Abstract
Cardiovascular events are the primary cause of mortality in patients with obstructive sleep apnea and obesity. The rising prevalence of obstructive sleep apnea in recent decades has been linked to increasing rates of obesity. Obstructive sleep apnea has also been linked with many different cardiovascular diseases including coronary artery disease, stroke, heart failure, hypertension, and atrial fibrillation. Obesity is an increasing health concern globally, in part because obesity complications such as hypertension, diabetes, and obstructive sleep apnea increase the risk of cardiovascular diseases. More than 10% weight loss may be required to prevent or reverse obesity complications. Treatment approaches to obesity include nutritional therapy, exercise therapy, pharmacotherapy, and surgical therapies. This review intends to identify the effects of weight loss on cardiovascular outcomes in patients with obesity and obstructive sleep apnea. Despite the strong association between cardiovascular diseases and obstructive sleep apnea, randomized trials have failed to demonstrate that treatment of obstructive sleep apnea reduces cardiovascular events, even in patients with established cardiovascular diseases. Weight loss in patients with obstructive sleep apnea improves HbA1c, systolic blood pressure, HDL cholesterol, and triglycerides, but thus far no changes in cardiovascular events have been shown. The combination of weight loss with continuous positive airway pressure (CPAP) appears more beneficial than either treatment in isolation. Large well-controlled trials in patients with obstructive sleep apnea to assess the effects of different weight reduction programs on cardiovascular disease are still needed.
1. Introduction
Obstructive sleep apnea is characterized by repetitive upper airway collapse during sleep resulting in a temporary cessation of breathing (apnea), shallow breathing (hypopnea), or respiratory-related arousals. The apnea–hypopnea index measures the number of apnea and hypopnea events per hour of sleep. The apnea–hypopnea index is used to further classify obstructive sleep apnea as mild (5 ≤ apnea–hypopnea index < 15), moderate (15 ≤ apnea–hypopnea index < 30), or severe (apnea–hypopnea index ≥ 30) [1]. The pathophysiology of obstructive sleep apnea is commonly believed to be primarily due to anatomical anomalies of the upper airway. While a defect in the upper airway anatomy is common, it is not the only pathogenic process at work. Anatomical and non-anatomical elements have been included in a novel model of obstructive sleep apnea pathogenesis. These non-anatomical aspects include (1) impairments in the upper airway dilator muscle function during sleep, (2) respiratory control instability, and (3) low respiratory arousal threshold [2].
Obstructive sleep apnea has a global prevalence of 13–33% in middle-aged men and 6–19% in middle-aged women [3]. The rising prevalence of obstructive sleep apnea in the recent decades has been linked to increasing rates of obesity [4]. Obstructive sleep apnea has been linked with many different cardiovascular diseases including hypertension, stroke, heart failure, coronary artery disease, and atrial fibrillation [5,6]. Adults with obstructive sleep apnea, in addition to increased risk of developing cardiovascular disease, also have worse cardiovascular outcomes [7]. We reviewed the associations between obstructive sleep apnea and cardiovascular disease and whether weight loss may improve the cardiovascular outcomes of patients with obstructive sleep apnea and obesity.
2. Obstructive Sleep Apnea Increases the Risk Factors of Cardiovascular Disease
Among the mechanisms which explain the association between obstructive sleep apnea and myocardial infarction (MI), common risk factors include male sex, age, hypertension, obesity, and smoking [8]. However, other direct effects of obstructive sleep apnea merit consideration. The combination of repetitive apnea–hypopnea, hypoxia, and arousal from sleep increases sympathetic activity, which is maintained during wakefulness, thus increasing myocardial oxygen demand [9]. The mechanistic understanding which connects obstructive sleep apnea and cardiovascular disease is poorly understood due to the diverse and complicated elements of obstructive sleep apnea and the multiple other comorbid conditions (especially obesity) impacting cardiovascular health. When obstructive apnea or hypopnea occurs, the upper airway collapses throughout sleep, affecting a complete or partial interruption of airflow even with sustained respiratory struggle. The sympathetic tone is stimulated, and respiratory work increases as opposed to the closed upper airway, increasing negative intrathoracic pressure. Stimulation of the sympathetic tone across the parasympathetic system affects heart rate and blood pressure [10]. Awakening from sleep terminates the asphyxia event, with re-establishing airflow and re-oxygenation but further increased sympathetic tone. Obstructive sleep apnea seems to be correlated with increased levels of inflammatory cytokines. Furthermore, metabolic dysregulation is observed in obstructive sleep apnea patients (with abnormalities in both fat and glucose metabolism. This contributes to atherosclerosis and endothelial damage with enhanced arterial stiffness. However, it remains unclear whether metabolic abnormalities and inflammation are exacerbated by obstructive sleep apnea, whether these are epiphenomena are due to obesity [10].
2.1. Hypertension
Obstructive sleep apnea is common in middle-aged and older people, although hypertension is also prevalent among middle-aged and older people. This increases the chance of significant complications between hypertension and obstructive sleep apnea. The level of the complications of hypertension and obstructive sleep apnea is significantly greater than expected. Hypertension is prevalent in patients with obstructive sleep apnea and contributes to vascular injury and cardiovascular events. Several pathophysiologic mechanisms contribute to the increased risk of hypertension in individuals with obstructive sleep apnea, including upregulation of neurohormonal pathways, endothelial dysfunction, and inflammation [6]. Although patients with obstructive sleep apnea have a higher incidence of hypertension [11], the inverse is also true because patients with hypertension are more likely to experience sleep-disordered breathing, especially those who have failed to respond to traditional treatment. Up to 84% of this subset of patients may have undetected obstructive sleep apnea [12].
Animal experiments have provided direct proof that obstructive sleep apnea causes hypertension. When obstructive sleep apnea is induced, it results in acute transient rises in nighttime blood pressure and ultimately culminates in persistent daytime hypertension [11]. When blood pressure is strictly regulated in rats, it also decreases sleep apneas [13].
In humans, a causal link between obstructive sleep apnea and hypertension has not been established because variables such as age and obesity confound the association. However, epidemiological data suggest that hypertension was found in approximately 50% of patients with obstructive sleep apnea (7).
2.2. Dyslipidemia
Obstructive sleep apnea is commonly associated with elevated plasma triglycerides, low-density lipoprotein cholesterol (LDL-c), and total cholesterol. Moreover, the reduction in high-density lipoprotein (HDL) may, in part, be due to deleterious oxidative processes commonly found in patients with obstructive sleep apnea [14,15,16]. The effect of treating obstructive sleep apnea in children with adenotonsillectomy is variable as regards the impact on lipid profiles [17] because chronic intermittent hypoxia may affect both lipid biosynthesis and lipid peroxidation [18].
