Abstract
A human papillomavirus (HPV) infection is globally one of the most common causes of sexually transmitted infections of the mucous membranes (genital, anal and oral). Over the last decade, an increasing number of young patients have been infected due to the changes in sexual habits in the general population. The majority of the lesions are benign; however, substantial scientific evidence has suggested a role for the HPV family in the carcinogenesis of squamous cell carcinoma (SCC). It is proposed that dentists, in addition to ENT specialists, should apply standardized management protocols in order to construct a well-defined pathway in terms of diagnosis, which is based on a PCR diagnostic technique and the management of those lesions.
It is the opinion of the authors of this paper that the growing clamour regarding HPV-positive oropharyngeal cancer is a welcome opportunity for reconsidering and focusing on HPV oral diseases, which may affect areas of common interest for dentists and ENT doctors, such as the oral mucosa. Of particular importance are those lesions which are traditionally associated with Human Papillomavirus (HPV). These include: warts, papillomas and condylomata (Figure 1). Departing from a lively interest in “HPV and oropharynx cancer” [1,2], the psychological management of patients (young and old) affected by such lesions can be considered a challenge. If, on the one hand, this condition is a sign of the general awareness regarding the presence of sexually transmitted lesions and the oncogenicity of viral lesions, on the other, it risks becoming a nightmare for many teenagers and adults, who may be terrified by terrible malignant neoplasias.
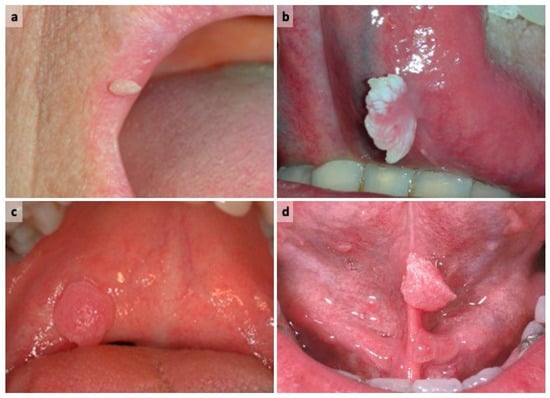
Figure 1.
Oral lesions traditionally associated with LR-HPV: (a) wart on upper lips; (b) papilloma on ventral surface of tongue; (c) condyloma on soft palate; (d) condyloma on ventral surface of tongue.
It is common knowledge in the medical profession that genital HPV infection is one of the most widespread sexually transmitted infections (STIs) throughout the global population. In the United States it has been estimated that the prevalence of infection in women aged between 19 and 54 years is approximately 40%, being markedly associated with risk factors related to sexual behaviour [3]; in Europe, the prevalence of cervical HPV infection with a high oncological risk is 3–15% in women aged 20 to 60 but it is significantly higher (29–45%) in younger women (20–24 years) [4]. In light of the changes in sexual habits in the general population in recent decades (for example, a reduction in the age of the onset of sexual activity, an increase in the number of partners, oro–genital sexual habits), the epidemiological characteristics of the HPV infection have changed as a consequence. Both in the genital area and in the oropharyngeal area, there has been an increase in the number of younger patients being exposed to this infection [5], such that many epidemiologists have now defined HPV infection as endemic.
This phenomenon would explain the increase in the frequency of HPV-related squamous cell carcinoma (SCC) in the genital tract and oropharyngeal area. Specifically, it has been found that the SCC of the tonsillar crypts and the base of tongue are significantly associated with the detection of high risk (HR) HPV (i.e., HR HPV 16) in epithelial cells (a risk of infection increased 13-fold in subjects with carcinoma, as compared to healthy controls) [6]. These cancers have the same prognostic characteristics as other oropharyngeal SCC, which should be treated in a preventive manner through targeted awareness campaigns around the world. For example, in order to disseminate preventive messages regarding HPV-related oral cancer among the general population and patients, an initiative has been introduced at the University Hospital of Palermo (Italy) in the form of a flyer (http://giuseppinacampisi.it/wp-content/uploads/flyers/Flyer_cancro_orale_e_hpv.pdf (accessed on 27 April 2021)), and YouTube video (https://www.youtube.com/watch?v=-MaLE9JwGvk&t=14s (accessed on 27 April 2021)).
