Abstract
Background and Clinical Significance: Vascular complications occurring in the context of trans-trochanteric fractures are rare (mean incidence 0.2–0.5%) but can be fatal if not recognized and treated promptly. Most of the previously reported vascular injuries are iatrogenic, and various mechanisms of injury and producing agents have been reported. Case Presentation: We present a rare but severe vascular complication following proximal femur fracture fixation in the case of a 77-year-old patient, specifically, a deep femoral artery injury after DHS osteosynthesis. CT angiography identified the lesion in the territory of the profunda femoris artery, precisely at the level of the most distal screw, suggesting over-drilling as the underlying cause. The case is presented in the context of a literature review, updating the most important features of the vascular complications, incidence, diagnosis and treatment. Conclusions: This case highlights the critical role of early diagnosis and prompt interdisciplinary collaboration between orthopedic and vascular surgeons in managing iatrogenic vascular complications, achieving a favorable outcome.
1. Introduction and Clinical Significance
The elderly are more prone to fractures of the proximal femur (trochanteric fractures), undergoing hip replacement as a standard surgical treatment [1,2]. Vascular complications and injuries occurring during the course of internal fixation, manipulation and surgical procedures are rare, as most reports indicate an incidence of 0.2–0.5% [1,2,3], pseudoaneurysm being the predominant lesion type (67.03%) [4]. Approximately 80% of the lesions described in the literature affect the deep femoral artery [1,3,5,6], justifying the special attention that has to be paid to this vessel. Demographic changes and the increasing number of orthopedic interventions suggest that these complications will be encountered more frequently in practice [1,7]. Vascular injuries can occur either at the time of fracture, or during surgery, or even later, after weeks or months.
The present case illustrates a rare but severe vascular complication following proximal femur fracture fixation. Notably, intraoperative observation revealed that positioning the patient on the orthopedic traction table alters the anatomical relationship between the femoral shaft and the deep femoral artery, increasing the risk of injury during distal drilling. This observation emphasizes the need for heightened awareness, careful instrumentation, and appropriate imaging to prevent iatrogenic damage.
2. Case Presentation
A 77-year-old female patient was transported by ambulance to the emergency department, complaining of pain and functional impairment in the left hip, 2 days after falling from the same level at home. The patient had a medical history of arterial hypertension, mixed dementia, bronchial asthma, and chronic hepatitis C. The radiological examination reveals a per-trochanteric comminuted fracture with medial displacement of the lesser trochanter and atherosclerosis of the deep femoral artery. The patient was admitted to the orthopedic department of Bihor County Hospital, Oradea, Romania, and scheduled for surgery.
The patient was positioned in a dorsal recumbent position on the orthopedic surgery table, while axial traction and internal rotation of the left lower limb were practiced to reduce the fracture. Upon opening the fascia lata, a hematoma of ~400 mL was evacuated and significant active bleeding was observed. The involvement of a vascular surgeon was urgently required intraoperatively, but no significant vascular injury such as damage to the profunda femoris artery was observed. Only small-caliber vessels were identified as sources of active bleeding and were controlled by electrocautery and ligation, allowing hemostasis and enabling the fracture to be fixed with a dynamic hip screw (DHS) system, as presented in Figure 1.
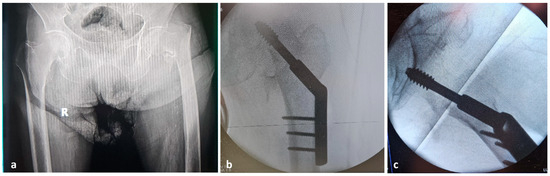
Figure 1.
Radiologic images: (a) preoperative; (b) postoperative anteroposterior; (c) postoperative lateral view.
A few hours after surgery, the patient’s general condition had deteriorated drastically, the left thigh increased significantly in volume and the hemoglobin level decreased from 14.6 g/dL (at the time of admission) to 5.7 g/dL. Angio-CT investigation was performed, identifying a lesion in the deep femoral artery, within the area of the most distal screw (Figure 2).
