Abstract
The article describes measurements and measuring devices as they apply to assessment, therapy and research in orofacial myology and myofunctional therapy. Although the list is by no means complete, a wide range of items, their objectivity, complexity, applicability and accuracy is presented.
INTRODUCTION
The need for a reliable set of measurements to support orofacial myology (OFM) and myofunctional therapy was reason enough to contact various clinicians across three continents and inquire about their measurements and measuring devices. The result was the awareness that although there are indeed many different devices commercially available for assessment, therapy and even research, their reliability remains questionable, as well as their application to OFM in daily practice. It is also difficult to find universal agreement that they measure what they are supposed to measure. Nevertheless, many instruments and procedures are discussed in this article.
The IAOM recognizes the need to provide an evidence-based practice (EBP) description of the various processes associated with myofunctional disorders, the result of which should increase the clinician’s knowledge and skills (ASHA, 1992). To this end, this article reviews selected instrumental and clinical documentation procedures, many of which have been utilized in diagnostic and therapeutic procedures with myofunctional disorders.
In a Position statement, in 2005, the American Speech-Language and Hearing Association (ASHA) stated that an evidence-based practice should integrate both clinical expertise and systematic research. Therefore, in order for clinicians to validate their experience and develop an evidence-based practice, there is the need for them to have access to affordable, reliable and valid measurement instruments (Clark, 2003; Robey, 2005).
Documentation should be a part of daily clinical work rather than being left solely to laboratory experimentation. Documentation is needed to fully validate myofunctional therapy. This aspiration can be achieved by using a variety of measurement tools to obtain quantitative data, in combination with qualitative data obtained through clinical experience. Therefore, clinical documentation should represent a joint collaboration between clinical processes and the research laboratory.
OVERVIEW OF INSTRUMENTATION AND MEASUREMENTS
Measurements can be obtained to describe and quantify specific functions or dysfunctions either during screenings or full evaluations by referencing selected anatomic landmarks. Measurements at landmarks are useful to establish a therapy baseline, to monitor progress, and to determine whether stated goals of therapy have been accomplished.
While some types of measurements may lack scientific support, they can be of great motivational value for patients. As long as such measures are used for this purpose, and this purpose is recognized by the clinician, such measures can and should be incorporated into clinical practice.
While most measurements presented here are useful in documenting daily clinical progress, not all of the measurements and measuring devices may be considered appropriate for research purposes. Whenever possible, the author will recommend instruments that may be considered for current studies or for promising future research.
Due to the interdisciplinary nature of myofunctional therapy, measurement techniques and procedures have been derived from a variety of professional fields. As a result, orofacial myofunctional therapists (OMT) may utilize measurements familiar to speech language pathologists (SLP), orthodontists, and otorhinolaryngologists-head and neck surgeons, (ENT).
There are many types of measurements and measuring devices available to OMT. An example of a subjective and functional measurement is describing the strength of the masseter muscles by asking the patient to bite into occlusion while the therapist palpates the muscles. Another example is estimating the strength of the tongue by pushing the tongue forward against a tongue depressor held with resistance against it.
Examples of more objective and structural measurements include determining the bicanine width by using a caliper or a ruler, or evaluating the strength of the tongue with the Iowa Oral Performance Instrument (IOPI). An example of a low-tech device is the use of a simple ruler as opposed to a high tech palatometer. An example of an inexpensive device is a range of motion ruler, in contrast to an expensive instrument such as the Surface Electromyograph (SEMG). Some measuring devices may be expensive and still unsuitable for research, such as the myoscanner, while others, like the palatometer are promising for research in orofacial myology. However, just as in other professions, an economic investment is needed to document success. Over time the price of technology usually becomes less expensive even for the typical private practice setting.
SUBJECTIVE MEASURES APPROPRIATE FOR INCLUSION IN EXAMINATION REPORTS
The Mallampati Score
The Mallampati score is routinely used by anesthesiologists to estimate the difficulty of an impending intubation (Mallampati et al., 1985; Ovassapian et al., 2002).
It describes, in relative gradations, the visibility of the oral isthmus and posterior pharyngeal wall. The boundaries of the oral isthmus extend laterally between the faucial pillars and vertically from the uvula/posterior end of the soft palate to the base of the tongue. This dimension represents the area of separation of the oral cavity from the nasopharynx.
This scoring system is divided in four classes:
Class 1 denotes that a full view is available of the faucial arches, the posterior pharyngeal wall and the uvula. For dentists, orthodontists, dental hygienists or orofacial myologists, a Class 1 view of the faucial isthmus would represent the best view of this area.
In Class 2, the uvula is 50% visible, with a partial view of the posterior pharyngeal wall.
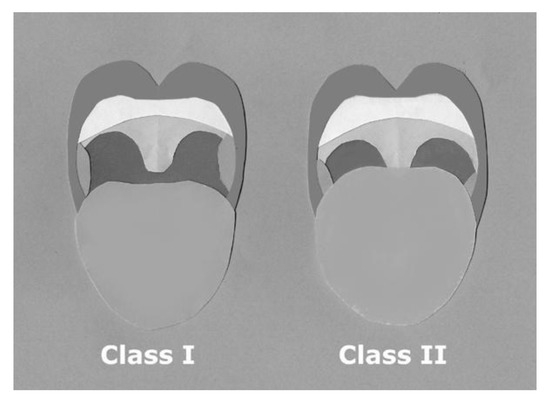
Figure 1.
Mallampati Score Class I and Class II.
In Class 3, only a small part of the uvula is visible where it joins the posterior of the soft palate.
In Class 4, nothing but the tongue is visible. It is easy to imagine why this is the most difficult situation for anesthesiologists and for any other professionals who provide treatment in the oral cavity.
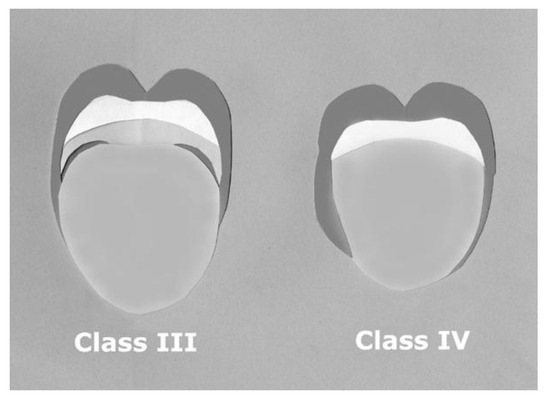
Figure 2.
Mallampati Score Class III and Class IV.
Overall, the Mallampati score is a clinically useful and simple way to describe the degree of visibility of the oral isthmus and nasopharynx because it involves a subjective, 4-point rating scale to quantify the size of the isthmus. The results of the oral visibility should be recorded in patient charts in the practice of orofacial myology. Over time, as insights are gleaned from such observations, there may be guidelines developed from specific Mallampati scores to select a particular type of swallow therapy.
Tonsil Grading
During intraoral screenings and more complete evaluations, it would be appropriate to estimate the size of the faucial tonsils (Harley, 2002; Li et al., 2002). Such descriptions are not intended as a diagnosis of tonsillar pathology, but are intended merely as a descriptive estimate of tonsillar size. This is an appropriate inclusion in a myofunctional therapist’s evaluation protocol.
The tonsils are typically graded based on the percentage of oropharyngeal space occupied by them. In viewing the faucial tonsils, the clinician could assign a grade zero (0) in an adult with no tonsils visible in the tonsillar fossae. Since the growth cycle for faucial tonsils usually results in complete involution (or atrophy) of these tonsillar masses by age 20, it would not be surprising to find no tonsillar tissue remnants in the fossae.
Also, for those adults who have had a tonsillectomy, the tonsillar space would be graded as a zero. In case of granular tissue after a tonsillectomy, the grade assigned would be zero. Furthermore, the presence of retained tonsils in patients over age 20 signals a history of earlier bouts of tonsillitis, which often results in the maintenance of tonsillar tissue beyond the expected range of full involution of the tonsils.
If the tonsils are just slightly protruding or visible in the fossae, they could be graded 1, as long as they protrude less that approximately 25% into the oropharyngeal space.
The faucial tonsils can be given a grade 2 if the space they occupy accounts for up to 50% of the oral isthmus.
A grade 3 indicates tonsillar hypertrophy beyond 50% of the horizontal diameter of the oral isthmus.
A grade 4 is given for tonsils that occupy 75% or more of the space.
The most difficult situation of all is grade 4+, or kissing tonsils, in which tonsils are so hypertrophic that they approximate. When tonsils are hypertrophic to this extent, they may appear asymmetric and not necessarily touching in the midline.
