Abstract
Background/Objectives: Kinematic measurements obtained from functional tests have been used to identify associated and risk factors for the development of lower limb dysfunction, allowing targeted interventions to reduce potential risks and guide rehabilitation. It is necessary to identify variables and tests with adequate reliability and with the capability to discriminate individuals with and without lower limb functional deficits. This study aimed to determine which single-legged test (single-leg squat and single-leg landing) and variables (angle at deepest instant and range of motion) present the best reliability and capability to discriminate individuals with and without lower limb functional deficits. Methods: The frontal plane kinematics of 86 adults, divided into 2 groups (43 with lower limb functional deficits and 43 without), as classified by the Lower Extremity Functional Scale, were assessed during single-leg squat and single-leg landing tasks. The differences between groups in trunk, pelvis, hip, and knee ranges of motion and angles were tested using the independent T test or Mann–Whitney U test, and the test–retest, inter-rater, and intra-rater absolute (standard error of measurement and minimal detectable difference) and relative (intraclass correlation coefficient) reliability were calculated. Results: Trunk (r = 0.47), hip (r = 0.40), and knee (r = 0.35) angles at the deepest instant, as well as range of motion of the trunk (r = 0.33), pelvis (r = 0.47), and knee (r = 0.32) during the single-leg landing discriminated between groups (p < 0.05). For the single-leg squat, no variable discriminated the groups. Test–retest, inter-rater, and intra-rater reliability ranged from poor to excellent, with minimal detectable differences remaining below 19°. Conclusions: The single-leg landing and pelvis range of motion were the most effective tests and variables for discriminating individuals with and without lower limb functional deficits. Most variables demonstrated moderate test–retest and excellent inter-rater and intra-rater reliability.
1. Introduction
Single-legged functional tests, such as the single-leg squat (SLS) and the single-leg landing (SLL), are commonly used to assess function and dynamic control of the lower limbs [1,2,3,4]. Features of the SLS and SLL are associated with the demands of daily life and sports tasks [5,6,7,8]. Two-dimensional (2D) frontal plane measurements have been used to identify individuals at increased risk of injury and to discriminate individuals with and without lower limb dysfunction [9,10,11,12]. A medial collapse of the knee in the SLS, leading to an augmented knee frontal plane projection angle (FPPA), is thought to increase the risk of patellofemoral pain [10] and of acute injuries in the lower limbs [12].
Measurement properties, such as the reliability, validity, and responsiveness, of a test should be determined before its full implementation in clinical practice [13]. The use of 2D frontal plane analysis in SLS has been supported by studies investigating its concurrent [14,15,16,17], predictive [10,12,18], and discriminative validity [7,9,11,19,20,21,22] and test–retest reliability [14,15,16,17,23,24]. Regarding the SLL, although a smaller number of concurrent [15,25], predictive [1,18], and discriminative validity [9] and test–retest reliability [23,24] studies have been conducted, most also support its use in clinical practice.
The SLL is faster, resulting in a greater impact but in smaller kinematic changes than the SLS [3,26,27]. These different demands possibly result in different discriminative and predictive capabilities of lower limb function. With regards to the reliability, most studies are focused on the test–retest reliability of the knee FPPA [14,15,16,17,23,24]. There is a lack of information about other forms of reliability, such as inter-rater [15,28] and intra-rater [28], and other joints, such as the trunk [14,23,28], pelvis [23], and hip [14,15,23]. Consequently, other fundamental measurement properties, such as the standard error of measurement (SEM), related to these other forms of reliability and other joints have also been poorly reported. Knowing the magnitude of the SEM is needed to distinguish true changes in the individual’s and/or group state from random measurement errors [29].
Most studies that investigated the discriminative validity of 2D kinematics during SLS and/or SLL analyzed measurements at a single instant, usually corresponding to the deepest instant of movement [2,4,7,9,20,21,22,27]. Another less common approach is the analysis of range of motion (RoM) [4,19,30]. RoM analysis considers the total angular amplitude during the gesture and not the angle at a single instant in time. These measurements might represent different features of the movement and consequently have a different discriminative capability.
Identifying 2D kinematic variables and tests that have adequate reliability and can better discriminate individuals with lower limb functional deficits is necessary for a more assertive and effective assessment, allowing us to select the most appropriate measures for clinical application and future research. The need to discriminate these individuals is not limited to separating the groups, but rather to validate tools that can be used for clinical assessment and for monitoring of compensatory movement patterns. This approach allows better targeting of interventions and improves decision-making in rehabilitation. Therefore, the purpose of this study was to determine which single-legged test (SLS vs. SLL) and which variables (angle at the deepest instant vs. RoM) present the best reliability and the best capability to discriminate individuals with and without lower limb functional deficits. We hypothesized that the analysis of joint RoM would yield a better discriminative capability than the analysis of joint angles and that the SLL could better discriminate individuals with and without lower limb functional deficits than the SLS. RoM can reflect movement variability throughout task execution, potentially revealing compensations and motor strategies that may not appear in a single-frame analysis.
The remainder of this paper is organized as follows: Section 2 describes the participants, experimental procedures, data analysis, and statistical analyses performed. Section 3 presents the main results of the study, including between-group comparisons and reliability data for kinematic variables during SLS and SLL. In Section 4, we discuss the implications of the findings, comparisons with previous studies, potential clinical applications, and limitations of the study. Finally, Section 5 highlights the main conclusions of the study and suggestions for future research.