2.3. Type 2 Diabetes
Inflammation in patients with type 2 diabetes is characterized by elevated levels of proinflammatory cytokines or a rising number of white blood cells in the blood or tissue. Stimulation of the inflammatory process often indicates abnormalities such as tissue injury and organ dysfunction. Obesity might cause chronic low-grade inflammation and hat is involved in type 2 diabetes. In addition, adipose-specific cytokines (leptin adiponectin, leptin, and interleukin 6 (IL-6)) are secreted by visceral adipocytes and inflammatory cytokines (tumor necrosis factor α (TNF-α)). An elevated amount of fatty tissue draining into the chemokines, portal vein, and IL-6 production can induce liver and systemic insulin resistance [19,20]. Although obesity is a serious risk factor for type 2 diabetes mellitus, coexistent severe obstructive sleep apnea may independently add to the risk. The relationship between intermittent hypoxia and insulin resistance [21] has been assessed by evaluating the effect of hypoxia–reoxygenation cycles on insulin target tissues. Rodent models suggest that chronic exposure to intermittent hypoxia induces insulin resistance [22].
2.4. Atrial Fibrillation
Obstructive sleep apnea is a common risk factor for atrial fibrillation [23]. Recurrent episodes of obstructive sleep apnea may lead to cardiac structural and electric remodeling. Repetitive episodes of obstructive sleep apnea in an animal model can cause atrial fibrosis and important changes in connexin-43 distribution and expression, thus leading to slow atrial conduction. This increases the vulnerability to arrhythmias, including atrial fibrillation [24]. Furthermore, untreated obstructive sleep apnea doubles the risk of recurrence of atrial fibrillation in patients after electrical cardioversion. Treatment of obstructive sleep apnea with CPAP attenuates the risk of atrial fibrillation [25]. Obstructive sleep apnea shares many common risk factors with atrial fibrillation. The prevalence of both atrial fibrillation and obstructive sleep apnea is rising due to increases in obesity and cardiovascular disease. The close association between obstructive sleep apnea and cardiovascular disease, and atrial fibrillation and cardiovascular disease may obscure a directly causal relationship between atrial fibrillation and obstructive sleep apnea. The interplay of the pathophysiology of these chronic diseases is complex and likely bidirectional. Obstructive sleep apnea may contribute to atrial fibrillation, and, in turn, atrial fibrillation promotes the development of obstructive sleep apnea. Nonetheless, these entities are associated with one another, independently of other cardiovascular diseases [26].
2.5. Heart Failure
Sleep apnea is predictable in patients with heart failure, with a prevalence of between 50% and 70% [27]. Mainly, central sleep apnea accounts for two-thirds of the sleep apnea cases in this population, while obstructive sleep apnea is less frequent. Central sleep apnea is a frequent concomitant finding in patients with severely impaired cardiac function [27]. Another study aimed to assess the prevalence of sleep-disordered breathing and its associated risk factors in French patients with heart failure showed that 30% of syndromes were classified as central and 70% as obstructive [28]. Coexisting sleep apnea in patients with heart failure has been associated with an increased risk of adverse outcomes, including mortality [29]. Several pathophysiological processes resulting from apneic events may explain this association. These involve stimulation of the sympathetic nervous system [30] and increased preload and afterload resulting from perturbation of intrathoracic pressure while struggling to inspire against blocked airways [31]. Worsening hypertension, increased risk of arrhythmias including sudden cardiac death [32], and myocardial infarctions [33] are other mechanisms by which sleep apnea may worsen outcomes in patients with heart failure [34].
The relationship between obstructive sleep apnea and cardiovascular events remains unclear. A systematic review and meta-analysis conducted by Loke, Yoon K., et al. suggested that obstructive sleep apnea may be an independent risk factor for cardiovascular, stroke, and overall mortality. Due to imprecision and inconsistencies in the data, the strength of potential association between obstructive sleep apnea and ischemic heart disease remains unclear [35]. A cohort study evaluating the relationship between obstructive sleep apnea-related variables and the risk of CV events revealed that several obstructive sleep apnea-related factors other than the apnea–hypopnea index were important predictors of a composite CV outcome [36]. Hence, the need for a randomized controlled trial is crucial.
3. Continuous Positive Airway Pressure (CPAP) Reduces Risk Factors for Myocardial Infarction, Atrial Fibrillation, and Heart Failure
Randomized controlled trials demonstrated that CPAP lowers blood pressure by 2–3 mm Hg [37]. Among patients with obstructive sleep apnea and resistant hypertension, CPAP treatment for 12 weeks decreased the 24 h mean and diastolic blood pressure and increased the nocturnal blood pressure [38]. CPAP also improved dyslipidemia (decrease in total cholesterol and LDL and increase in HDL). This may contribute to a potential reduction in cardiovascular and cerebrovascular events [39]. In patients with moderate-to-severe obstructive sleep apnea, compliant CPAP usage may improve insulin secretion and insulin resistance. The latter was associated with an improvement in leptin even after short-term CPAP therapy [40,41].
Both epidemiological studies and cohort studies suggest that CPAP reduces atrial fibrillation recurrence risk after cardioversion and ablation [42,43]. In 426 individuals undergoing pulmonary vein isolation, 62 patients with verified obstructive sleep apnea who used CPAP had a higher rate of atrial fibrillation-free survival than those who did not use CPAP (72% vs. 37%). The atrial fibrillation-free survival rate among CPAP users was comparable to that of individuals without obstructive sleep apnea. However, randomized controlled trials are still awaited [44]. Not surprisingly, given the association between obstructive sleep apnea and atrial fibrillation, there is also an association between obstructive sleep apnea and stroke [45,46]. CPAP may attenuate this risk [46], but this has not been studied prospectively.
4. CPAP Does Not Reduce Myocardial Infarction
The potential associations of CPAP to reduce composite cardiovascular events, all-cause, and cardiovascular death in patients with concomitant cardiovascular disease and obstructive sleep apnea rely on data from observational studies [47]. There is currently no level 1 evidence to suggest that CPAP can prevent future cardiovascular events in patients, including obstructive sleep apnea and coronary artery disease [48]. A randomized controlled trial that studied the impact of CPAP on cardiovascular outcomes showed no reduction in long-term adverse cardiovascular outcomes in the intention-to-treat population [49]. A clinical trial comparing usual care with usual care plus CPAP therapy found that the addition of CPAP did not prevent cardiovascular events in patients with moderate-to-severe obstructive sleep apnea and preexisting cardiovascular disease [50]. However, no significant beneficial effects of CPAP were shown in patients with obstructive sleep apnea in the trials evaluating CPAP therapy on major adverse cardiovascular events [49,50,51]. CPAP did not reduce the rate of complex cardiovascular events at a median follow-up of 3.7 years in the SAVE (Sleep Apnea Cardiovascular Endpoints) trial that randomized 2717 participants with cerebrovascular disease with moderate-to-severe obstructive sleep apnea or [50]. Furthermore, no effect of CPAP therapy on major adverse cardiovascular events in obstructive sleep apnea with or without cardiovascular morbidities was shown in several meta-analyses of randomized trials [52,53,54]. However, the study populations of the included studies are diverse, from the general population to patients with severe coronary artery disease (such as myocardial infarction), thus precluding definitive conclusions.
