Abstract
Maternal mental illness significantly impacts caregiving, influencing both mothers and their children. This narrative review examines the challenges faced by mothers with conditions such as depression, anxiety, bipolar disorder, and schizophrenia, which often disrupt caregiving routines, emotional stability, and social integration. These difficulties can hinder secure attachments and contribute to adverse developmental outcomes in children, including heightened risks of anxiety, depression, behavioral issues, and cognitive impairments. Children of mothers with mental illnesses are 1.8 times more likely to develop emotional or behavioral problems and face a 2.7 times higher risk of suicidal ideation during adolescence. Intergenerational transmission of mental illness is also prevalent, with affected children showing a 2.5 times greater likelihood of developing mental illnesses in adulthood. Effective interventions include cognitive behavioral therapy (CBT), family-based approaches, and community programs integrating parenting education and mental health resources. These strategies have demonstrated improvements in maternal well-being and child resilience. The review highlights the need for comprehensive policies addressing maternal mental health, early intervention for children, and culturally sensitive support systems to break cycles of intergenerational mental illness. Future research should prioritize evaluating long-term intervention effectiveness and exploring innovative tools like digital mental illnesses solutions to support affected families.
1. Introduction
Motherhood is a demanding role that requires emotional stability, resilience, and consistent caregiving. For mothers experiencing mental illnesses, these demands can become significantly more challenging [1]. Mental illnesses such as depression, anxiety, bipolar disorder, and schizophrenia can interfere with a mother’s ability to provide stable and nurturing care [2]. These challenges may lead to difficulties in forming secure attachments, maintaining routine caregiving tasks, and managing stress, which can, in turn, impact the child’s emotional and cognitive development [3]. Moreover, societal stigma and lack of adequate support further exacerbate the struggles faced by these mothers [4].
Children and adolescents raised by parents with mental illnesses often face unique adversities. The instability that can accompany parental mental illness may lead to increased exposure to stress, neglect, and even trauma [5]. Studies indicate that children of parents with mental health conditions are at a higher risk for developing emotional, behavioral, and cognitive difficulties themselves [6]. These children may struggle with identity formation, social relationships, and academic performance, potentially leading to long-term psychological effects [7]. Additionally, they may take on caregiving responsibilities at a young age, which can impact their own well-being and development [8].
Generally, studies have revealed a high correlation between children’s behavioral disorders and parents’ mental illnesses [6], mothers’ mental stress [9,10], mothers’ poor mental health [6,9] mothers’ irrational beliefs [6], parenting stress [11,12], poor child–parent interaction [13], depression [14,15,16,17] caused by economic problems, social [18] and cultural [19] pressures, and parenting styles [20]. Therefore, environmental stress factors (in parents) can create psychological disorders and many other complications for children.
When these two challenges—maternal mental illness and its impact on child development—are combined, the effects can be particularly profound. The interplay between a mother’s mental illness and her child’s upbringing creates a dynamic that may perpetuate cycles of mental health issues across generations [21,22]. Family environments characterized by unpredictability, emotional distress, and inadequate coping mechanisms can hinder the child’s ability to develop resilience [21,23,24]. Furthermore, the lack of appropriate social and healthcare support can leave both mothers and their children vulnerable to persistent difficulties [25,26,27].
Despite the growing body of literature on maternal mental disorders and their impact on children, important gaps remain. These include a limited focus on how maternal psychopathology specifically affects child cognitive development, a lack of integration between clinical and social frameworks in the analysis, and insufficient attention to resilience mechanisms that might protect against intergenerational transmission of mental health problems. Addressing these gaps is essential to designing more holistic and effective support strategies for affected families.
This narrative review aims to explore the dual challenge of maternity with a mental illness and its impact on children and adolescents. By synthesizing the existing literature, this review will highlight the primary difficulties faced by mothers with mental illnesses, the challenges encountered by their children, and the broader implications of these intersecting experiences. Additionally, it will discuss available support mechanisms and potential interventions to mitigate these difficulties [28]. Understanding these complex dynamics is essential for developing effective policies and programs that support affected families and promote better mental health outcomes for both mothers and their children [29].
