Abstract
Introduction: Difficult airway management is a critical challenge in anesthesia, often necessitating advanced techniques to ensure patient safety. A patient presented with a malignant lesion on the epiglottis, significantly altering the airway anatomy. Flexible rhinolaryngoscopy revealed a laryngeal carcinoma affecting the entire epiglottis, causing thickening and displacement, which suggested the potential for difficult intubation. Methods: Given the expected feasibility of bag-mask ventilation and front-of-neck access, an asleep intubation technique was selected. The combined use of a McGrath video laryngoscope and C-MAC video stylet allowed for fast and easy atraumatic intubation on the first attempt. The anesthetic and surgical course was uneventful. Discussion: This case report highlights the successful use of a combined approach involving a video laryngoscope and video stylet for intubation in a patient with known difficulties in airway management, providing insights into the benefits of enhanced visualization and maneuverability. The rigid design and steerable tip of the C-MAC video stylet provide advantages over traditional flexible optics, offering better maneuverability and reducing the need for a second operator. Although this technique was successful in this case, its use in patients with complex airway pathologies warrants careful preoperative assessment and collaboration with an experienced airway management team.
1. Introduction
Difficult airway management remains a significant challenge in anesthesia, necessitating the use of advanced techniques to ensure patient safety. When direct laryngoscopy fails, a video laryngoscope is often used, offering improved visualization of the laryngeal structure due to its blade design and the image sensor at the blade tip. Meta-analyses have reported a higher success rate for intubations and a higher frequency of first-attempt intubations with video laryngoscopy compared to direct laryngoscopy [1]. Flexible intubation scopes can provide a solution for patients or situations in which a direct laryngoscopy is difficult to perform. However, they require an experienced clinician and an airway that is mostly clear of blood and secretions. Video stylets may allow for a shorter intubation time compared to flexible intubation scopes, with a high first-pass success rate and clear glottic visualization [2], but they seem to remain underutilized in clinical practice. The combination of a video laryngoscope and video stylet has recently been proposed as new approach to difficult airway management [3]. This case report presents the successful use of this combination in a patient with a known difficult airway, highlighting the benefits of visualization and maneuverability in securing airway access. By examining the technical aspects and the outcome of this case, we aim to contribute to the ongoing discussion on optimizing airway management strategies in similar clinical scenarios. The clinical case is described below, followed by a discussion providing the context for this case.
2. Case Description
A 60-year old female, ASA III, was scheduled for the removal of a sentinel lymph node in her neck due to a laryngeal carcinoma. She reported pharyngeal discomfort for approximately one year. One month before the surgical procedure, she presented with hemoptysis. An ear, nose, and throat (ENT) doctor in a peripheral hospital was consulted and identified a hemorrhagic tumor in the laryngeal region. Tranexamic acid and dexamethasone were started in order to stop the bleeding, reduce swelling, and obtain a more adequate visualization of the tumorous process. Subsequently, the patient was referred to the ENT department of our university hospital.
A flexible rhinolaryngoscopy showed an abnormal anatomy of the epiglottis (Figure 1). A laryngeal carcinoma, arising from the anterior side of the epiglottis and extending bilaterally into the aryepiglottic fold, was observed. The entire epiglottis was thickened and rotated to the left, with the vallecula completely filled up. The lateral pharyngeal wall, both arytenoids, and the false and true vocal cords were free of tumor on both sides. The vocal cords showed no abnormalities besides a hyperplastic, polyp-like spot (Figure 2). CT imaging showed that the carcinoma measured 26 × 25 mm axially and 18 mm sagittally. The CT scan obtained the following additional findings: “Filling of the vallecula on the right more than on the left, also involving the lingual side. Primarily right-sided involvement of the aryepiglottic fold at the cranial side. Involvement of the pre-epiglottic fat, with subtle bilateral cranial paralaryngeal fat involvement at the supraglottic level. No involvement of the (cartilaginous) thyroid or hyoid bone. No extension into the base of the tongue. No enlarged lymph nodes”. The histology of the sentinel lymph node in the neck would further determine the treatment algorithm.