5. Obesity
Obesity is a chronic multifactorial disease. Obesity is caused by inherited biological and ecological factors, diet, physical activity, and exercise choices. It is a medical problem that raises the threat of other diseases and health problems, such as high blood pressure, certain cancers, diabetes, and heart disease [55].
Various risk factors, involving obesity, age, sex, heritable and race/ethnicity factors, are well-known in the pathogenesis of sleep apnea. However, obesity has usually been known to be one of the most significant sleep apnea risk factors [56]. Some cross-sectional experiments have always found a connection between the obstructed sleep apnea risk and body mass index. The registered prevalence of sleep apnea ranges from 40% to 90% in individuals with a body mass index > 40 kg/m2 (severe obesity) [57,58]. Significant sleep apnea appears in over 70% of sleep apnea patients with obesity and 40% of people with obesity [59].
Obesity is the only major obstructive sleep apnea risk factor that is variable. Weight decrease in the short term of one to two years steer to better metabolic control in patients with obstructive sleep apnea [60]. A prospective study of Wisconsin citizens indicated that a 10% weight loss anticipated a 26% reduction in the sleep apnea severity apnea–hypopnea index [58]. Moreover, another cohort research observed decreased apnea occurrence after weight loss [61]. Even though the mechanisms by which weight loss decrease obstructive sleep apnea symptoms are not entirely understood, factors such as decreased visceral fat deposition play an important role [62]. Airway structures and altered neurophysiologic control of respiration during weight loss are likely also important [63]. Moreover, obesity may control the chemoreflex function through neurohormonal mediators such as leptin, which reduces when sleep apnea patients lose weight [60]. Therefore, these potential methods likely work in concert to act as a vicious cycle in the body weight gain pathogenesis and obstructive sleep apnea (Figure 1).
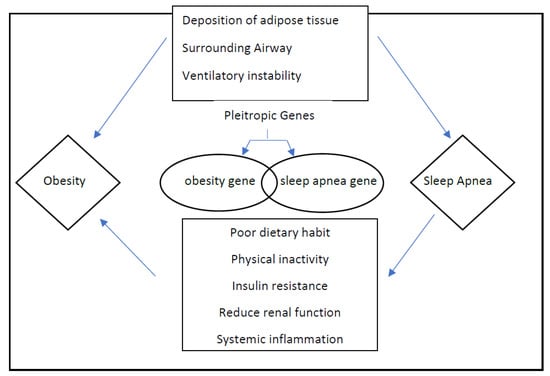
Figure 1.
Proposed mechanisms acting as a vicious cycle in the pathogenesis of obstructive sleep apnea and obesity and the potential influences of shared and non-shared genes.
Obesity complications such as hypertension, diabetes, insulin resistance, and obstructive sleep apnea increase the risk of cardiovascular diseases [64]. Obesity may also independently contribute to atherosclerosis and coronary artery disease [47,65,66,67]. To prevent or reverse obesity complications, more than 10% weight loss may be required [68], and the previously suggested 5% to 10% weight loss may not be sufficient [69,70].
In the case of obesity, evaluation before the intervention should include a comprehensive weight history, a complete individual and family medical history, blood studies, a physical examination looking for signs of the complications of obesity, and a behavioral history [71]. This approach may identify primary causes for weight gain, such as an endocrine disorder, medications linked with weight gain, an underlying eating disorder, or differences in the condition that have led to decreased activity and an energy imbalance. Body mass index and waist circumference should also be included in this initial evaluation. Blood tests should consist of a measurement of thyroid function, insulin sensitivity, liver function, and lipid profile [71]. Once a diagnosis of obesity has been made, the management of obesity should be stratified. Treatment approaches for obesity include nutritional therapy, pharmacotherapy, and surgical therapies, as shown in Table 1 [72].

Table 1.
Treatment options of obesity.
5.1. Weight Loss as a Treatment to Reduce Cardiovascular Events
Currently, no randomized control trials have shown that intentional weight loss reduces the cardiovascular death risk [73,74,75]. Non-randomized long-term follow-up data from a prospective cohort Swedish Obese Subjects study showed that bariatric surgery resulted in reduced cardiovascular mortality and occurrence of first-time (fatal and nonfatal) cardiovascular events [76]. The Look AHEAD clinical trial was designed to assess the long-term effects of nutritional therapy and exercise therapy delivered over ten years in patients with obesity and type 2 diabetes. The primary outcome was time to the incidence of a major cardiovascular disease event. The study revealed that weight loss produced improvements in HbA1c, systolic blood pressure, HDL triglycerides, and cholesterol at years 1 and 4 (all p ≤ 0.02) [77], but no changes in cardiovascular events over ten years [77]. However, the subgroup of patients who lost more than 10% of their weight did have a reduction in mortality [78]. Another two-year follow-up cohort study also demonstrated that 5–10% weight loss improves risk factors but not cardiovascular events [79].
5.2. Weight Loss as a Treatment for Obstructive Sleep Apnea
Although weight loss can facilitate obstructive sleep apnea treatment, it can rarely cure it and still requires a combination with continuous positive airway pressure [80]. A systematic review and meta-analysis conducted to assess the effect of lifestyle therapy on the oxygen desaturation index, apnea–hypopnea index, and excessive daytime sleepiness among adults revealed significant reductions in all these components after weight loss. However, most patients still had diagnosable obstructive sleep apnea [81]. The SCALE sleep apnea study compared the effects of 3.0 mg liraglutide to placebo on obstructive sleep apnea severity and body weight loss in patients with obstructive sleep apnea and obesity. This study showed that 3.0 mg liraglutide produced greater reductions in ischemic heart disease, body weight, systolic blood pressure, and HbA1c in patients with obesity with moderate/severe obstructive sleep apnea, but most patients still had diagnosable obstructive sleep apnea at the end of the study [82]. A prospective multicenter study investigated the effects of a laparoscopic Roux–en–Y gastric bypass. One year after surgery, the prevalence of obstructive sleep apnea decreased, but more than half of those with obstructive sleep apnea at baseline still had it after surgery. Obstructive sleep apnea was cured in 45% and improved in another 33% of the patients, but moderate or severe obstructive sleep apnea persisted in 20% of the patients after the operation [83]. A recent prospective cohort study showed that patients with moderate-to-severe obstructive sleep apnea may lose less weight with bariatric surgery than those with milder disease [84]. A systematic review included 19 surgical (n = 525), and 20 nonsurgical (n = 825) studies assessing the body mass index and the apnea–hypopnea index before and after intervention [85]. The results showed that bariatric surgery and non-surgical weight loss both had beneficial effects on obstructive sleep apnea through body mass index and apnea–hypopnea index reduction. However, bariatric surgery may result in a significantly greater improvement in the body mass index and the apnea–hypopnea index than nonsurgical alternatives [85]. The exact relationship between bariatric surgery and nonsurgical weight loss interventions in OSA resolution remains a challenge due to the need in randomized controlled trials [85].