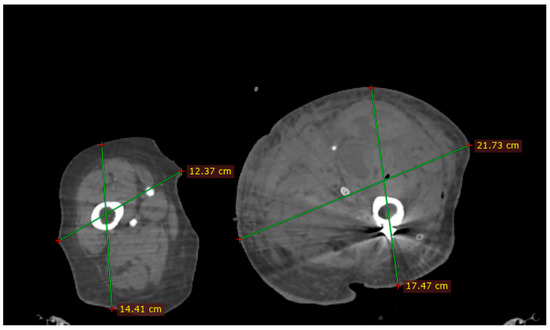
Figure 2.
Angio CT image: Dimensional difference between left and right thigh.
Emergency surgery re-intervention was performed. The profunda femoris artery was accessed and repaired through the same lateral incision used for fracture fixation. Bleeding was initially controlled by direct manual compression and electrocautery of small branches until the artery was clamped. No endovascular balloon occlusion was used. The lesion consisted of a perforation of the profunda femoris artery which was treated by primary repair (direct arteriorrhaphy) without ligation. Postoperative monitoring of arterial patency was performed clinically and with Doppler ultrasound during the entire hospitalization period. The patient was discharged in good condition. No information was available about the patient after discharge.
In order to identify the causes of the complication, the Angio-CT images were analyzed using 3D Slicer 5.0.3 and RadiAnt DICOM Viewer 2025.2 software (Figure 3). We identified a spatial separation between the screw direction (which corresponds to the drill trajectory) and the location of the vascular lesion. In the axial plane, a perpendicular line drawn from the screw trajectory to the site of the profunda femoris artery lesion measured 28.90 mm. In the sagittal plane, a vertical line drawn from the lesion to the screw trajectory showed a distance of 4.85 mm. These findings suggest that the geometry of the anatomical relationship between the femoral diaphysis and the profunda femoris artery may have been altered during fracture reduction maneuvers on the orthopedic traction table, bringing the artery into closer proximity to the femoral cortex than under normal conditions.
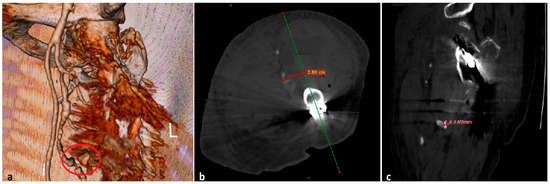
Figure 3.
Angio-CT image investigation: (a) vascular injury associated with contrast medium extravasation (red circle); (b) the distance between the screw trajectory (green line) and the profunda femoris artery lesion, axial view (red line); (c) the distance between the vascular lesion and screw direction, sagittal view.
3. Discussion
The fixation of proximal femoral fractures and the management of their associated complications continue to be a subject of great interest to clinicians, presenting a high risk of morbidity and mortality. Often, these vascular complications involve the deep femoral artery, as a consequence of protrusion of various surgical instruments, retractor manipulation, bone fragment displacement, etc. Most of the reported vascular injuries are iatrogenic, while various mechanisms of injury and producing agents were reported. Table 1 summarizes the most relevant studies presented in the literature, highlighting the details of mechanisms and causes of lesions, types of lesions, anatomical location, implant types and treatment techniques.

Table 1.
Summary of the most relevant studies reporting vascular injuries associated with trochanteric fractures.
In our case, the length of the distal screw was verified and found to be correct, thus excluding direct perforation of the profunda femoris artery by the screw itself. During the procedure, Farabeuf retractors were used and were consistently positioned lateral to the femoral diaphysis. Based on our measurements, the combination of the pelvic support compressing the medial aspect of the thigh, axial traction and internal rotation may have displaced the profunda femoris artery approximately 28.9 mm anteriorly and 4.85 mm proximally. Lateral displacement could not be determined. These measurements were derived from the distance between the vascular lesion and the trajectory of the drill bit at the level of the most distal screw.
