A Retrospective Database Study of Health Costs among United States Older Adults Who Documented Having Pain and Functional Impairment
Abstract
1. Introduction
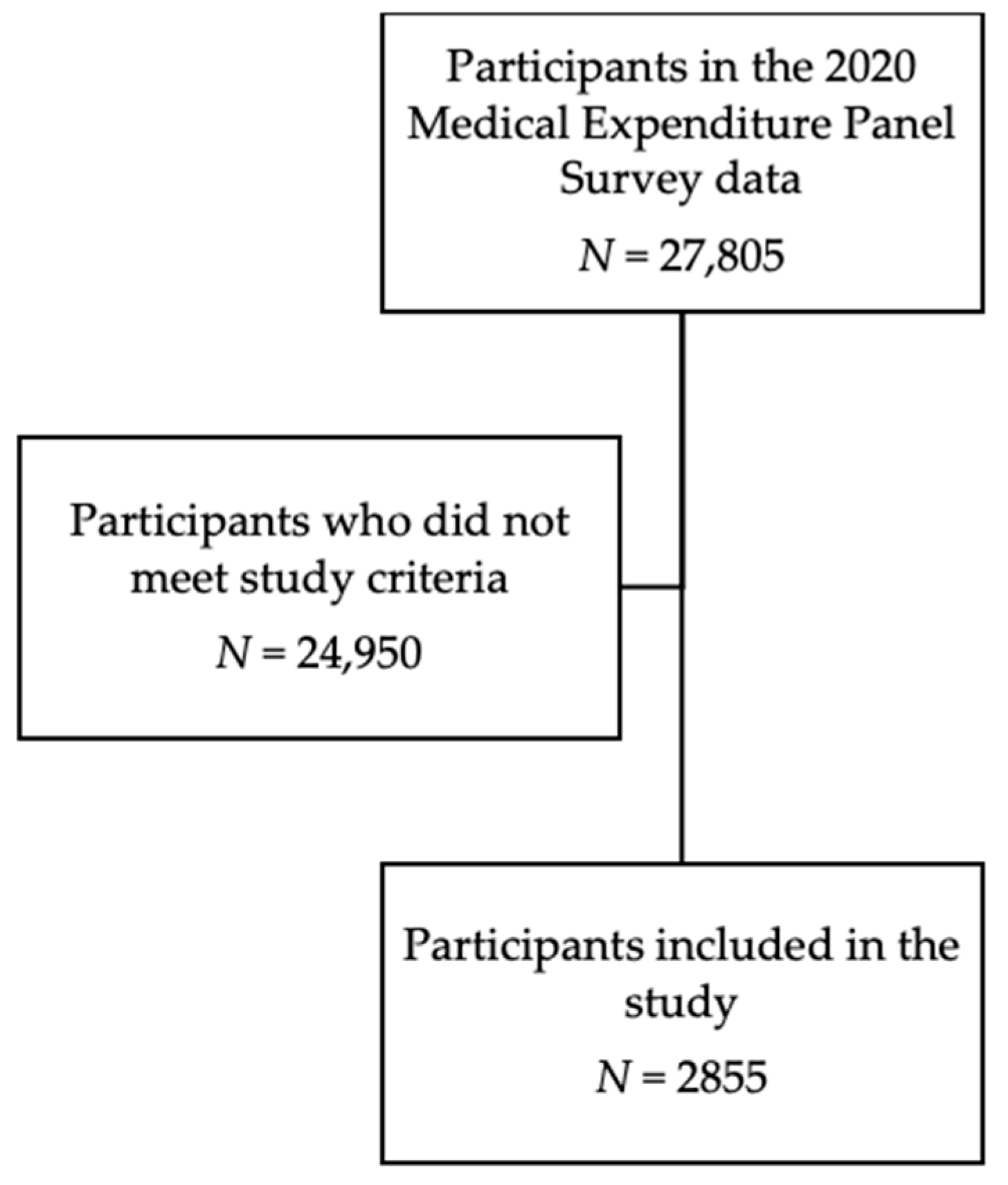
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nahin, R.L. Estimates of pain prevalence and severity in adults: United States, 2012. J. Pain 2015, 16, 769–780. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.V.; Guralnik, J.M.; Dansie, E.J.; Turk, D.C. Prevalence and impact of pain among older adults in the United States: Findings from the 2011 National Health and Aging Trends Study. Pain 2013, 154, 2649–2657. [Google Scholar] [CrossRef]
- Axon, D.R.; Patel, M.J.; Martin, J.R.; Slack, M.K. Use of multidomain management strategies by community dwelling adults with chronic pain: Evidence from a systematic review. Scand. J. Pain 2019, 19, 9–23. [Google Scholar] [CrossRef]
- Axon, D.R.; Bhattacharjee, S.; Warholak, T.L.; Slack, M.K. Xm2 scores for estimating total exposure to multimodal strategies identified by pharmacists for managing pain: Validity testing and clinical relevance. Pain Res. Manag. 2018, 2018, 2530286. [Google Scholar] [CrossRef]
- Gaskin, D.J.; Richard, P. The economic costs of pain in the United States. J. Pain 2012, 13, 715–724. [Google Scholar] [CrossRef]
- Stamm, T.A.; Pieber, K.; Crevenna, R.; Dorner, T.E. Impairment in the activities of daily living in older adults with and without osteoporosis; osteoarthritis and chronic back pain: A secondary analysis of population-based health survey data. BMC Musculoskelet. Disord. 2016, 17, 139. [Google Scholar] [CrossRef]
- Valderrama-Hinds, L.M.; Al Snih, S.; Rodriguez, M.A.; Wong, R. Association of arthritis and vitamin D insufficiency with physical disability in Mexican older adults: Findings from the Mexican Health and Aging Study. Rheumatol. Int. 2017, 37, 607–616. [Google Scholar] [CrossRef]