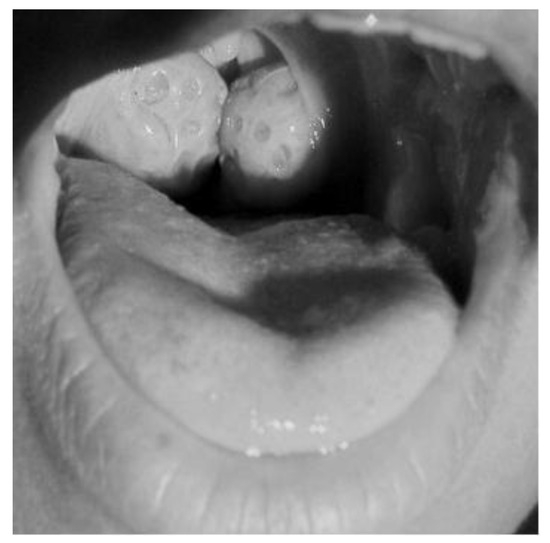
Figure 3.
Kissing Tonsils. (Courtesy of National Institute of Health).

Figure 4.
Tonsillectomy. (Courtesy of Monroe Community College, Rochester, New York).
The life cycle of faucial tonsils and adenoids may be similar, but it is not unusual for the tonsils to grow and involute at a different rate from the adenoids (also known as the pharyngeal tonsils). Moreover, the adenoid has an extra layer of respiratory epithelium not present on the tonsils, so they differ even at the histological level. Therefore, clinicians are advised not to presume anything about the size of the adenoids from viewing the tonsils.
Clearly, even with a grading system, calculating the percentage of oropharyngeal space remains a subjective skill that requires experience. Good inter-and intra-reliability judgments can be achieved through experience. As a descriptive measure, however, the features of this grading system have great utility for the clinician, and are important inclusions in clinical reports.
Rulers
A simple device to assess the facial growth is the Facial INDex of Esthetic Relations (FINDER) ruler, Finder Ruler which was developed by WilliamHang in 1998. Hang adapted the Finder Ruler from a design by Dr. John Mew from England.
This disposable device utilizes a small scale to measure the distance between the upper incisor edges to the tip of the nose. This simple procedure is designed to estimate maxillary growth in relationship to the rest of the face. It can serve as an especially useful device to employ when treating children with thumb sucking, to record any teeth and maxillary bone position changes over time as a result of therapy.
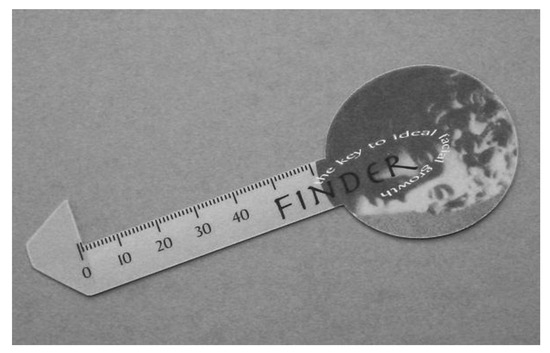
Figure 5.
Finder Ruler. (Courtesy of W. Hang, DDS, Westlake, California).
At age five, the distance between upper incisor edge and tip of the nose is expected to be 28 mm for both females and males. This distance is reported to increase by one mm per year until age 15 and reaches the range of 38-42 mm in adult females and 40-44 mm in adult males. When there is more or less than five mm from the expected distance, this is an indication of a less desirable facial growth. However, genetic characteristics within families contribute to a wide range of acceptability in evaluating any measure of lip height.
Another disposable screening ruler, called the Bite Down Early, is easy to use, and makes it easy for parents to understand the concept of excessive overjet. These disposable rulers can be purchased through the California Association of Orthodontists (CAO). As with the Finder Ruler, an explanatory brochure is included with each ruler, which explains the importance of identifying early excessive overjet and making an appropriate referral. The rulers are indicated for children by age seven to grossly assess the need to address an excessive overjet.

Figure 6.
Bite Down Early Ruler (Courtesy of the California Association of Orthodontists).
This is a simple device to use. When lined up with the edge of the mandibular incisors, if the maxillary incisors fall within the green area (1-3 mm) the overjet is considered to be within the normal range. If the upper incisor edges fall anywhere in the red area, it is recommended by CAO that the child should be referred to an orthodontist.
This little device can be used by those who are not familiar with dental malocclusions, to quickly screen and identify children who may have excessive overjet. Although the diagnosis of malocclusion is made by the orthodontist, this instrument can be used for a descriptive assessment of overjet. Many orthodontists do not embrace early treatment, preferring to wait for the eruption of permanent teeth before instituting any treatment. Moreover, not all instances of excessive overjet in children in mixed dentition will be or need to be corrected. If, however, an overjet is excessive enough to create a risk of tooth loss from injury, early treatment may be required (Mason, 2006). Both the Finder ruler and the Bite Down Early ruler offer objective but restricted measurements of structural landmarks.
Another disposable ruler used to evaluate the range of motion and dimensions of the mouth opening was developed by Therabite. These rulers are part of a therapy kit intended to increase the range of motion in patients with temporomandibular joint dysfunctions. A Therabite system purchase includes literature to support the method, however the rulers can be purchased separately (Chase et al., 1995; Mercuri et al. 2002).
The Therabite range of motion ruler is easy to use. The adult average opening is between 35 to 50 mm, which is the size of three fingers inserted vertically, up to the first knuckle, in the mouth. However, it is not unusual for some children to have an aperture of +55mm.
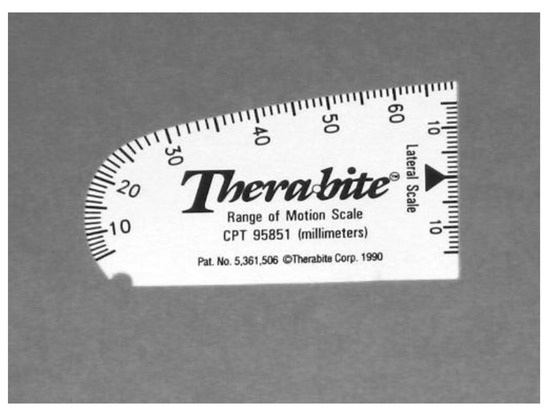
Figure 7.
Therabite Range of Motion Ruler. (Courtesy of Atos Medical, Milwaukee, Wisconsin).
A versatile ruler is the one produced by Grobet. Since it is made of stainless steel it can be washed, disinfected or sterilized easily. This ruler can be used to measure the range of motion as well as dimensions between landmarks, such as the width of diastemata, intercanine distance, interlabial gap, distance between eye and mouth corner, and more.
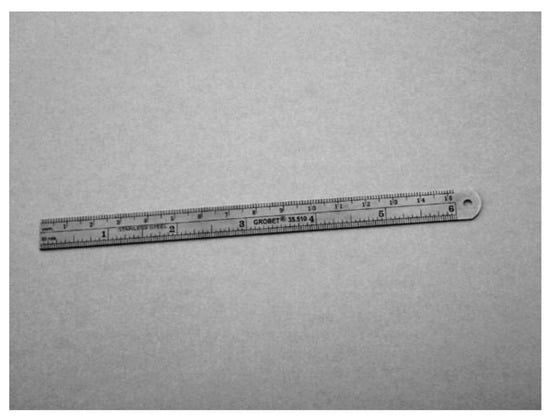
Figure 8.
Grobet Ruler. (Courtesy of Zimco Products, Redmond, Washington).
Both the Therabite and the Grobet rulers can be considered as objective measurements of structural landmarks. However when the Grobet ruler is used to measure soft tissues or functions, the results could be affected by subjective judgments.
Gauges or Calipers
A useful and easily obtained instrument for measurement can be the caliper or gauge. Many orthodontists and orofacial myologists are familiar with the Boley gauge, but other models are available through dental dealers or even hardware stores. The caliper can be a simple mechanical or digital instrument.
The caliper may be used for measurements of structural features such as leeway space, diastemas, dimension of lips, length of nasal piltrum, and more or functional measurements such as the full mouth opening (Winter, 1985; Goulet, Clark and Flack, 1993; Shellhart et al, 1995; Scarbrough, Ghali and Smith, 1997; Quintal et al., 2004; Queiroz Marchesan, 2005) About 35-50 mm is the range of a normal opening for adults. This measurement is more useful when the patient presents a limited oral opening and therapy addresses such a limitation.

Figure 9.
Gauge or Caliper. (Courtesy of I. Queiroz Marchesan, PhD, Sao Paulo, Brazil).
This gauge may be used directly on the patient as well as on photographs and orthodontic study models. It can be washed, disinfected or sterilized based on the model (digital vs. mechanical). A cellophane wrap may be used to isolate the gauge without negatively impacting the effectiveness of the measurement.
The caliper may be used to calculate the dimension of tongue elevation in cases of ankyloglossia or tongue-tie (Queiroz Marchesan, 2005). An easy way to assess the need for referral to an oral surgeon is to measure the full opening then to ask the patient to touch the tip of the tongue against the alveolar papilla and then remeasure the mouth opening. If the new measure is equal or less than half of the previous full mouth opening, the patient needs to be referred to an oral surgeon for evaluation.
