze, Markus Strauss, Arne Bokemeyer, Joost Buskermolen, Tina Schomacher, Julia Fischer, Jonel Trebicka and Richard Vollenberg
Diseases 2026, 14(2), 54; https://doi.org/10.3390/diseases14020054 - 1 Feb 2026
Abstract
►▼
Show Figures
Background: The efficacy of upadacitinib in patients with Crohn’s disease (CD) has been shown in pivotal randomized controlled trials. However, real-world data is needed to assess its effectiveness and safety in routine clinical care with biologic-experienced patients. This study aimed to evaluate the
[...] Read more.
Background: The efficacy of upadacitinib in patients with Crohn’s disease (CD) has been shown in pivotal randomized controlled trials. However, real-world data is needed to assess its effectiveness and safety in routine clinical care with biologic-experienced patients. This study aimed to evaluate the clinical and endoscopic efficacy, patient-reported outcomes (PROs), and safety of upadacitinib in biologic-experienced patients with CD in a real-world setting. Methods: This prospective bi-centric real-world study enrolled 28 anti-TNF-experienced patients with CD receiving upadacitinib 45 mg daily for 12 weeks (induction), followed by 30 mg daily maintenance through week 52. Primary endpoints included endoscopic response (≥50% SES-CD reduction or ≥2-point decrease from baseline for baseline SES-CD ≤ 4) and clinical remission (Harvey–Bradshaw Index [HBI] ≤ 4). Secondary endpoints included endoscopic remission, clinical response (HBI decrease ≥ 3 points), and quality of life (IBD-Disk). Statistical analysis used the Wilcoxon signed-rank test with 95% confidence intervals (CIs). Results: Median patient age was 37 years; 75% had ≥3 prior biologic failures. Clinical remission rates (HBI) were 59% (95% CI: 41–75%) at week 12, 44% (95% CI: 27–63%) at week 26, and 53% (95% CI: 29–76%) at week 52. Endoscopic response rates were 48% (95% CI: 44–52%) at week 26 and 46% (95% CI: 21–72%) at week 52. Endoscopic remission was achieved in 43% (95% CI: 40–48%) at week 26 and 27% (95% CI: 10–57%) at week 52. Clinical response (HBI) improved progressively from 65% at week 2 to 71% at week 52. Quality of life, as assessed by the IBD-Disk, showed significant improvement: Reduced Disease Burden (defined as a decrease of 70% or a CED-Disk Score of ≤15) was observed in 33% of patients at week 12 and 35% at week 52. Median SES-CD decreased from 9 points (IQR: 6–17) at baseline to 5 points (IQR: 1–12, p = 0.005) at week 52. Adverse events occurred in 11% of patients (4% lymphopenia, 7% skin disease), with no serious adverse events or deaths. Conclusions: Upadacitinib demonstrates significant clinical and endoscopic efficacy in biologic-experienced, anti-TNF-pretreated patients with CD, achieving remission rates comparable to or exceeding those of the pivotal trials despite a highly refractory population (75% with ≥3 prior biologic failures). The favorable safety profile supports upadacitinib as an important therapeutic option in sequential treatment of refractory CD.
Full article

Figure 1
Open AccessArticle
The Diagnostic Value of Cellular Phenotyping and Pathological Casts Using Urine Flow Cytometry in Children with Lupus Nephritis
by
Ferdy Royland Marpaung, Risky Vitria Prasetyo, Anggia Augustasia Lumban Toruan, Djoko Santoso and Aryati Aryati
Diseases 2026, 14(2), 53; https://doi.org/10.3390/diseases14020053 - 1 Feb 2026
Abstract
►▼
Show Figures
Introduction: Dysmorphic RBC (DysRBC) as a marker of glomerular abnormalities is expected to have added value in screening for glomerular abnormalities along with other examinations, including renal tubular epithelial cells (RTECs) and pathological casts (PathCasts) that indicate tubular abnormalities in lupus nephritis (LN).
[...] Read more.
Introduction: Dysmorphic RBC (DysRBC) as a marker of glomerular abnormalities is expected to have added value in screening for glomerular abnormalities along with other examinations, including renal tubular epithelial cells (RTECs) and pathological casts (PathCasts) that indicate tubular abnormalities in lupus nephritis (LN). Therefore, this study intended to assess the diagnostic performance of urinary cell and cast characteristics, including DysRBC, RTECs, and PathCast, as measured by the urine flow cytometry in lupus nephritic children. Methods: Urine samples from 317 patients (50.47% female and 49.53% male) were collected. The diagnostic value was evaluated using receiver operating characteristic (ROC) analysis. Results: The ROC analysis demonstrated that all parameters exhibited acceptable discriminatory performance, including %DysRBC (AUC = 0.954, p < 0.001), RTEC (AUC = 0.580, p = 0.001), and PathCast (AUC = 0.664, p = 0.001). Conclusions: DysRBC, RTECs, and PathCast may have added value in the diagnosis of LN in children, notably with excellent diagnostic value in distinguishing LN in %DysRBC. This promising result warrants evaluation with a large-scale site study.
Full article