When scientifically defined, and according to the most recent ICD-3-0 site/histology classification, i.e., excluding the base of the tongue, the frequency of HPV infection in the oral squamous cell carcinoma (OSCC) in the oral cavity ranges between 3.3% to 13% [7,8,9,10]. It can therefore be considered appropriate to clarify various aspects relating to benign HPV oral lesions in order to share their management through a standardized protocol.
What does HPV oral oncology have in common with warts, papillomas and condylomata of the oral cavity and the oropharynx?
“Not much” might be the reply, notwithstanding bad press and hearsay. HPVs are typically distinguished by: (a) skin type, mainly infecting the hands and feet; and (b) mucosal type, targeting: the mucosa of the oral cavity, the upper airways and digestive tract, the anogenital district, the urethra and the conjunctiva. Based on the biological behaviour of the lesions caused by the virus, there is a further classification of HPV into three groups: HPV with a high oncogenic potential (high risk or HR-HPV), such as HPVs 16, 18, 45, 56, 59, 66, 67, 70, 73, 68, 82, associated with potentially and evidently malignant lesions (e.g., anogenital and head-neck SCC); HPV of intermediate cancerogenic potential, such as HPVs 31, 33, 35, 39, 51, 52, 53, 58; and HPVs with low oncological potential (low risk or LR-HPV), such as cutaneous HPVs 2, 4, 27 and the mucosal types 6, 11, 13, 32, 42, both of which are prevalently associated with benign diseases (i.e., wart, condyloma, papilloma and focal epithelial hyperplasia), as discussed in this paper. Referring to the latter (benign) lesions, it would be opportune to engage with the patient, to reassure them about a clinical diagnosis which is not associated with oral SCC or any malignant transformation. Thereafter the possibility of an HPV infection and its possible genotype should be investigated.
Currently, the diagnosis of an HPV infection makes use of the techniques of nuclear biology, the aim of which is to detect the DNA of the virus inside the cells by means of marked genetic probes. The most sensitive and most appropriate biomolecular method for identifying the HPV genome is the PCR (Polymerase Chain Reaction). Recently, an SPF10-LiPA system has been introduced, which successively enhances the PCR method and genotype identification. It has been found to display elevated sensitivity and specificity, ease of use and the possibility of identifying multiple and persistent infections [11]. Many in the field consider that PCR techniques are preferrable to indirect techniques of viral activity as the latter are responsible for a variable rate of false negatives. Regarding a definitively safe and standardized HPV detection technique, a standard diagnostic protocol relating to the oral cavity has not yet been established in terms of: (a) the sample type under biomolecular investigation (e.g., histological sample vs. exfoliated cells); (b) the cytological sampling method (e.g., brush vs. oral rinse); (c) a procedure for the preservation of the histological sampling (e.g., frozen fresh vs. fixed in formalin and paraffin); and (d) a specific biomolecular technique to be used. The direct consequences of these weaknesses are evident. Irrespective of such weaknesses, a protocol can be used thus: in the presence of a single/multiple exophytic lesion(s) with a slow-growing, warty surface in the absence of local traumatic factors (e.g., mechanical, physical, chemical), the HPV test can be performed on cytological sampling, which must be performed prior to the excision of the oral lesion, or directly onto a paraffin section of the histological sample (according to the criteria of a given microbiological laboratory of referral) (Figure 2). Thereafter, an excisional biopsy of the lesion and confirmation of the histopathological diagnosis will be conducted. Follow-up at 6 and 12 months is advisable in order to ascertain any recurrence [12]. Where an HPV test is positive, follow-up should reoccur at 6–12 months and, where possible, after another 12-month period until the test is negative [12]. Many authors believe that it is indispensable to share this latter clinical protocol with dentists and ENT doctors in order to construct a not dissimilar pathway of the diagnosis and management of these benign lesions, which are typically associated with an LR-HPV infection.
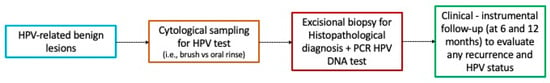
Figure 2.
Proposed protocol for suspected HPV-related oral lesions.
Author Contributions
G.C. and V.P. contributed to the conceptualization of the study, and to the manuscript revision. R.M. and P.T. wrote the original draft of the manuscript, and contributed to the visualization. All authors have read and agreed to the published version of the manuscript.