2. Materials and Methods
2.1. Participants
Eighty-six individuals participated in this study, divided into two groups of forty-three participants each: without lower limb functional deficits (control group) and with lower limb functional deficits (experimental group). The Ethical Committee of the University of the State of Santa Catarina approved this study (No. 96023618.0.0000.0118 and No. 87478418.5.0000.0118), and all participants signed an informed written consent form, as per the Declaration of Helsinki.
Lower limb functional deficit status was based on the Lower Extremity Functional Scale (LEFS, Portuguese version) [31]. The LEFS is an 80-point scale, with 0 indicating the worst functional capacity and 80 the best. Individuals presenting values ≥ 75 points in LEFS were considered free from lower limb functional deficits, based on previous data [32]. Those presenting scores ≤ 72 points (75 minus the SEM of LEFS of 2.4 points) [33] were classified as with functional deficits.
Inclusion criteria for the control group were as follows: (I) age ≥ 18 years, (II) do not present any pain in the lower limbs that has prevented the performance of physical and daily life activities in the last six months, (III) involved in physical training at least three times per week, (IV) no history of surgery on the lower limbs and/or spine in the last two years, and (V) LEFS score ≥ 75 points. Inclusion criteria for the experimental group were as follows: (I) age ≥ 18 years, (II) sought medical or physical therapy services due to complaints related to the knee(s) and/or hip(s), and (III) LEFS ≤ 72 points. This approach of separating groups based on the LEFS score was chosen to reflect overall functionality so that we could identify variables associated with functional deficit regardless of the specific joint affected.
In both groups, participants who reported cardiovascular, pulmonary, neurological, and/or systemic diseases that could limit the performance of the assessments were excluded. The groups were paired by age, sex, body mass index, and dominance.
Based on data from a previous study (Cohen’s d effect size of 0.85 for knee FPPA difference between individuals with and without patellofemoral pain) [20], we calculated the sample size for the comparison between groups (discriminative validity) considering an alpha value of 0.05, where 23 participants per group were required to reach an estimated power of 80%. In studies estimating random error, a sample of 25 or more participants would be required [34]. Therefore, our sample size was sufficient for the proposed objectives.
2.2. Measures
Age, sex, lateral dominance, physical activity level, history of pain and injuries in the lower limbs, body mass, height, and LEFS score for the control group individuals were registered using an anamnesis form. For the experimental group, characterization data were extracted from medical and physiotherapeutic records from the private service where participants were assessed as part of their diagnosis/treatment routine.
The 2D kinematics during SLS and SLL was assessed by using a digital camera attached to a tripod and positioned perpendicular to the frontal plane at a sufficient distance to frame the participant in the image. During the study, due to resource availability, two different cameras were used: Casio EX-FH20 (Shibuya, Tokyo, Japan, sampling at 30 Hz for SLS and 210 Hz for SLL analyses) to evaluate the control group and part of the experimental group, and an Apple iPhone 11 smartphone camera (Cupertino, California, USA, sampling at 30 Hz for SLS and 240 Hz for SLL analyses) to evaluate the other part of the experimental group.
2.3. Design and Procedures
This was a measurement property study. We followed the reporting guidelines from the consensus-based standards for the selection of health measurement instruments (COSMIN) [13]. This article is a revised and expanded version of a paper entitled “Repetibilidade e capacidade discriminativa da análise cinemática bidimensional durante o agachamento e aterrissagem unilaterais em indivíduos com e sem disfunção nos membros inferiores”, which was presented at XX Brazilian Congress of Biomechanics, which took place between 18 and 22 April 2023 in the city of Bauru/SP, Brazil [35].
Data collection of participants in the control group was carried out at the University of the State of Santa Catarina. The experimental group consisted of patients attending the Instituto FisioLab physiotherapy clinic (Florianópolis, SC, Brazil), where kinematic evaluations were performed as part of the care routine. The data collection protocol was identical for both groups, as described below.
After anamnesis and anthropometrical measurements, markers were placed at the xiphoid process, jugular notch, and bilaterally at the anterior superior iliac spines, 15 cm projection below the anterior superior iliac spines, middle thigh (2.5 cm above the superior border of the patella), tibial tuberosity, and central and anterior point between the malleoli from the ankle. The markers were approximately 2 cm2, with the exception of the 15 cm projection below the anterior superior iliac spines, and the positions were found by palpating the anatomical structures and measuring the distances. After this, participants were then asked to perform a double-leg squat exercise, up to 60° of knee flexion controlled by a goniometer. In this position, the distance from the floor to the gluteal fold was measured and used to limit the RoM using a tactile device.
Next, participants’ kinematics was assessed during SLS and SLL tests, in that order. Before each test, the participants underwent a period of familiarization with the gesture. For the SLS, participants stood on the support limb with their hands on their waist and held the non-stance limb beside the stance limb so that the knee was flexed at approximately 90°. The participant should flex the knee of the support leg until touching the tactile device with the buttock, at a cadence of 45 beats per minute. For the SLL, participants stood on the support limb on the top of a 30 cm-high base with hands on the waist. The participant should unbalance themself forward and land on the ground with the same leg as in the initial position, ensuring that the contralateral leg does not contact the surface. After landing, the participant should regain balance by maintaining an upright single-legged posture. Three valid repetitions of the SLS and one of the SLL without losing balance and touching the floor with the contralateral leg were performed for each lower limb, starting with the right one.
