Abstract
Purpose: This study evaluates and compares the effect of printing layer thickness (LT) and post-polymerization time (PPT) on the flexural strength and hardness of three 3D-printed resins after thermal aging. Methods: A bar shape (64 × 10 × 3.3 mm) and a disc shape (15 × 2 mm) were designed for flexural strength and hardness testing, respectively. ASIGA, NextDent, and FormLabs 3D-printed resins were used to print specimens with different LTs (25 µm, 50 µm, and 100 µm). Each thickness group was post-polymerized (PP) for different times (15, 30, 60, and 90 min). All printed specimens were thermally cycled (5000 cycles) and then tested, measuring the flexural strength and hardness using a universal testing machine and Vickers hardness tester, respectively. The data were analyzed using ANOVA and a post hoc Tukey’s test (α = 0.05). Results: A PPT of 90 min showed the highest flexural strength. In comparisons of the LTs, 25 µm and 50 µm significantly increased flexural strength compared with 100 µm, which showed the lowest value for each PPT. The hardness increased as the PPT increased for all materials. In our LT comparison, 25 µm and 50 µm significantly increased the hardness for NextDent and FormLabs resins, while only 25 µm showed high hardness compared with 50 µm and 100 µm for ASIGA. Conclusion: Both parameters (LT and PPT) impact flexural strength and hardness. Increased PPT with the minimum LT is recommended.
1. Introduction
Rapidly prototyping three-dimensional (3D)-printing technology is an aspect of advanced computer-aided design (CAD) and computer-aided manufacturing (CAM) technologies in the dental and medical fields. This process has become popular due to its ease of fabrication, accuracy, and cost-effectiveness [1,2,3,4]. This printing technology converts STL (standard triangulation language) format files into physical models that can be used for various applications using a layering technique followed by post-curing [5]. In general, the most common 3D-printing technologies are fused deposition modeling (FDM), stereolithography (SLA), and digital light projection (DLP) [6,7]. The most common 3D-printing technologies in dental applications are SLA and DLP [8]. SLA technology polymerizes resin by applying laser light tracking [9], whereas DLP technology flashes lights from a digital screen on each layer to construct 3D objects [10]. DLP technology is also faster than SLA technology [5,10].
Many dental applications can be fabricated through 3D-printing technology, including diagnostic casts, provisional crowns, fixed partial dentures, implant components, surgical guides, orthodontic aligners, and removable partial and complete dentures [11]. Numerous studies have used 3D-printing technology in the removable prosthodontics field [12,13,14,15,16,17,18]. Several factors affect the flexural strength of 3D-printed objects, such as adding reinforcement agents to the resin, printing orientation, printing speed, layer thickness, post-polymerization time and methods, and finishing and polishing the final product [19,20,21,22,23]. Some studies have found that applying reinforcement agents such as SiO2NP can improve flexural strength [13,18,24,25]. Regarding printing orientation, some studies show that printing at 0 degrees enhances flexural strength more than that at 45 or 90 degrees [12,26,27,28]. Conversely, Väyrynen et al. [28] and Unkovskiy et al. [29] found that 90 degrees offers more flexural strength in compression than 0 and 45 degrees.
Only a few studies [5,30,31,32,33] have investigated the effect of printing layer thickness on flexural strength. Perea-Lowery et al. [30] found a positive effect on flexural strength associated with lower layer thickness. By contrast, Alshamrani et al. [5] found that a 100 μm layer thickness enhances flexural strength better than 25 μm and 50 μm. Another study examined layer thickness and storage time [33], concluding that different values can impact the dimensional stability of 3D-printed specimens. Two studies [7,16] have examined the effect of post-polymerization time on flexural strength, and both found that increased post-polymerization time significantly improved this factor. Another study [15] found significantly increased flexural strength and hardness with prolonged post-polymerization times. Regarding the influence of thermal cycling on 3D-printed specimens, some studies [9,18,24,26] have concluded that flexural strength is negatively affected by thermal cycling testing.
Although several studies have investigated the effect of different printing variables on the strength of 3D-printed resins, none have investigated or compared the effect of printing layer thickness and post-polymerization time on the strength of 3D-printed resins. Therefore, this study investigated and compared the effect of printing layer thickness and post-polymerization time on the flexural strength and hardness of 3D-printed resins. Our null hypothesis is that these printing variables have no significance in the flexural strength and hardness of 3D printed resins.
