Abstract
Background and Clinical Significance: Ingestion of foreign bodies may lead to perforation of the gastrointestinal tract in its various segments. This may be accompanied by infections of the mediastinum after esophageal perforations and peritonitis after perforations of the stomach and bowel. Case Presentation: A 64-year-old man was admitted to the hospital because of abdominal pain and fever. The laboratory testing showed increased indices of inflammation. A CT scan of the abdomen revealed perforation of the stomach pylorus wall from a foreign body. Additionally, there were imaging findings suggesting concealed peritonitis in the adjacent area of stomach perforation. A 3.9 cm foreign body was removed with gastroscopy. The investigation into the nature of the foreign body suggested that it was a fish otolith (a structure composed of calcium carbonate, also known as an ear bone). The patient adhered to a Mediterranean diet. He recalled ingesting parts of the head of a 2.5 kg sea bream about 40 days before his admission to the hospital. The patient received broad-spectrum antimicrobial treatment, specifically intravenous ampicillin/sulbactam (2 g/1 g) every 8 h. He had complete resolution of his infection, with full resolution of symptoms and normalization of all abnormal signs noted in the physical examination at outpatient follow-up. Conclusions: Ingestion of a fish otolith may lead to perforation of the gastrointestinal tract and subsequent intra-abdominal infection. Prompt diagnosis with abdominal imaging, especially a CT scan, removal of the foreign body by upper gastrointestinal endoscopy (if possible), and broad-spectrum antibiotics are necessary for the successful management of such cases.
1. Introduction
Ingestion of foreign bodies may lead to perforation of the gastrointestinal tract at various segments, including the esophagus, stomach, small intestine, and large intestine [,,,,,]. The perforation of the gastrointestinal tract at the level of the esophagus may lead to mediastinal infections. Such infections in the mediastinum may be severe with devastating consequences [,,,]. Perforation of the gastrointestinal tract due to ingestion of a foreign body of various types, including bones, metals, and magnets, may have serious consequences for the patient, especially if there is a delay in the diagnosis and/or inappropriate use of antimicrobial treatment. In this article, we present a case of perforation of the stomach in the pylorus by a foreign body, leading to concealed peritonitis [,,,,,,,,,,,].
2. Case Report
A 64-year-old male patient was admitted to the hospital via the emergency department due to severe abdominal pain, fever, and malaise. His symptoms started about two days before his admission to the hospital and had increasing intensity. He did not have any diarrhea or changes in the color of his stool.
His past medical history was positive for arterial hypertension. He had no previous history of gastrointestinal tract disease, neoplasia, diabetes mellitus, aortic or other vascular disease. His body weight was normal.
The physical examination revealed tenderness in the epigastric area. There was no rebound tenderness or abdominal rigidity. His bowel sounds were normal. The rest of the physical examination, including the respiratory, cardiovascular, and urinary systems, revealed no abnormal findings.
The laboratory testing revealed an elevated white blood cell count (15.940/mm3 of blood) with neutrophilia (polymorphonuclear white blood cells 89%). Also, there was an elevation of C-reactive protein (CRP) [21.01 mg/dL (normal range: ≤0.5 mg/dL)] and D-dimer (2.11 µg/mL (normal range: ≤0.5 µg/mL)). The rest of the routine hematological and biochemical testing, including hemoglobin, hematocrit, platelet count, transaminases, cholestatic enzymes, amylase, direct and indirect bilirubin, urea, creatinine, and electrolytes, were all within normal ranges.
The abdominal CT scan showed a foreign body in the pylorus of the stomach that was penetrating the wall of the stomach (Figure 1). There was also air outside the stomach, along with signs of inflammation in the adjacent adipose fatty tissue (Figure 2 and Figure 3). The diagnosis of perforation of the stomach wall with a foreign body was made, leading to subsequent concealed, local peritonitis.
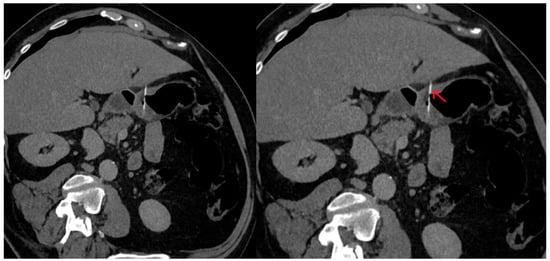
Figure 1.