2. Results
This review included a total of 18 studies published between 2009 and 2024, covering a range of research methodologies such as longitudinal cohort studies, cross-sectional surveys, and randomized controlled trials. These studies were identified through a literature search conducted in PubMed, PsycINFO, and Google Scholar. Keywords included “maternal mental illness”, “parenting and mental health”, “children of parents with mental disorders”, and “adolescent psychological development”. The analysis revealed key findings related to maternal challenges, child and adolescent impact, cognitive deficits, suicide risks, intergenerational transmission of mental illness, and intervention strategies; these concepts are defined in Table 1.

Table 1.
Key concepts in the review results.
Maternal Challenges: A significant proportion (approximately 68%) of mothers with a diagnosed mental illness reported difficulties in maintaining consistent caregiving routines. Mothers with severe mental illnesses, such as schizophrenia and bipolar disorder, were more likely to experience social isolation and lack of support compared to those with mild to moderate conditions [30,31].
Child and Adolescent Impact: Children of mothers with mental illness exhibited a 1.8 times higher likelihood of developing anxiety and depression compared to those with mentally healthy mothers [32]. Behavioral issues, including aggression and social withdrawal, were reported in 35% of cases [33,34]. Additionally, increased stress and self-blame were identified as common experiences among these children [35,36].
Cognitive Deficits in Offspring: Several studies identified cognitive impairments in children of mothers with mental illnesses, particularly in executive functioning, memory, and attention. These deficits were observed as early as preschool age and persisted into adolescence, potentially affecting academic performance and social integration [37,38]. Deficits in problem-solving abilities and verbal fluency were also common, highlighting the need for early cognitive interventions to support affected children. The evidence suggests that children exposed to more severe or psychotic parental psychopathology may present broader and more persistent impairments across multiple cognitive domains, reinforcing the need for early neurodevelopmental screening and intervention [39].
Suicide Risks and Self-Harm: Adolescents raised by mothers with mental illness were at an increased risk of suicidal ideation and self-harm behaviors. The suicide risk was approximately 2.7 times higher compared to peers with mentally healthy mothers [40,41]. Factors such as emotional neglect, familial instability, and a lack of coping mechanisms contributed to this elevated risk. Early screening and psychological support for at-risk adolescents are critical in mitigating these dangers.
Intergenerational Transmission: Studies revealed that children raised in households with maternal mental illness had a 2.5 times greater risk of experiencing mental illness in adulthood. These children also demonstrated lower academic performance and increased school dropout rates. Emotional dysregulation and attachment issues in early life were identified as mediators in the persistence of mental illness across generations [42,43,44]. This risk often extended beyond the specific diagnostic category of the parent, indicating a transdiagnostic vulnerability that includes both affective and psychotic disorders [45].
Intervention and Support Systems: Psychological interventions, such as cognitive behavioral therapy (CBT) and parental support groups, were found to be effective in mitigating negative outcomes. Family-based interventions showed a 40% improvement in child well-being and a 30% reduction in maternal stress levels [46,47]. Community support programs that integrated parenting education and mental health resources demonstrated promising results in improving long-term outcomes for both mothers and children [31].
Overall, the results highlight the significant challenges faced by mothers with mental disorders and their children. The findings emphasize the need for targeted interventions aimed at reducing psychological distress and breaking the intergenerational cycle of mental illness. Future research should focus on evaluating the long-term effectiveness of intervention programs and developing culturally sensitive approaches to supporting affected families. Table 2 presents a critical analysis of these studies.

Table 2.
Main results of the selected articles in the narrative review.
3. Discussion
The findings of this review emphasize the significant challenges faced by mothers with mental illnesses and their children, highlighting the need for targeted interventions to break the cycle of intergenerational mental illness. The combination of maternal mental illness and the developmental impact on children creates a complex dynamic that requires multifaceted approaches for intervention and support.
