Abstract
Background: This study aimed to explore the effect of haematological markers as well as patient characteristics on stump healing in patients who underwent a lower limb amputation procedure. In addition, a practical model regarding factors that affected stump healing was developed. Methods: Patients who underwent a major lower limb amputation (above knee and below knee) at the Royal Infirmary of Edinburgh from the period of 2007 to 2010 were included in this study. A prognostic model utilizing backward stepwise logistical regression was developed to measure the probability of lower limb stump healing. The relationship between the dependent and independent variables was identified using univariate and multivariate logistic regression. Results: Three variables, namely serum sodium, serum creatinine and serum high density lipid cholesterol were identified which influenced stump healing. Patients with normal serum sodium were 75% more likely to have lower limb stump healing compared to that of patients with abnormal serum sodium (odds ratio [OR] 1.756; 95% confidence interval [CI] 1.048–2.942). Patients with normal serum creatinine were 66% more likely to have their stump healed (OR 1.664; 95% CI 0.94 to 2.946). The healing rate of patients with a normal level of serum high density lipid cholesterol was 75%, in contrast to patients with an aberrant level of serum high density lipids cholesterol (OR 1.753; 95% CI 1.061 to 2.895). The effectiveness of the retrospective stump-healing model was demonstrated by the area under the ROC curve (0.612), which was supported by the Hosmer and Lemeshow goodness-of-fit test (p = 0.879). Conclusions: Serum sodium, serum high density lipid cholesterol and serum creatinine have a strong correlation with lower limb stump healing. However, serum sodium and serum high density lipid cholesterol secondary to multiple co-morbidities in this cohort group could be altered secondary to disease pathology itself.
1. Introduction
Lower extremity amputations (LEAs) are a major source of morbidity and mortality in patients with diabetes mellitus [1]. According to estimates, every half a minute a patient with diabetes mellitus loses a leg due to an amputation [2]. The life expectancy rate among individuals who have been subjected to major amputation procedures is low and is comparable to survival rates in cancer patients (5-year mortality rates up to 55% for colon cancer vs. 73% in lower limb amputation) [3]. According to Schofield et al. [4], diabetes itself is a marker of mortality, with people with diabetes mellitus having a 55% greater risk of death than those without the disease. Diabetes foot disease requires patients to spend a considerable period of time in hospital, contributing to 25% of the hospital expenditure for diabetes mellitus [5]. There is a growing necessity for interdisciplinary treatment for amputations secondary to diabetes mellitus given the complex nature of its pathophysiology, as the number of people with diabetes mellitus continues to increase.
The proportion of the elderly in the population of the United Kingdom is considerable, signifying that an increasing number of patients with diabetes mellitus of advanced age will go on to require some form of lower limb amputation surgery [6,7]. This poses questions about the viability of subjecting older patients to surgical procedures, given the reduced healing and the co-existence of multiple conditions such as diabetes mellitus and peripheral vascular disease. Most patients in the United Kingdom referred for an amputation procedure are 75 years of age or older [8]. The increased age of this group puts them at a higher risk of developing amputation-related complications and demands the creation of more efficient treatment to ensure survival of these patients.
Healthcare professionals are faced with the challenge of assessing the different risk factors and deciding which one of them have a greater influence on the stump healing rate. There are currently an insufficient number of studies regarding factors effecting lower limb amputation. The available studies exhibit wide variation in structure and outcome. In addition, the related literature shows discrepancies regarding methods of patient selection, surgical procedures and post-operative implications. The variation exhibited by these studies makes it difficult to reach a conclusion about the way stump healing affects limb rehabilitation. It is imperative that further studies are conducted to enable the creation of a set of guidelines regarding factors contributing to the healing of the stumps following leg amputation [9].
The biomarkers used in this study were chosen because they were readily available given the scope of the study. A good biomarker is one that is relevant to the study, is cost effective, easily reproducible, has a high sensitivity, specificity and validity proven towards that disease and least prone to measurement errors and bias. The markers used in this study were factors that played a role in healing of a diabetic foot ulcer as noted in several studies and played a role in the pathophysiological pathways of peripheral vascular disease and diabetes, which are the main causes for a lower limb amputation surgery [10]. These biomarkers were easy to use, readily available for a surgeon/physician on a day-to-day basis for decision-making, were cost effective and did not require any equipment or any expertise to use or interpret. The main purpose of this study was to retrospectively explore the potential influence of blood markers and patient factors (risk factors, kidney function profile, coagulation profile, lipid profile and infection markers) on stump healing of patients with diabetes mellitus who had undergone lower extremity amputation surgery.