2. Materials and Methods
Power analysis was performed to calculate the sample size. Means and standard deviations to determine the sample size were obtained from a previously published study [5]. The power was set as 80% with a 5% margin of error; the calculated sample size was 10 samples per group.
2.1. Specimens Preparation
Flexural strength was determined according to ISO 20795-1:2013 recommendations, where a bar shape (64 × 10 × 3.3) was designed using the open-source AutoCAD software. (123D Design, Autodesk version 2.2.14, San Francisco, CA, USA). For hardness, a disc shape (15 × 2 mm) was designed. Both specimens’ dimensions were stored as standard tessellation language (STL) files and then exported to each printer (Figure 1). The specimens (N = 720, 240/resin, 120/FS, and 120/hardness) were grouped according to the study flow, wherein each resin was placed in 3 groups according to printing layer thickness (LT). Each LT group was subdivided into 4 according to post-polymerization times (PPTs) of 15, 30, 60, and 90 min, with 10 specimens per group and each tested property (n = 10).
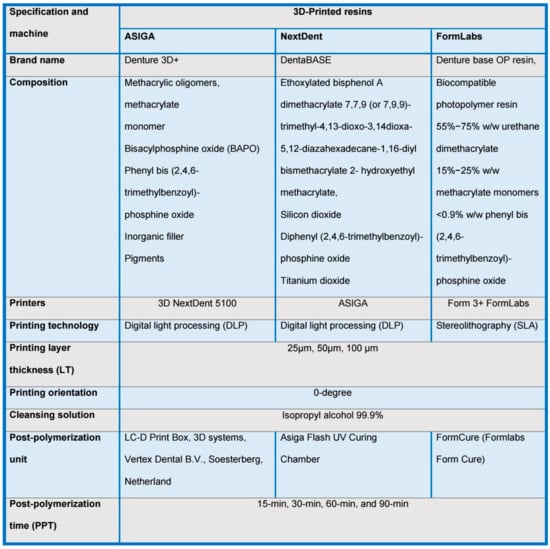
Figure 1.
Material specifications and machines and printing parameters used for specimen fabrication.
After exporting the STL files to each printer, the printing LTs were set to 25, 50, and 100 µm. Each resin was prepared according to the manufacturer’s recommendations: for NextDent and ASIGA, each resin container was shaken for 1 h before filling the resin tank; conversely, the FormLabs container was directly mounted on the printing machine. Finally, all printers were ordered to begin specimen printing. The printer, printing resin, and printing details are summarized in Figure 1.
After printing, the specimens were subjected to PPT using each machine with its respective resin (NextDent, ASIGA, and FormLabs) with four standardized PPTs (15, 30, 60, and 90 min). After polymerization, all supports were removed, and all specimens were checked for defects and evaluated for proper dimensions using a digital caliper. All specimens that met the required dimensions were polished using an automated polishing machine (Metaserv 250 grinder–polisher; Buehler GmbH, Lake Bluff, IL, USA).
After polishing, the specimens in each group were stored in distilled water for 48 h at 37 °C. Before testing, all specimens were thermally stressed for 5000 cycles using a thermal cycling unit (Thermocycler, THE-1100/THE-1200, SD Mechatronik GMBH Miesbacher Str. 34 83,620 Feldkirchen-Westerham, Germany) with 30 s of dwell time and soaked for 5 s between 5 °C and 55 °C. Thermal stress was applied to mimic the oral cavity environment.
2.2. Specimens Testing
2.2.1. Flexural Strength
To test flexural strength, all specimens were horizontally placed on 2 supports 50 mm apart and loaded at the center using a universal testing machine (Instron Model 8871; Instron Corp., Canton, MA, USA). A 5 kN load was applied with a crosshead speed of 5 mm/min until specimen failure occurred, recording the fracture force (N). The recorded force (N) was used to calculate the flexural strength (MPa) with the following equation:
FS = 3 WL/2bh2
2.2.2. Hardness
The Vickers microhardness test (VHN) was completed with the aid of a Vickers tester (Tukon 1102, Wilson Hardness, ITW Test & Measurement, Shanghai, China) with a 25 gf load application for 30 s at the center of each specimen with an indenter. Indentations were determined under a microscope to evaluate hardness. Three indentations were made on each specimen at specific locations. Subsequently, the averages for each specimen were calculated.
