Journal Description
Emergency Care and Medicine
Emergency Care and Medicine
is an international, peer-reviewed, open access journal on advancements and developments in emergency medical services, emergency medicine, acute internal medicine, and acute care surgery practice, theory, nursing, training, and education published quarterly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 18.9 days after submission; acceptance to publication is undertaken in 5.5 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names are published annually in the journal.
- Emergency Care and Medicine is a companion journal of Biomedicines.
Latest Articles
Anthropometric Characteristics and Fitness Status of Emergency Medical Services (EMS) Personnel
Emerg. Care Med. 2025, 2(4), 50; https://doi.org/10.3390/ecm2040050 - 19 Oct 2025
Abstract
Background/Objectives: This study aimed to assess the anthropometric and body composition characteristics, blood profiles and fitness-related parameters of emergency medical services (EMS) professionals. Methods: A total of 39 EMS professionals participated in the study, consisting of 18 males (age: 37.78 ±
[...] Read more.
Background/Objectives: This study aimed to assess the anthropometric and body composition characteristics, blood profiles and fitness-related parameters of emergency medical services (EMS) professionals. Methods: A total of 39 EMS professionals participated in the study, consisting of 18 males (age: 37.78 ± 10.62 years, height 180.87 ± 6.00 cm, weight 105.42 ± 25.40 kg) and 21 females (age: 33.05 ± 7.44 years, height 167.29 ± 3.89 cm, weight 90.63 ± 21.20 kg). The testing included anthropometric measurements, blood profiling, handgrip and low back strength assessments, vertical jump evaluation, flexibility testing, sit-up and push-up assessments, as well as timed performance measurements for a 300 m sprint and a 1.5-mile run. Results: According to the body mass index (BMI), 41% of the EMS professionals were classified as obese. Self-reported data indicated a smoking prevalence of 23%, while diabetes (n = 3), asthma (n = 2), and hypertension (n = 2) were also reported. Our results reveal that a great proportion of EMS professionals demonstrated suboptimal body composition and performance levels, with many failing to meet recommended health and performance standards. Elevated BMI, waist and hip circumferences, and body fat percentages were observed, along with relatively low performance in the strength and endurance tests. Conclusions: These findings highlight the need for targeted interventions among EMS professionals, who are expected to maintain adequate levels of aerobic capacity, flexibility, muscular strength and endurance.
Full article
Open AccessArticle
Pharmacist Review of Medicines Following Ambulance-Attended Falls—A Multi-Methods Evaluation of a Quality Improvement Initiative
by
William Mulrooney, Caitlin Wilson, Richard Pilbery, Ruth Fisher, Sarah Whiterod, Heather Smith, Emily Turner, Heather Edmonds, Peter Webster, Graham Prestwich, Fiona Bell and Rebecca McLaren
Emerg. Care Med. 2025, 2(4), 49; https://doi.org/10.3390/ecm2040049 - 18 Oct 2025
Abstract
►▼
Show Figures
Background: Falls in older adults are a leading cause of morbidity, particularly when compounded by polypharmacy. There is mixed evidence of the efficacy of medicine reviews, but there is little work exploring this in the ambulance setting. A new referral pathway enabling ambulance
[...] Read more.
Background: Falls in older adults are a leading cause of morbidity, particularly when compounded by polypharmacy. There is mixed evidence of the efficacy of medicine reviews, but there is little work exploring this in the ambulance setting. A new referral pathway enabling ambulance staff to connect patients to primary care pharmacists aimed to address this. This study explored staff and patient experiences with the pathway and its potential to improve medication safety after a fall. Methods: A mixed-method service evaluation was conducted to assess the implementation and impact of this pathway. Routine data from an ambulance trust and pharmacist proformas were used to address objectives relating to referral rates, clinical appropriateness, and fall recurrence. Patient and staff stakeholder perspectives were gathered through two cross-sectional surveys designed to explore emotional, behavioral, and practical responses to the intervention. Quantitative data were analyzed descriptively and using ordinal logistic regression where appropriate. Free-text responses were analyzed thematically. Results: Between May 2019 and March 2020, referrals were initiated for 775 older adults after ambulance attendance for a fall, with pharmacists completing medicine reviews on 340 patients. Survey data revealed improvements in patients’ emotional responses to their medicines. Ambulance clinicians identified patient disclosure, stockpiling, and the presence of expired medicines as key indicators of poor medicines management and valued the ability to refer patients. Conclusions: Overall, referral to the pathway demonstrates a marginal improvement in recontact rates in the short-term but does not necessarily represent an improvement in overall patient safety. The cost of such an intervention and patient expectations need further exploration to prove efficacy and patient satisfaction.
Full article

