Abstract
This systematic review explores the role of family cohesion and health literacy in shaping the physical, mental, and behavioral health of parents and adolescents. Family cohesion and health literacy are recognized social determinants that influence communication, shared decision-making, and engagement in preventive health behaviors. Following PRISMA 2021 guidelines, a comprehensive search across major databases identified 16 eligible studies meeting the inclusion criteria between 2010 and 2025. The findings indicate that higher levels of family cohesion promote healthier behaviors, strengthen emotional regulation, and enhance adolescents’ perceived well-being, while also increasing parental involvement in health-related decisions. Health literacy emerged as a key explanatory and contextual factor in the association between family cohesion and health outcomes. However, socioeconomic disadvantages—such as low income, limited access to healthcare, and lower parental education—were shown to weaken these protective pathways, creating disparities in health outcomes. Cultural and contextual factors also influenced the effectiveness of health literacy interventions. Overall, the review underscores the relevance of family-centered, culturally tailored public health strategies that simultaneously strengthen family cohesion and health literacy to support equitable health outcomes for parents and adolescents.
1. Introduction
Family cohesion and health literacy as social determinants of health seem to play a key role either jointly or separately in health outcomes, healthcare services utilization, and adherence to healthy practices [1]. Family cohesion, defined as levels of emotional connection and support within the family, is widely considered to have a modulating effect on stress and morbidity, particularly among adolescents [2]. Health literacy refers to the ability to access, understand, and use information for appropriate health self-management and decision-making; it also serves as a central determinant of health promotion and disease prevention [3]. Therefore, health literacy and family cohesion provide a framework that potentially influences the standards of healthy lifestyle activities.
Adolescence is widely regarded as a crucial period for the development of positive health behaviors that influence lifestyle choices into adulthood [4]. Family cohesion and parental health literacy have been increasingly recognized as significant determinants of adolescents’ health-related behavior. Health literacy (HL) appears to mediate the relationship between academic achievement and substance use [5,6]. On the other hand, family cohesion has been linked to adolescents’ self-perceived need for dental care [4,5].
The importance of family characteristics in promoting adolescents’ health highlights the need for family-centered, integrated public health approaches. Strong family relationships can act as a protective factor, reducing negative health effects associated with challenges such as parental unemployment, low income, and limited access to healthcare services, not only among youth but across all family members [7]. Simultaneously, low health literacy has been associated with poorer health outcomes, particularly in families experiencing financial hardship, emphasizing the need for effective health education strategies [6].
Despite the growing body of research linking these factors to health outcomes, a significant gap in studies focusing on the positive determinants of health and well-being for both parents and adolescents still remains [8]. Exploring how health literacy and family cohesion interact can provide valuable insights into protective mechanisms of family health.
From a theoretical perspective, the interrelationships among family cohesion, health literacy, and health outcomes can be understood through complementary conceptual frameworks. Family systems theory emphasizes that family-level characteristics—such as emotional bonding, communication, and shared decision-making—shape individual behaviors, coping strategies, and health-related practices. Within cohesive family environments, health-related information is more likely to be exchanged, discussed, and collectively interpreted, thereby influencing both parental and adolescent health behaviors.
In parallel, the social determinants of health framework conceptualizes health literacy as a form of social and cultural capital that affects individuals’ capacity to access, understand, and apply health information in daily life. Health literacy may therefore operate as a facilitating mechanism through which family cohesion supports healthier behaviors and well-being. Importantly, within the scope of this review, these relationships are conceptualized as interrelated mechanisms rather than empirically tested causal pathways.
This conceptual framing informed the synthesis of the reviewed evidence and guided the interpretation of how family cohesion and health literacy are jointly associated with health outcomes across diverse contexts.
Additionally, more research is needed to examine the long-term effects of family cohesion and health literacy on adolescent health outcomes, particularly in non-Western and low-income populations. Also, with increasing reliance on digital health resources, studies should explore how family dynamics influence digital health literacy adoption [9]. Furthermore, future research should examine how different family structures (e.g., blended families, single-parent households) impact health literacy and adolescent health outcomes [10].
From a conceptual standpoint, the relationships among family cohesion, health literacy, and health outcomes are understood as interrelated mechanisms operating within the family context rather than as empirically tested causal pathways. Although health literacy is frequently discussed in the literature as a potential mediator or moderator, the present review does not aim to establish causal mediation or moderation effects. Instead, these terms are used descriptively to reflect how health literacy is proposed to help explain or strengthen associations between family cohesion and health outcomes across different contexts.