Figure 1
Open AccessReview
Investigating Properties of Palmitoylethanolamide in Physiology and Disease: Far Beyond an Anti-Inflammatory Shield
by
Chiara Veredice, Ida Turrini, Helena Pelanda, Ilaria Contaldo and Donato Rigante
Diseases 2026, 14(2), 52; https://doi.org/10.3390/diseases14020052 - 31 Jan 2026
Abstract
Palmitoylethanolamide (PEA) among N-acylethanolamides displays a noteworthy impact on different inflammatory conditions and promises to become a valuable anti-inflammatory tool that does not interfere with the cyclooxygenase pathway. Mounting evidence confirms the multi-dimensional PEA-mediated crosstalk between microglia and mast cells, which would
[...] Read more.
Palmitoylethanolamide (PEA) among N-acylethanolamides displays a noteworthy impact on different inflammatory conditions and promises to become a valuable anti-inflammatory tool that does not interfere with the cyclooxygenase pathway. Mounting evidence confirms the multi-dimensional PEA-mediated crosstalk between microglia and mast cells, which would open new therapeutic opportunities targeting a neuroimmune axis and influencing both health and disease. In particular, PEA acts as a preserver of cellular homeostasis by regulating microglia cell activity and inhibiting mast cell activation in the central nervous system. The improved bioavailability and efficacy of ultramicronized formulations of PEA reflect its ultimate usefulness for different clinical applications, including significantly relieving inflammation but also reducing the pro-inflammatory burden of complex patients with either neuropathies or non-neurologic afflictions. This review aims to comprehensively delineate the therapeutic potential of PEA beyond its mere indication for acute inflammation and to highlight PEA activity as a broad-spectrum pan-tissue protective agent through the results of different preclinical and also some clinical studies. Much more remains to be learned about further PEA mechanisms of action that regulate neuroinflammation, and additional studies will have to investigate the exact role of microglia and mast cells in inflammatory diseases.
Full article
(This article belongs to the Section Neuro-psychiatric Disorders)
Open AccessReview
Reproductive Toxicity of Immune Checkpoint Inhibitors in Triple-Negative Breast Cancer: A Case Report with a Literature Review
by
Cristina Tanase-Damian, Nicoleta Zenovia Antone, Diana Loreta Paun, Ioan Tanase and Patriciu Andrei Achimaș-Cadariu
Diseases 2026, 14(2), 51; https://doi.org/10.3390/diseases14020051 - 30 Jan 2026
Abstract
►▼
Show Figures
Triple-negative breast cancer (TNBC) is an aggressive malignancy that disproportionately affects young women. The integration of immune checkpoint inhibitors (ICIs) has significantly improved outcomes in both early-stage and metastatic TNBC, shifting attention toward long-term survivorship issues, particularly endocrine function and fertility. However, the
[...] Read more.
Triple-negative breast cancer (TNBC) is an aggressive malignancy that disproportionately affects young women. The integration of immune checkpoint inhibitors (ICIs) has significantly improved outcomes in both early-stage and metastatic TNBC, shifting attention toward long-term survivorship issues, particularly endocrine function and fertility. However, the reproductive safety profile of ICIs remains insufficiently characterized. This narrative review synthesizes current preclinical and clinical evidence on ICI-associated reproductive toxicity, focusing on both direct immune-mediated gonadal injury and indirect disruption of the hypothalamic–pituitary–gonadal axis. Experimental models consistently demonstrate immune cell infiltration of ovarian and testicular tissue, cytokine-driven inflammatory cascades, follicular atresia, impaired spermatogenesis, and altered steroidogenesis following PD-1/PD-L1 and CTLA-4 blockade. Emerging clinical data report cases of immune-related orchitis, azoospermia, testosterone deficiency, diminished ovarian reserve, and premature ovarian insufficiency. Secondary hypogonadism due to immune-mediated hypophysitis represents an additional and frequently underdiagnosed mechanism. We further discuss the oncofertility challenges faced by young patients with TNBC treated with chemoimmunotherapy, emphasizing the uncertainty of fertility risk stratification and the importance of early fertility counseling and individualized fertility preservation strategies. To illustrate the potential clinical impact, we present the case of a 34-year-old nulliparous woman who developed premature ovarian insufficiency two years after neoadjuvant chemoimmunotherapy including atezolizumab, despite ovarian suppression. In conclusion, while ICIs have transformed the therapeutic landscape of TNBC, their potential long-term impact on reproductive and endocrine health represents a clinically significant concern. A precautionary, multidisciplinary oncofertility approach and prospective clinical registries are essential to define the true incidence and mechanisms of ICI-associated reproductive toxicity.
Full article