Figure 1
Open AccessArticle
In-Hospital Cardiac Arrest Management: Retrospective Cohort and Process–Outcomes Analysis in a Costa Rica Hospital
by
Abigail Fallas-Mora, Jeaustin Mora-Jiménez, Kevin Cruz-Mora, José Miguel Chaverri-Fernández, José Pablo Díaz-Madriz, Guillermo Fernández-Aguilar and Esteban Zavaleta-Monestel
Emerg. Care Med. 2025, 2(4), 48; https://doi.org/10.3390/ecm2040048 - 14 Oct 2025
Abstract
Background/Objectives: In-hospital cardiac arrest (IHCA) remains a critical event with high mortality, requiring coordinated multidisciplinary response. Return of spontaneous circulation (ROSC) and hospital discharge rates are key quality indicators in resuscitation efforts. In Costa Rica, there is limited published data on team performance,
[...] Read more.
Background/Objectives: In-hospital cardiac arrest (IHCA) remains a critical event with high mortality, requiring coordinated multidisciplinary response. Return of spontaneous circulation (ROSC) and hospital discharge rates are key quality indicators in resuscitation efforts. In Costa Rica, there is limited published data on team performance, protocol adherence, and the pharmacist’s role in code blue events, despite similar evidence gaps across Latin America. This study aimed to evaluate clinical outcomes and operational performance of in-hospital cardiac arrest events at a Costa Rica hospital. Methods: This retrospective cohort study included 77 adult patients who experienced IHCA at Clínica Bíblica between 2020 and 2024. Data collection was conducted between February and May 2025 from electronic medical records and code blue activation logs. Clinical variables, comorbidities, pharmacologic interventions, and outcomes were analyzed. Predictive models (Charlson Comorbidity Index [CCI], IHCA-ROSC, RISQ-PATH) and Kaplan–Meier survival analysis were applied. Results: ROSC was achieved in 55.8% of patients, and 21% were discharged alive. Asystole was the predominant initial rhythm (76.6%), and comorbidities such as renal disease and myocardial infarction were most frequent. A higher comorbidity burden was significantly associated with lower discharge rates (p = 0.032). Despite 98.7% of patients being classified as low probability for ROSC by the IHCA-ROSC model, observed outcomes exceeded expectations (predicted: 5.53% vs. actual: 55.84%; p < 0.000001). The code team adhered to institutional protocols in 100% of cases, with clinical pharmacists playing a key role in documentation and medication tracking. Conclusions: Structured multidisciplinary response was associated with ROSC rates notably higher than predicted by validated models. Opportunities for improvement include post-event laboratory testing, pharmacist-led documentation, and therapeutic hypothermia in shockable rhythms.
Full article
(This article belongs to the Special Issue Emergency Medicine Update: Cardiopulmonary Resuscitation)
►▼
Show Figures

Figure 1
Open AccessArticle
Paediatric Emergency Injury Presentations During the COVID-19 Pandemic in Regional Victoria, Australia: A Silver Lining?
by
Kate Kloot, Blake Peck and Daniel Terry
Emerg. Care Med. 2025, 2(4), 47; https://doi.org/10.3390/ecm2040047 - 27 Sep 2025
Abstract
►▼
Show Figures
Background/Objectives: The COVID-19 pandemic caused a widespread shift to remote work, significantly altering child supervision. In Australia, prolonged lockdowns created unique conditions where many parents were working from home while simultaneously caring for children. This study aimed to investigate potential changes in the
[...] Read more.
Background/Objectives: The COVID-19 pandemic caused a widespread shift to remote work, significantly altering child supervision. In Australia, prolonged lockdowns created unique conditions where many parents were working from home while simultaneously caring for children. This study aimed to investigate potential changes in the epidemiology of paediatric injury-related presentations to emergency health services among children in Southwest Victoria, Australia, during the COVID-19 pandemic. Methods: A retrospective cross-sectional study was conducted using deidentified emergency presentation data from ten health services in regional Victoria for children aged 0–14 years between 2018 and 2023. Injury data were analysed across three timeframes (Pre-COVID, COVID, Post-COVID). Chi-squared tests assessed differences in injury presentations by age, gender, and service type. Significance was determined at p < 0.05. Results: A total of 21,072 child injury-related presentations occurred. Males accounted for 57.6% of presentations, with the 10–14 age group comprising 39.8% of cases. During lockdown, injury presentations increased among 0–4-year-old females (from 30.2% to 32.0%), likely reflecting reduced supervision as parents juggled work-from-home responsibilities. Conversely, rates declined among older children, particularly 10–14-year-olds, potentially due to reduced participation in sports and outdoor activities. More than half of all cases (59.1%) were presented to Victorian Emergency Minimum Dataset (VEMD)-reporting emergency departments. Conclusions: The shift to working from home during the pandemic had a measurable impact on childhood injury patterns, particularly among younger children. These findings highlight the importance of considering parental work and childcare arrangements in injury prevention strategies and highlight the benefits of additional regional data to provide a more accurate picture of regional health service use.
Full article

