Abstract
Background: This study represents the first registry to assess patients’ clinical characteristics and key predictors of 30-day post-cardiovascular surgery mortality in wartime Yemen. Methods: This study retrospectively analyzed 2169 patients who underwent cardiac surgery. Comprehensive patient data were extracted from Nabdh Al-Hayat Cardiac Center registries across Hadhramaut Governorate, Republic of Yemen, over 7 years from 2018 to 2024. Results: The study cohort comprised predominantly adult patients, with 69% aged 18 years and above, while 31% were under 18 years of age. The overall survival rate was high (95%), yet 5% of the patients experienced 30-day postoperative mortality. Cold cardioplegia and certain solution types were associated with increased mortality. Heart failure and ventricular dysfunction accounted for most mortality, though non-cardiac factors, such as cerebral hemorrhage and multi-organ failure, contributed as well. Conclusions: While Yemen’s crises have devastated healthcare delivery, the 30-day postoperative mortality data highlight the resilience of coordinated efforts. However, current standards remain far from universal benchmarks, highlighting the urgent need to rebuild local capacity and ensure equitable access to cardiac surgical services nationwide.
1. Introduction
Regrettably, neglecting cardiac surgery directly impedes global efforts to reduce the burden of cardiovascular disease (CVD), a leading contributor to worldwide non-communicable disease morbidity and mortality, especially in conflict zones [1,2].
The ongoing conflict in Yemen, which began in late 2014, has precipitated one of the world’s most severe humanitarian crises, profoundly impacting the nation’s healthcare system and heart disease management, including the provision of cardiac surgery [3,4].
Yemen’s protracted civil war has devastated its healthcare infrastructure, leaving only about half of the pre-war hospitals and health facilities functional [3]. The destruction of medical facilities, severe shortages of healthcare workers, and frequent attacks on hospitals have undermined the delivery of essential health services [4]. Humanitarian aid is often impeded by blockades and insecurity, exacerbating the population’s vulnerability to disease and limiting access to specialized care [5]. A recent study conducted in Sanaa, the Capital of the Yemeni Republic, reported four primary cardiovascular comorbidities: hypertensive heart disease (HHD: 26.42%), valvular heart disease (VHD: 22.44%), HFrEF (19.67%), and ischemic heart disease (IHD: 16.99%). Congenital heart defects (CHDs) affected 2.0% patients, with ASD (30.89%) and VSD (22.76%) being the most common. Among valvular pathologies, rheumatic heart disease (RHD) predominated (51.10%), followed by senile degenerative lesions (26.99%) and mitral valve prolapse (21.90%). Mitral insufficiency (20%) represented the most prevalent VHD subtype, while aortic insufficiency (19.10%), tricuspid insufficiency (4.60%), mitral stenosis (3.40%), and aortic stenosis (1.80%) demonstrated declining frequency [6].
The ongoing conflict and systemic weaknesses in Yemen severely constrain the provision of cardiac surgery. There is a chronic shortage of specialized medical staff, surgical supplies, and functioning equipment, with many hospitals lacking even basic medications and devices [7]. Yemen’s healthcare infrastructure has been devastated by years of conflict, with only 50% of the hospitals functional and severe shortages of specialists, equipment, and funding [8].
In Yemen, no formal registries or outcome analyses existed for cardiac interventions. Therefore, a reliable system to systematically record patient demographics and clinical data does not exist, representing a gap that impedes evidence-based practice in a nation where cardiovascular disease is a leading cause of death. This is the first registry to assess patient clinical data and cardiovascular surgery outcomes during wartime Yemen, reflecting the current situation.
2. Materials and Methods
This retrospective study included all patients who underwent cardiovascular surgical procedures during a seven-year period (2018–2024). These interventions were delivered as part of a coordinated cardiac care initiative led by the King Salman Humanitarian Aid and Relief Center, Saudi Arabia, in collaboration with the Nabdh Al-Hayat Cardiac Center under the supervision of the Yemeni Ministry of Health.
Data were obtained from a prospectively maintained institutional registry that systematically records demographic, clinical, procedural, and outcome variables for all eligible patients at the time of admission and throughout follow-up.
Comprehensive patient data were collected, including demographics, clinical histories, surgical procedures, body surface area (BSA) in square meters, ejection fraction, aortic x-clamp, and aortic cross clamp time in minutes.