5.3. Weight Loss as a Treatment to Reduce Cardiovascular Events in Patients with Obstructive Sleep Apnea
Cardiovascular events are the primary cause of mortality in patients with obstructive sleep apnea and obesity [86]. CPAP combined with weight loss may improve obstructive sleep apnea pathophysiology and the apnea–hypopnea index and reduce cardiovascular risk [87,88]. A randomized 24-week trial on 181 patients with moderate to severe obstructive sleep apnea and obesity comparing the effects of CPAP, weight loss, or combined CPAP and weight loss was conducted. Combining CPAP and weight loss did not reduce CRP levels more than either intervention alone. Weight loss provided an incremental reduction in serum triglycerides and the insulin resistance level when combined with CPAP. Weight loss and CPAP did incrementally reduce blood pressure compared with either intervention alone [89]. Another randomized control trial of 42 patients with obesity, severe obstructive sleep apnea (apnea–hypopnea index > 30 events/h) and treated with CPAP for a minimum of 6 months before the study allocated patients to an intensive weight loss program or standard lifestyle recommendations over 12 months. The effect of weight loss was assessed on obstructive sleep apnea severity and metabolic variables. The intensive weight loss program effectively reduces weight and obstructive sleep apnea severity while also improving lipid profiles, glycemic control, and inflammatory markers [90]. The authors concluded that weight loss intervention is an effective strategy to improve cardiovascular risk in patients with obesity and obstructive sleep apnea [66], but whether this will reduce cardiovascular events remains determined. Table 2 summarizes the available data assessing the effect of weight loss as a treatment for cardiovascular events risk reduction, obstructive sleep apnea, and to reduce cardiovascular events in patients with obstructive sleep apnea. This potential relationship is plausible because of prevailing pathophysiological mechanisms, but definitive evidence is still lacking. There is evidence that treatment with CPAP decreases blood pressure, but the impact of weight loss in patients with resistant hypertension is more profound than in those with acute obstructive sleep apnea. Current data supporting the impact of CPAP on cardiovascular events come from nonrandomized studies, and higher-quality evidence is needed to change clinical practice. We also require using the concept of individualized medicine for this matter and focusing on genetic variations and why a few patients with OSA develop cardiovascular effects while others do not. Such research will assist in reporting on the clinical trials that are required to be performed. Weight loss in patients with obstructive sleep apnea produced improvements in HbA1c, systolic blood pressure, HDL cholesterol, and triglycerides, but thus far, no changes in cardiovascular events have been shown. This will require cooperation among specialists in cardiology and sleep apnea.

Table 2.
Summary of weight loss as a treatment for cardiovascular events risk reduction, obstructive sleep apnea and to reduce cardiovascular events in patients with obstructive sleep apnea.
6. Conclusions
Despite the association between cardiovascular disease and obstructive sleep apnea, randomized trials have failed to demonstrate that obstructive sleep apnea treatment improves the outcomes of cardiovascular events, even in patients with established cardiovascular disease [50]. The combination of weight loss with continuous positive airway pressure (CPAP) appears to be more helpful than either treatment in isolation. Large well-controlled trials in patients with obstructive sleep apnea to evaluate the impact of different weight reduction programs on cardiovascular disease are still required.
Author Contributions
A.A. wrote the original draft manuscript, H.A. wrote, reviewed, and edited the manuscript, J.G. reviewed and edited the manuscript, and C.W.l.R. reviewed and edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
A.A., H.A., and J.G. declare no conflict of interest. C.W.l.R. reports grants from the Irish Research Council, Science Foundation Ireland, Anabio, and the Health Research Board. He served on advisory boards of NovoNordisk, Herbalife, GI Dynamics, Eli Lilly, Johnson and Johnson, Sanofi Aventis, Astra Zeneca, Janssen, Bristol-Myers Squibb, Keyron, and Boehringer-Ingelheim, outside the area of work commented on here.