Thirty participants of the control group returned for a second visit, in which the procedures were repeated. The time between visits ranged from 3 to 13 days. We consider this time interval was large enough to minimize the learning effects of the test and small enough to minimize changes in the movement pattern due to training adaptations, routines, or injuries, as previously used [14,16,23].
2.4. Data Analysis
SLS and SLL videos of all participants were imported into Kinovea software (version 0.8.27, Kinovea open-source project, Bordeaux, France) for virtual reconstruction of body segments and calculation of joint angles. The FPPA of the trunk (angle between the trunk segment and a vertical line), pelvis (angle between the pelvis segment and a horizontal line), hip (angle between the thigh and pelvis segments subtracted from 90°), and knee (angle between leg and thigh segments subtracted from 180°) was calculated. Positive values indicate ipsilateral trunk lean (trunk inclination), contralateral pelvic drop (pelvis drop), hip adduction, and knee abduction. Figure 1 shows the markers, body segments, and joint angles analyzed.
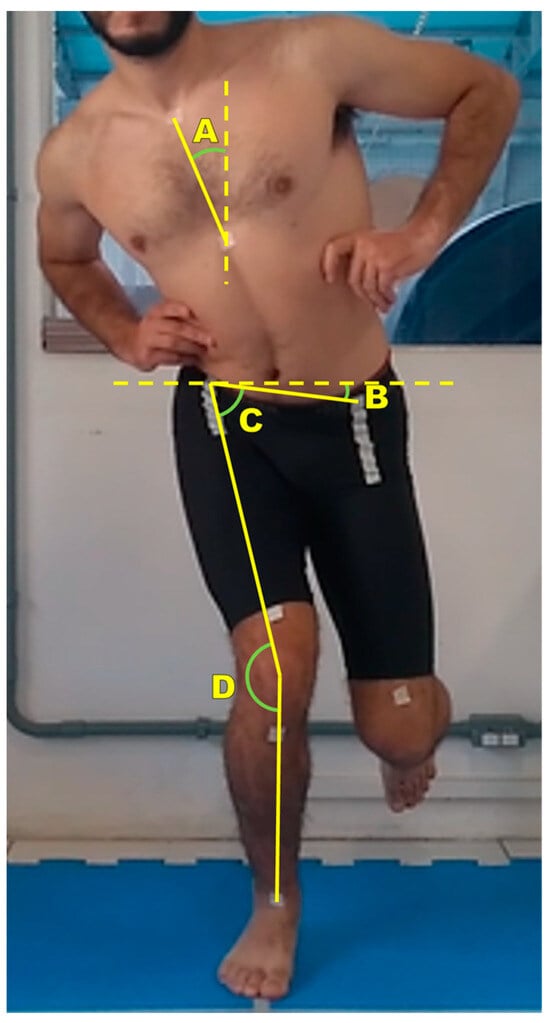
Figure 1.
Markers, body segments, and joint angles analyzed. A: trunk angle; B: pelvis angle; C: hip angle; D: knee angle.
For each joint, the angles at the deepest instant of movement and RoM were extracted. RoM was calculated as the difference between the joint angles at the deepest and initial (standing) instants. The deepest instant was defined as the instant in which the marker of the anterior superior iliac spine reached the lowest position. The initial instant was defined as (i) the instant in which the participant was standing still with the hip and knee in their maximum extension, immediately before the first descending movement of the marker of the anterior superior iliac spine, for the SLS, and as (ii) the instant of initial contact with the ground for the SLL.
The values of the affected lower limb of the experimental group and the paired lower limb of the control group according to lateral dominance were used in the analyses. In cases of bilateral dysfunction, the lower limb to be analyzed was randomly selected. For the SLS, the average of the three repetitions performed was used.
The analyses described above were performed by one rater for the entire sample. A second independent rater performed the same analyses on 30 individuals from each group to verify inter-rater reliability. The first rater re-analyzed these 30 individuals per group 1 week later to check for intra-rater reliability. In addition, he analyzed the data from the 2 visits of the 30 individuals in the control group to verify the test–retest reliability.
2.5. Statistical Analysis
The Shapiro–Wilk and Levene tests were performed to verify whether the data had normal distribution and homogeneity of variances, respectively. Comparison between groups was performed using the independent T test or the Mann–Whitney U test depending on whether the data were normally distributed. To avoid an increase in the type I error rate due to multiple comparisons, we applied the Bonferroni correction to the p-value. Since we performed 16 comparisons (0.05/16 = 0.003125), a p-value < 0.0031 was considered significant. For each significant difference, the effect size (ES) r was calculated (r less than 0.1 was poor, between 0.1 and 0.3 was small, between 0.3 and 0.5 was medium, and greater than or equal to 0.5 was large). ES r was calculated using Equation (1) for the T test and Equation (2) for the U test. Thus, the test (SLS or SLL) that best discriminated the groups was defined based on the number of differences found, and the variables that best discriminated were defined based on the effect sizes and magnitude of the SEMs:
To verify the inter-rater, intra-rater, and test–retest reliability, the intraclass correlation coefficient (ICC) estimates were calculated based on single measures, absolute agreement, and a 2-way mixed model. An ICC of less than 0.5 was considered low, between 0.5 and 0.75 was moderate, between 0.75 and 0.9 was good, and greater than 0.9 was excellent. For each ICC, the SEM was calculated using Equation (3), and the minimal detectable difference (MDD) using Equation (4):
All statistical tests were performed using the Statistical Package for Social Sciences software (version 20.0, IBM, Armonk, NY, USA; p < 0.05, except for discriminative comparisons), except for ES r calculations, which were performed using Microsoft Excel software (version 2212, Microsoft, Redmond, WA, USA).