Figure 1
Open AccessReview
Decoding Leukemic Stem Cells in AML: From Identification to Targeted Eradication
by
Elisavet Apostolidou, Vasileios Georgoulis, Dimitrios Leonardos, Leonidas Benetatos, Eleni Kapsali and Eleftheria Hatzimichael
Diseases 2026, 14(2), 50; https://doi.org/10.3390/diseases14020050 - 30 Jan 2026
Abstract
Acute myeloid leukemia (AML) continues to pose significant therapeutic challenges, with high relapse rates driven largely by leukemic stem cells (LSCs), a rare, therapy-resistant population with self-renewal capacity, niche adaptation, and the ability to re-initiate disease. In this state-of-the-art review, we synthesize recent
[...] Read more.
Acute myeloid leukemia (AML) continues to pose significant therapeutic challenges, with high relapse rates driven largely by leukemic stem cells (LSCs), a rare, therapy-resistant population with self-renewal capacity, niche adaptation, and the ability to re-initiate disease. In this state-of-the-art review, we synthesize recent advances in LSC biology, addressing (i) how LSCs differ functionally and phenotypically from normal hematopoietic stem cells (HSCs), (ii) practical approaches for LSC quantification using multiparameter flow cytometry and LSC-enriched marker panels, (iii) the dysregulated signaling, metabolic and epigenetic programs that enable LSC persistence under chemotherapy and contribute to measurable residual disease, and (iv) current therapeutic strategies targeting LSC eradication, including antibody-based therapies, apoptosis and metabolic inhibitors, and emerging epigenetic agents. We also examine the key translational barriers, particularly antigen overlap with normal progenitors, microenvironmental protection, and the need for assay harmonization, while proposing a practical framework for integrating LSC assessment into risk stratification and therapeutic development.
Full article
(This article belongs to the Special Issue Advances in Molecular Pathogenesis, Precision Medicine, and Artificial Intelligence in Hematologic Malignancies)
Open AccessArticle
Seminal Interleukin-6 as a Biomarker of Inflammation, Oxidative Stress, and Sperm Dysfunction in Infertile Men
by
Loïc Koumba, Ouafaa Aniq Filali, Mariame Kabbour, Salma Ed-doumy, Mariem Norredine, Ahlam Zarhouti, Modou Mamoune Mbaye, Bouchra Ghazi, Noureddine Louanjli, Moncef Benkhalifa and Rajaa Ait Mhand
Diseases 2026, 14(2), 49; https://doi.org/10.3390/diseases14020049 - 30 Jan 2026
Abstract
►▼
Show Figures
Background/Objectives: Interleukin-6 (IL-6), a pleiotropic cytokine involved in immune regulation, is consistently detected in human semen, even in the absence of overt infection. Its contribution to sperm dysfunction, oxidative stress, and inflammation remains incompletely understood. This study evaluated the associations between seminal IL-6
[...] Read more.
Background/Objectives: Interleukin-6 (IL-6), a pleiotropic cytokine involved in immune regulation, is consistently detected in human semen, even in the absence of overt infection. Its contribution to sperm dysfunction, oxidative stress, and inflammation remains incompletely understood. This study evaluated the associations between seminal IL-6 concentrations and markers of semen quality, oxidative stress, nuclear integrity, and genital tract inflammation in infertile men. Methods: A cohort of 204 infertile men was assessed. Seminal IL-6 was quantified by electrochemiluminescence immunoassay. Semen parameters, malondialdehyde (MDA), catalase (CAT) activity, sperm DNA fragmentation index (DFI), sperm chromatin decondensation index (SDI), leukocytospermia, and bacteriospermia were measured. Analyses included correlation testing, IL-6 threshold stratification (<30, 30–60, 60–100, ≥100 pg/mL), and multivariate regression. Results: IL-6 was detectable in all samples (median: 31.52 pg/mL; range: 1.5–5000 pg/mL). Higher IL-6 levels were significantly associated with reduced sperm concentration, progressive motility, and vitality, and with increased DFI, SDI, MDA, leukocyte counts, and bacteriospermia (p < 0.001). In multivariate models, IL-6 independently predicted reduced progressive motility (β = −0.005; p = 0.032) and elevated leukocyte count (β = 0.0018; p < 0.0001). Logistic regression further showed that IL-6 increased the odds of DFI ≥ 30%, SDI ≥ 30%, and bacteriospermia (p < 0.05). Conclusions: Seminal IL-6 emerges as a sensitive biomarker of immuno-oxidative stress and sperm dysfunction in infertile men. Its integration into clinical evaluation may improve the assessment of inflammatory and oxidative contributors to male infertility.
Full article

Figure 1
Open AccessArticle
Association of IL6 Gene Polymorphisms with COVID-19 Susceptibility and Inflammation in Pregnant Women
by
Imene Ben Dhifallah, Kaouther Ayouni, Ghassen Kharroubi, Zeineb Belaiba, Majdi Ben Ameur, Henda Touzi, Walid Hammemi, Nesrine Abderahmane, Amel Sadraoui, Khaoula Magdoud, Hiba Mkadmi, Samia Kacem, Myriam Cheour, Hajer Chourou, Rim Ben Hmid, Youssef Atef, Khaled Neji, Mohamed Bedis Channoufi, Emna Barkaoui, Dalenda Chelli, Henda Triki and Mariem Gdouraadd
Show full author list
remove
Hide full author list
Diseases 2026, 14(2), 48; https://doi.org/10.3390/diseases14020048 - 30 Jan 2026
Abstract
Background/Objectives: Pregnancy is characterized by complex immunological adaptations that may increase susceptibility to infections, including SARS-CoV-2. Interleukin-6 (IL-6), a key pro-inflammatory cytokine, plays a crucial role in the immune response and has been strongly implicated in the pathogenesis of COVID-19. Genetic variations in
[...] Read more.
Background/Objectives: Pregnancy is characterized by complex immunological adaptations that may increase susceptibility to infections, including SARS-CoV-2. Interleukin-6 (IL-6), a key pro-inflammatory cytokine, plays a crucial role in the immune response and has been strongly implicated in the pathogenesis of COVID-19. Genetic variations in the IL6 gene, particularly single-nucleotide polymorphisms (SNPs) in the promoter region, can modulate IL-6 expression and potentially influence individual susceptibility to viral infections. This study aimed to evaluate the relationship between promoter region IL6 gene polymorphisms and COVID-19 susceptibility, as well as the inflammatory response, in pregnant women. Methods: We enrolled in this study 204 pregnant women with evidence of SARS-CoV-2 infection in pregnancy and 134 pregnant women with no evidence of SARS-CoV-2 infection in the past. Genotyping was conducted for the two functional SNPs in the IL6 promoter region, rs1800796 and rs1800797, via Sanger sequencing, and for associations with COVID-19 susceptibility and IL-6 levels were analyzed. Results: No significant association was found between IL6 polymorphisms and COVID-19, IL-6 levels, age, or immunization status. IL-6 levels > 5 pg/mL were more frequent in SARS-CoV-2-negative pregnant women than in SARS-CoV-2-positive pregnant women (p = 0.032). Among vaccinated participants, IL-6 levels were significantly higher in SARS-CoV-2-negative pregnant women (p = 0.044), while no difference was observed in the unvaccinated group. Conclusions:IL6 polymorphisms rs1800797 and rs1800796 were not associated with infection susceptibility or IL-6 levels. These results highlight the complex immunological interplay between pregnancy, infection, and genetic background and support the need for further research in larger cohorts.
Full article
(This article belongs to the Section Infectious Disease)
►▼
Show Figures