References
- Wang, S.; Li, S.; Wang, B.; Liu, J.; Tang, Q. Matrix metalloproteinase-9 is a predictive factor for systematic hypertension and heart dysfunction in patients with obstructive sleep apnea syndrome. BioMed Res. Int. 2018, 2018, 1569701. [Google Scholar] [CrossRef] [PubMed]
- Eckert, D.J.; White, D.P.; Jordan, A.S.; Malhotra, A.; Wellman, A. Defining phenotypic causes of obstructive sleep apnea. Identification of novel therapeutic targets. Am. J. Respir. Crit. Care Med. 2013, 188, 996–1004. [Google Scholar] [CrossRef] [PubMed]
- Senaratna, C.V.; Perret, J.L.; Lodge, C.J.; Lowe, A.J.; Campbell, B.E.; Matheson, M.C.; Hamilton, G.S.; Dharmage, S.C. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Med. Rev. 2017, 34, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Young, T.; Peppard, P.E.; Taheri, S. Excess weight and sleep-disordered breathing. J. Appl. Physiol. 2005, 99, 1592–1599. [Google Scholar] [CrossRef]
- Shahar, E.; Whitney, C.W.; Redline, S.; Lee, E.T.; Newman, A.B.; Javier Nieto, F.; O’CONNOR, G.T.; Boland, L.L.; Schwartz, J.E.; Samet, J.M. Sleep-disordered breathing and cardiovascular disease: Cross-sectional results of the Sleep Heart Health Study. Am. J. Respir. Crit. Care Med. 2001, 163, 19–25. [Google Scholar] [CrossRef]
- Peppard, P.E.; Young, T.; Palta, M.; Skatrud, J. Prospective study of the association between sleep-disordered breathing and hypertension. N. Engl. J. Med. 2000, 342, 1378–1384. [Google Scholar] [CrossRef]
- Johnson, K.G.; Johnson, D.C. Frequency of sleep apnea in stroke and TIA patients: A meta-analysis. J. Clin. Sleep Med. 2010, 6, 131–137. [Google Scholar] [CrossRef]
- Nieto, F.J.; Young, T.B.; Lind, B.K.; Shahar, E.; Samet, J.M.; Redline, S.; D’agostino, R.B.; Newman, A.B.; Lebowitz, M.D.; Pickering, T.G. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. JAMA 2000, 283, 1829–1836. [Google Scholar] [CrossRef]
- Spaak, J.; Egri, Z.; Kubo, T. Increased daytime muscle sympathetic nerve activity in heart failure patients with sleep apnea. Hypertension 2005, 46, 1327–1332. [Google Scholar] [CrossRef]
- Young, T.; Skatrud, J.; Peppard, P.E. Risk factors for obstructive sleep apnea in adults. JAMA 2004, 291, 2013–2016. [Google Scholar] [CrossRef]
- Brooks, D.; Horner, R.L.; Kozar, L.F.; Render-Teixeira, L.C.; Phillipson, E.A. Obstructive sleep apnea as a cause of systemic hypertension. Evidence from a canine model. J. Clin. Investig. 1997, 99, 106–109. [Google Scholar] [CrossRef] [PubMed]
- Torres, G.; Sánchez-de-la-Torre, M.; Barbé, F. Relationship between OSA and hypertension. Chest 2015, 148, 824–832. [Google Scholar] [CrossRef] [PubMed]
- Carley, D.W.; Trbovic, S.M.; Radulovacki, M. Hydralazine reduces elevated sleep apnea index in spontaneously hypertensive (SHR) rats to equivalence with normotensive Wistar-Kyoto rats. Sleep 1996, 19, 363–366. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Li, J.; Savransky, V.; Nanayakkara, A.; Smith, P.L.; O’Donnell, C.P.; Polotsky, V.Y. Hyperlipidemia and lipid peroxidation are dependent on the severity of chronic intermittent hypoxia. J. Appl. Physiol. 2007, 102, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Malakasioti, G.; Alexopoulos, E.; Befani, C.; Tanou, K.; Varlami, V.; Ziogas, D.; Liakos, P.; Gourgoulianis, K.; Kaditis, A.G. Oxidative stress and inflammatory markers in the exhaled breath condensate of children with OSA. Sleep Breath. 2012, 16, 703–708. [Google Scholar] [CrossRef]
- Vatansever, E.; Surmen-Gur, E.; Ursavas, A.; Karadag, M. Obstructive sleep apnea causes oxidative damage to plasma lipids and proteins and decreases adiponectin levels. Sleep Breath. 2011, 15, 275–282. [Google Scholar] [CrossRef]
- Gozal, D.; Capdevila, O.S.; Kheirandish-Gozal, L. Metabolic alterations and systemic inflammation in obstructive sleep apnea among nonobese and obese prepubertal children. Am. J. Respir. Crit. Care Med. 2008, 177, 1142–1149. [Google Scholar] [CrossRef]
- Li, J.; Grigoryev, D.N.; Ye, S.Q.; Thorne, L.; Schwartz, A.R.; Smith, P.L.; O’Donnell, C.P.; Polotsky, V.Y. Chronic intermittent hypoxia upregulates genes of lipid biosynthesis in obese mice. J. Appl. Physiol. 2005, 99, 1643–1648. [Google Scholar] [CrossRef]
- Ota, T. Obesity-induced inflammation and insulin resistance. Front. Media SA 2015, 4, 93. [Google Scholar]
- Coppack, S.W. Pro-inflammatory cytokines and adipose tissue. Proc. Nutr. Soc. 2001, 60, 349–356. [Google Scholar] [CrossRef]
- Iiyori, N.; Alonso, L.C.; Li, J.; Sanders, M.H.; Garcia-Ocana, A.; O’Doherty, R.M.; Polotsky, V.Y.; O’Donnell, C.P. Intermittent hypoxia causes insulin resistance in lean mice independent of autonomic activity. Am. J. Respir. Crit. Care Med. 2007, 175, 851–857. [Google Scholar] [CrossRef] [PubMed]
- Polak, J.; Shimoda, L.A.; Drager, L.F.; Undem, C.; McHugh, H.; Polotsky, V.Y.; Punjabi, N.M. Intermittent hypoxia impairs glucose homeostasis in C57BL6/J mice: Partial improvement with cessation of the exposure. Sleep 2013, 36, 1483–1490. [Google Scholar] [CrossRef] [PubMed]
- Dalgaard, F.; North, R.; Pieper, K.; Fonarow, G.C.; Kowey, P.R.; Gersh, B.J.; Mahaffey, K.W.; Pokorney, S.; Steinberg, B.A.; Naccarrelli, G. Risk of major cardiovascular and neurologic events with obstructive sleep apnea among patients with atrial fibrillation. Am. Heart J. 2020, 223, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, Y.-k.; Kato, T.; Xiong, F.; Shi, Y.-F.; Naud, P.; Maguy, A.; Mizuno, K.; Tardif, J.-C.; Comtois, P.; Nattel, S. Atrial fibrillation promotion with long-term repetitive obstructive sleep apnea in a rat model. J. Am. Coll. Cardiol. 2014, 64, 2013–2023. [Google Scholar] [CrossRef]
- Kanagala, R.; Murali, N.S.; Friedman, P.A.; Ammash, N.M.; Gersh, B.J.; Ballman, K.V.; Shamsuzzaman, A.S.M.; Somers, V.K. Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation 2003, 107, 2589–2594. [Google Scholar] [CrossRef]