Similar to the use of other rulers described earlier, this gauge can be used for objective measurements of specific structural landmarks such as inter-canine distance. Measurements become subjective for functional landmarks such as full mouth opening or soft tissues because of possible stretching or unintended muscle activity.
Study Models
For those who have the good fortune to work closely with an orthodontist, study models can provide a great source of information. They allow clinicians to see specific dentally-related details, and they also provide the opportunity to measure selected dental features and other structural landmarks such as tori, dental spaces, overjet, and overbite. Once the study model is provided, the objective measures that can be obtained only require low-tech, inexpensive devices such as rulers and calipers.
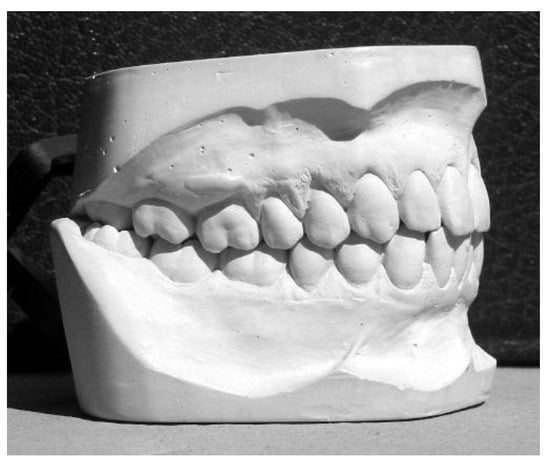
Figure 10.
Study Model. (Courtesy of D. LoCuoco, Udine, Italy).
Freeway Space
One aspect that has been under-reported in OFM is the impact of myofunctional disorders affecting the freeway space, which is the natural separation between the upper dental arch and the lower dental arch at rest (Mason, 2005). Teeth naturally come into contact only during chewing, swallowing and clenching, while for the vast majority of the day and night, teeth are apart. The normal resting interocclusal space between dental arches is about 2-3 mm posteriorly, or 3-5 mm anteriorly. Low tongue posture or a habitual open mouth posture may increase the freeway space, while some high dental restorations, such as crowns designed too high, may reduce the freeway space.
One way to document the freeway space is by applying two markers (paper or a pen mark), one at the base of the nose and one at the bottom of the chin. Ask the patient to moisten his or her lips, swallow, relax, take a deep breath and close the eyes. Then record the distance between the two points with a caliper, with the mandible in rest position. Ask the patient to gently approximate the lips. Record another measure. Then ask the patient to bite into occlusion, and measure again. Now three measures are available for comparison, all of which may be affected by myofunctional therapy. The freeway space can be measured before and after therapy and at follow-up evaluations (Mason, 2005).
Measuring the freeway space also gives the clinician the opportunity to document the tooth-upper lip relationship. With the lips at rest and slightly separated, about two millimeters of the upper teeth should be visible for a pleasing esthetic effect. This is a measurement that may be affected by myofunctional therapy. Also, the lower lip is ideally expected to cover, when lips are approximated, about two millimeters of the upper incisors. This is thought to help maintain a stable position of teeth after orthodontic treatment.
Measuring the freeway space can be accomplished objectively if the landmarks have been adequately identified on the skin and consistently revisited in subsequent measurements. The inclusion of information about the dimensions of the freeway space on clinical examination forms, and in clinical reports, is an important addition to the documentation process with myofunctional disorders. This is especially relevant since myofunctional conditions usually involve some relationship to the vertical plane of space, in contrast to the dental emphasis on teeth in occlusion.

Figure 11.
Freeway Space-Teeth in Bite. (Courtesy of S. Mohiuddin, Los Angeles, California).

Figure 12.
Freeway Space-Lips Slightly Apart. (Courtesy of S. Mohiuddin, Los Angeles, California).
Facial Symmetry
Sometimes, orofacial myofunctional disorders can contribute to facial asymmetry, which is easily perceived but not always documented. Many articles and books have included information on the subject of facial esthetics, including: Bateman and Mason, 1984; Ferrario et al, 1994; Al Wazzan, 2004.
Ideally, the three horizontal thirds of the face should be approximately equally in a well-proportioned face. In a child, the mid-face height and lower face heights will usually be about the same, while in adults, the proportions are often greater for lower face height than mid-face height with the lower third or the middle third disproportionate because of skeletal, dental or myofunctional disorders.
The first measurement, of lower face height, is the same previously used for the assessment of the freeway space. The upper limit is the base of the nose, where the columella and the philtrum meet. The lower limit is the menton, or the base of the chin. This measurement is sensitive to change from open mouth posture, overbite or open bite.
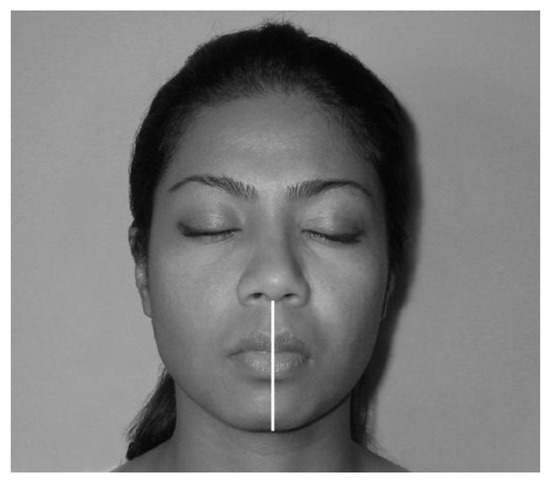
Figure 13.
Lower Third of Face. (Courtesy of S. Mohiuddin, Los Angeles, California).
The middle third of the face extends from the base of the nose (subnasal) to the eyebrow level, or glabella. This area can be influenced by breathing problems or may show differences related to genetic disposition.
The upper third of the face extends from the eyebrow area to the hairline (or glabella to trichion). This third may also vary according to genetic pattern, or family inheritance pattern. For patients with frontal baldness, if asked to raise their eyebrows, it can be identified as a crease or wrinkle where the hairline was previously located. To make it easy to remember the facial thirds, separate them as follows: bottom of the chin to base of the nose, base of nose to eyebrows, then to hairline.
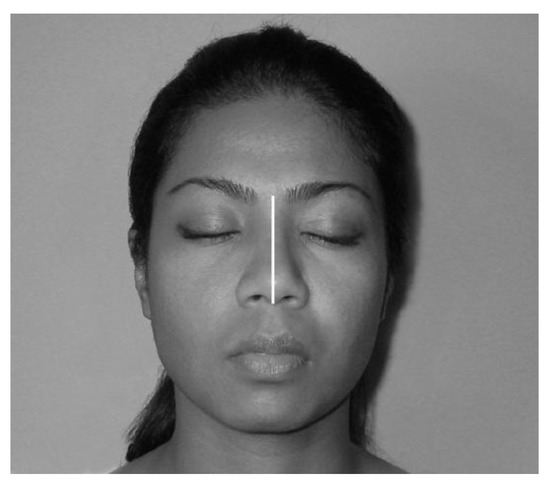
Figure 14.
Middle Third of Face. (Courtesy of S. Mohiuddin, Los Angeles, California)
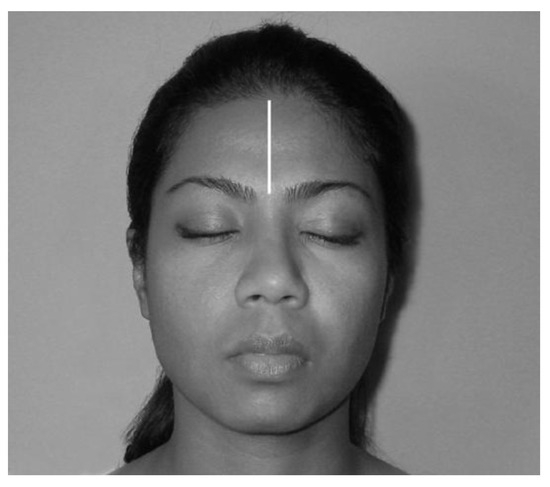
Figure 15.
Upper Third of Face. (Courtesy of S. Mohiuddin, Los Angeles, California).
Observing the profile allows the assessment of the lower third of the face in relationship to the esthetic line, or E-line, which extends from the tip of the nose to the chin. This line is often used by orthodontists to evaluate the need to perform extraction of premolars, if the lips rest ahead of the E-line. In Caucasians, the lips should rest a few millimeters behind the E-line but there are, of course, different standards for different racial groups. Orofacial myofunctional therapy may affect the position of the lips in relationship to the E-line, so it is advisable to document the distance of both upper and lower lips from the E-line.

Figure 16.
Esthetic Line. (Courtesy of S. Mohiuddin, Los Angeles, California).
One more measurement of symmetry is to separate the face from a fontal view into two vertical halves, then look for variations from one side to the other. First, one needs to look for any variations in the vertical plane. Minor asymmetries are normal while major variations are easier to detect and should be described and documented as accurately as possible.