2. Materials and Methods
2.1. Research Design
This was a single-centre exploratory study that involved the collection of retrospective data from the Royal Infirmary of Edinburgh and identification of those independent predictors for a predictive model that affect stump healing in patients who have undergone a major lower limb amputation procedure. A favourable ethical opinion was obtained from the National Health Service Lothian ethics committee and Queen Margaret University ethics committee for the study, and the requirement for individual informed consent was waived.
Using the retrospective clinical database of patients with diabetes, we identified 300 patients between February 2007 and October 2010 who had undergone lower limb amputation. Purposive sampling technique was used for patient’s recruitment.
2.2. Study Participants
The potential participants were retrospectively purposively chosen by the researcher on the basis of the inclusion and exclusion criteria from those who underwent a below or an above knee amputation procedure at the Royal Infirmary of Edinburgh.
2.2.1. Inclusion Criteria
- -
- Patients whose age was 18 years and above.
- -
- Both genders (male and female) were eligible for the study.
- -
- Patients who had an amputation at a level of below or above knee for the first time.
2.2.2. Exclusion Criteria
- -
- Patients who had a revision of their stump either at the same level or at a higher level [11].
- -
- Patients who had a traumatic amputation due to an accident [12].
- -
- Patients with incomplete complete information required for the study.
Study was performed systematically in different steps from identification, screening, recruitment, data collection of potential participants and finally data analysis by using appropriate statistical test (Figure 1).
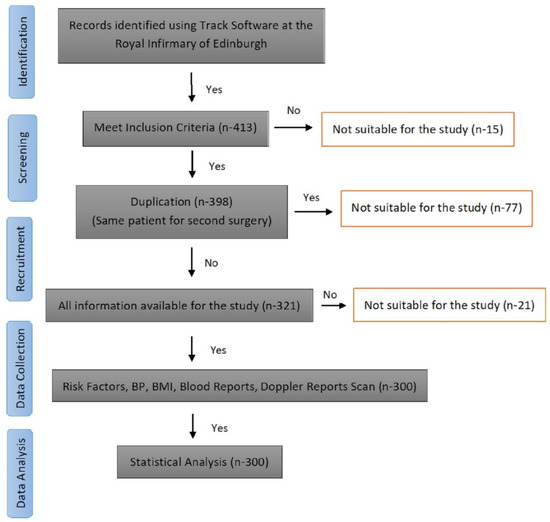
Figure 1.
Flow Diagram showing Steps from Recruitments of Subjects to Data Analysis.
A list detailing patients who had undergone above or below knee amputation surgery was initially obtained from the Department of Vascular Surgery, Royal Infirmary of Edinburgh. To recruit patients a selective sampling technique was used. The hospital’s vascular database was probed for a retrospective case note review of patients who had undergone amputation surgery. Case files were obtained from the medical records (Apex® software) for those patients whose amputation surgery was conducted at the Royal Infirmary Edinburgh between 2007 and 2010. Analysis of potential participants was undertaken through interrogation of the data. Patients’ pre-operative assessments, the clinical outcomes of their operation and follow up case notes were all utilised to compile a full report on each patient.
A total of 384 lower limb amputation surgical procedures were performed during the period. From these 300 cases who underwent either a below knee or an above knee amputation surgery for the first time were identified. Patients were excluded due to incomplete information in relation to the stump healing outcomes (n = 36) or those who had a revision of their stump either at the same level (n = 31) (below knee amputation (BKA) followed by a revision at the same level) or at a higher level (n = 17) (BKA followed by an above knee amputation (AKA).
