Abstract
Introduction: Nursing students establish therapeutic relationships with their patients and as future nursing professionals, they should be trained to be effective communicators. The objective of this systematic review was to know the impact of educational interventions on nursing students to develop their communication skills with patients. Methods: A systematic review of literature was carried out. The following databases were consulted: CINAHL, PubMed (Ovid Medline), SCOPUS and Web of Science. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses guided this review. As for inclusion criteria, published articles in English from 2000 to 2020 were included. The methodological rigor of the included articles was evaluated with the JBI Critical Appraisal Checklist for Randomized Controlled Trial or Quasi-Experimental Studies. Changes in communication skills with the patient after the implementation of an intervention were analyzed. Results: Of the included studies in this systematic review (N = 19), two studies were randomized controlled trials, others were single group quasi-experimental studies (N = 11) and two group quasi-experimental studies (n = 6). The majority of the studies were carried out in the USA (n = 7). The most frequent educational intervention was simulation (n = 11). As for the improvement of communication skills, 13 of the 19 articles found statistically significant differences in patient-centered communication skills of nursing students. Conclusions: This systematic review provides preliminary evidence of the effectiveness of interventions used to train nursing students in patient-centered communication. Although all the interventions obtained significant results in communication skills, it has not yet been determined which methodology is more effective.
1. Introduction
Therapeutic communication (TC) is defined as the process of using verbal and nonverbal communication to connect with patients [1]. TC is holistic, patient-centered and involves aspects of the physiological, psychological, environmental and spiritual care of the patient [2]. It is based on understanding and addressing the patient’s situation, including life circumstances, beliefs, perspectives, relevant concerns and needs in order to plan adequate patient care [3,4]. TC between the nurse and patient is considered one of the most significant clinical methods of communication and the basis of nursing care [5].
The TC that nurses establish with their patients has been explored in various clinical areas. In particular, with psychiatric patients, it has shown improved health outcomes and decreased clinical anxiety and depression [6]. In the case of chronically ill patients, it has contributed to an increase in adherence to treatment [7], and therefore, an improvement in the self-management of their disease [8]. Additionally, in palliative care, communication skills are essential to provide the patient with effective symptom management, psychosocial and spiritual support and advance care planning [9].
A nurse’s ability to communicate in an effective way is essential for developing therapeutic relationships with their patients and obtain greater patient satisfaction. It also minimizes treatment errors and improves the quality of nursing care [10,11]. Patients and their caregivers positively value professionals who attentively listen, the depth of conversation, the moment of delivering information and communicating in an empathetic way [12]. However, various studies have shown that nurses lack communication skills due to inadequate training or a failure to appreciate the importance of patient-centered communication [7,13]. For this reason, nursing professors must find active and effective ways to foster communication skills in the education of nursing students [14].
Teaching and training how to effectively communicate can be complicated due to the variety of potentially difficult conversations that nursing students may face in clinical settings [15]. This situation constitutes a challenge for university professors in charge of educating nursing students [15,16]. Nursing students establish therapeutic relationships with their patients, and as future nursing professionals, they should be trained to be effective communicators [17]. Therefore, the concept of TC should be emphasized in the nursing curriculum to meet the educational needs of the students, as well as the needs of the patients [18,19,20]. However, most interventions aimed at improving patient-centered communication have been for doctors [21,22]. Given the above, the question was posed as to whether nursing students that receive educational interventions could improve their communication skills with patients. Therefore, the objective of this systematic review was to know the impact of educational interventions on nursing students to develop their communication skills with patients.
2. Method
2.1. Search Strategy
A systematic review was carried out from September 2019 to January 2020. For this purpose, a critical evaluation of all related evidence was conducted, following a widely documented methodology, in order to answer the specific research question [23]. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist was used as a guide for the search and presentation of the results [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46].
An initial search was conducted to obtain information on the breadth of publications and identify the words contained in the titles and abstracts on Google Scholar. A search was then made in the PubMed database (see Box 1) through the US National Library of Medicine in order to identify the Medical Subjects Headings (MeSH). However, the term MeSH ‘therapeutic communication’ and similar terms found were not linked to any educational subgroup in the search tree. Subsequently, a systematic search was performed using all the keywords identified in the following databases: CINAHL, PubMed (Ovid Medline), SCOPUS and Web of Science.
Box 1. Example of search strategy conducted in PubMed.