Figure 1
Open AccessReview
Hypertriglyceridaemia-Associated Acute Pancreatitis: Risk Stratification, Drivers, and Prevention of Recurrence
by
Federica Fogacci and Arrigo F. G. Cicero
Diseases 2026, 14(2), 47; https://doi.org/10.3390/diseases14020047 - 30 Jan 2026
Abstract
►▼
Show Figures
Hypertriglyceridaemia is the third most common aetiology of acute pancreatitis and a leading cause of recurrence in specialized lipid clinics. The risk of acute pancreatitis rises steeply once triglycerides exceed approximately 10 mmol/L (≈885 mg/dL). Still, clinically meaningful risk may occur at lower
[...] Read more.
Hypertriglyceridaemia is the third most common aetiology of acute pancreatitis and a leading cause of recurrence in specialized lipid clinics. The risk of acute pancreatitis rises steeply once triglycerides exceed approximately 10 mmol/L (≈885 mg/dL). Still, clinically meaningful risk may occur at lower levels in the presence of chylomicronaemia, metabolic stress, or pregnancy. This mini-review synthesizes contemporary evidence on epidemiology, mechanistic links between triglyceride-rich lipoproteins and pancreatic injury, and the practical distinction between secondary (acquired) and genetic drivers of severe hypertriglyceridaemia. We summarize acute management strategies aimed at rapid triglyceride reduction (including insulin-based approaches and therapeutic plasma exchange in selected scenarios) and focus on long-term prevention of recurrence through lifestyle interventions, correction of secondary contributors, and triglyceride-lowering pharmacotherapy. Finally, we discuss emerging RNA-targeted therapies against apolipoprotein C-III and angiopoietin-like 3, which are reshaping prevention strategies for familial and persistent chylomicronaemia and may reduce pancreatitis burden in the highest-risk phenotypes.
Full article

Graphical abstract
Open AccessReview
State of the Art of Systemic Therapy in HPV-Positive Oropharyngeal Squamous Cell Carcinoma: A Scoping Review
by
Fausto Petrelli, Mara Ghilardi, Agostina De Stefani, Massimiliano Nardone and Vincenzo Capriotti
Diseases 2026, 14(2), 46; https://doi.org/10.3390/diseases14020046 - 29 Jan 2026
Abstract
Objectives: To synthesize current evidence and emerging data on systemic treatment strategies for early-stage and locally advanced human papillomavirus (HPV)-positive oropharyngeal squamous cell carcinoma (OPSCC), with emphasis on treatment de-escalation and the integration of immunotherapy. Data Sources: We searched PubMed/MEDLINE, Scopus, and EMBASE
[...] Read more.
Objectives: To synthesize current evidence and emerging data on systemic treatment strategies for early-stage and locally advanced human papillomavirus (HPV)-positive oropharyngeal squamous cell carcinoma (OPSCC), with emphasis on treatment de-escalation and the integration of immunotherapy. Data Sources: We searched PubMed/MEDLINE, Scopus, and EMBASE for English-language studies published from 2010 to 2025 using terms related to HPV-positive disease, oropharyngeal carcinoma, de-escalation, chemoradiation, and immunotherapy. Review Methods: Peer-reviewed clinical trials, meta-analyses, and key translational studies addressing systemic therapy, biomarkers, and immunotherapeutic strategies in HPV-positive OPSCC were included. Emphasis was placed on phase II–III trials evaluating cisplatin-sparing regimens, cetuximab substitution, radiation dose reduction, and early-phase immunotherapy combinations. Evidence was synthesized qualitatively. Results: Cisplatin-based concurrent chemoradiation remains the standard of care for locally advanced HPV-positive OPSCC. De-intensification trials suggest that reduced-intensity regimens may be feasible in carefully selected low-risk patients; however, replacing cisplatin with cetuximab results in inferior survival. PD-1 inhibitors (e.g., pembrolizumab, nivolumab) provide durable responses in recurrent/metastatic disease and are under active evaluation in earlier stages and in combination with therapeutic vaccines, bispecific antibodies, and viral-vector platforms. Conclusions: Systemic therapy for HPV-positive OPSCC is moving toward biomarker-informed personalization. Cisplatin-based chemoradiation remains the curative backbone, while rational de-escalation and immunotherapy integration may preserve high cure rates while reducing long-term toxicity. Ongoing phase III trials will clarify which patient subsets are most suitable for de-intensified or immunotherapeutic approaches, guiding future standards of care.
Full article
Open AccessArticle
MRI-Based Bladder Cancer Staging via YOLOv11 Segmentation and Deep Learning Classification
by
Phisit Katongtung, Kanokwatt Shiangjen, Watcharaporn Cholamjiak and Krittin Naravejsakul
Diseases 2026, 14(2), 45; https://doi.org/10.3390/diseases14020045 - 28 Jan 2026
Abstract
Background: Accurate staging of bladder cancer is critical for guiding clinical management, particularly the distinction between non–muscle-invasive (T1) and muscle-invasive (T2–T4) disease. Although MRI offers superior soft-tissue contrast, image interpretation remains opera-tor-dependent and subject to inter-observer variability. This study proposes an automated deep
[...] Read more.
Background: Accurate staging of bladder cancer is critical for guiding clinical management, particularly the distinction between non–muscle-invasive (T1) and muscle-invasive (T2–T4) disease. Although MRI offers superior soft-tissue contrast, image interpretation remains opera-tor-dependent and subject to inter-observer variability. This study proposes an automated deep learning framework for MRI-based bladder cancer staging to support standardized radio-logical interpretation. Methods: A sequential AI-based pipeline was developed, integrating hybrid tumor segmentation using YOLOv11 for lesion detection and DeepLabV3 for boundary refinement, followed by three deep learning classifiers (VGG19, ResNet50, and Vision Transformer) for MRI-based stage prediction. A total of 416 T2-weighted MRI images with radiology-derived stage labels (T1–T4) were included, with data augmentation applied during training. Model performance was evaluated using accuracy, precision, recall, F1-score, and multi-class AUC. Performance un-certainty was characterized using patient-level bootstrap confidence intervals under a fixed training and evaluation pipeline. Results: All evaluated models demonstrated high and broadly comparable discriminative performance for MRI-based bladder cancer staging within the present dataset, with high point estimates of accuracy and AUC, particularly for differentiating non–muscle-invasive from muscle-invasive disease. Calibration analysis characterized the probabilistic behavior of predicted stage probabilities under the current experimental setting. Conclusions: The proposed framework demonstrates the feasibility of automated MRI-based bladder cancer staging derived from radiological reference labels and supports the potential of deep learning for stand-ardizing and reproducing MRI-based staging procedures. Rather than serving as an independent clinical decision-support system, the framework is intended as a methodological and work-flow-oriented tool for automated staging consistency. Further validation using multi-center datasets, patient-level data splitting prior to augmentation, pathology-confirmed reference stand-ards, and explainable AI techniques is required to establish generalizability and clinical relevance.
Full article
(This article belongs to the Special Issue Digital Pathology in Precision Oncology: Emerging Tools for Diagnosis and Treatment Guidance)
►▼
Show Figures

