Abstract
Many studies have identified that adverse childhood experiences (ACEs) are associated with non-suicidal self-injury (NSSI) and suicidality. However, most studies have been restricted to a few types of ACEs. This study aims to investigate the association of 13 common types of ACEs with NSSI, suicidal ideation (SI), and suicide attempts (SA), as well as the mediation of depressive and anxiety symptoms therein. A total of 1771 (994 male, 777 female) students aged 11–16 (12.9 ± 0.6) years who participated in the baseline survey of the Chinese Adolescent Health Growth Cohort study were included in the analysis. ACEs, including childhood maltreatment, other common forms of ACEs, and smoking, were measured via the Chinese version of the Child Trauma Questionnaire (CTQ) and a series of valid questionnaires that were derived from previous studies. NSSI was measured using the Chinese version of the Functional Assessment of Self-mutilation. SI and SA were measured using questions derived from the Global School Based Student Health Survey. Depressive symptoms were measured via the Chinese version of the Center for Epidemiologic Studies Depression Scale, and anxiety symptoms were measured via the General Anxiety Disorder-7. Of the included participants, 92.0% reported one or more category of ACEs. Smoking, parent–child separation, emotional abuse, physical abuse, and being bullied were positively associated with NSSI; smoking, parent–child separation, emotional abuse, physical abuse, emotional neglect, and being bullied were positively associated with SI; smoking, emotional abuse, and being bullied were positively associated with SA. The associations of ACEs with NSSI, SI, and SA were each partially or completely mediated through depressive and anxiety symptoms. Children and adolescents who had experiences of smoking, physical abuse, and being bullied during childhood are consistently and independently associated with NSSI and suicidality, and these associations may be largely mediated through depressive and anxiety symptoms. In conclusion, not all the types of ACEs are independently associated with NSSI, and suicidality and other associations may mediate through depressive and anxiety symptoms. Target interventions for adolescents’ NSSI and suicidality should focus on those who have a history of ACEs and depressive and anxiety symptoms.
1. Introduction
Non-suicidal self-injury (NSSI), defined as direct, deliberate damage of one’s body tissue (e.g., cutting, burning) without suicidal intent, is different from suicidal behaviors (e.g., suicidal ideation (SI) and suicidal attempts (SA)) in purpose and frequency. NSSI, SI, and SA are major public health concerns among adolescents worldwide [1], and their prevalence may have increased during the COVID-19 pandemic [2,3]. NSSI and suicidality represent the strongest and most consistent predictors of future suicidal behaviors among youths in clinical patients and general populations [4]. Thus, it is of great importance to further understand the complex interplay between these many recognized risk factors (such as neglect and abuse).
A substantial body of research has demonstrated independent associations between adverse childhood experiences (ACEs), NSSI, and suicidality [5]. Yet, our current knowledge surrounding these associations has predominantly been derived from adults or clinical patients in high-income countries (HICs) [6,7,8], with only a few studies conducted among community adolescents in low- and middle-income countries (LMICs) [9,10]. Findings from HICs may not be generalized to LMICs due to socio-economic and cultural differences. ACEs include a broad set of potentially traumatic events, such as experiencing violence, abuse, neglect, and other aspects of the child’s environment that can undermine their sense of safety, stability, and bonding [11]. However, most prior studies that have examined the associations between ACEs and NSSI and suicidality have been rather limited in their scope, focusing on a narrow range of ACEs, such as childhood maltreatment [12], parent–child separation [13], and violent experiences [14]. It is uncertain whether other types of ACEs are independently associated with NSSI and suicidality.
In addition to ACEs, a lot of research indicated that depressive and anxiety symptoms were also associated with NSSI and suicidality [15,16]. However, most of these studies were conducted among adults or college students. For example, Healthy Minds Study (HMS) 2018–2019 data suggested that college students with depressive and/or anxiety symptoms had a higher prevalence of NSSI, 10 times the odds of suicide ideation, 28 times the odds of suicide ideation with planning or attempt, and 47 times the odds of suicide ideation with planning and attempt, compared to students with no depressive and/or anxiety symptoms [15]. Compared with adults or college students, children and adolescents are more likely to be affected by depressive and/or anxiety symptoms because of their relatively low psychological maturity and susceptibility to emotionally charged situations [17], and studies have reported that depressive and anxiety symptoms are the most common mental health difficulties in adolescents worldwide [18,19]. Therefore, the association of depressive and/or anxiety symptoms with NSSI and suicidality among children and adolescents needs to be further unraveled.
Furthermore, a growing number of studies have provided evidence to support that those with a history of ACEs are more likely to have depressive and/or anxiety symptoms than those who have no history of ACEs [20,21]. To sum up, although previous studies have demonstrated the association of ACEs with depressive and/or anxiety symptoms, depressive and/or anxiety symptoms with NSSI and suicidality, as well as ACEs with NSSI and suicidality, few studies have examined whether there are combined mediation effects of depressive and anxiety symptoms on the association of ACEs with NSSI, SI, and SA [22]. Identifying the potential mediation effects of depressive and anxiety symptoms on the association of ACEs with NSSI and suicidality is of substantial public health importance, since it will not only help to better understand the development and mechanism of NSSI and suicidality, but also may be meaningful for public policymakers to implement interventions of NSSI and suicidality.
Accordingly, the primary purpose of the present study was to investigate the associations between a broad range of ACEs and NSSI and suicidality among Chinese adolescents. We hypothesized that not all ACEs will independently associate with NSSI and suicidality, after adjusting for demographic characteristics and potential confounders, such as social support and emotional management ability. The secondary purpose of our study was to estimate the mediation effects of depressive and anxiety symptoms on the association between ACEs and NSSI and suicidality. We hypothesized that the effects of ACEs on NSSI and suicidality would be partially mediated through depressive and anxiety symptoms.