- Makris, U.E.; Fraenkel, L.; Han, L.; Leo-Summers, L.; Gill, T.M. Restricting back pain and subsequent mobility disability in community-living older persons. J. Am. Geriatr. Soc. 2014, 62, 2142–2147. [Google Scholar] [CrossRef]
- Eggermont, L.H.P.; Leveille, S.G.; Shi, L.; Kiely, D.K.; Shmerling, R.H.; Jones, R.N.; Guralnik, J.M.; Bean, J.F. Pain characteristics associated with the onset of disability in older adults: The maintenance of balance, independent living, intellect, and zest in the elderly Boston study. J. Am. Geriatr. Soc. 2014, 62, 1007–1016. [Google Scholar] [CrossRef]
- Freedman, V.A.; Spillman, B.C.; Andreski, P.M.; Cornman, J.C.; Crimmins, E.M.; Kramarow, E.; Lubitz, J.; Martin, L.G.; Merkin, S.S.; Schoeni, R.F.; et al. Trends in late-life activity limitations in the United States: An update from five national surveys. Demography 2013, 50, 661–671. [Google Scholar] [CrossRef]
- Fuller-Thomson, E.; Yu, B.; Nuru-Jeter, A.; Guralnik, J.M.; Minkler, M. Basic ADL disability and functional limitation rates among older AMERICANS from 2000-2005: The end of the decline? The Journals of Gerontology. Ser. A Biol. Sci. Med. Sci. 2009, 64, 1333–1336. [Google Scholar] [CrossRef]
- Dieleman, J.L.; Cao, J.; Chapin, A.; Chen, C.; Li, Z.; Liu, A.; Horst, C.; Kaldjian, A.; Matyasz, T.; Scott, K.W.; et al. US health care spending by payer and health condition, 1996–2016. JAMA 2020, 323, 863–884. [Google Scholar] [CrossRef]
- Wolff, J.L.; Starfield, B.; Anderson, G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch. Intern. Med. 2002, 162, 2269–2276. [Google Scholar] [CrossRef]
- Axon, D.R.; Le, D. Association of self-reported functional limitations among a national community-based sample of older United States adults with pain: A cross-sectional study. J. Clin. Med. 2021, 10, 1836. [Google Scholar] [CrossRef]
- Individuals Living in the Community with Chronic Conditions and Functional Limitations: A Closer Look. Available online: https://aspe.hhs.gov/sites/default/files/private/pdf/75961/closerlook.pdf (accessed on 3 April 2023).
