Abstract
Many dietary supplements may contain harmful ingredients or compounds. One of them is caffeine, a stimulant that has been utilized globally for centuries, primarily for its ability to improve mental alertness. This report described a case involving a young woman who most likely intentionally took an energy booster containing pure caffeine. Gross and microscopic examination showed extensive necrotic changes with esophageal perforation in the upper gastrointestinal tract. Harmful contents have moved to the posterior mediastinum and the left pleural cavity, causing injuries within them. Postmortem toxicological tests (gas chromatography with the mass detector—GC-MS) have shown the presence of lethal levels of caffeine in the blood (92.0 ug/mL). The remaining toxicological tests were negative.
1. Introduction
Dietary supplements can benefit our health, but taking supplements, including energy boosters, can also involve health risks. The risks associated with taking nutritional supplements can be very diverse. One of the most common risks of taking supplements is using them with microbial contamination [1,2]. The other threat may be due to heavy metal contamination [3,4]. Some products may also contain unapproved pharmaceutical ingredients [5]. Some supplements contain substances in high concentrations, the ingestion of which can lead to severe complications or death [6]—one of the ingredients of slimming preparations might be caffeine. An overdose of caffeine alone, intentional or not, might be deadly [7]. Caffeine is absorbed from the gastrointestinal tract, reaching its maximum concentration in the blood 30–60 min after consumption, depending on individual conditions of the organism and the presence of food content in the stomach [8,9]. Caffeine is distributed by the blood to all tissues and does not accumulate in the body. The existence of similar caffeine concentrations in human blood and brain suggests that caffeine can readily cross the blood–brain barrier due to its hydrophobic nature. It is almost entirely metabolized by the liver in adults, including CYP1A2, a cytochrome P450 superfamily of enzymes. It represents 15% of all cytochrome P450 in the human liver and accounts for more than 90% of caffeine metabolism [10]. Only 1–5% of consumed caffeine is excreted unchanged in the urine in adults. The half-life of caffeine in adults ranges from 3 to 7 h [11]. Symptoms of caffeine intoxication may include headache, fever, nausea, vomiting, tachycardia, dizziness, tinnitus, anxiety, irritability, insomnia, and seizures [12,13,14]. Toxic levels of caffeine are associated with hypokalemia, hyperglycemia, rhabdomyolysis, renal failure, and hyperlacticaemia [15]. Heavy toxicity from caffeine exposure may also result from adrenaline and noradrenaline release, resulting in sympathetic nervous system overdrive and heart rhythm disturbances, including tachyarrhythmias or dysrhythmias [16]. As we know, the available literature does not describe massive injuries to the upper gastrointestinal tract following an overdose of caffeine.
2. Case Report
2.1. Case History
A 22-year-old female was found in her parents’ apartment, where they lived together. She had got no clinical history. The family account shows that the individual was closed, so family members could not comment on the deceased’s habits. The prosecutor’s investigation also did not reveal whether the deceased had taken energy booster or pure caffeine before. The body was found on the morning, lying on the bed. A sheet and a floor in the room bore traces of emesis in the colors of brown. There was a plastic bag on the night shelf next to it with the inscription “Myprotein 100-g caffeine” with a small amount of the substance. A forensic autopsy was performed approximately 24 h after her death.
2.2. Autopsy Findings
2.2.1. External Examination
The external examination showed a trace of dusty brown contents in the mouth. Besides, natural body openings were free. On the nose, the lips, near the mouth and the left cheek, and the palmar surface of the left metacarpal, parchment-like dried lesions were found, with a slightly increased cohesiveness—around the mouth forming a streak.