2. Materials and Methods
2.1. Participants Selection and Data Collection
2.1.1. Participants Selection
This study used the baseline survey data from the Chinese Adolescent Health Growth Cohort (CAHGC), an ongoing cohort study initiated in 2021 across three study sites: Qidong County, Hengyang City in Hunan province, Guangming District in Shenzhen City, and Zhongshan City in Guangdong Province, China. We selected these three cities as the study sites because their social economy reflected the status quo in China. The CAHGC aimed to understand the epidemiological characteristics, developmental trajectory, and influence of high-risk behaviors (mainly on self-harm and aggressive behaviors) among children and adolescents, and to provide evidence on polices and measurements development for reducing these behaviors. The study baseline survey was conducted from the 18 February to the 14 July 2021, when participants first completed a questionnaire on their sociodemographic profile, psychosocial variables, and behavioral characteristics, and received physical examinations (such as height, weight, waist, hip, blood pressure measurements, etc.).
We selected seventh-grade students as the study population due to the typical onset of NSSI and suicidality during early adolescence [19]. In each study site, we employed a random cluster sampling method to recruit participants. First, we identified approximately 10% of the junior high schools in each study site with the assistance of local educational administration. Then, we selected seventh-grade students from the selected schools to participate in the baseline survey of the CAHGC study, except for those with severe mental disorders (such as severe depression, schizophrenia, paranoid psychosis, and bipolar disorder) who were identified by the head teacher and/or health care professionals. Consent forms were distributed to a total of 1844 students across 42 classes in 11 schools, comprising 4 public schools and 7 private schools. These forms were provided by the head teacher of each selected class to request the students’ participation. Students were required to take the consent form home and discuss it carefully with their parents or guardians. Interested students were only allowed to participate in the baseline survey if they could provide written informed consent from their parents or guardians.
Of 1844 initial potential participants, 40 individuals did not return the consent form, 28 were absent from school during the investigation, and 5 submitted questionnaires with at least 15% of the items left unanswered. The omission of these yielded a final sample of 1771 (96.0%) participants. There were no significant differences in residential area, school type, age, and sex between respondents and non-respondents (Table S1 in the Supplementary Materials). Among these 1771 final participants, 994 were male (56.1%) and 777 were female (43.9%), with 60.7% living in Zhongshan City. The participants’ ages ranged from 11 to 16 years, with a mean (SD) age of 12.9 (0.6) years. All students were in the seventh-grade, 96.6% were Han ethnicity, 17.0% were a single child, 357 (20.2%) reported depressive symptoms, and 548 (30.9%) reported anxiety symptoms. Additional characteristics of the participants according to sex are summarized in Table 1.

Table 1.
Characteristics of participants with respect to sex.
2.1.2. Data Collection
Throughout the survey period, all the selected schools were in areas with a low risk of COVID-19 transmission, which implemented routine prevention and control measures and polices for COVID-19, including wearing masks when going out and regularly testing nucleic acid freely. Thus, most daily, and social activities were not affected. The questionnaire survey was administered by trained investigators, consisting of both teachers and postgraduates. These investigators were readily available at each study site to address any participant queries, provide clarification, and assist with questions related to the questionnaire. Participants were asked to complete the questionnaire independently within a designated timeframe of 45 to 60 min. Following completion, the questionnaires were reviewed for completeness and accuracy by the trained investigators. Clinical professionals from local medical institutions then conducted physical examinations as part of the study procedures. The authors affirm that all processes and activities associated with this study adhere to the ethical standards stipulated by the relevant national and institutional committees governing human experimentation. Additionally, the study follows the principles outlined in the Helsinki Declaration of 1975, as revised in 2008. This human study was approved by Institutional Review Board of Guangzhou Medical University (protocol code: 2021010002; 13 January 2021). All parents or guardians provided written informed consent for the minors to participate in this study.
2.2. Measures
2.2.1. Sociodemographic Profile, Emotional Management Ability, and Social Support
A self-designed questionnaire was used to collect categorical data on socioeconomic, familial, and parenting variables. These variables encompassed regional areas (Qidong County, Guangming District, Zhongshan City), school type (public or private), ethnicity (Han or others), age, sex (male or female), single child (yes or no), the educational attainment of the primary caregiver (junior high school or lower, senior high school or technical school, college or higher), and parenting style (strict, pampering, indulgent/rude/frequently changing, or open-minded). Whether the participant had begun puberty (yes or no) was measured by questions developed with reference to the criteria proposed by Ye [23]. Emotional management ability and social support were measured by the 4-item subscale of the Emotional Intelligence Inventory [24] and the 17-item Adolescents Social Support Scale [25], respectively. The Cronbach α coefficient of the scales were 0.84 and 0.96, respectively.
2.2.2. ACEs
ACEs were defined as having experienced potentially traumatic events that occurred in childhood, which included childhood maltreatment, other common forms of ACEs, and smoking in the present study. Childhood maltreatment was evaluated by the Chinese version of Child Trauma Questionnaire (CTQ) [26], which measures five different categories of childhood trauma, including emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect. The CTQ comprises a sum of 28 questions with responses rated on a 5-point Likert scale: 1 (never like this), 2 (rarely like this), 3 (sometimes like this), 4 (often like this), and 5 (always like this). Respondents were considered to have experienced a particular category of childhood maltreatment if they responded ‘3, sometimes like this’, ‘4, often like this’ or ‘5, always like this’ to any item within that category [9]. The CTQ has demonstrated good internal consistency, with a Cronbach a coefficient of 0.74 in a previous study [9] and 0.79 in the present study. Questions used to assess the presence of other forms of ACEs were derived from previous studies [5,6], and include: (a) parental divorce (yes or no); (b) being bullied by peers (yes or no); (c) family financial difficulties (household income less than CNY 5000 (equivalent to USD 700) per month [27], yes or no); (d) poor living environment (per capita living area of family member less than 20 square meters, yes or no); (e) parent–child separation (separation longer than 6 months before 6 years old [28], yes or no); (f) family history of psychiatric diseases (yes or no), and (g) no close friends (yes or no). The Cronbach α coefficient of these questions was 0.74. Respondents were classified as exposed to this type of ACEs if the participants responded ‘yes’ to any of these questions. We defined smoking as a form of ACEs since it may be a proxy variable of having witnessed parental substance abuse [29]. Items used to assess smoking were adapted from Global Youth Tobacco Surveys, and participants who reported smoking a cigarette on at least 1 day during the past 30 days were categorized as smokers [30].