Oxygen partial pressure (PO2) pre-cardiopulmonary bypass (CPB) off [refers to the PO2 measured immediately before discontinuation of CPB, after rewarming and re-establishing cardiac activity, but before aortic decannulation, obtained from arterial blood gas analysis using a standardized point-of-care analyzer from a radial or femoral arterial line], cardioplegia temperature, and recovery outcomes were extracted.
During data extraction, all variables were cross-checked for internal consistency and to ensure that no missing values were present. Cases with incomplete essential data, such as operative details or postoperative survival status, were re-examined using operative logs and mortality records. When verification was not possible (affecting fewer than 2% of the records), the respective variables were coded as “unknown” and excluded from variable-specific analyses but retained for overall demographic summaries. This approach ensured that the dataset represented a consecutive, high-fidelity record of all eligible cardiac surgery cases performed during the study period.
Clinically, this study includes all patients who suffered from heart diseases requiring cardiac surgical intervention. This includes patients with ischemic heart disease, mitral valve disease, aortic valve disease, tricuspid valve disease, thoracic aortic lesions, such as ascending aortic aneurysm, and aortic dissections. Patients with cardiac tumors, such as cardiac myxoma, or adults with CHDs, were also included in the analysis.
The overall 30-day mortality rate was identified using hospital records and postoperative follow-up visits, as well as phone call follow-ups when a patient did not attend the clinic after surgery. Outpatient records were reviewed to determine survival status.
The cardiac surgical procedures performed included the following (elective as well as emergency): coronary artery bypass grafting (CABG), mitral valve repair or replacement, aortic valve replacement, and tricuspid valve repair or replacement, mainly combined with mitral valve surgery, especially in patients with rheumatic heart disease.
Analyses
Statistical analyses were performed using IBM SPSS Statistics, Version 26 (Armonk, NY, USA). Continuous variables were assessed for normality via Shapiro–Wilk tests and are presented as mean ± standard deviation. Group comparisons were used to examine relationships with 30-day mortality. We used independent T-tests for continuous data and chi-square tests for categorical variables. Binary logistic regression was used to identify predictors of 30-day mortality. Odds ratios (ORs) and adjusted odds ratios (Os) with 95% confidence intervals were reported. Model calibration was evaluated using the Hosmer–Lemeshow goodness-of-fit test, and model discrimination was assessed by the area under the ROC curve (AUC). Collinearity among independent variables was examined using Variance Inflation Factors (VIFs) and tolerance values, with all VIFs < 2.0. Variables with p < 0.20 on univariate analysis or deemed clinically relevant were entered into the multivariable model. A backward stepwise selection method was used to identify independent predictors, controlling for confounding effects. Statistical significance was defined as a two-tailed p-value < 0.05.
A multivariable binary logistic regression model was constructed to identify predictors of 30-day mortality. Candidate variables were selected based on clinical relevance and the prior literature, including age, sex, BSA, ejection fraction (EF%), aortic cross-clamp time, total cardiopulmonary bypass (CPB) duration, reperfusion time, PO2 pre-CPB, cardioplegia type and temperature (warm, cold, none), and CP solution (MICS “Minimally Invasive Cardiac Surgery”, Myotherm, Custodiol, or del Nido). Continuous variables were examined for linearity in the logit using the Box–Tidwell test; non-linear terms were transformed or categorized when appropriate. Multicollinearity was assessed using Variance Inflation Factors, with a threshold of <5 considered acceptable. Model diagnostics included assessing the overall model fit using the Hosmer–Lemeshow goodness-of-fit test and observed probabilities. Sensitivity analyses were performed by excluding variables with >10% missing data and by testing alternate cardioplegia groupings. Statistical significance was set at p < 0.05.
3. Results
3.1. Demographic Data
The patients’ demographic and basic data are presented in Table 1.

Table 1.
Baseline demographic clinical characteristics.
A total of 2169 patients who underwent cardiovascular surgery were included in this analysis. The majority (2064; 95%) survived, while 105 (5%) experienced 30-day postoperative mortality, as depicted in Figure 1. The study cohort comprised predominantly adult patients, with 69% (n = 1496) aged 18 years and above, while 31% (n = 673) were under 18 years of age. This distribution indicates that most cardiovascular surgical interventions were performed in adults, although a notable proportion of late adolescent and younger patients also underwent surgery (Figure 1).
