Abstract
Deep margin elevation (DME) is a widely adopted technique for managing subgingival cervical proximal margins by repositioning them to a supragingival location. This approach enhances access, visibility, and control in these anatomically challenging areas. This narrative review aimed to evaluate current evidence on the indications, materials, clinical protocols, and outcomes of DME. A structured search was conducted in PubMed, the Cochrane Library and Scopus up to February 2025, using keywords such as “deep margin elevation”, “proximal box elevation” and “subgingival margin.” Clinical studies, in vitro investigations, relevant reviews and reports in English were included. A total of 59 articles were selected based on eligibility criteria. The hypothesis was that DME can serve as a reliable alternative to surgical crown lengthening in appropriate cases. A variety of materials have been investigated for use as the intermediate layer, with composite resins of varying viscosities and filler compositions being preferred due to their favorable long-term mechanical properties. DME may reduce the need for surgical intervention while maintaining periodontal health; however further randomized clinical trials are needed to clarify the material selection, establish long-term outcomes, and standardize clinical protocols. Understanding the indications, limitations, and protocol of DME is critical for achieving biologically sound and predictably functional restorations.
1. Introduction
Achieving optimal restoration in the presence of subgingival margins remains a significant clinical challenge in restorative dentistry [1]. Such margins complicate essential procedures including rubber dam isolation, matrix placement, material adaptation, and cervical finishing [2]. Additionally, they hinder impression-taking, cementation, and adhesive bonding, particularly for indirect restorations, often resulting in plaque accumulation, gingival inflammation, supracrestal tissue attachment (STA) violation, and restoration failure [3,4,5].
Traditional solutions like surgical crown lengthening and orthodontic extrusion aim to reestablish supragingival margins but present notable drawbacks [6,7,8]. Crown lengthening may compromise periodontal support and esthetics [9], while orthodontic extrusion demands prolonged treatment and patient compliance [10]. These limitations underline the need for a minimally invasive, time-efficient alternative that preserves periodontal health.
In this context, Deep margin elevation (DME) has gained attention as a conservative technique that relocates subgingival margins coronally through the placement of a composite resin layer [11,12]. Originally described by Dietschi and Spreafico in 1998 [13] for indirect restorations, its indications have since expanded to include direct and chairside-fabricated restorations [14]. DME offers improved access, isolation, and marginal integrity, and may reduce the biological complications associated with deep margins [14,15,16]. Despite its increasing use, the DME technique remains under-researched. Current literature lacks consensus on ideal materials, clinical protocols, and long-term outcomes [17]. Additionally, few randomized clinical trials (RCTs) have evaluated its periodontal impact, and there is insufficient guidance on when and how to implement the technique effectively.
This narrative review aims to synthesize existing evidence on the clinical application of DME, with particular focus on its indications, materials, procedural techniques, and reported outcomes. While several reviews have previously addressed DME, there remains significant variability in the materials and protocols recommended, ranging from resin-modified glass ionomers to high-viscosity flowables and bulk-fill composites, as well as differing adhesive and layering strategies. This heterogeneity may create uncertainty among clinicians regarding its optimal implementation. By critically examining the available literature, this review aims to clarify current clinical practices, identify methodological inconsistencies, and highlight the need for standardized guidelines and further research to establish the long-term effectiveness and biological safety of DME.
2. Materials and Methods
This study was conducted as a narrative review incorporating a structured search strategy to identify relevant literature on DME and related restorative techniques. The review followed a modified PICO framework: Population (P): posterior teeth with subgingival margins; Intervention (I): Deep margin elevation using adhesive materials; Comparison (C): alternative techniques such as surgical crown lengthening or orthodontic extrusion; and Outcomes (O): clinical performance, periodontal response, marginal integrity, and long-term success of the restorations. A comprehensive electronic search was conducted across three major databases (PubMed, the Cochrane Library, and Scopus) from January 1998 (the year DME was first introduced) to February 2025. The search terms included: deep margin elevation, proximal box relocation, subgingival margins, adhesive restorative techniques, posterior teeth, combined using Boolean operators (“AND,” “OR”) and adjusted according to the database syntax to optimize sensitivity. Web of Science was not included, as preliminary scoping revealed substantial overlap with the results retrieved from Scopus. The latter was prioritized due to its broader indexing of both clinical and laboratory-based dental research.
Inclusion criteria incorporated studies that directly addressed DME techniques and provided information on indications, contraindications, materials used, clinical or laboratory protocols, and reported outcomes. Eligible publication types included systematic reviews, meta-analyses, randomized and non-randomized clinical trials, case series, case reports, and in vitro or in vivo experimental studies. Only articles published in English were considered. Studies were excluded if they did not specifically discuss DME or margin relocation in a restorative context, or if they were non-English publications.
The selection process was conducted in two phases: the initial screening of titles and abstracts to assess their relevance, followed by full-text evaluation to decide upon its final inclusion. Three independent reviewers assessed study eligibility, and any disagreements were resolved through discussion and consensus. The selection workflow followed the specific guidelines illustrated in the corresponding PRISMA flow diagram. A qualitative synthesis approach was used to summarize the findings related to clinical indications, materials, procedural techniques, and the reported outcomes. Furthermore, the included studies were critically appraised to evaluate their methodological rigor, identify inconsistencies, and highlight current gaps in the literature that warrant further investigation.
The structured search strategy was informed by published guidance [18], which is included in the main reference list to ensure consistent citation formatting. The selection process and eligibility assessment are outlined in the relevant Prisma Flow diagram (Figure 1).
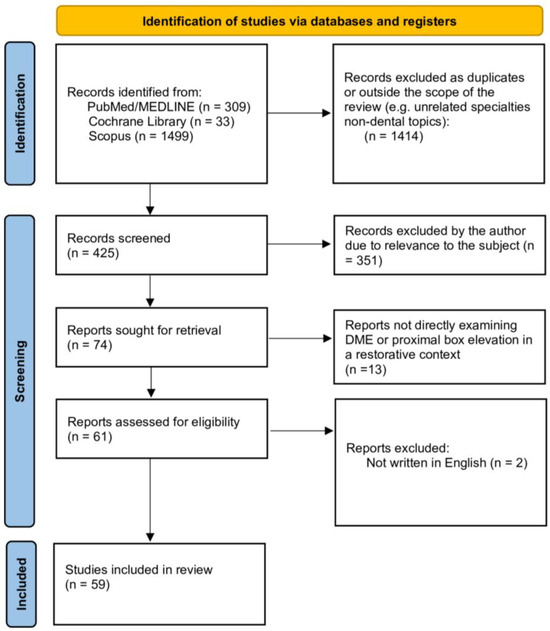
Figure 1.
PRISMA Flow Diagram.
The reviewed literature included various study types. Among the 59 items analyzed, 11 were clinical experimental studies. Additionally, the review comprised 23 in vitro studies, 20 systematic or narrative reviews, 2 case reports, 2 finite element analyses and 1 clinical technique description paper. The distribution of each type of evidence, along with the corresponding percentages, are presented in Figure 2.
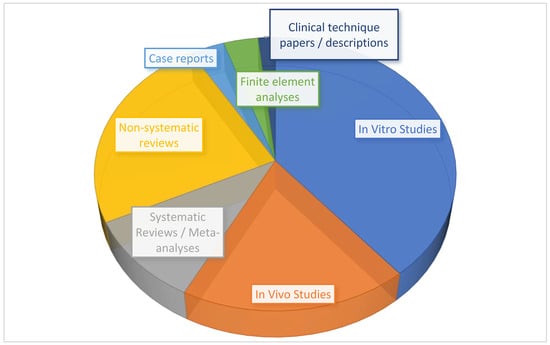
Figure 2.