The foreign body is observed within the stomach lumen, projecting outside the stomach wall margins, suggesting perforation (red arrow).
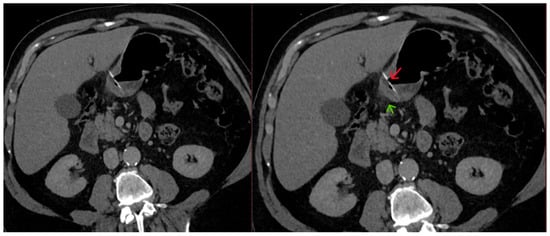
Figure 2.
A linear foreign body is present in the stomach lumen (red arrow), perforating the gastric wall, with surrounding fat stranding (green arrow) resulting from inflammation.
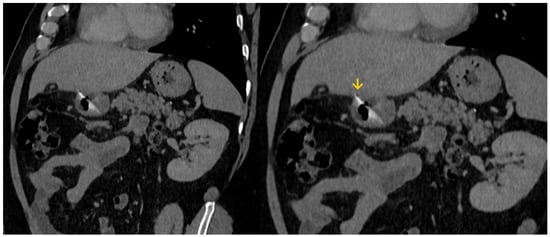
Figure 3.
A small amount of gas (yellow arrow) is depicted outside the stomach wall, due to perforation.
The patient was administered intravenous antimicrobial treatment with ampicillin/sulbactam (2 g/1 g) every 8 h. Ringer’s lactate intravenous hydration (80 mL/hour), and intravenous omeprazole. Additionally, he did not receive food or water orally for 6 days.
A gastroscopy was performed two days after his admission to the hospital for the removal of the foreign body. A 3.9 cm body was removed that looked like a fish bone (Figure 4 and Figure 5).

Figure 4.
The removed foreign body was a fish otolith (part of it had a greenish appearance).
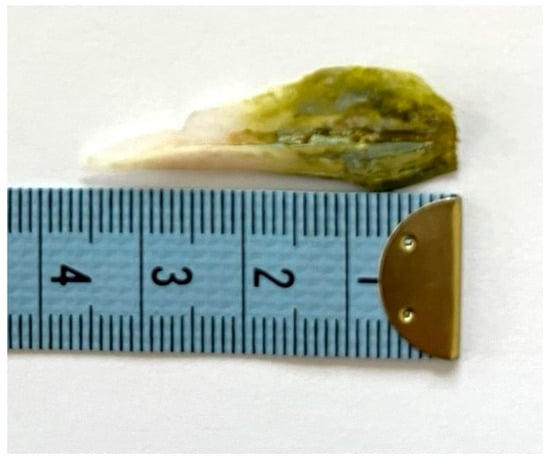
Figure 5.
The length of the removed foreign body was about 3,9 cm (together with the small broken piece of it shown in Figure 4).
The patient continued to experience abdominal tenderness in the epigastric area due to ongoing local inflammation (concealed peritonitis). There was a gradual reduction in CRP [13.02 mg/dL on the third day, 4.63 mg/dL on the fifth day, 1.93 mg/dL on the seventh day, 0.90 mg/dL on the ninth day of his hospitalization]. D-dimer was still elevated on the ninth day of his hospitalization (1.16 µg/mL).
Due to the severity of his overall clinical condition, the patient continued to receive intravenous antimicrobial treatment [intravenous ampicillin/sulbactam (2 g/1 g) every 8 h] and intravenous fluids for an additional three days. He was discharged after 11 days of hospitalization and had medical follow-up on an outpatient basis. The patient received outpatient antimicrobial treatment (moxifloxacin 400 mg tablet once a day) for six days. His health returned to normal, with no symptoms, signs from the physical examination, or abnormalities in his hematological and biochemical testing, including indices of inflammation.
3. Discussion
Perforation of the gastrointestinal tract is a rare complication after ingestion of foreign bodies [,,,,,,,,]. Overall, it occurs in about 1% of foreign body ingestions. However, the probability of perforation of the gastrointestinal tract greatly depends on the specific characteristics of the ingested foreign body. Most reported perforations are caused by sharp, pointed objects (such as chicken bones, fish bones, toothpicks, metallic staples, and metallic wires) rather than smooth, small calcified structures. The perforation of the gastrointestinal tract usually occurs soon after the ingestion of the foreign body (within two weeks). However, there are case reports of unusual delayed perforations related to various ingested foreign bodies [,]. For example, a wooden chopstick ingestion was associated with duodenal perforation 9 months later. The patient in that case report was treated with laparotomy, foreign body removal, and duodenography [].