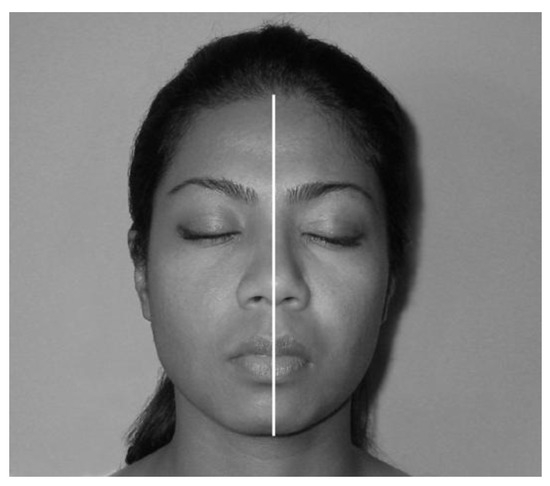
Figure 17.
Vertical Symmetry-Halves. (Courtesy of S. Mohiuddin, Los Angeles, California).
Once the vertical symmetry of the face is assessed, then horizontal symmetry may be evaluated. One way to assess this is to draw an imaginary line across the face between the pupils, or from the external eye corners and compare that line to a line drawn across the mouth from commissure to commissure (outside corner of the lip) with the patient not smiling. The two lines should be parallel. In some instances, orofacial myofunctional therapy may positively affect this horizontal proportion.
A useful clinical perspective is that the face is “five eyes” wide, that is, the face can conveniently be separated into five horizontal parts. One eye width is usually found to occupy the space of the bony tissues that separate the two eyes. The wider the space, the flatter the nasal bridge. Pathological spacing between the eyes is called hypertelorism and is a feature of some craniofacial disorders. The space between the medial corners of the eyes should be equal to the width of the nose, with some exceptions for various ethnic groups.
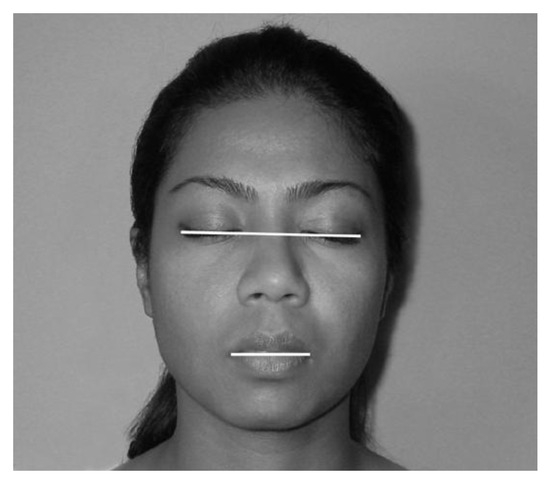
Figure 18.
Horizontal Proportions. (Courtesy of S. Mohiuddin, Los Angeles, California).
Another measurement perspective is that, with some exceptions for various ethnic groups, the width of the nose, or alar base width, is the same as the distance between the medial corners of the eye, or inner canthus. In other words, intercanthal width and alar base width are usually the same.
Another measurement that may change positively following orofacial myofunctional therapy is the symmetry between the distal corner of the eye (the lateral canthus) and the corner or the mouth. Ideally both left and right measurements should be equal and can be measured with face at rest or during smiling, although many individuals have a normal asymmetry in their smile. This measurement may be affected by Bell’s palsy, stroke or some genetic malformation.
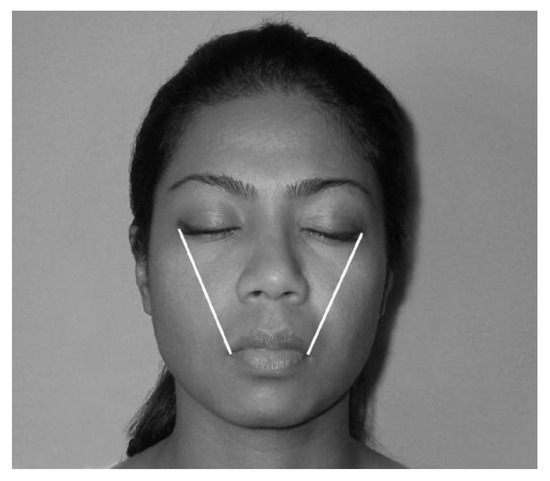
Figure 19.
Commissure-to-Commissure Proportions. (Courtesy of S. Mohiuddin, Los Angeles, California)
Observations reflecting the relationship of soft tissues should also be recorded, including a measurement of the length of the philtrum, from the base of the nose to the vermillion of the lip, or the lower lip from the wet line to the vermillion limit. The wet line indicates that location on the lip where the dry outer surface and the wet inner surface meet. This can be easily observed by rolling the lower lip forward and down.
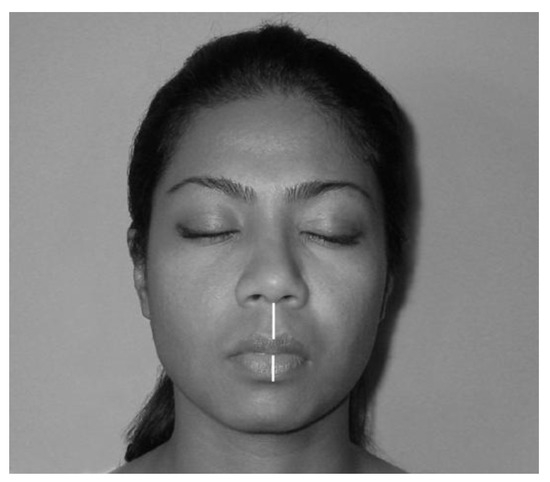
Figure 20.
Lip Measurements. (Courtesy of S. Mohiuddin, Los Angeles, California).
It would be important to measure and record any interlabial gap present, which is the vertical space between the lips in a rest posture. There should be no space between resting lips in adults, while in children under age 13, a space may be seen normally. Although the lips continue to grow vertically until around age 17, lip closure, or competence at rest, is usually expected by age 13. If the gap seen in children is more than 4 mm, it may be appropriate to address this situation in therapy.
Making and recording observations of facial symmetry according to facial landmarks is quite useful as well as objective (Hanson and Mason, 2003). Measurements made at landmarks result in the documentation of structural features as well as functional characteristics such as facial drooping or hypertrophic muscles.
The Gudin Test
It is common in myofunctional therapy diagnostics to see patients who present an open mouth posture, raising a suspicion about the adequacy of the nasal airway for normal nasal respiration (Garretto, 2003; Garretto, 2005). While a patient with known or confirmed nasal airway interference should be referred to an ENT specialist for definitive diagnosis and treatment, the clinician can conduct some preliminary assessments of the nasal airway without diagnosing the problem as airway interference.
The Gudin test is a subjective but useful assessment measurement in which one nostril is held closed by the clinician while the other is compressed for one second. This maneuver should elicit the “flaring reflex” which is present in healthy nose breathing subjects. In children with poor nasal breathing the reflex is diminished or absent. The presence of this reflex is tested in both nostrils. It takes a bit of practice to see the reflex when it’s diminished so this test is subjective. The results of the Gudin assessment should be recorded on a pass/fail basis. Overall this test only provides a crude estimate of the functionality of nasal breathing, but it can serve as an indicator of a nasal breathing difficulty.
The Rosenthal Test
This is another easy and low-tech test to estimate nasal patency (Garretto, 2003; Garretto, 2005). The patient is asked to take 20 breaths through the nose, with lips together while observing whether the patient’ s mouth opens before 20 breaths are completed. This is best accomplished after the patient blows his/her nose prior to this test, since the presence of nasal debris can influence the result. Clearly, someone with a congested nose will need to gasp for air well before the 20 breaths are completed. Clinicians may want to record the maximum number of breaths taken by the patient. However, this is also a subjective measurement of nasal breathing capability. If a patient has a cold on the day you are assessing, has a bout of asthma, or a stuffy nose, the clinician will obtain an inaccurate assessment. Nonetheless, this test does provide a clue to breathing pattern.
The Nasal Mirror
There are several nasal mirrors available, some of them referred to as Glatzel mirrors in recognition of the inventor (Garretto, 2003; Garretto, 2005; Queiroz Marchesan, 2005). Usually, nasal mirrors consist of a shiny stainless steel plate. The mirror may have an indentation that contours the nose or has flat edges and may or may not have an etched grid or a series of concentric semicircles imbedded in the metal to quantify the amount of nasal vapor. The nasal mirror is placed under the patient’s nose and the nasal vapor emission is recorded. Photos of the vapor can be taken by placing the camera at an appropriate angle so as not to record a reflection.