Figure 1
Open AccessSystematic Review
Coronary CT Angiography for Acute Chest Pain in the Emergency Department: A Systematic Review of Clinical Utility
by
Kyvan Irannejad, Logan Hubbard, Aditya Narashim, Ruben Mora, Beshoy Iskander, Natdanai Punnanithinont, Keishi Ichikawa, April Kinninger, Suvasini Lakshmanan, Sion Roy, Donald Chang, Matthew Budoff and Srikanth Krishnan
Emerg. Care Med. 2025, 2(3), 46; https://doi.org/10.3390/ecm2030046 - 22 Sep 2025
Cited by 1
Abstract
►▼
Show Figures
Introduction: Chest pain is one of the most common and high-risk presentations in the emergency department (ED), necessitating timely and accurate evaluation to prevent adverse cardiovascular outcomes. Coronary Computed Tomography Angiography (CCTA) has emerged as a promising non-invasive modality with high sensitivity (90–100%)
[...] Read more.
Introduction: Chest pain is one of the most common and high-risk presentations in the emergency department (ED), necessitating timely and accurate evaluation to prevent adverse cardiovascular outcomes. Coronary Computed Tomography Angiography (CCTA) has emerged as a promising non-invasive modality with high sensitivity (90–100%) and a negative predictive value (98–100%) for ruling out significant coronary artery disease (CAD), as evidenced by trials such as ROMICAT II and ACRIN-PA. Despite its expanding role in ED triage, further evaluation of its impact on patient-centered outcomes is essential. Methods: A systematic review was conducted in accordance with PRISMA guidelines. Studies published between January 2010 and June 2025 were identified from PubMed, Embase, and the Cochrane Library. Eligible studies included randomized controlled trials and prospective cohort studies assessing CCTA in ED patients with suspected acute coronary syndrome (ACS), compared with alternative diagnostic strategies, and reporting outcomes, including diagnostic accuracy, time to diagnosis, ED discharge rates, hospital admissions, and cost-effectiveness. Results: Twenty-three studies comprising over 60,000 patients were included. CCTA in low- to intermediate-risk patients significantly reduced diagnostic time (up to 54%), increased early ED discharges, and lowered unnecessary admissions. It consistently demonstrated excellent diagnostic performance, with pooled sensitivity ≥90% and near-perfect negative predictive value. Economic evaluations showed reduced costs due to shorter ED stays and less downstream testing. Challenges included radiation exposure, contrast use, and incidental findings. Conclusions: CCTA enhances ED efficiency and safety in ACS evaluation, offering accurate CAD exclusion and resource optimization. Future studies should explore its long-term cost-effectiveness and integration into high-sensitivity troponin protocols.
Full article

Figure 1
Open AccessReview
From the Emergency Department to Follow-Up: Clinical Utility of Biomarkers in Mild Traumatic Brain Injury
by
Giacomo Spaziani, Gloria Rozzi, Silvia Baroni, Benedetta Simeoni, Simona Racco, Fabiana Barone, Mariella Fuorlo, Francesco Franceschi and Marcello Covino
Emerg. Care Med. 2025, 2(3), 45; https://doi.org/10.3390/ecm2030045 - 8 Sep 2025
Cited by 1
Abstract
Mild traumatic brain injury (mTBI) remains a clinical challenge, particularly in cases with normal computed tomography (CT) findings but persistent or evolving symptoms. Conventional diagnostic approaches relying solely on clinical criteria and neuroimaging often lack adequate sensitivity and may lead to unnecessary radiation
[...] Read more.
Mild traumatic brain injury (mTBI) remains a clinical challenge, particularly in cases with normal computed tomography (CT) findings but persistent or evolving symptoms. Conventional diagnostic approaches relying solely on clinical criteria and neuroimaging often lack adequate sensitivity and may lead to unnecessary radiation exposure. Recent advances in biomarker research have identified several blood-based proteins such as glial fibrillary acidic protein (GFAP), ubiquitin carboxy-terminal hydrolase L1 (UCH-L1), S100 calcium-binding protein B (S100B), Tau protein, neuron-specific enolase (NSE), and neurofilament light chain (NFL) as potential tools for improving diagnostic precision and guiding clinical decisions. In this study, we synthesize current evidence evaluating the diagnostic and prognostic utility of these biomarkers using sensitivity, specificity, negative predictive value (NPV), and area under the receiver operating characteristic curve (AUC). GFAP and UCH-L1 have shown high sensitivity in detecting intracranial lesions and are now FDA-cleared for emergency department triage within 12 h of injury. While S100B remains widely investigated, its low specificity limits its application beyond select clinical scenarios (i.e., in patients without polytrauma). Additionally, Tau, NSE, and NFL are emerging as prognostic markers, with studies suggesting associations with persistent symptoms and long-term neurocognitive outcomes. Overall, the integration of biomarker-based data into clinical workflows may enhance early mTBI diagnosis, reduce reliance on imaging, and enable individualized follow-up and prognostic stratification. Future research should refine optimal sampling windows and explore multimarker panels to maximize diagnostic and prognostic performance.
Full article
Open AccessArticle
Brain Computed Tomography Overutilization in an Emergency Department Setting
by
Anne Marie Lund, Jesper Juul Larsen and Thomas A. Schmidt
Emerg. Care Med. 2025, 2(3), 44; https://doi.org/10.3390/ecm2030044 - 6 Sep 2025
Abstract
►▼
Show Figures
Background: Brain computed tomography (CT) is the primary imaging modality for patients with acute neurological complaints in emergency departments, despite having a low diagnostic yield for many conditions. This study aimed to assess the common indications for brain CT, evaluate the prevalence of
[...] Read more.
Background: Brain computed tomography (CT) is the primary imaging modality for patients with acute neurological complaints in emergency departments, despite having a low diagnostic yield for many conditions. This study aimed to assess the common indications for brain CT, evaluate the prevalence of acute pathologies, and explore whether certain patient groups may be overexposed to unnecessary scans, impacting both patient safety and healthcare costs. Methods: We conducted a retrospective review of brain CT requests from the General Emergency Department in a single center over a one-month period. We recorded patient demographics (sex, age), scan indications, presence of focal neurological symptoms, acute pathology on CT, and final diagnoses. Descriptive statistics, including means ± SEM, were calculated using GraphPad Prism version 10.4.1. Results: A total of 584 brain CT scans were requested, of which 532 (91.1%) were normal, and 52 (8.9%) showed acute pathology. The age of all included patients were 70.8 ± 0.7 years with women (n = 304, 52.1%) being 71.9 ± 1.0 years old and men (n = 280, 47.9%) 69.7 ± 1.0 years old (p > 0.1). The most common indication for CT was head trauma (265, 45.4%) followed by ischemic stroke (130, 22.3%). The most frequent pathologies were ischemic stroke (2.7%), subdural hematoma (1.7%), and other traumatic bleeds (1.7%). Of the 52 patients with acute pathology, 42 (80.8%) exhibited focal neurological deficits. Conclusions: 91.1% of the brain CT scans in the emergency department were normal and did not lead to further intervention. While this may indicate a low diagnostic yield in certain patient groups—particularly those presenting with mild or nonspecific neurological symptoms—it does not alone confirm overuse. These findings highlight the importance of careful clinical evaluation to optimize imaging decisions. Reducing potentially unnecessary brain CT scans could lower healthcare costs and minimize radiation exposure, but the health-economic impact depends on balancing the savings with the potential costs of missing critical diagnoses and the associated societal consequences.
Full article