The clinical manifestations after perforation of the gastrointestinal tract by foreign bodies may be unusual and sometimes surprising to clinicians. For example, the perforation of the large intestine by a fish bone led to left lower quadrant abdominal pain with increasing intensity for 12 days in an 80-year-old male. The clinical presentation and findings from the imaging studies on that patient led to the excision of a mass that was adjacent to the sigmoid colon and had signs of an abscess. A sharp fish bone was found intraoperatively, although no relevant findings were noted preoperatively [].
The investigation of the nature of the removed foreign body in our case suggested that it was a fish otolith. Otoliths are also known as ear stones or ear bones. In humans, otoliths are microscopic, are made of calcium carbonate embedded in a gel-like matrix, and are located inside the vestibular system of the inner ear (utricle and saccule). They play a crucial role in maintaining balance and detecting gravity. In fish, otoliths are larger and more mineralized than in mammals. They play a role in detecting sound, balance, and movement. Fish otoliths are located in the inner ear and grow in layers (like tree rings). Subsequently, they serve as “biological black boxes” because scientists can measure their rings to determine a fish’s age and track growth []. Fisheries biologists extract otoliths to study fish age, population dynamics, and migration patterns []. Additionally, the chemical composition of otoliths can reflect the water chemistry where the fish lived.
The patient in our case adhered to a Mediterranean diet and frequently consumed various species of fish. He recalled eating parts of the head of a large sea bream weighing approximately 2.5 kg about 40 days before his hospital admission. Such a fish measures approximately 60 cm in length and may have long otoliths. Additionally, the patient recalled that he had vague complaints of dyspepsia during the last month before his hospital admission.
The greenish color of the part of the fish otolith removed from the stomach of our patient could be attributed to the staining with bile, regurgitated from the duodenum to the stomach pylorus. Additionally, bacterial infections can alter the color of the surface of foreign bodies. For example, Pseudomonas aeruginosa may lead to the production of greenish pus and the formation of greenish biofilms due to the excretion of color-producing substances, including pyoverdine and pyocyanin.
The frequent development of abdominal infection after perforation of the stomach or the bowel by an ingested foreign body necessitates the administration of antimicrobial treatment. The severity of the condition (concealed or non-concealed peritonitis) leads to inpatient management, including intravenous antibiotics. The main differential diagnosis of severe epigastric pain, which was one of the symptoms of our patient, includes peptic ulcer disease, severe gastritis, perforation of the stomach or the duodenum, pancreatitis, biliary tree disease, aortic dissection, and inferior wall myocardial ischemia. Perforation of the ascending colon may lead to pain in the right lower abdominal quadrant. Sometimes it is accompanied by minimal signs in the physical examination. Differential diagnosis of right lower quadrant pain with minimal physical findings includes acute appendicitis (in the case of a retrocecal appendix, since this location prevents direct peritoneal irritation). It also includes acute acalculous cholecystitis (especially among elderly patients who may have only minimal findings). Another condition to consider is a perforated peptic ulcer as microperforations may seal quickly. Although such conditions usually cause epigastric pain, this pain may be referred to the right lower quadrant as the fluid descends. Early bowel obstruction should also be considered, as the initial stages may present with mild, nonspecific symptoms. Infections resulting from perforation of the gastrointestinal tract typically have a mixed microbial etiology, comprising both aerobic and anaerobic Gram-negative and Gram-positive bacteria. Thus, combinations of antibiotics or drugs with a broad antimicrobial spectrum are used for this indication [,,,].
Concealed peritonitis may occur in patients with various types of intra-abdominal infections, including appendicitis and diverticulitis. In some cases, symptoms may be limited and mild. Additionally, patients with concealed peritonitis may not have apparent signs from the physical examination. Thus, the clinical condition of a patient with concealed peritonitis may be underestimated, leading to delay of appropriate diagnostic and therapeutic measures.