2.2.2. Internal Examination
Postmortem examination did not reveal any traumatic changes explaining the cause of death. The internal organs were congested, and the heart was not dilated, containing blood without clots (a common sign of acute death). The liver presented signs of steatosis. In addition, numerous pieces of evidence related to the effects of the toxic substance on the deceased were found: the lower section of the thoracic part of the esophagus, just above the hiatus, presented a perforation—1.4 cm in diameter, with smooth and softening edges (Figure 1); the wall of the esophagus surrounding the perforation is intensely softening and thinning; the esophageal mucosa was covered with dense, greasy, dark-brown content; the mucous membrane of the stomach’s cardiac part and the fundus of the stomach was smooth, thinned, pale gray, with a visible brown aggregation of tiny vessels (Figure 2); the parietal pleura in the left pleural cavity was softening and presented the pale grey coloring (Figure 3). Similar changes were visible on the posterior surface of the lower lobe of the left lung with single bubbles within the visceral pleura (Figure 4). Finally, the petechial within the tunica adventitia of the descending aorta were found.
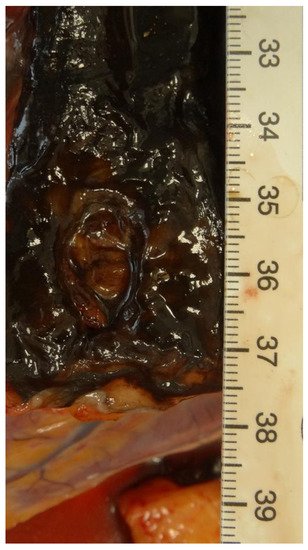
Figure 1.
Perforation of the lower section of the thoracic part of the esophagus.

Figure 2.
The mucous membrane of the stomach’s cardiac part and the fundus of the stomach.
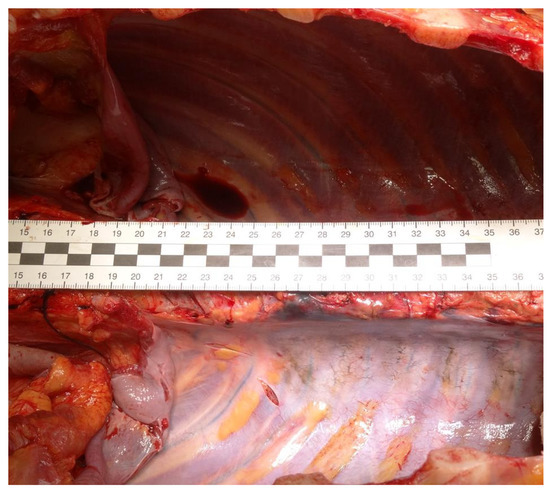
Figure 3.
The parietal pleura in the pleural cavities.
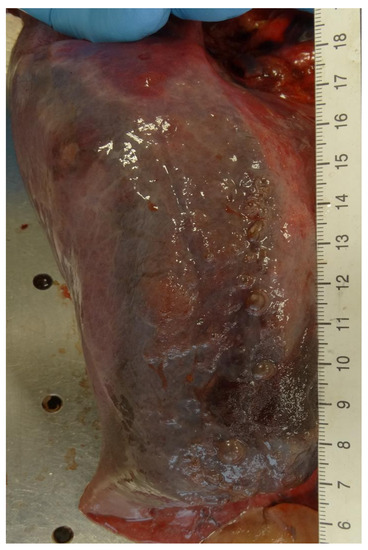
Figure 4.
Posterior surface of the lower lobe of the left lung.
2.2.3. The Microscopic Examinations
There were no remarkable findings in the brain and cerebellum, thyroid gland, pancreas, spleen, and suprarenal glands on hematoxylin-eosin staining. The lungs shoved edema and hyperemia (Figure 5). The heart shoved congestion and waviness and fragmentation of muscle fibers (Figure 6). The liver presented diffuse steatosis and lesions of the hepatocytes degeneration. In the stomach and esophagus, hemorrhagic changes, evidence of inflammatory infiltrates, thinning of the mucosa, and evident necrotic changes of the mucosa were visible (Figure 7 and Figure 8). Kidneys presented hyperemia and the necrosis within the tubular epithelium (Figure 9). Thoracic aorta shoved hemorrhagic changes and extravasation in peri-arterial tissues.