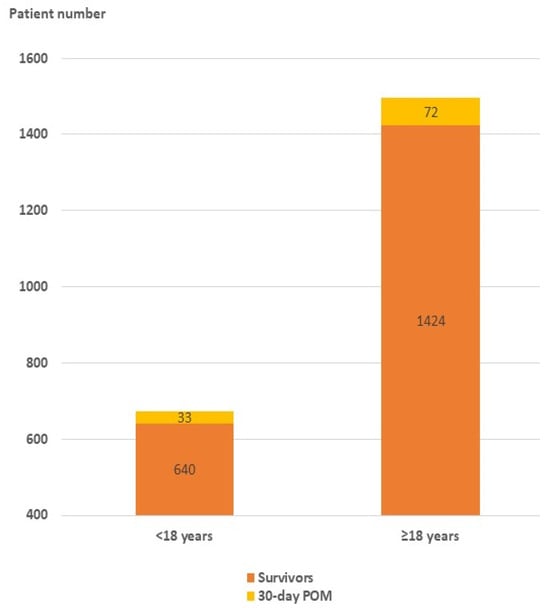
Figure 1.
Distribution of survivors and 30-day postoperative mortality by age group among the study cohort (n = 2169). POM: postoperative mortality.
Among the total patients included in this study, IHD represented the most prevalent comorbidity, accounting for 39% (n = 844) of all cases. This was followed by CHD at 38% (n = 827), RHD at 18% (n = 392), and compound comorbidities (CCs) at 5% (n = 106), as presented in Figure 2.
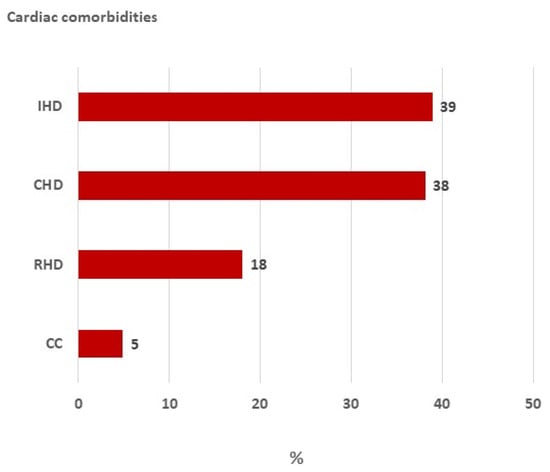
Figure 2.
Distribution of cardiac comorbidities among the patients included in this study. CC: compound comorbidity; RHD: rheumatic heart disease; CHD: congenital heart disease; IHD: ischemic heart disease.
3.2. Causes of Mortality
The leading cause of 30-day postoperative mortality was heart failure, observed in 57 (54%) of non-survivors. Heart failure was defined as clinical and echocardiographic evidence of inadequate cardiac output despite maximal pharmacologic and mechanical support. Among these, right ventricular failure, characterized by right-sided dilatation with elevated central venous pressure and low cardiac output, accounted for 11 (10%), whereas left ventricular failure, identified by reduced left ventricular EF with pulmonary congestion and low systemic perfusion, contributed to 9 (9%) deaths. Combined biventricular dysfunction was present in eight (8%) cases. Multi-organ failure, defined as the concurrent dysfunction of at least two vital organ systems (e.g., renal, hepatic, respiratory, or neurologic) following circulatory collapse or sepsis, was responsible for seven (7%) deaths. Less frequent causes included cerebral hemorrhage (diagnosed by imaging or post-mortem confirmation of intracranial bleeding), circulatory failure (persistent hypotension unresponsive to vasoactive therapy), aortic arch tearing with massive bleeding, circulatory arrest after extubation, air embolism, apnea, pulmonary edema, and other miscellaneous causes, collectively accounting for 13 (12%) deaths (Figure 3).
3.3. Clinical and Intraoperative Variables Associated with Mortality
Mortality was significantly associated with patient sex (p = 0.01), with a relatively higher proportion of deaths among female patients compared to males. The type of cardioplegia temperature used (warm vs. cold) showed a statistically significant association with survival (p < 0.001): patients managed with cold cardioplegia demonstrated increased mortality compared to those managed with warm cardioplegia. Similarly, different cardioplegia solutions (MICS, MYOtherm, Custodiol, del Nido, and none) were associated with significantly different survival outcomes (p < 0.001). Notably, a higher percentage of deaths was observed in patients administered Custodiol and NidoMic solutions (Table 2).