Study types in the available literature.
While this diversity proves the multifaceted interest in the topic, it also reflects the inherent limitations of the available evidence. Many of the clinical studies included were small in scale and only 2 of them featured follow-up periods of longer than 5 years. A significant proportion of the clinical studies did not employ randomized designs, which may introduce bias and limit the generalizability of their findings. Similarly, while in vitro and finite element studies provide valuable insights into mechanical behavior, they may not fully simulate intraoral conditions. These limitations have been taken into account during the synthesis and interpretation of the findings.
3. Results
3.1. Evolution of DME
DME is based on relocating deep cervical margins coronally with an intermediate material layer, offering an alternative to surgical crown lengthening and orthodontic extrusion (Figure 3) [15,19]. Dietschi and Spreafico proposed the use of composite resin for this purpose [13]. The technique evolved from the open-sandwich technique, which used glass ionomer cement or resin-modified glass ionomer cement [20]. Today, composite resins of various viscosities with layered application options are predominantly used [21].
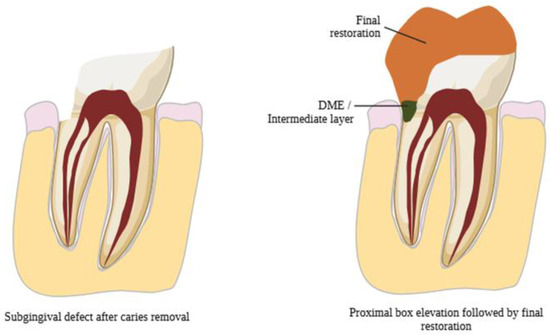
Figure 3.
The basic principle of DME.
In 1998, Dietschi and Spreafico introduced the technique commonly referred to as deep margin relocation. This technique gained wider recognition in 2012 with the term “deep margin elevation”, which was proposed by Magne and Spreafico [14]. The goal of this technique is to elevate the cervical margin of a cavity coronally, either at or above the gingival level, using composite resin.
However, the article by Dietschi and Spreafico was not the first to reference the use of material for relocating the cervical margin of a cavity. As early as 1977, McLean and Wilson proposed the placement of a glass ionomer cement layer at the cervical margin of Class II restorations with subgingival margins, followed by overlaying this layer with composite resin. This method, widely known as the “open-sandwich technique”, demonstrated limited success due to the dissolution and mechanical degradation of conventional glass ionomer when exposed to the oral environment [22].
To address these limitations, resin-modified glass ionomer cement was introduced, offering improved mechanical properties, easier handling and significantly higher success rates compared to traditional glass ionomer. Nevertheless, advancements in composite resin materials and the ability to ensure proper isolation and moisture control, have shifted the focus of most researchers towards the exclusive use of various types of composite resins for cervical margin elevation [23,24].
3.2. Indications for DME
DME is primarily indicated for clinical situations where deep cervical proximal margins extend subgingivally but remain within the limits of the junctional epithelium [25]. The successful application of DME relies heavily on preserving the biological width, now more precisely termed the supracrestal tissue attachment (STA). To avoid STA violation, it is critical to ensure that the restorative margin is positioned at least 2.04 mm coronal to the alveolar bone crest, accounting for the dimensions of both the junctional epithelium and the connective tissue attachment [5].
In addition, DME is particularly beneficial when managing deep margins during indirect restorative procedures such as inlays, onlays, and overlays. Elevating the margin to a supragingival or easily accessible location offers multiple clinical advantages. These include improved moisture control, enhanced visibility, facilitated impression-taking, more predictable bonding conditions, and the easier removal of excess restorative material [2]. Achieving a supragingival margin significantly enhances the clinician’s ability to isolate the operative field, a crucial factor for the success of adhesive procedures. However, a fundamental prerequisite for performing DME is the ability to achieve complete and effective isolation of the operative field using a rubber dam [14]. Without adequate isolation, the risk of contamination increases, compromising the adhesive interface and the longevity of the restoration. Therefore, DME should only be considered in cases where proper rubber dam placement and stable isolation are feasible [26].
3.3. DME Technique
According to the protocol suggested by Magne et al. [14], DME should be performed only when the field can be properly isolated with a rubber dam and the matrix system provides a firm seal.
After placing a rubber dam, old restorations and carious tissues are removed. Radiographic examination of the margin is essential to verify STA integrity and pulp involvement. Periodontal evaluation ensures predictable healing [27].
Tofflemire circumferential metal matrices are preferred, covering the cervical margin fully. In cases where the margin lies above the cemento-enamel junction (CEJ), conventional matrices suffice. For sub-CEJ margins, curved metal matrices, trimmed to 2–3 mm, slightly above the desired margin height- ensure proper adaptation and a proper emergence profile. (Figure 4) [14].
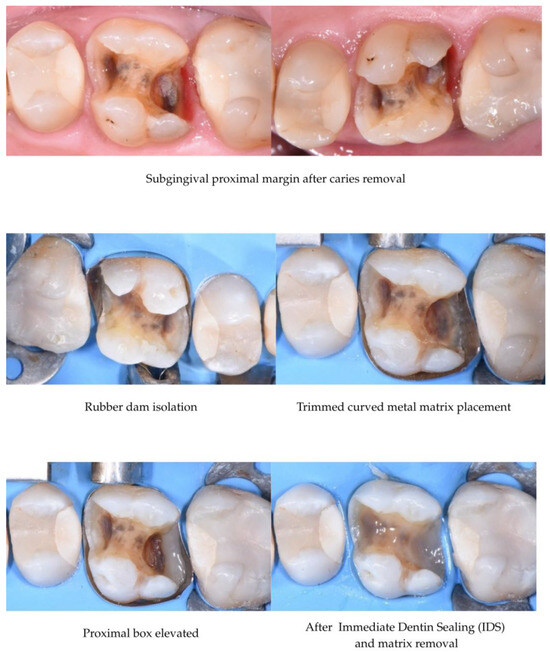
Figure 4.
DME with a curved metal matrix.
A critical focal point during DME is to ensure that neither the gingival tissues nor portions of the rubber dam interfere in the area between the prepared margin and the matrix band. Proper matrix adaptation is essential for achieving an accurate restoration contour and an optimal seal [28]. Additionally, sufficient height and stability of the buccal and lingual walls are crucial, as these structures support the matrix system and maintain its proper positioning during the composite placement [29].
Before proceeding with bonding procedures, Magne et al. [12] recommend the gentle re-preparation of the cavity margins using an ultrasonic instrument or a fine-grit diamond bur. This step aims to remove any debris or contamination that may have occurred during matrix placement, thereby optimizing the substrate for adhesive bonding.
For the adhesive protocol, the use of a three-step etch-and-rinse adhesive system combined with Immediate Dentin Sealing (IDS) is advised to enhance the bond strength and long-term stability. Composite resin is then applied incrementally to elevate the margin by approximately 1.5 to 3 mm. Preheated composite resin (at approximately 55 °C) is preferred, as the increased temperature reduces the viscosity of the material, allowing for an improved adaptation to cavity walls and minimizing the risk of void formation.