Funding
R.M. is supported by Ministero dell’Istruzione dell’Università e della Ricerca (MIUR), grant PON-AIM Line 1—Id. AIM1892002.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Acknowledgments
The authors would like to acknowledge colleagues from University of Palermo (Olga Di Fede, Giuseppa Capra and Nicoletta Termine) for having contributed to diagnosing HPV lesions and collecting the clinical pictures. The authors thank J. O. Davies for the positive contribution to language editing.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Termine, N.; Campisi, G. Oral infection by Human papillomavirus: From warts to oral cancer. Focus on epidemiology, clinics, prevention and therapy. Dent. Cadmos 2015, 83, 307–321. [Google Scholar] [CrossRef]
- Campisi, G.; Panzarella, V. Human Papillomavirus Infection: A Risk Factor for Oral and Oropharyngeal Cancers. In Textbook of Oral Cancer Prevention, Diagnosis and Management; Warn, S., Greenspan, J.S., Eds.; Springer: Cham, Switzerland, 2020; pp. 31–45. [Google Scholar] [CrossRef]
- Hariri, S.; Unger, E.R.; Sternberg, M.; Dunne, E.F.; Swan, D.; Patel, S.; Markowitz, L.E. Prevalence of genital human papillomavirus among females in the United States, the National Health and Nutrition Examination Survey, 2003–2006. J. Infect. Dis. 2011, 204, 566–573. [Google Scholar] [CrossRef] [PubMed]
- De Vuyst, H.; Clifford, G.; Li, N.; Franceschi, S. HPV infection in Europe. Eur. J. Cancer 2009, 45, 2632–2639. [Google Scholar] [CrossRef] [PubMed]
- Gillison, M.L.; Broutian, T.; Pickard, R.K.L.; Tong, Z.Y.; Xiao, W.; Kahle, L.; Gilliso, M.L. Prevalence of oral HPV infection in the United States, 2009–2010. JAMA J. Am. Med. Assoc. 2012, 307, 693–703. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, G.; Kreimer, A.R.; Viscidi, R.; Pawlita, M.; Fakhry, C.; Koch, W.M.; Westra, W.H.; Gillison, M.L. Case–Control Study of Human Papillomavirus and Oropharyngeal Cancer. N. Engl. J. Med. 2007, 356, 1944–1956. [Google Scholar] [CrossRef] [PubMed]
- Elango, K.J.; Suresh, A.; Erode, E.M.; Subhadradevi, L.; Ravindran, H.K.; Iyer, S.K.; Iyer, S.K.R.; Kuriakose, M.A. Role of human papilloma virus in oral tongue squamous cell carcinoma. Asian Pac. J. Cancer Prev. 2011, 12, 889–896. [Google Scholar] [PubMed]
- Chernock, R.D.; Zhang, Q.; El-Mofty, S.K.; Thorstad, W.L.; Lewis, J.S. Human papillomavirus-related squamous cell carcinoma of the oropharynx: A comparative study in whites and African Americans. Arch. Otolaryngol Head Neck Surg. 2011, 137, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Farasat, S.; Yu, S.S.; Neel, V.A.; Nehal, K.S.; Lardaro, T.; Mihm, M.C.; Byrd, D.R.; Balch, C.M.; Califano, J.A.; Chuang, A.Y.; et al. A new American Joint Committee on Cancer staging system for cutaneous squamous cell carcinoma: Creation and rationale for inclusion of tumor (T) characteristics. J. Am. Acad. Dermatol. 2011, 64, 1051–1059. [Google Scholar] [CrossRef] [PubMed]
- Syrjänen, S.; Lodi, G.; von Bültzingslöwen, I.; Aliko, A.; Arduino, P.; Campisi, G.; Challacombe, S.; Ficarra, G.; Flaitz, C.; Zhou, H.M.; et al. Human papillomaviruses in oral carcinoma and oral potentially malignant disorders: A systematic review. Oral. Dis. 2011, 17, 58–72. [Google Scholar] [CrossRef] [PubMed]
- Pannone, G.; Rodolico, V.; Santoro, A.; Lo Muzio, L.; Franco, R.; Botti, G.; Aquino, G.; Pedicillo, M.C.; Cagiano, S.; Campisi, G.; et al. Evaluation of a combined triple method to detect causative HPV in oral and oropharyngeal squamous cell carcinomas: p16 Immunohistochemistry, Consensus PCR HPV-DNA.; and In Situ Hybridization. Infect. Agent. Cancer 2012, 7, 4. [Google Scholar] [CrossRef] [PubMed]
- Warnakulasuriya, S.; Greenspan, J.S. Textbook of Oral Cancer: Prevention, Diagnosis and Management; Springer: Cham, Switzerland, 2020. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).