Considering the aforementioned, the aim of this systematic review was to synthesize evidence on the role of health literacy and family cohesion and their potential influence on the health of adolescents and their parents. Specifically, this review seeks to address the following research questions:
- How does family cohesion influence the health and well-being of parents and adolescents?
- What role does health literacy play in mediating (explaining the process) or moderating (influencing the strength) the relationship between family cohesion and adolescent health outcomes?
- Are there any differences in the impact of these factors across socioeconomic, cultural, or demographic contexts?
By integrating findings across diverse contexts, this review aims to identify the mechanisms through which family cohesion and health literacy jointly shape adolescents’ health behaviors and outcomes.
2. Materials and Methods
This systematic review was conducted using the PRISMA [11] guidelines to ensure a structured and transparent process for investigating the relationship between health literacy, family cohesion, and health outcomes among parents and adolescents [11]. The review protocol was prospectively registered with the International Prospective Register of Systematic Reviews (PROSPERO; registration number CRD420251267393).
2.1. Inclusion and Exclusion Criteria
The predefined inclusion and exclusion criteria were applied during screening. The criteria are presented in Table 1.

Table 1.
Eligibility criteria for study selection.
In this review, references to “mediating” and “moderating” roles are conceptual rather than statistical. Given that most included studies employed cross-sectional designs, the synthesis does not infer causality but focuses on summarizing how health literacy is discussed in the literature as a potential explanatory or reinforcing factor in the association between family cohesion and health outcomes.
Qualitative and mixed-methods studies were included to enhance the conceptual and contextual understanding of how family cohesion and health literacy operate within family environments. These studies were not used to infer causal mediation or moderation effects but to elucidate family communication processes, shared decision-making practices, and contextual factors that help explain observed associations reported in quantitative research.
Moreover, the review adopted a family-centered public health perspective, allowing the synthesis of diverse health outcomes, including mental health, oral health, substance use, and preventive health behaviors. These health domains were considered collectively because they are influenced by shared family-level determinants, such as family cohesion, communication patterns, and health literacy, rather than being examined as isolated clinical conditions.
2.2. Literature Search
A comprehensive literature search was conducted across multiple databases to identify studies relevant to the research objectives. The databases searched included PubMed/MEDLINE, Embase, Cochrane Library, APA PsycInfo, and CINAHL. Additional searches were conducted in ClinicalTrials.gov, ANZCTR, and ICTRP.
2.3. Search Strategy
A compound search strategy was developed using a combination of controlled vocabulary (e.g., MeSH terms) and free-text keywords, adapted for each database. The core Boolean search string applied across databases was as follows: (“health literacy” OR “family health literacy” OR “oral health literacy” OR “mental health literacy”) AND (“family cohesion” OR “family functioning” OR “family connectedness” OR “family relationships”) AND (adolescent* OR youth OR “young people” OR parent* OR family) AND (“health outcomes” OR “mental health” OR “oral health” OR “substance use” OR “health behavior*”).
Search terms were modified as necessary to accommodate the indexing systems and syntax of each database. The search was limited to articles published in English and Greek between January 2010 and March 2025. Both languages were selected as they represent the primary languages of publication in this research field. No restrictions were placed on study design to ensure comprehensive coverage of the evidence. The review does not focus on a specific national context.
PubMed was prioritized due to its extensive coverage of peer-reviewed biomedical, public health, and epidemiological journals, which substantially overlap with public health-focused journals indexed in multidisciplinary databases such as Scopus and Web of Science.
Grey literature was excluded to maintain methodological rigor by focusing on peer-reviewed evidence.
2.4. Screening and Selection Process
The screening followed a two-phase process:
- Title and Abstract Screening: Duplicates were removed, and titles and abstracts were screened for relevance.
- Full-Text Review: Full articles were retrieved and assessed against the inclusion and exclusion criteria.