2.3. Data Collection
A comprehensive review of the patient’s inpatient and outpatient records including the medical and surgical history was performed. The relevant demographic and clinical data collected from all medical and surgical consultations was examined and entered into Excel spreadsheet (Microsoft, Redmond, WA, USA). The Principal Investigator was aware of the identity of the patients in order to access the patients’ notes. All data was collected as per the Caldicott principles. Throughout the duration of the study, the information collected from patients was securely stored in a safe place in the vascular department of the Royal Infirmary of Edinburgh and accessibility was restricted to research team members only. Each patient was issued with a unique identification number, which corresponded to his or her personal details, personal information and consent forms. This same number was used in all stages of the study to ensure confidentiality and to protect identifying personal details. Access to the link anonymised data collected by the principal investigator throughout the study was only available to the key investigators and associate collaborators. Data storage and subsequent destruction was in accordance with the Data Protection Act 1998. Patients’ confidentiality was paramount during the collection of the data and the subsequent submission of manuscripts for publication. As per the health care records policy, these records would be destroyed after 5 years following discharge.
2.4. Predictive Measure—Stump Healing
Stump healing was defined as the complete painless closure of the wound/stump fit enough to take prosthesis for functional purposes [13]. It was determined at the end of 12 weeks from the day of lower limb amputation surgery by the single vascular consultant in the Royal Infirmary of Edinburgh [9,14].
2.5. Sample Size
Vergouwe et al. [15] recommended that, ideally, at least 100 events and 100 non-events should be used to ensure that the external validation studies are accurate. Therefore, a model should be developed from a base of no fewer than 100 events and 100 non-events to ensure adequacy of power. This recommendation was based on the observation that samples consisting of approximately 100 events were able to identify considerable discrepancies in model efficiency in up to 80% of cases. The proportion of events (stump healing rates) varied greatly in previous studies and the lowest healing rate was taken in order to have enough patients to power the study which was 30% [16]. This would mean that a sample size of 100 patients would provide 30 events and in order to obtain 100 events, a sample size of 330 would be needed to adequately power the model. According to Vergouwe et al. [15] statistically significant variations in model performance can be highlighted from an approximation of 80% power provided by an initial sample of 100 events. As a generalisation, prognostic models tend to be overly optimistic and as such, do not always work well in practice.
2.6. Statistical Analysis
Statistical analysis was performed using SPSS (IBM SPSS Statistics for Windows, Version 20.0. IBM Corp., Armonk, NY USA). Data was expressed as mean, standard deviation (SD) and 95% confidence interval (CI) or as proportions. The association between the independent factors and outcome i.e., stump healing was assessed initially employing univariable logistic regression and following this a multivariable model was produced utilising backward stepwise logistic regression with those variables found to be significant in the univariable regression at p < 0.25. The odds ratios and associated 95% confidence intervals for variables in the final model were reported. The significance level for the multivariable model was set at a p <0.05. Multicollinearity in the model was investigated to assess the relationship between the independent factors. We evaluated the calibration and discrimination performance of the model. For the calibration, the Hosmer-Lemeshow test was employed to investigate how well the predicted probabilities agreed with the observed probabilities. Discrimination, which refers to the ability of a model to distinguish between the healed and unhealed stump, was quantified using the ROC curve. The ROC curve plots the sensitivity (true positive rate) against 1—specificity (false positive rate) for consecutive cut-offs for the probability of an outcome [17].
3. Results
Retrospective data was obtained for 300 patients who underwent lower limb amputation. Ages of the participants ranged from 34 to 97 years, with a mean age of 71.16 ± 14.5 years. Percentage of patients who underwent an above knee amputation was 53.7% (n = 161) with 46.3% (n = 139) undergoing a below knee amputation. Healing of the stump as defined was achieved in sixty three percent (n = 189) of patients.
3.1. Univariable Associations
Retrospective analysis of the derivation set of 300 lower limb stumps that were performed between 2005 and 2009 revealed a failure to heal rate of 37% (n = 111). Access characteristics and univariate analysis of clinical variables for the prediction of stump healing are shown in Table 1. Univariate analysis found seven variables to be associated with lower limb stump healing: type of amputation (OR 1.64; 95% CI 1.02–2.63), gender (OR 1.53; 95% CI 0.97–2.49), hypertension (OR 0.35; 95% CI 0.09–1.24), smoking (OR 0.35; 95% CI 0.09–1.24), serum sodium (OR 1.71 95% CI 1.04–2.82), serum creatinine (OR 1.59; 95% CI 0.92–2.75) and high density lipids (OR 1.62; 95% CI 0.99–2.64). Further variables, namely age (OR 2.0; 95% CI 0.54–7.47), diabetes mellitus (OR 0.89; 95% CI 0.56–1.43), white cell count (OR 1.03; 95% CI 0.639–1.66) and prothrombin time (OR 0.99; 95% CI 0.59–1.52) were added to the model secondary to their strong clinical association with the stump healing.