(((((((("students, nursing"[MeSH Terms] AND prelicensure[Title/Abstract]) OR undergraduate[Title/Abstract]) AND intervention[Title/Abstract]) OR effectiveness[Title/Abstract]) AND therapeutic communication[Title/Abstract]) OR nurse-patient communication[Title/Abstract]) OR patient-centered communication[Title/Abstract]) OR interpersonal communication[Title/Abstract]) AND English[Language]
A systematic strategy was used derived from the terms ‘nursing students’ (population); ‘education’ or ‘teaching’ and ‘therapeutic communication’ (intervention); ‘undergraduate’ or ‘prelicensure’ or ‘university’ (context); and ‘effectiveness’ or ‘impact’ (outcome). Finally, manual searches were conducted in the references lists of recent studies and reviews in search of eligible articles that could have been previously lost.
As for inclusion criteria, the review included quantitative studies whose design were Randomized Clinical Trials (RCT) and quasi-experimental trials published in English from January 2000 to January 2020. Regarding the participants, studies were included with participants that were undergraduate (or pre-licensure) nursing students, regardless of their age, sex or country of origin. With respect to the types of intervention, the review included studies of TC training or patient-centered training. In regards to the types of measured results, the review considered any objectively measured or self-reported quantitative data reporting on therapeutic communication outcomes.
2.2. Data extraction
A total of 5,845 articles were identified in the initial search. All citations and abstracts identified in the search strategy were downloaded to Mendeley. The first author (LG) assessed the titles of the articles obtained from the search in the databases. The search yielded 612 articles after eliminating duplicates (see the systematic review flow diagram in Figure 1). The abstracts were reviewed and studies were excluded if: (a) the intervention was not aimed at TC or patient-centered; (b) if the intervention was not aimed at nursing students; (c) articles that were systematic reviews, meta-analysis, qualitative studies, case studies, doctoral thesis or conference abstracts; (d) articles not written in English. Of the 86 abstracts reviewed, 27 articles were selected by the first author for revision of the full text. From the manual search, 10 relevant articles were identified for inclusion in the review. Both reviewers independently analyzed the 27 articles taking the preestablished criteria into account.
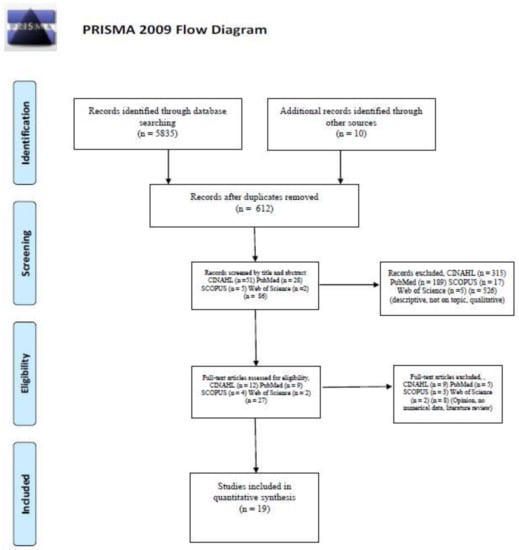
Figure 1.
Systematic review flow diagram.
Data from the included articles were reviewed by two independent reviewers (LG and VM), using the JBI-MAStARI data extraction tool. The reviewers extracted information from each of the articles including data on design, theoretical framework, participants, intervention, outcome measures and results. The most relevant characteristics of the studies included in the review are summarized in Table 1. Due to variations in the intervention methods and outcome measures, it was not possible to carry out a meta-analysis.

Table 1.
Main characteristics of the selected studies.
2.3. Quality appraisal
The selected articles were independently evaluated by two reviewers (GA and VG), before being included in this review. The methodological validity was evaluated using the Joanna Briggs Institute Meta-Analysis of Statistics Assessment and Review Instrument standardized critical appraisal instrument (JBI MAStARI). For the RCTs, the JBI MAStARI for RCTs was used. This checklist is made up of thirteen items. The possible answers to the items are yes, no, unclear or not applicable. If “yes” is answered, a point is obtained. For the study to be included, it had to obtain a score equal to or greater than seven. In the quasi-experimental studies, JBI MASTARI for quasi-experimental studies was used. This checklist is made up of nine items that can be rated yes, no, unclear or not applicable. If “yes” is chosen for the item, a point is obtained. For the study to be included in the systematic review, it had to obtain a score equal to or greater than five. This process enabled an increase in methodological rigor and evaluated possible biases and threats to the validity [25]. The discrepancies between the reviewers of the articles that were to be included in the review were discussed until a consensus was reached. After review, evaluation and discussion, eight articles were excluded that were not based on TC interventions, as defined in the inclusion criteria, or for methodological reasons. Finally, 19 articles were included after confirmation by both reviewers.
3. Results
3.1. Characteristics of the study
The overall sample size of the studies included in this review was N = 1,295 participants. In the included studies, there was a great deal of variation in the sample size, ranging from 26 to 147 (median, n = 62). Although the literature search was conducted from the year 2000, the first study included in this review was from 2006. Ninety percent of the studies (n = 18) were carried out in the last ten years and more than fifty percent (n = 10) were conducted in the last five years. Most studies (n = 9) were in mental health. The other areas represented were end-of-life and maternity. As for the study designs, the majority were quasi-experimental studies (n = 17) followed by RCTs (n = 2). In all of the included studies, pre-test and post-test measurements were performed (N = 19) (Table 1).