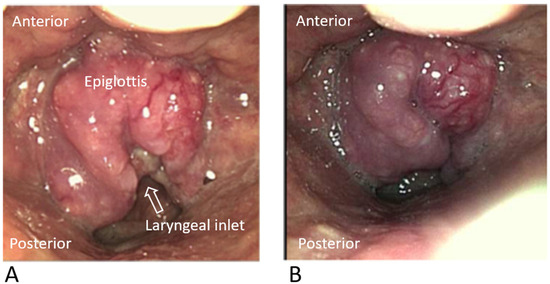
Figure 1.
Visualization of the laryngeal carcinoma, arising from the anterior side of the epiglottis, by using a flexible rhinolaryngoscope (A,B).
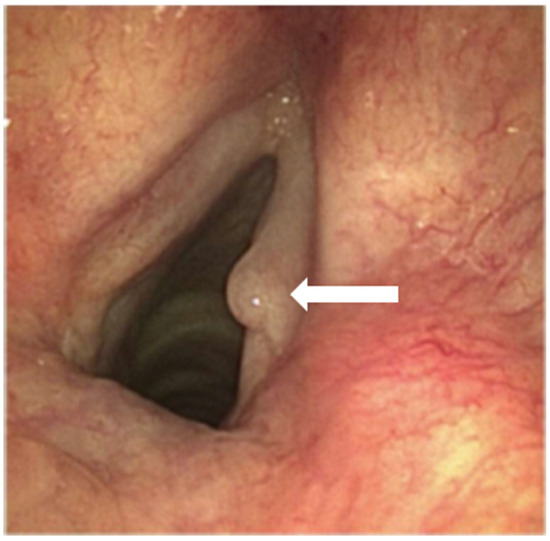
Figure 2.
Visualization of the vocal cords with a hyperplastic, polyp-like spot (white arrow) through a flexible rhinolaryngoscope.
As usual, the patient was seen by an anesthesiologist preoperatively. The regular airway assessment showed a normal mouth opening, thyromental distance, and neck circumference. The neck extension was slightly limited. The Mallampati score and the upper lip bite test were graded as IV and I, respectively. Front-of-neck access was deemed feasible. Since the bag-mask ventilation and front-of-neck access were deemed feasible, an asleep airway-management technique was chosen. As the carcinoma was intensely vascularized, indicating a propensity for easy bleeding, the main goal was to intubate as atraumatically as possible. Hence, a combination of a McGrath video laryngoscope and C-MAC video stylet was used.
After the connection of the regular vital sign monitoring equipment, optimal patient positioning, and adequate preoxygenation (i.e., end-tidal O2-concentration of >90%), general anesthesia was induced. After two minutes of propofol infusion (7 mg/kg/h) and remifentanil infusion (45 µg/kg/h), a propofol bolus of 100 mg was administered, followed by a 40 mg bolus of rocuronium and sequential reduction in the remifentanil infusion to 11 µg/kg/h. Bag-mask ventilation was carried out easily. Two minutes later, the McGrath video laryngoscope was introduced with the left hand. The epiglottis was visualized. However, the vocal cords and arytenoids could not be visualized using the video laryngoscope alone. Further introduction and manipulation of the video laryngoscope were avoided to prevent bleeding or further swelling of the epiglottis. The C-MAC video stylet with a pre-installed tracheal tube was introduced by the same person using the right hand alongside the video laryngoscope. During advancement towards the epiglottis, the video stylet progressed alongside the posterior pharyngeal wall. Inadvertent manipulation of the tumorous process could easily be avoided through the carefully monitoring of the movement of the video stylet on the screen of the video laryngoscope. The handle was pulled in order to bend the steerable tip of the stylet, which enabled the complete visualization of the arytenoids and the vocal cords on the screen of the video stylet. The tip of the C-MAC video stylet was placed between the vocal cords and an assistant could easily advance the endotracheal tube from the video stylet into the trachea (Figure 3A–F). The endotracheal intubation was easy and fast, took only one attempt, and was fully atraumatic.
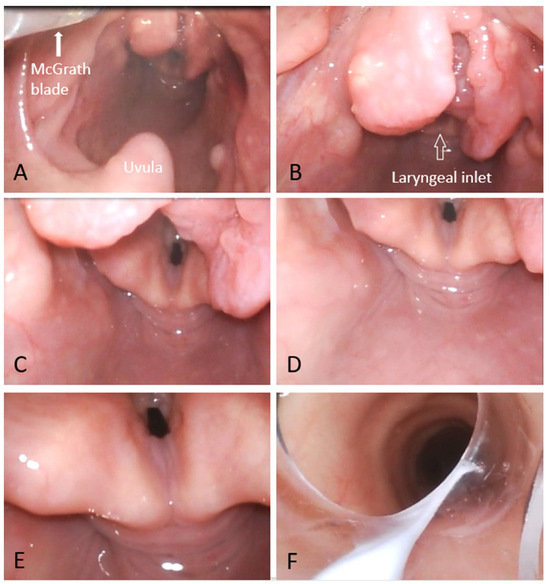
Figure 3.