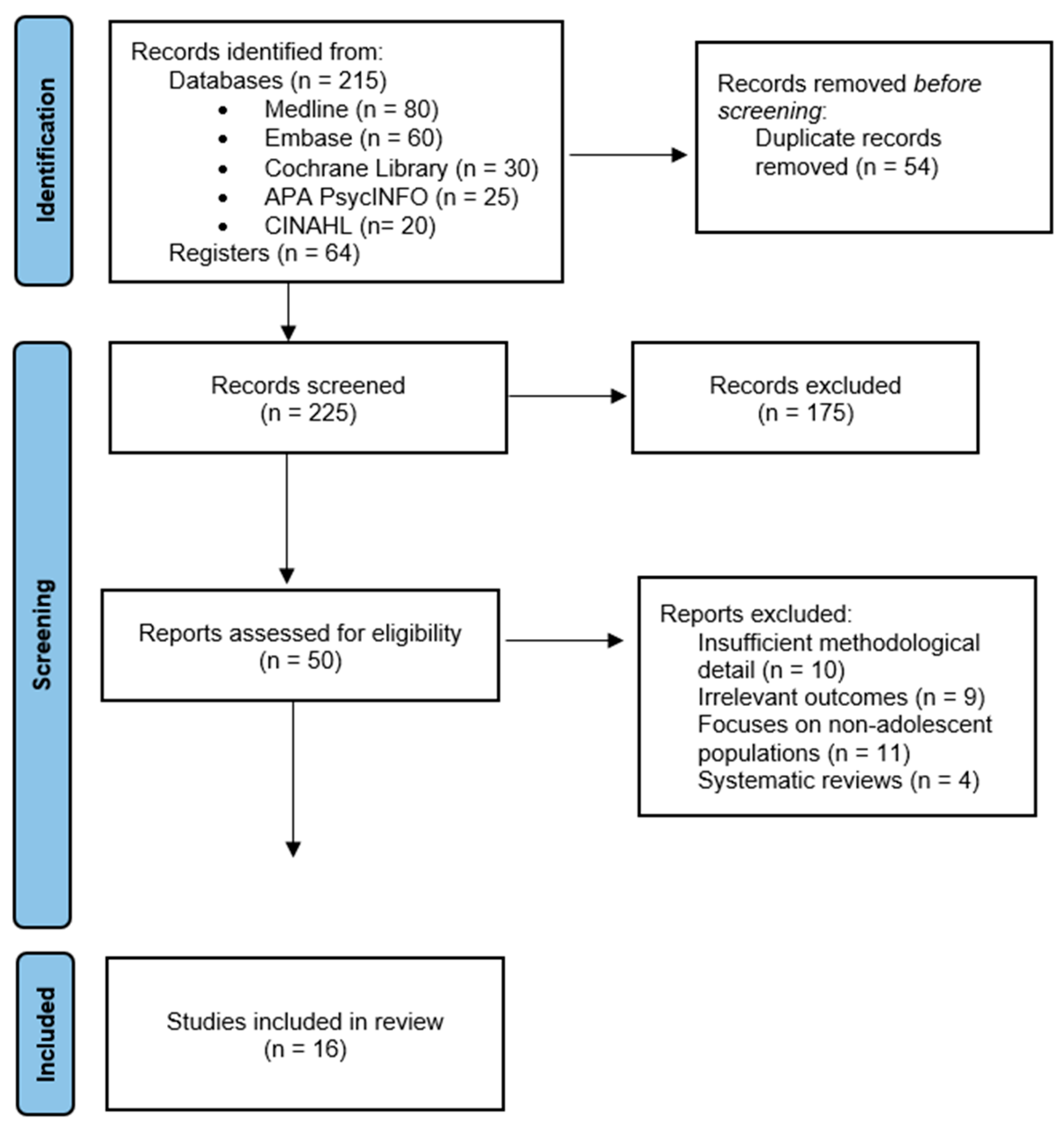
A total of 279 records were initially identified. After removing 54 duplicates, 225 titles and abstracts were screened, of which 175 were excluded. Fifty full-text articles were assessed for eligibility, and 34 were excluded due to methodological limitations or lack of relevance. Ultimately, 16 studies met the inclusion criteria and were incorporated into the review. The study selection process is illustrated in Figure 1.
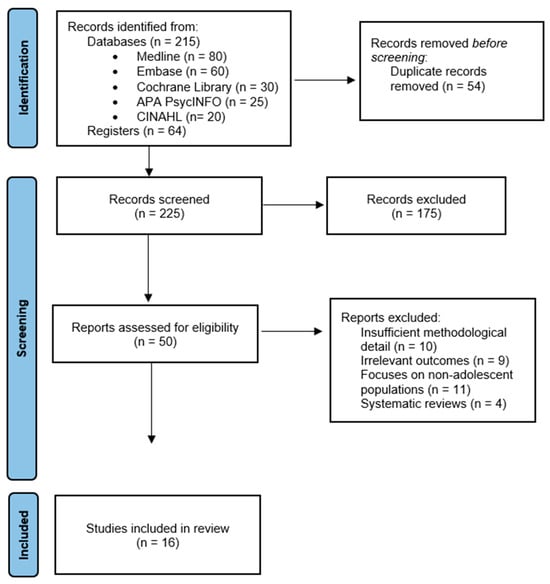
Figure 1.