Following the composite placement, excess material should be meticulously removed using a No. 12 surgical blade. Flossing between contacts and polishing with abrasive strips help refine the interproximal surfaces and ensure a proper emergence profile. Radiographic confirmation, preferably using periapical X-rays, is a recommended final step to verify the correct adaptation of the material, the absence of gaps or voids, and a harmonious emergence profile before proceeding with the final indirect restoration (Figure 5).
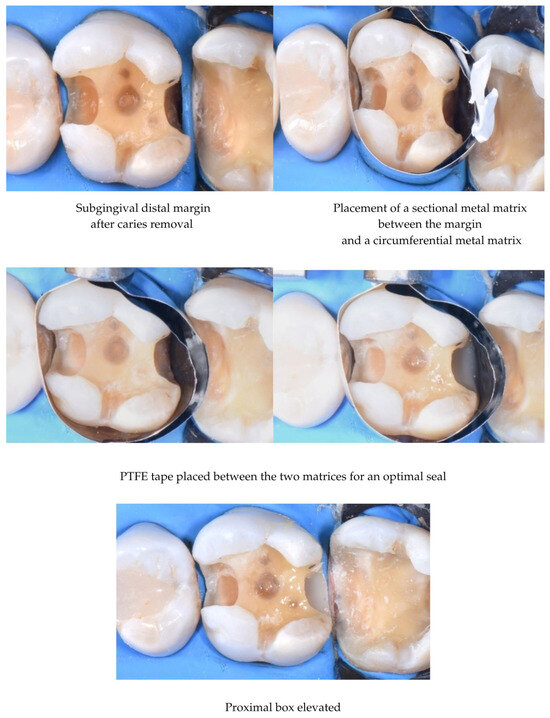
Figure 5.
Matrix-in-matrix technique.
Despite the emphasis placed on the rubber dam and matrix system placement, Frese et al. described a technique that utilizes neither of these: the R2-technique [27]. This approach relies on the principle that moisture control during the cervical margin relocation process is confined within a small section of the defect, which is easily managed not to be contaminated by saliva, blood, and crevicular fluid. In the first step of this technique, after etching and bonding, a thin layer of flowable composite is placed on the surface, followed by a layer of nanohybrid composite without a matrix (Figure 6). Both layers are light-cured simultaneously (snowplow technique). The inevitable excess is removed at this point using a No. 12 scalpel blade or a fine diamond bur. Afterwards, if a direct restoration is planned, a rubber dam, a sectional matrix, and a wedge are placed to shape the proximal surface [27,30].
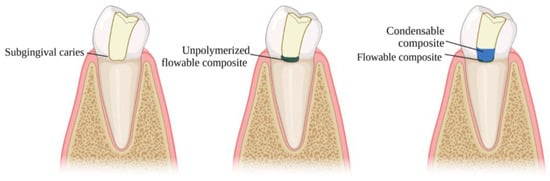
Figure 6.
Snowplow technique for DME: A thin layer (1mm) of flowable composite is applied to the margin, followed by an increment of condensable composite resin, which is then directed toward the margin and polymerized simultaneously with the flowable layer.
Although the DME technique was first described for indirect restorations, it can be a useful tool for defects that will be restored directly. In this way, rings are easily placed and a better emergence profile and tight proximal contacts are achieved.
The following tables (Table 1, Table 2, Table 3, Table 4 and Table 5) present a structured summary of all 59 studies on DME included in this review. Each entry is categorized by study type and provides essential background information, such as the materials and methods used, the aging simulation, the means of evaluation and key findings. The data ranges from basic in vitro studies to long-term clinical evaluations and systematic reviews, reflecting the variability of the current literature on this topic.

Table 1.
Summary of in vitro studies included.

Table 2.
Summary of in vivo studies included.

Table 3.
Summary of reviews included.

Table 4.
Summary of case reports/case series included.

Table 5.
Summary of studies (protocol papers, finite element analyses) included.
3.4. Microleakage & Marginal Adaptation
Microleakage and proper marginal adaptation is a critical concern in DME due to the challenges of bonding to deep margins, as well as the difficulty in achieving a firm contact between the matrix and the cervical margin. Bulk-fill flowable and bioactive composites showed acceptable adaptation, while glass ionomer cement (GIC) exhibited poor mechanical properties over time. Flowable composites are beneficial in DME due to their low viscosity, which allows for excellent marginal adaptation [34]; however, evidence suggests that thicker layers of flowable composites are prone to polymerization shrinkage [42], making the snowplow technique particularly useful in DME scenarios by minimizing the thickness of the flowable layer and reducing the risk of long-term failure. Moreover, the existing literature consistently indicates that self-curing resin cement generates a significantly higher number of microgaps, rendering it unsuitable for DME applications [48].
3.5. Bond Strength & Layering
Securing a strong bond in the deep cervical margin is crucial to ensuring the long-term stability of the restoration. The literature remains inconclusive regarding the performance of flowable composites as an intermediate layer. Flowable and condensable composite resins demonstrated similar fracture resistance [32], with no significant impact observed from variations in the DME layer height. Self-etching or universal adhesive systems are recommended for DME procedures, especially in cases when the tooth substrate is exclusively root dentin, or cementum. In an in vitro study by Magne et al. [69], preheating the adhesive system (3-step etch-and-rinse) resulted in a significantly increased μTBS between the composite resin and the underlying dentin. Whilst this technique is still under investigation, it could potentially enhance the bond strength and improve the long-term restoration performance and is therefore a valuable suggestion for further research, particularly in DME scenarios where bonding to dentin is a challenge.
3.6. Periodontal Response
The relationship between DME and periodontal health has long been a topic of debate, with heterogeneous results in the literature. It is generally accepted that DME is contraindicated when the cervical margin is located less than 2 mm from the bone crest; in such instances, surgical crown lengthening should be considered (Figure 7 and Figure 8). Before determining the treatment plan, clinicians should carefully assess the distance from the bone crest through radiographic examination and bone sounding. When the supracrestal tissue attachment (STA) is preserved (more than 2.04 mm from the bone crest), DME can be compatible with periodontal health, provided that the patient maintains adequate oral hygiene (Figure 9). It is essential to establish an emergence profile that enables the patient to maintain effective oral hygiene. Undercontoured profiles and STA violation may result in open contact points, food traps, gingival inflammation, and ultimately, restoration failure (Figure 10). Additionally, the stages of excess removal, finishing, and polishing of the composite are critical, as only a perfectly smooth composite surface can facilitate the formation of a healthy junctional epithelium, thereby promoting periodontal health [25].
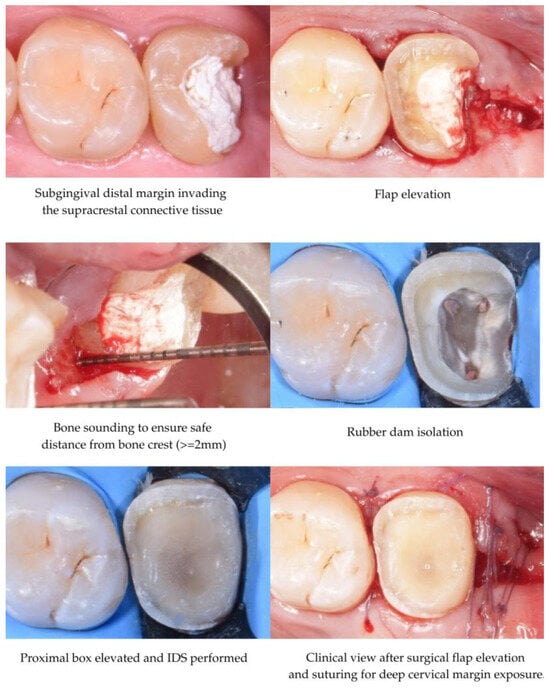
Figure 7.