Table 2.
Clinical and intraoperative variables associated with mortality following cardiovascular surgery.
Non-survivors were considerably younger (mean age: 18.2 ± 2.4 years) than survivors (36.2 ± 0.5 years, p < 0.001) and demonstrated significantly lower body weight and BSA (p < 0.001 for both). Non-survivors also exhibited longer aortic cross-clamp times (107.6 ± 7.1 vs. 71.5 ± 0.9 min, p < 0.001) and total bypass times (190.3 ± 16.6 vs. 103.9 ± 1.1 min, p < 0.001), as well as prolonged reperfusion times (26.3 ± 0.2 vs. 12.2 ± 0.2 min, p < 0.001). The mean cardioplegia temperature in non-survivors was significantly lower (30.0 ± 0.3 °C) compared to survivors (31.5 ± 0.1 °C, p < 0.001). No significant differences were observed between the groups in pre-bypass PO2 or EF (Table 2).
3.4. Clinical Variables Predicting Mortality in Post-Cardiovascular Surgical Patients
BSA emerged as a strong protective factor, with a significantly lower odds ratio (OR: 0.008, 95% CI: 0.001–0.057; p < 0.001), suggesting that patients with higher BSA were notably less likely to experience mortality. In contrast, increased PO2 pre-CPB off was independently associated with a higher risk of death (OR: 1.03, 95% CI: 1.02–1.10; p < 0.001). Aortic cross-clamp duration showed a significant association with postoperative mortality (OR = 0.98, 95% CI = 0.97–0.99, p = 0.01), indicating that for every additional minute of cross-clamp time, the odds of 30-day mortality increased by approximately 2%. Patient age and weight modestly influenced risk (OR: 1.0, 95% CI: 1.00–1.1; p = 0.01). However, ejection fraction, total bypass time, reperfusion time, and cardioplegia temperature were not independently associated with mortality on multivariate analysis, as their respective odds ratios were not statistically significant (Table 3).

Table 3.
Clinical predictors of mortality following cardiovascular surgery.
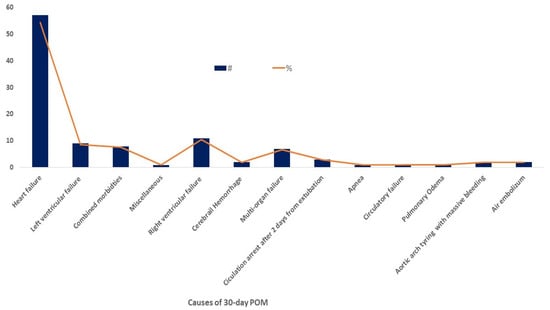
Figure 3.
Causes of 30-day postoperative mortality among patients who underwent cardiovascular surgery. POM: postoperative mortality; #: Number of patients; %: Percentage of patients.
4. Discussion
To the best of our knowledge, the present study represents the first registry to evaluate cardiovascular surgery outcomes during wartime in Yemen. Despite Yemen’s protracted conflict, political instability, and economic collapse, our findings reaffirm the high overall survival rate in contemporary cardiovascular surgical practice (95%), within the range of the 3–5% benchmark reported recently in high-resource centers [9,10].
Regarding the etiology of mortality, cardiac complications, predominantly heart failure, right and left ventricular failure, and combined comorbidities, were the leading causes of death, echoing previous registries that highlight cardiac dysfunction as the chief determinant of early mortality after cardiac surgery [11]. Non-cardiac causes, including cerebral hemorrhage, multi-organ failure, and circulatory failure, also contributed, reflecting the complex interplay of perioperative insults.
In our cohort, non-survivors experienced markedly longer bypass and cross-clamp durations than survivors. This finding is congruent with reports demonstrating that extended CPB and ischemic intervals precipitate systemic inflammatory responses, coagulopathy, and multi-organ dysfunction [12]. Notably, our study further identified prolonged reperfusion time as being strongly associated with 30-day postoperative mortality in univariate analysis, aligning with the notion that delayed myocardial recovery increases vulnerability to low cardiac output and multi-organ failure [13].
Gender, and the type and temperature of the cardioplegia solution also influenced the outcomes. Females, and those who received cold cardioplegia and Custodiol or del Nido solutions demonstrated significantly higher mortality. In agreement with our study, a report comparing Custodiol, del Nido, and blood cardioplegia found no significant differences in in-hospital or 30-day mortality rates between Custodiol, del Nido, and blood cardioplegia, with Custodiol having a slightly higher probability of being ranked the first mortality factor [14].