Two main mechanisms of vascular injury after proximal femur fracture fixation have been described in the literature: displaced fragments of the lesser trochanter and iatrogenic trauma from surgical instruments, drill bits, or screws. In our case, overdrilling during DHS fixation was the mechanism leading to the profunda femoris artery injury. Nevertheless, displaced bone fragments can also injure adjacent vessels, and both mechanisms should be borne in mind during surgical planning and intraoperative vigilance.
In our literature review, we included patients reported in the literature who experienced vascular injuries associated with surgical fixation of proximal femur fractures. Specifically, we considered cases of intertrochanteric, subtrochanteric, femoral neck, and combined trochantero-diaphyseal fractures and subsequently developed an arterial complication. Both iatrogenic and fracture-related vascular injuries were included, proving that the fracture was located in the proximal femur.
We excluded all patients who did not experience a proximal femur fracture, as well as those with periprosthetic fractures, isolated traumatic pseudoaneurysms without fracture, and cases in which the fracture location or mechanism of injury could not be clearly determined. Duplicate cases that had already been reported earlier were also excluded to avoid double-counting.
As shown in Table 1, most vascular injuries associated with proximal femur fracture fixation were reported in intertrochanteric fractures treated with either dynamic hip screws or intramedullary nails [1,2,3,4,5,6,8,9,10,11,12,13,14,15,16]. The deep femoral artery was by far the most frequently affected vessel, accounting for more than half of all lesions, followed by the superficial and common femoral arteries [1,4,6]. Intrapelvic injuries were uncommon (<10%). The majority of cases were iatrogenic, mainly related to over-drilling or excessively long screws [12,13,14,16,17,18], while displaced lesser trochanter fragments were also an important cause [1,6,19,20,21]. Pseudoaneurysms represented the predominant type of vascular lesion, whereas arteriovenous fistulas were rare but well-documented, usually between the deep femoral artery and vein [4,8,12,13,15,16,18,20,21,22,23,24,25,26,27,28,29,30]. The International Surgery Journal (2023) also reported a profunda femoris artery pseudoaneurysm following dynamic hip screw fixation for an intertrochanteric fracture [31]. Additional recent case reports also confirm pseudoaneurysms as the most frequent vascular lesion after hip fracture fixation [12,14,29]. Overall, almost all patients required surgical or endovascular repair, with conservative management being exceptional [1,2,3,4,5,6,8,9,10,11].
3.1. Clinical and Paraclinical Diagnosis
Clinical alarm signs included cutaneous pallor, expanding hematoma with dimensional increase in the thigh, intense pain, local temperature change and, sometimes, the presence of a pulsatile mass [1,2,4,5,8]. Acute hemorrhage is manifested by hypotension and tachycardia, but patients treated with beta-blockers may have subtle signs [2,6]. Pseudoaneurysms may be silent and are often diagnosed late; they may cause progressive anemia, thigh edema, and chronic pain [1,3,4,9,15,18,28,29,30,32]. Investigation methods ranged from Doppler ultrasound and CT angiography to diagnostic and therapeutic angiography [1,9,20,33].
3.2. Treatment and Prognosis
Treatment strategies for vascular injuries associated with proximal femur fractures vary widely, ranging from conservative management (compression or observation) to complex surgical or endovascular interventions. The most frequently reported approaches included open surgical repair, vascular ligation, arterial suturing, endovascular coil embolization, and stent-graft placement. In several cases, thrombin injection guided by Doppler ultrasound has also been successfully employed [2,9,10,19]. Segal et al. [2] reported various endovascular techniques such as ultrasound-guided thrombin injection and coil embolization, including cases managed without endovascular intervention. Neubauer et al. [20] observed a complete recovery in 66% of patients, although the complication rate remained substantial. Across the reviewed literature, endovascular embolization emerged as the most frequently used therapeutic approach, particularly in the treatment of iatrogenic pseudoaneurysms [3,4,5,6,8,9,10,19,32,33,34,35,36,37]. Open surgical treatment was primarily indicated in cases of delayed diagnosis, ongoing bleeding, or failed endovascular management. Despite therapeutic advances, the overall morbidity and mortality associated with these vascular complications remain high, with a combined rate of approximately 18% [2,20].