2.2.3. Depressive Symptoms
A Chinese version of the Center for Epidemiologic Studies Depression Scale (CES-D) was employed to assess depressive symptoms [30]. This scale comprises 9 questions, with responses rated on a 4-point Likert scale: 0 (never true), 1 (rarely true), 2 (often true), and 3 (always true). Thus, the total scores on the CES-D range from 0 to 27. The higher scores are indicative of a greater risk of depression or more severe depressive symptoms [28]. Participants were categorized into two groups based on He’s proposed cut-off point. Participants with CES-D scores between 10 and 27 were considered to have depressive symptoms, while those with CES-D scores between 0 and 9 were deemed not to have depressive symptoms [31]. The Cronbach α coefficient of the scale in the present study was 0.83.
2.2.4. Anxiety Symptoms
Anxiety symptoms were assessed using the General Anxiety Disorder-7 (GAD-7) [32], a questionnaire consisting of 7 questions with responses rated on a 4-point Likert scale: 0 (never true), 1 (rarely true), 2 (often true), and 3 (always true). Total scores on the GAD-7 can range from 0 to 21, where higher scores are indicative of a greater risk of anxiety or more severe anxiety symptoms. Participants were categorized into two groups based on the total scores on the GAD-7: (1) scores between 5 and 21 were classified as indicative of anxiety symptoms; (2) scores between 0 and 4 were classified as not indicative of anxiety symptoms [32]. In the present study, the Cronbach α coefficient of the scale was 0.92.
2.2.5. NSSI, SI, and SA
NSSI during the past 12 months was assessed using the Chinese version of the Functional Assessment of Self-mutilation (FASM) [28]. All participants were asked the question, “During the past 12 months, have you harmed yourself in a way that was deliberate, but not intended to take your life?”. A total of 8 distinct methods were presented, encompassing hitting, hair-pulling, head-banging, pinching, scratching, biting, burning, and cutting. For those participants who reported involvement in NSSI, their NSSI frequency was examined. In the present study, NSSI was dichotomized (categorizing a frequency of three or more acts in the past year as “YES” and fewer than three as “NO”) for analytical purposes [9]. The internal consistency reliability of FASM in the present study was 0.80.
SI and SA were assessed using questions derived from the Global School-Based Student Health Survey [33]. SI was defined as an affirmative response to the question, “During the past 12 months, have you ever seriously considered attempting suicide?” SA was assessed by the question, “During the past 12 months, how many times did you actually attempt suicide?”, with SA defined as once or more.
2.3. Statistical Analysis
We used frequencies and proportions for categorical variables and mean (SD) for continuous variables to describe the characteristics of the participants and their experiences with NSSI or suicidality by the study variables. We used χ2 tests or 2-tailed, unpaired t-tests to compare the distribution between males and females according to the study variables, which is important as that may provide information for deep data analysis. To assess the association of ACEs with NSSI and suicidality, we employed logistic regression to separately estimate the unadjusted odds ratios (ORs), adjusted ORs, and their corresponding 95% confidence intervals (CIs) for NSSI, SI, and SA for 13 types of ACEs. In the adjusted models, we adjusted for regional areas, school type, ethnicity, sex, single child, caregiver’s educational level, parenting style, puberty, mutually exclusive ACEs, social support (continuous data), and emotional management ability (continuous data). We also estimated the graded associations of ACEs with NSSI and suicidality, in which an ordinal number of ACEs categories score was created by summing the dichotomous ACEs items (range, 0 [unexposed] to 13 [exposed to 13 types of ACEs assessed]). The total score of ACEs was then converted into three categories (0–2, 3–4, 5–13) based on its tertile, with 0–2 experiences selected as the referent for analysis purposes.
To assess the potential mediating role of depressive and anxiety symptoms in the association of ACEs with NSSI, SI, and SA, we performed mediation analyses. This involved decomposing the total effects into direct and indirect effects using the “ldecomp” command in Stata [34]. We separately estimated the indirect effects of depressive and anxiety symptoms as well. Figure 1 shows the conceptual framework underlying our mediation analysis. In our mediation analysis, we reported the ORs specifically for the ACEs that demonstrated independent associations with NSSI and suicidality in logistic regression models.
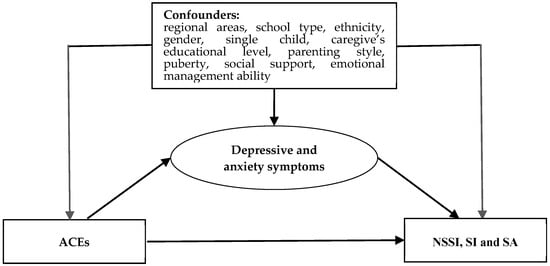
Figure 1.
Hypothesized mediation model.
Data were missing in ethnicity (7.8%), caregiver’s educational level (2.1%), single child (0.1%), and parenting style (1.0%). We addressed these missing covariates using the monotone logistic regression method, employing other sociodemographic variables as a basic, and generating 20 imputed datasets. A significance level of p = 0.05 was chosen, and all statistical tests conducted with a 2-tailed approach. The data analysis procedures were carried out using IBM SPSS Statistics, version 26.0 (IBM Corp, Armonk, NY, USA) and Stata (version 14.0, Stata Corp LLC, College Station, TX, USA).
3. Results
3.1. Prevalence of ACE, NSSI, SI and SA
We included 1771 participants in the final analysis. Ninety-two percent of the overall sample experienced one or more childhood adversities; the mean number of ACEs was 3.5 (SD = 1.9, median = 3, mode = 2, range = 1–10) (Table S2 in the Supplementary Materials). Emotional neglect (56.6%), physical neglect (47.1%), parent– child separation (44.0%), and emotional abuse (36.0%) were the most frequently reported ACEs among the participants.
The 12-month prevalence of NSSI was 17.1%, SI was 24.6%, and SA was 8.3%. Among the 17.1% of the entire sample who had engaged in NSSI at least three times in the 12 months before the survey, 89.1% reported 1 to 5 methods of NSSI (with a mean of 3.0, SD of 1.7, median of 3, mode of 2, and a range from 1 to 8). More specifically, self-hitting, self-pinching, and self-scratching were the most frequently reported forms of NSSI in the study population (Table S3 in the Supplementary Materials).
