Abstract
The purpose of this study was to investigate the distribution of causes of dysphagia and the types of treatments being provided at the Dysphasia/Dysphagia Rehabilitation Clinic of Showa University Dental Hospital. The subjects included 173 dysphagic patients. Fifty-three percent of patients ranged 0–12 age, and 24% of them were over 60 years old. The survey results showed that diseases of the central nervous system, such as cerebral palsy (CP), was a major diagnosis in young patients, and cerebrovascular accident (CVA) was a predominant cause in adult and elderly patients. Diagnosis distribution showed that swallowing dysfunction was the most frequent diagnosis for patients on their first visit when compared to other feeding dysfunctions including malfunction of lips, tongue, and mastication. Almost 40% of patients still continue to have rehabilitation for their dysphagic symptoms at the end of March 2002. This suggests that dysphagia rehabilitation is needed for a long time for many disabled individuals.
INTRODUCTION
The role of dentistry is to maintain and improve oral health, and the role of the orofacial region is eating, pulmonary breathing and communication. There are many individuals who are not able to masticate or swallow food safely due to various diseases. Even though the goal of dentistry is to improve and maintain oral health, professionals in dentistry should provide their advanced technology for individuals who have dysphagia. Dysphagia, a feeding disorder, is a difficulty in one or more stages of deglutition from placement of food in the mouth, oral motor manipulation and control of the bolus, triggering of the swallowing action and pharyngeal peristalsis, through relaxation of the cricopharyngeal sphincter which allows the bolus to pass into the esophagus. Etiologies of such disturbances include varied neuropathologies, head and neck disease, in addition to other medical and psychological problems which may affect oral nutritional intake (Groher, 1992). The causes of dysphagia are divided into the morphological abnormality, neurological muscular disorder, and declining function due to aging (Kaneko, 1998). The anatomical cause includes a congenital cause such as cleft palate, or an acquired cause such as post-operative defect of the oral and pharyngeal region. Neuromuscular disorders include developmental causes such as cerebral palsy or mental retardation, and half way failures such as cerebrovascular disease (half way failures include diseases, injuries, or degeneration that occur as a person ages). And, the etiology, which should not be forgotten, is a deterioration of function by aging. (Figure 1).
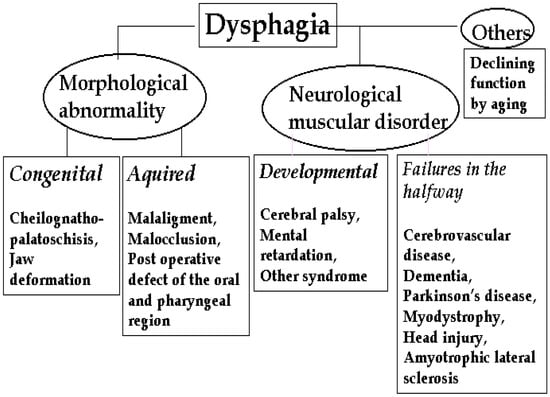
Figure 1.
Causes of Dysphagia
The problem is that various diseases may cause dysphagia at any time. Particularly, the main effect of aging for the oral region is tooth loss. In addition to the edentulous situation, there are many anatomical changes that occur, including the loss of tone in muscles supporting larynx. There are reports that the elderly present with the laryngeal position located lower than in the healthy adult (Blonsky, Logemann, Boshes, Fisher, 1975; Kahane, 1981).
Therefore, the muscle must move the larynx for longer distance with weaker power. Thus, it is important to know what kind of disease and factors frequently cause dysphagia. The purpose of this study was to investigate the distribution of causes of dysphagia and indicate the kind of treatments we are doing at the Dysphasia/Dysphagia Rehabilitation Clinic of Showa University Dental Hospital (DDRC).