DME with an open flap.
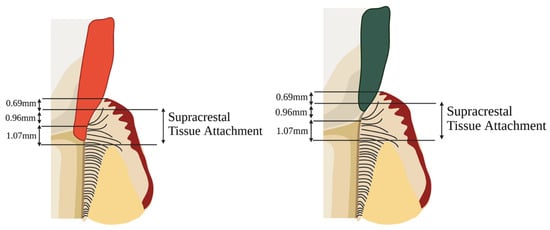
Figure 8.
(left) Subgingival margin with deep STA violation. In such cases, crown lengthening should be considered. (right) Subgingival margin with minor STA violation. In such cases, DME can be tolerated in such cases.

Figure 9.
(left) Subgingival caries in the mesial surface of a maxillary second molar. (right) Proper emergence profile after DME.
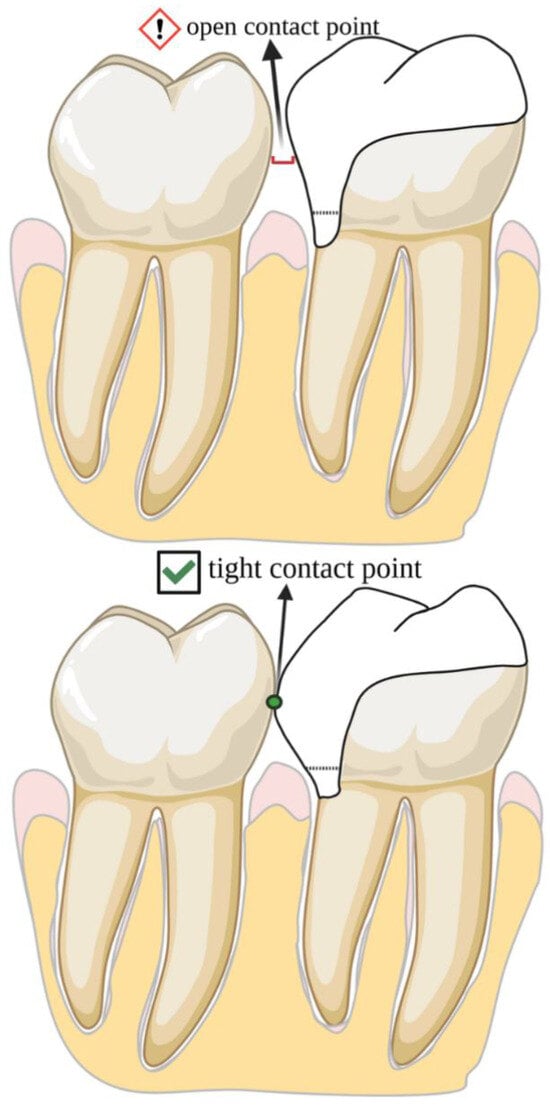
Figure 10.
A proper emergence profile of the intermediate layer allows for a tight contact point, preventing material overhangs and ensuring periodontal health.
3.7. Failure Rate
DME restorations demonstrate high survival rates, especially when combined with indirect restorations. Bresser et al. [56] reported a 95.9% five-year survival rate for partial-coverage restorations with prior DME, while Cieplik et al. [53] found comparable outcomes between restorations with and without DME. Similarly, Roggendorf et al. [46] observed no statistically significant differences in the failure rates between DME and non-DME groups. Reported failure modes primarily include secondary caries, fractures, and pulpal complications [65,70,71]. However, existing studies differ in terms of their follow-up duration, sample size, and methodologies, which limits the strength of the conclusions. Although short- and medium-term data are favorable, further large-scale, long-term clinical trials are necessary to fully validate the longevity and reliability of DME restorations.
A critical factor in assessing the long-term performance of DME restorations is a comprehensive evaluation that includes not only the DME itself but also the overlying restoration. Although DME was initially introduced as a technique for indirect partial coverage restorations, the existing literature predominantly focuses on cases where the final restoration was direct composite resin. This discrepancy may influence the interpretation of the results and the conclusions drawn regarding the long-term efficacy of DME. Therefore, future research should account for this limitation. Of the (in vitro and in vivo) studies included, 13 exclusively used direct composite resin restorations, 11 used indirect partial coverage restorations, 1 examined both and 4 used full coverage crowns. The distribution of the final restoration types is presented in Figure 11.
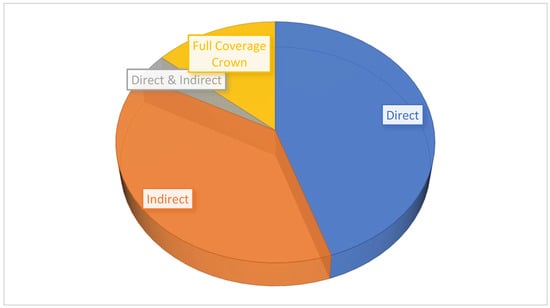
Figure 11.
Type of final restoration utilized in study.
4. Discussion
To critically evaluate DME’s clinical applicability, this discussion addresses key parameters influencing the success of the technique. These include the adhesive protocols and material selection, the mechanical properties of available restorative materials, and current evidence on long-term clinical outcomes. Additionally, the biological and periodontal implications of DME are explored, particularly in comparison with alternative treatment options such as surgical crown lengthening and orthodontic extrusion
4.1. Adhesive Strategies and Material Selection for Deep Margins
Bonding at subgingival margins presents significant clinical challenges, especially when the margins extend below the cementoenamel junction (CEJ) and lack residual enamel. This anatomical limitation necessitates specific adhesive strategies to optimize bonding without over-etching the dentin or cementum. Clinical protocols consistently recommend selective enamel etching combined with self-etch adhesives to reduce the risks associated with total-etch techniques [28,30]. Historically, glass ionomer cements (GICs) and resin-modified GICs (RMGICs) were used in deep margin elevation (DME) via the open sandwich technique. In vitro studies have demonstrated that while RMGICs exhibit favorable hydrophilicity and fluoride release, they present inferior marginal integrity and weaker bonding compared to resin composites [37]. This has led to a clinical preference for resin-based materials. In addition, flowable composites, particularly those with high viscosity, have gained traction due to their improved marginal adaptation and better performance under mechanical loading. In an in vitro study, Baldi et al. [38], found high-viscosity flowables to offer superior marginal sealing after cyclic loading. However, the lower filler content in these materials increases the risk of polymerization shrinkage [47]. Consequently, clinical protocols suggest limiting the thickness to 1–1.5 mm and recommend techniques such as "snowplow" layering to enhance interfacial adaptation [72]. Moreover, preheated bulk-fill composites have also demonstrated promising results, supported by both in vitro evidence and limited clinical data. Their enhanced flow characteristics, combined with higher filler content and favorable flexural properties, support their use in margins located at or just below the CEJ [35].
Despite advancements in composite technology, polymerization shrinkage remains a central concern. Through laboratory analysis, Lefever et al. [45] emphasized the inadequacy of self-etch adhesives in enamel bonding, reaffirming the clinical reliance on fourth- and fifth-generation adhesives with selective enamel etching. Roggendorf et al. [46] demonstrated via microleakage studies that a three-layer composite protocol could achieve marginal integrity comparable to that obtained through direct dentin bonding. Simplified clinical workflows using self-adhesive bulk-fills have also shown promise in vitro [53], although further clinical validation is necessary. Conversely, dual-cure resin cements have exhibited poor marginal adaptation in multiple laboratory investigations [45,46,60] and should be used cautiously.