3.2. Association of ACEs with NSSI, SI and SA
Table 2 shows the frequencies and prevalence of NSSI according to the 13 types of ACEs. The prevalence of NSSI ranged from 17.3% among participants whose family income was less than CNY 5000 (USD 700) per month, to 38.1% in participants who had a family history of psychiatric diseases. All 13 forms of ACEs, except in the case of a family income less than CNY 5000 (USD 700) per month, were significantly associated with NSSI in the unadjusted model. However, in the adjusted model, significant associations were only found between smoking, parent–child separation, emotional abuse, physical abuse, and being bullied, and NSSI, with the adjusted OR of 2.41 (95%CI 1.01–5.75) 1.80 (95%CI 1.28–2.54), 1.69 (95%CI 1.21–2.37), 2.08 (95%CI 1.44–3.01), and 1.87 (95%CI 1.35–2.59), respectively (Adjusted model in Table 2).

Table 2.
Frequencies, prevalence, and odds ratio of 13 types of ACEs according to NSSI.
Table 3 shows the frequencies and prevalence of SI according to the 13 types of ACEs. The prevalence of SI ranged from 25.1% in participants whose family income was less than CNY 5000 per month, to 56.3% in participants who reported smoking. All ACEs, except in the case of a family income less than CNY 5000 (USD 700) per month and a family history of psychiatric diseases, were significantly associated with SI in the unadjusted model. In the adjusted model, significant associations remained between smoking, parent–child separation, emotional abuse, physical abuse, emotional neglect, and being bullied, and SI, with the adjusted OR of 4.03 (95%CI 1.66–9.81), 1.42 (95%CI 1.07–1.90), 1.91 (95%CI 1.41–2.59), 1.80 (95%CI 1.27–2.57), 1.78 (95%CI 1.28–2.49), and 2.08 (95%CI 1.54–2.81), respectively.

Table 3.
Frequencies, prevalence, and odds ratio of 13 types of ACEs according to SI.
Table 4 shows the frequencies and prevalence of SA according to the 13 types of ACEs. The prevalence of SA ranged from 8.6% in participants whose family income was less than CNY 5000 (USD 700) per month, to 34.4% in participants who reported smoking. All 13 types of ACEs, except in the case of a family income less than CNY 5000 (USD 700) and a family history of psychiatric diseases, were significantly associated with SA in the unadjusted model. In the adjusted model, significant associations of smoking, emotional abuse, and being bullied with SA remained, and the adjusted OR were 4.30 (95%CI, 1.67–11.10), 2.42 (95%CI, 1.58–3.72), and 1.75 (95%CI, 1.17–2.60), respectively (Adjusted in Table 4).

Table 4.
Frequencies, percentage, and odds ratio of 13 types of ACEs according to SA.
3.3. Mediation Analysis
The results from the mediation analyses indicated that the combined indirect effects of depressive and anxiety symptoms on the association of ACEs with NSSI, SI, and SA were all significant (p < 0.05), with the aOR ranging from 1.12 (1.05–1.19) to 1.97 (1.58–2.46) (Table 5). The direct effects of emotional abuse on NSSI, and being bullied on SA, were no longer significant in the mediation model, with aORs of 1.27 (0.89–1.84) and 1.43 (0.98–2.12), respectively. Similar results were found in participants stratified by sex (Tables S4 and S5 in the Supplementary Materials).

Table 5.
Logistic regression model of direct and indirect effects of ACEs through mediators on NSSI and suicidality.
4. Discussion
This study used baseline data of a multi-center cohort study to investigate the potential associations of 13 common types of ACEs with NSSI and suicidality. We also explored the potential mediating effects of depressive and anxiety symptoms on these associations. The findings indicated that not all the types of ACEs are independently associated with NSSI, SI, and SA, and these associations may mediate through depressive and anxiety symptoms.
ACEs, defined as experiences that pose a threat to a child’s physical, familial, or social wellbeing [11], are quite common. Data from the Behavioral Risk Factor Surveillance System (BRFSS) have shown that 61.55% of the US adult population has experienced at least 1 of 8 types of ACEs [35]. Although much of the existing literature on ACEs has focused on childhood maltreatment and household dysfunction, there is a lack of consensus on precisely what constitutes ACEs given the interindividual variation in threat perception [36], which has made the prevalence of ACEs directly incomparable between different studies. In the present study, we assessed 13 types of ACEs, ranging from broad categories of maltreatment and household dysfunction to more specific experiences such as bullying, smoking, and economic disadvantage. Our data demonstrated that 92.0% of the participants have experienced at least one type of ACEs, which was similar to a previous study that measured 10 types of ACEs defined by the ACE study [9].
4.1. Associations of ACEs with NSSI, SI, and SA
Previous research has demonstrated that many types of ACEs, including physical and sexual abuse [37], parent–child separation [28], and other familiar stressors are associated with NSSI and suicidality. Indeed, an investigation of 1404 college students in China suggested that individuals who experienced sexual abuse in childhood were more at risk of engaging in NSSI and suicidality [38]. Similarly, data from the UK 1958 British Birth Cohort Study also suggested that parental divorce, physical abuse, and sexual abuse in childhood were associated with SI at the age of 45 [39]. Our study extends this line of research by exploring associations between broader types of ACEs and NSSI and suicidality within Chinese community populations. This notwithstanding, the associations observed between all ACEs types and NSSI and suicidality in the present study were not all consistent with prior research involving clinical [40] and community populations [39]. For instance, whereas a significant association between physical abuse and NSSI has been documented in previous studies [38] this was not the case in our study. Similar with previous studies [9], varied associations were found across different types of ACEs, as ACEs were not significantly associated with NSSI and suicidality after adjusting for paternal care [41]. The discrepancies in the findings between studies for the associations of ACEs with NSSI and suicidality may be that the risk factors for NSSI and suicidality in LIMCs are different from those in HICs [42]. A previous study has identified that the strongest diagnostic risk factor for SA is mood disorders in HICs, but impulse control disorders in LMICs [42]. Cultural differences between LIMCs and HICs may also contribute to these discrepancies. Studies have suggested that the views on drug abuse and divorce of people in HICs are different from people in LIMCs, which has led to different prevalences of drug abuse and/or divorce [43]. Additionally, the associations of ACEs with NSSI and suicidality may be affected by the COVID-19 pandemic [2,3], although the study sites had a low risk of COVID-19 transmission during the study period.