Flow chart and article selection.
2.5. Study Quality and Methodological Considerations
A formal methodological quality appraisal using standardized checklists (e.g., Newcastle–Ottawa Scale or Joanna Briggs Institute tools) was not conducted. This decision was based on the heterogeneity of the included studies, which comprised cross-sectional, qualitative, and mixed-methods designs, making the application of a single appraisal instrument methodologically challenging.
To mitigate this limitation, studies with insufficient methodological detail, unclear outcome definitions, or unavailable full texts were excluded during the screening and full-text review process. The absence of a formal quality scoring procedure is acknowledged as a limitation of the present review.
3. Results
3.1. The Influence of Family Cohesion on the Health and Well-Being of Parents and Adolescents
Evidence consistently identifies family cohesion as an important predictor of the physical and psychological health of both parents and adolescents. Family connectedness facilitates effective communication that promotes health literacy and healthy practices. Moreover, families with high levels of cohesion engaged more frequently in health-related discussions; therefore, they make wiser decisions on their health and are healthier [12].
A study conducted by Feinberg et al. indicated that participants from highly cohesive families were more inclined to attribute improved health to effective communication, collaborative family decision-making, and shared familial responsibilities in health matters [13].
Self-perceived need for dental treatment was lower among adolescents with higher family cohesion, which implied that family cohesion may have a protective role against health neglect and poor oral hygiene behaviors [4]. Family cohesion is also associated with improved emotional regulation and stress coping mechanisms, where adolescents and parents in high-cohesive families showed more stable emotions and a better ability to cope with stressors [2] (Table 2).

Table 2.
Summary of Studies Examining the Influence of Family Cohesion on the Health and Well-Being of Parents and Adolescents.
3.2. The Role of Health Literacy in Explaining and Strengthening the Relationship Between Family Cohesion and Health Outcomes
The role of health literacy in explaining and shaping the relationship between family cohesion and health outcomes:
Family cohesion is understood with respect to health literacy to explain how it affects health. It is also indicated that better health literacy in integrated families results in lower substance use, better diets, and enhanced academic achievement [5].
Health literacy also influenced the strength of the relationship between family cohesion and health outcomes. Research suggested that in families with lower health literacy, the protective effects of family cohesion were weakened, leading to increased health disparities [6]. Specifically, studies have indicated that single-parent households and families with lower levels of health literacy face greater challenges in accessing health resources and making informed health decisions [14].
In addition, previous work has established that there is a positive relationship between parental health literacy and preventive healthcare behaviors, including better child oral hygiene [15] (Table 3). This finding would mean that health literacy enhances the relationship between family cohesiveness and health status, highlighting the potential relevance of family-oriented health education approaches.

Table 3.
Summary of Studies Investigating the Conceptual Mediating and Moderating Role of Health Literacy in the Relationship Between Family Cohesion and Adolescent Health Outcomes.
3.3. The Impact of Socioeconomic Status (SES), Cultural, and Demographic Factors on Family Cohesion and Health Literacy
The association between family cohesion and health literacy is affected by various socio-economic, cultural and demographic factors. The present review documented that low-income families are vulnerable to having poor health literacy as they do not have access to health care services and educational opportunities that will improve family health, in general.
Research showed that parental health literacy and socioeconomic status (SES) are linked to the frequency of preventive dental visits among teenagers. It was found that those with poor health literacy were also at a higher risk of dental caries, thus highlighting the link between SES and oral health [16]. Social determinants like financial hardships, food insecurity and housing instability were associated with poor health outcomes and early death. Poverty, or low socioeconomic status, was associated with numerous social issues, which increase the likelihood of experiencing adverse childhood experiences. Socioeconomic disparities, such as lack of transportation and insufficient health insurance, have been documented to negatively affect the ability to access comprehensive care. These factors impede patients from receiving effective and timely detection of adverse health conditions, particularly in cases of chronic diseases, which in turn increase both psychological stress and healthcare costs [19]. Parents from the working-class with limited access to health care facilities tend to delay their children’s preventive healthcare [17].
Other factors that are related to cultural values include the impact of health literacy interventions. The need to culturally appropriate health interventions, mainly for youth health literacy on substance use and mental health, is highlighted. Broad health promotion interventions may not address the specific needs of various populations, so culturally appropriate, community-based interventions should be considered [9,14].