Table 1.
Univariate analysis of independent variables to lower limb stump healing.
3.2. Multivariable Associations
Three variables were identified which influenced lower limb stump healing in the multivariable logistic regression analysis (Table 2). The lower limb stump healing was relatively 75% more likely in patients with normal serum sodium compared to that of patients with abnormal serum sodium (OR 1.76; 95% CI 1.04–2.94; p 0.03). Patients with normal serum creatinine were 66% more likely to have their stump healed (OR 1.66; 95% CI 0.94 to 2.95; p 0.05). A normal serum high density lipid cholesterol resulted in a 75% more likely chance of healing compared to those with abnormal serum high density lipid cholesterol (OR 1.75; 95% CI 1.06 to 2.89; p <0.03).

Table 2.
Multivariable predictors of lower limb stump healing in the retrospective data.
The overall risk score for each patient was estimated by summing the scores of each significant independent variable. Using the prediction model, the following prognostic equation was developed:
where β0 is the intercept, β1 till βn are the regression coefficients and X1 to Xn are independent variables.
where all variables are coded 0 for no or 1 for yes. The value −0.18 is called the intercept, and the other numbers are the estimated regression coefficients for the predictors, which indicate their mutually adjusted relative contribution to the outcome risk.
Risk Score − log odds of failure of stump healing [log/(1/1 − P)] = −1.82
+ (0.56 × Serum Sodium) + (0.51 × Serum Creatinine) + (0.56 × High Density Lipid)
+ (0.56 × Serum Sodium) + (0.51 × Serum Creatinine) + (0.56 × High Density Lipid)
It’s important to examine the appropriateness of fitted models. The performance of the final prognostic model assessed in terms of calibration using Hosmer-Lemeshow test was not significant (p = 0.87). This suggests that there was no statistically significant difference between predicted and observed outcomes. Receiver operating characteristic curve (ROC) figures are two-dimensional figures in which true positive rate is plotted on the Y axis and false positive rate is plotted on the X axis. In this study the corresponding receiver operating characteristic curve was constructed by calculating the sensitivity and specificity for consecutive cut-off points according to the predicted probabilities from the logistic regression models. The area under the receiver operating characteristic curve for prediction of stump healing was 0.61 (95% bias-corrected CI: 0.55–0.68), which indicates good model discrimination (Figure 2).
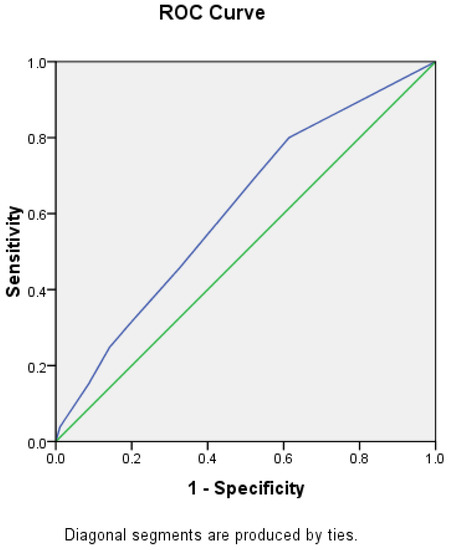
Figure 2.
Receiver Operating Curve analysis for prognostic model performance.
4. Discussion
The results of this study identified three blood markers, each of which was independently associated with successful lower limb stump healing: serum sodium, serum creatinine and serum high density lipid cholesterol. In the present study, gender emerged as a significant marker for the prediction of stump healing in univariate analysis but not in multivariate analysis. This could be the effect of unbalanced sample size with the males being in higher proportions compared to the females (n = 214 vs. n = 86). Wang et al. [18] also noted that gender was not associated with predicting wound healing.
In this study, sixty three percent (n = 189) of lower limb stumps healed. This study’s findings that primary healing rates are better in above knee stumps in comparison to below knee stumps are consistent with other studies including that of Dormandy et al. [16]. Above-knee amputations have been shown to heal in 90% of cases, whilst the healing rate of below-knee amputations varies greatly, from 30% to 92%, an average being 60% in below knee amputations. Vanross et al. [19] who conducted clinical trials in 250 new lower-limb amputees reported that the healing rates in below knee stumps were 74%. However, there are other studies where stump healing was noted to be better in below knee amputation. According to Jensen and Mandrup-Poulsen [20] the success rate of below knee amputations with regards to stump healing and prosthetic fitting was 83% in contrast to 69% healing rates and prosthesis fitting in above knee amputation. Similar findings were reported in other studies [21].