Findings from the present study demonstrated that parent–child separation was associated with NSSI and SI but not with SA, which was consistent with one of our previous studies involving a national representative sample [28]. A similar association was also established for physical abuse. Varied associations of the same type of ACEs with NSSI, SI, and SA may imply etiology differences between NSSI, SI, and SA, although the existing literature indicates that the risk factors of NSSI and suicidality are regularly consistent [44]. Smoking in childhood, defined as an ACEs in the present study, was associated with NSSI and suicidality, even after adjusting for many potential confounders and mutually exclusive ACEs, which was in line with previous studies [45]. Harrison and colleagues, using the UK Biobank data, found associations of smoking behaviors with SI and SA, although the subsequent Mendelian randomization analysis did not find clear evidence for a causal effect of smoking on SI and SA [45]. Of note, the frequencies of smokers among the present study participants were relatively small, requiring further studies to identify whether the associations of smoking with NSSI and suicidality are occasional or significant. Moreover, although many studies suggested that child smoking could be a proxy variable of having witnessed parental smoking or other substance use [29], whether child smoking can be defined as one form of ACEs also needs further studies.
The findings of our study suggested that being bullied was associated with an increased risk of NSSI and suicidality, which was also consistent with previous studies conducted among the community population [33] but differed from studies involving clinical patients [46]. Being bullied may increase the risk of adverse psychological outcomes, including NSSI and suicidality, both in the short and over the long term [46]. Thus, it would be reasonable to suggest that intervention strategies could be implemented based on the association between being bullied, NSSI, and suicidality.
4.2. The Mediation of Depressive and Anxiety Symptoms on Associations of ACEs with NSSI, SI, and SA
Many studies have examined whether the associations between ACEs and NSSI and suicidality are mediated by different variables. In most cases, however, these mediators include factors such as social support or alexithymia [47]. Our study extends knowledge in this area by demonstrating the associations of ACEs with NSSI and suicidality were mediated through depressive and anxiety symptoms. The association between ACEs, depressive and anxiety symptoms, NSSI, SI, and SA is complex. Many previous studies have demonstrated that depressive symptoms may be a partial mediator between ACEs and NSSI among young adults [46]. For example, the UK 1958 British Birth Cohort study found that ACEs predicts SI in midlife and is partially mediated by adolescent internalizing and externalizing disorders [46]. Duan and colleagues found that the association between being bullied and suicide risk was mediated through negative coping styles and depressive symptoms [48]. Indeed, exposure to ACEs may increase the risk of adverse psychological symptoms. As such, it seems be reasonable to suggest that depressive and anxiety symptoms, which are the most prevalent mental symptoms in adolescents [28], may mediate the association of ACEs with NSSI, SI, and SA. Interestingly, we found the direct effects of emotional abuse and smoking on NSSI, and being bullied on SA, were not significant, while the indirect effects were significant, suggesting the effects were completely mediated through depressive and anxiety symptoms. A possible explanation of the null direct effects of emotional abuse on NSSI and being bullied on SA may be due to sex differences in the prevalence of depressive and anxiety symptoms. Previous studies have indicated that there are sex differences between the mediation effect of depressive symptoms on the association of ACEs with NSSI [49]. Overall, depressive and anxiety symptoms may partially or completely mediate the association of ACEs with NSSI and suicidality, suggesting that interventions targeting depressive and anxiety symptoms might mitigate the negative effects of ACEs among adolescents. Further studies are warranted to determine these complex associations between ACEs, depressive and anxiety symptoms, NSSI, and suicidality.
4.3. Strengths and Limitations
One strength of the present study is the representativeness of the sample within China. For this study, we used a random cluster sampling method to recruit 1771 students at early adolescence across three cities, the social economy and cultures of which reflect the status quo in China. In addition, examining the associations between 13 types of ACEs and NSSI, SI, and SA extends the existing literature on these associations, and our mediation analyses provides a deeper understanding of the nature of these associations. Collectively, these finding may have utility for developing preventions and interventions of NSSI and suicidality.
Several limitations should be acknowledged. Firstly, although our study used data from a large cohort study, the present study itself was a cross-sectional design; therefore, it is difficult to establish causal associations or to account for the temporal nature of the relations examined, and thus it may be inappropriate to examine the mediation of depressive and anxiety symptoms. Nonetheless, mediation analysis has been applied in a previous similar study [12], and our findings, particularly regarding the association of ACEs with NSSI, SI, and SA, are consistent with those from several previous cohort studies [40,47]. Secondly, given the study design, recall bias may have occurred as data were collected by retrospective self-report. The prevalence of ACEs, especially those with less of an impression, could thus be underestimated. As a result, the observed associations may be weaker than they truly are [27]. However, the prevalence of ACEs, NSSI, SI, SA, depression, and anxiety were comparable with previous studies [2,3,50], and systematic reviews have demonstrated that data garnered from school-based students regarding self-harm and risk factors are likely to be reliable [51]. Thirdly, although our definition of adolescent smoking as a form of ACEs may be rational, it may cause problems in the interpretation of our results, since adolescent smoking is a risk factor associated with suicidality and NSSI. Fourthly. our study only focused on the presence of different types of ACEs; it may be important to understand the duration of these ACEs and an individual’s subjective experience of the events. This may help to index the extent to which the ACEs impacted participants. Fifthly, the present study was conduct during the COVID-19 pandemic period; thus, the associations of ACEs with NSSI and suicidality may be affected by the COVID-19 pandemic [2,3], although the study sites had a low risk of COVID-19 transmission during the whole study period. Finally, our study only included seventh-grade children and adolescents in traditional school environments. Therefore, we cannot extrapolate our findings to other phases of education or to individuals who are absent from school, potentially due to mental health difficulties. This is important, because the prevalence of some types of ACEs focused on in the present study, such as smoking and being bullied, may change with study phases, and ACEs may be more prevalent in students with a low educational achievement and socioeconomic status [51]. Replication using other populations would help to determine the generality of the findings. Overall, it is advisable to exercise caution when applying our results to the broader population of Chinese children and adolescents.