- Housing America’s Older Adults. Available online: https://www.jchs.harvard.edu/sites/default/files/media/imp/Harvard_JCHS_Housing_Americas_Older_Adults_2018.pdf (accessed on 3 April 2023).
- Chan, L.; Beaver, S.; Maclehose, R.F.; Jha, A.; Maciejewski, M.; Doctor, J.N. Disability and health care costs in the Medicare population. Arch. Phys. Med. Rehabil. 2002, 83, 1196–1201. [Google Scholar] [CrossRef]
- Van der Heyden, J.; Van Oyen, G.H.; Berger, N.; De Bacquer, D.; Van Herck, K. Activity limitations predict health care expenditures in the general population in Belgium. BMC Public Health 2015, 15, 267. [Google Scholar] [CrossRef]
- National Health Expenditures; 2019: Steady Spending Growth Despite Increases in Personal Health Care Expenditures in Advance of the Pandemic. Available online: https://www.ama-assn.org/system/files/2021-05/prp-annual-spending-2019.pdf (accessed on 3 April 2023).
- Medical Expenditure Panel Survey Background. Available online: https://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp (accessed on 3 April 2023).
- MEPS HC-224 2020 Full Year Consolidated Data File. Available online: https://meps.ahrq.gov/data_stats/download_data/pufs/h224/h224doc.pdf (accessed on 3 April 2023).
- MEPS HC-224 2020 Full Year Consolidated Data Codebook. Available online: https://meps.ahrq.gov/data_stats/download_data/pufs/h224/h224cb.pdf (accessed on 3 April 2023).
- High-Need; High-Cost Patients: Who Are They and How Do They Use Health Care? Available online: https://www.commonwealthfund.org/publications/issue-briefs/2016/aug/high-need-high-cost-patients-who-are-they-and-how-do-they-use (accessed on 3 April 2023).
- Anderson, W.L.; Armour, B.S.; Finkelstein, E.A.; Wiener, J.M. Estimates of state-level health-care expenditures associated with disability. Public Health Rep. 2010, 125, 44–51. [Google Scholar] [CrossRef]
- Guccione, A.A.; Felson, D.T.; Anderson, J.J.; Anthony, J.M.; Zhang, Y.; Wilson, P.W.; Kelly-Hayes, M.; Wolf, P.A.; Kreger, B.E.; Kannel, W.B. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am. J. Public Health 1994, 84, 351–359. [Google Scholar] [CrossRef]
- Lee, J.; Abdel-Kader, K.; Yabes, J.G.; Cai, M.; Chang, H.-H.; Jhamb, M. Association of self-rated health with functional limitations in patients with CKD. Kidney Med. 2021, 3, 745–752. [Google Scholar] [CrossRef]
- Jindai, K.; Nielson, C.M.; Vorderstrasse, B.A.; Quinones, A.R. Multimorbidity and functional limitations among adults 65 or alder, NHANES 2005-2012. Prev. Chronic Dis. 2016, 13, E151. [Google Scholar] [CrossRef]
- Marupuru, S.; Axon, D.R. Association of multimorbidity on healthcare expenditures among older United States adults with pain. J. Aging Health 2021, 33, 741–750. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Goodin, A.J.; Pahor, M.; Manini, T.; Brown, J.D. Healthcare utilization and physical functioning in older adults in the United States. J. Am. Geriatr. Soc. 2020, 68, 266–271. [Google Scholar] [CrossRef] [PubMed]
- Whaley, C.; Reed, M.; Hsu, J.; Fung, V. Functional limitations, medication support, and responses to drug costs among Medicare beneficiaries. PLoS ONE 2015, 10, e0144236. [Google Scholar] [CrossRef] [PubMed]