The biomechanical environment of deep cervical margins, particularly under functional occlusal loading, plays a critical role in material selection. Using finite element analysis Wu et al. [67], demonstrated that vertical occlusal forces concentrate at the cervical margin, particularly in the absence of enamel. Oblique loading, especially in premolars, further amplifies stress in this region [73]. Moreover, materials with an elastic modulus similar to dentin, such as high-filled flowables and RMGICs, may offer stress-buffering effects. Although this is primarily based on mechanical simulation and in vitro studies [68], it suggests that material selection should account not only for adhesive properties but also for biomechanical behavior.
4.2. Long-Term Clinical Performance and Failures
Long-term clinical evidence on DME remains limited. However, mid-term outcomes are encouraging. In a clinical study, Bresser et al. [36], found that molars restored with lithium disilicate and DME exhibited more favorable repairability after fracture compared to subgingival ceramic restorations without DME. Ismail et al. [58] confirmed, under thermomechanical loading conditions, that composite-based DME restorations outperformed those using GICs, reinforcing the clinical shift towards composite materials.
In terms of caries risk, Kuper et al. [70] found no increased incidence of secondary caries in sub-CEJ restorations over a five-year clinical follow-up. Bresser et al. [56] reported a five-year survival rate of 95.9%, with only a 2.5% incidence of secondary caries. Additionally, DME may improve fracture resistance under a functional load [65,71], though these findings are primarily from in vitro studies. The above-mentioned results suggest that with appropriate case selection and adherence to clinical protocols, DME can provide reliable mid-term outcomes. However, robust longitudinal clinical trials beyond five years remain necessary to confirm the long-term efficacy.
Maintaining periodontal health in DME procedures is critical. Through clinical observation, Ferrari et al. [25] showed that subgingival margins placed within 2 mm of the alveolar crest resulted in increased bleeding on probing and higher plaque indices—likely due to violation of the supracrestal tissue attachment (STA). This reinforces the need to respect the STA during restorative procedures. However, Sarfati et al. [61] and Van Dijken et al. [74] presented contrasting clinical data suggesting that a long epithelial attachment can be maintained on well-finished resin margins if optimal plaque control is ensured. Nevertheless, in vitro evidence indicates that residual monomers from resin-based materials may elicit an inflammatory response, even in plaque free conditions [55]. Thus, meticulous finishing and polishing are essential to minimize adverse tissue reactions. Overall, while the short-term clinical outcomes regarding periodontal compatibility appear favorable, long-term biological integration is influenced by operator skill, margin positioning, and the chemical composition of the materials used.
4.3. DME Compared to Alternative Margin Management Techniques
DME provides a minimally invasive option compared to more invasive alternatives such as surgical crown lengthening (SCL) and orthodontic extrusion (OE). SCL has demonstrated effectiveness in exposing deep margins but is associated with post-operative discomfort, an esthetic compromise, and potentially unfavorable crown-to-root ratios [19]. OE preserves soft tissue esthetics but is time-consuming and carries risks such as root resorption and relapse, particularly with rapid extrusion protocols [59,75]. While these limitations are acknowledged, there is a lack of direct comparative clinical data evaluating DME against SCL or OE in terms of patient-centered outcomes such as recovery time, esthetic satisfaction, or cost-effectiveness. Future research should incorporate these metrics to provide a more comprehensive clinical decision framework. Preserving the natural tooth structure whenever feasible remains a central therapeutic goal, as extraction can lead to ridge collapse in the absence of immediate ridge preservation techniques and may ultimately result in significantly higher biological and financial costs for the patient.
4.4. Case Selection, Classifications, and Clinical Guidelines
Recent classification systems have improved clinical decision-making for DME. Veneziani [63] proposed a three-grade system based on isolation feasibility and bone crest proximity. Ghezzi et al. [66] expanded this by incorporating periodontal anatomical considerations, recommending that margins be placed within the junctional epithelium rather than the connective tissue. Clinical parameters such as the gingival biotype, the margin location, and hygiene status must be assessed carefully. The anterior region presents a greater risk due to esthetic demands and thin biotypes. Current evidence in anterior applications is limited [17], warranting further investigation. In general, DME is best suited for direct or indirect partial-coverage restorations. It is contraindicated in full-coverage crown preparations, where margin placement on natural tooth structure is essential for long-term success [28].
4.5. Future Research Directions
There is a need for long-term clinical studies exceeding five years, particularly for those evaluating DME in anterior teeth and in patients with varying periodontal biotypes. Comparative clinical trials assessing different composite types (e.g., high-filled flowables vs. preheated bulk-fills) under realistic conditions are lacking. Furthermore, the biological response to newer low-shrinkage and bio-interactive materials in the subgingival environment requires both clinical and histologic investigation. Additional research should explore the interface between restorative margins and the periodontal attachment using clinical trials that incorporate inflammatory biomarkers to better understand tissue-material interactions.
4.6. Summary and Clinical Recommendations
DME is a conservative technique that offers a viable alternative for managing deep subgingival margins, especially in posterior teeth. Clinical success depends on respecting the STA, using appropriately selected materials (such as high-viscosity flowables or preheated bulk-fills), employing selective enamel etching protocols, and ensuring meticulous margin finishing. With careful case selection and adherence to biological principles, DME presents a predictable strategy for integrating restorative and periodontal outcomes. However, further high-quality clinical research is essential to fully establish its long-term efficacy and comparative advantage.
5. Conclusions
DME offers a minimally invasive solution for managing subgingival margins, enhancing isolation and adhesive control in posterior restorations. When performed with proper case selection, maintaining at least 2 mm distance from the alveolar crest and using appropriate materials and adhesive protocols, DME shows promising clinical potential; however, care must be taken not to exceed 0.5 mm into the junctional epithelium or to invade the supracrestal connective tissue, as such violations may lead to chronic inflammation and jeopardize periodontal health. High-filled flowable or preheated composites are the most supported materials. Despite encouraging short-term outcomes, the current evidence is limited by heterogeneity and a lack of long-term clinical trials. Further research is needed to refine protocols and to confirm the biological compatibility as well as the long-term success of DME, particularly in complex or anterior cases.