Figure 1
Open AccessArticle
CD36 rs1761667 Polymorphism and Its Impact on Molecular Signatures in Bladder Cancer
by
Mihai Ioan Pavalean, Ioana Maria Lambrescu, Gisela Gaina, Victor Lucian Madan, Mihail Eugen Hinescu and Laura Cristina Ceafalan
Diseases 2026, 14(2), 44; https://doi.org/10.3390/diseases14020044 - 28 Jan 2026
Abstract
►▼
Show Figures
Background: Bladder cancer remains a heterogeneous disease, and genetic factors are increasingly recognized as potential contributors to its pathogenesis. CD36, a multifunctional scavenger receptor implicated in lipid metabolism and tumor progression, has not been previously investigated in relation to bladder cancer-associated polymorphisms. Objectives:
[...] Read more.
Background: Bladder cancer remains a heterogeneous disease, and genetic factors are increasingly recognized as potential contributors to its pathogenesis. CD36, a multifunctional scavenger receptor implicated in lipid metabolism and tumor progression, has not been previously investigated in relation to bladder cancer-associated polymorphisms. Objectives: This study examined the relationship between the rs1761667 variant and CD36 mRNA expression. Methods: Our study included 30 patients with bladder cancer and 19 controls. PCR–RFLP genotyping for rs1761667 and RT–qPCR quantification of CD36 mRNA expression, with GAPDH as the reference gene, were performed. Expression levels were analyzed using the 2−ΔΔCt method, and statistical significance was defined as p < 0.05. Results: In patients, CD36 expression varied significantly across rs1761667 genotypes with reduced expression in AA carriers compared with GG carriers (post hoc, p = 0.009, with a Holm-adjusted p = 0.03). No significant genotype-related differences were observed among controls. Genotype distributions did not differ significantly between cases and controls (χ2, p = 0.053). Conclusions: These results indicate that rs1761667 may modulate CD36 transcription in a genotype-dependent manner, particularly in the disease context. Overall, our findings point to a potential biological connection between inherited CD36 variation and bladder cancer-related pathways, underscoring the need for further validation in tumor tissues
Full article

Figure 1
Open AccessArticle
Association Between Workday Sleep Deprivation, Weekend Catch-Up Sleep, and Abdominal Adiposity Indicators: A Cross-Sectional Study Among Brazilian Female Fixed-Shift Workers
by
Anderson Garcez, Sofia Vilela, Janaína Cristina da Silva, Ingrid Stähler Kohl, Harrison Canabarro de Arruda and Maria Teresa Anselmo Olinto
Diseases 2026, 14(2), 43; https://doi.org/10.3390/diseases14020043 - 28 Jan 2026
Abstract
►▼
Show Figures
Background: Sleep deprivation may contribute to increased abdominal adiposity. Although weekend catch-up sleep is associated with various health outcomes, its role in abdominal adiposity remains unclear, particularly among female fixed-shift workers. Therefore, this study aimed to explore the association of workday sleep deprivation
[...] Read more.
Background: Sleep deprivation may contribute to increased abdominal adiposity. Although weekend catch-up sleep is associated with various health outcomes, its role in abdominal adiposity remains unclear, particularly among female fixed-shift workers. Therefore, this study aimed to explore the association of workday sleep deprivation and weekend catch-up sleep with abdominal adiposity indicators in Brazilian female fixed-shift workers. Methods: A cross-sectional study was conducted on 450 female fixed-shift workers aged ≥ 18 years from a large industrial group in Southern Brazil. Abdominal adiposity indicators linked to cardiovascular risk were assessed: waist circumference (WC ≥ 88 cm), waist-to-height ratio (WHtR > 0.5), weight-to-waist index (WWI ≥ 11), conicity index (C-Index ≥ 1.27), and WC & Body Mass Index (combined WC ≥ 88 cm and BMI ≥ 30 kg/m2). Workday sleep deprivation was defined as <6 h (h) of sleep on workdays, and weekend catch-up sleep (absolute difference between weekend and workday sleep duration) was defined as >2 h longer sleep on weekends vs. workdays. Associations were estimated using a Poisson regression with robust variance adjusted for demographic, socioeconomic, behavioral, reproductive, and occupational confounders. Results: The mean age was 34.9 ± 9.9 years. The prevalence rates of abdominal adiposity were 45.3% for WC, 47.6% for WHtR, 26.2% for WWI and C-Index, and 28.7% for WC&BMI. Workday sleep deprivation and weekend catch-up sleep were reported by 27.1% and 43.3% of the participants, respectively. After adjustment for confounders, workday sleep deprivation was consistently associated with higher abdominal adiposity: Prevalence Ratio (PR) = 1.37 (95% CI: 1.10–1.69) for WC; 1.25 (95% CI: 1.02–1.53) for WHtR; 1.48 (95% CI: 1.07–2.04) for WWI; 1.43 (95% CI: 1.03–1.99) for C-Index, and 1.59 (95% CI: 1.17–2.16) for WC&BMI. Longer weekend catch-up sleep was positively associated with WHtR (PR = 1.24; 95% CI: 1.03–1.49) and WC&BMI (PR = 1.39; 95% CI: 1.04–1.85). Conclusions: Workday sleep deprivation was consistently linked to increased abdominal adiposity, whereas associations with longer weekend catch-up sleep were less consistent. These findings underscore the potential metabolic risk of insufficient sleep among female shift workers.
Full article