3. Results
Participants’ characteristics are described on Table 1. Groups were similar with regards to age, body mass index, and the proportion of men and women (p > 0.05). In the experimental group, of the 13 participants who had bilateral dysfunction, 7 were on both hips and 6 on both knees. Also, among participants who underwent at least one surgery in the last 2 years, there was a mean (SD) of 183 (56) days between the last surgery and the kinematic evaluation.

Table 1.
Characterization of participants without (control) and with lower limb functional deficits a.
For the SLS, no significant differences between groups were found (Figure 2). For SLL, the experimental group had greater ipsilateral trunk leaning (Δ° = 4°; U = 423.500; p < 0.001; ES = medium), greater ipsilateral trunk leaning RoM (Δ° = 3°; U = 573.000; p = 0.002; ES = medium), greater contralateral pelvic drop RoM (Δ° = 4°; t [84] = −4.555; p < 0.001; ES = medium), less hip adduction (Δ° = 5°; t [84] = 4.100; p < 0.001; ES = medium), less knee abduction (Δ° = 7°; t [84] = 3.443; p = 0.001; ES = medium), and less knee abduction RoM (Δ° = 5°; t [84] = 3.077; p = 0.003; ES = medium) when compared to the control group (Figure 2).
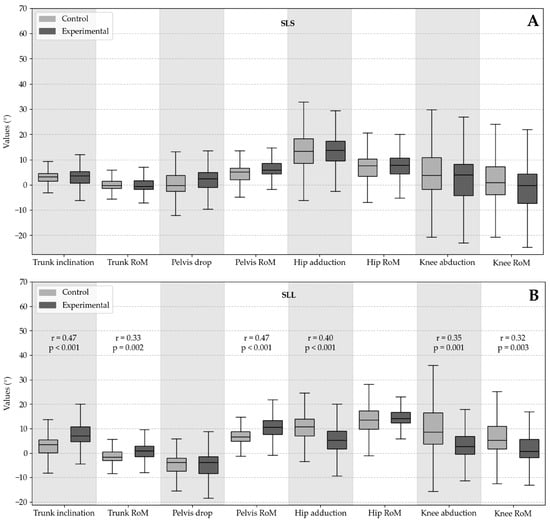
Figure 2.
Boxplot of two-dimensional kinematic variables of functional tests between individuals with and without lower limb functional deficits: (A) single-leg squat boxplot and (B) single-leg landing boxplot.
The ICC, SEM, and MDD values of the 2D kinematic variables of the SLS and SLL are presented in Table 2, Table 3 and Table 4, for test–retest, inter-rater, and intra-rater reliability, respectively. Based on the ICC values, the test–retest reliability varied across variables and tests (Table 2), with the errors attributed to the rater being typically a small fraction of the SEM contained in the assessment (Table 3 and Table 4). As expected, inter-rater errors were generally greater than intra-rater errors.

Table 2.
Test–retest reliability a.

Table 3.
Inter-rater reliability a.

Table 4.
Intra-rater reliability a.
4. Discussion
The objective of this study was to evaluate the discriminative validity and reliability of 2D kinematic variables during SLS and SLL in individuals with and without lower limb functional deficits. Our findings indicated that the SLL can better discriminate individuals with and without lower limb functional deficits when compared to the SLS. Additionally, differences in pelvis RoM and trunk inclination between groups during SLL showed the largest effect sizes (r = 0.47). However, even with moderate test–retest reliability (ICC = 0.51), pelvis RoM during SLL was the only variable whose difference between groups was greater than the test–retest SEM.
Differences between groups were observed for all four joints analyzed (angle at the deepest instant of movement of the trunk, hip, and knee and RoM of the trunk, pelvis, and knee) in SLL, and none in SLS. The best discriminative validity of the SLL may be related to the task demand. During SLS, the individual needs to deal with loads corresponding to the body weight in a slow and controlled manner, while when landing with a single leg from a height of 30 cm, the peak ground reaction force can reach seven times the body weight [36]. Thus, movement strategies are needed to balance and dissipate the impact, which could make evident motor control deficits reflected in the kinematics of individuals with functional deficits in the lower limbs. As far as we know, the only study that compared the kinematics of the SLS and SLL between subgroups of individuals with complaints related to the lower limbs showed that there was a group and test effect on the kinematics, but without interaction [9]. However, the author analyzed only the knee FPPA [9]. In our results, pairwise comparisons for each test demonstrated that this variable was different between groups for SLL and not for SLS.
The knee angle in the frontal plane during SLS has been extensively investigated. Several studies have shown that the knee abduction angle during SLS is greater in individuals with patellofemoral pain [7,9,11,20,21,30] and in individuals who underwent hip arthroscopy [22]. Such differences may not have been found in our study due to the investigated populations. Unlike the aforementioned studies, we did not investigate individuals with patellofemoral pain, but individuals with functional deficits based on a functional capacity scale related to the lower limbs. Additionally, even though there were individuals who underwent hip arthroscopy in the sample, they did not represent the majority of the group. On the other hand, athletes with anterior cruciate ligament injury adopted more rigid movement strategies in single-legged functional tests, with less knee movement in the sagittal plane [37] and frontal plane [27,38,39]. This may partially explain our findings, as our experimental group comprised 67% of individuals with knee dysfunction, of which 45% underwent reconstruction of the anterior cruciate ligament. In addition to the population studied, the difference between our results and those of previous studies may be related to the movement cadence. We established the SLS cadence at 45 beats per minute, and other studies performed slower cadences, between 24 and 40 beats per minute [7,9,11,20,21,22,30]. The speed of SLS may affect dynamic postural control [40], which may trigger effects on the kinematics of the lower limbs.
