Abstract
Purpose: This study evaluates the association between supervising attending surgeons’ post-residency experience and complication rates during resident-performed phacoemulsification (cataract extraction) surgeries, and to determine whether this relationship changes as the academic year progresses. Methods: A retrospective analysis of 1263 cataract surgeries performed by eight PGY-4 residents under 14 board-certified attendings was conducted at a New York City residency program over two years. Attendings were divided into four groups based on years of post-residency experience. Primary complications included posterior capsule (PC) tears, anterior vitrectomy (AV), capsulorrhexis extensions (CE), and inability to place a one-piece intraocular lens (IOL). Chi-square analyses compared complication rates between attending groups overall, and between the first and second halves of the academic year. Results: A total of 167 primary complications (13.2%) were identified. Attendings with the fewest years of experience (Group 1) supervised significantly more cases with PC tears (χ2 = 8.173, p = 0.004), AV usage (χ2 = 7.748, p = 0.005), and inability to place a one-piece IOL (χ2 = 4.753, p = 0.029), particularly during the first half of the academic year. Notably, supervising attending experience was not correlated with resident complications in the second half of the academic year. Conclusions: Early in the academic year, less experienced attendings supervised cases with higher complication rates, underscoring the critical role of strategic case assignment and targeted mentorship during early surgical training. These findings suggest that aligning resident progression with appropriate supervision can enhance outcomes and support skill development, optimizing both education and patient safety.
1. Introduction
Cataract surgery is one of the most frequently performed procedures worldwide, making it a critical component of ophthalmology residency training [1]. Phacoemulsification has become the gold standard due to its improved safety profile, faster visual recovery, and excellent long-term outcomes when compared with older techniques [2]. While residents strive to achieve outcomes comparable to experienced surgeons, they face a steep learning curve that may manifest with higher complication rates early in their training [3,4,5,6,7]. The previous literature has demonstrated that residents gradually improve their surgical skills with increasing case volume, resulting in reduced complications such as vitreous loss, decreased phacoemulsification times, and improved visual outcomes [8,9,10].
Beyond technical skill acquisition, cataract surgery training also requires residents to develop intraoperative judgment, complication recognition, and decision-making under pressure, all of which are competencies that evolve at different rates across trainees. Early surgical errors are rarely attributable to a single lapse in technique, but rather reflect complex interactions between experience, situational awareness, and the ability to anticipate downstream consequences of intraoperative events. These challenges are most pronounced in the early phases of independent operating, when residents are simultaneously mastering foundational maneuvers and learning to manage unexpected anatomic or technical difficulties. As a result, the learning curve in cataract surgery is not purely mechanical but cognitive and adaptive, underscoring the importance of structured guidance during this critical period of training.
The influence of the supervising attending on resident learning and complication rates has generally been noted, but the specific relationship between supervising attending’s years of post-residency experience and resident surgical outcomes remains less explored. It is plausible that more experienced attendings may better anticipate complications, leading to improved results for cases performed by resident surgeons. On the other hand, some studies have found that beyond a certain point in the academic year, the supervising attending’s experience may have a diminished impact as residents become more proficient [1,3,7]. Understanding this interplay is critical for guiding faculty development, case allocation, and overall educational strategy within training programs.
In this context, the supervising attending functions not only as a safety net, but as a real-time clinical mentor whose experience may directly influence how intraoperative challenges are navigated. Experienced attendings often develop an intuitive sense for when to intervene, when to allow residents to proceed, and how to recalibrate surgical plans before minor issues escalate into major complications. Conversely, early-career attendings, despite strong technical proficiency, may still be refining supervisory skills such as anticipatory guidance, graded autonomy, and adaptive teaching under stress. These differences in supervisory style and experience may be especially consequential at the beginning of the academic year, when residents are most dependent on external guidance and when institutional workflows are still adjusting to new trainees and faculty roles. Yet, despite the centrality of supervision in surgical education, the attending’s experience level is rarely examined as an independent contributor to operative outcomes, and is often treated as a uniform variable across training environments.
In this study, we investigated the association between the attending surgeon’s post-training experience and complication rates during resident-performed cataract surgery. While prior studies have evaluated resident learning curves and overall complication rates, the independent effect of supervising attending surgeons’ post-residency experience, particularly how its influence may change over the course of the academic year, has not been previously examined. By further examining outcomes in both the first and second halves of the academic year, we aimed to elucidate how attending experience shapes resident performance over time. This information could help residency programs optimize mentorship models, enhance surgical teaching methodologies, and ultimately improve patient safety.
2. Materials and Methods
Cataract surgery operative notes at a residency training program in the New York City metropolitan area were analyzed over a two-year period as a part of this retrospective cohort study. All surgeries took place from June 2022 to May 2024, with all data collection completed by May 2024. Our analysis included eight resident surgeons in their final year (PGY-4) of training, representing 100% of resident-performed cataract cases during the study timeframe. Specific complications and years of experience of the supervising attending were documented and analyzed. Cases were further divided into the first and second half of the academic year. During data extraction, no operative notes were excluded from the study.