Figure 1
Open AccessReview
Microbiota Transplantation as a Future Novel Therapeutic Strategy Approach
by
Suresh Kumar, Himanshu, Pratibha Gaur, Saheem Ahmad, Paridhi Puri, V. Samuel Raj and Ramendra Pati Pandey
Diseases 2026, 14(2), 42; https://doi.org/10.3390/diseases14020042 - 28 Jan 2026
Abstract
►▼
Show Figures
Bacterial vaginosis (BV) is a leading cause of genital discomfort among women globally, and it arises from dysbiosis of the vaginal ecosystem characterized by the overgrowth of pathogenic bacteria. Current therapeutic strategies primarily rely on antibiotics and/or probiotics, which demonstrate clinical efficacy but
[...] Read more.
Bacterial vaginosis (BV) is a leading cause of genital discomfort among women globally, and it arises from dysbiosis of the vaginal ecosystem characterized by the overgrowth of pathogenic bacteria. Current therapeutic strategies primarily rely on antibiotics and/or probiotics, which demonstrate clinical efficacy but are frequently associated with limitations such as antimicrobial resistance, high recurrence rates, and incomplete restoration of a healthy vaginal microbiota. Inspired by the success of fecal microbiota transplantation in gastrointestinal disorders, vaginal microbiome transplantation (VMT) from healthy donors has emerged as a potential alternative therapeutic approach for BV. However, experimental and early clinical studies indicate that VMT efficacy is not uniform across individuals, with considerable inter-individual variability in treatment outcomes. Host genetic factors, baseline vaginal microbial composition, immune status, and environmental influences are likely to modulate therapeutic success, underscoring the need for personalized interventions. This article critically evaluates the shortcomings of existing standardized treatments, highlights the potential advantages and challenges of VMT, and discusses emerging, precision-based therapeutic strategies for BV in light of recent research advances and ongoing clinical trials worldwide.
Full article

Figure 1
Open AccessArticle
Lipoprotein(a) Concentration and Achieving Target Values of Low-Density Lipoprotein Cholesterol Calculated by Different Equations
by
Olga I. Afanasieva, Alexandra V. Tyurina, Elena A. Klesareva, Marat V. Ezhov and Sergei N. Pokrovsky
Diseases 2026, 14(2), 41; https://doi.org/10.3390/diseases14020041 - 27 Jan 2026
Abstract
Background: Low-density lipoprotein cholesterol (LDL-C) is a major cardiovascular risk factor and an indicator of hypolipidemic therapy effectiveness. However, direct and calculated methods for determining “LDL-C” present the sum of the cholesterol in all apoB-containing lipoproteins, including lipoprotein(a) [Lp(a)]. There has been an
[...] Read more.
Background: Low-density lipoprotein cholesterol (LDL-C) is a major cardiovascular risk factor and an indicator of hypolipidemic therapy effectiveness. However, direct and calculated methods for determining “LDL-C” present the sum of the cholesterol in all apoB-containing lipoproteins, including lipoprotein(a) [Lp(a)]. There has been an ongoing debate about the correctness of LDL-C in patients with elevated Lp(a) concentrations up to now. The aim of this study was to evaluate the effect of Lp(a) concentration on the LDL-C calculated by different equations. Methods: The study included the results of fasting lipids and Lp(a) concentration of 566 measurements from 283 patients (before and after lipid-lowering therapy prescribing, after exclusion of 17 patients with incomplete data). LDL-C and LDL-C corrected for Lp(a)-cholesterol (LDL-Ccorr) were calculated by Friedewald, Martin–Hopkins, and Sampson equations. Results: We assessed 566 measurements of lipids and Lp(a). The number of values reclassified to a higher risk category was 10% and 13% with Martin–Hopkins and Sampson equations compared to the Friedewald formula. The percentage of Lp(a)-cholesterol (Lp(a)-C) in the LDL-C calculated by three formulas was up to 90% or more depending on the concentration of LDL-C and Lp(a). When stratified by clinically significant LDL-C thresholds, the proportion of values LDL-Ccorr reclassified to a lower risk category ranged from 30 to 59%. Conclusion: Comparison of LDL-C concentrations calculated by Friedewald, Martin–Hopkins, and Sampson equations showed high consistency in patients without elevated triglycerides. The LDLcorr is reasonable to use in patients with Lp(a) concentration ≥ 30 and ≥41 mg/dL when using the Martin–Hopkins and Sampson equations, respectively. These data may help clinicians interpret LDL-C goal attainment in patients with elevated Lp(a) and avoid misclassification driven by the Lp(a)-cholesterol component.
Full article
(This article belongs to the Section Cardiology)
►▼
Show Figures