3.2. Theoretical frameworks
Only two of the 19 studies included in this systematic review included a description of a theoretical framework. Donova and Mullen [26] used the Constructivist Learning Theory by Merriam, Cafferella and Baumgartner [27]. While Shorey et al. [28] used a combination of the two frameworks (a) the Self-Efficacy Theory [29]; and (b) the Authentic Learning Concept [30].
3.3. Intervention characteristics
Eleven studies used simulation as the intervention. The majority of them (n = 8) used SP to facilitate learning [26,31,32,33,34,35,36,37] and three studies used simulation to aid in the assessment of communication skills, performed by a faculty member [38], peer [39], or both [40]. Nine were carried out through simulation using Standardized Patients (SP) [26,31,32,33,36,37,38,40]. One study used simulation through role playing [39] and with high-fidelity patient (n = 1) [34]. Three studies used innovative educational methodologies, such as a blended learning environment [28], cooperative learning methods [41], and Case-Based learning [42]. Five studies focused their intervention on the development of courses [43,44,45,46,47], and four of the courses indicated the included activities.
Regarding the contexts of the interventions, nine studies focused on mental health [26,31,33,35,36,37,38,39,40], three studies on end-of-life [32,43,47], one focused on maternity [34], and six studies focused on general patient-centered communication skills [28,41,42,44,45,46]. As for the duration of the interventions, it varied from one hour to one semester (Table 2).

Table 2.
Intervention characteristics.
3.4. Outcome measures
The included studies reported 19 different instruments of patient-centered communication. Most of the studies provided data on the reliability and validity of the instruments, either in previous studies or calculated for the study they carried out. However, several authors designed the instruments themselves to evaluate interpersonal communication. For six instruments, no validity data was provided [31,32,33,36,38,39].
3.5. Intervention impact on outcomes
Of the articles included in the review, thirteen determined a statistically significant improvement in the results. More than fifty percent (n = 11) of the studies used simulation as part of the training of patient-centered communication skills. Several studies that used simulation found no statistically significant differences between the groups [33,35,37]. However, they did determine an improvement in the patient-centered communication skills of the intervention group (IG) with respect to the control group (CG) [33,35,37] (see Table 3).

Table 3.
Main results and conclusions.
3.6. Quality assessment
Based on JBI criteria for the effectiveness of experimental designs, the two RCTs included were evaluated at level 1C (See Table 1). The quasi-experimental studies (n = 6) with two groups reported a level of evidence of 2C and the experimental studies with a single group (n = 11) reported evidence at level 2D for effectiveness, according to the criteria of evidence levels of JBI [25] (Table 4 and Table 5).

Table 4.
Results of critical appraisal for quasi-experimental studies.

Table 5.
Results of critical appraisal for Randomized Controlled Trials.
4. Discussion
This systematic review provides an overview of the research carried out on nursing students in order to develop communication skills with the patient. The objective of this systematic review was to identify, critically evaluate and synthesize the evidence of the impact of educational interventions on nursing students to develop their communication skills with patients. Despite the various educational pedagogies used to develop communication skills with the patient. All research agrees on the importance of developing interventions to improve communication skills with the patient in nursing students. From the main findings, it can be indicated that the majority of the analyzed studies used simulation as the methodology for communication skills training, obtaining statistically significant results. Regarding the countries in which they have carried out the studies, it is worth noting that the majority have been carried out in the USA, these data coincide with those reported in previous research on the analysis of scientific communication publications [48,49]. Regarding theoretical and conceptual frameworks to guide the intervention studies, only two studies used theoretical frameworks to guide the intervention [26,28]. However, the theoretical and conceptual frameworks are essential to develop experimental studies allowing the variables and the relationship between them to be established, described in previous studies. The conceptual frameworks provide information about the subjects, the way of collecting and statistical analysis of the data, making it possible to guide the interventions in the experimental studies and helping the interpretation of the data [50].
However, measuring patient-centered communication can be difficult due to the numerous definitions that exist to refer to this type of communication such as TC, nurse–patient communication or interpersonal communication. In addition, there are numerous aspects of communication with the patient that must be considered, as reflected in, for example, the conceptual framework of interpersonal relationships [2]. The instruments used must prove to be valid and reliable. However, only fourteen of the articles reviewed provided data on the validity and reliability of the tool [26,28,34,35,36,37,40,42,43,44,45,46,47]. These issues suggest that researchers should consider the relevance of instruments to assess patient-centered communication before using them. In addition to considering the validity and reliability of the instruments, if they were developed in previous studies, psychometric tests should be performed for the study population. In the case that these instruments were developed by the researchers of the study, they should report the psychometric properties of them. On the other hand, previous studies have indicated the need to develop and validate instruments to assess patient-centered communication skills of nursing students [51,52]. The development of validated instruments to assess communication skills with patients would allow evaluating the impact of the interventions developed on nursing students and determining which interventions are more effective.