5. Conclusions
These findings suggest that the risk factors contributing to NSSI, SI, and SA can vary, and that the same types of ACEs may have a different effect on NSSI, SI, and SA. Nevertheless, understanding a youth’s history of ACEs could help in the identification of adolescents who might be at risk of engaging in NSSI, SI, and SA. Moreover, depressive and anxiety symptoms may partially or, in some cases, completely mediate these associations, which suggests that interventions targeting depressive and anxiety symptoms might mitigate the negative effects of ACEs in this population. Further investigations are warranted to determine whether and how interventions for adolescents with a history of ACEs, or who have depressive and anxiety symptoms, can reduce the risk of NSSI and suicidality.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/future1030009/s1; Table S1: Comparison of characteristics between respondent and non-respondent participants; Table S2: Childhood adversity statistics; Table S3: Frequency and prevalence of 8 types of NSSI; Table S4: Logistic regression model of direct and indirect effects through mediators on NSSI and suicidality in males; Table S5: Logistic regression model of direct and indirect effects through mediators on NSSI and suicidality in females.
Author Contributions
Conceptualization, S.G. and J.T.; methodology, S.G.; software, S.G. and R.C.; validation, Y.M. and E.T.; formal analysis, S.G., Y.Y. and R.C.; investigation, S.G., J.T. and Y.M.; resources, J.T.; data curation, T.J. and Y.M.; writing—original draft preparation, S.G. and S.P.L.; writing—review and editing, S.G., T.J., Y.M., S.P.L., B.A.A., R.C., E.T., Y.Y. and J.T.; visualization, S.G. and B.A.A.; supervision, J.T.; project administration, Y.M.; funding acquisition, J.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Natural Science Foundation of China, grant numbers 82073571 and 81773457.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Guangzhou Medical University (protocol code: 2021010002; 13 January 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy.
Acknowledgments
We thank Xiaoqin Liu and Natalie Momen, National Centre for Register-based Research (NCRR), Aarhus University, for their comments and editing.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lim, K.-S.; Wong, C.H.; McIntyre, R.S.; Wang, J.; Zhang, Z.; Tran, B.X.; Tan, W.; Ho, C.S.; Ho, R.C. Global Lifetime and 12-Month Prevalence of Suicidal Behavior, Deliberate Self-Harm and Non-Suicidal Self-Injury in Children and Adolescents between 1989 and 2018: A Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 4581. [Google Scholar] [CrossRef]
- Sara, G.; Wu, J.; Uesi, J.; Jong, N.; Perkes, I.; Knight, K.; O’Leary, F.; Trudgett, C.; Bowden, M. Growth in emergency department self-harm or suicidal ideation presentations in young people: Comparing trends before and since the COVID-19 first wave in New South Wales, Australia. Aust. N. Z. J. Psychiatry 2022, 57, 58–68. [Google Scholar] [CrossRef]
- Yard, E.; Radhakrishnan, L.; Ballesteros, M.F.; Sheppard, M.; Gates, A.; Stein, Z.; Hartnett, K.; Kite-Powell, A.; Rodgers, L.; Adjemian, J.; et al. Emergency Department Visits for Suspected Suicide Attempts among Persons Aged 12–25 Years Before and During the COVID-19 Pandemic—United States, January 2019–May 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 888–894. [Google Scholar] [CrossRef]
- Ribeiro, J.D.; Franklin, J.C.; Fox, K.R.; Bentley, K.H.; Kleiman, E.M.; Chang, B.P.; Nock, M.K. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: A meta-analysis of longitudinal studies. Psychol. Med. 2016, 46, 225–236. [Google Scholar] [CrossRef]
- Hughes, K.; Bellis, M.A.; Hardcastle, K.A.; Sethi, D.; Butchart, A.; Mikton, C.; Jones, L.; Dunne, M.P. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health 2017, 2, e356–e366. [Google Scholar] [CrossRef]
- Russell, A.E.; Joinson, C.; Roberts, E.; Heron, J.; Ford, T.; Gunnell, D.; Moran, P.; Relton, C.; Suderman, M.; Mars, B. Childhood adversity, pubertal timing and self-harm: A longitudinal cohort study. Psychol. Med. 2021, 52, 3807–3815. [Google Scholar] [CrossRef]
- Satinsky, E.N.; Kakuhikire, B.; Baguma, C.; Rasmussen, J.D.; Ashaba, S.; Cooper-Vince, C.E.; Perkins, J.M.; Kiconco, A.; Namara, E.B.; Bangsberg, D.R.; et al. Adverse childhood experiences, adult depression, and suicidal ideation in rural Uganda: A cross-sectional, population-based study. PLoS Med. 2021, 18, e1003642. [Google Scholar] [CrossRef] [PubMed]
- Clements-Nolle, K.; Lensch, T.; Baxa, A.; Gay, C.; Larson, S.; Yang, W. Sexual Identity, Adverse Childhood Experiences, and Suicidal Behaviors. J. Adolesc. Health 2018, 62, 198–204. [Google Scholar] [CrossRef]