Parental employment status and educational level affect family cohesiveness and health literacy, as well. It is observed that parental unemployment reduces the educational achievement of adolescents; however, this was not the case in strong family relationships [7]. Furthermore, community safety (i.e., food security and housing stability) and parental education levels significantly influence adolescent health behaviors [20].
3.4. Health Literacy and Family Cohesion in Specific Health Contexts
Certain health conditions and behaviors illustrate the direct impact of family cohesion and health literacy on adolescent and parental health outcomes.
The research revealed that children’s oral health improved as their parents’ oral health knowledge increased [18]. Adolescents who have more knowledge about oral cavities are more likely to take preventative measures and make informed decisions about their oral health [21].
Well-informed adolescents about mental health tend to experience enhanced psychological health due to school-based programs on mental health and stress management [22]. Another study examined family support systems among adolescents with chronic conditions, highlighting the role of family cohesion in improving healthcare transition readiness [23].
In addition, there are a few studies exploring the issue of family cohesion. Evidence from those suggest that social determinants of health impacted both family cohesion and health literacy, affecting health disparities across different population groups [3]. These interconnected factors create a ripple effect, where weakened family cohesion and poor health literacy—driven by unfavorable social determinants—limit access to care, hinder disease prevention, and worsen health outcomes. There is also evidence that family cohesion mediates the relationship between health literacy and mental health, reinforcing the need for family-tailored interventions to address psychological well-being and healthcare engagement [12] (Table 4).

Table 4.
Summary of Literature Addressing Differences in the Impact of Family Cohesion and Health Literacy Across Socioeconomic, Cultural, and Demographic Contexts.
Overall, the findings are presented by thematic patterns rather than individual study narratives to facilitate synthesis across diverse study designs and health outcomes.
4. Discussion
This systematic review synthesized evidence on how family cohesion and health literacy influence health outcomes among parents and adolescents.
The findings can be interpreted through complementary theoretical lenses. From a family systems perspective, family cohesion reflects relational processes that shape shared health behaviors and communication patterns. From a public health and social determinants perspective, health literacy functions as a contextual resource that facilitates or constrains families’ capacity to engage in health-promoting practices across multiple health domains.
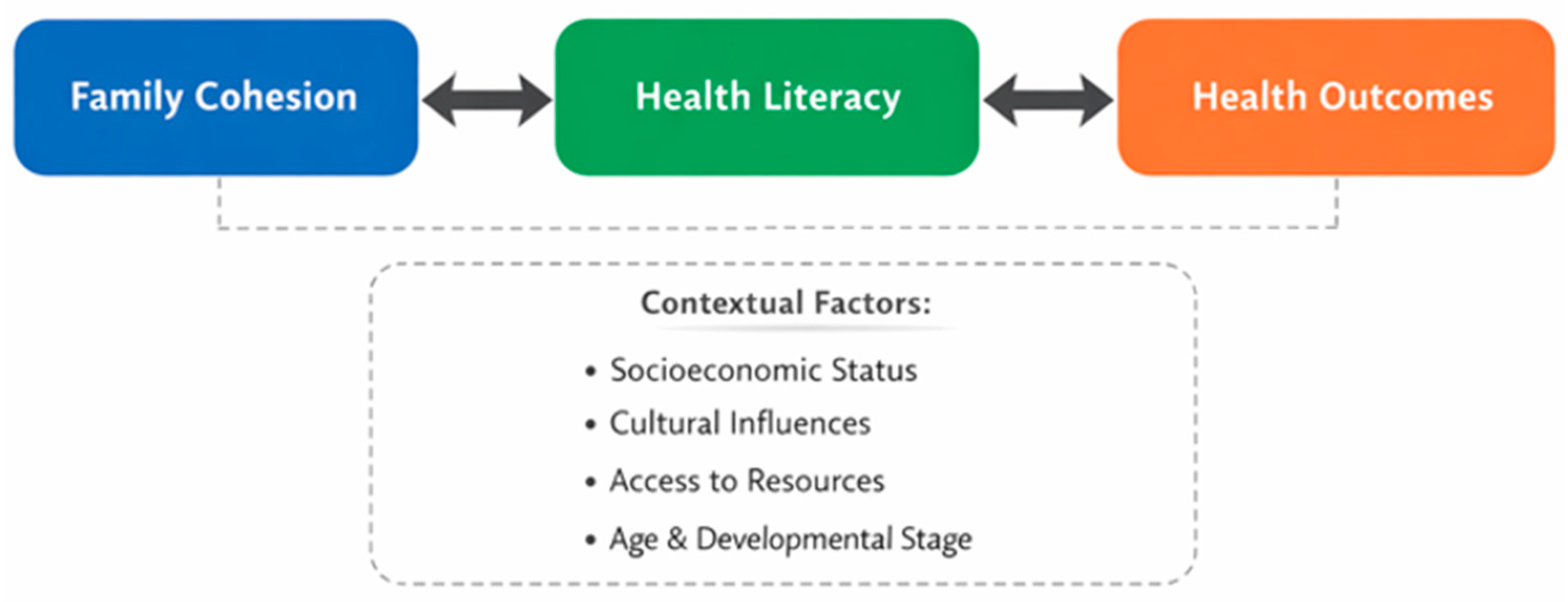
The conceptual relationships identified across the reviewed studies are summarized in Figure 2.