Regarding interventions to improve patient-centered communication skills of nursing students, it was observed that the majority focused on simulation, using SP (e.g., [26,32,33]), role-playing [39] or high-fidelity patient [34], to either facilitate learning or evaluate communication skills. Previous studies indicate the importance of incorporating simulation in communication skills training. In particular, simulation provides realistic scenarios that allow nursing students to practice and evaluate TC with patients, without putting real patients at risk [53]. In addition, various studies indicate that the simulation with SP offers nursing students the opportunity to practice TC before clinical practices, being able to improve communication with the patient in the clinical setting [54,55]. Simulation using SP can be effective in teaching patient-centered clinical skills [53,56]. On the other hand, previous studies have shown the training of individuals to treat patients in realistic situations provides an opportunity to improve the competencies of nursing students through human interaction and feedback [57,58]. In this review, all of the studies that implemented simulation conducted feedback with the nursing students. The process of providing feedback during or after the simulation sessions allowed them to address their strengths and weaknesses in order to improve their performance [57,58]. In conclusion, previous research indicates that the implementation of simulation in clinical skills training programs could be useful to improve nurses’ communication skills and the ability to interact with patients [6,52]. In relation to the application of innovative educational pedagogies, various studies have indicated the need to implement new active learning pedagogies that involve students in their training in order to improve their clinical skills [59,60]. Regarding the use of courses as an intervention to improve communication skills with the patient, they have been shown to be effective in some of the included studies. However, the development of courses based on master classes is not recommended as the only educational resource in the training of nursing students and should be combined with other educational pedagogies [61]. In short, previous studies indicate that the new generation of students prefer self-directed, immediate, exciting and immersive experiences [62]. They encourage nurse educators to superimpose the dissonances between traditional teaching and generational learning needs, based on active learning, simulations, reflective learning and educational games [63,64]. Hence, most studies are based on simulation or innovative pedagogies, to encourage student participation in the acquisition of skills.
Following the analysis of the included articles, the contexts were mainly based on mental health [26,31,33,35,36,37,38,39,40], end-of-life [32,43,47] and maternity [34]. Six studies focused on general patient-centered communication skills [28,41,42,44,45,46]. Previous studies have indicated that interventions to teach nurse-patient communication skills target the most challenging clinical interactions [52]. These data are consistent with the studies included in this review. In particular, previous studies indicate that nursing students feel challenged and anxious when they have to talk and interact with mental health patients [65,66]; hence, it is one of the most predominant clinical areas in this review. In addition a review indicated that further studies are needed to improve the available evidence on the clinical practice of nursing students with mental health patients [67]. However, the communication skills involved in everyday conversation with patients are equally important, especially given the perception that nurses lack the time to communicate with patients [68] or with chronically ill patients [7,8], and this was not addressed in the nursing students. Regarding the year that the nursing students were enrolled in, statistically significant improvements were observed in both the students enrolled in their first year [28,32,34,35,42] and those in their last year of the nursing degree [33,37,38,39,44,45,46]. In addition, several studies indicate that communication skills training should be incorporated into the nursing degree curriculum every year. Therefore, the students learn and practice various communication skills before beginning their clinical practices in different clinical areas [15,68].
In this systematic review, in which 19 quantitative studies on patient-centered communication interventions in nursing students were reviewed, half of them were found, specifically thirteen [26,28,32,34,36,38,39,40,42,44,45,46,47], to be effective in improving patient-centered communication skills. The differences between the obtained results may be due to the study design, as there was a lot of variability in the designs, sampling, teaching interventions, duration and sample size. In addition, several studies indicated improvements in patient-centered communication skills, although the results were not statistically significant in some of them (e.g., [33,35,37]). On the other hand, only one study evaluated the long-term impact of intervention on nursing students, finding statistically significant differences [38]. It would be necessary for future studies to evaluate the long-term impact of the interventions in order to improve their communication skills with patients and to determine the effectiveness over time.
A longitudinal study design is recommended to assess the stability and long-term influence of the improvements in communication skills observed in this study. Specifically, observational studies are needed to assess student performance in clinical areas.