PROCEDURES
The Dysphasia/Dysphagia Rehabilitation Clinic of Showa University Dental Hospital consists of multiple divisions: Hygiene and Oral Health, Oral Surgery, Pedodontics, Gerodontology, Dental Anesthesiology and others. During a three-year period, 285 patients have visited the DDRC, and 173 were dysphagic patients of the department of Hygiene and Oral Health. This study included patients who had medical and dental examinations at the department of Hygiene and Oral Health. The distribution of causes and treatments of dysphagia was investigated by surveying and statistical analysis on the data obtained from the patients' charts.
Patient’s Information
The subjects were 173 dysphagic patients. Fifty-three percent of patients ranged 0-12 age, and 24% of the patients were over 60 years old. (Figure 2) The survey results showed that disease of central nervous system, such as cerebral palsy (CP), was a major diagnosis in immature patients, while cerebrovascular accident (CVA) was a predominant cause in adult and elderly patients. (Figure 3) Dentists diagnosed each patient’s functional level using the 8 steps of developmental feeding course (Ayano, 1999) (Table 1) and the 8 steps of dysfunctional levels (Mukai, 1995).
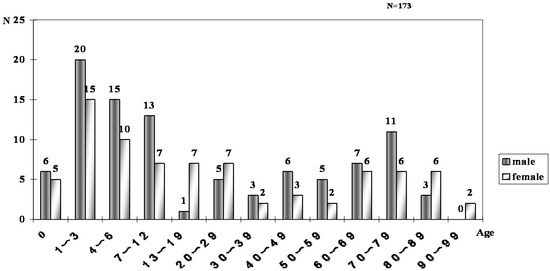
Figure 2.
Age and Sex
Diagnosis distribution showed that swallowing dysfunction was the most frequent diagnosis for patients on their first visit when compared to other feeding dysfunctions including malfunction of lips, tongue, and mastication. (Figure 4)
Treatment Process For Dysphagia At The Clinic
The treatment for dysphagic individuals’ processes at DDRC is shown in Table 2.
First, dentist and dental hygienists discuss the patient’s symptoms and feeding problems. Then an examination of the oral conditions and functions is completed. Next, assessment of the patient’s ability for feeding and swallowing is conducted using the Repetitive Saliva Swallowing Test (Oguchi, 2000) and the Food Test (Mukai, 1998). The Repetitive Saliva Swallowing Test (RSST) is an assessment of the patient’s potential to swallow saliva. It is performed by counting the frequency of swallowing over a 30 second period. Oguchi et al. investigated the correlation between the RSST and Videofluorography (VF) in association with aspiration. Using a standard of three swallowing cycles within a 30 second period, they demonstrated a high correlation between aspiration and RSST. The Food Test (FT) is an evaluation of tongue function during food bolus formation and transportation using some material test foods. If necessary, special evaluation methods are used including video-fluorography (Logemann, 1993), ultrasonography (Sonies, Baum, Shawker, 1984; Kenny, Cases, McPherson, 1989) and endoscopic observation (Bastian, 1991).
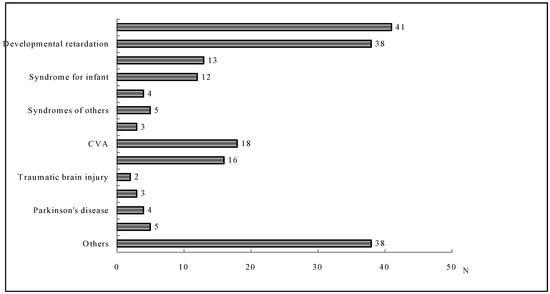
Figure 3.
Diagnosis
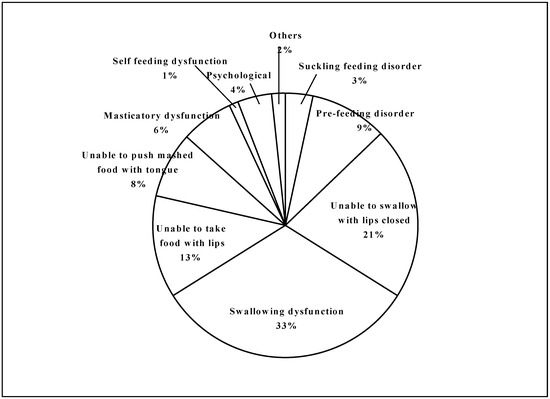
Figure 4.