Summary of Results: The reviewed studies confirm that maternal mental illness is strongly associated with difficulties in caregiving, affecting child emotional and cognitive development. Findings show that children of affected mothers have a higher prevalence of anxiety, depression, and behavioral disorders [32], with cognitive deficits observed as early as preschool age [36,37,39]. Adolescents from such backgrounds experience an increased risk of self-harm and suicidal ideation [40,41]. Additionally, intergenerational studies highlight the role of parental mental health in shaping adolescent outcomes [42,43,45]. Wang et al. (2024) further link early psychiatric symptoms to transdiagnostic cognitive impairments in at-risk youth [38]. These outcomes indicate that maternal mental health significantly influences the psychological resilience and social adaptation of children, reinforcing the need for early interventions.
Although clinical aspects are addressed throughout the following recommendations, we now highlight more explicitly the clinical implications of our findings. Several of the reviewed studies support the importance of the early identification of cognitive and emotional difficulties in children of mothers with mental illnesses, as well as the implementation of integrated care programs that combine maternal mental health treatment with pediatric follow-up. Interventions such as cognitive behavioral therapy and family-based programs not only improve maternal functioning but also reduce risk factors in children. These findings reinforce the need for multidisciplinary clinical approaches in primary care, perinatal services, and child mental health systems.
Recommendations for Mothers: Addressing maternal mental health is crucial in mitigating its impact on child development. Providing accessible maternal healthcare, integrating mental health services into prenatal and postnatal care, and promoting community-based support networks can improve maternal well-being and caregiving quality [31]. Cognitive behavioral therapy (CBT) and peer-support groups have shown effectiveness in reducing stress and improving maternal mental health outcomes [31]. Wadephul et al. (2016) highlight the benefits of antenatal psychological group interventions for improving maternal psychological well-being [47]. Reducing the stigma surrounding maternal mental illness is also essential in encouraging mothers to seek help without fear of judgment [30].
Recommendations for Children and Adolescents: Children of mothers with mental illnesses require targeted psychological support to mitigate their increased risk for emotional and cognitive impairments. School-based mental health programs, peer mentoring, and community outreach initiatives can provide stability and structured support [34]. Engaging children in structured activities such as arts, sports, and counseling programs can strengthen resilience and social skills, reducing the long-term effects of parental mental illness [33]. Educational initiatives that teach emotional regulation and problem-solving skills can empower children to manage stress more effectively. Intergenerational trauma studies also emphasize the importance of addressing resilience mechanisms to break cycles of adversity [35].
Recommendations for Family-Based Interventions: Family-based interventions that address both maternal and child mental health are essential. Joint therapy sessions, attachment-based interventions, and parental training programs can improve parent–child relationships and emotional co-regulation [37]. Establishing multidisciplinary support networks, including healthcare providers, educators, and social workers, can ensure that affected families receive comprehensive care tailored to their specific needs [34]. Addressing family-level stressors such as financial insecurity, housing instability, and lack of social support is also crucial in improving outcomes for both mothers and children [31].
Future Directions and Research Needs: Future research should focus on evaluating the long-term effectiveness of existing interventions and exploring culturally sensitive approaches that cater to diverse populations. More longitudinal studies are needed to understand the trajectory of children raised by mothers with mental illnesses, examining resilience factors that may mitigate adverse outcomes [43]. Sunde et al. (2024)—in their pre-print—highlight how socioeconomic differences influence mental illness across generations, suggesting that addressing these disparities is key to breaking intergenerational cycles of poor mental health [44]. Additionally, policymakers should consider integrating mental health support into primary healthcare systems to enable early detection and intervention. The growing field of digital mental health interventions should also be explored as a potential tool for reaching mothers and children who may have limited access to traditional mental health services [38].