Strengths and limitations
This review includes the following limitations. First, articles that were not in English were excluded, which may constitute a bias by not considering other languages. Most of the included studies used self-report measures to identify the results and few studies used more objective measures. Furthermore, the heterogeneity of the intervention methods and measurements of the studies’ results prevented a synthesis of results through meta-analysis. The studies need more evidence to address the possibility of bias due to the use of self-report measures and other potential forms of bias [69]. For example, the inclusion of quasi-experimental studies without randomization presents a selection bias. This aspect tends to overestimate the effects of intervention, even though a rigorous methodology and relevant data are presented. The studies of a single group that evaluate the impact of intervention, based on differences between pre-test and post-test measures, can interfere with internal validity by not being compared with students of the same cohort who were not exposed to the intervention. The studies where training was carried out over a period of time can lead to biases, as it is not possible to prove whether changes were due to the intervention or other academic activities. Another risk of bias in the studies is that the instructors who performed the interventions were not blinded due to the nature of the educational intervention studies. On the other hand, it is also important to consider that almost 50% of the studies were carried out within the context of mental health, as communication is a key element of the nurse-patient relationship in this area. However, it would be interesting in future research to be able to deepen the analysis of communication skills learning within the nursing curriculum and the subjects or areas in which it is involved.
This systematic review had some strengths. First, a broad search was performed using MeSH terms and keywords that addressed the communication of nursing students with the patient; and this search was performed in multiple databases. Despite this, research methods have been systematically applied in this review following the guidelines established for systematic review. In addition, a two-person review of what studies to include and the assessment of their quality increased the rigor of the findings. Therefore, the results obtained expand and update what was known thus far about patient-centered communication interventions for nursing students.
More research is needed to develop instruments that evaluate all aspects that interfere with patient-centered communication in order to improve patient-centered communication skills of nursing students through more effective educational strategies, guided by theoretical frameworks, in a more consistent way. In addition, studies should be carried out that report the perspective of the patient in regards to communication established with the nursing students.
5. Conclusions
This systematic review provides preliminary evidence of the effectiveness of interventions used to train nursing students in patient-centered communication. Although all the interventions obtained significant results in communication skills, it has not yet been determined which methodology is more effective. The majority of the analyzed studies used simulation as the methodology for communication skills training, obtaining statistically significant results. This methodology could be combined with other educational strategies that have indicated improved communication of nursing students with their patients.
Author Contributions
Conceptualization, L.G.-P. and V.V.M.-H.; Methodology, L.G.-P., V.V.M.-H., V.G.-P., G.A.-M.; Writing—Original Draft Preparation, L.G.-P., V.V.M.-H., and G.A.-M.; Writing—Review & Editing, V.G.-P. and G.G.-G.; Supervision: L.G.-P., V.V.M.-H.,V.G.-P., G.G.-G., G.A.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
Conflicts of Interest
The authors declare no conflict of interest.
References
- Rosenberg, S.; Gallo-Silver, L. Therapeutic communication skills and student nurses in the clinical setting. Teach. Learn. Nurs. 2011, 6, 2–8. [Google Scholar] [CrossRef]
- Peplau, H. Interpersonal Relations in Nursing: A Conceptual Frame of Reference for Psychodynamic Nursing; Springer Publishing Company: New York, NY, USA, 1991. [Google Scholar]
- Cusatis, R.; Holt, J.M.; Williams, J.; Nukuna, S.; Asan, O.; Flynn, K.E.; Neuner, J.; Moore, J.; Crotty, B.H. The impact of patient-generated contextual data on communication in clinical practice: A qualitative assessment of patient and clinician perspectives. Patient Educ. Couns. 2019. [Google Scholar] [CrossRef] [PubMed]
- Makoul, G.; Krupat, E.; Chang, C.H. Measuring patient views of physician communication skills: Development and testing of the Communication Assessment Tool. Patient Educ. Couns. 2007, 67, 333–342. [Google Scholar] [CrossRef] [PubMed]
- Abdolrahimi, M.; Ghiyasvandian, S.; Zakerimoghadam, M.; Ebadi, A. Antecedents and Consequences of Therapeutic Communication in Iranian Nursing Students: A Qualitative Research. Nurs. Res. Pract. 2017, 1, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Ryan, C.A.; Walshe, N.; Gaffney, R.; Shanks, A.; Burgoyne, L.; Wiskin, C.M. Using standardized patients to assess communication skills in medical and nursing students. BMC Med. Educ. 2010, 10, 24. [Google Scholar] [CrossRef] [PubMed]
- Hsu, L.L.; Chang, W.H.; Hsieh, S.I. The effects of scenario-based simulation course training on nurses’ communication competence and self-efficacy: A Randomized Controlled Trial. J. Prof. Nurs. 2015, 31, 37–49. [Google Scholar] [CrossRef]
- Kim, H.; Tietsort, C.; Posteher, K.; Michaelides, A.; Toro-Ramos, T. Enabling Self-management of a Chronic Condition through Patient-centered Coaching: A Case of an mHealth Diabetes Prevention Program for Older Adults. Health Commun. 2019, 12, 1–9. [Google Scholar] [CrossRef]
- Dahlin, C. National Consensus Project for Quality Palliative Care. Clinical Practice Guidelines for Quality Palliative Care; National Consensus Project: Pittsburgh, PA, USA, 2013. [Google Scholar]
- Pope, B.B.; Rodzen, L.; Spross, G. Raising the SBAR: How better communication improves patient outcomes. Nursing 2008, 38, 41–43. [Google Scholar] [CrossRef]
- Vaghee, S.; Lotfabadi, M.K.; Salarhaji, A.; Vaghei, N.; Hashemi, B.M. Comparing the Effects of Contact-Based Education and Acceptance and Commitment-Based Training on Empathy toward Mental Illnesses among Nursing Students. Iran. J. Psychiatry 2018, 13, 119–127. [Google Scholar]
- National Institute for Health and Care Excelence. End of Life Care for Infants, Children and Young People with Life-Limiting Conditions: Planning and Management 2016. Available online: https://www.nice.org.uk/guidance/ng61/ (accessed on 12 December 2019).