Figure 1
Open AccessCase Report
Ischemic Cerebellar Infarct During Recovery from Secondary Dengue Fever—A Case Report and Literature Review
by
Boon Ping Ting, Corinne Yee Lyn Lau, Puneet Seth, Jean Mui Hua Lee and Shao Hui Koh
Emerg. Care Med. 2025, 2(3), 43; https://doi.org/10.3390/ecm2030043 - 3 Sep 2025
Abstract
►▼
Show Figures
Background: Dengue fever is a global health problem and is endemic in Singapore, with a high economic burden. Neurological manifestations of dengue fever, although rare, are being increasingly reported. Ischemic stroke as a complication of dengue fever has rarely been reported. Methods:
[...] Read more.
Background: Dengue fever is a global health problem and is endemic in Singapore, with a high economic burden. Neurological manifestations of dengue fever, although rare, are being increasingly reported. Ischemic stroke as a complication of dengue fever has rarely been reported. Methods: This case report describes a case of ischemic cerebellar infarct during the recovery phase of secondary dengue fever with a review of similar cases previously described in the literature. Results: This is the first known case report of cerebellar ischemic stroke in Singapore following dengue fever, where Magnetic Resonance Angiography (MRA) demonstrated a possible occlusion or severe stenosis of a cerebral artery as the underlying pathophysiology of dengue-associated stroke. Dengue fever has been shown to increase the incidence of stroke. Conclusions: Physicians in dengue-endemic areas need to have a high index of suspicion to consider this diagnosis, especially in patients with dengue fever who present with neurologic deficits.
Full article

Figure 1
Open AccessReview
Approach to Precipitous Delivery in the Emergency Department: Best Practices for Managing Emergent Vaginal Deliveries and Associated Complications
by
Jessica Wimberly, Clates Adams and Chad Gorbatkin
Emerg. Care Med. 2025, 2(3), 42; https://doi.org/10.3390/ecm2030042 - 18 Aug 2025
Abstract
►▼
Show Figures
Precipitous deliveries in the emergency department are one of the highest-acuity events that emergency providers manage. These deliveries can range from uncomplicated to wrought with difficulty. They require emergency care providers to manage intrapartum complications, such as nuchal cords, shoulder dystocia, and breech
[...] Read more.
Precipitous deliveries in the emergency department are one of the highest-acuity events that emergency providers manage. These deliveries can range from uncomplicated to wrought with difficulty. They require emergency care providers to manage intrapartum complications, such as nuchal cords, shoulder dystocia, and breech presentation, and maternal complications such as uterine atony, birth canal trauma, and postpartum hemorrhage. Delivery may additionally necessitate resuscitative hysterotomy or neonatal resuscitation. Our narrative review discusses preparatory practices, normal labor and delivery progression, and brief guidelines for managing complications of precipitous deliveries for emergency medicine providers.
Full article