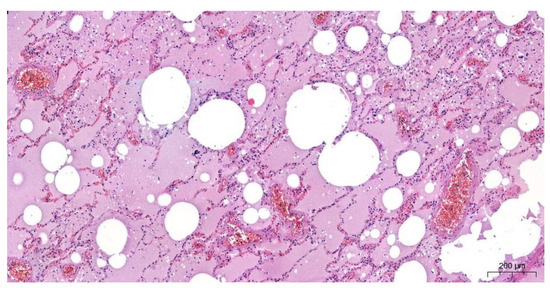
Figure 5.
Significant pulmonary oedema and hyperemia (Magnification 50×).
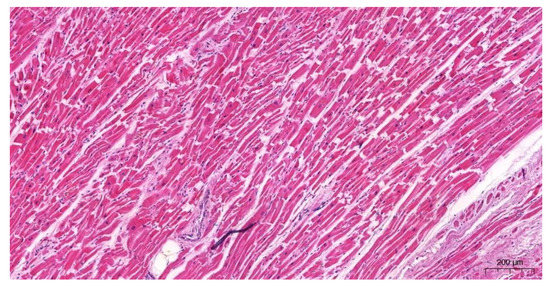
Figure 6.
Significant defragmentation in heart (Magnification 100×).
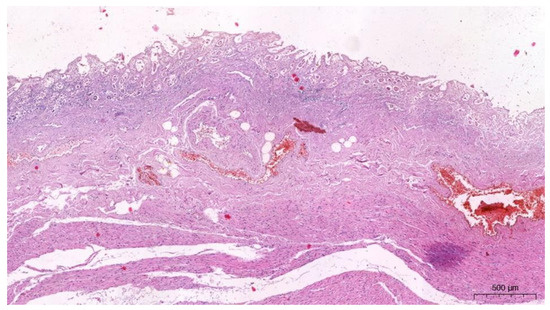
Figure 7.
Gastric mucosa with necrosis and inflammation. Submucosa with significant hyperemia and oedema (Magnification 50×).
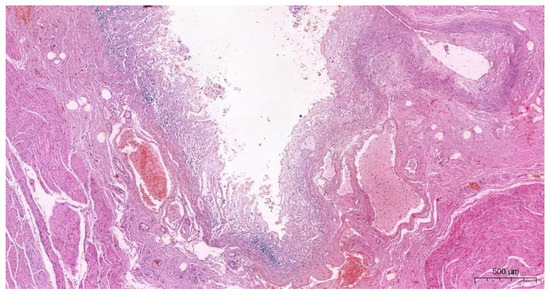
Figure 8.
Gastric mucosa with necrosis and inflammation (Magnification 50×).
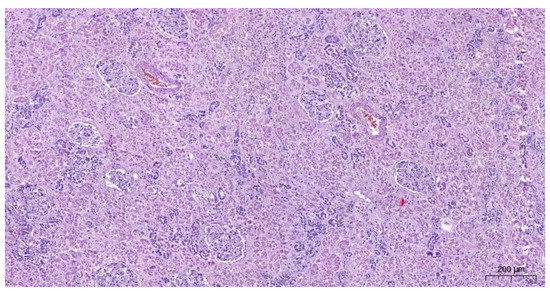
Figure 9.
Kidney’s hyperemia and the necrosis within the tubular epithelium (Magnification 100×).
2.2.4. Results of Toxicological Analyzes
The ELISA immuno-enzymatic blood tests detecting drugs and psychoactive substances were performed by the Neogen company, using reader RT-2100C. Reagent combinations were used to detect amphetamine, amphetamine/MDMA, cocaine and benzoylecgonine, tetrahydrocannabinol and its metabolites, benzodiazepines, and the opioid compound group. The toxicological tests of blood were prepared by gas chromatography (GC/MS). The postmortem concentrations of caffeine were 92.0 µg/mL in the peripheral blood. Neither blood alcohol nor any drugs were detected in the blood, which was routine toxicological screening examination.