2.3. Statistical Analysis
Data normality was tested using the Shapiro–Wilk test, and insignificant results showed that the data were normally distributed. Hence, parametric tests were used for inferential data analysis. One-way ANOVA was used to compare variations in the flexural strength and hardness averages caused by post-polymerization time and thickness at the given level of thickness and post-polymerization time, respectively. A post hoc Tukey’s test was used for pairwise comparison. Three-way ANOVA was used to study the interacting effects of the materials, thickness, and post-polymerization time on the tested properties (flexural strength and hardness). All p-values less than 0.05 were considered statistically significant.
3. Results
The interactions between the three variables (“PPT * LT * material”) are displayed in Table 1 based on the results of three-way ANOVA. For all tested properties, there were significant differences between all variables (p < 0.05).

Table 1.
Interacting effects of time, thickness, and materials for all tested properties (three-way ANOVA).
Table 2 summarizes the mean values, standard deviations, and significance of flexural strength with respect to LT and PPT effects per material. For ASIGA, both LT and PPT showed significant differences in flexural strength (p < 0.05). For each LT, as the PPT increased, the flexural strength increased, and 90 min showed the highest values. When the LTs were compared for fixed PPT, 100 µm showed a significant decrease in flexural strength and the lowest values compared with 25 and 50 µm, without a significant difference between the latter groups.

Table 2.
Flexural strength (MPa) results (mean, SD, and significance) for all tested resins.
For NextDent, LT and PPT showed significant differences in flexural strength (p < 0.008). For each LT, at 25 µm, flexural strength significantly increased as the PPT increased time-dependently, while the 50 µm and 100 µm thicknesses at 15 min showed significant decreases in flexural strength compared with other PPTs. Moreover, there was no significant difference between 30 min, 60 min, and 90 min at 100 µm. When each LT was compared for fixed PPT, there was a significant decrease in flexural strength at a 100 µm LT compared with 25µ, whereas at 60 min and 90 min, the flexural strength significantly decreased as the LT increased. A 100 µm LT showed the lowest flexural strength values for each PPT. For FormLabs, the LT and PPT showed significant differences in flexural strength (p < 0.001). For each LT, flexural strength increased as the PPT increased: 90 min had the highest value, and 15 min showed the lowest value for each LT. When each PPT was compared for fixed LT, 100 µm showed a significant decrease in flexural strength compared with 25 µm and 50 µm (p < 0.001), and there was no significant difference between 25 µm and 50 µm (p > 0.05).
Table 3 summarizes the mean values, standard deviations, and significance of hardness in relation to LT and PPT effects per material. For all materials, both factors significantly affected hardness, except for FormLabs at 15 min (p = 0.064). For each LT, hardness increased as the PPT increased, and 90 min showed the highest values. When each LT was compared for fixed PPT, 100 µm had the lowest values except for at 15 min, which showed no significant differences between different LTs, and 100 µm/30 min showed the lowest hardness value (28.2 ± 2.20 VHN). For ASIGA, 25 µm showed a significant increase in hardness for each PPT compared with 50 µm and 100 µm and no significant difference between 50 µm and 100 µm (p > 0.05). For NextDent and FormLabs, 100 µm showed a significant decrease in hardness compared with 25 µm and 50 µm and no significant difference between 25 µm and 50 µm (p > 0.05).

Table 3.
Hardness (VHN) results (mean, SD, and significance) for all tested resins.
4. Discussion
The objectives of this study were to compare the effects of the LT and PPT on the flexural strength and hardness of 3D-printed resins using two DLP printers and one SLA printer. The null hypothesis stated that these printing variables have no significance in the strength of 3D-printed resins. The null hypothesis is rejected, as both the LT and PPT had clinical significance in the strength and hardness of 3D-printed resins.
Five thousand thermal cycles were used for all samples to represent 6 months of clinical denture wear [34,35]. In addition, sample aging with temperature increased water sorption, affecting the mechanical properties of 3D-printed resins [36]. Water sorption can also influence layer thickness. Water diffusion can move apart and affect samples with multiple layers. Studies [9,18,24,26] have found that thermal cycling deteriorates physical properties like strength.