Visualization of the intubation route using the C-MAC video stylet while approaching the larynx from a posterior direction (A–E) until the endotracheal tube, mounted on the video stylet, could be advanced into the trachea (F). The tumorous process appears paler compared to Figure 1, due to the bright light of the C-MAC video stylet. Also, the size of the tumor declined, possibly due to a deterioration in the edema as a result of the dexamethasone.
Further anesthesia, surgery, extubation, and recovery were uneventful. The histology of the sentinel lymph node in the neck showed no malignancy and radiotherapy with curative intention was started. Lastly, the patient reported no orally or pharyngeally oriented symptoms, such as a sore throat or being hoarse.
3. Discussion
In this case report, we describe the easy and fast endotracheal intubation of a patient with anticipated difficulties in airway management caused by an easily bleeding malignant epiglottic process. We used a combined technique involving a McGrath video laryngoscope and a C-MAC video stylet.
A combined technique using a video laryngoscope and a flexible optic has been reported in a number of case reports. This is commonly named Video-Assisted Fiberoptic Intubation (VAFI). Initially, this technique was described as a method to assist in teaching flexible intubation to residents [4]. However, Lenhardt et al. [5] showed in a randomized trial that the combination of a video laryngoscope with a flexible optic may be advantageously used in patients with anticipated difficulties in airway management. Although the primary outcome measures (time to successful intubation and number of intubation attempts) were not significantly different, four patients could not be intubated within three attempts using the video laryngoscope only, but were successfully intubated after adding the flexible optic. In a comparable trial in 160 patients with anticipated difficulties in airway management, Mazzinari et al. [6] showed an improved first-attempt intubation success rate and a decreased time to successful intubation with a combination of a video laryngoscope and flexible optic.
Interestingly, in a high-fidelity pediatric simulator, no significant differences were observed between traditional fiberoptic intubation and video-assisted fiberoptic intubation in terms of time until the completion of tracheal intubation, the number of intubation attempts, and the first-attempt success rate [7]. However, this may reflect that this airway simulator did not mimic the real-world challenges of fiberoptic intubation, such as reduced oropharyngeal space and the presence of blood or secretions.
We used the C-MAC video stylet in our patient instead of a flexible optic. The C-MAC video stylet has a rigid shaft with a flexible tip. In our opinion, the C-MAC video stylet has several advantages in this setting compared to a flexible optic. The rigid shaft allows for easier and faster maneuvering in an open space such as the oropharyngeal space. Passing the optic through blood or secretions could potentially be better avoided when using a video stylet than when using a flexible optic. Furthermore, two operators are needed for the video-assisted fiberoptic intubation (i.e., one for the video laryngoscope and one for the flexible optic). In our set-up, intubation can be achieved with a single operator who uses the video laryngoscope with the one hand and the video stylet with the other hand. While a one-operator intubation procedure is possible with this set-up, it is not yet clear whether this introduces any additional risks, particularly in patients with airway malignancies. Alternatively, a two-operator approach can always be chosen, with one operator handling the video laryngoscope and the other managing the video stylet. Comparable to our case, Jhuang et al. [3] described a video-twin technique for airway management in a case series, combining the Trachway video-intubation stylet and a video laryngoscope. They reported intubation times (which they described as ‘from lip to trachea’) between 6 and 15 s. In their cases, they used a video stylet with a rigid shaft without a flexible tip. The C-MAC video stylet used in our case, with a rigid shaft and a flexible tip, might provide the advantage of even better maneuverability due to the steerable tip.