Fluoroquinolones and β-lactam antibiotics are among the first-line choices for patients with abdominal infection due to perforation of the gastrointestinal tract by an ingested foreign body, similarly to cases with intrabdominal infections of other causes [,,,,,,,,,]. A β-lactam/β-lactamase inhibitor, specifically ampicillin/sulbactam, was selected as the antimicrobial treatment in our patient. Additionally, combinations of antimicrobial agents, including metronidazole due to its excellent activity against anaerobic bacteria, such as Bacteroides fragilis and other Bacteroides species, are frequently considered in patients with abdominal infection following perforation of the stomach or bowel by an ingested foreign body [,,,,,].
Our case report highlights the significance of clinical awareness of the possibility of perforation of the gastrointestinal tract by a foreign body in patients with symptoms of abdominal infection. It is also didactic for gastrointestinal endoscopists and surgeons because it presents a case of perforation of the stomach that led to clinical manifestations late after ingestion of the foreign body. Surgical management may be necessary in cases of generalized peritonitis. Our case also underscores that localized peritonitis is a severe infection with potentially devastating consequences. The considerably increased CRP reflected the severity of the abdominal infection in our patient with concealed peritonitis after stomach perforation caused by the ingested foreign body.
4. Conclusions
In our case, the patient developed concealed peritonitis after perforation of the stomach pylorus wall from a fish otolith. Prompt diagnosis, especially using CT scan imaging, an effort to remove the foreign body by gastroscopy if technically feasible, along with the administration of broad-spectrum antimicrobial treatment, are necessary components for a successful outcome.
Author Contributions
M.E.F. had the idea for the article. M.E.F., A.H. and A.S. participated in the patient’s medical care. M.E.F., L.T.R. and M.T. conducted the literature search. M.E.F. wrote the first version of the manuscript. All authors (M.E.F., L.T.R., A.H., A.S. and M.T.) contributed to the revision of the article and have read and agreed to the published version of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the The Scientific Council of Hygeia Hospital (Approval No.674, Date: 12 November 2025).
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Acknowledgments
We thank the patient for his consent to publish this case report.
Conflicts of Interest
The authors declare that there are no conflicts of interest.
References
- Tomono, N.; Niiro, N.; Fujita, Y.; Amagai, T. Emergency Laparoscopic Removal of an Ingested Fishbone Perforating the Stomach After Endoscopy: A Case Report. Cureus 2025, 17, e81060. [Google Scholar] [CrossRef]
- Abuzneid, Y.S.; Alzeerelhouseini, H.I.A.; Rabee, A.; Aqel, W.; Ayyad, R.F.; Asad, T.M.; Abukarsh, R. Double Magnet Ingestion Causing Intestinal Perforation with Peritonitis: Case Report and Review of the Literature. Case Rep. Surg. 2022, 2022, 4348787. [Google Scholar] [CrossRef]
- Fleres, F.; Ieni, A.; Saladino, E.; Speciale, G.; Aspromonte, M.; Cannaò, A.; Macrì, A. Rectal Perforation by Inadvertent Ingestion of a Blister Pack: A Case Report and Review of Literature. World J. Clin. Cases 2018, 6, 384–392. [Google Scholar] [CrossRef]