Figure 2.
Conceptual model of family cohesion, health literacy and health outcomes.
Rather than reflecting uniform effects, the reviewed evidence revealed both converging and diverging patterns across health domains and study designs. While most studies reported positive associations between family cohesion, health literacy, and health outcomes, the strength and consistency of these associations varied depending on contextual factors such as age group, cultural setting, and outcome type. These inconsistencies underscore the complexity of family-level health processes and highlight the need for more methodologically comparable and longitudinal research.
While health literacy is often described as mediating or moderating the association between family cohesion and health outcomes, the available evidence primarily reflects cross-sectional associations rather than formally tested causal models. As such, the review highlights conceptual pathways and converging patterns suggested in the literature rather than definitive mediation or moderation effects.
The findings are in line with previous studies highlighting the role of family cohesion in facilitating health-promoting behaviors and strengthening health literacy among adolescents and parents [5,12,13]. Across different settings, family cohesion was found to enhance health literacy by facilitating open communication, shared decision-making, and stronger social support networks [13]. For example, cohesion contributed positively to improving collaboration and participation in health discussions, which subsequently enhanced parental and adolescent literacy in health issues. Family roles, such as parenting and household duties, continue to impact health literacy and behaviors [1].
The present review highlighted the importance of family cohesion in promoting health literacy and positive health outcomes. This is consistent with previous studies indicating that family is the first form of socialization and care delivery to its members, directly influencing their health [10]. Furthermore, health literacy is considered an important form of social and cultural capital, as it improves individuals’ access to health information and their ability to use it effectively, thus contributing to improved health and quality of life [14]. Limited or low health literacy presents a significant barrier to healthcare access, increasing the risk of hospitalization [24].
Importantly, qualitative and mixed-methods studies contributed interpretative depth to the review by illustrating how family cohesion and health literacy are experienced, negotiated, and applied within everyday family life. These studies highlighted mechanisms such as trust, emotional support, and collective interpretation of health information, which help contextualize why stronger associations between family cohesion, health literacy, and health outcomes are observed in quantitative studies. However, these insights are conceptual and do not constitute evidence of statistically tested mediation or moderation.
The impact of family cohesion on reducing substance use and improving academic performance was stronger in families with higher health literacy levels. Conversely, in families with low health literacy, the protective effects of family cohesion were weaker, highlighting the need for interventions that address both family cohesion and health literacy simultaneously [5].
Socioeconomic and cultural factors were consistently found to shape the extent to which family cohesion and health literacy influence health behaviors. Specifically, factors such as income level, educational background, and cultural health beliefs can either enhance or limit the effectiveness of family cohesion and health literacy in promoting positive health outcomes.
Access to healthcare, education, and preventive services remained limited for low-income families, even when family support was strong. According to Lopes et al., low socioeconomic status families with high family cohesion still struggled to seek dental care services [6]. This means that in order to be most effective, health literacy interventions must also address financial issues.
The effectiveness of health education programs depends on the extent to which cultural values fit with the target population [9,14].
One of the main limitations of this review is that most included studies were cross-sectional, which restricts the ability to infer that family cohesion directly influences health literacy or subsequent health outcomes. Cross-sectional designs rely heavily on self-reported data, making them vulnerable to recall and reporting biases, and they cannot establish the temporal ordering of variables. Consequently, although consistent associations were observed, the findings should be interpreted as correlational rather than causal. Future research employing longitudinal or experimental designs is needed to clarify the directionality and underlying mechanisms linking family cohesion, health literacy, and health outcomes among adolescents. The limited number of longitudinal studies in this field may be attributed to the methodological complexity and resource demands of tracking family dynamics, health literacy, and adolescent health outcomes over time, as well as the predominance of cross-sectional designs within public health and school-based research.