Assessment of feeding functions for all patients at first visit

Table 1.
Developmental course of the feeding function
Table 1.
Developmental course of the feeding function
| First step | Suckle feeding and pre-feeding period |
| Second step | Acquiring the ability to swallow with lip closed |
| Third step | Acquiring the ability to take food with lip closed |
| Fourth step | Acquiring the ability to push the mashed food with tongue against anterior hard palate |
| Fifth step | Acquiring the ability to perform mastication |
| Sixth step | Beginning self-feeding |
| Seventh step | Beginning finger feeding |
| Eighth step | Beginning using tableware |

Table 2.
Treatment Process
Table 2.
Treatment Process

Videofluorography
Videofluorography (VF) is one of the most effective evaluation methods for diagnosing dysphagia. Functional movements of oral, pharyngeal, and esophageal organs as well as food bolus transfer can be evaluated by this technique. That is to say, the movements of food bolus and various organs are able to be seen using radiopaque-material-containing foods.
At DDRC, VF is performed twice a week for a maximum of eight people a day. The total number of patients who were examined using VF was 67. Year after year, the number of videofluorography examination has increased.
The distribution of diagnosed diseases within the cases using VF was investigated. Aspiration is a serious consequence of dysphagia. Aspiration is the passage of food or liquid through or under the vocal folds. Individuals who aspirate are at increased risk for the occurrence of series respiratory sequelae, including airway obstruction and aspiration pneumonia. Aspiration is often caused by impaired laryngeal closure, but it may also occur because of the overflow of food or liquids retained in the pharynx (Palmer, 2000). The results suggested that patients with diseases of central nervous system such as cerebral palsy for infants, and cerebrovascular accident for adults might have high risk of incidence for aspiration or other severe symptoms. (Figure 5) It needs to be understood that oral bacteria are one of the causes for aspiration pneumonia. Therefore, dental professional should prevent aspiration pneumonia by proper oral health care. At DDRC, dental hygienists are instructed about a patient’s oral hygiene control on a case-by-case basis. (Figure 6)
Dysphagia Rehabilitation
- 1)
- Environmental therapy
After a dentist assesses a patient’s functional level, the dentist applies feeding training to improve the patient’s dysphagic symptoms. Dysphagia rehabilitation includes not only special training but also environmental therapy. For the environmental therapy, the following are necessary: psychological consideration, comfortable atmosphere for the meal, helper’s efforts, and selection of appropriate utensils. In addition, guidance for an appropriate feeding posture is also very important to eating safety.
- 2)
- Diet therapy
An appropriate food type for safe patient swallowing needs to be identified. This includes thickened food, solid food, and pureed food. Sometimes a natural material is added to increase viscosity of the meal. Careful attention needs to be paid so that patients do not become victims of malnutrition and dehydration.
- 3)
- Positive training
Functional training includes indirect therapy without food ingestion and direct therapy using foods.
- Indirect training
Indirect therapy can be applied to tube-feeding patients as no risk of food aspiration is anticipated (Table 3). Most of the techniques have been developed at Children’s Hospital in Vangede in Denmark (Kaneko, 1987). One of the techniques of indirect therapy called “Gum-rubbing” is shown in Figure 6. The operator rubs the alveolar mucosa, and that stimulation provokes a swallowing reflex.
- Direct training
Direct therapy is functional therapy using foods in feeding and swallowing (Table 4) Guided necessary movements for feeding and swallowing during the meal are provided by holding the patient's head in the mid-position not leaning backward, and by assisting jaw and lip movements when the patient's tongue-thrust is prominent.
Figure 6.