3.3. Risk Factors
Anatomical and procedural factors have been associated with an increased risk of vascular injury following proximal femur fracture fixation. The deep femoral artery and its branches, due to their close anatomical proximity to the femoral shaft and lesser trochanter, are particularly vulnerable during drilling, screw placement, or nail insertion [1,2,37]. Risk is further elevated in cases involving displaced lesser trochanter fragments or fragment migration, which may cause direct arterial laceration [3,5,32,34]. Additional procedural risks include over-drilling, excessive screw length, incorrect trajectory, and implant mispositioning [1,10,33]. Several recent case reports illustrate these complications in contemporary practice, including delayed pseudoaneurysm of the deep femoral artery after intertrochanteric fracture fixation [38,39,40], pseudoaneurysm of the lateral femoral artery after pertrochanteric fracture fixation [41], and profunda femoris artery injury following proximal femoral fracture fixation [42]. Similar iatrogenic injuries have also been described, including a guide pin–related vascular complication and a profunda femoris artery pseudoaneurysm secondary to a displaced lesser trochanter fragment treated by coil embolization [41,43].Patient-related factors such as advanced age, severe osteoporosis, pre-existing vascular disease, and anticoagulant use may also contribute to vessel fragility and delayed diagnosis [1,2,4]. Inadequate intraoperative fluoroscopic control and lack of awareness of arterial landmarks further increase the likelihood of iatrogenic injury [11,19,37]. A comprehensive understanding of femoral vascular anatomy, meticulous surgical technique, and proper implant selection are essential to minimize these complications.
Among the 209 patients analyzed, 200 vascular injuries (95.69%) were considered iatrogenic. Of these, 28.71% (n = 60) were caused by bone fragments, most frequently the lesser trochanter (96.67% of cases). In 32.54% cases (n = 68), vascular damage resulted from uncontrolled drill bit advancement or the use of excessively long screws. Additional reported mechanisms included traction on the orthopedic table (4 cases), insertion of guidewires or reamers (8 cases) [22], the use of a retractor (1 case), ender elastic nails (1 case), an external fixator screw (1 case), and intrapelvic migration of screws (4 cases). In 53 patients, the precise cause could not be definitively identified, although uncontrolled drilling was the most frequently suspected mechanism [1,2,3,4,5,6,8,9,10,11]. A combined pseudoaneurysm and arteriovenous fistula of a branch of the profunda femoris artery after hip fracture fixation, successfully treated by endovascular embolization, was recently reported by Castelli Jr et al. (2022), illustrating the spectrum of vascular lesion types encountered [44].
3.4. Preventive Considerations
- Preoperative vascular assessment—Patients with visible arterial calcifications on radiographs or known vascular comorbidities may benefit from preoperative vascular imaging, such as Doppler ultrasound or CT angiography, to evaluate arterial proximity and fragility [1,2,37].
- Management of the lesser trochanter fragment—In cases with significant medial displacement, surgical reduction or excision of the lesser trochanter can reduce the risk of delayed arterial erosion, particularly of the deep femoral artery [3,5,32].
- Instrumentation control—The use of drill stops, proper intraoperative measurement of screw length, and multiplanar fluoroscopic verification during implant placement are essential to prevent arterial penetration [1,10,33].