- Alasad, J.; Ahmad, M. Communication with critically ill patients. J. Adv. Nurs. 2005, 50, 356–362. [Google Scholar] [CrossRef]
- Mullan, B.A.; Kothe, E.J. Evaluating a nursing communication skills training course: The relationships between self-rated ability, satisfaction, and actual performance. Nurse Educ. Pract. 2010, 10, 374–378. [Google Scholar] [CrossRef] [PubMed]
- Neilson, S.J.; Reeves, A. The use of a theatre workshop in developing effective communication in pediatric end of life care. Nurse Educ. Pract. 2019, 36, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, S.; Perry, R.; Blanchard, K.; Linsell, L. Effectiveness of a three-day communication skills course in changing nurses’ communication skills with cancer/palliative care patients: A randomised controlled trial. Palliat. Med. 2008, 22, 365–375. [Google Scholar] [CrossRef]
- Kiani, F.; Balouchi, A.; Shahsavani, A. Investigation of nursing students’ verbal communication quality during patients’ education in zahedan hospitals: Southeast of Iran. Glob. J. Health Sci. 2016, 8, 331–336. [Google Scholar] [CrossRef]
- Bhana, V.M. Interpersonal skills development in Generation Y student nurses: A literature review. Nurse Educ. Today 2014, 34, 1430–1434. [Google Scholar] [CrossRef] [PubMed]
- Heidari, H.; Mardani Hamooleh, M. Improving communication skills in clinical education of nursing students. J. Client Cent. Nurs. Care 2015, 1, 77–82. [Google Scholar]
- Shafakhah, M.; Zarshenas, L.; Sharif, F.; Sarvestani, R.S. Evaluation of nursing students’ communication abilities in clinical courses in hospitals. Glob. J. Health Sci. 2015, 7, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Epstein, R.M.; Fiscella, K.; Lesser, C.S.; Stange, K.C. Why the nation needs a policy push on patient-centered health care. Health Aff. 2010, 29, 1489–1495. [Google Scholar] [CrossRef]
- Robinson, J.H.; Callister, L.C.; Berry, J.A.; Dearing, K.A. Patient-centered care and adherence: Definitions and applications to improve outcomes. J. Am. Acad. Nurse Pract. 2008, 20, 600–607. [Google Scholar] [CrossRef]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0; Cochrane Collaboration: London, UK; Jonh Wiley & Sons Ltd: London, UK, 2011. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Joanna Briggs Institute. Joanna Briggs Institute Reviewers’ Manual: 2014 Edition; The Joanna Briggs Institute: Adelaide, Australia, 2014. [Google Scholar]
- Donovan, L.M.; Mullen, L.K. Expanding nursing simulation programs with a standardized patient protocol on therapeutic communication. Nurse Educ. Pract. 2019, 38, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Merriam, S.B.; Cafferella, R.S.; Baumgartner, L.M. Learning in Adulthood a Comprehensive Guide, 3rd ed.; John Wiley & Sons Inc: San Francisco, CA, USA, 2012. [Google Scholar]
- Shorey, S.; Kowitlawakul, Y.; Devi, M.K.; Chen, H.C.; Soong, S.K.A.; Ang, E. Blended Learning Pedagogy designed for Communication Module among Undergraduate Nursing Students: A quasi-experimental study. Nurse Educ. Today 2018, 61, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-Efficacy: The Exercise of Control; Freeman: New York, NY, USA, 1997. [Google Scholar]
- Herrington, J.; Reeves, T.; Oliver, R. A Guide to Authentic E-Learning; Routledge: New York, NY, USA, 2010. [Google Scholar]
- Becker, K.L.; Rose, L.E.; Berg, J.B.; Park, H.; Shatzer, J.H. The Teaching Effectiveness of Standardized Patients. J. Nurs. Educ. 2006, 45, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Bloomfield, J.G.; O’Neill, B.; Gillett, K. Enhancing student communication during end-of-life care: A pilot study. Palliat. Supportive Care 2015, 13, 1651–1661. [Google Scholar] [CrossRef]
- Gaylle, D. In-simulation Debriefing Increases Therapeutic Communication Skills. Nurs. Educ. 2019, 44, 295–299. [Google Scholar] [CrossRef]