Strengths and limitations: This narrative review methodology presents both strengths and limitations. Among its strengths are the breadth of databases consulted and the inclusion of diverse study types addressing both clinical and psychosocial dimensions. The thematic synthesis approach allowed for the integration of heterogeneous findings in a coherent and structured manner. However, the absence of a predefined systematic protocol may reduce reproducibility, and the article selection process—though carefully executed—may still be influenced by subjective interpretation. These methodological considerations should be taken into account when interpreting and applying the findings of this review. Although this review covers a wide range of social and contextual stressors, we identified a lack of studies specifically addressing single motherhood. This is a relevant omission, given the potential compounding effects of parenting, economic hardship, and reduced social support on maternal and child mental health. Future research should explore how single motherhood intersects with mental illness and influences caregiving, child outcomes, and access to services.
4. Materials and Methods
This narrative review was conducted through a comprehensive literature search in major electronic databases, including PubMed, PsycINFO, and Google Scholar. The search targeted peer-reviewed studies published between January 2005 and March 2025, addressing the challenges of motherhood in the context of mental illness and the developmental impact on children and adolescents. The search was limited to articles published in English, with full-text availability, and focused on populations ranging from birth to 18 years of age. Keywords included “maternal mental illness”, “parenting and mental health”, “children of parents with mental disorders”, and “adolescent psychological development”. Boolean operators and controlled vocabulary were used when applicable to optimize the search process. In addition, quality gray studies, such as doctoral theses [48], were considered when they provided relevant evidence not available in peer-reviewed articles. These documents were identified and marked as gray literature. The study selection process is illustrated in the flow diagram presented in Figure 1.
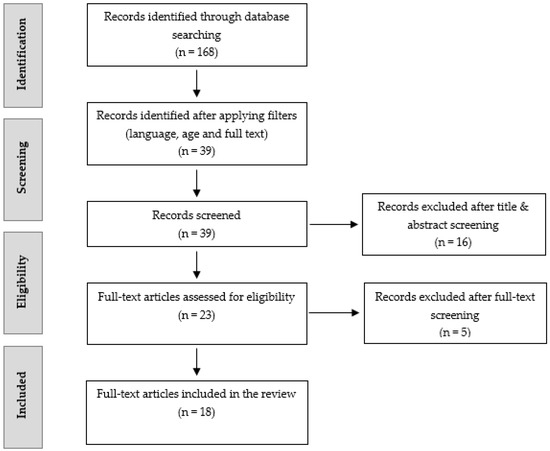
Figure 1.
Flow diagram of study selection process.
Studies were selected based on their thematic relevance, methodological rigor, and overall contribution to understanding the psychological, cognitive, and social implications of parental mental illness. Priority was given to empirical research involving children or adolescents exposed to maternal psychopathology, including both observational and interventional designs. In addition, studies exploring protective factors, support systems, and resilience-enhancing strategies were included to provide a holistic perspective on potential outcomes and interventions.
The review employed a thematic synthesis approach, organizing the findings into core categories: maternal caregiving challenges, emotional and behavioral outcomes in children and adolescents, cognitive impairments, intergenerational transmission of mental illness, suicide risk, and intervention frameworks. This allowed for the integration of findings across diverse methodologies while maintaining conceptual coherence. The gray literature—including health organization reports and policy guidelines—was incorporated when relevant to broaden the practical and contextual understanding of the topic.
The initial identification of the articles, including the selection of titles and abstracts to determine their relevance, was carried out by the first author. The second author independently reviewed the selected articles for relevance and methodological quality. Discrepancies were discussed until a consensus was reached. Articles that met the full-text inclusion criteria were then retrieved and assessed for eligibility. Additional references were located by manually searching the bibliographies of the included studies.
Only publicly accessible, peer-reviewed, and ethically approved studies were included. Ethical considerations were respected by excluding any research that did not clearly report ethical compliance.