This finding may be related to differences in patient selection, operative complexity, ischemic duration, or perfusion temperature management, especially in a conflict zone, rather than the cardioplegic temperature alone.
Cold cardioplegia leads to superior myocardial preservation and potentially improved survival, particularly in high-risk or prolonged ischemic procedures. Earlier reports proposed that hypothermia reduces myocardial oxygen demand and limits ischemic injury, leading to better myocardial protection. Although several studies have found a similar incidence of postoperative outcomes [15,16], our study demonstrated higher myocardial-related mortality among patients who received cold cardioplegia compared with those who received warm solutions. These distinctive findings may reflect the influence of the conflict-affected healthcare environment in which this study was conducted. In such settings, intermittent power supply, limited perfusion equipment, inconsistent temperature control, and restricted access to specialized cardioplegic solutions can affect both the administration and efficacy of myocardial protection strategies. Additionally, conflict-affected zones often experience delayed presentations, advanced disease stages, and reduced postoperative care continuity, which can obscure the marginal benefits of one cardioplegic strategy over another. The variability in surgical team composition and infrastructure, common in humanitarian or transitional care systems, may further contribute to the observed diversity in outcomes [17,18].
However, regarding safety outcomes, current evidence indicates that selecting warm versus cold cardioplegia can be based on surgeon preference, as neither method has demonstrated a clear superiority in mortality risk [16].
Aortic cross-clamp duration and PO2 before off CPB were also independently associated with increased mortality, consistent with the established literature [19].
Interestingly, while advanced age and body weight are frequently cited as risk factors [20], our cohort’s relatively young mean age and low body weight may serve as a predictor of post-cardiovascular surgery. Studies show that younger age, particularly in the pediatric population, is associated with longer postoperative hospital stays and potentially more challenging recovery. In a cohort comparing children undergoing cardiac surgeries before and after 4 months of age, those who were younger at surgery had a significantly longer adjusted mean length of hospital stay, even after adjusting for other relevant variables [21]. Multiple studies demonstrate that low body weight or a low body mass index (BMI) is independently associated with increased risks after cardiovascular surgery. A low BMI is linked to higher rates of postoperative complications, longer mechanical ventilation, prolonged intensive care, and increased in-hospital and long-term mortality. For example, infants with low body weight, especially those under 2.2 kg, have a higher risk of ICU morbidity and hospital mortality compared to those of normal weight. Similarly, adult and pediatric studies consistently report that underweight or low-BMI patients face higher odds of adverse outcomes, including unplanned readmission and need for further interventions within a year following surgery [22,23].
5. Conclusions
Working in a conflict-affected setting like Yemen is extremely difficult. Yet, thanks to the strong commitment and wide experience of the cardiology team gained through both national and international collaborations, this system was successfully established. We hope that this effort will support the center’s growth and improve the cardiovascular healthcare quality in Yemen. In summary, our findings emphasize body habitus, bypass and ischemic durations, and cardioplegia strategy as pivotal determinants of early mortality after cardiovascular surgery. These results are broadly in line with major established studies and meta-analyses, underscoring the need for tailored perioperative management in high-risk groups, especially in a conflict zone.
Limitations
This study has some limitations that should be mentioned. Being retrospective and conducted at a single center, the findings may reflect local practices and patient characteristics, which could limit their broad applicability to other settings. The lack of extended follow-up data also prevents assessment of long-term outcomes or late complications. Moreover, the absence of international or multicenter comparisons reduces the ability to generalize results across diverse healthcare systems. Despite these limitations, this study offers valuable and context-specific evidence, highlighting important trends and clinical insights within a challenging research environment.
Author Contributions
A.A.S., A.M., T.B., E.A. and Y.E.: conceptualization, study design, investigation, and data collection. M.A.-H.: manuscript preparation and data analysis. Y.E.: manuscript revision. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding. The article processing charge (APC) was funded by the authors.
Institutional Review Board Statement
The Ministry of Health, Republic of Yemen, through its Institutional Review Board (MOH-IRB-2024-01, 3 June 2025), formally approved this study. This study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki and its subsequent amendments.