Test–retest reliability was low in 6 out of 16 variables and moderated in 10 out of 16 variables. This type of reliability was based on two kinematic assessments performed on different days and included variation originated from the analysis performed by the rater. As we had good intra-rater reliability, the low test–retest reliability was mainly due to variations in the performance of the test between days. Even respecting, in most cases, a seven-day interval between assessments to avoid a learning factor, it might have occurred. Other studies investigated the test–retest reliability of the FPPA of the trunk, pelvis, hip, or knee at the deepest instant of movement of the SLS or SLL and obtained ICC values between 0.74 and 0.95, with SEM varying between 1° and 4° [14,15,16,23]. In these studies, data variability (standard deviation) was similar to ours for the corresponding variables, but the ICC was higher and the SEM lower, especially those related to SLL [14,15,16,23].
Most of the inter-rater (21 out of 32 variables) and intra-rater (29 out of 32 variables) reliability was classified as good or excellent. Knee FPPA ICCs at the deepest instant of movement during SLS and SLL found in the literature ranged between 0.88 and 0.99 for inter-rater reliability [15,41,42] and between 0.80 and 0.93 for intra-rater reliability [41]. Data for other kinematic variables during SLS and SLL are still poorly reported.
We observed lower ICCs and higher SEMs for the SLL when compared to the SLS data. In similar studies, SLL data were based on the average of three attempts [15,23], while in the present study only one repetition was analyzed. The use of the average could bring greater stability to the measurements between days in case of high variability between repetitions performed on the same day. However, the use of only one repetition in clinical practice occurred to reduce the physical demand for individuals with pain complaints and the total evaluation time. In addition, there was a careful familiarization procedure to ensure that one repetition was able to represent the phenomenon of interest.
Data from the experimental group were from patients treated at a physiotherapy clinic, and all procedures performed are routinely part of clinical practice. Thus, it is expected that the results are easy to interpret and apply to professionals. In addition to the joint angles at the deepest instant of the SLS and SLL, the RoMs were analyzed. The RoM analysis, although not frequent in studies, represents a different phenomenon than the angle in a single instant and resulted in a variable with better discriminative validity. Finally, the analysis of two single-leg tests with different physical demands may facilitate the identification of kinematic variables that undergo increments in magnitude with the increase in task demand.
Our findings contribute to the selection of more appropriate tests and variables for assessing lower limb alignment in individuals with functional deficits. In clinical practice, the selection of tests and variables with good reliability and that detect compensatory movement patterns allows for more efficient assessments. Furthermore, the reliability, SEM, and MDD data presented in this study allow for more accurate monitoring of responses to therapeutic interventions. Our results also provide support for the selection of screening tools to be tested in future prospective studies on the predictive validity of these variables in identifying individuals at higher risk of developing lower limb dysfunctions.
Study Limitations
First, two different cameras were used for filming. The cameras had different resolutions and different framing distances. Therefore, it is possible that this affected the results. However, the use of different instruments can be a practical reality. It is noteworthy that in both cameras, the resolution was sufficient to identify the anatomical markers in the image and the frame rate was similar. Since these experimental conditions are similar, the impact of using the two cameras on the results was probably not relevant and did not affect the conclusion.
Second, the height of the platform for performing the SLL was not normalized by the height of the participant. Instead, we used a default height of 30 cm. Although this may represent a greater demand for individuals with smaller stature, the standard height of 30 cm is usually used in clinical practice and in other similar studies [1,9,15,26].
Third, we combined individuals with knee- and hip-related dysfunction into a single group. Even though the LEFS scores were similar in both cases, the nature of the dysfunction is different and could affect the results. We made this decision to form a general experimental group based on the LEFS score only.
Finally, we do not have test–retest reliability data for the experimental group. However, the natural history of the individual with dysfunction is to improve, even more so if they are undergoing treatment. In this case, kinematic differences that could be observed in a second data collection could come from the patient’s improvement and not from measurement errors. Furthermore, test–retest reliability values of 2D kinematic variables during SLS in individuals with patellofemoral pain [14] and healthy individuals [15] were similar. Also, we observed similar intra-rater reliability values between groups in our results. Therefore, possibly the test–retest reliability values for the experimental group would be similar to those of the control group.
5. Conclusions
Pelvis RoM in the frontal plane of SLL was able to discriminate controls and individuals with lower limb functional deficits, and the difference between groups was greater than the test–retest SEM. In SLL, the trunk and knee RoMs in the frontal plane and the angles of the trunk, hip, and knee at the deepest instant of landing were also able to discriminate the groups, with differences being greater than the inter-rater and intra-rater SEM and smaller than the test–retest SEM.
Such results support the hypothesis that, compared to SLS, the kinematic variables of SLL have a better ability to discriminate groups of individuals with lower limb functional deficits and controls. Prospective studies are warranted to investigate whether such kinematic parameters associated with lower limb functional deficits may also be risk factors for related complaints/injuries.