Diabetes mellitus remains a risk factor for lower limb amputation. Many studies have concluded that diabetes mellitus is an independent risk factor for foot ulcers and lower limb amputation. However, few studies have been done with regards to diabetes mellitus as a risk factor for stump healing including Low et al. [22] who reviewed 60 below knee amputations in patients with diabetes mellitus, many risk factors for foot ulcer healing were common to those of stump healing in lower limb amputation. Reiber et al. [23] reported that diabetes mellitus was a predictor of stump healing (p = 0.01), a finding shared by other studies including Moss et al. [24]. Similar findings were also reported by Criado et al. [25] and Apelqvist et al. [26] who carried out a prospective study on 314 sequentially presenting patients with diabetic foot ulcers.
Serum sodium was found to be an important predictor for stump healing. Yaghoubian et al. [27] also made comparable observations in individuals with necrotising soft tissue infection who underwent an amputation procedure. The deranged serum sodium in patients who underwent major lower limb amputation in this study is probably as a consequence of the disruption to the metabolism secondary to the injury post a major surgery. According to Nissen et al. [28] the preoperative physical condition and the presence of comorbidity influence not just the stump healing but also the functional outcomes following a lower limb amputation surgery including the prosthesis wearing rates a finding shared by Chen et al. [29] Other studies including a study done by Sheahan et al. [30] who looked at 670 patients who underwent 920 minor amputations on 747 limbs noted that end-stage renal disease (serum creatinine levels > 2.0 mg/dL) was an independent risk predictor (p < 0.001, OR 1.72, 95% CI 1.12–2.83) for limb loss and a further amputation at a higher level due to poor stump healing.
In this study, serum high density lipoproteins cholesterol was found to be a predictive marker for lower limb stump healing both in the univariate as well as the multivariate analysis. Patients with a normal serum high density lipoproteins had a 75% likelihood of stump healing, in contrast to the patients with an aberrant serum high density lipoproteins cholesterol (OR 1.75; 95% CI 1.06 to 2.89; p < 0.03). This study however did not take into account the anti-lipid medications. The cardiovascular risk factors optimisation was not looked into in this study. This is one of the limitations of the study.
Few studies have looked at lipid profile as a marker for stump healing. However, the role of anti-lipid therapies and their effect on lowering the lipid profile leading to a decreased risk in cardiovascular mortality and morbidity is well document. The STENO-2 trial [31] showed that there was a 50% reduction in microvascular and macrovascular events in the intensive arm, which included a target of total cholesterol below 175 mg/dL, and triglycerides below 150 mg/dL. In another multivariable analysis, Suckow et al. [32] who studied 436 patients with lower limb amputations between 2003 and 2008 found that the patients most likely to remain ambulatory after a lower extremity amputation were those with preoperative statin use. Similar findings were also reported by Lazzarini et al. [33] and Lee et al. [34]. Chaturvedi et al. [35] noted in their study that serum triglycerides to be an independent risk factor for lower limb amputation.
In contrast to the findings by the above studies, the Heart Protection Study [36] showed no difference in amputation rates between the groups for leg amputation (67 [2·2%] vs. 67 [2·2%]), or leg ulcer (40 [1·3%] vs. 46 [1·5%]). Rajamani et al. [37] who carried out the Fenofibrate Intervention and Event Lowering in Diabetes mellitus (FIELD) study concluded that lipid profile or statin therapy did not alter the risk of a major amputation or effect stump healing (HR 0·93, 0·53–1·62; p = 0·79).
The present study has a number of limitations. One of the major determinants of the level of amputation is that it did not take into account patients vascular supply status. This is effectively measured by radiological imaging. This study did not take into account any form of radiological imaging techniques in determining ideal level of amputation and the subsequent stump healing. According to Kern et al. [38], lower limb amputations are associated with a number of risk factors, including chronic kidney disease and peripheral neuropathy. Most of the subjects included in this study had multiple co-morbidities, the severity of which was hard to quantify. The extent of some of the co-morbidities including the duration, control and extent of complications of diabetes mellitus and the extent of renal impairment were not taken into consideration. The impact of medication on stump healing including anticoagulation therapy (aspirin vs. warfarin) was not looked into. Surgical factors such as intraoperative heparin, which may play an important role on the surgical outcome, were not considered in this study. Finally, due retrospective research design and unavailability of data regarding socio-economic status/race/ethnicity in the medical records, we did not include in the study.