Primary complications included posterior capsule tear, utilization of anterior vitrectomy, capsulorrhexis extensions, and cases where a one-piece intraocular lens was not placed in the eye. Cases where a one-piece intraocular lens was not placed included situations where the patient was left aphakic, an anterior chamber intraocular lens was used, or a three-piece intraocular lens was placed. This was generally due to several etiologies such as posterior capsular tear, severe zonular loss, anterior capsule run out, or lens drop. Each complication was recorded and analyzed as a distinct outcome given its independent clinical and educational relevance. Secondary complications measured were severe zonular loss, central Descemet’s membrane detachment, iridodialysis, and retrobulbar hemorrhage.
Fourteen supervising attendings were included in this analysis. All attendings in this study were board-certified by the American Board of Ophthalmology. Each attending was placed into one of four groups based upon years of experience after their own training was completed. Group one consisted of seven attendings who had zero to two years of experience after residency; group two consisted of three attendings with three to five years of experience; group three consisted of two attendings with five to twenty-five years of experience; and group four had two attendings with over twenty-five years of experience. Cases were assigned based on the institution’s standard operating room scheduling practices rather than resident skill level or case complexity. Moreover, attending groups were defined exclusively by years of post-residency experience and did not reflect resident training level or surgical volume.
A chi-square statistical model was utilized for statistical analyses. We generated multiple models to determine if the years of attending experience correlated to complications during resident cataract surgery, and whether these complications occurred more frequently in the first half of the year when compared to the second half of the year. Statistical Package for the Social Sciences (SPSS), Version 30 (IBM Inc. Armonk, NY), was utilized and a p-value < 0.05 was considered statistically significant for all analyses.
This study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki and applicable institutional and federal regulations governing human subject research. The protocol was reviewed by the Institutional Review Board (IRB) of NYC Health and Hospitals (IRB # 23-12-374-05H, approval date: 29 June 2023) and determined to be exempt due to the retrospective nature of the study and the use of fully de-identified data.
