Abstract
People aged 65+ are generally polymedicated. In this age group, it is important to be aware of the potential for drug-induced photosensitivity. Sunscreen use is an effective way to prevent sun damage to the skin. Our study aimed to evaluate sunscreen use habits in 104 non-institutionalized elderly people aged 65 years and older and the taking/use of photosensitizing medications. It was concluded that all but one of the elderly take photosensitizing drugs but do not use sunscreen regularly. Although all therapies were prescribed or advised by health professionals, virtually all the elderly stated that they did not receive advice on this matter.
1. Introduction
Photodermatoses are a group of skin problems induced by ultraviolet radiation and, in some cases, visible light. Drug-induced photosensitivity includes photoallergy and phototoxicity and is one of the most common photodermatoses [1]. The rate of cases of photosensitization has been steadily increasing. This may be associated with excessive sun exposure to achieve a socially valued suntan, but also with an increase in exogenous triggers present in foods, dietary supplements, cosmetics, and pharmaceuticals. Medicines represent a large percentage of photosensitizing substances, leading to an increased risk of sunburn, rashes, and other types of skin lesions. Hundreds of drugs administered topically or systemically are implicated in photosensitivity reactions by means of complex mechanisms [2]. These include antimicrobial, cardiovascular, antihyperlipidemic, psychotropic, antineoplastic [2], and non-steroidal anti-inflammatory [3] drugs. Photosensitivity is a skin-related adverse drug reaction which can lead to additional complications demanding hospitalization and the restriction of the use of some medications. The elderly population are particularly prone to drug-induced photosensitivity due to multiple pathologies and polypharmacy-related problems; complex therapeutic regimens, mainly in industrialized societies, result in a burden on healthcare systems.
Regular use of sunscreen is one of the main methods of preventing photodermatoses. However, compliance with sun protection guidelines is highly variable and tends to be poor and gender dependent [4,5]. The prevalence of sunscreen non-usage reported in the literature ranges from 9.9% to 68% [6,7]. In 2020, the percentage of seniors over 65 who always used sunscreen was 13.6% in men and 30.9% in women [5]. Nevertheless, little is known about sun protection habits in the medicated elderly, especially those living in a familiar environment and subject to some daily sun exposure. Thus, our study aimed to analyze the sun protection practices of non-institutionalized elderly people medicated with at least two medications and to evaluate the relationship between these practices and the use of photosensitizing drugs.
2. Materials and Methods
A cross-sectional study was conducted in May 2023 with elderly people over 65 years old, taking at least two medicines and living alone or with relatives, in Portugal and abroad. Upon acceptance of the participants, informed consent was signed. Participants were requested to show the packages of all medicines they were taking at the time of the interview, and a series of demographic and anthropometric data were collected, such as age, gender, nationality, and composition of the family household. Additionally, habits of sun protection were assessed through the question “Do you use sunscreen?”. Respondents had four options, namely: “never”, “rarely”, “only in summer”, and “regularly”.
Medicines taken by the elderly were characterized in terms of ATC code, route of administration, prescriber, and photosensitizing potential. Drug-induced photosensitivity appears to be underreported, mainly due to issues of difficult clinical recognition and scarce documentation in public databases. For the present work, the potential for drug photosensitivity was assessed through an extensive literature search, including reviews, clinical cases, summary of product characteristics (SmPC), package leaflets (PL), and databases such as Medscape [8].
Since variables of interest are measured on a nominal or ordinal scale, the association between them was assessed using the Spearman correlation coefficient or contingency tables and the chi-square test of independence. All statistical tests were applied at the 5% level of significance, using SPSS 28 (Armonk, NY, USA: IBM Corp.). An association between habits of sun protection and nationality was not assessed due to the scarcity of data per cell.
3. Results
3.1. Subjects
Demographic, Anthropometric, and Social Behavior Data
A total of 104 seniors with an average age of 78.4 years old (range 65 to 96 years) were included in the study. Table 1 lists the frequency of the variables of interest. The percentage of individuals who do not use sunscreen is undistinguishable from those who use it only in summer (sig. = 0.305), but it is higher than those who rarely (sig. = 0.002) or regularly use it (sig. < 0.001).

Table 1.
Demographic and social behavior data of participants.
3.2. Therapeutics
3.2.1. Therapeutic Groups
A total of 489 drugs were taken by the participants (average 4.7 drugs/elderly), corresponding to 168 different molecules from 14 therapeutic groups. The top three groups were cardiovascular system (28.7%); nervous system (19.5%); and alimentary tract and metabolism (14.9%).
3.2.2. Route of Administration
More than 93% of the drugs were administered via the oral route (Figure 1).
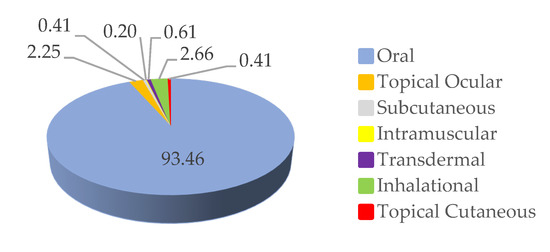
Figure 1.
Routes of drug administration used by the elderly in the study.