- Wan, Y.; Chen, R.; Ma, S.; McFeeters, D.; Sun, Y.; Hao, J.; Tao, F. Associations of adverse childhood experiences and social support with self-injurious behaviour and suicidality in adolescents. Br. J. Psychiatry 2019, 214, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Wang, S.; Gao, X.; Jiang, Z.; Xu, H.; Zhang, S.; Sun, Y.; Tao, F.; Chen, R.; Wan, Y. Patterns of adverse childhood experiences and suicidal behaviors in adolescents: A four-province study in China. J. Affect. Disord. 2021, 285, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Loveday, S.; Hall, T.; Constable, L.; Paton, K.; Sanci, L.; Goldfeld, S.; Hiscock, H. Screening for Adverse Childhood Experiences in Children: A Systematic Review. Pediatrics 2022, 149, e2021051884. [Google Scholar] [CrossRef] [PubMed]
- Peng, C.; Wang, M.; Cheng, J.; Tan, Y.; Huang, Y.; Rong, F.; Kang, C.; Ding, H.; Wang, Y.; Yu, Y. Mediation of Internet addiction on association between childhood maltreatment and suicidal behaviours among Chinese adolescents. Epidemiol. Psychiatr. Sci. 2021, 30, E64. [Google Scholar] [CrossRef]
- Astrup, A.; Pedersen, C.B.; Mok, P.L.; Carr, M.J.; Webb, R.T. Self-harm risk between adolescence and midlife in people who experienced separation from one or both parents during childhood. J. Affect. Disord. 2017, 208, 582–589. [Google Scholar] [CrossRef] [PubMed]
- Wu, N.; Hou, Y.; Zeng, Q.; Cai, H.; You, J. Bullying Experiences and Nonsuicidal Self-injury among Chinese Adolescents: A Longitudinal Moderated Mediation Model. J. Youth Adolesc. 2021, 50, 753–766. [Google Scholar] [CrossRef]
- Casey, S.M.; Varela, A.; Marriott, J.P.; Coleman, C.M.; Harlow, B.L. The influence of diagnosed mental health conditions and symptoms of depression and/or anxiety on suicide ideation, plan, and attempt among college students: Findings from the Healthy Minds Study, 2018–2019. J. Affect. Disord. 2022, 298 Pt A, 464–471. [Google Scholar] [CrossRef]
- Hu, Z.; Yu, H.; Zou, J.; Zhang, Y.; Lu, Z.; Hu, M. Relationship among self-injury, experiential avoidance, cognitive fusion, anxiety, and depression in Chinese adolescent patients with nonsuicidal self-injury. Brain Behav. 2021, 11, e2419. [Google Scholar] [CrossRef]
- Shen, Y.; Meng, F.; Xu, H.; Li, X.; Zhang, Y.; Huang, C.; Luo, X.; Zhang, X.Y. Internet addiction among college students in a Chinese population: Prevalence, correlates, and its relationship with suicide attempts. Depress. Anxiety 2020, 37, 812–821. [Google Scholar] [CrossRef]
- Brausch, A.M.; Whitfield, M.; Clapham, R.B. Comparisons of mental health symptoms, treatment access, and self-harm behaviors in rural adolescents before and during the COVID-19 pandemic. Eur. Child Adolesc. Psychiatry 2023, 32, 1051–1060. [Google Scholar] [CrossRef]
- Ma, L.; Mazidi, M.; Li, K.; Li, Y.; Chen, S.; Kirwan, R.; Zhou, H.; Yan, N.; Rahman, A.; Wang, W.; et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 293, 78–89. [Google Scholar] [CrossRef]
- Iob, E.; Baldwin, J.R.; Plomin, R.; Steptoe, A. Adverse childhood experiences, daytime salivary cortisol, and depressive symptoms in early adulthood: A longitudinal genetically informed twin study. Transl. Psychiatry 2021, 11, 420. [Google Scholar] [CrossRef]
- Shah, S.M.; Nowshad, G.; Dhaheri, F.A.; Al-Shamsi, M.H.; Al-Ketbi, A.M.; Galadari, A.; Joshi, P.; Bendak, H.; Grivna, M.; Arnone, D. Child maltreatment and neglect in the United Arab Emirates and relationship with low self-esteem and symptoms of depression. Int. Rev. Psychiatry 2021, 33, 326–336. [Google Scholar] [CrossRef]
- Holden, R.R.; Lambert, C.E.; La Rochelle, M.; Billet, M.I.; Fekken, G.C. Invalidating childhood environments and nonsuicidal self-injury in university students: Depression and mental pain as potential mediators. J. Clin. Psychol. 2021, 77, 722–731. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Mi, J. Methods for evaluating sexual development in adolescence and its relationship with metabolic syndrome. Chin. J. Evid. Based Pediatr. 2006, 1, 285–291. [Google Scholar] [CrossRef]
- Goleman, D. Emotional Intelligence; Bantam Books: New York, NY, USA, 1995. [Google Scholar]
- Ye, Y.; Dai, X. Development of social support scale for university students. Chin. J. Clinl. Psychol. 2008, 5, 456–458. [Google Scholar]
- Zhao, X.; Zhang, Y.; Li, L.; Zhou, Y.; Li, H.; Yang, S. Reliability and validity of the Chinese version of childhood trauma questionnaire. Chin. J. Clin. Rehabil. 2005, 9, 105–107. [Google Scholar]
- Chen, J.; Guo, C.; Chen, H.; Wang, Y. Investigation of mental health status of pregnant women in late pregnancy and analysis of the influencing factors. Chin. J. Woman Child Health Res. 2021, 32, 1162–1165. [Google Scholar] [CrossRef]
- Ma, Y.; Guo, H.; Guo, S.; Jiao, T.; Zhao, C.; Ammerman, B.A.; Gazimbi, M.M.; Yu, Y.; Chen, R.; Wang, H.H.X.; et al. Association of the Labor Migration of Parents with Nonsuicidal Self-injury and Suicidality among Their Offspring in China. JAMA Netw. Open 2021, 4, e2133596. [Google Scholar] [CrossRef] [PubMed]
- Alcalá, H.E.; von Ehrenstein, O.S.; Tomiyama, A.J. Adverse Childhood Experiences and Use of Cigarettes and Smokeless Tobacco Products. J. Community Health 2016, 41, 969–976. [Google Scholar] [CrossRef]
- Ma, C.; Xi, B.; Li, Z.; Wu, H.; Zhao, M.; Liang, Y.; Bovet, P. Prevalence and trends in tobacco use among adolescents aged 13–15 years in 143 countries, 1999–2018: Findings from the Global Youth Tobacco Surveys. Lancet Child Adolesc. Health 2021, 5, 245–255. [Google Scholar] [CrossRef]