Figure 1
Open AccessArticle
Colorectal Cancer in Brazil: Regional Disparities and Temporal Trends in Diagnosis and Treatment, 2013–2024
by
Luiz Vinicius de Alcantara Sousa, Jean Henri Maselli-Schoueri, Laércio da Silva Paiva and Bianca Alves Vieira Bianco
Diseases 2026, 14(2), 40; https://doi.org/10.3390/diseases14020040 - 26 Jan 2026
Abstract
►▼
Show Figures
Background/Objectives: Colorectal cancer (CRC) is a major public health challenge in Brazil, characterized by marked regional disparities. Although national legislation mandates that treatment begin within 60 days after diagnosis, compliance remains inconsistent, particularly within the Unified Health System (SUS). This study aimed to
[...] Read more.
Background/Objectives: Colorectal cancer (CRC) is a major public health challenge in Brazil, characterized by marked regional disparities. Although national legislation mandates that treatment begin within 60 days after diagnosis, compliance remains inconsistent, particularly within the Unified Health System (SUS). This study aimed to analyze the time to treatment initiation for colon (C18) and rectal (C20) cancer in Brazil from 2013 to 2024, assessing regional inequalities, temporal trends, and factors associated with treatment delays. Methods: We conducted an ecological study using secondary data from the Ministry of Health’s PAINEL-Oncologia platform, which integrates information from SIA/SUS, SIH/SUS, and SISCAN. Records of patients diagnosed with colon and rectal cancer (ICD-10 C18–C20) were evaluated. Temporal trends were analyzed using Joinpoint regression, and factors associated with delayed treatment initiation (>60 days) were identified through multiple logistic regression models. Results: Persistent discrepancies were observed between diagnostic and treatment trends from 2013 to 2024, with the Annual Percent Change (APC) for diagnosis exceeding that for treatment, particularly among adults aged 55–69 years. The Southeast and South regions accounted for over 70% of all diagnosed cases, starkly contrasting with the less than 25% in the North and Northeast. More than 50% of patients across all clinical stages initiated treatment after the legally mandated 60-day period. Women with rectal cancer had a 28% higher risk (RR = 1.28) of being diagnosed at stage IV. Chemotherapy was the predominant initial therapeutic modality, while the need for combined chemo-radiotherapy was associated with markedly elevated risk ratios for delay (e.g., RR = 26.53 for stage IV rectal cancer). Treatment initiation delays (>60 days) were significantly associated with residence in the North/Northeast regions, female sex (for rectal cancer), advanced-stage disease, and complex therapeutic regimens. Conclusions: The study demonstrates persistent regional inequalities and highlights a substantial mismatch between diagnostic capacity and therapeutic availability in Brazil. These gaps contribute to treatment delays and reinforce the need to strengthen and expand oncological care networks to ensure equitable access and improve outcomes, particularly in underserved regions.
Full article

Figure 1
Open AccessSystematic Review
Efficacy of Phytotherapy for Cancer-Related Fatigue: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
by
Silvio Matsas, Ursula Medeiros Araujo de Matos, Carolina Molina Llata and Auro del Giglio
Diseases 2026, 14(2), 39; https://doi.org/10.3390/diseases14020039 - 26 Jan 2026
Abstract
►▼
Show Figures
Background: Cancer-related fatigue (CRF) is one of the most common and burdensome symptoms faced by patients with cancer, yet effective drug-based treatments remain limited. In recent years, phytotherapeutic agents have drawn attention as complementary options, supported by plausible anti-inflammatory, antioxidant, and immunomodulatory mechanisms.
[...] Read more.
Background: Cancer-related fatigue (CRF) is one of the most common and burdensome symptoms faced by patients with cancer, yet effective drug-based treatments remain limited. In recent years, phytotherapeutic agents have drawn attention as complementary options, supported by plausible anti-inflammatory, antioxidant, and immunomodulatory mechanisms. Methods: We performed a systematic review and meta-analysis to quantitatively synthesize randomized controlled trial evidence on the efficacy of phytotherapeutic interventions for cancer-related fatigue and to assess the certainty of evidence. Databases were searched from inception, with the final search update completed in October 2025. Eligible studies included adults with CRF and compared herbal interventions with placebo controls. Standardized mean differences (SMDs) were pooled using a DerSimonian–Laird random-effects model. We also evaluated risk of bias (RoB 2), publication bias, and certainty of evidence using GRADE. This systematic review and meta-analysis was conducted in accordance with the PRISMA 2020 guidelines. Results: Fourteen trials were included, studying agents such as Paullinia cupana, Panax ginseng, multi-herbal Traditional Chinese Medicine formulations, and other botanical extracts. Overall, phytotherapy provided a modest improvement in CRF (SMD = 0.31; 95% CI, 0.08–0.53; p = 0.022), though heterogeneity was substantial (I2 = 56.7%). In subgroup analyses, only the group of “other formulations” demonstrated significant benefit; ginseng and guaraná did not demonstrate statistically significant effects. Most trials had high or unclear risk of bias, and the certainty of evidence was rated very low. Conclusions: Current evidence does not firmly support phytotherapeutic agents as effective treatments for CRF, hindered largely by methodological weaknesses, heterogeneous interventions, and imprecise effect estimates. Even so, the biological rationale and the variability in clinical responses point toward an opportunity for the emerging field of precision herbal oncology. Well-designed, multicenter trials are essential to determine whether phytotherapy can meaningfully contribute to CRF management.
Full article