The area covered by the vapor is referred to as the pneumatype, which will differ between the two nasal chambers and in adults and is expected to alternate every 30 to 90 minutes as the natural shift of breathing from one nasal cavity to the other occurs; that is, there is always one nostril that is less active than the other. The nasal mirror is able to identify nasal cavities that are completely or severely blocked.
The results of nasal assessment with the nasal mirror can be recorded as a pass/fail. This subjectively documents the status of nasal breathing at the moment of evaluation only.
While this test may have some functional value, the quantification of the amount of nasal vapor is, at best, a crude estimate of breathing capability. Nonetheless, it does provide information to the examiner that may be useful in a referral for a definitive ENT or pediatric evaluation.
The Lip Gauge
The lip gauge represents a bit of history related to orofacial myofunctional therapy. It is a moderately low-tech instrument popularized by Daniel Garliner. Many therapists still use it to estimate the strength of the peri-oral muscles and the orbicularis oris (Barber and Bonus, 1975; Satomi, 2001; Garretto, 2003; Hahn, 2003; Andretta, 2005, Garretto, 2005). Early texts, including Garliner’s, report that the average strength of lip resistance to pull should normally be from three to five pounds. However, these figures are unsupported estimates that have no scientific verification, so the results should not be included in referral requests and reports. While such testing simply provides an impression of facial and lip muscle strength, the gauge can be used in therapy where strengthening exercises may be indicated.
The use of the gauge in therapy can also serve as a great motivational device for patients, many of whom actually like using it to visualize increased improvement of their resistive strength. Usually on their first visit the measurement is about 1/2 pound to one pound. By the second visit the patient may demonstrate two pounds of resistive strength, giving them a great sense of accomplishment. Use of the gauge can help patients become more aware of their lips and facial muscles by providing a numerical frame of reference. Therefore, because of its modality of measuring, the lip gauge yields only a subjective measurement and its primary value is as a therapy motivational aid.
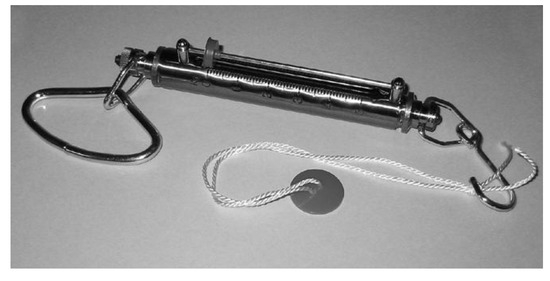
Figure 21.
Lip Gauge. (Courtesy of NeoHealth, Coconut Creek, Florida).
The Myoscanner
Another familiar device recommended by Garliner is the myoscanner, which has also acquired other names such as the myometer or myobox (Garretto, 2003; Hahn, 2003; Andretta, 2005; Garretto, 2005). It purports to measure compressive lip strength, protruding tongue pressure and masseter contraction. Although some norms are available, the measurements obtained through the myoscanner have been found to be of low significance in OMT. For example, protrusion of the tongue outside the mouth, as the myoscanner requires, involves using a different set of muscles than those used for swallowing or for speech. The compressive lip pressure is not significant because, at rest lips do not press against each other. For the masseters, the measurement obtained reflects an overall activation, with no distinction of laterality or any portion of the muscle activated.

Figure 22.
Myometer. (Courtesy of Mft-products, Matzendorf, Switzerland).
Although there are no scientific reports concerning the validity and reliability of measurement obtained with the myoscanner, there are many anecdotal reports of its accuracy. Data derived from use of this instrument has been included in several reports worldwide, to establish the effectiveness of OMT, but some elements of the device (especially the latex straps) make it a flawed instrument. However, it can serve as a useful motivational instrument for some patients, and in the hands of experienced therapists, it can yield predictable results. In summary, the myoscanner may indeed provide some functional data to document daily clinical progress, but the value and validity of the information obtained remains uncertain.
The IOPI
The Iowa Oral Performance Instrument or IOPI is a device that may eventually be of interest and used in research and therapy in OMT. The IOPI is advertised to measure tongue strength and fatigability by having the tongue press against a small balloon transducer placed against the hard palate. The IOPI has been employed in many studies, especially with patients with Parkinson Disease (Lazarus et al., 2000; Solomon, 2004; Solomon and Munson, 2004; Lazarus, 2005; O’Day et al., 2005).
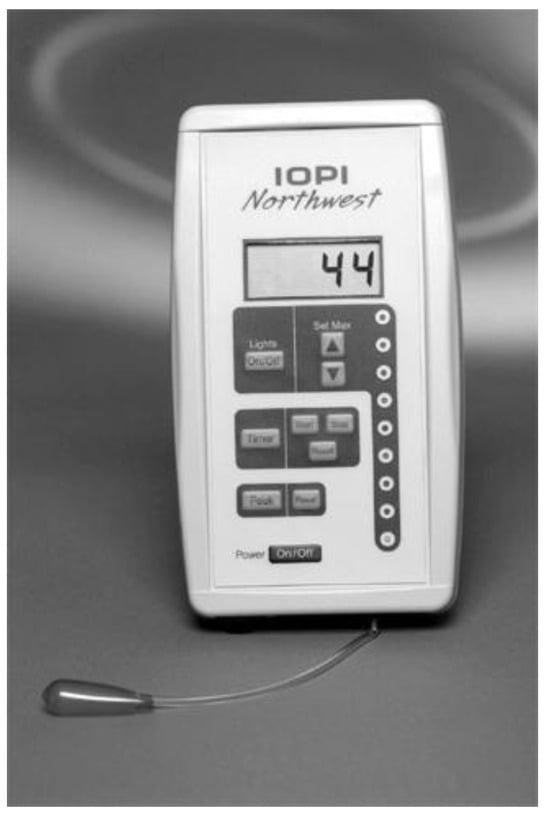
Figure 23.
IOPI. (Courtesy of Blaise Medical Hendersonville, Tennessee).
Its usefulness in OMT may come from its ability to indicate when a given exercise for tongue pressure results in the value chosen for an individual’s tongue strength. Robbins, Gangnon, Theis, Kays, Hewitt, and Hind (2005) found that the use of the IOPI in an isometric exercise program with older individuals resulted in increase tongue pressure, increased swallowing pressure, and in some individuals increased lingual volume. The IOPI may eventually help in resolving a recurring problem in OMT, of not knowing how many times or for how long certain exercises need to be repeated to be effective, or to help determine when exercises reach their musculature physiological limit.
Overall, the IOPI may eventually develop into one of the most objective of the devices commercially available to measure selected tongue functions, but it may also prove useful in therapy as a motivational tool and to assess the endurance limit of certain exercises. The IOPI may have a promising future in myofunctional offices although further development is needed.
Mapping Swallowing Contact Areas
For many years, myofunctional therapists have strived to develop procedures to visualize swallowing activity and identify the tongue thrust swallow. One of the traditional methods is the Payne technique named after its inventor (Rivera-Torres, 1992; Garretto, 2003; Hahn, 2003; Garretto, 2005). Garliner was a passionate proponent of this technique to map and trace an area of tongue contact, which featured a type of toothpaste mixed with fluorescine. After the patient swallows, the fluorescine highlights the area that the tongue contacted on the hard palate and teeth, as visualized with a black, ultraviolet light.
There are no available peer reviewed studies supporting this method. This technique is not well regarded in dentistry although it is still popular among some myofunctional therapists. The use of an ultraviolet light is used often in dentistry for teeth bleaching and placement of braces. However, caution is of critical importance in the use of an ultraviolet light because it has the potential to create permanent damage to the eyes. Therefore, anyone using an ultraviolet light source should look through a light shield, which should be attached to the flange of the light source. Care should be taken to protect the patient’s eyes as well.
Many therapists do not feel comfortable in using fluorescine, so instead they use blue cake icing which is well loved by children but can be used only once per session as the food coloring coats the entire tongue. The lack of objectivity from use of any coating in the mouth is related to the fact that clinicians must instruct the patient to keep the tongue away from the palate until they swallow, which creates an unnatural starting point for a swallow and thus, the resulting image of the swallow is not a natural production.
The Surface Electromyograph (SEMG)
Another promising measuring device is the SEMG, which uses sensors applied to skin as opposed to needles inserted in specific muscles. Because of its technological complexity, the need for specific training, and considerable cost, at present the SEMG is primarily a research tool (Palmer et al., 1999; Ding et al., 2002; Rahal and Pinatel Lopasso, 2004; Vaimar, Segal and Eviatar, 2004; Rahal, 2005). Over time, and as the cost is reduced, it may have more general use in clinical diagnostics in OMT.
In surface EMG, the adhesive electrodes are applied to the skin over specific muscle groups. As a result, the data obtained express muscle electrical activity from a generic area rather than the response from a specific muscle. A more accurate recording of individual muscle activity is possible with needle electromyography.