- Tavarez, M.M.; Saladino, R.A.; Gaines, B.A.; Manole, M.D. Prevalence, Clinical Features and Management of Pediatric Magnetic Foreign Body Ingestions. J. Emerg. Med. 2013, 44, 261–268. [Google Scholar] [CrossRef]
- Hauser, H.; Pfeifer, J.; Uranüs, S.; Klimpfinger, M. Perforation of the Cecum by a Toothpick. Case Report and Review of the Literature. Langenbecks Arch. Chir. 1994, 379, 229–232. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.P.; Gardner, J.A. Perforation of the Sigmoid Colon by Swallowed Chicken Bone: Case Reports and Review of Literature. Int. Surg. 1981, 66, 181–183. [Google Scholar]
- AlAbdullah, H.S.; Kabbani, M.S.; Ismail, S.R.; Hijaz, O.; AlGhamdi, A. Esophageal Perforation with Mediastinitis Leading to Mycotic Aortic Pseudoaneurysm in a Pediatric Patient: A Complication of Sharp Foreign Body Ingestion. SAGE Open Med. Case Rep. 2025, 13, 2050313X251366363. [Google Scholar] [CrossRef]
- Liu, B.; Kuang, S.; Cao, M.; Li, X. Esophageal Foreign Bodies: A Retrospective Analysis of 275 Cases. J. Thorac. Dis. 2025, 17, 4136–4144. [Google Scholar] [CrossRef]
- Letrillart, J.; Talbotec, C.; Payen, E.; Abi-Nader, E.; Lambe, C.; Campeotto, F.; Ronconi, M.; Ruemmele, F.; Simon, F.; Thierry, B.; et al. Oesophageal Impaction of Button Batteries in Children: A Tertiary Centre Experience. Arch. Dis. Child. 2025, 110, 997–1002. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Liu, H.; Shu, X.; Liu, X. Risk Factors for the Poor Prognosis of Benign Esophageal Perforation: 8-Year Experience. BMC Gastroenterol. 2022, 22, 537. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Baek, S.-E.; Lee, C.W.; Kim, Y.C.; Kim, M.-J. Foreign Body Ingestion: Radiologic Evaluation, Findings, and Management. Korean J. Radiol. 2025, 26, 638–649. [Google Scholar] [CrossRef] [PubMed]
- Arcia, A.; Muñoz, G.A.; Jimenez, G.E.; Albuja, M.G.; Yumbla, T.S.; Venegas, O.H.; Velasco, A.G.; Parrales, D.; Molina, G.A. Fishbone Perforation of the Stomach into the Lesser Sac and Pancreas with Abscess, a Fishy Business. J. Surg. Case Rep. 2024, 2024, rjae787. [Google Scholar] [CrossRef]
- Abboud, B.; Dar, R.; Bramnick, Z.; Farraj, M. Gastric Perforation Secondary to Prolonged Multiple Foreign Body Ingestions in a Patient with Schizophrenia. Isr. Med. Assoc. J. IMAJ 2024, 26, 52–53. [Google Scholar] [PubMed]
- Peyron, P.-A.; Villard, C.; Baccino, E. Fatal Bowel Perforation Caused by Ingestion of High-Powered Magnets in a 6-Year-Old Boy. Int. J. Legal Med. 2024, 138, 1659–1662. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Fang, W.; Chen, Z.; Tang, S. Bowel Perforation Caused by Foreign Body Ingestion Presenting as Intestinal Obstruction: A Case Report Highlighting the Importance of Early Diagnosis. Ann. Med. Surg. 2025, 87, 5205–5208. [Google Scholar] [CrossRef]
- Claassens, E.L.; van Berckel, M.M.G.; Wevers, K.P. A Case Report of a Sigmoid Perforation within an Inguinoscrotal Hernia Sac Caused by Ingestion of a Chicken Wishbone. Int. J. Surg. Case Rep. 2025, 128, 111062. [Google Scholar] [CrossRef]
- Okumura, M.; Koga, H.; Eguchi, H.; Sato, N.; Utsunomiya, R.; Wakahara, Y.; Morimoto, K.; Sugiyama, K. Ascending Colon Perforation by a Migrated Pancreatic Spontaneous Dislodgment Stent: A Case Report. Clin. J. Gastroenterol. 2025, 18, 383–388. [Google Scholar] [CrossRef]