Informed Consent Statement
As this was a retrospective chart review of de-identified patient records, the requirement for individual informed consent was formally waived by the IRB in accordance with national and institutional regulations. This study involved no direct patient contact or intervention, and all data were handled strictly for research purposes.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Jawad, M.; Vamos, E.P.; Najim, M.; Roberts, B.; Millett, C. Impact of Armed Conflict on Cardiovascular Disease Risk: A Systematic Review. Heart 2019, 105, 1388–1394. [Google Scholar] [CrossRef]
- Roth, G.A.; Johnson, C.; Abajobir, A.; Abd-Allah, F.; Abera, S.F.; Abyu, G.; Ahmed, M.; Aksut, B.; Alam, T.; Alam, K.; et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017, 70, 1–25. [Google Scholar] [CrossRef]
- Alsabri, M.; Alsakkaf, L.M.; Alhadheri, A.; Cole, J.; Burkle, F.M. Chronic Health Crises and Emergency Medicine in War-Torn Yemen, Exacerbated by the COVID-19 Pandemic. West. J. Emerg. Med. 2022, 23, 276–284. [Google Scholar] [CrossRef] [PubMed]
- Ripoll Gallardo, A.; Burkle, F.M.; Ragazzoni, L.; Della Corte, F. Yemen’s Unprecedented Humanitarian Crisis: Implications for International Humanitarian Law, the Geneva Convention, and the Future of Global Health Security. Disaster Med. Public Health Prep. 2016, 10, 701–703. [Google Scholar] [CrossRef] [PubMed]
- Salem, A.; Rosen, A.; Alharazi, I.; Gamallat, Y.; Aldbyani, A.; Amer, B.; Chimpandu, N. Healthcare Accessibility in Yemen’s Conflict Zones: Comprehensive Review Focused on Strategies and Solutions. Confl. Health 2025, 19, 42. [Google Scholar] [CrossRef]
- Jayed, D.; Al-Huthi, M.A.; Al-Zandani, A.; Al-Shuki, S.; Al-Dholae, M.; Al-Moqri, M. Spectrum of Heart Diseases in Sanaa, Capital of Yemen Republic. Open Access Libr. J. 2023, 10, 1–14. [Google Scholar] [CrossRef]
- Mohamed Ibrahim, M.I.; Alshakka, M.; Al-abd, N.; Bahattab, A.; Badulla, W. Availability of Essential Medicines in a Country in Conflict: A Quantitative Insight from Yemen. Int. J. Environ. Res. Public Health 2021, 18, 175. [Google Scholar] [CrossRef]
- Munibari, A.-N.; Alansi, A.K.; Al-Jaber, N.; Hidar, F.; Al-Kadi, A.-A. The Economic Burden of Cardiovascular Diseases in Yemen: An Example of Annual Direct Costs from the Cardiac Center–Althawra Teaching General Hospital- Sana’a. Hadhramout J. Med. Sci. 2014, 3, 253–258. [Google Scholar]
- Silva-Tejada, H.; Sisniegas-Razón, J.; Martínez-Ninanqui, F.; Díaz-Chávez, Z.; Ríos-Ortega, J.C. Perioperative morbidity and mortality of cardiac surgeries at the Instituto Nacional Cardiovascular, Lima, Peru, during the year 2023. Arch. Peru. Cardiol. Cir. Cardiovasc. 2025, 6, 36–43. [Google Scholar] [CrossRef]
- Siregar, S.; Groenwold, R.H.H.; de Mol, B.A.J.M.; Speekenbrink, R.G.H.; Versteegh, M.I.M.; Brandon Bravo Bruinsma, G.J.; Bots, M.L.; van der Graaf, Y.; van Herwerden, L.A. Evaluation of Cardiac Surgery Mortality Rates: 30-Day Mortality or Longer Follow-Up? Eur. J. Cardiothorac. Surg. 2013, 44, 875–883. [Google Scholar] [CrossRef] [PubMed]
- Vogt, A.; Grube, E.; Glunz, H.G.; Hauptmann, K.E.; Sechtem, U.; Mäurer, W.; Tebbe, U.; Heinrich, K.W.; Engel, H.J.; Kettner, W.; et al. Determinants of Mortality after Cardiac Surgery: Results of the Registry of the Arbeitsgemeinschaft Leitender Kardiologischer Krankenhausärzte (ALKK) on 10 525 Patients. Eur. Heart J. 2000, 21, 28–32. [Google Scholar] [CrossRef]