The images of SEMG tracings shown here have been provided by Adriana Rahal, from San Paulo, Brazil, who uses the SEMG routinely in her university myofunctional therapy practice. Several peer-reviewed articles have been published about the application of the SEMG in swallowing analysis (Palmer et al., 1999; Ding et al., 2002; Rahal and Pinatel Lopasso, 2004; Vaimar, Segal and Eviatar, 2004; Rahal, 2005).
The first image, visualized with SEMG, shows a graphic readout of a normal swallow with activation of both anterior digastric muscles. Compare the activation of the anterior digastric muscles in the first image with a saliva swallow and an extended contraction of the orbicularis in the second display. Note that while the normal swallow is accomplished rapidly, with a distinct peak of force, the contraction of the orbicularis for the saliva swallow reveals a less coordinated muscle movement and an ill-defined peak.
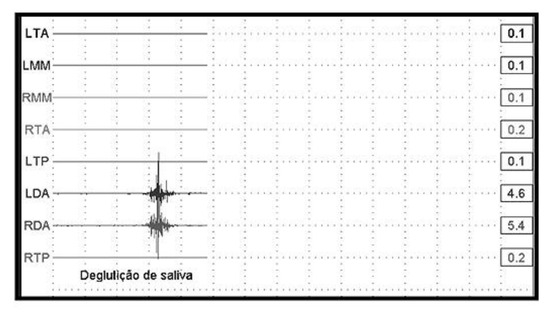
Figure 24.
SEMG Tracing-Normal Swallow. (Courtesy of Myotronics, Tukwila, Washington).
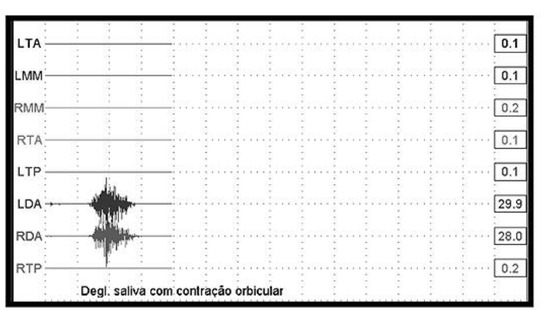
Figure 25.
SEMG Tracing of Swallowing with Lips Contraction, Tracing-Tongue Thrust. (Courtesy of A. Rahal, PhD Sao Paulo, Brazil)
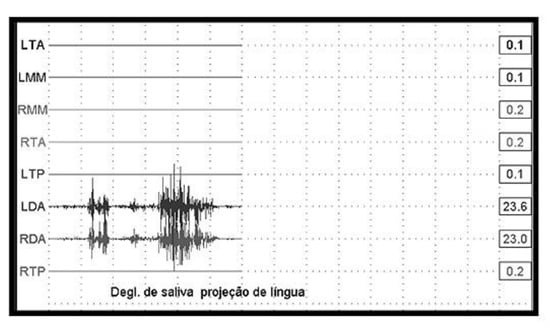
Figure 26.
SEMG Tracing of Tongue Thrust. (Courtesy of A. Rahal, PhD Sao Paulo, Brazil).
The next display shows a noticeable difference between a normal swallow and a tongue thrust swallow. Again, there is evidence of excessive and uncoordinated muscle recruitment, with a prolonged attempt to exert maximum effort (see the multiple peaks).
While SEMG has evolved into an objective instrument to quantify selected aspects of a swallow, the movement pattern involved in a swallow, which includes all planes of space, limits surface EMG from fully describing a swallow. This technique is best used in combination with other instrumentation, such as radiography, which can assess some components of a swallow not measurable by SEMG. At present, SEMG is a useful instrument for research, and for a general assessment. It also may have clinical value as a motivational and feedback tool in therapy.
Palatometer
The palatometer represents an instrument which may eventually hold great promise for use by the orofacial myofunctional clinician. This technique is also referred to as electropalatography. The palatometer technology has progressed to the extent that it is now possible to store an image, to freeze frame, slow motion, to record in real time, to provide for an interaction between clinician and client, and much more.
Palatometers, in various configurations, have been used for decades. They have been utilized specifically in research to study articulation, and also in the feedback procedures in the treatment of persons with profound deafness (Fletcher, 1985; Fletcher, Dagenais and Critz-Crosby, 1991; Dagenais et al, 1994; Scoobie, Wood and Wrench, 2004; McAuliffe, Ward and Murdoch, 2006). Although many articles have been published, world-wide, that describe the applications of the palatometer for assessment and feedback with speech disorders, only a few publications show an application to swallowing disorders. Historically, palatometers were cumbersome and prohibitively expensive, but some manufacturers are currently making an effort to develop and market user-friendly and affordable palatometers.
The palatometer can yield data useful for research as well as therapy purposes. The downside is that its high tech and complex nature requires a customized palatal carrier appliance to be constructed for each patient. This involves having a dentist or orthodontist take an impression of the palate followed by a technician constructing a customized electropalatographic plate for the patient. The palatometer itself requires linkage to a computer in order to analyze and manipulate the data.
The complexity and cost of the palatometer place it beyond the range of a typical private practice setting. However, this device is being refined by researchers on a regular basis, and like the computer, is becoming more user-friendly and less expensive. Hopefully, in the near future, this instrument will be affordable and adaptable to the interests of the orofacial myofunctional clinician.
Cephalograms
Although few myofunctional clinicians have training in interpreting cephalometric x-ray films or tracings, the oriented and standardized lateral and frontal cephalograms obtained in an orthodontic office are excellent sources for objective structural measures (Bertolini et al., 2003). In some orthodontic practices, computerized programs are used to aid in predicting growth and development, or even proposing a treatment plan. While some orthodontists utilize computer-aided programs for identifying landmarks and tracing films, only the human eye can properly identify bone defects, or describe the features of craniofacial disorders, or evaluate many other important patient characteristics such as the status of the cervical spine, the size of the adenoids, and much more.
Cephalometric measures can be used in research and in therapy as references to compare before and after treatment results and patient characteristics through superimposition of tracings. Such comparisons are ideal for retrospective studies, as well as serving as an important and reliable research tool for prospective research.
Whenever a patient is treated jointly with an orthodontist, the clinician might want to contact the orthodontist to ask about the possibility of having the orthodontist explain the x-ray findings, especially with regard to characteristics, measurements, and soft tissue findings that are relevant to the clinician’s treatment planning. Most orthodontists would welcome this interaction. Some of the items that orofacial myofunctional clinicians would be interested in learning from an orthodontist include: any deviation of the occlusal plane, especially when it is suspected that differential eruption has occurred (increased maxillary posterior eruption and less anterior eruption); the vertical length of the ramus of the mandible; the resting position of the hyoid bone (a sign of where the tongue is at rest); the Curve of Spee; and the size of the nasopharynx.
While the images seen on a lateral cephalogram can give the therapist an idea of the status of the soft tissues (including tonsils, adenoids, and the airway), a lateral ceph provides only a midline view of all tissues, so caution is urged in making definite comments about the relationship of the observations to breathing. This caution also applies to the frontal film, especially where there is deviation of the septum. What the clinician sees cephalometrically does not necessarily correlate with how well the individual is able to breathe intranasally.
Cephalometric x-ray films are obtained by decision of a dentist or orthodontist. While it is useful for the orofacial myofunctional therapist to have cephalometric data available, this is a medical decision and only doctors should recommend imaging.
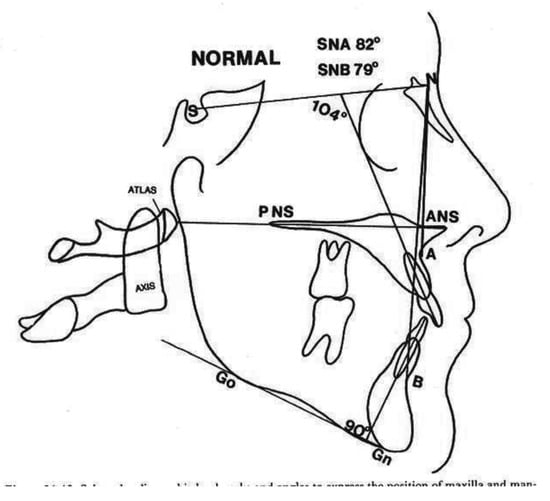
Figure 27.
Cephalometric Tracings. (Courtesy of R. Mason, MDM, PhD Durham, North Carolina).
Speech Screenings
As most speech-language pathologists (SLP) have learned, professionals from other fields are often at a loss to know when to refer a patient for speech or orofacial myofunctional examination. A simple screening procedure can be taught to these professionals as a means of helping them detect gross misarticulations involving a frontal or lateral tongue thrust.
Simple sentences involving the /s/ sound at the beginning, middle and end of words help to identify an audible and visible tongue thrust. The /r/ sound in all word positions helps detect a lateral tongue elevation. In English, the /l/ sound in all positions allows an examiner to identify the “flying L”, as Dianne Fonssagrives, COM, describes it, or the /l/ produced interdentally.