- Dupont, D.H.; Umejiego, L.M.; Satoskar, S.; Soumya, N.; Rosa Santana, M.; Sikka, A.; Ayele, N.; Riera Gonzalez, C.; Bahadur, N.; Singh, A. Fishbone Foreign Body Ingestion with Gastric Impaction and Intestinal Micro-Perforation in an Adult Female: A Case Report. Cureus 2024, 16, e72099. [Google Scholar] [CrossRef]
- Mokbul, M.I.; Roy, S.; Roy, A.N.; Shrestha, A.; Nawys, M. Not Your Typical Abdominal Pain: Case Report of a Fisherman Presenting to the Trauma & Emergency Surgery Department with Intestinal Perforation Due to an Eel Fish. Int. J. Surg. Case Rep. 2024, 124, 110401. [Google Scholar] [CrossRef]
- Panday, B.; Bhatta, O.P.; Gyawali, P.; Dangol, R.S.; Joshi, M.D.; Neupane, B.R. Ileal Perforation Peritonitis Secondary to Accidental Ingestion of a Chicken Bone: A Case Report. Int. J. Surg. Case Rep. 2024, 123, 110284. [Google Scholar] [CrossRef]
- Lin, C.-Y.; Pu, T.-W. Colon Perforation with Severe Peritonitis Caused by Erotic Toy Insertion and Treated Using Vacuum-Assisted Closure: A Case Report. World J. Clin. Cases 2024, 12, 3548–3554. [Google Scholar] [CrossRef]
- Ndoye, N.A.; Welle, I.B.; Lamega, B.; Diawara, A.; Zeng, F.T.A.; Ngom, G. Ileal Perforation Peritonitis Secondary to Ingestion of Magnetic Beads in the Older Child: A Case Report. Int. J. Surg. Case Rep. 2024, 121, 109915. [Google Scholar] [CrossRef]
- Mejri, A.; Yaacoubi, J.; Mseddi, M.A.; Omry, A. Gastrointestinal Perforations by Ingested Foreign Bodies: A Preoperative Diagnostic Flowchart-Based Experience. A Case Series Report. Int. J. Surg. Case Rep. 2022, 95, 107216. [Google Scholar] [CrossRef]
- Zamary, K.R.; Davis, J.W.; Ament, E.E.; Dirks, R.C.; Garry, J.E. This Too Shall Pass: A Study of Ingested Sharp Foreign Bodies. J. Trauma Acute Care Surg. 2017, 82, 150–155. [Google Scholar] [CrossRef]
- Demiroren, K. Management of Gastrointestinal Foreign Bodies with Brief Review of the Guidelines. Pediatr. Gastroenterol. Hepatol. Nutr. 2023, 26, 1. [Google Scholar] [CrossRef]
- Odeghe, E.; Osueni, A.; Owoseni, O.O.; Adeniyi, F.; Lesi, O. Upper Gastrointestinal Bleeding Secondary to an Incidental, Impacted Foreign Body in the Duodenum. Cureus 2020, 12, e6971. [Google Scholar] [CrossRef]
- Ambe, P.; Weber, S.A.; Schauer, M.; Knoefel, W.T. Swallowed Foreign Bodies in Adults. Dtsch. Arzteblatt Int. 2012, 109, 869–875. [Google Scholar] [CrossRef]
- Ebrahimi, M.; Malmir, J.; Mahmoudi-Gharaee, A.; Foroughian, M. A Rare Case of Gastrointestinal Tract Foreign Body; Glassy Stomach. Emerg. Tehran Iran 2017, 5, e44. [Google Scholar]
- Almoudaris, A.M.; Chow, A.; Kaneria, S.; Jiyad, Z.; Hadjiminas, D.J. Fish Bone Perforation Mimicking Acute Appendicitis. J. Med. Cases 2011, 2, 296–299. [Google Scholar] [CrossRef]
- Gopinath, B.; Mishra, P.R.; Dash, N.R.; Kumar, G.; Rajendran, J.; Panwar, R. Ingestion of a Saw-Edge Knife in a Patient with Mental Illness: A Unique and Uncommon Presentation. JEM Rep. 2023, 2, 100044. [Google Scholar] [CrossRef]
- Pîrvulescu, I.C.; Najm, A.; Popa, E.C.; Chiotoroiu, A.L.; Cretoiu, S.M.; Gaspar, B.S. A Unique Case of Foreign Body Acquired by Stabbing and Retained for 7 Years in the Sigmoid Colon. Reports 2023, 6, 24. [Google Scholar] [CrossRef]
- Bhasin, S.; Kachroo, S.; Kumar, V.; Kumar, R.; Chandail, V. 7” Long Knife for 7 Years in the Duodenum: A Rare Case Report and Review of Literature. Int. Surg. J. 2014, 1, 29. [Google Scholar] [CrossRef]
- Li, C.; Yong, C.-C.; Encarnacion, D.D. Duodenal Perforation Nine Months after Accidental Foreign Body Ingestion, a Case Report. BMC Surg. 2019, 19, 132. [Google Scholar] [CrossRef]