- Postoperative surveillance—A sudden drop in hemoglobin levels, expanding hematoma, or persistent thigh pain should prompt immediate imaging evaluation (Doppler ultrasound or CT angiography). Clinicians should also be aware that beta-blocker therapy may mask tachycardia, potentially delaying recognition of internal bleeding [2,20].
- Interdisciplinary collaboration—Early involvement of vascular surgeons and imaging specialists is strongly recommended in suspected or confirmed cases to ensure timely diagnosis and appropriate management [9,19,20].
3.5. Limitation
One limitation of our report is that we did not directly measure or demonstrate the displacement of vessels and soft tissues under traction table positioning. Future cadaveric or imaging-based modeling studies simulating standard positions on the traction table would be valuable to quantify such displacements and to better understand the risk of vascular injury during proximal femur osteosynthesis. These aspects would be valuable from didactic and educational perspective.
4. Conclusions
Vascular injuries associated with proximal femur fracture fixation are rare but potentially life-threatening events. The profunda femoris artery and its branches are particularly vulnerable due to their close anatomical relationship with the femoral cortex, surgical implants, and displaced fracture fragments—especially the lesser trochanter. Iatrogenic injury may occur intraoperatively through uncontrolled drilling or improper screw placement, or postoperatively due to secondary displacement or hardware migration.
This case presentation underscores the critical role of detailed preoperative planning, precise surgical technique, and high vigilance during and after surgery. Early recognition of vascular injury—guided by clinical signs such as unexplained anemia or expanding hematoma, and confirmed by Doppler ultrasound or CT angiography—is essential for timely intervention and favorable outcomes. Importantly, our findings suggest that intraoperative maneuvers, such as axial traction and internal rotation on the orthopedic traction table, may significantly alter the spatial relationship between the profunda femoris artery and the femoral diaphysis. This positional shift can bring the vessel closer to the drill or screw trajectory, increasing the risk of vascular injury. Surgeons should be aware of both anatomical and dynamic risk factors, particularly in elderly patients with fragile vasculature or atypical fracture patterns.
Author Contributions
Conceptualization, R.B., S.D.C. and A.T.; methodology, R.B.; investigation, R.B.; writing—original draft preparation, R.B., A.T. and S.D.C.; writing—review and editing, R.B., A.T. and S.D.C.; supervision, S.D.C.; project administration, R.B.; funding acquisition, R.B. All authors have read and agreed to the published version of the manuscript.
Funding
The work was funded by University of Oradea, Romania.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board and the Ethical Council of the Emergency County Clinical Hospital, Oradea, Bihor, Romania (no. 39135/09.11.2023 and 39657/15.11.2023).
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Barquet, A.; Gelink, A.; Giannoudis, P.V. Proximal Femoral Fractures and Vascular Injuries in Adults: Incidence, Aetiology and Outcomes. Injury 2015, 46, 2297–2313. [Google Scholar] [CrossRef]