Table 3 provides a structured overview of the key studies analyzed in this review, ensuring clarity and comprehensiveness in presenting the research findings. Further details on the characteristics of each article—including objectives, methodology, sample, data collection, main findings, robustness, contributions, and limitations—can be found in Supplementary Material Table S1, which expands on the critical analysis of the studies.

Table 3.
Summary of reviewed studies.
5. Conclusions
The interplay between maternal mental illness and child development presents significant challenges that require a comprehensive and multi-tiered approach to intervention. Providing accessible maternal mental healthcare, enhancing child support systems, and implementing family-focused interventions are critical steps toward breaking the intergenerational transmission of mental illness. Limitations of the review include potential publication bias and the exclusion of non-English language studies, which may have led to the omission of relevant research from different cultural contexts. Future studies should continue to explore innovative intervention strategies and policies that support affected families, ensuring better mental health outcomes for both mothers and their children.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/women5030026/s1: Table S1: Critical analysis of the articles.
Author Contributions
R.A.-A.: conceptualization, initial literature search and synthesis, data interpretation, writing—review and editing, and writing—original draft. C.P.: advanced literature search and synthesis, data interpretation, writing—review and editing, and writing—original draft. A.D.-P.: data interpretation and writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
Dra. Rosa Ayesa-Arriola was financed by a Miguel Servet contract from the Carlos III Health Institute (CP18/00003) and a Consolidator Grant from the Ministerio de Ciencia e Invovación (CNS2022-136110).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Díaz-Pons, A.; Soler-Andrés, M.; Ortiz-García de la Foz, V.; Murillo-García, N.; Yorca-Ruiz, A.; Magdaleno Herrero, R.; Castaño-Castaño, S.; González-Rodríguez, A.; Setién-Suero, E.; Ayesa-Arriola, R. Exploring parenthood in first episode of psychosis: The potential role of the offspring in the outcome of women. Arch. Womens Ment. Health 2024, 27, 693–703. [Google Scholar] [CrossRef] [PubMed]
- Modak, A.; Ronghe, V.; Gomase, K.P.; Mahakalkar, M.G.; Taksande, V. A Comprehensive Review of Motherhood and Mental Health: Postpartum Mood Disorders in Focus. Cureus 2023, 15, e46209. [Google Scholar] [CrossRef] [PubMed]
- Frosch, C.A.; Schoppe-Sullivan, S.J.; O’Banion, D.D. Parenting and Child Development: A Relational Health Perspective. Am. J. Lifestyle Med. 2021, 15, 45–59. [Google Scholar] [CrossRef] [PubMed]
- Kirkbride, J.B.; Anglin, D.M.; Colman, I.; Dykxhoorn, J.; Jones, P.B.; Patalay, P.; Pitman, A.; Soneson, E.; Steare, T.; Wright, T.; et al. The social determinants of mental health and disorder: Evidence, prevention and recommendations. World Psychiatry Off. J. World Psychiatr. Assoc. WPA 2024, 23, 58–90. [Google Scholar] [CrossRef] [PubMed]
- Beesdo, K.; Knappe, S.; Pine, D.S. Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatr. Clin. N. Am. 2009, 32, 483–524. [Google Scholar] [CrossRef] [PubMed]
- Karimzadeh, M.; Rostami, M.; Teymouri, R.; Moazzen, Z.; Tahmasebi, S. The association between parental mental health and behavioral disorders in pre-school children. Electron. Physician 2017, 9, 4497–4502. [Google Scholar] [CrossRef] [PubMed]