3.2.3. Photosensitizing Drugs
Ninety-nine percent of the elderly people who participated in the study use between 1 and 13 photosensitizing drugs (Figure 2). Only one elderly person was not taking any photosensitizing medicine.
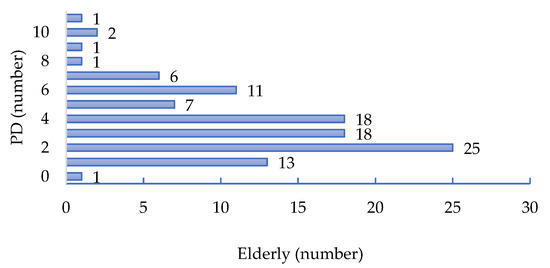
Figure 2.
Number of photosensitizing drugs (PD) taken by the elderly.
3.3. Associations between Use of Sunscreen Habits and Variables of Interest
3.3.1. Gender
There is no association between gender and use of sunscreen habits according to the chi-square test for independence (sig. = 0.470).
3.3.2. Use of Photosensitizing Drugs
A Spearman correlation coefficient of −0.104 was estimated from the data of n = 104 subject, with an estimated significance of 0.157. In conclusion, no association exists between skin protection and the use of photosensitizing medicines.
3.3.3. Household
The association with ‘living alone’ was assessed using contingency tables and the chi-square test of independence, which showed that the variables are not associated (sig. = 0.297). The same lack of association was observed between skin protection behavior and living with younger adults (<65 y.o.) (sig. = 0.428).
4. Discussion and Conclusions
Nearly all the elderly people in this study took several photosensitizing drugs, but they did not have regular habits of sun protection. In fact, only 7.4% of the participants used sunscreen regularly. This value is lower than 13.6% and 30.9% previously reported for men and women in the same age group [5]. To our knowledge, there are no published data on the sun protection habits of the elderly (institutionalized or in a home environment) who take photosensitizing medications. In the present study, no questions were asked about the eventual symptoms of photodermatoses. Moreover, the duration of the treatments is not known. Although all the medicines were prescribed by a doctor (99.6%) or advised to be taken by a pharmacist (0.4%), only in two cases did a participant report being informed of the importance of using sunscreen during the therapy. To minimize the risk of skin lesions caused by photosensitizing drugs, it is of the utmost importance that the elderly be advised to use sunscreen whenever therapy includes such medication.
Author Contributions
Conceptualization, M.D.A. and I.M.C.; formal analysis, J.B. and M.D.A.; investigation, M.D.A. and I.M.C.; writing—original draft preparation, M.D.A.; writing—review and editing, M.D.A., I.M.C. and J.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Egas Moniz School of Health and Science (protocol code 1230, 25th of May 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions.
Acknowledgments
The authors acknowledge the third-year students of the Integrated Masters in Pharmaceutical Sciences of IUEM, Egas Moniz School of Health and Science for their help with data collection.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Blakely, K.M.; Drucker, A.M.; Rosen, C.F. Drug-Induced Photosensitivity-An Update: Culprit Drugs, Prevention and Management. Drug Saf. 2019, 42, 827–847. [Google Scholar] [CrossRef] [PubMed]
- Kowalska, J.; Rok, J.; Rzepka, Z.; Wrześniok, D. Drug-Induced Photosensitivity-From Light and Chemistry to Biological Reactions and Clinical Symptoms. Pharmaceuticals 2021, 14, 723. [Google Scholar] [CrossRef] [PubMed]
- Blanca-Lopez, N.; Soriano, V.; Garcia-Martin, E.; Canto, G.; Blanca, M. NSAID-induced reactions: Classification, prevalence, impact, and management strategies. J. Asthma Allergy 2019, 12, 217–233. [Google Scholar] [CrossRef] [PubMed]
- Bocquier, A.; Fressard, L.; Legleye, S.; Verger, P.; Peretti-Watel, P. Social Differentiation of Sun-Protection Behaviors: The Mediating Role of Cognitive Factors. Am. J. Prev. Med. 2016, 50, e81–e90. [Google Scholar] [CrossRef] [PubMed]
- Rep, M.M.M. QuickStats: Percentage of Adults Aged ≥18 Years Who Always Use Sunscreen When Outside for >1 Hour on a Sunny Day, by Sex and Age Group—National Health Interview Survey, United States, 2020; Centers for Disease Control and Prevention (CDC): Hyattsville, MD, USA, 2022; Volume 71, p. 747. [Google Scholar] [CrossRef]
- Bertolin, M.; Cercatto, M.C.; Requena, C.; Serra-Guillen, C.; Llombart, B.; Sanmartin, O.; Guillen, C.; Nagore, E. Awareness, Attitude, and Adherence to Preventive Measures in Patients at High Risk of Melanoma. A Cross-Sectional Study on 185 Patients. J. Cancer Educ. 2015, 30, 552–566. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, E.S.; Dumith, S.C. Non-use of sunscreen among adults and the elderly in southern Brazil. An. Bras. Dermatol. 2019, 94, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Drugs & Diseases. Available online: https://reference.medscape.com/ (accessed on 16 May 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).