3. Discussion
In recent years, the risk of purposely or not ingesting lethal caffeine levels has been raised by its easy availability. Energy drinks consistent caffeine, or products with high caffeine content, are easily found in shops and health stores. Powder or tablets that include pure caffeine can be bought online [17,18]. Caffeine poisoning does occur but is not shared. For example, in a listing of the drugs identified in blood in ~25,000 forensic autopsies in Sweden representing all causes of death, caffeine was in the nineteenth position in terms of prevalence [19]. The fatal concentration of caffeine in the blood reported in the literature was between 33 and 567 µg/mL [20]. There is no doubt that levels more than 80 µg/mL can be associated with caffeine-related fatalities [21]. However, relationships between blood levels of caffeine and clinical symptoms are challenging to establish due to interindividual variability, comorbidities, and tolerance [22].
Usually, the autopsy findings in caffeine-related deaths are non-specific and acute toxicity is mainly ascribed to adverse cardiovascular events, especially cardiac arrhythmias [23,24]. Heart arrhythmia, like other circulatory disorders (hyper- or hypotension), due to caffeine intoxication, is mainly associated with: adenosine receptor blockage; rises in the level of cyclic AMP through inhibition of phosphodiesterase; an increased calcium level inside cells [7,25,26]. The mechanism of death is usually attributed to heart disorders, as might be expected ventricular dysrhythmia. However, unwanted caffeine effects are not limited to arrhythmogenesis [27].
Caffeine’s effect can also be associated with antagonizing adenosine receptors and inhibition of phosphodiesterases [28], and in the digestive tract can cause gastrin release [29] or gastric acid secretion [30]. The above mechanism depends on a chemosensory answer for a bitter substance, like caffeine. Chemosensation potentially can also act in the gut through the induction of gastrin and/or histamine release from enteroendocrine cells and/or by modulating acid production in gastric acid secretion-producing parietal cells [31]. In our hypothesis, the excessive secretion of gastric acid could damage the gastrointestinal mucosa and finally perforate the esophagus.
It is not without significance that caffeine poisoning causes vomiting, damaging the mucous membrane of the digestive tract and leading to significant hypokalemia. This common symptom of caffeine poisoning can stimulate sodium-potassium pumps, immediately lead to lower serum K+ level, and increase the riskiness of losing ion, mainly due to vomiting. All described disorders can finally result in shock and might be associated with the deceased’s death after pure caffeine intoxication.
The other immediate causes of esophageal rupture, and fatal disorders, are much less probably. The postmortem examination did not reveal classic symptoms of Mackler’s triad, especially subcutaneous pneumothorax due to rupture of the esophagus, which must be visible to recognize Boerhaave’s syndrome [32]. On the other hand, it cannot be ruled out that the deceased had a risk of esophageal perforation associated with previously induced vomiting. However, the family or the investigation did not confirm information about the earliest vomiting.
4. Conclusions
The forensic pathologists’ primary duty often assists the prosecuting and judicial authorities in evaluating the cause-and-effect relationship between determining abnormalities and a victim’s death. For this purpose, a careful postmortem inspection of the body, including gross, microscopic, and toxicological examination, must be conducted because the rare death mechanisms require detailed study. The case described by us is an example that confirms the above observations.
5. Impact Statement
Although fatal caffeine poisoning has been reported in the medico-legal literature, the mechanisms and causes of death were primarily associated with complications in the cardiovascular system. The described case concerns rare complications within the digestive track with perforation of the esophagus, damage to the stomach’s mucous membrane, and deterioration of the left parietal pleura and the left lung. The postmortem revealed complications of fatal caffeine poisoning were also discussed in the mechanism and cause of deceased death.
Author Contributions
Conceptualization, M.S., A.S. and A.N.-J.; methodology related to autopsy, A.S., P.D. and J.R.-G.; formal analysis, M.S., A.S., A.N.-J. and J.R.-G.; writing—original draft preparation, M.S., A.S., P.D., A.N.-J. and J.R.-G.; writing—review and editing M.S., A.N.-J. and J.R.-G. All authors have read and agreed to the published version of the manuscript.
Funding
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript.
Institutional Review Board Statement
All procedures were performed according to the ethical and legal standards.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data in the article are in accordance with consent statement.
Conflicts of Interest
The authors have no conflict of interest to declare. No writing assistance was obtained in the production of this manuscript.