Author Contributions
Conceptualization, A.K. and E.P.; methodology, A.K. and E.P.; validation, A.K. and M.F.; formal analysis, M.A.; investigation, A.K. and M.F.; data curation, A.K.; writing—original draft preparation, A.K.; writing—review and editing, M.F., M.A. and E.P.; visualization, A.K.; supervision, M.F., M.A. and E.P.; project administration, M.A. and E.P.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable. This study did not involve human participants or animal experiments and is based solely on previously published literature.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| DME | Deep Margin Elevation |
| STA | Supracrestal Tissue Attachment |
| IDS | Immediate Dentin Sealing |
| PTFE | Polytetrafluoroethylene |
| GIC | Glass Ionomer Cement |
| μTBS | Micro Tensile Bond Strength |
| BoP | Bleeding on Probing |
| PI | Plaque Index |
| PPD | Probing Pocket Depth |
| GI | Gingival Index |
| SCL | Surgical Crown Lengthening |
| RMGIC | Resin Modified Glass Ionomer |
| OE | Orthodontic Extrusion |
References
- Sadeghnezhad, P.; Sarraf Shirazi, A.; Borouziniat, A.; Majidinia, S.; Soltaninezhad, P.; Nejat, A.H. Enhancing subgingival margin restoration: A comprehensive review and meta-analysis of deep margin elevation’s impact on microleakage. Evid. Based Dent. 2024, 25, 212. [Google Scholar] [CrossRef]
- Aldakheel, M.; Aldosary, K.; Alnafissah, S.; Alaamer, R.; Alqahtani, A.; Almuhtab, N. Deep margin elevation: Current concepts and clinical considerations—A review. Medicina 2022, 58, 1482. [Google Scholar] [CrossRef]
- Palma, P.J.; Neto, M.A.; Messias, A.; Amaro, A.M. Microtensile Bond Strength of Composite Restorations: Direct vs. Semi-Direct Technique Using the Same Adhesive System. J. Compos. Sci. 2025, 9, 203. [Google Scholar] [CrossRef]
- Alam, M.N.; Ibraheem, W.; Ramalingam, K.; Sethuraman, S.; Basheer, S.N.; Peeran, S.W. Identification, evaluation, and correction of supracrestal tissue attachment (previously biologic width) violation: A case presentation with literature review. Cureus 2024, 16, e58128. [Google Scholar] [CrossRef]
- Felemban, M.F.; Khattak, O.; Alsharari, T.; Alzahrani, A.H.; Ganji, K.K.; Iqbal, A. Relationship between deep marginal elevation and periodontal parameters: A systematic review. Medicina 2023, 59, 1948. [Google Scholar] [CrossRef]
- Fichera, G.; Mazzitelli, C.; Picciariello, V.; Maravic, T.; Josic, U.; Mazzoni, A.; Breschi, L. Structurally compromised teeth. Part II: A novel approach to peripheral build-up procedures. J. Esthet. Restor. Dent. 2023, 36, 20–31. [Google Scholar] [CrossRef]
- Lee, B.; Shin, J.; Jeong, T.; Park, S.; Lee, E. Combined treatment of surgical extrusion and crown lengthening procedure for severe crown-root fracture of a growing patient: A case report. BMC Oral Health 2024, 24, 1498. [Google Scholar] [CrossRef]
- Uravić Crljenica, M.; Perasso, R.; Imelio, M.; Viganoni, C.; Pozzan, L. A systematic and comprehensive protocol for rapid orthodontic extrusion. J. Esthet. Restor. Dent. 2024, 36, 838–844. [Google Scholar] [CrossRef]
- Tu, K.-W.; Kuo, C.-H.; Hung, C.-C.; Yan, D.-Y.; Mau, J.L.P. Strategic sequencing of orthodontic treatment and periodontal regenerative surgery: A literature review. J. Dent. Sci. 2025, 20, 1391–1397. [Google Scholar] [CrossRef]
- Feu, D. Orthodontic treatment of periodontal patients: Challenges and solutions, from planning to retention. Dent. Press J. Orthod. 2020, 25, 79–116. [Google Scholar] [CrossRef]
- Bazos, P.; Magne, P. Bio-emulation: Biomimetically emulating nature utilizing a histoanatomic approach; visual synthesis. Int. J. Esthet. Dent. 2014, 9, 330–352. [Google Scholar]
- Magne, P.B. Biomimetic Restorative Dentistry; Quintessence: Batavia, IL, USA, 2022; Volume 1, pp. 360–363. [Google Scholar]
- Dietschi, D.; Spreafico, R. Current clinical concepts for adhesive cementation of tooth-colored posterior restorations. Pract. Periodontics Aesthet. Dent. 1998, 10, 47–54. [Google Scholar]
- Magne, P.; Spreafico, R. Deep Margin Elevation: A Paradigm Shift. Am. J. Esthet. Dent. 2012, 2, 86–96. Available online: https://s3.amazonaws.com/kajabi-storefronts-production/sites/24049/themes/419830/downloads/uzJurSGFQvGCHAzU40tF_Deep_Margin_Elevation.pdf (accessed on 28 April 2025).
- Taylor, A.; Burns, L. Deep margin elevation in restorative dentistry: A scoping review. J. Dent. 2024, 146, 105066. [Google Scholar] [CrossRef]
- Kwon, T.; Lamster, I.B.; Levin, L. Current concepts in the management of periodontitis. Int. Dent. J. 2021, 71, 462–476. [Google Scholar] [CrossRef]
- Chun, E.P.; de Andrade, G.S.; Grassi, E.D.A.; Garaicoa, J.; Garaicoa-Pazmino, C. Impact of deep margin elevation procedures upon periodontal parameters: A systematic review. Eur. J. Prosthodont. Restor. Dent. 2023, 31, 10–21. [Google Scholar] [CrossRef]
- University of Derby. Literature Reviews: Systematic Searching at Various Levels. Available online: https://libguides.derby.ac.uk/literature-reviews/prisma-lr (accessed on 28 April 2025).
- Mugri, M.H.; Sayed, M.E.; Nedumgottil, B.M.; Bhandi, S.; Raj, A.T.; Testarelli, L.; Khurshid, Z.; Jain, S.; Patil, S. Treatment prognosis of restored teeth with crown lengthening vs. deep margin elevation: A systematic review. Materials 2021, 14, 6733. [Google Scholar] [CrossRef]
- Loguercio, A.D.; Alessandra, R.; Mazzocco, K.C.; Dias, A.L.; Busato, A.L.; Singer, J.D.M.; Rosa, P. Microleakage in class II composite resin restorations: Total bonding and open sandwich technique. J. Adhes. Dent. 2002, 4, 137–144. [Google Scholar]
- Spreafico, R.; Marchesi, G.; Turco, G.; Frassetto, A.; Di Lenarda, R.; Mazzoni, A.; Cadenaro, M.; Breschi, L. Evaluation of the in vitro effects of cervical marginal relocation using composite resins on the marginal quality of CAD/CAM crowns. J. Adhes. Dent. 2016, 18, 355–362. [Google Scholar] [CrossRef]
- Welbury, R.R.; Murray, J.J. A clinical trial of the glass-ionomer cement-composite resin “sandwich” technique in Class II cavities in permanent premolar and molar teeth. Quintessence Int. 1990, 6, 507–512. [Google Scholar]
- Andersson-Wenckert, I.E.; van Dijken, J.W.; Kieri, C. Durability of extensive Class II open-sandwich restorations with a resin-modified glass ionomer cement after 6 years. Am. J. Dent. 2004, 17, 43–50. [Google Scholar] [PubMed]
- Da Silva Gonçalves, D.; Cura, M.; Ceballos, L.; Fuentes, M.V. Influence of proximal box elevation on bond strength of composite inlays. Clin. Oral Investig. 2017, 21, 247–254. [Google Scholar] [CrossRef]