- Marulanda-Londono, E.; Chaturvedi, S. The interplay between obstructive sleep apnea and atrial fibrillation. Front. Neurol. 2017, 8, 668. [Google Scholar] [CrossRef]
- Oldenburg, O.; Lamp, B.; Faber, L.; Teschler, H.; Horstkotte, D.; Töpfer, V. Sleep-disordered breathing in patients with symptomatic heart failure A contemporary study of prevalence in and characteristics of 700 patients. Eur. J. Heart Fail. 2007, 9, 251–257. [Google Scholar] [CrossRef]
- Paulino, A.; Damy, T.; Margarit, L.; Stoïca, M.; Deswarte, G.; Khouri, L.; Vermes, E.; Meizels, A.; Hittinger, L.; d’Ortho, M.-P. Prevalence of sleep-disordered breathing in a 316-patient French cohort of stable congestive heart failure. Arch. Cardiovasc. Dis. 2009, 102, 169–175. [Google Scholar] [CrossRef]
- Oldenburg, O.; Wellmann, B.; Buchholz, A.; Bitter, T.; Fox, H.; Thiem, U.; Horstkotte, D.; Wegscheider, K. Nocturnal hypoxaemia is associated with increased mortality in stable heart failure patients. Eur. Heart J. 2016, 37, 1695–1703. [Google Scholar] [CrossRef]
- Leung, R.S. Sleep-disordered breathing: Autonomic mechanisms and arrhythmias. Prog. Cardiovasc. Dis. 2009, 51, 324–338. [Google Scholar] [CrossRef]
- Bradley, T.D.; Hall, M.J.; Ando, S.; Floras, J.S. Hemodynamic effects of simulated obstructive apneas in humans with and without heart failure. Chest 2001, 119, 1827–1835. [Google Scholar] [CrossRef] [PubMed]
- Gami, A.S.; Olson, E.J.; Shen, W.K.; Wright, R.S.; Ballman, K.V.; Hodge, D.O.; Herges, R.M.; Howard, D.E.; Somers, V.K. Obstructive sleep apnea and the risk of sudden cardiac death: A longitudinal study of 10,701 adults. J. Am. Coll. Cardiol. 2013, 62, 610–616. [Google Scholar] [CrossRef] [PubMed]
- Peker, Y.; Carlson, J.; Hedner, J. Increased incidence of coronary artery disease in sleep apnoea: A long-term follow-up. Eur. Respir. J. 2006, 28, 596–602. [Google Scholar] [CrossRef] [PubMed]
- Logan, A.; Tkacova, R.; Perlikowski, S.; Leung, R.; Tisler, A.; Floras, J.; Bradley, T. Refractory hypertension and sleep apnoea: Effect of CPAP on blood pressure and baroreflex. Eur. Respir. J. 2003, 21, 241–247. [Google Scholar] [CrossRef]
- Loke, Y.K.; Brown, J.W.L.; Kwok, C.S.; Niruban, A.; Myint, P.K. Association of obstructive sleep apnea with risk of serious cardiovascular events: A systematic review and meta-analysis. Circ. Cardiovasc. Qual. Outcomes 2012, 5, 720–728. [Google Scholar] [CrossRef]
- Kendzerska, T.; Gershon, A.S.; Hawker, G.; Leung, R.S.; Tomlinson, G. Obstructive sleep apnea and risk of cardiovascular events and all-cause mortality: A decade-long historical cohort study. PLoS Med. 2014, 11, e1001599. [Google Scholar] [CrossRef]
- Fava, C.; Dorigoni, S.; Dalle Vedove, F.; Danese, E.; Montagnana, M.; Guidi, G.; Narkiewicz, K.; Minuz, P. Effect of continuous positive airway pressure (CPAP) on blood pressure in patients with obstructive sleep apnea/hypopnea. A systematic review and meta-analysis. Chest 2013, 26, 13–1115. [Google Scholar]
- Martínez-García, M.-A.; Capote, F.; Campos-Rodríguez, F.; Lloberes, P.; Díaz de Atauri, M.J.; Somoza, M.; Masa, J.F.; González, M.; Sacristán, L.; Barbé, F.; et al. Effect of CPAP on Blood Pressure in Patients with Obstructive Sleep Apnea and Resistant Hypertension: The HIPARCO Randomized Clinical Trial. JAMA 2013, 310, 2407–2415. [Google Scholar] [CrossRef]
- Nadeem, R.; Singh, M.; Nida, M.; Kwon, S.; Sajid, H.; Witkowski, J.; Pahomov, E.; Shah, K.; Park, W.; Champeau, D. Effect of CPAP treatment for obstructive sleep apnea hypopnea syndrome on lipid profile: A meta-regression analysis. J. Clin. Sleep Med. 2014, 10, 1295–1302. [Google Scholar] [CrossRef]
- Çuhadaroğlu, Ç.; Utkusavaş, A.; Öztürk, L.; Salman, S.; Ece, T. Effects of Nasal CPAP Treatment on Insulin Resistance, Lipid Profile, and Plasma Leptin in Sleep Apnea. Lung 2019, 187, 75–81. [Google Scholar] [CrossRef]
- Kapsimalis, F.; Varouchakis, G.; Manousaki, A.; Daskas, S.; Nikita, D.; Kryger, M.; Gourgoulianis, K. Association of Sleep Apnea Severity and Obesity with Insulin Resistance, C-Reactive Protein, and Leptin Levels in Male Patients with Obstructive Sleep Apnea. Lung 2008, 186, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Neilan, T.G.; Farhad, H.; Dodson, J.A.; Shah, R.V.; Abbasi, S.A.; Bakker, J.P.; Michaud, G.F.; van der Geest, R.; Blankstein, R.; Steigner, M. Effect of sleep apnea and continuous positive airway pressure on cardiac structure and recurrence of atrial fibrillation. J. Am. Heart Assoc. 2013, 2, e000421. [Google Scholar] [CrossRef] [PubMed]
- Fein, A.S.; Shvilkin, A.; Shah, D.; Haffajee, C.I.; Das, S.; Kumar, K.; Kramer, D.B.; Zimetbaum, P.J.; Buxton, A.E.; Josephson, M.E. Treatment of obstructive sleep apnea reduces the risk of atrial fibrillation recurrence after catheter ablation. J. Am. Coll. Cardiol. 2013, 62, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Schoch, O.D.; Baty, F.; Niedermann, J.; Rüdiger, J.J.; Brutsche, M.H. Baseline predictors of adherence to positive airway pressure therapy for sleep apnea: A 10-year single-center observational cohort study. Respiration 2014, 87, 121–128. [Google Scholar] [CrossRef]
- Yaggi, H.K.; Concato, J.; Kernan, W.N.; Lichtman, J.H.; Brass, L.M.; Mohsenin, V. Obstructive sleep apnea as a risk factor for stroke and death. N. Engl. J. Med. 2005, 353, 2034–2041. [Google Scholar] [CrossRef]
- Campos-Rodriguez, F.; Martinez-Garcia, M.A.; Reyes-Nuñez, N.; Caballero-Martinez, I.; Catalan-Serra, P.; Almeida-Gonzalez, C.V. Role of sleep apnea and continuous positive airway pressure therapy in the incidence of stroke or coronary heart disease in women. Am. J. Respir. Crit. Care Med. 2014, 189, 1544–1550. [Google Scholar] [CrossRef]