Most kinematic variables were classified as low to moderate test–retest reliability and good to excellent inter-rater and intra-rater reliability. Our results provide reliability, SEM, and MDD data for 2D kinematics in the frontal plane of the trunk, pelvis, hip, and knee in two unilateral functional tests with different physical demands. These data can help researchers and professionals to better analyze variations in kinematics between groups and over time.
Author Contributions
Conceptualization, J.M.M., M.P.d.C., A.d.S., F.X.d.A., H.d.B.F. and C.R.; methodology, J.M.M., M.P.d.C., A.d.S., F.X.d.A., H.d.B.F. and C.R.; validation, J.M.M.; formal analysis, J.M.M.; investigation, J.M.M., M.P.d.C., A.d.S. and C.A.A.P.; resources, M.P.d.C. and C.R.; data curation, J.M.M. and M.P.d.C.; writing—original draft preparation, J.M.M.; writing—review and editing, J.M.M., M.P.d.C., A.d.S., C.A.A.P., F.X.d.A., H.d.B.F. and C.R.; visualization, J.M.M.; supervision, M.P.d.C. and C.R.; project administration, C.R.; funding acquisition, J.M.M., A.d.S. and C.R. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Programa de Bolsas Universitárias de Santa Catarina (UNIEDU; grant numbers 16479 and 16925) and the Fundação de Amparo à Pesquisa e Inovação do Estado de Santa Catarina (FAPESC; grant numbers 2021TR1098 and 2023TR000336).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of the University of the State of Santa Catarina (protocol codes 96023618.0.0000.0118 and 87478418.5.0000.0118).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Abbreviations
The following abbreviations are used in this manuscript:
| ACL | Anterior cruciate ligament |
| BMI | Body mass index |
| CI | Confidence interval |
| COSMIN | Consensus-based standards for the selection of health measurement instruments |
| ES | Effect size |
| FPPA | Frontal plane projection angle |
| ICC | Intraclass correlation coefficient |
| LEFS | Lower Extremity Functional Scale |
| MCL | Medial collateral ligament |
| MDD | Minimal detectable difference |
| MPFL | Medial patellofemoral ligament |
| RoM | Range of motion |
| SD | Standard deviation |
| SEM | Standard error of measurement |
| SLL | Single-leg landing |
| SLS | Single-leg squat |
| TT | Tibial tuberosity |
References
- Poston, G.R.; Schmitt, L.C.; Ithurburn, M.P.; Hugentobler, J.A.; Thomas, S.; Paterno, M. V Reduced 2-d Frontal Plane Motion during Single-Limb Landing Is Associated with Risk of Future Anterior Cruciate Ligament Graft Rupture after Anterior Cruciate Ligament Reconstruction and Return to Sport: A Pilot Study. J. Orthop. Sports Phys. Ther. 2021, 51, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Harris-Hayes, M.; Hillen, T.J.; Commean, P.K.; Harris, M.D.; Mueller, M.J.; Clohisy, J.C.; Salsich, G.B. Hip Kinematics during Single-Leg Tasks in People with and without Hip-Related Groin Pain and the Association among Kinematics, Hip Muscle Strength, and Bony Morphology. J. Orthop. Sports Phys. Ther. 2020, 50, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Wilczyński, B.; Zorena, K.; Ślęzak, D. Dynamic Knee Valgus in Single-Leg Movement Tasks. Potentially Modifiable Factors and Exercise Training Options. A Literature Review. Int. J. Environ. Res. Public Health 2020, 17, 8208. [Google Scholar] [CrossRef] [PubMed]
- Willson, J.D.; Davis, I.S. Lower Extremity Mechanics of Females with and without Patellofemoral Pain across Activities with Progressively Greater Task Demands. Clin. Biomech. 2008, 23, 203–211. [Google Scholar] [CrossRef]
- Bailey, R.W.; Richards, J.; Selfe, J. A Biomechanical Investigation of Selected Lumbopelvic Hip Tests: Implications for the Examination of Walking. J. Manip. Physiol. Ther. 2016, 39, 411–419. [Google Scholar] [CrossRef]
- Scholtes, S.A.; Salsich, G.B. Consistency of Dynamic Knee Valgus Kinematics and Pain across Functional Tasks in Females with Patellofemoral Pain: A Cross-Sectional Study. Int. J. Sports Phys. Ther. 2020, 15, 985–994. [Google Scholar] [CrossRef]
- Rees, D.; Younis, A.; MacRae, S. Is There a Correlation in Frontal Plane Knee Kinematics between Running and Performing a Single Leg Squat in Runners with Patellofemoral Pain Syndrome and Asymptomatic Runners? Clin. Biomech. 2019, 61, 227–232. [Google Scholar] [CrossRef]
- Jones, P.A.; Herrington, L.C.; Munro, A.G.; Graham-Smith, P. Is There a Relationship between Landing, Cutting, and Pivoting Tasks in Terms of the Characteristics of Dynamic Valgus? Am. J. Sports Med. 2014, 42, 2095–2102. [Google Scholar] [CrossRef]