- Ferrari, M.; Koken, S.; Grandini, S.; Ferrari Cagidiaco, E.; Joda, T.; Discepoli, N. Influence of cervical margin relocation (CMR) on periodontal health: 12-month results of a controlled trial. J. Dent. 2018, 69, 70–76. [Google Scholar] [CrossRef]
- Ismail, E.H.; Ghazal, S.S.; Alshehri, R.D.; Albisher, H.N.; Albishri, R.S.; Balhaddad, A.A. Navigating the practical-knowledge gap in deep margin elevation: A step towards a structured case selection—A review. Saudi Dent. J. 2024, 36, 674–681. [Google Scholar] [CrossRef]
- Frese, C.; Wolff, D.; Staehle, H.J. Proximal box elevation with resin composite and the dogma of biological width: Clinical R2-technique and critical review. Oper. Dent. 2014, 39, 22–31. [Google Scholar] [CrossRef]
- Samartzi, T.K.; Papalexopoulos, D.; Ntovas, P.; Rahiotis, C.; Blatz, M.B. Deep margin elevation: A literature review. Dent. J. 2022, 10, 48. [Google Scholar] [CrossRef]
- Alizadeh Oskoee, P.; Dibazar, S. Deep margin elevation; indications and periodontal considerations. J. Adv. Periodontol. Implant Dent. 2024, 16, 91–93. [Google Scholar] [CrossRef]
- Eggmann, F.; Ayub, J.M.; Conejo, J.; Blatz, M.B. Deep margin elevation—Present status and future directions. J. Esthet. Restor. Dent. 2023, 35, 26–47. [Google Scholar] [CrossRef]
- Daghrery, A.; Jabarti, E.; Baras, B.H.; Mitwalli, H.; Al Moaleem, M.M.; Khojah, M.Z.; Khayat, W.; Albar, N.H. Impact of thermal aging on marginal adaptation in lithium disilicate CAD/CAM crowns with deep proximal box elevation. Med. Sci. Monit. 2025, 31, e947191. [Google Scholar] [CrossRef]
- Balci, Ş.N.; Tekçe, N.; Tuncer, S.; Demirci, M. The effect of different deep margin elevation methods on the fracture strength of CAD-CAM restorations. Am. J. Dent. 2024, 37, 115–120. [Google Scholar]
- Ismail, H.S.; Ali, A.I.; Elawsya, M.E. Influence of curing mode and aging on the bonding performance of universal adhesives in coronal and root dentin. BMC Oral Health 2024, 24, 1188. [Google Scholar] [CrossRef]
- Baldi, A.; Rossi, T.; Comba, A.; Monticone, L.; Paolone, G.; Sannino, I.; Vichi, A.; Goracci, C.; Scotti, N. Three-Dimensional Internal Voids and Marginal Adaptation in Deep Margin Elevation Technique: Efficiency of Highly Filled Flowable Composites. J. Adhes. Dent. 2024, 26, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Francois, P.; Attal, J.P.; Fasham, T.; Troizier-Cheyne, M.; Gouze, H.; Abdel-Gawad, S.; Le Goff, S.; Dursun, E.; Ceinos, R. Flexural Properties, Wear Resistance, and Microstructural Analysis of Highly Filled Flowable Resin Composites. Oper. Dent. 2024, 49, 597–607. [Google Scholar] [CrossRef]
- Bresser, R.A.; Carvalho, M.A.; Naves, L.Z.; Melma, H.; Cune, M.S.; Gresnigt, M.M.M. Biomechanical Behavior of Molars Restored with Direct and Indirect Restorations in Combination with Deep Margin Elevation. J. Mech. Behav. Biomed. Mater. 2024, 152, 106459. [Google Scholar] [CrossRef]
- Reddy, K.H.; Priya, B.D.; Malini, D.L.; Mohan, T.M.; Bollineni, S.; Gandhodi, H.C. Deep margin elevation in class II cavities: A comparative evaluation of microleakage and interface integrity using confocal laser microscopy and scanning electron microscopy. J. Conserv. Dent. Endod. 2024, 27, 529–534. [Google Scholar] [CrossRef]
- Baldi, A.; Comba, A.; Rossi, T.; Monticone, L.; Berutti, E.; Scotti, N. Effect of flowable viscosities on deep margin elevation: A microCT study. Dent. Mater. 2023, 39 (Suppl. 1), e69–e70. [Google Scholar] [CrossRef]
- Vichitgomen, J.; Srisawasdi, S. Deep margin elevation with resin composite and resin-modified glass-ionomer on marginal sealing of CAD-CAM ceramic inlays: An in vitro study. Am. J. Dent. 2021, 34, 327–332. [Google Scholar]
- Zhang, H.; Li, H.; Cong, Q.; Zhang, Z.; Du, A.; Wang, Y. Effect of proximal box elevation on fracture resistance and microleakage of premolars restored with ceramic endocrowns. PLoS ONE 2021, 16, e0252269. [Google Scholar] [CrossRef]
- Juloski, J.; Köken, S.; Ferrari, M. No correlation between two methodological approaches applied to evaluate cervical margin relocation. Dent. Mater. J. 2020, 39, 624–632. [Google Scholar] [CrossRef]
- Jawaed, N.U.; Abidi, S.Y.; Qazi, F.U.; Ahmed, S. An in-vitro evaluation of microleakage at the cervical margin between two different Class II restorative techniques using dye penetration method. J. Coll. Physicians Surg. Pak. 2016, 26, 748–752. [Google Scholar]
- Frankenberger, R.; Hehn, J.; Hajtó, J.; Krämer, N.; Naumann, M.; Koch, A.; Roggendorf, M.J. Effect of proximal box elevation with resin composite on marginal quality of ceramic inlays in vitro. Clin. Oral Investig. 2013, 17, 177–183. [Google Scholar] [CrossRef]
- De Mattos Pimenta Vidal, C.; Pavan, S.; Briso, A.L.; Bedran-Russo, A.K. Effects of three restorative techniques in the bond strength and nanoleakage at gingival wall of Class II restorations subjected to simulated aging. Clin. Oral Investig. 2013, 17, 627–633. [Google Scholar] [CrossRef]
- Lefever, D.; Gregor, L.; Bortolotto, T.; Krejci, I. Supragingival Relocation of Subgingivally Located Margins for Adhesive Inlays/Onlays with Different Materials. J. Adhes. Dent. 2012, 14, 561–567. [Google Scholar] [CrossRef]
- Roggendorf, M.J.; Krämer, N.; Dippold, C.; Vosen, V.E.; Naumann, M.; Jablonski-Momeni, A.; Frankenberger, R. Effect of proximal box elevation with resin composite on marginal quality of resin composite inlays in vitro. J. Dent. 2012, 40, 1068–1073. [Google Scholar] [CrossRef] [PubMed]
- De Goes, M.F.; Giannini, M.; Di Hipólito, V.; Carrilho, M.R.; Daronch, M.; Rueggeberg, F.A. Microtensile Bond Strength of Adhesive Systems to Dentin with or without Application of an Intermediate Flowable Resin Layer. Braz. Dent. J. 2008, 19, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Stockton, L.W.; Tsang, S.T. Microleakage of Class II posterior composite restorations with gingival margins placed entirely within dentin. J. Can. Dent. Assoc. 2007, 73, 255. [Google Scholar]
- Hausdörfer, T.; Lechte, C.; Kanzow, P.; Rödig, T.; Wiegand, A. Periodontal health in teeth treated with deep-margin-elevation and CAD/CAM partial lithium disilicate restorations—A prospective controlled trial. Clin. Oral Investig. 2024, 28, 670. [Google Scholar] [CrossRef]
- Adson, O.; Sarıkaya, T.Y.; Şükran, B. Margin Elevation for Posterior Indirect Restorations: 6-Month Clinical Outcomes. Int. Dent. J. 2024, 74 (Suppl. 1), S176. [Google Scholar] [CrossRef]