- Marin, J.M.; Carrizo, S.J.; Vicente, E.; Agusti, A.G. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: An observational study. Lancet 2005, 365, 1046–1053. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, Y.; Dong, Z.; Fan, J.; Nie, S.; Wei, Y. Effect of continuous positive airway pressure on long-term cardiovascular outcomes in patients with coronary artery disease and obstructive sleep apnea: A systematic review and meta-analysis. Respir. Res. 2018, 19, 61. [Google Scholar] [CrossRef]
- Peker, Y.; Glantz, H.; Eulenburg, C.; Wegscheider, K.; Herlitz, J.; Thunström, E. Effect of positive airway pressure on cardiovascular outcomes in coronary artery disease patients with nonsleepy obstructive sleep apnea. The RICCADSA randomized controlled trial. Am. J. Respir. Crit. Care Med. 2016, 194, 613–620. [Google Scholar] [CrossRef]
- McEvoy, R.D.; Antic, N.A.; Heeley, E.; Luo, Y.; Ou, Q.; Zhang, X.; Mediano, O.; Chen, R.; Drager, L.F.; Liu, Z. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N. Engl. J. Med. 2016, 375, 919–931. [Google Scholar] [CrossRef]
- Barbé, F.; Durán-Cantolla, J.; Sánchez-de-la-Torre, M.; Martínez-Alonso, M.; Carmona, C.; Barceló, A.; Chiner, E.; Masa, J.F.; Gonzalez, M.; Marin, J.M. Effect of continuous positive airway pressure on the incidence of hypertension and cardiovascular events in nonsleepy patients with obstructive sleep apnea: A randomized controlled trial. JAMA 2012, 307, 2161–2168. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Zhou, Z.; McEvoy, R.D.; Anderson, C.S.; Rodgers, A.; Perkovic, V.; Neal, B. Association of positive airway pressure with cardiovascular events and death in adults with sleep apnea: A systematic review and meta-analysis. JAMA 2017, 318, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Abuzaid, A.S.; Al Ashry, H.S.; Elbadawi, A.; Ld, H.; Saad, M.; Elgendy, I.Y.; Elgendy, A.; Mahmoud, A.N.; Mentias, A.; Barakat, A. Meta-analysis of cardiovascular outcomes with continuous positive airway pressure therapy in patients with obstructive sleep apnea. Am. J. Cardiol. 2017, 120, 693–699. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Sun, Y.; Xue, L.-J.; Huang, Z.-Y.; Wang, Y.-S.; Zhang, L.; Zhou, G.-H.; Yuan, L.-X. Effect of CPAP therapy on cardiovascular events and mortality in patients with obstructive sleep apnea: A meta-analysis. Sleep Breath. 2016, 20, 965–974. [Google Scholar] [CrossRef] [PubMed]
- Alruwaili, H.; Dehestani, B.; le Roux, C.W. Clinical impact of liraglutide as a treatment of obesity. Clin. Pharmacol. Adv. Appl. 2013, 13, 53. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, A.R.; Patil, S.P.; Laffan, A.M.; Polotsky, V.; Schneider, H.; Smith, P.L. Obesity and obstructive sleep apnea: Pathogenic mechanisms and therapeutic approaches. Proc. Am. Thorac. Soc. 2008, 5, 185–192. [Google Scholar] [CrossRef]
- Kuczmarski, R.J.; Flegal, K.M. Criteria for definition of overweight in transition: Background and recommendations for the United States. Am. J. Clin. Nutr. 2000, 72, 1074–1081. [Google Scholar] [CrossRef]
- Peppard, P.E.; Young, T.; Palta, M.; Dempsey, J.; Skatrud, J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA 2000, 284, 3015–3021. [Google Scholar] [CrossRef]
- Vgontzas, A.N.; Tan, T.L.; Bixler, E.O.; Martin, L.F.; Shubert, D.; Kales, A. Sleep apnea and sleep disruption in obese patients. Arch. Intern. Med. 1994, 154, 1705–1711. [Google Scholar] [CrossRef]
- Pillar, G.; Shehadeh, N. Abdominal fat and sleep apnea: The chicken or the egg? Diabetes Care 2008, 31, S303–S309. [Google Scholar] [CrossRef]
- Smith, P.L.; Gold, A.R.; Meyers, D.A.; Haponik, E.F.; Bleecker, E.R. Weight loss in mildly to moderately obese patients with obstructive sleep apnea. Ann. Intern. Med. 1985, 103, 850–855. [Google Scholar] [CrossRef] [PubMed]
- Davies, R.; Ali, N.; Stradling, J. Neck circumference and other clinical features in the diagnosis of the obstructive sleep apnoea syndrome. Thorax 1992, 47, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Wolk, R.; Shamsuzzaman, A.S.; Somers, V.K. Obesity, sleep apnea, and hypertension. Hypertension 2003, 42, 1067–1074. [Google Scholar] [CrossRef]
- Poirier, P.; Giles, T.D.; Bray, G.A.; Hong, Y.; Stern, J.S.; Pi-Sunyer, F.X.; Eckel, R.H. Obesity and cardiovascular disease: Pathophysiology, evaluation, and effect of weight loss: An update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation 2006, 113, 898–918. [Google Scholar]
- McGill, H.C., Jr.; McMahan, C.A.; Herderick, E.E.; Zieske, A.W.; Malcom, G.T.; Tracy, R.E.; Strong, J.P. Obesity accelerates the progression of coronary atherosclerosis in young men. Circulation 2002, 105, 2712–2718. [Google Scholar] [CrossRef] [PubMed]
- Manson, J.E.; Colditz, G.A.; Stampfer, M.J.; Willett, W.C.; Rosner, B.; Monson, R.R.; Speizer, F.E.; Hennekens, C.H. A prospective study of obesity and risk of coronary heart disease in women. N. Engl. J. Med. 1990, 322, 882–889. [Google Scholar] [CrossRef] [PubMed]
- Wilson, P.W.; D’Agostino, R.B.; Sullivan, L.; Parise, H.; Kannel, W.B. Overweight and obesity as determinants of cardiovascular risk: The Framingham experience. Arch. Intern. Med. 2002, 162, 1867–1872. [Google Scholar] [CrossRef]
- Magkos, F.; Fraterrigo, G.; Yoshino, J.; Luecking, C.; Kirbach, K.; Kelly, S.C.; de Las Fuentes, L.; He, S.; Okunade, A.L.; Patterson, B.W. Effects of moderate and subsequent progressive weight loss on metabolic function and adipose tissue biology in humans with obesity. Cell Metab. 2016, 23, 591–601. [Google Scholar] [CrossRef]
- Jensen, M.D.; Ryan, D.H.; Apovian, C.M.; Ard, J.D.; Comuzzie, A.G.; Donato, K.A.; Hu, F.B.; Hubbard, V.S.; Jakicic, J.M.; Kushner, R.F. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J. Am. Coll. Cardiol. 2014, 63, 2985–3023. [Google Scholar] [CrossRef]
- NICE Clinical Guidance 43. Obesity: Guidance on the Prevention Identification Assessment and Management of Overweight and Obesity in Adults and Children. 2006. Available online: https://www.nice.org.uk/guidance/cg189/evidence/obesity-update-appendix-p-pdf-6960327450 (accessed on 2 March 2020).