- Paulus, F.W.; Ohmann, S.; Möhler, E.; Plener, P.; Popow, C. Emotional Dysregulation in Children and Adolescents With Psychiatric Disorders. A Narrative Review. Front. Psychiatry 2021, 12, 628252. [Google Scholar] [CrossRef] [PubMed]
- Phillips, R.; Durkin, M.; Engward, H.; Cable, G.; Iancu, M. The impact of caring for family members with mental illnesses on the caregiver: A scoping review. Health Promot. Int. 2023, 38, daac049. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, K.; Patel, M.; Ragavan, M.I.; Rojas, C.R. Prioritizing caregiver mental health to promote child health. Pediatr. Res. 2024. [Google Scholar] [CrossRef] [PubMed]
- Ciciolla, L.; Gerstein, E.D.; Crnic, K.A. Reciprocity among maternal distress, child behavior, and parenting: Transactional processes and early childhood risk. J. Clin. Child Adolesc. Psychol. 2014, 43, 751–764. [Google Scholar] [CrossRef] [PubMed]
- Radley, J.; Barlow, J.; Johns, L.C. Parenting and psychosis: An experience sampling methodology study investigating the inter-relationship between stress from parenting and positive psychotic symptoms. Br. J. Clin. Psychol. 2022, 61, 1236–1258. [Google Scholar] [CrossRef] [PubMed]
- Tahmasian, K.; Anari, A.; Fathabadi, M. Evaluation of Effective Maternal Characteristics in Behavioral Problems of 2–6 Years Old Children. J. Mod. Psychol. Res. 2012, 7, 89–104. [Google Scholar]
- Dubois-Comtois, K.; Bernier, A.; Tarabulsy, G.M.; Cyr, C.; St-Laurent, D.; Lanctôt, A.-S.; St-Onge, J.; Moss, E.; Béliveau, M.-J. Behavior problems of children in foster care: Associations with foster mothers’ representations, commitment, and the quality of mother-child interaction. Child Abuse Negl. 2015, 48, 119–130. [Google Scholar] [CrossRef] [PubMed]
- Narayanan, M.K.; Nærde, A. Associations between maternal and paternal depressive symptoms and early child behavior problems: Testing a mutually adjusted prospective longitudinal model. J. Affect. Disord. 2016, 196, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Aunola, K.; Ruusunen, A.-K.; Viljaranta, J.; Nurmi, J.-E. Parental Affection and Psychological Control as Mediators Between Parents’ Depressive Symptoms and Child Distress. J. Fam. Issues 2015, 36, 1022–1042. [Google Scholar] [CrossRef]
- Dette-Hagenmeyer, D.E.; Reichle, B. Parents’ depressive symptoms and children’s adjustment over time are mediated by parenting, but differentially for fathers and mothers. Eur. J. Dev. Psychol. 2014, 11, 196–210. [Google Scholar] [CrossRef]
- Bagner, D.M.; Pettit, J.W.; Lewinsohn, P.M.; Seeley, J.R.; Jaccard, J. Disentangling the temporal relationship between parental depressive symptoms and early child behavior problems: A transactional framework. J. Clin. Child Adolesc. Psychol. 2013, 42, 78–90. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Godinet, M.T.; Arnsberger, P. Protective factors among families with children at risk of maltreatment: Follow up to early school years. Child. Youth Serv. Rev. 2011, 33, 139–148. [Google Scholar] [CrossRef]
- Ferrari, A.M. The impact of culture upon child rearing practices and definitions of maltreatment. Child Abuse Negl. 2002, 26, 793–813. [Google Scholar] [CrossRef] [PubMed]
- Wolfradt, U.; Hempel, S.; Miles, J.N.V. Perceived parenting styles, depersonalisation, anxiety and coping behaviour in adolescents. Personal. Individ. Differ. 2003, 34, 521–532. [Google Scholar] [CrossRef]