5. Conclusions
The findings of this systematic review reinforce the critical role of family cohesion and health literacy in promoting positive health outcomes among parents and adolescents.
Socioeconomic disparities and cultural differences must be addressed during the design of any program implementation so as to be fully effective. This review serves as a foundation for future health promotion strategies, advocating for family-centered and equity-driven approaches to improve health literacy and well-being in diverse populations. However, the findings should be interpreted with caution, as the reviewed evidence is primarily cross-sectional and does not include longitudinal or intervention studies. Future longitudinal research is needed to examine how health education programs support families in improving their overall well-being over time. Consequently, recommendations for family-centred interventions and policy initiatives are proposed as directions for future research and practice rather than as conclusions supported by causal evidence.
Author Contributions
Conceptualization, A.L., V.N. and C.G.; methodology, A.L. and K.A.; validation, A.L., V.N. and K.A.; formal analysis, K.A.; investigation, K.A.; resources, A.L. and V.N.; data curation, K.A.; writing—original draft preparation, K.A.; writing—review and editing, C.G., A.L. and V.N.; visualization, K.A.; supervision, A.L. and V.N.; project administration. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| HL | Health Literacy |
| FC | Family Cohesion |
| WHO | World Health Organization |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| MeSH | Medical Subject Headings |
| SES | Socioeconomic Status |
| ADHD | Attention-Deficit/Hyperactivity Disorder |
References
- Kanellopoulou, A.; Notara, V.; Panagiotakos, D.B. The role of family structure in health literacy in children and adolescents: A narrative review. Glob. Health Promot. 2022, 29, 45–58. [Google Scholar] [CrossRef] [PubMed]
- van Eickels, R.L.; Tsarpalis-Fragkoulidis, A.; Zemp, M. Family cohesion, shame-proneness, expressive suppression, and adolescent mental health—A path model approach. Front. Psychol. 2022, 13, 921250. [Google Scholar] [CrossRef] [PubMed]
- Schillinger, D. The intersections between social determinants of health, health literacy, and health disparities. Stud. Health Technol. Inform. 2020, 269, 22–41. [Google Scholar] [CrossRef] [PubMed]
- Prata, I.M.L.F.; Granville-Garcia, A.F.; Neves, É.T.B.; Lima, L.C.M.; Dutra, L.C.; Perazzo, M.F.; Ferreira, F.M.; Paiva, S.M. Family cohesion is associated with the self-perceived need for dental treatment among adolescents. Biomed. Res. Int. 2021, 2021, 4504030. [Google Scholar] [CrossRef]
- Kinnunen, J.M.; Paakkari, L.; Rimpelä, A.H.; Kulmala, M.; Richter, M.; Kuipers, M.A.G.; Kunst, A.E.; Lindfors, P.L. The role of health literacy in the association between academic performance and substance use. Eur. J. Public Health 2022, 32, 182–187. [Google Scholar] [CrossRef]
- Lopes, R.T.; Neves, É.T.B.; Dutra, L.C.; Gomes, M.C.; Paiva, S.M.; Abreu, M.H.N.G.; Ferreira, F.M.; Granville-Garcia, A.F. Socioeconomic status and family functioning influence oral health literacy among adolescents. Rev. Saúde Pública 2020, 54, 30. [Google Scholar] [CrossRef]
- Askeland, K.G.; Radlick, R.L.; Bøe, T.; Hysing, M.; La Greca, A.M.; Nilsen, S.A. Parental unemployment and educational outcomes in late adolescence: The importance of family cohesion, parental education, and family income in a Norwegian study. Scand. J. Public Health 2024, 53, 52–61. [Google Scholar] [CrossRef]
- Lopes, R.T.; Neves, É.T.B.; Gomes, M.C.; Paiva, S.M.; Ferreira, F.M.; Granville-Garcia, A.F. Family structure, sociodemographic factors and type of dental service associated with oral health literacy in early adolescence. Cienc. Saude Colet. 2021, 26, 5241–5250. [Google Scholar] [CrossRef]