- He, J.; Chen, Z.; Guo, F.; Zhang, J.; Yang, Y.; Wang, Q. A short Chinese version of center for epidemiologic studies depression scale. Chin. J. Behav. Med. Brain Sci. 2013, 22, 1133–1136. [Google Scholar] [CrossRef]
- Zhou, Y.; Bi, Y.; Lao, L.; Jiang, S. Application of GAD-7 in population screening for generalized anxiety disorder. Chin. J. Gen. Pract. 2018, 17, 735–737. [Google Scholar] [CrossRef]
- Tang, J.J.; Yu, Y.; Wilcox, H.C.; Kang, C.; Wang, K.; Wang, C.; Wu, Y.; Chen, R. Global risks of suicidal behaviours and being bullied and their association in adolescents: School-based health survey in 83 countries. eClinicalMedicine 2020, 19, 100253. [Google Scholar] [CrossRef] [PubMed]
- Buis, M.L. Direct and Indirect Effects in a Logit Model. Stata J. 2010, 10, 11–29. [Google Scholar] [CrossRef]
- Merrick, M.T.; Ford, D.C.; Ports, K.A.; Guinn, A.S. Prevalence of Adverse Childhood Experiences From the 2011-2014 Behavioral Risk Factor Surveillance System in 23 States. JAMA Pediatr. 2018, 172, 1038–1044. [Google Scholar] [CrossRef] [PubMed]
- Suglia, S.F.; Koenen, K.C.; Boynton-Jarrett, R.; Chan, P.S.; Clark, C.J.; Danese, A.; Faith, M.S.; Goldstein, B.I.; Hayman, L.L.; Isasi, C.R.; et al. Childhood and Adolescent Adversity and Cardiometabolic Outcomes: A Scientific Statement from the American Heart Association. Circulation 2018, 137, e15–e28. [Google Scholar] [CrossRef]
- Liu, R.T.; Scopelliti, K.M.; Pittman, S.K.; Zamora, A.S. Childhood maltreatment and non-suicidal self-injury: A systematic review and meta-analysis. Lancet Psychiatry 2018, 5, 51–64. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Wang, W.; Yang, J.; Guo, F.; Yin, Z. The effects of alexithymia, experiential avoidance, and childhood sexual abuse on non-suicidal self-injury and suicidal ideation among Chinese college students with a history of childhood sexual abuse. J. Affect. Disord. 2021, 282, 272–279. [Google Scholar] [CrossRef]
- Stansfeld, S.A.; Clark, C.; Smuk, M.; Power, C.; Davidson, T.; Rodgers, B. Childhood adversity and midlife suicidal ideation. Psychol. Med. 2017, 47, 327–340. [Google Scholar] [CrossRef]
- Armiento, J.; Hamza, C.A.; Stewart, S.L.; Leschied, A. Direct and indirect forms of childhood maltreatment and nonsuicidal self-injury among clinically-referred children and youth. J. Affect. Disord. 2016, 200, 212–217. [Google Scholar] [CrossRef]
- Johnstone, J.M.; Carter, J.D.; Luty, S.E.; Mulder, R.T.; Frampton, C.M.; Joyce, P.R. Childhood predictors of lifetime suicide attempts and non-suicidal self-injury in depressed adults. Aust. N. Z. J. Psychiatry 2016, 50, 135–144. [Google Scholar] [CrossRef]
- Nock, M.K.; Borges, G.; Bromet, E.J.; Alonso, J.; Angermeyer, M.; Beautrais, A.; Bruffaerts, R.; Chiu, W.T.; de Girolamo, G.; Gluzman, S.; et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br. J. Psychiatry 2008, 192, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Noel, J.K. Associations between Alcohol Policies and Adolescent Alcohol Use: A Pooled Analysis of GSHS and ESPAD Data. Alcohol Alcohol. 2019, 54, 639–646. [Google Scholar] [CrossRef] [PubMed]
- Hawton, K.; Saunders, K.E.A.; O’Connor, R.C. Self-harm and suicide in adolescents. Lancet 2012, 379, 2373–2382. [Google Scholar] [CrossRef] [PubMed]
- Harrison, R.; Munafò, M.R.; Davey Smith, G.; Wootton, R.E. Examining the effect of smoking on suicidal ideation and attempts: Triangulation of epidemiological approaches. Br. J. Psychiatry 2020, 217, 701–707. [Google Scholar] [CrossRef] [PubMed]
- Serafini, G.; Aguglia, A.; Amerio, A.; Canepa, G.; Adavastro, G.; Conigliaro, C.; Nebbia, J.; Franchi, L.; Flouri, E.; Amore, M. The Relationship between Bullying Victimization and Perpetration and Non-suicidal Self-injury: A Systematic Review. Child Psychiatry Hum. Dev. 2021, 54, 154–175. [Google Scholar] [CrossRef] [PubMed]
- Ford, J.D.; Gómez, J.M. The relationship of psychological trauma and dissociative and posttraumatic stress disorders to nonsuicidal self-injury and suicidality: A review. J. Trauma Dissociation 2015, 16, 232–271. [Google Scholar] [CrossRef]
- Duan, S.; Duan, Z.; Li, R.; Wilson, A.; Wang, Y.; Jia, Q.; Yang, Y.; Xia, M.; Wang, G.; Jin, T.; et al. Bullying victimization, bullying witnessing, bullying perpetration and suicide risk among adolescents: A serial mediation analysis. J. Affect. Disord. 2020, 273, 274–279. [Google Scholar] [CrossRef]
- Garisch, J.A.; Wilson, M.S. Prevalence, correlates, and prospective predictors of non-suicidal self-injury among New Zealand adolescents: Cross-sectional and longitudinal survey data. Child Adolesc. Psychiatry Ment. Health 2015, 9, 28. [Google Scholar] [CrossRef]
- Posner, K.; Melvin, G.A.; Stanley, B.; Oquendo, M.A.; Gould, M. Factors in the assessment of suicidality in youth. CNS Spectr. 2007, 12, 156–162. [Google Scholar] [CrossRef]
- Kessler, R.C.; Berglund, P.; Borges, G.; Nock, M.; Wang, P.S. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. JAMA 2005, 293, 2487–2495. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