- Kim, H.Y.; Ko, E.; Lee, E.S. Effects of simulation-based education on communication skill and clinical competence in maternity nursing practicum. Korean J. Women Health Nurs. 2012, 18, 312–320. [Google Scholar] [CrossRef]
- Lin, E.C.L.; Chen, S.L.; Chao, S.Y.; Chen, Y.C. Using standardized patient with immediate feedback and group discussion to teach interpersonal and communication skills to advanced practice nursing students. Nurse Educ. Today 2013, 33, 677–683. [Google Scholar] [CrossRef]
- Martin, C.T.; Chanda, N. Mental Health Clinical Simulation: Therapeutic Communication. Clin. Simul. Nurs. 2016, 12, 209–214. [Google Scholar] [CrossRef]
- Ok, E.; Kutlu, F.Y.; Ates, E. The Effect of Standardized Patient Simulation Prior to Mental Health Rotation on Nursing Students’ Anxiety and Communication Skills. Issues Ment. Health Nurs. 2020, 41, 251–255. [Google Scholar] [CrossRef]
- Webster, D. Using Standardized Patients to teach Therapeutic Communication in Psychiatric Nursing. Clin. Simul. Nurs. 2014, 10, e81–e86. [Google Scholar] [CrossRef]
- Blake, T.; Blake, T. Improving Therapeutic Communication in Nursing through Simulation Exercise. Teach. Learn. Nurs. 2019, 14, 260–264. [Google Scholar] [CrossRef]
- Lai, C.Y. Training Nursing Students’ Communication Skills with Online video peer Assessment. Comput. Educ. 2016, 97, 21–30. [Google Scholar] [CrossRef]
- Baghcheghi, N.; Koohestani, H.R.; Rezaei, K. A comparison of the cooperative learning and traditional learning methods in theory classes on nursing students’ communication skill with patients at clinical settings. Nurse Educ. Today 2011, 31, 877–882. [Google Scholar] [CrossRef] [PubMed]
- Yoo, M.S.; Park, H.R. Effects of case-based learning on communication skills, problem-solving ability, and learning motivation in nursing students. Nurs. Health Sci. 2015, 17, 166–172. [Google Scholar] [CrossRef]
- Jo, K.H.; An, G.J. Effect of end-of-life Care Education using Humanistic Approach in Korea. Collegian 2015, 22, 91–97. [Google Scholar] [CrossRef]
- Lau, Y.; Wang, W. Development and evaluation of a learner-centered training course on communication skills for baccalaureate nursing students. Nurse Educ. Today 2013, 33, 1617–1623. [Google Scholar] [CrossRef]
- Lau, Y.; Wang, W. Development and Evaluation of a learner-centered educational Summer Camp Program on Soft Skills for baccalaureate nursing students. Nurse Educ. 2014, 39, 246–251. [Google Scholar] [CrossRef]
- Taghizadeh, R.; Hasanpour-Dehkordi, A.; Shakhaei, S.; Motaarefi, H. The Effects of Teaching Communication Skills to Nursing Students on the Quality of Care for Patients. Asian J. Pharm. 2018, 12, S1252–S1255. [Google Scholar]
- Wittenberg-Lyles, E.; Goldsmith, J.; Richardson, B.; Hallett, J.S.; Clark, R. The practical nurse: A case for COMFORT communication training. Am. J. Hosp. Palliat. Med. 2013, 30, 162–166. [Google Scholar] [CrossRef]
- Kim, J.N.; Park, S.C.; Yoo, S.W.; Shen, H. Mapping health communication scholarship: Breadth, depth, and agenda of published research in health communication. Health Commun. 2010, 25, 487–503. [Google Scholar] [CrossRef]
- Castillo-Esparcia, A.; Castillero-Ostio, E. Communication research. Methodologies, themes and sources. Rev. Int. Rel. Public. 2019, 18, 197–218. [Google Scholar]
- Reidl-Martínez, L.M. Marco conceptual en el proceso de investigación. Invest. Educ. Med. 2012, 1, 146–151. [Google Scholar]
- Levett-Jones, T.; Cant, R.; Lapkin, S. A systematic review of the effectiveness of empathy education for undergraduate nursing students. Nurse Educ. Today 2019, 75, 80–94. [Google Scholar] [CrossRef] [PubMed]
- MacLean, S.; Kelly, M.; Geddes, F.; Della, P. Use of simulated patients to develop communication skills in nursing education: An integrative review. Nurse Educ. Today 2017, 48, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Foronda, C.; Liu, S.; Bauman, E.B. Evaluation of simulation in undergraduate nurse education: An integrative review. Clin. Simul. Nurs. 2013, 9, e409–e416. [Google Scholar] [CrossRef]