- Stevenson, C.; Wakefield, J.R.H.; Kellezi, B.; Stack, R.J.; Dogra, S. Families as support and burden: A mixed methods exploration of the extent to which family identification and support predicts reductions in stress among disadvantaged neighbourhood residents. J. Soc. Pers. Relatsh. 2022, 39, 886–907. [Google Scholar] [CrossRef]
- Putnick, D.L.; Bell, E.M.; Ghassabian, A.; Mendola, P.; Sundaram, R.; Yeung, E.H. Maternal antenatal depression’s effects on child developmental delays: Gestational age, postnatal depressive symptoms, and breastfeeding as mediators. J. Affect. Disord. 2023, 324, 424–432. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Guo, X.W.; Song, Q.X.; Liang, Q.W.; Su, W.Y.; Li, N.; Ding, X.X.; Qin, Q.R.; Chen, M.C.; Sun, L.; et al. Adverse childhood experiences of emotional and physical abuse and emotional and behavioral problems: The mediating effects of family function and resilience. Psychol. Health Med. 2023, 28, 2121–2136. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; Dang, Q.; Zhang, B.; Wu, R.; Rasool, A. The effects of parenting differences on psychological resilience in adolescent students: The role of gratitude. Child. Youth Serv. Rev. 2021, 130, 106224. [Google Scholar] [CrossRef]
- Hock, E.S.; Blank, L.; Fairbrother, H.; Clowes, M.; Cuevas, D.C.; Booth, A.; Clair, A.; Goyder, E. Exploring the impact of housing insecurity on the health and wellbeing of children and young people in the United Kingdom: A qualitative systematic review. BMC Public Health 2024, 24, 2453. [Google Scholar] [CrossRef] [PubMed]
- De Sousa Machado, T.; Chur-Hansen, A.; Due, C. First-time mothers’ perceptions of social support: Recommendations for best practice. Health Psychol. Open 2020, 7, 2055102919898611. [Google Scholar] [CrossRef] [PubMed]
- Kay, T.L.; Moulson, M.C.; Vigod, S.N.; Schoueri-Mychasiw, N.; Singla, D.R. The Role of Social Support in Perinatal Mental Health and Psychosocial Stimulation. Yale J. Biol. Med. 2024, 97, 3–16. [Google Scholar] [CrossRef] [PubMed]
- United Nations Children’s Fund; World Health Organization; United Nations Educational, Scientific and Cultural Organization. Five Essential Pillars for Promoting and Protecting Mental Health and Psychosocial Well-Being in Schools and Learning Environments: A Briefing Note for National Governments. Available online: https://unesdoc.unesco.org/ark:/48223/pf0000384614 (accessed on 3 April 2025).
- Thomas, P.A.; Liu, H.; Umberson, D. Family Relationships and Well-Being. Innov. Aging 2017, 1, igx025. [Google Scholar] [CrossRef] [PubMed]
- Seeman, M.V. Grappling with Issues of Motherhood for Women with Schizophrenia. Healthcare 2023, 11, 2882. [Google Scholar] [CrossRef] [PubMed]
- Tuncer, G.Z.; Sarı, A.; Çetinkaya Duman, Z.; Taşkın, N. Domestic difficulties faced by women with a severe mental disorder: A qualitative study. Health Care Women Int. 2025, 46, 375–400. [Google Scholar] [CrossRef] [PubMed]
- Barker, E.D.; Copeland, W.; Maughan, B.; Jaffee, S.R.; Uher, R. Relative impact of maternal depression and associated risk factors on offspring psychopathology. Br. J. Psychiatry 2012, 200, 124–129. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-I.; Kim, S.M.; Park, S.J.; Song, J.; Lee, J.; Kim, K.H.; Park, S.M. Association of parental depression with adolescent children’s psychological well-being and health behaviors. BMC Public Health 2024, 24, 1412. [Google Scholar] [CrossRef] [PubMed]
- Wirehag Nordh, E.-L.; Grip, K.; Axberg, U. The patient and the family: Investigating parental mental health problems, family functioning, and parent involvement in child and adolescent mental health services (CAMHS). Eur. Child Adolesc. Psychiatry 2024. [Google Scholar] [CrossRef] [PubMed]