- Campbell, P.J.; Axon, D.R.; Taylor, A.M.; Smith, K.; Pickering, M.; Black, H.; Warholak, T.; Chinthammit, C. Hypertension, cholesterol and diabetes medication adherence, health care utilization and expenditure in a Medicare Supplemental sample. Medicine 2021, 100, e27143. [Google Scholar] [CrossRef] [PubMed]
- Maresova, P.; Javanmardi, E.; Barakovic, S.; Husic, J.B.; Tomsone, S.; Krejcar, O.; Kuca, K. Consequences of chronic diseases and other limitations associated with old age—A scoping review. BMC Public Health 2019, 19, 1431. [Google Scholar] [CrossRef] [PubMed]
- Von Bonsdorff, M.B.; Rantanen, T. Progression of functional limitations in relation to physical activity: A life course approach. Eur. Rev. Aging Phys. Act. 2011, 8, 23–30. [Google Scholar] [CrossRef]
- Lubitz, J.; Cai, L.; Kramarow, E.; Lentzner, H. Health, life expectancy, and health care spending among the elderly. N. Engl. J. Med. 2003, 349, 1048–1055. [Google Scholar] [CrossRef]

| Variables | Total (Weighted N = 40,092,210) Weighted % (95% Confidence Interval) | Functional Impairment (Weighted N = 14,847,351) Weighted % (95% Confidence Interval) | No Functional Impairment (Weighted N = 25,244,859) Weighted % (95% Confidence Interval) | p |
|---|---|---|---|---|
| Age (years) | <0.0001 | |||
| 50–64 | 46.1 (43.7, 48.6) | 38.7 (35.2, 42.3) | 50.5 (47.4, 53.6) | |
| ≥65 | 53.9 (51.4, 56.3) | 61.3 (57.7, 64.8) | 49.5 (46.4, 52.6) | |
| Gender | <0.0001 | |||
| Male | 45.4 (43.4, 47.4) | 39.1 (35.9, 42.3) | 49.1 (46.3, 51.9) | |
| Female | 54.6 (52.6, 56.6) | 60.9 (57.7, 64.1) | 50.9 (48.1, 53.7) | |
| Education attained | 0.0005 | |||
| Up to and including high school | 44.8 (42.3, 47.3) | 49.6 (45.7, 53.4) | 41.9 (39.1, 44.8) | |
| Higher than high school | 55.2 (52.7, 57.7) | 50.4 (46.6, 54.3) | 58.1 (55.2, 60.9) | |
| Employment status | <0.0001 | |||
| Employed | 37.1 (34.7, 39.5) | 18.5 (15.6, 21.3) | 48.1 (45.2, 51.1) | |
| Unemployed | 62.9 (60.5, 65.3) | 81.5 (78.7, 84.4) | 51.9 (48.9, 54.8) | |
| Poverty level | <0.0001 | |||
| Poor to low income | 30.3 (28.0, 32.6) | 41.8 (38.4, 45.1) | 23.6 (20.9, 26.2) | |
| Middle to high income | 69.7 (67.4, 72.0) | 58.2 (54.9, 61.6) | 76.4 (73.8, 79.1) | |
| Health insurance coverage | <0.0001 | |||
| Private | 56.4 (53.9, 58.8) | 44.1 (40.8, 47.4) | 63.6 (60.7, 66.5) | |
| Public | 41.0 (38.7, 43.3) | 54.1 (50.9, 57.3) | 33.3 (30.5, 36.1) | |
| Uninsured | 2.7 (1.9, 3.4) | 1.8 (1.0, 2.6) | 3.2 (2.1, 4.3) | |
| Marital status | <0.0001 | |||
| Married | 56.5 (53.7, 59.2) | 44.5 (41.1, 47.9) | 63.5 (60.3, 66.8) | |
| Other | 43.5 (40.8, 46.3) | 55.5 (52.1, 58.9) | 36.5 (33.2, 39.7) | |
| Chronic conditions | <0.0001 | |||
| ≥3 | 63.5 (61.1, 65.9) | 78.4 (75.4, 81.4) | 54.8 (51.8, 57.8) | |
| <3 | 36.5 (34.1, 38.9) | 21.6 (18.6, 24.6) | 45.2 (42.2, 48.2) | |
| Frequent exercise | <0.0001 | |||
| Yes | 42.8 (40.3, 45.2) | 28.7 (25.4, 32.0) | 51.1 (47.9, 54.3) | |
| No | 57.2 (54.8, 59.7) | 71.3 (68.0, 74.6) | 48.9 (45.7, 52.1) | |
| Pain level | <0.0001 | |||
| Quite a bit to extreme | 22.9 (21.1, 24.8) | 43.1 (39.9, 46.2) | 11.1 (9.1, 13.1) | |
| Little to moderate | 77.1 (75.2, 78.9) | 56.9 (53.8, 60.1) | 88.9 (86.9, 90.9) | |