- Segal, D.; Yaacobi, E.; Marom, N.; Feldman, V.; Aliev, E.; Palmanovich, E.; Bartal, G.; Brin, Y.S. The Incidence of Life Threatening Iatrogenic Vessel Injury Following Closed or Open Reduction and Internal Fixation of Intertrochanteric Femoral Factures. Int. Orthop. 2017, 41, 1845–1850. [Google Scholar] [CrossRef] [PubMed]
- Regus, S.; Lang, W. Arterial Injury and Pseudoaneurysm Formation after Lesser Trochanter Fracture. Int. J. Surg. Case Rep. 2015, 14, 4–6. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Orapiriyakul, W.; Chewakidakarn, C.; Dissaneewate, K.; Dissaneewate, P.; Kritsaneephaiboon, A. Silent Iatrogenic Pseudoaneurysm after Intertrochanteric Fracture Fixation with Proximal Femoral Nailing and Cerclage Wiring: Case Report and Review of Literature. Eur. J. Orthop. Surg. Traumatol. Orthop. Traumatol. 2023, 33, 2667–2681. [Google Scholar] [CrossRef] [PubMed]
- Potenza, V.; Saputo, U.; Catellani, F.; Farsetti, P.; Caterini, R. Laceration of a Branch of the Profunda Femoris Artery Caused by a Spike of the Displaced Lesser Trochanter in an Inter-Trochanteric Femoral Fracture. A Case Report. Int. J. Surg. Case Rep. 2016, 24, 195–198. [Google Scholar] [CrossRef]
- Samaan, M.; Idres, F.A.; Hawa, Y.; Madania, M. Late Deep Femoral Artery Injury after Intertrochanteric Hip Fracture Treatment: A Case Report. Int. J. Surg. Case Rep. 2023, 105, 107983. [Google Scholar] [CrossRef]
- Agustín, M.R.; Sauras, Á.C.; Granados, A.C.U.; Fuentes, J.G.; Reyes, L.I.; García, M.R. Seudoaneurisma de la arteria femoral lateral: Revisión sistemática a propósito de una complicación infrecuente en pacientes con fracturas pertrocantéricas. Rev. Asoc. Argent. Ortop. Traumatol. 2022, 87, 95–110. [Google Scholar] [CrossRef]
- Kim, J.S.; Lee, S.A.; Chee, H.K.; Hwang, J.J.; Kim, H.Y.; Kim, J.Y.; Choi, S.M.; Kim, Y.H.; Lee, W.S. Femoral Arteriovenous Fistula Associated with Surgery of Proximal Femoral Fracture: A Systematic Review of the Literature and Case Presentation. Ann. Transl. Med. 2020, 8, 291. [Google Scholar] [CrossRef]
- Vande Voorde, K.; Dauwe, J.; Van Oost, J. Late Presentation of an Iatrogenic Pseudoaneurysm of the Profunda Femoris Artery Following Intramedullary Nailing. Case Rep. Orthop. 2018, 2018, 8270256. [Google Scholar] [CrossRef]
- Yoon, H.K.; Oh, H.C.; Park, J.; Oyunbat, C.; Kim, T. Rupture of the Deep Femoral Artery during Proximal Femoral Nailing Following an Intertrochanteric Fracture: A Case Report. Hip Pelvis 2016, 28, 54–59. [Google Scholar] [CrossRef]
- Zhang, B.-F.; Cong, Y.-X.; Wang, P.-F.; Huang, H.; Wang, H.; Zhuang, Y. Deep Femoral Artery Branch Pseudoaneurysm Formation and Injury after Hip Fracture Surgery. Medicine 2018, 97, e9872. [Google Scholar] [CrossRef]
- Bowden, S.; Jaberi, A.; Roche-Nagle, G. Large Pseudoaneurysm Arising from the Deep Femoral Artery after Hip Fracture Fixation. J. Surg. Case Rep. 2020, 2020, rjaa408. [Google Scholar] [CrossRef]
- Hamdulay, K.; Beresford, T. Profunda Femoris Pseudoaneurysm Rupture Post Dynamic Hip Screw Fixation after Physiotherapy. Ann. R. Coll. Surg. Engl. 2021, 103, e81–e84. [Google Scholar] [CrossRef] [PubMed]