- Gillen, M.; Goodman, A.; Danaher, F.; Bosson, R.; Greenwald, M.; Jasrasaria, R. Intergenerational Trauma and Resilience among Im/Migrant Families: Child Mental Health Outcomes and Psychosocial Mechanisms of Transmission. Health 2024, 16, 888–920. [Google Scholar] [CrossRef]
- Stein, A.; Pearson, R.M.; Goodman, S.H.; Rapa, E.; Rahman, A.; McCallum, M.; Howard, L.M.; Pariante, C.M. Effects of perinatal mental disorders on the fetus and child. Lancet 2014, 384, 1800–1819. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, J.d.S.; Pastor-Valero, M.; Trambaiolli, L.R.; Bozzini, A.B.; Matijasevich, A. Impact of maternal depressive symptoms on offspring executive functions: A systematic review. Braz. J. Psychiatry 2024, 46, e20233387. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.J.; Lavigne, K.M.; Raucher-Chéné, D. Back to The Future: Linking Early Psychiatric Symptoms to Transdiagnostic Cognitive Impairments in At-Risk Youth from the Adolescent Brain Cognitive Development Study. arXiv 2024. [Google Scholar] [CrossRef]
- MacKenzie, L.E.; Howes Vallis, E.; Rempel, S.; Zwicker, A.; Drobinin, V.; Pavlova, B.; Uher, R. Cognition in offspring of parents with psychotic and non-psychotic severe mental illness. J. Psychiatr. Res. 2020, 130, 306–312. [Google Scholar] [CrossRef] [PubMed]
- di Giacomo, E.; Aliberti, F.; Colmegna, F.; Pescatore, F.; Clerici, M. The Burden of Intergenerational Transmission of Self-Threatening Behaviors in Adolescence; Elsevier B.V.: Amsterdam, The Netherlands, 2024. [Google Scholar] [CrossRef]
- Goldstein, T.R.; Obreja, M.; Shamseddeen, W.; Iyengar, S.; Axelson, D.A.; Goldstein, B.I.; Monk, K.; Hickey, M.B.; Sakolsky, D.; Kupfer, D.J.; et al. Risk for Suicidal Ideation Among the Offspring of Bipolar Parents: Results From the Bipolar Offspring Study (BIOS). Arch. Suicide Res. 2011, 15, 207–222. [Google Scholar] [CrossRef] [PubMed]
- Bertolín-Guillén, J.M. Salud mental intergeneracional. Rev. Neuro-Psiquiatr. 2023, 86, 35–44. [Google Scholar] [CrossRef]
- Labriola, M.; Lund, T.; Lindholdt, L. An intergenerational study of mental health among parents and adolescents. Eur. J. Public Health 2024, 34, ckae144.1100. [Google Scholar] [CrossRef]
- Sunde, H.F.; Eilertsen, E.M.; Kinge, J.M.; Kleppesto, T.H.; Nordmo, M.; Caspi, A.; Moffitt, T.E.; Torvik, F.A. Parental income and psychiatric disorders from age 10 to 40: A genetically informative population study. arXiv 2024. [Google Scholar] [CrossRef]
- Rasic, D.; Hajek, T.; Alda, M.; Uher, R. Risk of mental illness in offspring of parents with schizophrenia, bipolar disorder, and major depressive disorder: A meta-analysis of family high-risk studies. Schizophr. Bull. 2014, 40, 28–38. [Google Scholar] [CrossRef] [PubMed]
- McFarlane, E.; Burrell, L.; Duggan, A.; Tandon, D. Outcomes of a Randomized Trial of a Cognitive Behavioral Enhancement to Address Maternal Distress in Home Visited Mothers. Matern. Child Health J. 2017, 21, 475–484. [Google Scholar] [CrossRef] [PubMed]
- Wadephul, F.; Jones, C.; Jomeen, J. The Impact of Antenatal Psychological Group Interventions on Psychological Well-Being: A Systematic Review of the Qualitative and Quantitative Evidence. Healthcare 2016, 4, 32. [Google Scholar] [CrossRef] [PubMed]
- Sunde, H.F. Reproduction of Socioeconomic Differences and Mental Health Across Generations. Ph.D. Thesis, Department of Psychology, University of Oslo, Oslo, Norway, 2024. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).