This study can have several follow-up studies including the role of endothelial dysfunction markers in chronic limb ischaemia with relation to the haematological like Endothelin-1, von Willibrand factor, vascular endothelial growth factor (VEGF). Prophylactic antibiotics and its role in stump healing can be looked into on a larger scale. Another follow up of this study could be on the factors that influence the rehabilitation outcomes in lower limb amputation. The impact of early mobility on stump healing could also be explored.
5. Conclusions
Successful stump healing is a pre-requisite for ambulation following a lower limb amputation surgery. In order to identify which lower limb stumps would heal following a major lower limb amputation surgery, a pre-surgery prediction rule was formulated. It was found to be simple and easily reproducible and applied to predictive risk categories. Three markers namely serum sodium, serum creatinine and serum high density lipids cholesterol was recognized as being important predictors of lower limb stump healing. The clinical utility of these risk categories in the successful healing of the stump following a lower limb amputation surgery requires further validation in the newly treated patients.
Author Contributions
Conceptualization, Z.R. and T.C.; methodology, S.A., D.S. and R.R.; formal analysis, M.S. and S.A.; writing—original draft preparation, S.A., M.S.; writing—review and editing, M.S., S.A., D.S., R.R., T.C. and Z.R.; supervision, Z.R., T.C. and D.S.; project administration, S.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and protocol was approved by the South East Scotland Research Ethics Committee, Edinburgh, UK of National Health Services Scotland (No: 11/AL/0305).
Informed Consent Statement
Patient consent was waived by research ethics board as this study meets criteria a-f of Article 5.5 in the Tri-Council Policy Statement-2 (TCPS).
Data Availability Statement
The datasets during and/or analysed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
We thank statistician Catriona Graham (Wellcome Trust Clinical Research Facility, University of Edinburgh) for her advice in the data analysis.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hambleton, I.R.; Jonnalagadda, R.; Davis, C.R.; Fraser, H.S.; Chaturvedi, N.; Hennis, A.J. All-cause mortality after diabetes-related amputation in Barbados: A prospective case-control study. Diabetes Care 2009, 32, 306–307. [Google Scholar] [CrossRef]
- Boulton, A.J.; Vileikyte, L.; Ragnarson-Tennvall, G.; Apelqvist, J. The global burden of diabetic foot disease. Lancet 2005, 366, 1719–1724. [Google Scholar] [CrossRef]
- Armstrong, D.G.; Lavery, L.A. Negative pressure wound therapy after partial diabetic foot amputation: A multicentre, randomised controlled trial. Lancet 2005, 366, 1704–1710. [Google Scholar] [CrossRef]
- Schofield, C.J.; Libby, G.; Brennan, G.M.; MacAlpine, R.R.; Morris, A.D.; Leese, G.P. Mortality and hospitalization in patients after amputation: A comparison between patients with and without diabetes. Diabetes Care 2006, 29, 2252–2256. [Google Scholar] [CrossRef]
- Canavan, R.J.; Unwin, N.C.; Kelly, W.F.; Connolly, V.M. Diabetes- and nondiabetes-related lower extremity amputation incidence before and after the introduction of better organized diabetes foot care: Continuous longitudinal monitoring using a standard method. Diabetes Care 2008, 31, 459–463. [Google Scholar] [CrossRef] [PubMed]
- National Amputee Statistical Database (NASDAB). National Amputee Statistical Database Annual Report 2005/2006. Edinburgh: NASDAB [Online]. 2006. Available online: http://www.nasdab.co.uk (accessed on 4 November 2017).