Figure 1
Open AccessArticle
Association Between Polyethylene Glycol Dose and Length of Hospital Stay in Body Packing Patients: A Retrospective Review
by
Sara Fouad Mahmoud, Ashraf El Malik, Ziad Ibdah, Mohamed Saudi, Guillaume Alinier and Mohamed Omar Saad
Emerg. Care Med. 2025, 2(3), 41; https://doi.org/10.3390/ecm2030041 - 14 Aug 2025
Abstract
Objectives: Body packing is one of the methods used to smuggle illicit drugs and items. Identifying the drug and eradicating drug packs are essential tasks to complete in the shortest possible time to reduce the risk of toxicity. Polyethylene glycol is one of
[...] Read more.
Objectives: Body packing is one of the methods used to smuggle illicit drugs and items. Identifying the drug and eradicating drug packs are essential tasks to complete in the shortest possible time to reduce the risk of toxicity. Polyethylene glycol is one of the safer laxatives to use if surgical exploration is not indicated. The objective of this study is to evaluate the association of the dose of polyethylene glycol (PEG) and the length of hospital stay and/or time for body packers to evacuate drug packs. Methods: This is a retrospective analysis completed at Hamad Medical Corporation in Qatar, studying adult patients who received polyethylene glycol to evacuate drug packs from January 2018 to September 2019. Results: The primary and secondary outcomes are association between PEG doses and length of hospital stay and time to drug pack clearance, respectively. There were a total of 39 patients included in this study. A minority of patients developed signs of systemic toxicity. The average hospital length of stay for all patients was 86.2 h. The results show that the PEG dose at 12 h is inversely proportional to the length of hospital stay where each extra 1 g will decrease length of hospital stay by 0.098 h. The results are even more statistically significant when analyzed compared to time to clearance with a regression coefficient of −0.136 (p = 0.022). Conclusions: This study shows that a higher polyethylene glycol dose, especially at 12 h, is safe and reduces the time needed to clear drug packs and reduces length of hospital stay.
Full article
Open AccessReview
On the Move: A Review of Mobile and Military Surgery
by
Colton D. Wayne, Taylor H. Jacobs, Kyle Alexander, Zachary Dumbauld, Siddharth Narayanan, Omar Rokayak and Forrest O. Moore
Emerg. Care Med. 2025, 2(3), 40; https://doi.org/10.3390/ecm2030040 - 14 Aug 2025
Abstract
►▼
Show Figures
The ability to provide ambulatory and mobile surgery services in rural and austere environments has seen tremendous growth in recent decades due to innovations in surgical techniques and equipment. These advances have been implemented in both civilian and military settings, increasing the capabilities
[...] Read more.
The ability to provide ambulatory and mobile surgery services in rural and austere environments has seen tremendous growth in recent decades due to innovations in surgical techniques and equipment. These advances have been implemented in both civilian and military settings, increasing the capabilities of surgeons and surgical subspecialists across the globe. This review aims to briefly explore the history of ambulatory and mobile surgery and describe the recent efforts to make advancements in this field to improve global surgery opportunity and access, as well as to provide an overview of both military and civilian utilizations of mobile surgical teams and strategies.
Full article

Figure 1
Open AccessReview
Hemodynamic Support in Cardiogenic Shock in the Cardiac Catheterization Laboratory
by
Cesar Jiménez-Méndez, Ana Lara-Palomo, Ana Pérez-Asensio, Luis Martín-Alfaro, Mauricio Urgiles, Rafael Vázquez-García and Livia Gheorghe
Emerg. Care Med. 2025, 2(3), 39; https://doi.org/10.3390/ecm2030039 - 13 Aug 2025
Abstract
►▼
Show Figures
Cardiogenic shock is a life-threatening, time-sensitive syndrome characterized by clinical and biochemical tissue hypoperfusion caused by circulatory failure secondary to inadequate cardiac output. Inadequate cardiac contractility secondary to acute myocardial infarction appears on the top of the list of the most prevalent etiologies
[...] Read more.
Cardiogenic shock is a life-threatening, time-sensitive syndrome characterized by clinical and biochemical tissue hypoperfusion caused by circulatory failure secondary to inadequate cardiac output. Inadequate cardiac contractility secondary to acute myocardial infarction appears on the top of the list of the most prevalent etiologies of this syndrome. Despite some advances in its management, this primary cardiac disorder still has an extremely high mortality. In addition to treating the main etiology, immediate hemodynamic support is necessary to reduce the risk of developing multi-organ dysfunction and to preserve cell metabolism, as soon as we suspect it, even when needed in the catheterization laboratory. The cardiac catheterization laboratory has become a pivotal setting for implementing rapid hemodynamic support measures, such as pharmacological interventions and mechanical circulatory support, during critical procedures. Despite inotrope pharmacological treatment, mechanical circulatory support has recently garnered significant interest in this field. The aim of this review is to analyze hemodynamic support in cardiogenic shock in the most common contemporary scenario: the cardiac catheterization laboratory.
Full article