Three different layer thicknesses were used in this study (25, 50, and 100 µm); 25 µm and 50 µm layer thicknesses showed higher flexural strength than 100 µm. Conversely, Alshamrani et al. [5] showed opposite results, finding that higher flexural values (100 µm) have more flexural strength than 25 and 50 µm. However, thermocycling was not performed after specimen printing in their study. In addition, different DLP printers with different resins can affect results.
Increased flexural strength with small layer thicknesses compared with 100 µm could be attributable to enhancing the light intensity polymerizing of thin layers compared with thick layers [31]. Additionally, resin photopolymerization in SLA and DLP 3D printers can construct objects in layers. For DLP printers, the light is produced by a flashed projector screen through the whole layer. However, a laser light track is used in SLA printers. Free radicals interact with resin monomers and convert them into resin polymers [37]. To optimize the polymerization process, the intensity and amount of light passing through the layers should be great to decrease residual monomers and increase the degree of conversion, thus increasing the flexural strength of the final product [4].
Post-polymerization applications on 3D-printed objects are important for reducing residual monomers [6] and enhancing mechanical properties [7,35]. Post-polymerization manufacturer protocols recommend UV light at higher temperatures for 15–30 min. Some authors [7,19] recommend up to 2 h of post-polymerization time. In the present study, four post-polymerization times were selected (15, 30, 60, and 90 min). We found that the PPT significantly differed in flexural strength in all groups. As the PPT increased, the flexural strength increased. The flexural strength values increased as post-polymerization time increased for both layer thicknesses 25 and 50 µm. Similar results have been found in previous studies [7,16,36]. Kim et al. [7] examined the flexural strength of 3D-printed resins, finding significantly increased flexural strength in association with increased post-polymerization times (60 and 90 min). Aati et al. [16] reported the effect of post-polymerization times (5–20 min) on the flexural properties of 3D-printed resins and concluded that flexural strength increases as post-polymerization times increase.
Hardness is a sign of resistance to plastic deformation caused by surface abrasion or dimensional changes during mechanical processes like hard brushing [33,37,38]. The effect of hardness was another mechanical factor tested in the present study. The average hardness of 3D-printed specimens typically ranges from 30.17 to 34.62 VHN [35]. In the present study, increased hardness was notable at 25 µm and 50 µm layer thicknesses. However, no increase in hardness is associated with 100 µm layer thickness. This agrees with a previous study [5], which showed that a 50 µm thickness increases hardness. Perea-Lowery et al. [30] also investigated the effect of two layer thicknesses (50 μm and 100 μm) for printed splints and made similar conclusions: hardness increased with 50 μm. Moreover, Borella et al. [39] compared the hardness of 3D-printed resins with two different LTs, 50 μm and 100 μm, reporting that a 100 μm layer thickness showed lower hardness than 50 μm. Increased hardness is associated with decreased layer thickness, possibly owing to light penetration through thin layers and an increased degree of conversion [30,37]. There is a direct relationship between hardness and post-polymerization time. Moreover, increased post-polymerization times improve the degree of conversion and reduce residual monomers, increasing hardness [37]. Surface properties have a relationship with printing orientations regarding specimen layer direction [4]. Previous studies have shown that a 0-degree orientation offers more flexural strength than 45 or 90 degrees [12,27,28,35]. The present study used a 0-degree value, making the layer direction perpendicular to the indenter. During testing, the indenter vertically passes through different layers, which could make them more resistant to the indenter compared with other orientations. Moreover, PPT has more of an effect on the surfaces of specimens than the cores of materials, as the surface is more exposed to light during PPT [16,37].
The ISO has standardized 65 MPa as the minimum acceptable value for flexural strength. All values in the present study were above this for all materials, except for 100 µm with a 15 min PPT. Layer thicknesses with higher values than this dramatically increased as the PPT increased. As reported in the literature, parameters affecting the strength of 3D-printed resins and combinations of two or more parameters require further investigation. This study shows that combining the PPT and LT has clinical significance in strength and hardness. Therefore, a minimum layer thickness and increased PPT are recommended to obtain 3D-printed denture bases with appropriate service strengths for long periods and to overcome the limitations of clinically implementing 3D-printed resins. The flexural strength values of the present study fall within acceptable ISO standardized values.