- Gözetici-Çil, B.; Öztürk-Bozkurt, F.; Genç-Çalışkan, G.; Yılmaz, B.; Aksaka, N.; Özcan, M. Clinical Performance of Posterior Indirect Resin Composite Restorations with the Proximal Box Elevation Technique: A Prospective Clinical Trial up to 3 Years. J. Adhes. Dent. 2024, 26, 19–30. [Google Scholar] [CrossRef]
- Aziz, A.M.; Suliman, S.; Sulaiman, T.A.; Abdulmajeed, A. Clinical and Radiographical Evaluation of CAD-CAM Crowns with and without Deep Margin Elevation: 10-Year Results. J. Prosthet. Dent. 2024, in press. [Google Scholar] [CrossRef]
- Cieplik, F.; Hiller, K.A.; Buchalla, W.; Federlin, M.; Scholz, K.J. Randomized clinical split-mouth study on a novel self-adhesive bulk-fill restorative vs. a conventional bulk-fill composite for restoration of class II cavities—Results after three years. J. Dent. 2022, 125, 104275. [Google Scholar] [CrossRef] [PubMed]
- Muscholl, C.; Zamorska, N.; Schoilew, K.; Sekundo, C.; Meller, C.; Büsch, C.; Wolff, D.; Frese, C. Retrospective Clinical Evaluation of Subgingival Composite Resin Restorations with Deep-Margin Elevation. J. Adhes. Dent. 2022, 24, 335–344. [Google Scholar] [CrossRef] [PubMed]
- Bertoldi, C.; Monari, E.; Cortellini, P.; Generali, L.; Lucchi, A.; Spinato, S.; Zaffe, D. Clinical and histological reaction of periodontal tissues to subgingival resin composite restorations. Clin. Oral Investig. 2020, 24, 1001–1011. [Google Scholar] [CrossRef]
- Bresser, R.A.; Gerdolle, D.; van den Heijkant, I.A.; Sluiter-Pouwels, L.M.A.; Cune, M.S.; Gresnigt, M.M.M. Up to 12 years clinical evaluation of 197 partial indirect restorations with deep margin elevation in the posterior region. J. Dent. 2019, 91, 103227. [Google Scholar] [CrossRef]
- Oppermann, R.V.; Gomes, S.C.; Cavagni, J.; Cayana, E.G.; Conceição, E.N. Response to proximal restorations placed either subgingivally or following crown lengthening in patients with no history of periodontal disease. Int. J. Periodontics Restor. Dent. 2016, 36, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Ismail, H.S.; Ali, A.I.; Mehesen, R.E.; Juloski, J.; Garcia-Godoy, F.; Mahmoud, S.H. Deep proximal margin rebuilding with direct esthetic restorations: A systematic review of marginal adaptation and bond strength. Restor. Dent. Endod. 2022, 47, e15. [Google Scholar] [CrossRef]
- Plotino, G.; Abella Sans, F.; Duggal, M.S.; Grande, N.M.; Krastl, G.; Nagendrababu, V.; Gambarini, G. Present Status and Future Directions: Surgical Extrusion, Intentional Replantation and Tooth Autotransplantation. Int. Endod. J. 2022, 55 (Suppl. 3), 827–842. [Google Scholar] [CrossRef]
- Juloski, J.; Köken, S.; Ferrari, M. Cervical Margin Relocation in Indirect Adhesive Restorations: A Literature Review. J. Prosthodont. Res. 2018, 62, 273–280. [Google Scholar] [CrossRef]
- Sarfati, A.; Tirlet, G. Deep Margin Elevation versus Crown Lengthening: Biologic Width Revisited. Int. J. Esthet. Dent. 2018, 13, 334–356. [Google Scholar] [PubMed]
- Dablanca-Blanco, A.B.; Blanco-Carrión, J.; Martín-Biedma, B.; Varela-Patiño, P.; Bello-Castro, A.; Castelo-Baz, P. Management of Large Class II Lesions in Molars: How to Restore and When to Perform Surgical Crown Lengthening? Restor. Dent. Endod. 2017, 42, 240–252. [Google Scholar] [CrossRef]
- Veneziani, M. Adhesive Restorations in the Posterior Area with Subgingival Cervical Margins: New Classification and Differentiated Treatment Approach. Eur. J. Esthet. Dent. 2010, 5, 50–76. [Google Scholar]
- Padbury, A., Jr.; Eber, R.; Wang, H.L. Interactions between the gingiva and the margin of restorations. J. Clin. Periodontol. 2003, 30, 379–385. [Google Scholar] [CrossRef]
- Butt, A. Cervical margin relocation and indirect restorations: Case report and literature review. Dent. Update 2021, 48, 93–97. [Google Scholar] [CrossRef]
- Ghezzi, C.; Brambilla, G.; Conti, A.; Dosoli, R.; Ceroni, F.; Ferrantino, L. Cervical margin relocation: Case series and new classification system. Int. J. Esthet. Dent. 2019, 14, 272–284. [Google Scholar] [PubMed]
- Wu, F.; Su, X.; Shi, Y.; Bai, J.; Feng, J.; Sun, X.; Wang, X.; Wang, H.; Wen, J.; Kang, J. Comparison of the Biomechanical Effects of the Post-Core Crown, Endocrown and Inlay Crown after Deep Margin Elevation and Its Clinical Significance. BMC Oral Health 2024, 24, 990. [Google Scholar] [CrossRef]
- Mahmoudi Yamchi, F.; Abbasi, M.; Atri, F.; Ahmadi, E. Influence of Deep Margin Elevation Technique with Two Restorative Materials on Stress Distribution of e.max Endocrown Restorations: A Finite Element Analysis. Int. J. Dent. 2024, 2024, 6753069. [Google Scholar] [CrossRef]
- Magne, P.; Mori Ubaldini, A.L. Thermal and bioactive optimization of a unidose 3-step etch-and-rinse dentin adhesive. J. Prosthet. Dent. 2020, 124, 487.e1–487.e7. [Google Scholar] [CrossRef]
- Kuper, N.K.; Opdam, N.J.; Bronkhorst, E.M.; Huysmans, M.C. The influence of approximal restoration extension on the development of secondary caries. J. Dent. 2012, 40, 241–247. [Google Scholar] [CrossRef]
- Amesti-Garaizabal, A.; Agustín-Panadero, R.; Verdejo-Solá, B.; Fons-Font, A.; Fernández-Estevan, L.; Montiel-Company, J.; Solá-Ruíz, M.F. Fracture resistance of partial indirect restorations made with CAD/CAM technology: A systematic review and meta-analysis. J. Clin. Med. 2019, 8, 1932. [Google Scholar] [CrossRef]
- Ölçer Us, Y.; Aydınoğlu, A.; Erşahan, Ş.; Erdem Hepşenoğlu, Y.; Sağır, K.; Üşümez, A. A Comparison of the Effects of Incremental and Snowplow Techniques on the Mechanical Properties of Composite Restorations. Aust. Dent. J. 2024, 69, 40–48. [Google Scholar] [CrossRef]
- Guo, J.; Wang, Z.; Li, X.; Sun, C.; Gao, E.; Li, H. A Comparison of the Fracture Resistances of Endodontically Treated Mandibular Premolars Restored with Endocrowns and Glass Fiber Post-Core Retained Conventional Crowns. J. Adv. Prosthodont. 2016, 8, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Van Dijken, J.W.; Sjöström, S.; Wing, K. The Effect of Different Types of Composite Resin Fillings on Marginal Gingiva. J. Clin. Periodontol. 1987, 14, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Reichardt, E.; Krug, R.; Bornstein, M.M.; Tomasch, J.; Verna, C.; Krastl, G. Orthodontic Forced Eruption of Permanent Anterior Teeth with Subgingival Fractures: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 12580. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).