Figure 1
Open AccessCorrection
Correction: Gianazza et al. Asymptomatic Intestinal Ischemia Secondary to Thrombosis of the Spleno-Mesenteric Portal Axis: Usefulness of Laparoscopic Approach for Diagnosis and Therapeutical Decisions—Case Report and Review of the Literature. Emerg. Care Med. 2024, 1, 39–45
by
Simone Gianazza, Marika Morabito, Davide Inversini, Sabrina Garbarino, Marta Ripamonti, Giuseppe Ietto and Giulio Carcano
Emerg. Care Med. 2025, 2(3), 38; https://doi.org/10.3390/ecm2030038 - 12 Aug 2025
Abstract
In the original publication [...]
Full article
Open AccessArticle
Evaluating the Safety of Tenecteplase Versus Alteplase for Acute Ischemic Stroke
by
Salma Guerrero Miranda, Ifoma Ofoegbuna, Maicuc Tran, Ada Selina Jutba and Christine Vo
Emerg. Care Med. 2025, 2(3), 37; https://doi.org/10.3390/ecm2030037 - 8 Aug 2025
Abstract
►▼
Show Figures
Background/Objectives: This study aims to compare the safety of tenecteplase versus alteplase for acute ischemic stroke. Methods: This was a multicenter, retrospective cohort study including 11 Memorial Hermann Health System hospitals in Houston from 7 December 2022 to 7 June 2023. Adults presenting
[...] Read more.
Background/Objectives: This study aims to compare the safety of tenecteplase versus alteplase for acute ischemic stroke. Methods: This was a multicenter, retrospective cohort study including 11 Memorial Hermann Health System hospitals in Houston from 7 December 2022 to 7 June 2023. Adults presenting with an acute ischemic stroke who received alteplase or tenecteplase were included in this study. The primary outcome was the incidence of hemorrhagic conversion after 24 h of thrombolytic administration. Secondary outcomes included door-to-needle time, incidence of a major or minor bleed, length of hospital stay, incidence of any adverse effect, modified Rankin score at discharge, patient discharge disposition, medication cost, and mortality. Results: A total of 173 patients were reviewed, with 87 patients in the tenecteplase group and 86 patients in the alteplase group. Gender, actual body weight, and use of aspirin or dual antiplatelet therapy within 24 h of thrombolytic administration were statistically disproportionate between both groups. Hemorrhagic conversion occurred in seven patients in the tenecteplase group and eight patients in the alteplase group (p = 0.79). Medication cost was statistically significant between both groups. All other secondary outcomes were similar between tenecteplase and alteplase. Conclusions: In this underpowered study, we did not observe a statistically significant difference in the rate of 24 h hemorrhagic conversion between the tenecteplase and alteplase groups. Further studies with a large sample size are warranted to assess safety outcomes.
Full article

Figure 1
Open AccessArticle
Efficacy of Portable Fugitive Aerosol Mitigation Systems for Nebulizer Therapy During High-Flow Nasal Cannula and Non-Invasive Ventilation
by
Adithya Shyamala Pandian, Bhavesh Patel, Karam Abi Karam, Amelia Lowell, Kelly McKay, Sabrina Jimena Mora, Piyush Hota, Gabriel Pyznar, Sandra Batchelor, Charles Peworski, David Rivas, Devang Sanghavi, Ngan Anh Nguyen, Aliaa Eltantawy, Xueqi Li, Xiaojun Xian, Michael Serhan and Erica Forzani
Emerg. Care Med. 2025, 2(3), 36; https://doi.org/10.3390/ecm2030036 - 29 Jul 2025
Abstract
►▼
Show Figures
Objectives: This study evaluates the efficacy of existing and new aerosol mitigation methods during nebulization (Neb) in combination with high-flow nasal cannula (HFNC) oxygen supplementation and non-invasive ventilation (NIV). Methods: We recorded fugitive aerosol particle concentrations over time and assessed the peak (P)
[...] Read more.
Objectives: This study evaluates the efficacy of existing and new aerosol mitigation methods during nebulization (Neb) in combination with high-flow nasal cannula (HFNC) oxygen supplementation and non-invasive ventilation (NIV). Methods: We recorded fugitive aerosol particle concentrations over time and assessed the peak (P) and area (A) efficacy of active and passive mitigation methods, comparing them to a no-mitigation condition. Peak efficacy was measured by the reduction in maximum aerosol concentration, while area efficacy was quantified by the reduction of the area under the aerosol concentration–time curve. Results: For HFNC with Neb, we found that active mitigation using a mask with a biofilter and a fan (referred to as the aerosol barrier mask) significantly outperformed passive mitigation with a face mask. The peak and area efficacy for aerosol reduction were 99.0% and 96.4% for active mitigation and 35.9% and 7.6% for passive mitigation, respectively. For NIV with Neb, the active mitigation method, using a box with a biofilter and fan, also outperformed passive mitigation using only the box. The peak and area efficacy for aerosol reduction were 92.1% and 85.5% for active mitigation and 53.7.0% and 25.4% for passive mitigation, respectively. Conclusion: We concluded that active mitigation set up systems advantageous for effective reduction of airborne aerosols during aerosol generated procedures.
Full article