| General health state | <0.0001 | |||
| Excellent to good | 73.8 (71.7, 75.9) | 56.6 (52.8, 60.4) | 83.8 (81.6, 86.1) | |
| Fair to poor | 26.2 (24.1, 28.3) | 43.4 (39.6, 47.2) | 16.2 (13.9, 18.4) | |
| Mental health state | <0.0001 | |||
| Excellent to good | 86.4 (84.6, 88.1) | 78.0 (74.8, 81.1) | 91.3 (89.6, 93.1) | |
| Fair to poor | 13.6 (11.9, 15.4) | 22.0 (18.9, 25.2) | 8.7 (6.9, 10.4) | |
| Smoking status | 0.0003 | |||
| Smoker | 12.9 (11.5, 14.3) | 16.4 (14.1, 18.7) | 10.9 (9.0, 12.7) | |
| Non-smoker | 87.1 (85.7, 88.5) | 83.6 (81.3, 85.9) | 89.1 (87.3, 91.0) |
| Health Costs | Functional Impairment Mean $ (Standard Error) | No Functional Impairment Mean $ (Standard Error) | p |
|---|---|---|---|
| Total cost | 21,261 (1871) | 11,524 (866) | <0.0001 |
| Office cost | 4979 (776) | 3616 (294) | 0.0996 |
| Outpatient cost | 4471 (689) | 4138 (1046) | 0.7892 |
| Emergency department cost | 1852 (317) | 1847 (187) | 0.9890 |
| Inpatient cost | 24,974 (4988) | 26,500 (5351) | 0.8346 |
| Prescribed drug cost | 5533 (471) | 3105 (336) | <0.0001 |
| Health Cost | Unadjusted Beta (Standard Error) | Significance | Adjusted Beta (Standard Error) | Significance |
|---|---|---|---|---|
| Total cost | ||||
| Functional impairment | 0.84 (0.07) | <0.0001 | 0.45 (0.09) | <0.0001 |
| No functional impairment | Reference | Reference | ||
| Office cost | ||||
| Functional impairment | 0.31 (0.06) | <0.0001 | 0.14 (0.07) | 0.0528 |
| No functional impairment | Reference | Reference | ||
| Outpatient cost | ||||
| Functional impairment | 0.13 (0.12) | 0.2781 | 0.15 (0.14) | 0.2795 |
| No functional impairment | Reference | Reference | ||
| Emergency department cost | ||||
| Functional impairment | −0.04 (0.09) | 0.7463 | 0.05 (0.15) | 0.7613 |
| No functional impairment | Reference | Reference | ||
| Inpatient cost | ||||
| Functional impairment | −0.20 (0.17) | 0.2274 | −0.07 (0.17) | 0.6861 |
| No functional impairment | Reference | Reference | ||
| Prescribed drug cost | ||||
| Functional impairment | 0.94 (0.09) | <0.0001 | 0.43 (0.10) | <0.0001 |
| No functional impairment | Reference | Reference |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Axon, D.R.; Ullah, H. A Retrospective Database Study of Health Costs among United States Older Adults Who Documented Having Pain and Functional Impairment. Disabilities 2023, 3, 196-205. https://doi.org/10.3390/disabilities3020013
Axon DR, Ullah H. A Retrospective Database Study of Health Costs among United States Older Adults Who Documented Having Pain and Functional Impairment. Disabilities. 2023; 3(2):196-205. https://doi.org/10.3390/disabilities3020013
Chicago/Turabian StyleAxon, David R., and Humza Ullah. 2023. "A Retrospective Database Study of Health Costs among United States Older Adults Who Documented Having Pain and Functional Impairment" Disabilities 3, no. 2: 196-205. https://doi.org/10.3390/disabilities3020013
APA StyleAxon, D. R., & Ullah, H. (2023). A Retrospective Database Study of Health Costs among United States Older Adults Who Documented Having Pain and Functional Impairment. Disabilities, 3(2), 196-205. https://doi.org/10.3390/disabilities3020013