References
- Tournas, V.H. Microbial contamination of select dietary supplements. J. Food Saf. 2009, 29, 430–442. [Google Scholar] [CrossRef]
- Benedict, K.; Chiller, T.M.; Mody, R.K. Invasive Fungal Infections Acquired from Contaminated Food or Nutritional Supplements: A Review of the Literature. Foodborne Pathog. Dis. 2016, 13, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Genuis, S.J.; Schwalfenberg, G.; Siy, A.K.J.; Rodushkin, I. Toxic Element Contamination of Natural Health Products and Pharmaceutical Preparations. PLoS ONE 2012, 7, e49676. [Google Scholar] [CrossRef]
- Saper, R.B.; Phillips, R.S.; Sehgal, A.; Khouri, N.; Davis, R.B.; Paquin, J.; Thuppil, V.; Kales, S.N. Lead, Mercury, and Arsenic in US- and Indian-Manufactured Ayurvedic Medicines Sold via the Internet. JAMA 2008, 300, 915–923. [Google Scholar] [CrossRef] [PubMed]
- Tucker, J.; Fischer, T.; Upjohn, L.; Mazzera, D.; Kumar, M. Unapproved Pharmaceutical Ingredients Included in Dietary Supplements Associated With US Food and Drug Administration Warnings. JAMA Netw. Open 2018, 1, e183337. [Google Scholar] [CrossRef]
- Holmgren, P.; Lotta Nordén-Pettersson, L.; Johan Ahlner, J. Caffeine fatalities—Four case reports. Forensic Sci. Int. 2004, 139, 71–73. [Google Scholar] [CrossRef] [PubMed]
- Magdalan, J.; Zawadzki, M.; Skowronek, R.; Czuba, M.; Porębska, B.; Sozański, T.; Szpot, P. Nonfatal and fatal intoxications with pure caffeine—Report of three different cases. Forensic Sci. Med. Pathol. 2017, 13, 355–358. [Google Scholar] [CrossRef]
- Cornelis, M.C.; El-Sohemy, A. Coffee, caffeine, and coronary heart disease. Curr. Opin. Lipidol. 2007, 18, 13–19. [Google Scholar] [CrossRef]
- Ullrich, S.; de Vries, Y.; Kühn, S.; Repantis, D.; Dresler, M.; Ohla, K. Feeling smart: Effects of caffeine and glucose on cognition, mood and self-judgment. Physiol. Behav. 2015, 151, 629–637. [Google Scholar] [CrossRef] [PubMed]
- Arnaud, M.J. Pharmacokinetics and metabolism of natural methylxanthines in animal and man, in Methylxanthines. Handb. Exp. Pharmacol. 2011, 200, 33–91. [Google Scholar]
- Grosso, L.M.; Bracken, M.B. Caffeine metabolism, genetics and perinatal outcomes: A review of exposure assessment considerations during pregnancy. Ann. Epidemiol. 2005, 15, 460–466. [Google Scholar] [CrossRef]
- Yamamoto, T.; Yoshizawa, K.; Kubo, S.; Emoto, Y.; Hara, K.; Waters, B.; Umehara, T.; Murase, T.; Ikematsu, K. Autopsy report for a caffeine intoxication case and review of the current literature. J. Toxicol. Pathol. 2015, 28, 33–36. [Google Scholar] [CrossRef]
- Banerjee, P.; Ali, Z.; Levine, B.; Fowler, D.R. Fatal caffeine intoxication: A series of eight cases from 1999 to 2009. J. Forensic Sci 2014, 59, 865–868. [Google Scholar] [CrossRef]
- Musgrave, I.F.; Farrington, R.L.; Hoban, C.; Byard, R.W. Caffeine toxicity in forensic practice: Possible effects and under-appreciated sources. Forensic Sci. Med. Pathol. 2016, 12, 299–303. [Google Scholar] [CrossRef] [PubMed]
- Andrade, A.; Sousa, C.; Pedro, M.; Fernandes, M. Dangerous mistake: An accidental caffeine overdose. Case Rep. 2018, 2018. [Google Scholar] [CrossRef] [PubMed]
- James, J.E. Critical review of dietary caffeine and blood pressure: A relationship that should be taken more seriously. Psychosom. Med. 2004, 66, 63–71. [Google Scholar] [CrossRef]
- Caffeine in Food and Dietary Supplements: Examining Safety: Workshop Summary. Washington (DC): National Academies Press (US). 2014. Available online: https://www.ncbi.nlm.nih.gov/books/NBK202230/ (accessed on 27 December 2021).