Gum-rubbing
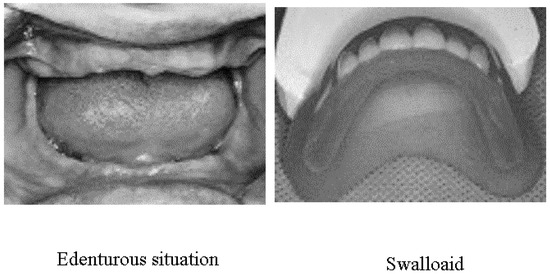
Figure 7.
Edentulous Situation & Swalloaid

Table 3.
Indirect training
Table 3.
Indirect training
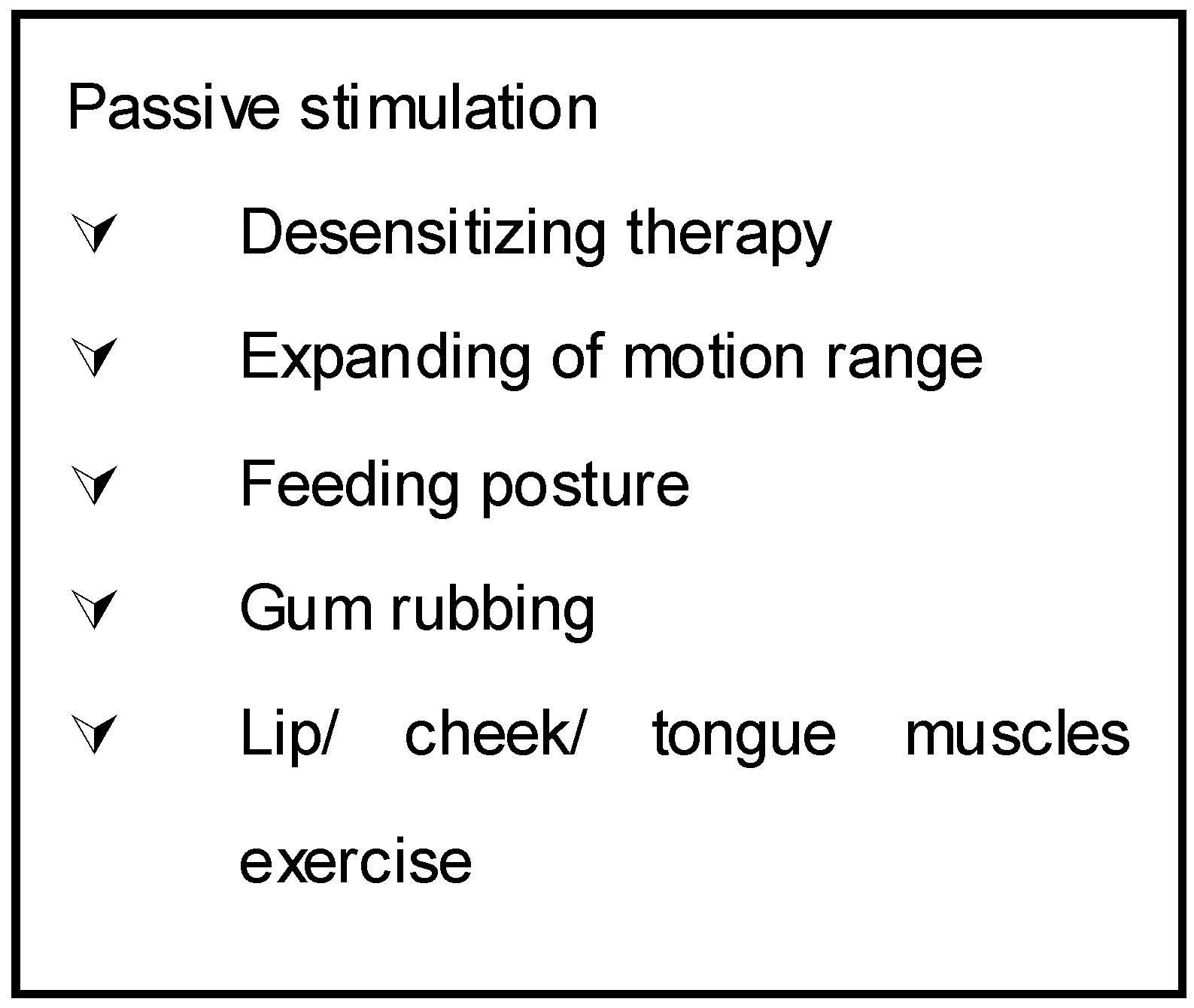

Table 4.