- Herrington, L. Knee Valgus Angle during Single Leg Squat and Landing in Patellofemoral Pain Patients and Controls. Knee 2014, 21, 514–517. [Google Scholar] [CrossRef]
- Nakagawa, T.H.; dos Santos, A.F.; Lessi, G.C.; Petersen, R.S.; Silva, R.S. Y-Balance Test Asymmetry and Frontal Plane Knee Projection Angle During Single-Leg Squat as Predictors of Patellofemoral Pain in Male Military Recruits. Phys. Ther. Sport 2020, 44, 121–127. [Google Scholar] [CrossRef]
- Warner, M.B.; Wilson, D.A.; Herrington, L.; Dixon, S.; Power, C.; Jones, R.; Heller, M.O.; Carden, P.; Lewis, C.L. A Systematic Review of the Discriminating Biomechanical Parameters during the Single Leg Squat. Phys. Ther. Sport 2019, 36, 78–91. [Google Scholar] [CrossRef] [PubMed]
- Räisänen, A.M.; Pasanen, K.; Krosshaug, T.; Vasankari, T.; Kannus, P.; Heinonen, A.; Kujala, U.M.; Avela, J.; Perttunen, J.; Parkkari, J. Association between Frontal Plane Knee Control and Lower Extremity Injuries: A Prospective Study on Young Team Sport Athletes. BMJ Open Sport Exerc. Med. 2018, 4, e000311. [Google Scholar] [CrossRef] [PubMed]
- Gagnier, J.J.; Lai, J.; Mokkink, L.B.; Terwee, C.B. COSMIN Reporting Guideline for Studies on Measurement Properties of Patient-Reported Outcome Measures. Qual. Life Res. 2021, 30, 2197–2218. [Google Scholar] [CrossRef]
- Kingston, B.; Murray, A.; Norte, G.E.; Glaviano, N.R. Validity and Reliability of 2-Dimensional Trunk, Hip, and Knee Frontal Plane Kinematics during Single-Leg Squat, Drop Jump, and Single-Leg Hop in Females with Patellofemoral Pain. Phys. Ther. Sport 2020, 45, 181–187. [Google Scholar] [CrossRef]
- Herrington, L.; Alenezi, F.; Alzhrani, M.; Alrayani, H.; Jones, R. The Reliability and Criterion Validity of 2D Video Assessment of Single Leg Squat and Hop Landing. J. Electromyogr. Kinesiol. 2017, 34, 80–85. [Google Scholar] [CrossRef]
- Gwynne, C.R.; Curran, S.A. Quantifying Frontal Plane Knee Motion during Single Limb Squats: Reliability and Validity of 2-Dimensional Measures. Int. J. Sports Phys. Ther. 2014, 9, 898–906. [Google Scholar]
- Jamaludin, N.I.; Sahabuddin, F.N.A.; Rasudin, N.S.; Shaharudin, S. The Concurrent Validity and Reliability of Single Leg Squat Among Physically Active Females with and without Dynamic Knee Valgus. Int. J. Sports Phys. Ther. 2022, 17, 574–584. [Google Scholar] [CrossRef]
- Alrayani, H.; Herrington, L.; Liu, A.; Jones, R. Frontal Plane Projection Angle Predicts Patellofemoral Pain: Prospective Study in Male Military Cadets. Phys. Ther. Sport 2023, 59, 73–79. [Google Scholar] [CrossRef]
- Levinger, P.; Gilleard, W.; Coleman, C. Femoral Medial Deviation Angle during a One-Leg Squat Test in Individuals with Patellofemoral Pain Syndrome. Phys. Ther. Sport 2007, 8, 163–168. [Google Scholar] [CrossRef]
- Scholtes, S.A.; Salsich, G.B. A Dynamic Valgus Index That Combines Hip and Knee Angles: Assessment of Utility in Females with Patelofemoral Pain. Int. J. Sports Phys. Ther. 2017, 12, 333–340. [Google Scholar]
- Willson, J.D.; Davis, I.S. Utility of the Frontal Plane Projection Angle in Females with Patellofemoral Pain. J. Orthop. Sports Phys. Ther. 2008, 38, 606–615. [Google Scholar] [CrossRef] [PubMed]
- Charlton, P.C.; Bryant, A.L.; Kemp, J.L.; Clark, R.A.; Crossley, K.M.; Collins, N.J. Single-Leg Squat Performance Is Impaired 1 to 2 Years After Hip Arthroscopy. PM&R 2016, 8, 321–330. [Google Scholar] [CrossRef]
- Werner, D.M.; Stasi, S.; Lewis, C.L.; Barrios, J.A. Test-Retest Reliability and Minimum Detectable Change for Various Frontal Plane Projection Angles during Dynamic Tasks. Phys. Ther. Sport 2019, 40, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Munro, A.; Herrington, L.; Carolan, M. Reliability of 2-Dimensional Video Assessment of Frontal-Plane Dynamic Knee Valgus during Common Athletic Screening Tasks. J. Sport Rehabil. 2012, 21, 7–11. [Google Scholar] [CrossRef]
- DiCesare, C.A.; Bates, N.A.; Myer, G.D.; Hewett, T.E. The Validity of 2-Dimensional Measurement of Trunk Angle during Dynamic Tasks. Int. J. Sports Phys. Ther. 2014, 9, 420–427. [Google Scholar]
- Donohue, M.R.; Ellis, S.M.; Heinbaugh, E.M.; Stephenson, M.L.; Zhu, Q.; Dai, B. Differences and Correlations in Knee and Hip Mechanics during Single-Leg Landing, Single-Leg Squat, Double-Leg Landing, and Double-Leg Squat Tasks. Res. Sports Med. 2015, 23, 394–411. [Google Scholar] [CrossRef]