Phrases like: Please pass the pepper or Teddy had a puppy called Kitty, especially if evaluated using a stethoscope placed underneath a nostril, can help detect an audible nasal emission which should signal the need to be referred to a SLP for full evaluation. While only an SLP should administer an articulation test, it is advisable for every orofacial myofunctional therapist to know how to detect at least gross audible and visible misarticulations.
Oral Diadochokinesis
To screen the velocity and coordination of the speech articulators (lips, tongue and soft palate), an oral diadochokinetic rate can be obtained by asking the patient to repeat syllables such as puh-puh-puh; tuh-tuh-tuh; and kuh/kuh/kuh. In addition, it is recommended that patients repeat a combination of syllables such as puh-tuh-kuh or buttercup (Fletcher, 1972). Normative data is available for utterance rates. Adults should be able to produce about one combination within one second (Prathanee, 1998). The author also recommends using syllable trains like fuh-suh-shuh, tuh-duh-nuh and vary on the vowels, like too-doo-noo, to observe orofacial changes.
Diadochokinetic testing is a simple but effective assessment measure. These rates are important inclusions in an initial examination protocol as a way of assessing the developmental level of the patient’s neuromotor system for speech. Special attention should be given to the ability or inability of the patient to contact the tongue tip at the incisive papilla area.
Percentage and Scales
Another simple screening measurement is derived from the evaluation of the number and kinds of cues needed to help the patient. Cues can be given verbally as in asking the patient to protrude the tongue, or given visually as in showing how to protrude the tongue, or provided by touch as in protruding the tongue until it touches a stick.
There is no universal agreement on what constitutes a minimal, moderate or maximum cue. If the patient is able to execute a given task after only a verbal request, no additional cues are needed. If cues need to be provided up to 10% of the cueing time, (one out of 10), that would represent minimum cueing. Moderate cueing would involve cueing up to 50% and maximum anywhere above 50%. Total assist would represent 80-100% cueing, a situation that would be rare in an orofacial myofunctional practice. The exception is where a patient has a severe oral-motor sensory disorder, and even under such circumstances, the tasks would be divided into smaller, more manageable actions.
Another time and duration measurement that can be useful in therapy is the recording of the number of correct responses expressed as a percentage such as 60% or in numbers like 17/20. This type of documentation is useful when patients are instructed to swallow correctly 15 times. The therapist can then add whatever cues the patient needs, if any, followed by determining the time it takes for the patient to chew a given bolus and organize it for a swallow.
Time
Since “time” can easily be measured, the duration of various tasks should be included in assessments. The duration of many behaviors can be recorded: seconds of tongue suctions on the palate, minutes of habitual open mouth posture, and hours without biting fingernail or days without sucking thumbs. Time can be an excellent motivator by measuring the duration of specific activities during therapy sessions, but such measurements become very subjective when patients record their own time on task. Since patient self-recordings of time spent on task are based on an honor system, the veracity of such reports may be questionable.
Charts
One subjective patient recording task, which relies on the honor system, is a motivational or exercise chart. The charts are taken home by the patient and marked according to the task: button pulls, slurp and swallow, self checking reminders, hours without biting nails or sucking thumbs, and correct swallowing at meals. It is important to have the patient honestly conduct a regular self-evaluation and record their perceived progress in therapy. After all, therapy involves collaboration between patient and therapist. Any type of chart can be created, as long as it involves the patient in the decision-making process.
Objective Language
The clinician’s professional stature with patients, parents and referral sources can be increased by using references to patient behaviors that include quantifiable items. For example, instead of reporting “his tongue is getting stronger”, it’s preferable to say “he’s now able to hold water on his tongue and seal it against the palate”, “able to open his mouth over 15 mm”, “hold a posture for 20 sec”, and “produce more than 10 trials with minimal verbal cues”. Also, instead of reporting “she had TMJ pain”, it is better to specify that “she complained of popping sounds and pain in her left TMJ area, but only while eating”.
SUMMARY
In summary, selected instrumental and non-instrumental measurement approaches have been compared and contrasted. Some instruments are most appropriate for research, while others have utility as motivational tools in therapy. Many simple clinical procedures described require no monetary outlay.
Questions remain as to the validity of the tools of research highlighted in this article. Subsequent research should elucidate which instruments can demonstrate reliability and validity in measuring those behavioral parameters claimed to be measured.
Those instrumental systems mentioned that may eventually evolve as appropriate for research related to orofacial myofunctional disorders include the IOPI, the SEMG, and the palatograph. At present, however, they are rarely utilized in the typical OMT private practice setting.
While the search for appropriate tools of research and clinical documentation in myofunctional therapy continues, it is hoped that this review of selected instruments and procedures will encourage clinicians to investigate further the utility of the various tools and clinical procedures mentioned, to incorporate them into clinical practices as appropriate, and to search out other instruments or procedures not included here. Documentation is an especially important part of any orofacial myofunctional practice. In addition, careful and consistent documentation is necessary for the further growth and enhancement of the field of orofacial myology. Only with good documentation and further developments of appropriate tools for research, examination, and treatment will orofacial myology enjoy the reputation we aspire for it. The responsibility for enhancing the field should be shared by all orofacial myofunctional therapists.
DISCLAIMER
As the marketing chair of the IAOM, the author is in contact with several companies that either produce or distribute some of the devices highlighted in this article. The author does not receive any direct or indirect compensation by including and discussing any instruments or evaluation approaches in this article.
Acknowledgments
This manuscript is based on a presentation titled: Securing Objective Data, Past, Present and Future, given at the Mid-Winter Conference of the International Association of Orofacial Myology (IAOM) in Orlando Florida, January, 2006. The author is very grateful to Robert Mason, D.M.D., Ph.D., for the extensive mentoring during the writing of the article and to everyone who contributed through illustrations, information and ideas.
References
- Al Wazzan, K. A. 2004. The visible portion of anterior teeth at rest. Journal of Contemporary Dental Practice 5, 1: 53–62. [Google Scholar] [CrossRef] [PubMed]
- American Speech, and Language and Hearing Association (ASHA). 1992. Orofacial Myofunctional Disorders: Knowledge and Skills. Position paper.
- American Speech, and Language and Hearing Association (ASHA). 2005. Evidence Based Practice in Communication Disorders. Position paper.
- Andretta, P. 2005. Personal correspondence.
- Barber, T.K., and H. W. Bonus. 1975. Dental relationship in tongue-thusting children as affected by circumoral myofunctional exercise. Journal of the American Dental Association 90, 5: 979–988. [Google Scholar] [CrossRef]
- Bateman, H., and R. M. Mason. 1984. Applied anatomy and physiology of the speech and hearing mechanisms. Springfield, Il: CC Thomas Publishers. [Google Scholar]
- Bertolini, M. M., S. Vilhegas, D. Y. Norato, and J. R. Paschoal. 2003. Cephalometric evaluation in children presenting adapted swallowing during mixed dentition. International Journal of Orofacial Myology 29: 29–41. [Google Scholar] [CrossRef]
- Camargo Tanigute, C. 2005. Edited by I. Queiroz Marchesan. A documentacao como ferramenta para o diagnostico e controle da degluticao. In Tratamento da degliticao: A atuacao do fonoaudiologo em diferentes paises. Sao Jose dos Campos SP, Brazil: Pulso, pp. 107–115. (In Brazilian) [Google Scholar]