3. Results
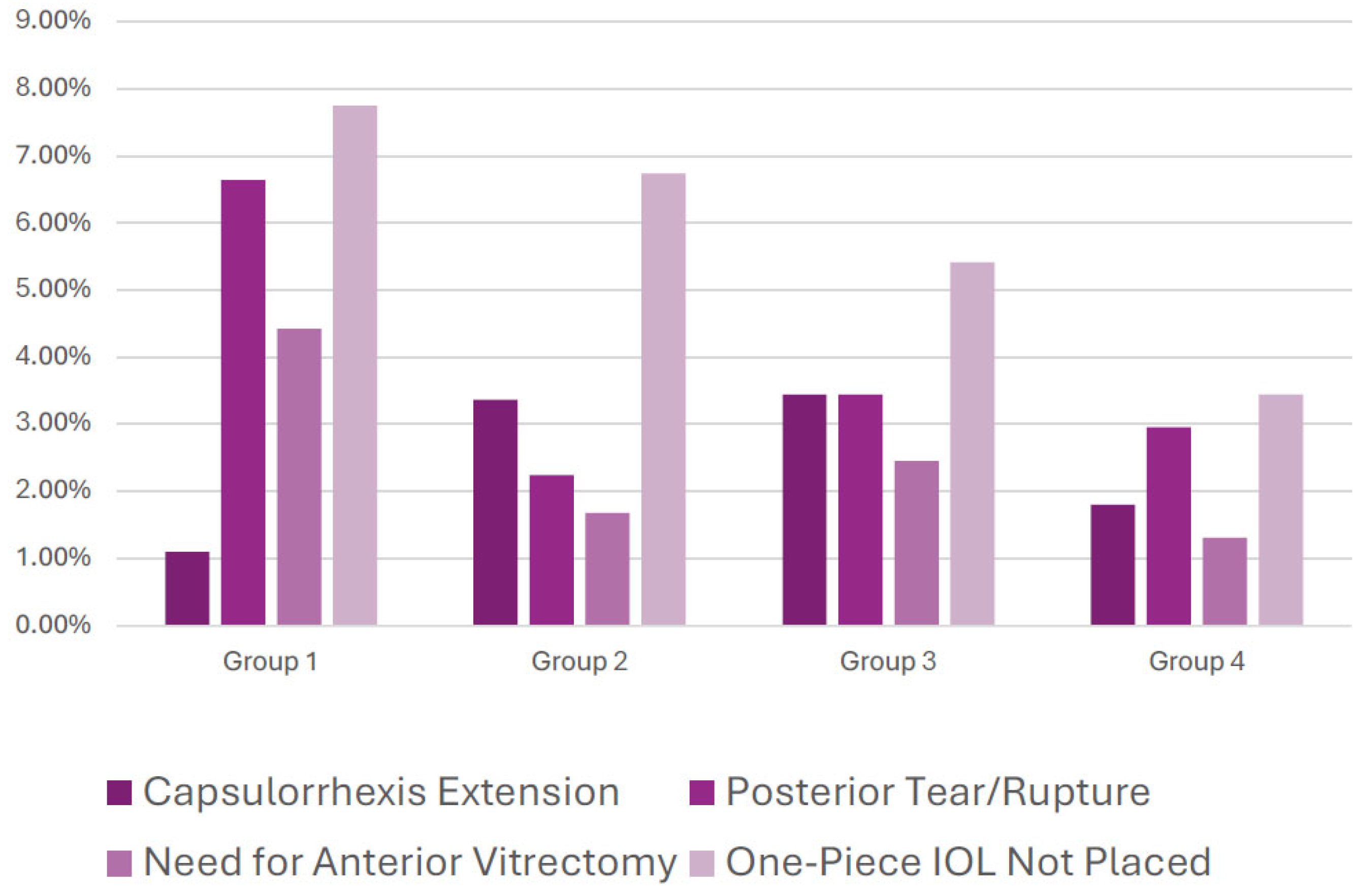
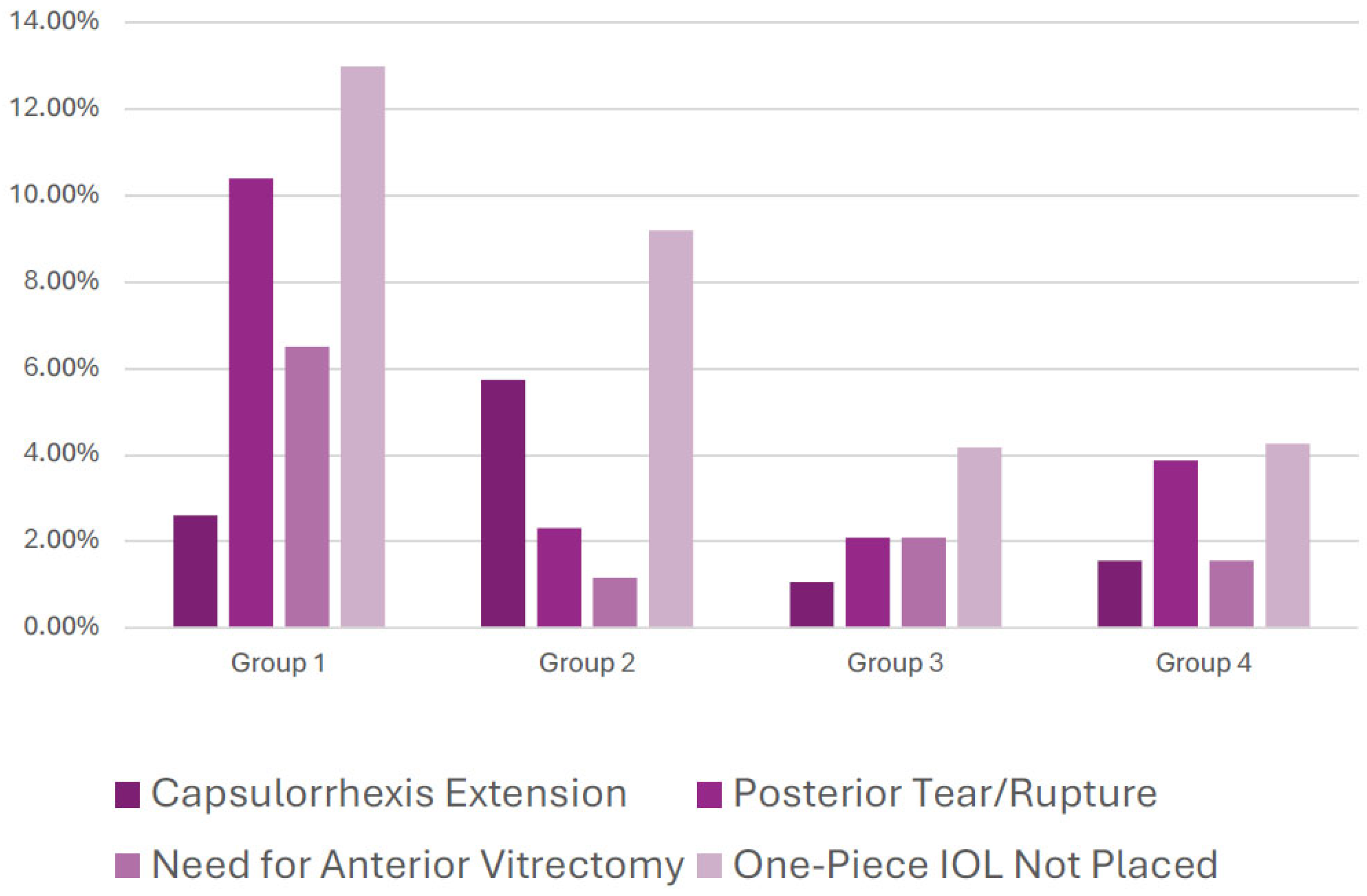
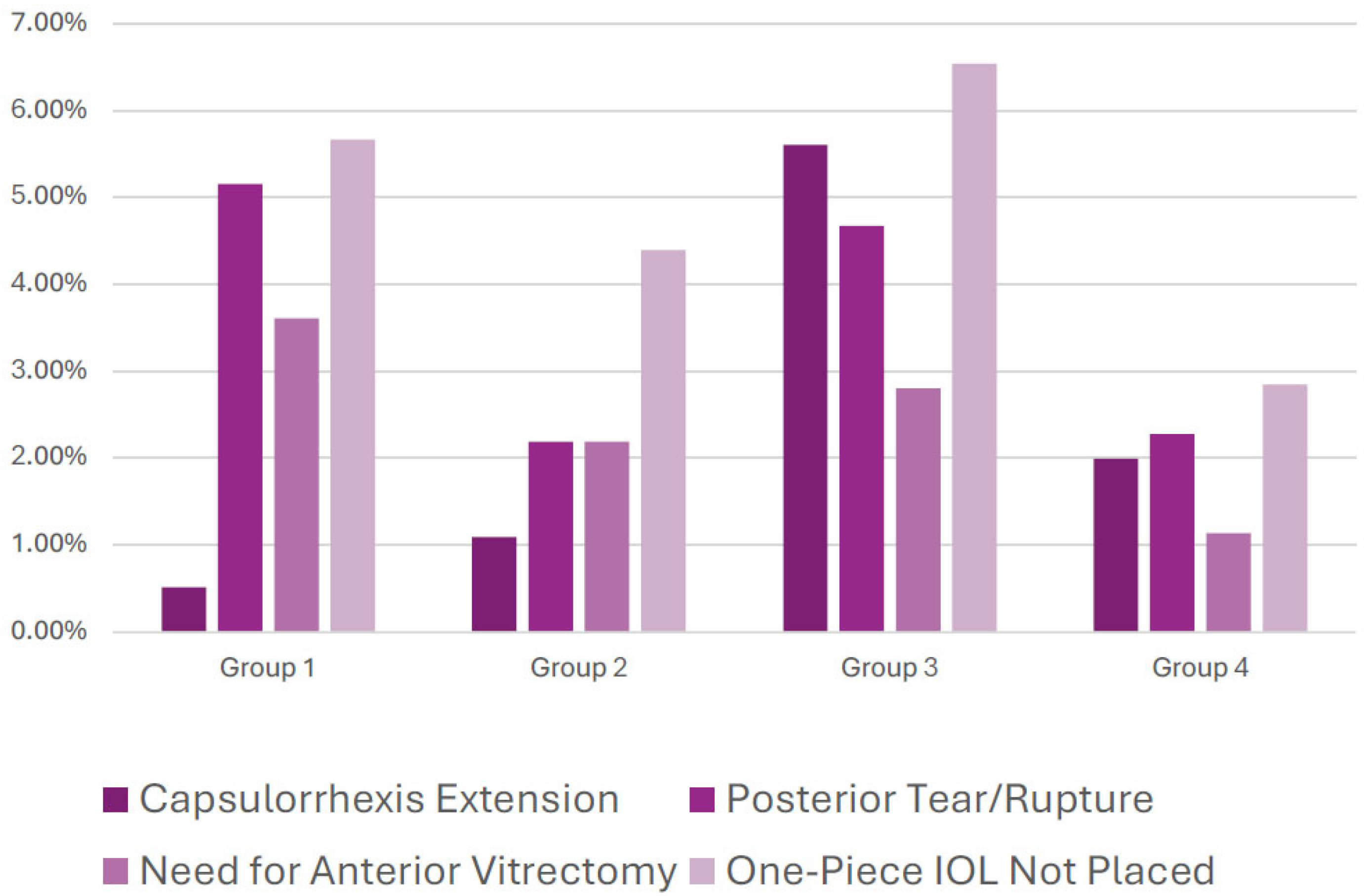
A total of 1263 cataract surgery cases were included in our analysis. Overall, 167 primary complications occurred over the two-year study period (13.2%). Primary complications were most likely to occur in Group 1 (19.9%) and least likely to occur in group 4 (9.5%). Complications are depicted graphically for the entire two-year study period in Figure 1, with detailed numerical data summarized in Table 1. Time-based stratifications include the first half of the academic year (Figure 2) and the second half of the academic year (Figure 3), with corresponding numerical data also included in the lower portion of Table 1.
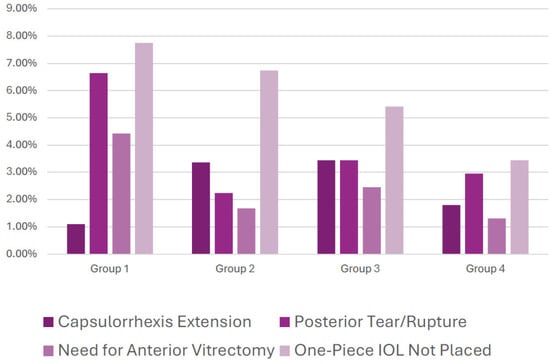
Figure 1.
Rates of primary resident cataract complications, subdivided by complication and attending group, over the full 2-year study period. Groups 1–4 represent supervising attendings with 0–2, 2–5, 5–25, and 25+ years of postgraduate experience, respectively.