Although the present study included different denture base resins and thermal aging values, it has some limitations related to in vitro studies and other standardized printing parameters. For example, using flat specimens in an in vitro study means we could not simulate denture configurations, and the oral environment (saliva, enzyme, daily intake, and chewing forces) was absent. Other limitations were related to standardized printing parameters, resin modifications, printing orientations, and post-printing conditions. Therefore, we recommend further investigations of 3D-printed resins with this parameter combination that simulate oral conditions with denture designs, in addition to testing other properties to evaluate the overall performances of 3D-printed resins in terms of parameter combinations.
5. Conclusions
Within the limitations of this study, we can conclude the following.
The flexural strength and hardness of 3D-printed denture base resins were improved with increasing PPT. Printing layer thicknesses of 25 µm and 50 µm tend to increase flexural strength and hardness compared to that of 100 µm. In terms of strength, decreased layer thickness and increased PPT resulted in 3D-printed resins with appropriate strengths.
Author Contributions
Conceptualization, H.S.A. and M.M.G.; methodology, H.S.A.; software, H.S.A.; validation, H.S.A. and M.M.G.; formal analysis, M.M.G.; investigation, H.S.A.; resources, H.S.A.; data curation, M.M.G.; writing—original draft preparation, M.M.G.; writing—review and editing, H.S.A. and M.M.G.; visualization, M.M.G.; supervision, M.M.G.; project administration, M.M.G.; funding acquisition, H.S.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Witkowski, S. (CAD-)/CAM in dental technology. Quintessence Dent. Technol. 2005, 28, 169–184. [Google Scholar]
- Revilla-León, M.; Özcan, M. Additive Manufacturing Technologies Used for Processing Polymers: Current Status and Potential Application in Prosthetic Dentistry. J. Prosthodont. 2019, 28, 146–158. [Google Scholar] [CrossRef]
- Jawahar, A.; Maragathavalli, G. Applications of 3D printing in dentistry—A review. J. Pharm. Sci. Res. 2019, 11, 1670–1675. [Google Scholar]
- Gad, M.M.; Fouda, S.M. Factors affecting flexural strength of 3D-printed resins: A systematic review. J. Prosthodont. 2023, 32, 96–110. [Google Scholar] [CrossRef]
- Alshamrani, A.A.; Raju, R.; Ellakwa, A. Effect of Printing Layer Thickness and Postprinting Conditions on the Flexural Strength and Hardness of a 3D-Printed Resin. BioMed Res. Int. 2022, 2022, 8353137. [Google Scholar] [CrossRef]
- Barazanchi, A.; Li, K.C.; Al-Amleh, B.; Lyons, K.; Waddell, J.N. Additive Technology: Update on Current Materials and Applications in Dentistry. J. Prosthodont. 2017, 26, 156–163. [Google Scholar] [CrossRef]
- Kim, D.; Shim, J.S.; Lee, D.; Shin, S.H.; Nam, N.E.; Park, K.H.; Shim, J.S.; Kim, J.E. Effects of Post-Curing Time on the Mechanical and Color Properties of Three-Dimensional Printed Crown and Bridge Materials. Polymers 2020, 12, 2762. [Google Scholar] [CrossRef] [PubMed]
- Scotti, C.K.; Velo, M.M.A.C.; Rizzante, F.A.P.; Nascimento, T.R.L.; Mondelli, R.F.L.; Bombonatti, J.F.S. Physical and surface properties of a 3D-printed composite resin for a digital workflow. J. Prosthet. Dent. 2020, 124, 614.e1–614.e5. [Google Scholar] [CrossRef]
- KEßLER, A.; Hickel, R.; Ilie, N. In vitro investigation of the influence of printing direction on the flexural strength, flexural modulus and fractographic analysis of 3D-printed temporary materials. Dent. Mater. J. 2021, 40, 641–649. [Google Scholar] [CrossRef] [PubMed]