- Herrera Hernández, D.; Barragán Jiménez, E.M.; Cano Herrera, P.; Flores García, P.P.; Paternina Gonzalez, I.Y.; Páramo Hernández, D.L.; Burciaga Castañeda, R.; Treviño Flores, J.C. Perforation of the Large Intestine by a Fish Bone Mimicking Cancer: A Rare Case Report. Cureus 2025, 17, e85867. [Google Scholar] [CrossRef]
- Wadie, W.F.; Reskalla, S.I.; Dowidar, N.M. Age and Growth Studies of the Sphyraenidae Family in the Southeastern Mediterranean Based on Otolith Measurements. Folia Morphol. 1989, 37, 38–56. [Google Scholar]
- Bellodi, A.; Asciutto, E.; Malara, D.; Longo, F.; Agus, B.; Bacchiani, C.; Follesa, M.C.; Porcu, C.; Mangano, M.C.; Battaglia, P. Age Determination, Growth and Otolith Shape Analysis of Lepidotrigla Cavillone from Sardinian and Sicilian Waters (Mediterranean Sea). J. Fish Biol. 2025, 107, 1018–1029. [Google Scholar] [CrossRef] [PubMed]
- You, H.; Sweeny, A.; Cooper, M.L.; Von Papen, M.; Innes, J. The Management of Diverticulitis: A Review of the Guidelines. Med. J. Aust. 2019, 211, 421–427. [Google Scholar] [CrossRef]
- Haddad, N.; Kanj, S.S.; Awad, L.S.; Abdallah, D.I.; Moghnieh, R.A. The 2018 Lebanese Society of Infectious Diseases and Clinical Microbiology Guidelines for the Use of Antimicrobial Therapy in Complicated Intra-Abdominal Infections in the Era of Antimicrobial Resistance. BMC Infect. Dis. 2019, 19, 293. [Google Scholar] [CrossRef] [PubMed]
- Lalisang, T.J.M.; Usman, N.; Hendrawidjaya, I.; Handaya, A.Y.; Nasution, S.; Saunar, R.Y.; Loho, T.; Karuniawati, A.; Moenadjat, Y.; Widyahening, I.S. Clinical Practice Guidelines in Complicated Intra-Abdominal Infection 2018: An Indonesian Perspective. Surg. Infect. 2019, 20, 83–90. [Google Scholar] [CrossRef]
- Mazuski, J.E.; Tessier, J.M.; May, A.K.; Sawyer, R.G.; Nadler, E.P.; Rosengart, M.R.; Chang, P.K.; O’Neill, P.J.; Mollen, K.P.; Huston, J.M.; et al. The Surgical Infection Society Revised Guidelines on the Management of Intra-Abdominal Infection. Surg. Infect. 2017, 18, 1–76. [Google Scholar] [CrossRef]
- Falagas, M.E.; Barefoot, L.; Griffith, J.; Ruthazar, R.; Snydman, D.R. Risk Factors Leading to Clinical Failure in the Treatment of Intra-Abdominal or Skin/Soft Tissue Infections. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 1996, 15, 913–921. [Google Scholar] [CrossRef]
- Salö, M.; Tiselius, C.; Rosemar, A.; Öst, E.; Sohlberg, S.; Andersson, R.E. Swedish National Guidelines for Diagnosis and Management of Acute Appendicitis in Adults and Children. BJS Open 2025, 9, zrae165. [Google Scholar] [CrossRef]
- Huston, J.M.; Barie, P.S.; Dellinger, E.P.; Forrester, J.D.; Duane, T.M.; Tessier, J.M.; Sawyer, R.G.; Cainzos, M.A.; Rasa, K.; Chipman, J.G.; et al. The Surgical Infection Society Guidelines on the Management of Intra-Abdominal Infection: 2024 Update. Surg. Infect. 2024, 25, 419–435. [Google Scholar] [CrossRef]
- Falagas, M.E.; Matthaiou, D.K.; Bliziotis, I.A. Systematic Review: Fluoroquinolones for the Treatment of Intra-Abdominal Surgical Infections. Aliment. Pharmacol. Ther. 2007, 25, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Yoon, Y.K.; Moon, C.; Kim, J.; Heo, S.T.; Lee, M.S.; Lee, S.; Kwon, K.-T.; Kim, S.-W.; Korean Society for Antimicrobial Therapy. Korean Society of Infectious Diseases Korean Guidelines for Use of Antibiotics for Intra-Abdominal Infections in Adults. Infect. Chemother. 2022, 54, 812–853. [Google Scholar] [CrossRef]