Table 1.
Rate of primary resident cataract complications, subdivided by complication, attending group, and by the first and second halves of the academic year. Groups 1–4 represent supervising attendings with 0–2, 2–5, 5–25, and 25+ years of postgraduate experience, respectively. Chi-square analyses for each subgroup are also included, with each statistically significant model marked with an asterisk (*).
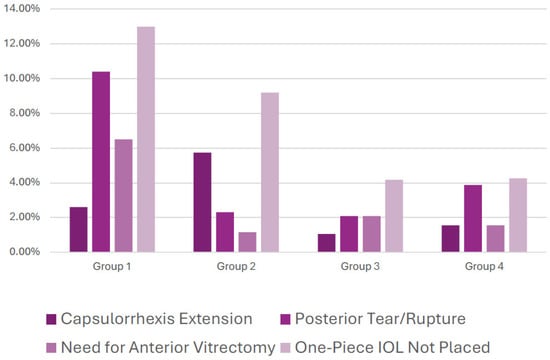
Figure 2.
Rates of primary resident cataract complications, subdivided by complication and attending group, over the first half of each academic year, only. Groups 1–4 represent supervising attendings with 0–2, 2–5, 5–25, and 25+ years of postgraduate experience, respectively.
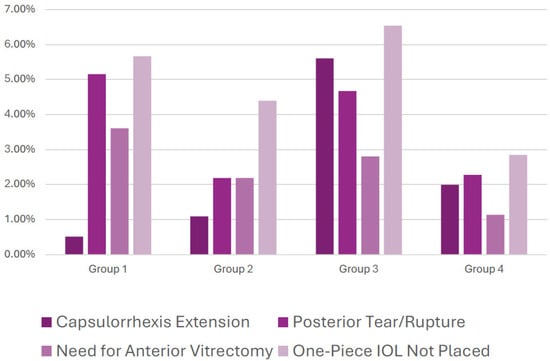
Figure 3.
Rates of primary resident cataract complications, subdivided by complication and attending group, over the second half of each academic year, only. Groups 1–4 represent supervising attendings with 0–2, 2–5, 5–25, and 25+ years of postgraduate experience, respectively.
Attendings in Group 1 supervised a significantly greater percentage of cases complicated by posterior capsule tears, both overall (χ2 = 8.173, p = 0.004) and in the first six months (χ2 = 8.39, p = 0.004) of the year, as compared to other groups. Cases necessitating anterior vitrectomy were also more frequently encountered under Group 1 supervision, both overall (χ2 = 7.748, p = 0.005) and in the first half of the year (χ2 = 6.973. p = 0.008). Similarly, Group 1 attendings oversaw a significantly greater proportion of cases in which a one-piece intraocular lens could not be placed, both overall (χ2 = 4.753, p = 0.029) and in the first six months (χ2 = 8.390, p = 0.010). Importantly, none of these three complications—posterior capsule tear (χ2 = 2.587, p = 0.108), need for anterior vitrectomy (χ2 = 2.637, p = 0.104), or inability to place a one-piece IOL (χ2 = 1.194, p = 0.277)—differed significantly across attending groups during the second half of the academic year. Capsulorrhexis extension rates did not differ significantly between groups overall (χ2 = 1.762, p = 0.184), in the first half of the academic year (χ2 = 0.032, p = 0.859), or in the second half of the academic year (χ2 = 3.00, p = 0.084).
4. Discussion
Our findings highlight a notable interplay between attending experience and resident surgical outcomes during the initial months of training. Attending surgeons with 0–2 years of post-residency experience supervised cases with significantly higher complication rates—specifically posterior capsule tears, the need for anterior vitrectomy, and inability to implant a one-piece IOL. Of note, these complications rates were significantly higher only during the first half of the academic year, and not in the second half. These results align with existing literature emphasizing that early in the learning curve, both resident and supervising surgeon experience can influence outcomes [5,6,7,11,12]. More senior attendings may possess a refined ability to anticipate difficulties, provide timely interventions, and guide residents through complex intraoperative scenarios, thereby reducing the likelihood of vision-threatening complications [13,14,15].
Beyond technical oversight, the role of the supervising attending during resident-performed surgery encompasses real-time guidance, situational awareness, and anticipatory judgment that may only be refined through years of independent surgical experience. Early-career attendings often possess excellent technical skill yet may still be developing the nuanced ability to recognize subtle intraoperative cues that precede major complications, such as early zonular instability, posterior capsular billowing, or progressive corneal wound distortion. These early warning signs frequently determine whether timely intervention prevents escalation into vitreous loss or lens instability. In contrast, senior attendings may intervene earlier, alter the surgical plan preemptively, or guide residents through micro-adjustments that avert complication cascades. This distinction is particularly relevant in the first half of the academic year, when residents themselves are still learning to recognize these inflection points. The convergence of two evolving learning curves, resident surgeon and early-career attending, may therefore compound procedural risk early in the year. Importantly, this does not imply a deficit in the abilities of newer attendings, but rather reflects the complex and often underappreciated skill set required for surgical teaching. Supervision in academic surgery is not merely oversight; it is a specialized form of clinical judgment that integrates pedagogy, patient safety, and operative strategy. These findings support the notion that teaching cataract surgery effectively represents a distinct competency that develops longitudinally and benefits from intentional faculty development, peer mentorship, and exposure to high-volume supervisory experience.