- Chase, D. C., J. W. Hudson, D. A. Gerard, R. Russell, K. Chambers, J. R. Curry, J. E. Latta, and R. W. Christensen. 1995. The Christensen prosthesis. A retrospective clinical study. Oral Surgery Oral Medicine Oral Pathology Oral Radiology and Endodontics 80, 3: 273–278, Comment in: Oral Surg Oral Med Oral Pathol Oral Radiol Endod. (1996), 81(2), 134–135. [Google Scholar]
- Clark, H. M. 2003. Neuromuscular treatments for speech and swallowing: A tutorial. American Journal of Speech Language Pathology 12, 4: 400–415. [Google Scholar] [CrossRef] [PubMed]
- Dagenais, P. A., P. Critz-Crosby, S. G. Fletcher, and M. J. McCutcheon. 1994. Comparing abilities of children with profound hearing impairments to learn consonants using electropalatography or traditional aural-oral techniques. Journal of Speech and Hearing Research 37, 3: 687–699. [Google Scholar] [CrossRef]
- Ding, R., C. R. Larson, J. A. Logemann, and A. W. Rademaker. 2002. Surface electromyographic and electroglottographic studies in normal subjects under two swallow conditions: Normal and during the Mendelsohn manuever. Dysphagia 17, 1: 1–12. [Google Scholar] [CrossRef] [PubMed]
- Ferrario, V. F., C. Sforza, C. E. Poggio, and G. Tartaglia. 1994. Distance from symmetry: A three-dimensional evaluation of facial asymmetry. Journal of Oral Maxillofacial Surgery 52, 11: 1126–1132. [Google Scholar] [CrossRef]
- Fletcher, S. G. 1972. Time-by-count measurement of diadochokinetic syllable rate. Journal of Speech and Hearing Research 15: 763–770. [Google Scholar] [CrossRef]
- Fletcher, S. G. 1985. Speech production and oral motor skill in an adult with an unrepaired palatal cleft. Journal of Speech and Hearing Disorders 50, 3: 254–261. [Google Scholar] [CrossRef]
- Fletcher, S. G., P. A. Dagenais, and P. Critz-Crosby. 1991. Teaching consonants to profoundly hearing-impaired speakers using palatometry. Journal of Speech and Hearing Research 34, 4: 929–942. [Google Scholar] [CrossRef]
- Garretto, A. L. 2003. Edited by M. L. Hanson and R. M. Mason. Orofacial Myology in Argentina. In Orofacial myology: International perspectives. Springfield, IL: CC Thomas, pp. 313–328. [Google Scholar]
- Garretto, A. L. 2005. Edited by I. Queiroz Marchesan. Experiencia fonoaudiologica no aprendimento odontopediatrico e ortodontico. In Tratamento da degluticao: A atuacao do fonoaudiologo em diferentes paises. Sao Jose do Campo, Brazil: Pulso, pp. 35–59. (In Brazilian) [Google Scholar]
- Goulet, J. P., G. T. Clark, and V. F. Flack. 1993. Reproducibility of examiner performance for muscle and joint palpation in the temporomandibular system following training and calibration. Community Dental and Oral Epidemiolgy 21, 2: 72–77. [Google Scholar] [CrossRef] [PubMed]
- Hahn, H. 2003. Edited by M. L. Hanson and R. M. Mason. Orofacial Myology: State of the art in Europe. In Orofacial Myology: International Perspectives. Springfield, IL: CC Thomas, pp. 354–361. [Google Scholar]
- Hanson, M. L., and R. M. Mason. 2003. Orofacial myology: International perspectives. Springfield, IL: CC Thomas Publisher. [Google Scholar]
- Harley, E. H. 2002. Asymmetric tonsil size in children. Archives of Otolaryngology and Head and Neck Surgery 128, 7: 767–769. [Google Scholar] [CrossRef]
- Lazarus, C. L. 2005. Lingual strengthening and swallowing. Perspectives on Swallowing and Swallowing Disorders (Dysphagia) 14, 2: 2–6. [Google Scholar] [CrossRef][Green Version]
- Lazarus, C. L., J. A. Logemann, B. R. Pauloski, A. W. Rademaker, C. R. Larson, B. B. Mittal, and M. Pierce. 2000. Swallowing and tongue function following treatment for oral and oropharyngeal cancer. Journal of Speech Language and Hearing Research 43, 4: 1011–1023. [Google Scholar] [CrossRef]
- Li, A. M., E. Wong, J. Kew, S. Hui, and T. F. Fok. 2002. Use of tonsil size in the evaluation of obstructive sleep apnoea. Archives of the Disorderd Child 87, 2: 156–159. [Google Scholar] [CrossRef]
- Mallampati, S. R., S. P. Gatt, L. D. Gugino, S. P. Desai, B. Waraksa, D. Freiberger, and P. L. Liu. 1985. A clinical sign to predict difficult tracheal intubation: A prospective study. Canadian Anaesthesiology Society Journal 32, 4: 429–434. [Google Scholar] [CrossRef] [PubMed]
- Mason, R. M. 2005. A retrospective and prospective view of orofacial myology. International Journal of Orofacial Myology 31, 1: 5–14. [Google Scholar] [CrossRef]
- Mason, R. M. 2006. Personal correspondence.
- McAuliffe, M. J., E. C. Ward, and B. E. Murdoch. 2006. Speech production in Parkinson’s disease: II. Acoustic and electropalatographic investigation of sentence, word and segment durations. Clinical Linguistics and Phonetics 20, 1: 19–33. [Google Scholar] [CrossRef]
- Mercuri, L. G., L. M. Wolford, B. Sanders, R. D. White, and A. Giobbie-Hurder. 2002. Long-term follow-up of the CAD/CAM patient fitted total temporomandibular joint reconstruction system. Journal of Oral Maxillofacial Surgery Comment in: J Oral Maxillofac Surg 60, 12: 1440–1448, Comment in: J Oral Maxillofac Surg. (2004), 62(7), 906–907.. [Google Scholar] [CrossRef]
- O’Day, C., E. Frank, A. Montgomery, M. Nichols, and H. McDade. 2005. Repeated tongue and hand strength measurements in normal adults and individuals with Parkinson’s disease. International Journal of Orofacial Myology 31: 15–25. [Google Scholar] [CrossRef]
- Ovassapian, A., R. Glassenberg, G. I. Randel, A. Klock, P. S. Mesnick, and J. M. Klafta. 2002. The unexpected difficult airway and lingual tonsil hyperplasia: A case series and a review of the literature. Anesthesiology 97, 1: 124–132. [Google Scholar] [CrossRef]
- Palmer, P. M., E. S. Luschei, D. Jaffe, and T. M. McCulloch. 1999. Contributions of individual muscles to the submental surface electromyogram during swallowing. Journal of Speech Language and Hearing Research 42, 6: 1378–1391. [Google Scholar] [CrossRef]
- Prathanee, B. 1998. Oral diadochokinetic rate in adults. Journal of Medical Association of Thailand 81, 10: 784–788. [Google Scholar]
- Queiroz Marchesan, I. 2005. Tratamento da degliticao: A atuacao do fonoaudiologo em diferentes paises. Sao Jose do Campo, Brazil: Pulso. (In Brazilian) [Google Scholar]
- Quintal, M., A. Tessitore, J. Rizzoato Paschoal, and L. Nizam Pfeilsticker. 2004. Facial paralysis quantification by digital paquimeter. Revista CEFAC 6, 2: 170–176. (In Brazilian). [Google Scholar]
- Rahal, A. 2005. Edited by I. Queiroz Marchesan. A electromiografia de superficie como ferramenta para o estudio da degluticao. In Tratamento da degliticao: A atuacao do fonoaudiologo em diferentes paises. Sao Jose do Campo, Brazil: Pulso, pp. 93–99. (In Brazilian) [Google Scholar]
- Rahal, A., and F. Pinatel Lopasso. 2004. Electromyography of the masseter and suprahyoid muscles in female patients with either normal occlusion or Angle’s Class I malocclusion, during oral phase of swallowing. Revista CEFAC 6, 4: 370–375. (In Brazilian). [Google Scholar]
- Rivera-Torres, P. 1992. The diagnostic importance of the Payne technique. Journal of General Orthodontics 3, 3: 13–17. [Google Scholar]
- Robbins, J., R. Gangnon, S. Theis, S. Kays, A. Hewitt, and J. Hind. 2005. The Effects of Lingual Exercises in Older Adults. Journal of American Geriatrics Society 53, 9: 1483–1489. [Google Scholar] [CrossRef]
- Robey, R. R. 2005. An Introduction to Clinical trials. The ASHA Leader 10, 7: 22–23. [Google Scholar] [CrossRef]
- Satomi, M. 2001. The relationship of lip strength and lip sealing in MFT. International Journal of Orofacial Myology 27, 1: 18–23. [Google Scholar] [CrossRef]
- Scarbrough, F. E., G. E. Ghali, and B. R. Smith. 1997. Anatomic guidelines for the placement of external references for maxillary repositioning. Oral Surgery Oral Medicine Oral Pathology Oral Radiology and Endodontics 84, 5: 465–468. [Google Scholar] [CrossRef] [PubMed]
- Scobbie, J. M., S. E. Wood, and A. A. Wrench. 2004. Advances in EPG for treatment and research: An illustrative case study. Clinical Linguistics and Phonetics 18, 6–8: 373–389. [Google Scholar] [CrossRef] [PubMed]
- Shellhart, W. C., D. W. Lange, G.T. Kluemper, E. P. Hicks, and A. L. Kaplan. 1995. Reliability of the Bolton tooth-size analysis when applied to crowded dentitions. The Angle Orthodontist 65, 5: 327–334. [Google Scholar] [PubMed]
- Solomon, N. P. 2004. Assessment of tongue weakness and fatigue. International Journal of Orofacial Myology 30: 8–19. [Google Scholar] [CrossRef]
- Solomon, N. P., and B. Munson. 2004. The effects of jaw position on measures of tongue strength and endurance. Journal of Speech Language and Hearing Research 43, 3: 584–594. [Google Scholar] [CrossRef]
- Vaiman, M., S. Segal, and E. Eviatar. 2004. Surface electromyographic studies of swallowing in normal children, age 4-12 years. International Journal of Pediatric Otorhinolaryngology 68, 1: 65–73. [Google Scholar] [CrossRef]
- Winter, A. 1985. Using the Boley gauge: How do you measure up? Dental Assistant. (Waco Tx) 4, 4: 24. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2008 by the authors. 2008 Licia Coceani Paskay,