- Szpak, A.; Allen, D. A case of acute suicidality following excessive caffeine intake. J. Psychopharmacol. 2012, 26, 1502–1510. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.W.; Holmgren, A. Concentration distributions of the drugs most frequently identified in post-mortem femoral blood representing all causes of death. Med. Sci. Law 2009, 49, 257–273. [Google Scholar] [CrossRef]
- Jones, A.W. Review of Caffeine-Related Fatalities along with Postmortem Blood Concentrations in 51 Poisoning Deaths. J. Anal. Toxicol. 2017, 41, 167–172. [Google Scholar] [CrossRef]
- Schulz, M.; Schmoldt, A. Therapeutic and toxic blood concentrations of more than 800 drugs and other xenobiotics. Pharmazie 2003, 58, 447–474. [Google Scholar]
- Bonsignore, A.; Sblano, S.; Pozzi, F.; Ventura, F.; Dell’Erba, A.; Palmiere, C. A case of suicide by ingestion of caffeine. Forensic Sci. Med. Pathol. 2014, 10, 448–451. [Google Scholar] [CrossRef][Green Version]
- Thelander, G.; Jonsson, A.K.; Personne, M.; Forsberg, G.S.; Lundqvist, K.M.; Ahlner, J. Caffeine fatalities—do sales restrictions prevent intentional intoxications? Clin. Toxicol. 2010, 48, 354–358. [Google Scholar] [CrossRef]
- Pelchovitz, D.J.; Goldberger, J.J. Caffeine and cardiac arrhythmias: A review of the evidence. Am. J. Med. 2011, 124, 284–289. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, M.K.F.; Gavioli, E.C.; Rosa, L.S.; Soares-Rachetti, V.D.P.; Lobão-Soares, B. Craving espresso: The dialetics in classifying caffeine as an abuse drug. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2018, 391, 1301–1318. [Google Scholar] [CrossRef] [PubMed]
- Jabbar, S.B.; Hanly, M.G. Fatal caffeine overdose: A case report and review of literature. Am. J. Forensic Med. Pathol. 2013, 34, 321–324. [Google Scholar] [CrossRef]
- Poussel, M.; Kimmoun, A.; Levy, B.; Gambier, N.; Dudek, F.; Puskarczyk, E.; Poussel, J.-F.; Chenuel, B. Fatal cardiac arrhythmia following voluntary caffeine overdose in an amateur body-builder athlete. Int. J. Cardiol. 2013, 166, e41–e42. [Google Scholar] [CrossRef] [PubMed]
- Fredholm, B.B.; Bättig, K.; Holmén, J.; Nehlig, A.; Zvartau, E.E. Actions of caffeine in the brain with special reference to factors that contribute to its widespread use. Pharmacol. Rev. 1999, 51, 83–133. [Google Scholar] [PubMed]
- Kidd, M.; Hauso, O.; Drozdov, I.; Gustafsson, B.I.; Modlin, I.M. Delineation of the chemomechanosensory regulation of gastrin secretion using pure rodent G cells. Gastroenterology 2009, 137, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Walker, J.; Hell, J.; Liszt, K.I.; Dresel, M.; Pignitter, M.; Hofmann, T.; Somoza, V. Identification of beer bitter acids regulating mechanisms of gastric acid secretion. J. Agric. Food Chem. 2012, 60, 1405–1412. [Google Scholar] [CrossRef]
- Schubert, M.L. Gastric secretion. Curr. Opin. Gastroenterol. 2004, 20, 519–525. [Google Scholar] [CrossRef]
- Lieu, M.T.; Layoun, M.E.; Dai, D.; Hoo, G.W.S.; Betancourt, J. Tension hydropneumothorax as the initial presentation of Boerhaave syndrome. Respir. Med. Case Rep. 2018, 25, 100–103. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).