- Pagac, M.; Hajnys, J.; Ma, Q.P.; Jancar, L.; Jansa, J.; Stefek, P.; Mesicek, J. A Review of Vat Photopolymerization Technology: Materials, Applications, Challenges, and Future Trends of 3D Printing. Polymers 2021, 13, 598. [Google Scholar] [CrossRef]
- Figueiredo-Pina, C.G.; Serro, A.P. 3D Printing for Dental Applications. Materials 2023, 16, 4972. [Google Scholar] [CrossRef]
- Srinivasan, M.; Kalberer, N.; Kamnoedboon, P.; Mekki, M.; Durual, S.; Özcan, M.; Müller, F. CAD-CAM complete denture resins: An evaluation of biocompatibility, mechanical properties, and surface characteristics. J. Dent. 2021, 114, 103785. [Google Scholar] [CrossRef]
- Chen, S.; Yang, J.; Jia, Y.G.; Lu, B.; Ren, L. A Study of 3D-Printable Reinforced Composite Resin: PMMA Modified with Silver Nanoparticles Loaded Cellulose Nanocrystal. Materials 2018, 11, 2444. [Google Scholar] [CrossRef]
- Perea-Lowery, L.; Gibreel, M.; Vallittu, P.K.; Lassila, L.V. 3D-Printed vs. Heat-Polymerizing and Autopolymerizing Denture Base Acrylic Resins. Materials 2021, 14, 5781. [Google Scholar] [CrossRef] [PubMed]
- Bayarsaikhan, E.; Lim, J.H.; Shin, S.H.; Park, K.H.; Park, Y.B.; Lee, J.H.; Kim, J.E. Effects of Postcuring Temperature on the Mechanical Properties and Biocompatibility of Three-Dimensional Printed Dental Resin Material. Polymers 2021, 13, 1180. [Google Scholar] [CrossRef] [PubMed]
- Aati, S.; Akram, Z.; Shrestha, B.; Patel, J.; Shih, B.; Shearston, K.; Ngo, H.; Fawzy, A. Effect of post-curing light exposure time on the physico-mechanical properties and cytotoxicity of 3D-printed denture base material. Dent. Mater. 2022, 38, 57–67. [Google Scholar] [CrossRef]
- Li, P.; Lambart, A.L.; Stawarczyk, B.; Reymus, M.; Spintzyk, S. Postpolymerization of a 3D-printed denture base polymer: Impact of post-curing methods on surface characteristics, flexural strength, and cytotoxicity. J. Dent. 2021, 115, 103856. [Google Scholar] [CrossRef] [PubMed]
- Gad, M.M.; Al-Harbi, F.A.; Akhtar, S.; Fouda, S.M. 3D-Printable Denture Base Resin Containing SiO2 Nanoparticles: An In Vitro Analysis of Mechanical and Surface Properties. J. Prosthodont. 2022, 31, 784–790. [Google Scholar] [CrossRef] [PubMed]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, N.; Osman, R.; Wismeijer, D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016, 115, 760–767. [Google Scholar] [CrossRef]
- Osman, R.B.; Alharbi, N.; Wismeijer, D. Build Angle: Does It Influence the Accuracy of 3D-Printed Dental Restorations Using Digital Light-Processing Technology? Int. J. Prosthodont. 2017, 30, 182–188. [Google Scholar] [CrossRef]
- Seelbach, P.; Brueckel, C.; Wöstmann, B. Accuracy of digital and conventional impression techniques and workflow. Clin. Oral. Investig. 2013, 17, 1759–1764. [Google Scholar] [CrossRef] [PubMed]
- Mangal, U.; Seo, J.Y.; Yu, J.; Kwon, J.S.; Choi, S.H. Incorporating Aminated Nanodiamonds to Improve the Mechanical Properties of 3D-Printed Resin-Based Biomedical Appliances. Nanomaterials 2020, 10, 827. [Google Scholar] [CrossRef]
- Aati, S.; Akram, Z.; Ngo, H.; Fawzy, A.S. Development of 3D printed resin reinforced with modified ZrO2 nanoparticles for long-term provisional dental restorations. Dent. Mater. 2021, 37, e360–e374. [Google Scholar] [CrossRef]
- Kwon, J.S.; Kim, J.Y.; Mangal, U.; Seo, J.Y.; Lee, M.J.; Jin, J.; Yu, J.H.; Choi, S.H. Durable Oral Biofilm Resistance of 3D-Printed Dental Base Polymers Containing Zwitterionic Materials. Int. J. Mol. Sci. 2021, 22, 417. [Google Scholar] [CrossRef]