In the study of Lenhardt et al. [5], patients with anticipated difficulties in airway management were included but patients with known larynx or pharynx pathology (e.g., a tumor or abscess) were excluded. In contrast, our patient had such a pathology. Using a thin flexible ENT rhinolaryngoscope, recent photos of the pathology were taken and documented by the ENT surgeon preoperatively. In close contact with the ENT surgeon, the experienced anesthesia airway team, in this case, decided that intubation with the combined use of a video laryngoscope and a C-MAC video stylet would be possible in this patient. Interestingly, Jhuang et al. [3] also included a patient with pharyngeal pathology (i.e., hypopharyngeal cancer) in their case series. The exact limits of this combined technique are not yet known. Nonetheless, for every individual patient, a well-considered decision should be made as to whether an awake fiberoptic intubation would be the safer option.
In patients with, for example, acute epiglottitis, or in uncooperative patients with anticipated difficulties regarding airway management, the best possible, most noninvasive approach is desired. In these cases, the video-twin technique combining a video-intubating stylet with video laryngoscope might be the best first approach.
For unanticipated difficulties regarding the airways, the 2022 ASA practice guideline for the management of difficult airways [1] states the following: “The consultants strongly agree and members of participating organizations agree or strongly agree that if difficulty is encountered with individual techniques, combination techniques may be performed”. A combination of a video laryngoscope with a video-intubating stylet could be considered as the preferred combination technique.
As with all airway management techniques, this combined technique has its own learning curve. Based on our experience, this learning curve is quite steep and from three to five intubations in asleep patients with a normal airway should be sufficient. This experience should also lower the threshold before switching to a combined technique in a scenario with unanticipated difficulties regarding airway management.
In conclusion, the reported combined technique might be a valuable addition to the armamentarium of every anesthesiologist that may possibly encounter difficulties in airway management.
Author Contributions
Conceptualization, methodology and investigation: R.L.W., J.B., R.M.K. and L.T.v.E.; writing—original draft preparation: R.L.W., R.M.K., N.H. and L.T.v.E.; writing—review and editing and supervision: J.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study because this is a retrospective case report, for which ethical approval is not applicable.
Informed Consent Statement
This case report was published with the written consent of the patient.
Data Availability Statement
Data of the patient is owned by the authors because of privacy reasons, but is available on reviewers request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Apfelbaum, J.L.; Hagberg, C.A.; Connis, R.T.; Abdelmalak, B.B.; Agarkar, M.; Dutton, R.P.; Fiadjoe, J.E.; Greif, R.; Klock, P.A.; Mercier, D.; et al. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology 2022, 136, 31–81. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Zhao, K.-Y.; Zhang, P.; Li, R.-H. Comparison of video laryngoscope, video stylet, and flexible videoscope for transoral endotracheal intubation in patients with difficult airways: A randomized, parallel-group study. Trials 2023, 24, 599. [Google Scholar] [CrossRef] [PubMed]
- Jhuang, B.-J.; Luk, H.-N.; Qu, J.Z.; Shikani, A. Video-Twin Technique for Airway Management, Combining Video-Intubating Stylet with Videolaryngoscope: A Case Series Report and Review of the Literature. Healthcare 2022, 10, 2175. [Google Scholar] [CrossRef] [PubMed]
- Doyle, D.J. GlideScope-assisted fiberoptic intubation: A new airway teaching method. Anesthesiology 2004, 101, 1252. [Google Scholar] [CrossRef] [PubMed]
- Lenhardt, R.; Burkhart, M.T.; Brock, G.N.; Kanchi-Kandadai, S.; Sharma, R.; Akça, O. Is video laryngoscope-assisted flexible tracheoscope intubation feasible for patients with predicted difficult airway? A prospective, randomized clinical trial. Anesth Analg. 2014, 118, 1259–1265. [Google Scholar] [PubMed]
- Mazzinari, G.; Rovira, L.; Henao, L.; Ortega, J.; Casasempere, A.; Fernandez, Y.; Acosta, M.; Belaouchi, M.; Esparza-Miñana, J.M. Effect of Dynamic Versus Stylet-Guided Intubation on First-Attempt Success in Difficult Airways Undergoing Glidescope Laryngoscopy: A Randomized Controlled Trial. Anesth Analg. 2019, 128, 1264–1271. [Google Scholar] [CrossRef] [PubMed]
- Isogai, H.; Kojima, T.; Kako, H. Fiberoptic Intubation vs. Video-Assisted Fiberoptic Intubation in a High-Fidelity Pediatric Simulator: A Randomized Controlled Trial. Cureus 2023, 15, e39280. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).