- Navarro-Flores, E.; Romero-Morales, C.; Becerro de Bengoa-Vallejo, R.; Rodríguez-Sanz, D.; Palomo-López, P.; López-López, D.; Losa-Iglesias, M.E.; Calvo-Lobo, C. Sex Differences in Frail Older Adults with Foot Pain in a Spanish Population: An Observational Study. Int. J. Environ. Res. Public Health 2020, 17, 6141. [Google Scholar] [CrossRef] [PubMed]
- UNIPOD. Limbless Statistics–Annual Report. University of Salford 2011/2012. Available online: https://shop.salford.ac.uk/product-catalogue/university-goods-and-services/limbless-statistics/limbless-statistics-annual-report-201112 (accessed on 20 June 2021).
- Nawijn, S.E.; van der Linde, H.; Emmelot, C.H.; Hofstad, C.J. Stump management after trans-tibial amputation: A systematic review. Prosthet. Orthot. Int. 2005, 29, 13–26. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Ros, P.; Navarro-Flores, E.; Julián-Rochina, I.; Martínez-Arnau, F.M.; Cauli, O. Changes in Salivary Amylase and Glucose in Diabetes: A Scoping Review. Diagnostics 2021, 11, 453. [Google Scholar] [CrossRef] [PubMed]
- Albino, F.P.; Seidel, R.; Brown, B.J.; Crone, C.G.; Attinger, C.E. Through knee amputation: Technique modifications and surgical outcomes. Arch. Plast. Surg. 2014, 41, 562–570. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.; Tang, T.; Wang, A.; Cui, S. Surgical revision for stump problems after traumatic above-ankle amputations of the lower extremity. BMC Musculoskelet. Disord. 2015, 16, 48. [Google Scholar] [CrossRef] [PubMed]
- Tisi, P.V.; Than, M.M. Type of incision for below knee amputation. Cochrane Database Syst. Rev. 2014, Cd003749. [Google Scholar] [CrossRef]
- Wong, C.K.; Edelstein, J.E. Unna and elastic postoperative dressings: Comparison of their effects on function of adults with amputation and vascular disease. Arch. Phys. Med. Rehabil. 2000, 81, 1191–1198. [Google Scholar] [CrossRef] [PubMed]
- Vergouwe, Y.; Steyerberg, E.W.; Eijkemans, M.J.; Habbema, J.D. Substantial effective sample sizes were required for external validation studies of predictive logistic regression models. J. Clin. Epidemiol. 2005, 58, 475–483. [Google Scholar] [CrossRef] [PubMed]
- Dormandy, J.; Heeck, L.; Vig, S. Major amputations: Clinical patterns and predictors. Semin. Vasc. Surg. 1999, 12, 154–161. [Google Scholar] [PubMed]
- Steyerberg, E.W.; Vickers, A.J.; Cook, N.R.; Gerds, T.; Gonen, M.; Obuchowski, N.; Pencina, M.J.; Kattan, M.W. Assessing the performance of prediction models: A framework for traditional and novel measures. Epidemiology 2010, 21, 128–138. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.L.; Wang, M.; Liu, T.K. Predictors for wound healing in ischemic lower limb amputation. J. Formos. Med Assoc. 1994, 93, 849–854. [Google Scholar]
- Vanross, E.R.; Johnson, S.; Abbott, C.A. Effects of early mobilization on unhealed dysvascular transtibial amputation stumps: A clinical trial. Arch. Phys. Med. Rehabil. 2009, 90, 610–617. [Google Scholar] [CrossRef] [PubMed]
- Steen Jensen, J.; Mandrup-Poulsen, T. Success rate of prosthetic fitting after major amputations of the lower limb. Prosthet. Orthot. Int. 1983, 7, 119–121. [Google Scholar] [CrossRef][Green Version]
- Christensen, S. Lower Extremity Amputations in the County of Aalborg 1961–1971: Population Study and Follow-Up. Acta Orthop. Scand. 1976, 47, 329–334. [Google Scholar] [CrossRef]
- Low, C.K.; Chew, W.Y.; Howe, T.S.; Tan, S.K. Factors affecting healing of below knee amputation. Singap. Med. J. 1996, 37, 392–393. [Google Scholar]
- Reiber, G.E.; Pecoraro, R.E.; Koepsell, T.D. Risk factors for amputation in patients with diabetes mellitus: A case-control study. Ann. Intern. Med. 1992, 117, 97–105. [Google Scholar] [CrossRef]