- Shim, J.S.; Kim, J.E.; Jeong, S.H.; Choi, Y.J.; Ryu, J.J. Printing accuracy, mechanical properties, surface characteristics, and microbial adhesion of 3D-printed resins with various printing orientations. J. Prosthet. Dent. 2020, 124, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Derban, P.; Negrea, R.; Rominu, M.; Marsavina, L. Influence of the Printing Angle and Load Direction on Flexure Strength in 3D Printed Materials for Provisional Dental Restorations. Materials 2021, 14, 3376. [Google Scholar] [CrossRef] [PubMed]
- Väyrynen, V.O.; Tanner, J.; Vallittu, P.K. The anisotropicity of the flexural properties of an occlusal device material processed by stereolithography. J. Prosthet. Dent. 2016, 116, 811–817. [Google Scholar] [CrossRef]
- Unkovskiy, A.; Bui, P.H.; Schille, C.; Geis-Gerstorfer, J.; Huettig, F.; Spintzyk, S. Objects build orientation, positioning, and curing influence dimensional accuracy and flexural properties of stereolithographically printed resin. Dent. Mater. 2018, 34, e324–e333. [Google Scholar] [CrossRef]
- Perea-Lowery, L.; Gibreel, M.; Vallittu, P.K.; Lassila, L. Evaluation of the mechanical properties and degree of conversion of 3D printed splint material. J. Mech. Behav. Biomed. Mater. 2021, 115, 104254. [Google Scholar] [CrossRef] [PubMed]
- Sabbah, A.; Romanos, G.; Delgado-Ruiz, R. Impact of Layer Thickness and Storage Time on the Properties of 3D-Printed Dental Dies. Materials 2021, 14, 509. [Google Scholar] [CrossRef] [PubMed]
- Kalberer, N.; Mehl, A.; Schimmel, M.; Müller, F.; Srinivasan, M. CAD-CAM milled versus rapidly prototyped (3D-printed) complete dentures: An in vitro evaluation of trueness. J. Prosthet. Dent. 2019, 121, 637–643. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M.; Abualsaud, R.; Alshahrani, F.A.; Al-Thobity, A.M.; Khan, S.Q.; Akhtar, S.; Ateeq, I.S.; Helal, M.A.; Al-Harbi, F.A. Strength and Surface Properties of a 3D-Printed Denture Base Polymer. J. Prosthodont. 2022, 31, 412–418. [Google Scholar] [CrossRef]
- Al-Dulaijan, Y.A.; Alsulaimi, L.; Alotaibi, R.; Alboainain, A.; Akhtar, S.; Khan, S.Q.; Al-Ghamdi, M.; Gad, M.M. Effect of Printing Orientation and Postcuring Time on the Flexural Strength of 3D-Printed Resins. J. Prosthodont. 2023, 32, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.; Lee, S.; Kim, G.B.; Hong, D.; Kwon, J.; Park, J.W.; Kim, N. Accuracy of a simplified 3D-printed implant surgical guide. J. Prosthet. Dent. 2020, 124, 195–201.e2. [Google Scholar] [CrossRef]
- Prpić, V.; Schauperl, Z.; Ćatić, A.; Dulčić, N.; Čimić, S. Comparison of Mechanical Properties of 3D-Printed, CAD/CAM, and Conventional Denture Base Materials. J. Prosthodont. 2020, 29, 524–528. [Google Scholar] [CrossRef]
- Jeong, M.; Radomski, K.; Lopez, D.; Liu, J.T.; Lee, J.D.; Lee, S.J. Materials and Applications of 3D Printing Technology in Dentistry: An Overview. Dent. J. 2023, 12, 1. [Google Scholar] [CrossRef] [PubMed]
- Al-Dulaijan, Y.A.; Alsulaimi, L.; Alotaibi, R.; Alboainain, A.; Alalawi, H.; Alshehri, S.; Khan, S.Q.; Alsaloum, M.; AlRumaih, H.S.; Alhumaidan, A.A.; et al. Comparative Evaluation of Surface Roughness and Hardness of 3D Printed Resins. Materials 2022, 15, 6822. [Google Scholar] [CrossRef]
- Borella, P.S.; Alvares, L.A.S.; Ribeiro, M.T.H.; Moura, G.F.; Soares, C.J.; Zancopé, K.; Mendonça, G.; Rodrigues, F.P.; das Neves, F.D. Physical and mechanical properties of four 3D-printed resins at two different thick layers: An in vitro comparative study. Dent. Mater. 2023, 39, 686. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).