- Brooks, H.; Irmansyah, I.; Syarif, A.K.; Pedley, R.; Renwick, L.; Rahayu, A.P.; Manik, C.G.; Prawira, B.; Hann, M.; Brierley, H.; et al. Evaluating a prototype digital mental health literacy intervention for children and young people aged 11–15 in Java, Indonesia: A mixed-method, multi-site case study evaluation. Child Adolesc. Psychiatry Ment. Health 2023, 17, 79. [Google Scholar] [CrossRef]
- Ho, Y.C.L.; Mahirah, D.; Ho, C.Z.H.; Thumboo, J. The role of the family in health promotion: A scoping review of models and mechanisms. Health Promot. Int. 2022, 37, daac119. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n1. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Sun, X.; He, F.; Liu, C.; Wu, Y. The mediating effect of family health on the relationship between health literacy and mental health: A national cross-sectional survey in China. Int. J. Soc. Psychiatry 2023, 69, 1490–1500. [Google Scholar] [CrossRef] [PubMed]
- Feinberg, M.; Hotez, E.; Roy, K.; Ledford, C.J.W.; Lewin, A.B.; Perez-Brena, N.; Childress, S.; Berge, J.M. Family health development: A theoretical framework. Pediatrics 2022, 149, e2021053509I. [Google Scholar] [CrossRef] [PubMed]
- Howe, E.J.; Bishop, L.; Torraville, B.S.; Rowe, E.C.; Kinzel, E.; Donnan, J. Canadian cannabis education resources to support youth health literacy: A scoping review and environmental scan. Health Educ. J. 2023, 82, 766–778. [Google Scholar] [CrossRef]
- Mirella, R.T.F.; Barbosa, T.; Melo, M.; Paiva, S.M.; Ferreira, F.M.; Granville-Garcia, A.F. Attention-deficit disorder, family factors, and oral health literacy. Int. Dent. J. 2022, 72, 565–571. [Google Scholar] [CrossRef]
- Barbosa, T.; Chaves, L.; Gomes, M.C.; Paiva, S.M.; Ferreira, F.M.; Granville-Garcia, A.F. Oral health literacy, sociodemographic, family, and clinical predictors of dental visits among Brazilian early adolescents. Int. J. Paediatr. Dent. 2020, 31, 204–211. [Google Scholar] [CrossRef]
- Zhong, Y.; Patel, N.; Ferris, M.; Rak, E. Health literacy, nutrition knowledge, and health care transition readiness in youth with chronic kidney disease or hypertension: A cross-sectional study. J. Child Health Care 2019, 24, 246–259. [Google Scholar] [CrossRef]
- Neves, É.T.B.; Dutra, L.C.; Lima, L.C.M.; Perazzo, M.F.; Ferreira, F.M.; Paiva, S.M.; Granville-Garcia, A.F. Structuring of the effects of oral health literacy on dental caries in 12-year-old adolescents. Community Dent. Oral Epidemiol. 2022, 51, 864–871. [Google Scholar] [CrossRef]
- Webb, J. Social aspects of chronic transfusions: Addressing social determinants of health, health literacy, and quality of life. Hematology 2020, 2020, 175–183. [Google Scholar] [CrossRef]
- Gomes, M.C.; Granville-Garcia, A.F.; Neves, É.T.B.; Dutra, L.C.; Ferreira, F.M.; Paiva, S.M. Family and contextual factors associated with licit drug use in adolescence. Rev. Saude Publica 2021, 55, 95. [Google Scholar] [CrossRef]
- Dutra, L.D.C.; de Lima, L.C.M.; Neves, É.T.B.; Gomes, M.C.; de Araújo, L.J.S.; Forte, F.D.S.; Paiva, S.M.; Ferreira, F.M.; Granville-Garcia, A.F. Adolescents with worse levels of oral health literacy have more cavitated carious lesions. PLoS ONE 2019, 14, e0225176. [Google Scholar] [CrossRef]
- Bjørnsen, H.N.; Espnes, G.A.; Eilertsen, M.E.B.; Ringdal, R.; Moksnes, U.K. The relationship between positive mental health literacy and mental well-being among adolescents: Implications for school health services. J. Sch. Nurs. 2017, 35, 107–116. [Google Scholar] [CrossRef]
- Pruette, C.S.; Ranch, D.; Shih, W.V.; Ferris, M.D.G. Health care transition in adolescents and young adults with chronic kidney disease: Focus on the individual and family support systems. Adv. Chronic Kidney Dis. 2022, 29, 318–326. [Google Scholar] [CrossRef]
- Allen-Meares, P.; Lowry, B.; Estrella, M.L.; Mansuri, S. Health literacy barriers in the health care system: Barriers and opportunities for the profession. Health Soc. Work 2020, 45, 62–64. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.