- Moss, S.E.; Klein, R.; Klein, B.E. The prevalence and incidence of lower extremity amputation in a diabetic population. Arch. Intern. Med. 1992, 152, 610–616. [Google Scholar] [CrossRef]
- Criado, E.; De Stefano, A.A.; Keagy, B.A.; Upchurch, G.R., Jr.; Johnson, G., Jr. The course of severe foot infection in patients with diabetes. Surg. Gynecol. Obstet. 1992, 175, 135–140. [Google Scholar] [PubMed]
- Apelqvist, J.; Agardh, C.D. The association between clinical risk factors and outcome of diabetic foot ulcers. Diabetes Res. Clin. Pract. 1992, 18, 43–53. [Google Scholar] [CrossRef]
- Yaghoubian, A.; de Virgilio, C.; Dauphine, C.; Lewis, R.J.; Lin, M. Use of admission serum lactate and sodium levels to predict mortality in necrotizing soft-tissue infections. Arch. Surg. 2007, 142, 840–846; discussion 844–846. [Google Scholar] [CrossRef] [PubMed]
- Nissen, S.J.; Newman, W.P. Factors influencing reintegration to normal living after amputation. Arch. Phys. Med. Rehabil. 1992, 73, 548–551. [Google Scholar]
- Chen, M.C.; Lee, S.S.; Hsieh, Y.L.; Wu, S.J.; Lai, C.S.; Lin, S.D. Influencing factors of outcome after lower-limb amputation: A five-year review in a plastic surgical department. Ann. Plast. Surg. 2008, 61, 314–318. [Google Scholar] [CrossRef]
- Sheahan, M.G.; Hamdan, A.D.; Veraldi, J.R.; McArthur, C.S.; Skillman, J.J.; Campbell, D.R.; Scovell, S.D.; LoGerfo, F.W.; Pomposelli, F.B., Jr. Lower extremity minor amputations: The roles of diabetes mellitus and timing of revascularization. J. Vasc. Surg. 2005, 42, 476–480. [Google Scholar] [CrossRef]
- Gaede, P.; Lund-Andersen, H.; Parving, H.H.; Pedersen, O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N. Engl. J. Med. 2008, 358, 580–591. [Google Scholar] [CrossRef] [PubMed]
- Suckow, B.D.; Goodney, P.P.; Cambria, R.A.; Bertges, D.J.; Eldrup-Jorgensen, J.; Indes, J.E.; Schanzer, A.; Stone, D.H.; Kraiss, L.W.; Cronenwett, J.L. Predicting functional status following amputation after lower extremity bypass. Ann. Vasc. Surg. 2012, 26, 67–78. [Google Scholar] [CrossRef]
- Lazzarini, P.A.; O’Rourke, S.R.; Russell, A.W.; Clark, D.; Kuys, S.S. What are the key conditions associated with lower limb amputations in a major Australian teaching hospital? J. Foot Ankle Res. 2012, 5, 12. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Lu, M.; Lee, V.S.; Russell, D.; Bahr, C.; Lee, E.T. Lower-extremity amputation. Incidence, risk factors, and mortality in the Oklahoma Indian Diabetes Study. Diabetes 1993, 42, 876–882. [Google Scholar] [CrossRef] [PubMed]
- Chaturvedi, N.; Stevens, L.K.; Fuller, J.H.; Lee, E.T.; Lu, M. Risk factors, ethnic differences and mortality associated with lower-extremity gangrene and amputation in diabetes. The WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia 2001, 44 (Suppl. 2), S65–S71. [Google Scholar] [CrossRef] [PubMed]
- Collins, R.; Armitage, J.; Parish, S.; Sleigh, P.; Peto, R. MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: A randomised placebo-controlled trial. Lancet 2003, 361, 2005–2016. [Google Scholar] [CrossRef]
- Rajamani, K.; Colman, P.G.; Li, L.P.; Best, J.D.; Voysey, M.; D’Emden, M.C.; Laakso, M.; Baker, J.R.; Keech, A.C. Effect of fenofibrate on amputation events in people with type 2 diabetes mellitus (FIELD study): A prespecified analysis of a randomised controlled trial. Lancet 2009, 373, 1780–1788. [Google Scholar] [CrossRef]
- Kern, E.F.O.; Maney, M.; Miller, D.R.; Tseng, C.-L.; Tiwari, A.; Rajan, M.; Aron, D.; Pogach, L. Failure of ICD-9-CM codes to identify patients with comorbid chronic kidney disease in diabetes. Health Serv. Res. 2006, 41, 564–580. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).