Direct therapy
Table 4.
Direct therapy
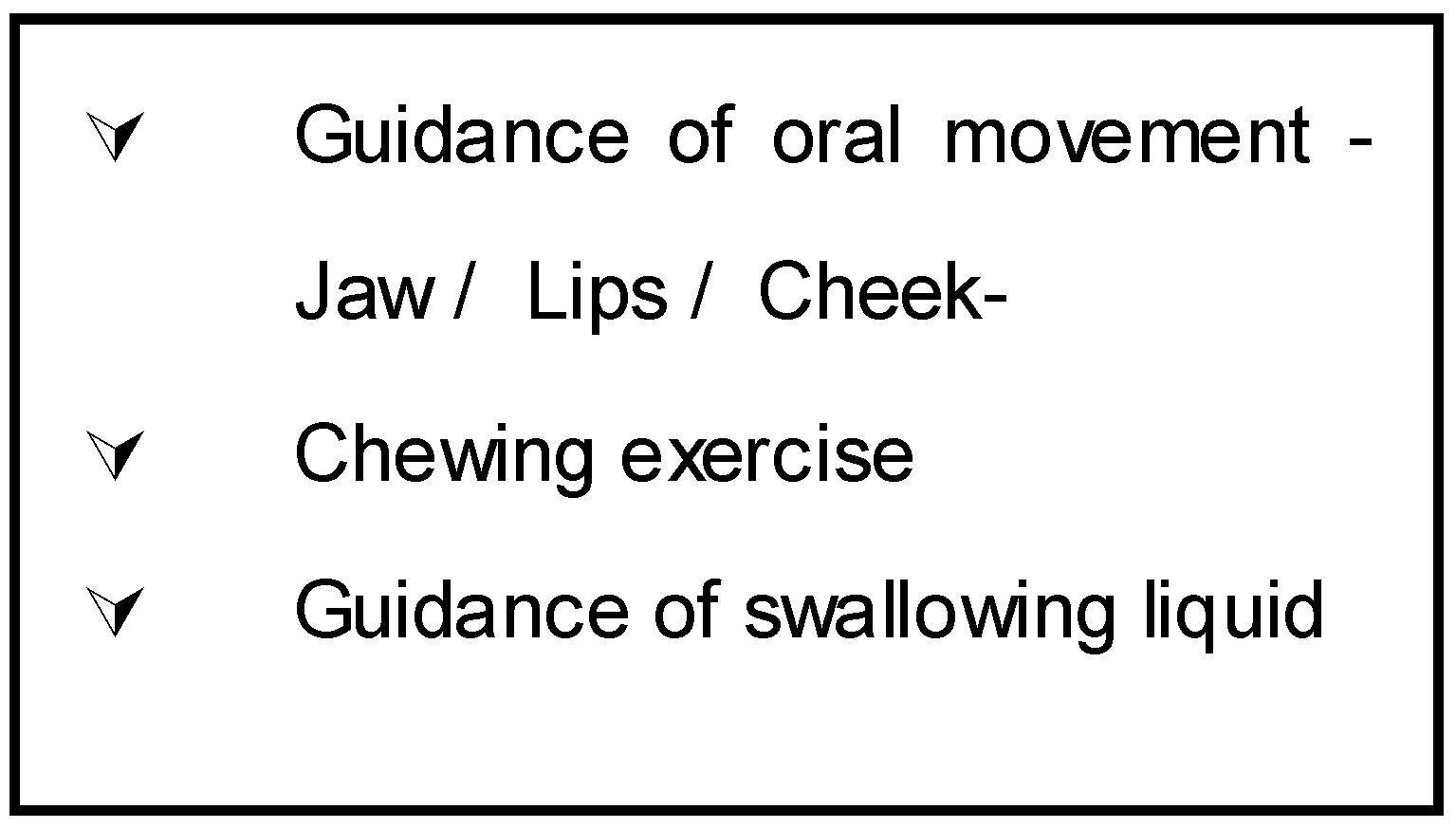
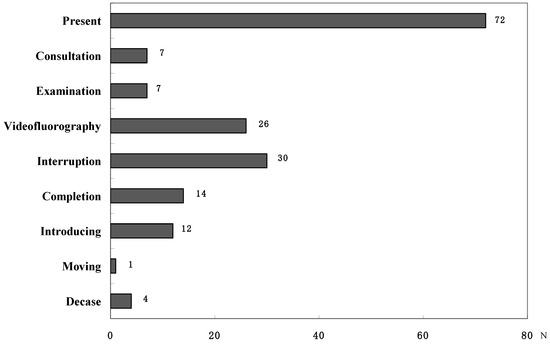
Figure 8.