- Mavros, M.N.; Theochari, N.A.; Kyriakidou, M.; Economopoulos, K.P.; Sava, J.A.; Falagas, M.E. Fluoroquinolone-Based versus β-Lactam-Based Regimens for Complicated Intra-Abdominal Infections: A Meta-Analysis of Randomised Controlled Trials. Int. J. Antimicrob. Agents 2019, 53, 746–754. [Google Scholar] [CrossRef]
- Collard, M.K.; Christou, N.; Lakkis, Z.; Mege, D.; Bridoux, V.; Millet, I.; Sabbagh, C.; Loriau, J.; Lefevre, J.H.; Ronot, M.; et al. Adult Appendicitis: Clinical Practice Guidelines from the French Society of Digestive Surgery and the Society of Abdominal and Digestive Imaging. J. Visc. Surg. 2021, 158, 242–252. [Google Scholar] [CrossRef]
- Rafailidis, P.I.; Ioannidou, E.N.; Falagas, M.E. Ampicillin/Sulbactam: Current Status in Severe Bacterial Infections. Drugs 2007, 67, 1829–1849. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Wu, J.; Wang, P.; Fang, X.; Yu, Y.; Tang, J.; Xiao, Y.; Wang, M.; Li, S.; Zhang, Y.; et al. Diagnosis and Management of Intraabdominal Infection: Guidelines by the Chinese Society of Surgical Infection and Intensive Care and the Chinese College of Gastrointestinal Fistula Surgeons. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2020, 71, S337–S362. [Google Scholar] [CrossRef] [PubMed]
- Pan, D.; Hills, G.; Hamilton, A.R.; Nash, T.; Hine, T.; Whitehorn, S.; Barlow, G. Recommended Antimicrobial Therapy for Common Inpatient Infections: A Comparative Review of Guidelines across 51 Hospital Trusts in England. Postgrad. Med. J. 2021, 97, 782–788. [Google Scholar] [CrossRef]
- Zeineddin, S.; Pitt, J.B.; Linton, S.; De Boer, C.; Hu, A.; Carter, M.; Alayleh, A.; Abdullah, F.; Raval, M.; Goldstein, S.D. Postoperative Antibiotics for Complicated Appendicitis in Children: Piperacillin/Tazobactam Versus Ceftriaxone with Metronidazole. J. Pediatr. Surg. 2023, 58, 1128–1132. [Google Scholar] [CrossRef] [PubMed]
- Matthaiou, D.K.; Peppas, G.; Bliziotis, I.A.; Falagas, M.E. Ciprofloxacin/Metronidazole versus Beta-Lactam-Based Treatment of Intra-Abdominal Infections: A Meta-Analysis of Comparative Trials. Int. J. Antimicrob. Agents 2006, 28, 159–165. [Google Scholar] [CrossRef]
- Kashtan, M.A.; Graham, D.A.; Melvin, P.; Hills-Dunlap, J.L.; Anandalwar, S.P.; Rangel, S.J. Ceftriaxone with Metronidazole versus Piperacillin/Tazobactam in the Management of Complicated Appendicitis in Children: Results from a Multicenter Pediatric NSQIP Analysis. J. Pediatr. Surg. 2022, 57, 365–372. [Google Scholar] [CrossRef]
- Kashtan, M.A.; Graham, D.A.; Melvin, P.; Cameron, D.B.; Anandalwar, S.P.; Hills-Dunlap, J.L.; Rangel, S.J. Ceftriaxone Combined with Metronidazole Is Superior to Cefoxitin Alone in the Management of Uncomplicated Appendicitis in Children: Results from a Multicenter Collaborative Comparative Effectiveness Study. Ann. Surg. 2021, 274, e995–e1000. [Google Scholar] [CrossRef] [PubMed]
- Hamdy, R.F.; Handy, L.K.; Spyridakis, E.; Dona, D.; Bryan, M.; Collins, J.L.; Gerber, J.S. Comparative Effectiveness of Ceftriaxone plus Metronidazole versus Anti-Pseudomonal Antibiotics for Perforated Appendicitis in Children. Surg. Infect. 2019, 20, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Hurst, A.L.; Olson, D.; Somme, S.; Child, J.; Pyle, L.; Ranade, D.; Stamatoiu, A.; Crombleholme, T.; Parker, S.K. Once-Daily Ceftriaxone Plus Metronidazole Versus Ertapenem and/or Cefoxitin for Pediatric Appendicitis. J. Pediatr. Infect. Dis. Soc. 2017, 6, 57–64. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).