By the second half of the year, no significant differences in complication rates were observed among groups, despite initial disparities. This temporal shift suggests that residents develop a level of competence and independence that reduces their reliance on the attending’s experience over time. This phenomenon parallels the findings of Randelman et al., who reported that resident complication rates and surgical times significantly improved beyond the first 80 cases, as well as several other authors who noted substantial improvements in skill and efficiency as residents’ case numbers increased [1,7,16,17]. Similar trends have been noted in other training environments, where residents eventually match or approach the performance standards of experienced surgeons, given adequate surgical volume and practice [18]. Therefore, one plausible explanation for our findings is that early-career supervising attendings and residents may share overlapping learning curves early in the academic year, with supervisory experience during resident-performed cases evolving alongside resident skill acquisition.
The lack of significant group differences in capsulorhexis extension rates may reflect improvements in teaching methods and the use of adjunctive tools. Various studies have highlighted techniques such as the use of capsular dyes, wet-lab training, and stepwise simulation exercises to build initial competency [19,20,21]. These educational innovations potentially standardize certain steps of the procedure, enabling even less experienced attendings to effectively guide trainees early on with these tasks. The development and implementation of systematic surgical evaluation techniques have significantly enhanced the assessment of resident surgical skills and competency. Tools such as the Global Rating Assessment of Skills in Intraocular Surgery (GRASIS) and the Objective Assessment of Skills in Intraocular Surgery (OASIS) have been proposed to provide structured and objective evaluations of surgical performance [22,23]. GRASIS evaluates not only technical surgical skills but also clinical knowledge, and interpersonal abilities, offering a comprehensive view of resident competence. Similarly, OASIS combines a standardized evaluation form with a unique database of surgical cases, enabling detailed assessments of surgical events and skill progression. These tools are particularly valuable in identifying areas where residents may require additional training, allowing for targeted interventions to address skill gaps and optimize outcomes.
In addition to direct evaluation, preoperative case difficulty scoring systems, such as the one proposed by Osborne et al., provide a complementary approach to improving resident training [24]. By predicting the likelihood of complications, such as posterior capsule rupture, these systems help designate appropriate cases to trainees based on their experience level, ensuring that residents are neither overwhelmed nor underchallenged during their training. Integrating such scoring systems into residency programs could also support inexperienced supervising attendings by guiding case selection, particularly during the early months of the academic year when resident skill acquisition is still in its nascent stages. These findings also highlight the importance of institutional support for early-career attending surgeons who supervise resident cases. Structured faculty mentorship, opportunities for co-supervision with senior attendings, and targeted teaching preparation may help newer attendings anticipate intraoperative challenges while simultaneously developing their instructional skills. Such approaches could enhance both resident education and patient safety, particularly during the early months of the academic year.
These findings also carry implications for how surgical outcomes are interpreted in the context of residency training. Complication rates in academic centers are often discussed primarily in relation to resident proficiency, yet our results suggest that supervisory experience represents an important contextual variable that warrants consideration in both quality metrics and benchmarking efforts. Programs comparing complication rates across institutions or over time may benefit from accounting for faculty experience distributions, particularly when evaluating early-year performance. Failure to do so risks attributing variation to resident capability alone, potentially obscuring meaningful opportunities for system-level improvement. Furthermore, in an era of increasing public transparency and patient-facing outcome reporting, understanding the multifactorial nature of surgical risk in training environments becomes essential for responsible communication with patients. Framing complications within a model that recognizes the dynamic interplay between trainee progression, supervisory expertise, and institutional structure allows for a more holistic interpretation of outcomes. It also reinforces the ethical imperative to design training systems that protect patients while preserving robust educational experiences. Rather than viewing supervision as a static safeguard, our findings support a more nuanced perspective that supervision itself evolves, and its maturation is an integral component of the educational ecosystem. Acknowledging this evolution can help programs better support faculty, optimize resident development, and ultimately align the goals of patient safety and surgical education.
The study’s limitations include its retrospective design and the relatively small numbers of attendings in the more experienced groups, which may limit generalizability due to selection bias. Differences in total case volume across attending groups reflect variation in faculty tenure and operating room schedules rather than intentional differences in case assignment, and each group included a sufficient number of cases to allow for statistical comparison. Other unmeasured factors, such as the teaching style of individual attendings or the distribution of resident case volume, could have affected complication rates. Resident surgical performance is also influenced by factors beyond direct attending supervision, including simulation training, wet-lab experience, didactic preparation, and cumulative case exposure, which were not independently assessed in this study. Furthermore, we did not stratify cases by complexity, which may have influenced complication rates. Some complications could have been influenced by patient-specific factors such as dense cataracts or preexisting zonular instability rather than attending or resident experience alone [25,26]. Additionally, Group 3 encompassed a broad range of attending experience (5–25 years), which may have masked differences within this cohort. Future directions should focus on prospective, multi-institutional studies and the incorporation of preoperative risk stratification tools to tailor case difficulty to resident skill level [24].