Treatment outcomes of individuals
- Prosthodontic approach
Various prostheses are effective for dysphagic symptoms. Stabilized occlusion of dentures is very important for the swallowing movement of the tongue (Tamura, 2002). Staff at DDRC has developed a new apparatus named Swalloaid for helping swallowing function of edentulous dysphagic patients who could not wear dentures due to some problem (Mukai, 1998; Tamura, 2002). The appliance consists of a modified maxillary denture with anterior denture teeth and posterior bite rims made of a soft denture liner. It was well accepted by the patient, and oral dyskinesia was improved. A more controlled swallow can be achieved through mandibular stabilization and minimization of unfavorable tongue thrust. This appliance can be a useful prosthetic treatment for edentulous dysphagic patients. Traditional prosthetic apparatus are also used for many cases, especially conventional dentures, palatal augmentation prostheses (PAP), palatal lift palate (PLP), as well as some other devices.
TREATMENT OUTCOMES
Figure 8 shows treatment progress at the end of March 2002. Almost 40 % of patients still continue to have rehabilitation for their dysphagic symptoms. It suggests that dysphagia rehabilitation is needed for a long time for many disabled individuals. There were many requests for videofluorography examination from the general practitioner. It is characteristic of DDRC to cooperate with the community.
CONCLUSIONS AND RECOMMENDATIONS
Dysphagia is a disability, which could happen to anybody at any moment. Thus, professionals in dentistry should contribute our knowledge and techniques to help dysphagic patients. The results of this study suggested that the professional dental approach and treatments at the DDRC with community cooperation are very important and promising for dysphagia rehabilitation.
ACKNOWLEDGEMENT
The authors wish to thank to Dr. Shiro Suzuki D.D.S., Ph.D. at The University Alabama at Birmingham, USA and Dr. Hiroshi Sasaki D.D.S., Ph.D. at UTAKA DENTAL OFFICE for their accommodating reinforcement.
REFFERENCES
- Ayano, R., F. Tamura, Y. Ohtsuka, and Y. Mukai. 2000. The development of normal feeding and swallowing: Showa University study of the feeding function. International Journal Orofacial Myology 26: 24–32. [Google Scholar] [CrossRef]
- Bastian, R. W. 1991. Videoendoscopic evaluation of patients with dysphagia: an adjunct to the modified barium swallow. Otolaryngol Head Neck Surg 104: 339–350. [Google Scholar] [CrossRef] [PubMed]
- Blonsky, E. R., J. A. Logemann, B. Boshes, and H. B. Fisher. 1975. Comparison of speech and swallowing in patients with tremor disorders and in normal geriatric patients: A cinefluorographic study. Journal of Gerontology 30: 299–303. [Google Scholar] [CrossRef] [PubMed]
© 2004 by the authors. 2004 Tamura, F., Ayano, R., Haishima, H., Ishida, R., Mizukami, M., Mukai, Y.