- Oh, P.J.; Jeon, K.D.; Koh, M.S. The effects of simulation-based learning using standardized patients in nursing students: A meta-analysis. Nurse Educ. Today 2015, 35, e6–e15. [Google Scholar] [CrossRef]
- INACSL Standards Committee. INACSL Standards of best practice: Simulation. Clin. Simul. Nurs. 2013, 12, S1–S50. [Google Scholar]
- Lewis, K.L.; Bohnert, C.A.; Gammon, W.L.; Hölzer, H.; Lyman, L.; Smith, C.; Thompson, T.M.; Wallace, A.; Gliva-McConvey, G. The association of standardized patient educators (ASPE) standards of best practice (SOBP). Adv. Simul. 2017, 2, 10–18. [Google Scholar] [CrossRef]
- Fioravanti, M.A.; Hagle, H.; Puskar, K.; Knapp, E.; Kane, I.; Lindsay, D.; Terhorst, L.; Mitchell, A.M. Creative learning through the use of simulation to teach nursing students screening, brief intervention, and referral to treatment for alcohol and other drug use in a culturally competent manner. J. Transcult. Nurs. 2018, 29, 387–394. [Google Scholar] [CrossRef]
- Kaplonyi, J.; Bowles, K.A.; Nestel, D.; Kiegaldie, D.; Maloney, S.; Haines, T.; Williams, C. Understanding the impact of simulated patients on health care learners’ communication skills: A systematic review. Med. Educ. 2017, 51, 1209–1219. [Google Scholar] [CrossRef]
- Henderson, A.; Rowe, J.; Watson, K.; Hitchen-Holmes, D. Graduating nurses’ self-efficacy in palliative care practice: An exploratory study. Nurse Educ. Today 2016, 39, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Henderson, A.; Harrison, P.; Rowe, J.; Edwards, S.; Barnes, M.; Henderson, S. Students take the lead for learning in practice: A process for building self-efficacy into undergraduate nursing education. Nurse Educ. Pract. 2018, 31, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Oyelana, O.; Martin, D.; Scanlan, J.; Temple, B. Learner-centred teaching in a non-learner-centred world: An interpretive phenomenological study of the lived experience of clinical nursing faculty. Nurse Educ. Today 2018, 67, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Chicca, J.; Shellenbarger, T. Connecting with Generation Z: Approaches in nursing education. Teach. Learn. Nurs. 2018, 13, 180–184. [Google Scholar] [CrossRef]
- Repsha, C.L.; Quinn, B.L.; Peters, A.B. Implementing a Concept-Based Nursing Curriculum: A Review of the Literature. Teach. Learn. Nurs. 2020, 15, 66–71. [Google Scholar] [CrossRef]
- Shatto, B.; Shagavah, A.; Krieger, M.; Lutz, L.; Duncan, C.E.; Wagner, E.K. Active learning outcomes on NCLEX-RN or standardized predictor examinations: An integrative review. J. Nurs. Educ. 2019, 58, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Sarikoc, G.; Ozcan, C.T.; Elcin, M. The impact of using standardized patients in psychiatric cases on the levels of motivation and perceived learning of the nursing students. Nurse Educ. Today 2017, 51, 15–22. [Google Scholar] [CrossRef]
- Williams, B.; Reddy, P.; Marshall, S.; Beovich, B.; McKarney, L. Simulation and mental health outcomes: A scoping review. Adv. Simul. 2017, 2, 2–9. [Google Scholar] [CrossRef]
- Øgård-Repål, A.; De Presno, Å.K.; Fossum, M. Simulation with standardized patients to prepare undergraduate nursing students for mental health clinical practice: An integrative literature review. Nurse Educ. Today 2018, 66, 149–157. [Google Scholar] [CrossRef]
- Chan, E.A. Cue-responding during simulated routine nursing care: A mixed method study. Nurse Educ. Today 2014, 34, 1057–1061. [Google Scholar] [CrossRef]
- Polit, D.F.; Beck, C.T. Nursing Research: Generating and Assessing Evidence for Nursing Practice; Wolter Kluwer: New York, NY, USA, 2008. [Google Scholar]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).