Despite these limitations, this study has several notable strengths that enhance the relevance and interpretability of its findings. First, the analysis includes a large, consecutive cohort of resident-performed cataract surgeries across multiple academic years, providing a robust sample that reflects real-world training environments rather than highly selected cases. Second, by stratifying outcomes not only by supervising attending experience but also by time within the academic year, this study captures the dynamic nature of surgical education, which is an aspect that is often overlooked in prior literature which typically treats training exposure as static. This temporal approach allows for a more nuanced understanding of when supervision matters most and identifies early academic months as a particularly important period for targeted intervention. Third, the study evaluates clinically meaningful complications that directly affect patient outcomes and resident learning, rather than relying solely on surrogate markers such as operative time or subjective performance scores. Finally, the exclusive focus on supervising attending experience as an independent variable represents a novel contribution to the cataract education literature. While previous studies have emphasized resident learning curves, few have examined how faculty experience shapes these curves in practice. By highlighting supervision as an active determinant of outcomes rather than a passive backdrop, this work expands the conversation around surgical safety in training programs and provides actionable insights for residency leadership, faculty development initiatives, and institutional policy.
Our findings emphasize the importance of pairing new residents operating as primary surgeons with experienced attendings, particularly during the critical early months of the academic year. Targeted mentorship, thoughtful case selection, and structured training protocols can help mitigate complications while fostering a supportive learning environment. By focusing on these dual dimensions of residents’ and teaching attendings’ growth, residency programs can enhance patient safety and equip trainees with the confidence and technical skills needed for independent practice.
5. Conclusions
To the best of our knowledge, this study is the first to directly quantify the association of attending experience on resident cataract complications using a refined quantitative approach. Our findings highlight the pivotal role of supervising attendings’ experience in influencing complication rates during the early months of resident-performed cataract surgeries. While less experienced supervision was associated with higher complication rates early in the first half of the year, these differences diminished as residents gained proficiency over time. This underscores the dynamic interplay between resident learning curves and attending expertise, reinforcing the need for programs to strategically allocate supervisory roles during early training. These findings are associative rather than causal, and future prospective studies are warranted.
Author Contributions
Conceptualization, P.P.S., J.M.N., S.V., D.Z., J.A.W. and I.C.; methodology, P.P.S., J.M.N., S.V., D.Z., J.A.W. and I.C.; validation, P.P.S., S.V. and I.C.; formal analysis, P.P.S.; investigation, P.P.S., J.M.N., S.V., D.Z., J.A.W. and I.C.; writing—original draft preparation, P.P.S., J.M.N. and I.C.; writing—review and editing, P.P.S., J.M.N., S.V., D.Z., J.A.W. and I.C.; supervision, J.A.W. and I.C.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. The full protocol was reviewed and determined to be exempt by the Institutional Review Board (IRB) of NYC Health and Hospitals (IRB # 23-12-374-05H, approval date: 29 June 2023) as all data was de-identified.
Informed Consent Statement
Patient consent was waived due to the retrospective nature of the study, and all data was de-identified.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Randleman, J.B.; Wolfe, J.D.; Woodward, M.; Lynn, M.J.; Cherwek, D.H.; Srivastava, S.K. The Resident Surgeon Phacoemulsification Learning Curve. Arch. Ophthalmol. 2007, 125, 1215–1219. [Google Scholar] [CrossRef] [PubMed]
- Davis, G. The Evolution of Cataract Surgery. Mo. Med. 2016, 113, 58–62. [Google Scholar] [PubMed]
- Quillen, D.A.; Phipps, S.J. Visual outcomes and incidence of vitreous loss for residents performing phacoemulsification without prior planned extracapsular cataract extraction experience. Am. J. Ophthalmol. 2003, 135, 732–733. [Google Scholar] [CrossRef] [PubMed]
- Tayanithi, P.; Pungpapong, K.; Siramput, P. Vitreous loss during phacoemulsification learning curve performed by third-year residents. J. Med. Assoc. Thail. 2005, 88, S89–S93. [Google Scholar]