- Yumuk, V.; Tsigos, C.; Fried, M.; Schindler, K.; Busetto, L.; Micic, D.; Toplak, H. European guidelines for obesity management in adults. Obes. Facts 2015, 8, 402–424. [Google Scholar] [CrossRef]
- Garvey, W.T. New tools for weight-loss therapy enable a more robust medical model for obesity treatment: Rationale for a complications-centric approach. Endocr. Pract. 2013, 19, 864–874. [Google Scholar] [CrossRef] [PubMed]
- James, W.P.T. The SCOUT study: Risk-benefit profile of sibutramine in overweight high-risk cardiovascular patients. Eur. Heart J. Suppl. 2005, 7, L44–L48. [Google Scholar] [CrossRef]
- Chan, E.; He, Y.; Chui, C.; Wong, A.; Lau, W.; Wong, I. Efficacy and safety of lorcaserin in obese adults: A meta-analysis of 1-year randomized controlled trials (RCTs) and narrative review on short-term RCTs. Obes. Rev. 2013, 14, 383–392. [Google Scholar] [CrossRef]
- Pi-Sunyer, X. The look AHEAD trial: A review and discussion of its outcomes. Curr. Nutr. Rep. 2014, 3, 387–391. [Google Scholar] [CrossRef]
- Sjöström, L.; Peltonen, M.; Jacobson, P.; Sjöström, C.D.; Karason, K.; Wedel, H.; Ahlin, S.; Anveden, Å.; Bengtsson, C.; Bergmark, G. Bariatric surgery and long-term cardiovascular events. JAMA 2012, 307, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Wing, R.R.; Espeland, M.A.; Clark, J.M.; Hazuda, H.P.; Knowler, W.C.; Pownall, H.J.; Unick, J.; Wadden, T.; Wagenknecht, L. Association of weight loss maintenance and weight regain on 4-year changes in CVD risk factors: The action for health in diabetes (Look AHEAD) clinical trial. Diabetes Care 2016, 39, 1345–1355. [Google Scholar] [PubMed]
- L. A. R. Group. Association of the magnitude of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: A post-hoc analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol. 2016, 4, 913–921. [Google Scholar] [CrossRef]
- Macek, P.; Terek-Derszniak, M.; Biskup, M.; Krol, H.; Smok-Kalwat, J.; Gozdz, S.; Zak, M. A two-year follow-up cohort study—Improved clinical control over CVD risk factors through weight loss in middle-aged and older adults. J. Clin. Med. 2020, 9, 2904. [Google Scholar] [CrossRef]
- Barvaux, V.; Aubert, G.; Rodenstein, D. Clinical Review Article: Weight loss as a treatment for obstructive sleep apnoea. Sleep Med. Rev. 2000, 4, 435–452. [Google Scholar] [CrossRef]
- Carneiro-Barrera, A.; Díaz-Román, A.; Guillén-Riquelme, A.; Buela-Casal, G. Weight loss and lifestyle interventions for obstructive sleep apnoea in adults: Systematic review and meta-analysis. Obes. Rev. 2019, 20, 750–762. [Google Scholar] [CrossRef]
- Collier, A.; Blackman, A.; Foster, G.; Zammit, G.; Rosenberg, R.; Wadden, T.; Aronne, L.; Claudius, B.; Jensen, T.; Mignot, E. S28 Liraglutide 3.0 mg Reduces Severity of Obstructive Sleep Apnoea and Body Weight in Obese Individuals with Moderate or Severe Disease, Scale Sleep Apnoea Trial; BMJ Publishing Group Ltd.: London, UK, 2014. [Google Scholar]
- Peromaa-Haavisto, P.; Tuomilehto, H.; Kössi, J.; Virtanen, J.; Luostarinen, M.; Pihlajamäki, J.; Käkelä, P.; Victorzon, M. Obstructive sleep apnea: The effect of bariatric surgery after 12 months. A prospective multicenter trial. Sleep Med. 2017, 35, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Guggino, J.; Tamisier, R.; Betry, C.; Coumes, S.; Arvieux, C.; Wion, N.; Reche, F.; Pépin, J.-L.; Borel, A.-L. Bariatric surgery short-term outcomes in patients with obstructive sleep apnoea: The Severe Obesity Outcome Network prospective cohort. Int. J. Obes. 2021, 45, 2388–2395. [Google Scholar] [CrossRef] [PubMed]
- Ashrafian, H.; Toma, T.; Rowland, S.P.; Harling, L.; Tan, A.; Efthimiou, E.; Darzi, A.; Athanasiou, T. Bariatric surgery or non-surgical weight loss for obstructive sleep apnoea? A systematic review and comparison of meta-analyses. Obes. Surg. 2015, 25, 1239–1250. [Google Scholar] [CrossRef] [PubMed]
- Hudgel, D.W. Critical review: CPAP and weight management of obstructive sleep apnea cardiovascular co-morbidities. Sleep Med. Rev. 2018, 37, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Tsuyumu, M.; Tsurumoto, T.; Iimura, J.; Nakajima, T.; Kojima, H. Response to a letter to the editor titled, “Weight loss in patients with obstructive sleep apnea: An interventional procedure”. Sleep Breath. 2020, 25, 1165–1166. [Google Scholar] [CrossRef]
- Joosten, S.A.; Hamilton, G.S.; Naughton, M.T. Impact of weight loss management in OSA. Chest 2017, 152, 194–203. [Google Scholar] [CrossRef]
- Chirinos, J.A.; Gurubhagavatula, I.; Teff, K.; Rader, D.J.; Wadden, T.A.; Townsend, R.; Foster, G.D.; Maislin, G.; Saif, H.; Broderick, P. CPAP, weight loss, or both for obstructive sleep apnea. N. Engl. J. Med. 2014, 370, 2265–2275. [Google Scholar] [CrossRef]
- López-Padrós, C.; Salord, N.; Alves, C.; Vilarrasa, N.; Gasa, M.; Planas, R.; Montsserrat, M.; Virgili, M.N.; Rodríguez, C.; Pérez-Ramos, S. Effectiveness of an intensive weight-loss program for severe OSA in patients undergoing CPAP treatment: A randomized controlled trial. J. Clin. Sleep Med. 2020, 16, 503–514. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).