- Yamazaki, J.; Muneta, T.; Ju, Y.J.; Sekiya, I. Differences in Kinematics of Single Leg Squatting between Anterior Cruciate Ligament-Injured Patients and Healthy Controls. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 56–63. [Google Scholar] [CrossRef]
- Dingenen, B.; Malfait, B.; Vanrenterghem, J.; Verschueren, S.M.P.; Staes, F.F. The Reliability and Validity of the Measurement of Lateral Trunk Motion in Two-Dimensional Video Analysis during Unipodal Functional Screening Tests in Elite Female Athletes. Phys. Ther. Sport 2014, 15, 117–123. [Google Scholar] [CrossRef]
- Furlan, L.; Sterr, A. The Applicability of Standard Error of Measurement and Minimal Detectable Change to Motor Learning Research—A Behavioral Study. Front. Hum. Neurosci. 2018, 12, 95. [Google Scholar] [CrossRef]
- Nakagawa, T.H.; Moriya, E.T.U.; MacIel, C.D.; Serrão, F. V Trunk, Pelvis, Hip, and Knee Kinematics, Hip Strength, and Gluteal Muscle Activation during a Single-Leg Squat in Males and Females with and without Patellofemoral Pain Syndrome. J. Orthop. Sports Phys. Ther. 2012, 42, 491–501. [Google Scholar] [CrossRef]
- Pereira, L.M.; Dias, J.M.; Mazuquin, B.F.; Castanhas, L.G.; Menacho, M.O.; Cardoso, J.R. Translation, Cross-Cultural Adaptation and Analysis of the Psychometric Properties of the Lower Extremity Functional Scale (LEFS): LEFS- BRAZIL. Braz. J. Phys. Ther. 2013, 17, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Dingemans, S.A.; Kleipool, S.C.; Mulders, M.A.M.; Winkelhagen, J.; Schep, N.W.L.; Goslings, J.C.; Schepers, T. Normative Data for the Lower Extremity Functional Scale (LEFS). Acta Orthop. 2017, 88, 422–426. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.P.; Fulton, A.; Quach, C.; Thistle, M.; Toledo, C.; Evans, N.A. Measurement Properties of the Lower Extremity Functional Scale: A Systematic Review. J. Orthop. Sports Phys. Ther. 2016, 46, 200–216. [Google Scholar] [CrossRef]
- Springate, S.D. The Effect of Sample Size and Bias on the Reliability of Estimates of Error: A Comparative Study of Dahlberg’s Formula. Eur. J. Orthod. 2012, 34, 158–163. [Google Scholar] [CrossRef]
- Machado, J.M.; de Souza, A.; Castro, M.P.d.; Pierri, C.A.A.; Ruschel, C. Repetibilidade e Capacidade Discriminativa Da Análise Cinemática Bidimensional Durante o Agachamento e Aterrissagem Unilaterais Em Indivíduos Com e Sem Disfunção Nos Membros Inferiores. In Proceedings of the XX Brazilian Congress of Biomechanics, Bauru, SP, Brazil, 18–22 April 2023; p. 42. [Google Scholar]
- Sakurai, A.; Harato, K.; Morishige, Y.; Kobayashi, S.; Niki, Y.; Nagura, T. Effects of Toe Direction on Biomechanics of Trunk, Pelvis, and Lower-Extremity during Single-Leg Drop Landing. J. Sport Rehabil. 2020, 29, 1069–1074. [Google Scholar] [CrossRef]
- Johnston, P.T.; McClelland, J.A.; Webster, K.E. Lower Limb Biomechanics During Single-Leg Landings Following Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. Sports Med. 2018, 48, 2103–2126. [Google Scholar] [CrossRef]
- Agostinone, P.; Di Paolo, S.; Grassi, A.; Pinelli, E.; Bontempi, M.; Bragonzoni, L.; Zaffagnini, S. ACL Deficiency Influences Medio-Lateral Tibial Alignment and Knee Varus–Valgus during in Vivo Activities. Knee Surg. Sports Traumatol. Arthrosc. 2020, 29, 389–397. [Google Scholar] [CrossRef]
- Markström, J.L.; Tengman, E.; Häger, C.K. ACL-Reconstructed and ACL-Deficient Individuals Show Differentiated Trunk, Hip, and Knee Kinematics during Vertical Hops More than 20 Years Post-Injury. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 358–367. [Google Scholar] [CrossRef]
- Talarico, M.K.; Lynall, R.C.; Mauntel, T.C.; Wasserman, E.B.; Padua, D.A.; Mihalik, J.P. Effect of Single-Leg Squat Speed and Depth on Dynamic Postural Control Under Single-Task and Dual-Task Paradigms. J. Appl. Biomech. 2019, 35, 272–279. [Google Scholar] [CrossRef]
- Lopes, T.J.A.; Ferrari, D.; Ioannidis, J.; Simic, M.; Azevedo, F.M.; Pappas, E. Reliability and Validity of Frontal Plane Kinematics of the Trunk and Lower Extremity Measured with 2-Dimensional Cameras during Athletic Tasks: A Systematic Review with Meta-Analysis. J. Orthop. Sports Phys. Ther. 2018, 48, 812–822. [Google Scholar] [CrossRef]
- Lu, Z.; Nazari, G.; MacDermid, J.C.; Modarresi, S.; Killip, S. Measurement Properties of a 2-Dimensional Movement Analysis System: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2020, 101, 1603–1627. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).