Graphical abstract
Open AccessArticle
Performance of the InfraScanner for the Detection of Intracranial Bleeding in a Population of Traumatic Brain Injury Patients in Colombia
by
Santiago Cardona-Collazos, Sandra Olaya-Perea, Laura Fernández, Dylan Griswold, Alvaro Villota, Sarita Aristizabal, Elizabeth Ginalis, Diana Sanchez, Angelos Kolias, Peter Hutchinson and Andres M. Rubiano
Emerg. Care Med. 2025, 2(3), 35; https://doi.org/10.3390/ecm2030035 - 23 Jul 2025
Abstract
►▼
Show Figures
Background/Objectives: Traumatic brain injury (TBI) is a global public health concern, affecting over 60 million people annually. It is associated with high rates of mortality and disability, particularly among young and economically active individuals, and remains the leading cause of death in
[...] Read more.
Background/Objectives: Traumatic brain injury (TBI) is a global public health concern, affecting over 60 million people annually. It is associated with high rates of mortality and disability, particularly among young and economically active individuals, and remains the leading cause of death in people under 40 years of age. Although computed tomography (CT) is the standard method for excluding intracranial bleeding (ICB), it is frequently unavailable in resource-limited settings where the burden of TBI is greatest. The InfraScanner 2000 is a near-infrared spectroscopy (NIRS) device designed to detect ICB and may serve as a triage tool in environments without access to CT imaging. This study aimed to evaluate the diagnostic performance of the InfraScanner 2000 for detecting ICB in the emergency department (ED) of a trauma center in a cohort of Colombian patients with TBI. Methods: This prospective study was conducted in Cali, Colombia, between December 2019 and February 2021. Adult patients presenting to the ED with blunt TBI were enrolled. InfraScanner assessments were performed according to a standardized protocol, and all participants underwent head CT within 6 h of injury. Results: A total of 140 patients were included. Of these, 66% were male and 34% were female. Most patients (63.57%) were between 18 and 39 years old, with a median age of 39 years (IQR: 18–86). The InfraScanner demonstrated a sensitivity of 60.0% (95% CI: 32.5–84.8), specificity of 78.4% (95% CI: 71.2–85.6), positive predictive value (PPV) of 25.0%, and negative predictive value (NPV) of 94.2% for detecting ICB. Conclusions: The InfraScanner 2000 showed good specificity and high NPV in identifying ICB among Colombian patients with TBI. These findings suggest it could serve as a useful triage tool to support decision-making in emergency settings with limited access to CT imaging.
Full article

Figure 1
Open AccessCorrection
Correction: Wang, A. The Role of Acupuncture in the Management of Bell’s Palsy: A Review of the Evidence and Perspectives in Emergency Care. Emerg. Care Med. 2024, 1, 230–239
by
Alan Wang
Emerg. Care Med. 2025, 2(3), 34; https://doi.org/10.3390/ecm2030034 - 16 Jul 2025
Abstract
There was an error in the original publication [...]
Full article
Open AccessArticle
Surgical Decision-Making for the Treatment of Acute Diverticulitis: A Single-Center Retrospective Study
by
Davide Inversini, Sara El Adla, Andrea Vigezzi, Simone Gianazza, Marika Morabito, Andrea Rizzi, Andrea Palillo, Giuseppe Ietto and Giulio Carcano
Emerg. Care Med. 2025, 2(3), 33; https://doi.org/10.3390/ecm2030033 - 14 Jul 2025
Abstract
►▼
Show Figures
Background: Several studies have suggested that laparoscopic peritoneal lavage for the treatment of diverticulitis might be associated with an increased event rate. The WSES (World Society of Emergency Surgery) guidelines recommend performing laparoscopic peritoneal lavage only in highly selected patients; however, selection criteria
[...] Read more.
Background: Several studies have suggested that laparoscopic peritoneal lavage for the treatment of diverticulitis might be associated with an increased event rate. The WSES (World Society of Emergency Surgery) guidelines recommend performing laparoscopic peritoneal lavage only in highly selected patients; however, selection criteria remain poorly described. This study, based on a single-center retrospective cohort of patients presenting with acute diverticulitis and undergoing surgery, aimed to assess the complication and long-term outcomes of the lavage group and to report our experience with the treatment of acute diverticulitis. Methods: Operative management of acute sigmoid diverticulitis was involved, in particular, laparoscopic peritoneal lavage, primary resection, and the Hartmann procedure. Results: Six-month follow-ups showed the occurrence of Clavien–Dindo complications in ≥2 in 21.9% of patients in the sigmoidectomy group versus 61.1% of patients in the lavage group (p = 0.0028). Among the 11 patients with complications after laparoscopic lavage, 9 required a second surgery. After a comparison between the patients with complications and those without who were managed with laparoscopic lavage, descriptive differences were found regarding the BMI (95% CI, 21.7–24.3 vs. 95% CI, 24.7–31.3, p = 0.0419). In analysis, a BMI of ≥27 kg/m2 (OR, 16 p = 0.049) was associated with short- and long-term complications in the lavage group. There was no evidence for an association between complications and a BMI of ≥27 kg/m2 in the primary resection (OR, 1.61 p = 1) or the Hartmann procedure group (OR, 4.25 p = 0.1438). Perforated colonic diverticulitis treated with laparoscopic peritoneal lavage was associated with a high morbidity rate. Conclusions: The choice of surgical strategy for acute diverticular pathology is complex, influenced by various conditions. BMI could be a prognostic factor for long-term outcomes, including recurrent diverticulitis and the occurrence of abscesses.
Full article
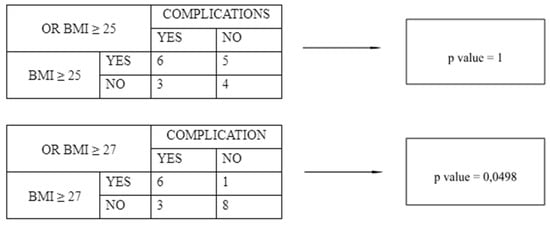
Figure 1
Open AccessCase Report
Magnetic Mishap: Multidisciplinary Care for Magnet Ingestion in a 2-Year-Old
by
Niharika Goparaju, Danielle P. Yarbrough and Gretchen Fuller
Emerg. Care Med. 2025, 2(3), 32; https://doi.org/10.3390/ecm2030032 - 8 Jul 2025
Cited by 1
Abstract
►▼
Show Figures
Background/Objectives: A 2-year-old male presented to the emergency department (ED) with vomiting and abdominal discomfort following ingestion of multiple magnets from a sibling’s bracelet. This case highlights the risks associated with magnet ingestion and the need for coordinated multidisciplinary care and public health
[...] Read more.
Background/Objectives: A 2-year-old male presented to the emergency department (ED) with vomiting and abdominal discomfort following ingestion of multiple magnets from a sibling’s bracelet. This case highlights the risks associated with magnet ingestion and the need for coordinated multidisciplinary care and public health intervention. Methods: Radiographs revealed magnets in the oropharynx, stomach, and small bowel. Emergency physicians coordinated care with otolaryngology, gastroenterology, and general surgery. Results: Laryngoscopy successfully removed two magnets from the uvula, and endoscopy retrieved 30 magnets from the stomach. General surgery performed a diagnostic laparoscopy, identifying residual magnets in the colon. Gastroenterology attempted a colonoscopy but was unable to retrieve magnets due to formed stool, leading to bowel preparation and serial imaging. The patient eventually passed 12 magnets per rectum without surgical intervention. Conclusions: This case emphasizes the importance of multidisciplinary collaboration in managing magnet ingestion, a preventable cause of serious gastrointestinal injury. Recent studies highlight the increasing incidence and severity of such cases due to accessibility and inadequate regulation. These findings underscore the need for public awareness and adherence to management protocols to mitigate morbidity and mortality in pediatric patients.
Full article