Figure 1
Open AccessArticle
Comparative Analysis of Oral Microbiome in Indian Type 2 Diabetes Mellitus (T2DM) and Periodontitis Cohorts
by
Meenakshi Murmu, Rajshri Singh, Rajesh Gaikwad, Akshaya Banodkar, Sagar Barage, Preethi Sudhakara and Aruni Wilson Santhosh Kumar
Diseases 2026, 14(2), 38; https://doi.org/10.3390/diseases14020038 - 23 Jan 2026
Abstract
►▼
Show Figures
Background: Type 2 diabetes mellitus (T2DM) and periodontitis are highly prevalent immune-inflammatory diseases that interact bidirectionally. However, how early-onset T2DM, periodontitis, and adverse lifestyle behaviors collectively remodel the gingival plaque microbiome at the ecological network level remains poorly understood in Indian populations. Methods:
[...] Read more.
Background: Type 2 diabetes mellitus (T2DM) and periodontitis are highly prevalent immune-inflammatory diseases that interact bidirectionally. However, how early-onset T2DM, periodontitis, and adverse lifestyle behaviors collectively remodel the gingival plaque microbiome at the ecological network level remains poorly understood in Indian populations. Methods: A cross-sectional 16S rRNA gene (V3–V4) sequencing study was conducted on supragingival and subgingival plaque from 60 adults (30–40 years) recruited in Mumbai. Participants were categorized as healthy (H, n = 10), periodontitis (P, n = 10), T2DM (n = 20), and T2DM with periodontitis (T2DM_P, n = 20). Comprehensive demographic, anthropometric, metabolic, periodontal, dietary, lifestyle, and oral hygiene data were collected. Sequence data were processed using QIIME2–DADA2, followed by diversity, differential abundance, and genus-level co-occurrence network analyses (Spearman |r| ≥ 0.6, FDR < 0.05; core prevalence ≥ 70%). Results: α-diversity showed no marked depletion across groups, whereas Bray–Curtis β-diversity revealed significant global separation, with maximal dissimilarity between H and T2DM_P. Healthy individuals with favorable lifestyle behaviors harbored scaffold-forming taxa such as Corynebacterium matruchotii, Lautropia mirabilis, and Capnocytophaga spp. In contrast, P and T2DM_P groups showed enrichment of proteolytic, inflammation-adapted genera including Porphyromonas, Tannerella, Treponema, Fretibacterium, Peptostreptococcus, and Selenomonas. Network analysis revealed a shift from commensal-rich modular networks to densely connected, keystone-centered disease modules. Conclusion: Early-onset T2DM and periodontitis, particularly under adverse lifestyle behaviors, reorganize plaque microbial composition and interaction architecture rather than depleting diversity, highlighting plaque-based keystone taxa and networks as targets for microbiome-informed risk stratification and integrated medical–dental–lifestyle interventions.
Full article

Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
9 December 2025
Meet Us at the 146th Annual Meeting of the Pharmaceutical Society of Japan (Osaka), 26–29 March 2026, Osaka, Japan
Meet Us at the 146th Annual Meeting of the Pharmaceutical Society of Japan (Osaka), 26–29 March 2026, Osaka, Japan

6 November 2025
MDPI Launches the Michele Parrinello Award for Pioneering Contributions in Computational Physical Science
MDPI Launches the Michele Parrinello Award for Pioneering Contributions in Computational Physical Science
Topics
Topic in
Cancers, Diagnostics, Diseases, IJMS, JPM
Advances in Genetics and Precision Medicine in Human Diseases: 2nd Edition
Topic Editors: Shun-Fa Yang, Shih-Chi SuDeadline: 14 November 2026
Topic in
Biomedicines, Diseases, JCM, JPM, Uro, Reports
Clinical, Translational, and Basic Research and Novel Therapy on Functional Bladder Diseases and Lower Urinary Tract Dysfunctions
Topic Editors: Hann-Chorng Kuo, Yao-Chi Chuang, Chun-Hou LiaoDeadline: 31 December 2026
Topic in
Dietetics, Diseases, Foods, Nutrients, JCM
Environmental Influences on Dietary Patterns and Disease Risk: Nutritional Pathways and Health Implications
Topic Editors: Yuquan Chen, Guanhu YangDeadline: 1 February 2027
Topic in
Life, Biomedicines, JCRM, Diseases, Emergency Care and Medicine, Anesthesia Research
Electrolytes and Acid-Base Disturbances: Advances in Pathophysiology and Treatment
Topic Editors: Caterina Carollo, Giuseppe MulèDeadline: 30 March 2027

Conferences
Special Issues
Special Issue in
Diseases
Gastric Cancer: New Trends in Endoscopic Diagnosis Staging and Treatment
Guest Editors: Germana de Nucci, Gianpiero ManesDeadline: 1 March 2026
Special Issue in
Diseases
Insights into the Management of Cardiovascular Disease Risk Factors
Guest Editors: Paweł Muszyński, Anna Tomaszuk-KazberukDeadline: 31 March 2026
Special Issue in
Diseases
Frailty and Frequent Hospitalizations in Older Adults: Risk, Management, and Interventions
Guest Editors: Francesco Ragusa, Nicola VeroneseDeadline: 31 March 2026
Special Issue in
Diseases
Dietary Effects on Health Status in South-East Asia Population
Guest Editor: Ciro Gargiulo IsaccoDeadline: 31 March 2026
Topical Collections
Topical Collection in
Diseases
Lysosomal Storage Diseases
Collection Editors: Jose Sanchez-Alcazar, Luis Jiménez Jiménez