- Blomquist, P.H.; Rugwani, R.M. Visual outcomes after vitreous loss during cataract surgery performed by residents. J. Cataract Refract. Surg. 2002, 28, 847–852. [Google Scholar] [CrossRef]
- Cruz, O.A.; Wallace, G.W.; Gay, C.A.; Matoba, A.Y.; Koch, D.D. Visual results and complications of phacoemulsification with intraocular lens implantation performed by ophthalmology residents. Ophthalmology 1992, 99, 448–452. [Google Scholar] [CrossRef]
- Corey, R.P.; Olson, R.J. Surgical outcomes of cataract extractions performed by residents using phacoemulsification. J. Cataract Refract. Surg. 1998, 24, 66–72. [Google Scholar] [CrossRef]
- Smith, J.H.; Seiff, S.R. Outcomes of cataract surgery by residents at a public county hospital. Am. J. Ophthalmol. 1997, 123, 448–454. [Google Scholar] [CrossRef]
- Badoza, D.A.; Jure, T.; Zunino, L.A.; Argento, C.J. State-of-the-art phacoemulsification performed by residents in Buenos Aires, Argentina. J. Cataract Refract. Surg. 1999, 25, 1651–1655. [Google Scholar] [CrossRef]
- Tarbet, K.J.; Mamalis, N.; Theurer, J.; Jones, B.D.; Olson, R.J. Complications and results of phacoemulsification performed by residents. J. Cataract Refract. Surg. 1995, 21, 661–665. [Google Scholar] [CrossRef]
- Albanis, C.V.; Dwyer, M.A.; Ernest, J.T. Outcomes of extracapsular cataract extraction and phacoemulsification performed in a university training program. Ophthalmic Surg. Lasers 1998, 29, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Hollander, D.A.; Vagefi, M.R.; Seiff, S.R.; Stewart, J.M. Bacterial endophthalmitis after resident-performed cataract surgery. Am. J. Ophthalmol. 2006, 141, 949–951. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, D.V.; Harrison, J.C.; Carriere, V.M. Cataract extraction with lens implantation at Biloxi Veterans Affairs Medical Center: Experience of ophthalmology residents. Ann. Ophthalmol. 1994, 26, 47–49. [Google Scholar] [PubMed]
- Karp, K.O.; Albanis, C.V.; Pearlman, J.B.; Goins, K.M. Outcomes of temporal clear cornea versus superior scleral tunnel phacoemulsification incisions in a university training program. Ophthalmic Surg. Lasers 2001, 32, 228–232. [Google Scholar] [CrossRef]
- Puri, S.; Kiely, A.E.; Wang, J.; Woodfield, A.S.; Ramanathan, S.; Sikder, S. Comparing resident cataract surgery outcomes under novice versus experienced attending supervision. Clin. Ophthalmol. 2015, 9, 1675–1681. [Google Scholar] [CrossRef]
- Lee, J.S.; Hou, C.H.; Yang, M.L.; Kuo, J.Z.; Lin, K.K. A different approach to assess resident phacoemulsification learning curve: Analysis of both completion and complication rates. Eye 2009, 23, 683–687. [Google Scholar] [CrossRef]
- Martin, K.R.G.; Burton, R.L. The phacoemulsification learning curve: Per-operative complications in the first 3000 cases of an experienced surgeon. Eye 2000, 14, 190–195. [Google Scholar] [CrossRef]
- Noecker, R.J.; Allinson, R.W.; Snyder, R.W. Resident phacoemulsification experience using the in situ nuclear fracture technique. Ophthalmic Surg. 1994, 25, 216–221. [Google Scholar] [CrossRef]
- Fisher, J.B.; Binenbaum, G.; Tapino, P.; Volpe, N.J. Development and face and content validity of an eye surgical skills assessment test for ophthalmology residents. Ophthalmology 2006, 113, 2364–2370. [Google Scholar] [CrossRef]
- Henderson, B.A.; Ali, R. Teaching and assessing competence in cataract surgery. Curr. Opin. Ophthalmol. 2007, 18, 27–31. [Google Scholar] [CrossRef]
- Binenbaum, G.; Volpe, N.J. Ophthalmology resident surgical competency: A national survey. Ophthalmology 2006, 113, 1237–1244. [Google Scholar] [CrossRef]
- Cremers, S.L.; Lora, A.N.; Ferrufino-Ponce, Z.K. Global Rating Assessment of Skills in Intraocular Surgery (GRASIS). Ophthalmology 2005, 112, 1655–1660. [Google Scholar] [CrossRef]
- Cremers, S.L.; Ciolino, J.B.; Ferrufino-Ponce, Z.K.; Henderson, B.A. Objective Assessment of Skills in Intraocular Surgery (OASIS). Ophthalmology 2005, 112, 1236–1241. [Google Scholar] [CrossRef]
- Osborne, S.A.; Severn, P.; Bunce, C.V.; Fraser, S.G. The use of a pre-operative scoring system for the prediction of phacoemulsification case difficulty and the selection of appropriate cases to be performed by trainees. BMC Ophthalmol. 2006, 6, 38. [Google Scholar] [CrossRef]
- Miller, K.M.; Oetting, T.A.; Tweeten, J.P.; Carter, K.; Lee, B.S.; Lin, S.; Nanji, A.A.; Shorstein, N.H.; David, C.; Musch, D.C. Cataract in the Adult Eye Preferred Practice Pattern. Ophthalmology 2022, 129, P1–P126. [Google Scholar] [CrossRef]
- Kang, C.; Lee, M.J.; Chomsky, A.; Oetting, T.A.; Greenberg, P.B. Risk factors for complications in resident-performed cataract surgery: A systematic review. Surv. Ophthalmol. 2024, 69, 638–645. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.