Figure 1
Open AccessArticle
No Learner Left Behind: How Medical Students’ Background Characteristics and Psychomotor/Visual–Spatial Abilities Correspond to Aptitude in Learning How to Perform Clinical Ultrasounds
by
Samuel Ayala, Eric R. Abrams, Lawrence A. Melniker, Laura D. Melville and Gerardo C. Chiricolo
Emerg. Care Med. 2025, 2(3), 31; https://doi.org/10.3390/ecm2030031 - 25 Jun 2025
Abstract
►▼
Show Figures
Background/Objectives: The goal of educators is to leave no learner behind. Ultrasounds require dexterity and 3D image interpretation. They are technologically complex, and current medical residency programs lack a reliable means of assessing this ability among their trainees. This prompts consideration as to
[...] Read more.
Background/Objectives: The goal of educators is to leave no learner behind. Ultrasounds require dexterity and 3D image interpretation. They are technologically complex, and current medical residency programs lack a reliable means of assessing this ability among their trainees. This prompts consideration as to whether background characteristics or certain pre-existing skills can serve as indicators of learning aptitude for ultrasounds. The objective of this study was to determine whether these characteristics and skills are indicative of learning aptitude for ultrasounds. Methods: This prospective study was conducted with third-year medical students rotating in emergency medicine at the New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY, USA. First, students were given a pre-test survey to assess their background characteristics. Subsequently, a psychomotor task (Purdue Pegboard) and visual–spatial task (Revised Purdue Spatial Visualization Tests) were administered to the students. Lastly, an ultrasound task was given to identify the subxiphoid cardiac view. A rubric assessed ability, and proficiency was determined as a 75% or higher score in the ultrasound task. Results: In total, 97 students were tested. An analysis of variance (ANOVA) was used to ascertain if any background characteristics from the pre-test survey was associated with the ultrasound task score. The student’s use of cadavers to learn anatomy had the most correlation (p-value of 0.02). Assessing the psychomotor and visual–spatial tasks, linear regressions were used against the ultrasound task scores. Correspondingly, the p-values were 0.007 and 0.008. Conclusions: Ultrasound ability is based on hand–eye coordination and spatial relationships. Increased aptitude in these abilities may forecast future success in this skill. Those who may need more assistance can have their training tailored to them and further support offered.
Full article

Figure A1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
AI, Algorithms, Diagnostics, Emergency Care and Medicine
Trends of Artificial Intelligence in Emergency and Critical Care Medicine
Topic Editors: Zhongheng Zhang, Yucai Hong, Wei ShaoDeadline: 30 November 2025
Topic in
Life, Biomedicines, JCRM, Diseases, Emergency Care and Medicine, Anesthesia Research
Electrolytes and Acid-Base Disturbances: Advances in Pathophysiology and Treatment
Topic Editors: Caterina Carollo, Giuseppe MulèDeadline: 30 March 2027

Conferences
Special Issues
Special Issue in
Emergency Care and Medicine
Emergency Medicine Update: Cardiopulmonary Resuscitation
Guest Editor: Sasa RajsicDeadline: 31 December 2025
Special Issue in
Emergency Care and Medicine
Traumatic Cardiac Arrest: Fundamentals and Advances
Guest Editor: Francisco EpeldeDeadline: 31 December 2025
Special Issue in
Emergency Care and Medicine
Application of Artificial Intelligence in Emergency Care
Guest Editor: Zhongheng ZhangDeadline: 31 December 2025
Special Issue in
Emergency Care and Medicine
New Advances in Airway Management for the 21st Century
Guest Editor: Luk Hsiang NingDeadline: 30 June 2026