- Squiccimarro, E.; Stasi, A.; Lorusso, R.; Paparella, D. Narrative Review of the Systemic Inflammatory Reaction to Cardiac Surgery and Cardiopulmonary Bypass. Artif. Organs 2022, 46, 568–577. [Google Scholar] [CrossRef] [PubMed]
- Aladwan, H.; Alshoubaki, W.; Alqaisi, A.I.; Abuamereh, H.A.; Alatoum, L.M.; Mohd, A.F. Impact of Duration of Cardiopulmonary Bypass on Recovery after Open Heart Surgery. Int. J. Adv. Med. 2024, 11, 185–188. [Google Scholar] [CrossRef]
- Chan, J.; Oo, S.; Butt, S.; Benedetto, U.; Caputo, M.; Angelini, G.D.; Vohra, H.A. Network Meta-Analysis Comparing Blood Cardioplegia, Del Nido Cardioplegia and Custodiol Cardioplegia in Minimally Invasive Cardiac Surgery. Perfusion 2023, 38, 464–472. [Google Scholar] [CrossRef] [PubMed]
- Abah, U.; Roberts, P.G.; Ishaq, M.; De Silva, R. Is Cold or Warm Blood Cardioplegia Superior for Myocardial Protection? Interact. Cardiovasc. Thorac. Surg. 2012, 14, 848–855. [Google Scholar] [CrossRef]
- Kot, T.K.M.; Chan, J.S.K.; Froghi, S.; Lau, D.H.H.; Morgan, K.; Magni, F.; Harky, A. Warm versus Cold Cardioplegia in Cardiac Surgery: A Meta-Analysis with Trial Sequential Analysis. JTCVS Open 2021, 6, 161–190. [Google Scholar] [CrossRef] [PubMed]
- Mve Mvondo, C.; Giamberti, A.; Ngowe Ngowe, M.; Mbuoh, H.A.; Milocco, I.; Tsague Kengni, H.N.; Cirri, S.; Frigiola, A. Cardiac Surgery Development in Cameroon: Unexpected Challenges From a Socio-Political Crisis. Front. Cardiovasc. Med. 2022, 9, 778075. [Google Scholar] [CrossRef]
- Slusher, T.M.; Kiragu, A.W.; Day, L.T.; Bjorklund, A.R.; Shirk, A.; Johannsen, C.; Hagen, S.A. Pediatric Critical Care in Resource-Limited Settings-Overview and Lessons Learned. Front. Pediatr. 2018, 6, 49. [Google Scholar] [CrossRef]
- Salsano, A.; Giacobbe, D.R.; Sportelli, E.; Olivieri, G.M.; Natali, R.; Prevosto, M.; Del Bono, V.; Viscoli, C.; Santini, F. Aortic Cross-Clamp Time and Cardiopulmonary Bypass Time: Prognostic Implications in Patients Operated on for Infective Endocarditis. Interact. Cardiovasc. Thorac. Surg. 2018, 27, 328–335. [Google Scholar] [CrossRef]
- Zhang, Y.; Zheng, Q.; Dai, X.; Xu, X.; Ma, L. Overweight Is Associated with Better One-Year Survival in Elderly Patients after Cardiac Surgery: A Retrospective Analysis of the MIMIC-III Database. J. Thorac. Dis. 2021, 13, 562. [Google Scholar] [CrossRef]
- Koth, A.M.; Algaze, C.A.; Sakarovitch, C.; Long, J.; Kamra, K.; Wright, G.E.; Alexander-Banys, B.; Maeda, K.; Shin, A.Y. Younger Age Remains a Risk Factor for Prolonged Length of Stay after Bidirectional Cavopulmonary Anastomosis. Cardiol. Young 2019, 29, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Mehmood, A.; Ismail, S.R.; Kabbani, M.S.; Abu-Sulaiman, R.M.; Najm, H.K. Outcome of Low Body Weight (<2.2 Kg) Infants Undergoing Cardiac Surgery. J. Saudi Heart Assoc. 2014, 26, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Potapov, E.V.; Loebe, M.; Anker, S.; Stein, J.; Bondy, S.; Nasseri, B.A.; Sodian, R.; Hausmann, H.; Hetzer, R. Impact of Body Mass Index on Outcome in Patients after Coronary Artery Bypass Grafting with and without Valve Surgery1. Eur. Heart J. 2003, 24, 1933–1941. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).