- Lal, A.; Jesudason, E.; Gwyn, R. Iatrogenic Injury to Profunda Femoris During a Dynamic Hip Screw Fixation for Intertrochanteric Fracture. Cureus 2023, 15, e33894. [Google Scholar] [CrossRef] [PubMed]
- Runge, N.E.; Sanii, R.; Kasto, J.; McCall, D.P. Pseudoaneurysm Development after Short Cephalomedullary Femoral Nailing: A Case Report. J. Orthop. Rep. 2024, 3, 100265. [Google Scholar] [CrossRef]
- Elzayat, M.; Ahmed, A.; O’Connell, J.; Davitt, S.; O’Neill, B.J. Pseudoaneurysm as a Complication of Femur Fracture Fixation. J. Orthop. Case Rep. 2025, 15, 146–149. [Google Scholar] [CrossRef]
- Toyota, T.; Horiuchi, H.; Takizawa, T.; Yamazaki, I.; Matsunaga, D.; Nakamura, Y.; Akizuki, S. A Case of Femoral Pseudoaneurysm after Surgery for Intertrochanteric Fracture. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 2017, 22, 362–365. [Google Scholar] [CrossRef]
- Murata, K.; Nagira, K.; Ishida, K.; Hayashi, I.; Okuno, M.; Nagashima, H. Pseudoaneurysms after Osteosynthesis of Hip Fractures: A Report of Two Cases and a Review of the Literature. JOS Case Rep. 2023, 2, 113–117. [Google Scholar] [CrossRef]
- Khoshnevis, J.; Sobhiyeh, M.R.; Fallah Zavareh, M. Deep Femoral Artery Branch Pseudoaneurysm After Orthopedic Procedure Requiring Surgical Treatment: A Case Report. Trauma Mon. 2012, 17, 305–308. [Google Scholar] [CrossRef]
- Neubauer, T.; Grechenig, S.; Leitner, L.; Auffarth, A.; Plecko, M. Vascular Complications in Plating of the Proximal Femur: Review. Arch. Orthop. Trauma Surg. 2016, 136, 539–551. [Google Scholar] [CrossRef]
- Arbeloa-Gutierrez, L.; Arenas-Miquelez, A.; Muñoa, L.; Gordillo, A.; Eslava, E.; Insausti, I.; Martínez de Morentin, J. Lateral Circumflex Femoral Artery False Aneurysm as a Complication of Intertrochanteric Hip Fracture with Displaced Lesser Trochanter. J. Surg. Case Rep. 2019, 2019, rjz184. [Google Scholar] [CrossRef]
- Kim, J.W.; Lee, J.I.; Park, K.C. Pseudoaneurysm of the Deep Femoral Artery Caused by a Guide Wire Following Femur Intertrochanteric Fracture with a Hip Nail: A Case Report. Acta Orthop. Traumatol. Turc. 2017, 51, 266–269. [Google Scholar] [CrossRef]
- Lee, P.Y.F.; Rao, P.V.R.; Golding, D.M.; Brock, J. Delayed Profunda Femoris Artery Bleeding After Intramedullary Nailing of an Unstable Intertrochanteric Fracture: A Case Report. JBJS Case Connect. 2017, 7, e60. [Google Scholar] [CrossRef] [PubMed]
- Lidder, S.S.; Epstein, D.J.; Courtice, V.; George, M.D. Proximal Femoral Erosion: A Sequelae of Psuedoaneursym Formation Following Operative Fixation of an Intertrochanteric Neck of Femur Fracture. Indian J. Orthop. 2019, 53, 479–481. [Google Scholar] [CrossRef] [PubMed]
- Mayurasakorn, C.; Phiphobmongkol, V.; Sridermma, W.; Bavonratanavech, S. Profunda Femoris Artery Injury Caused by Lesser Trochanter Fragment in Intertrochanteric Fracture: A Case Report. Trauma Case Rep. 2018, 13, 14–17. [Google Scholar] [CrossRef]
- Pandey, N.N.; Raju, S.N.; Rajagopal, R.; Kumar, S. Iatrogenic Profunda Femoris Artery Pseudoaneurysm: Late Presentation with Successful Endovascular Microcoil Embolisation. BMJ Case Rep. 2018, 11, e228314. [Google Scholar] [CrossRef]
- Piolanti, N.; Giuntoli, M.; Nucci, A.M.; Battistini, P.; Lisanti, M.; Andreani, L. Profunda Femoris Artery Pseudoaneurysm after Intramedullary Fixation for a Pertrochanteric Hip Fracture. J. Orthop. Case Rep. 2017, 7, 74–77. [Google Scholar] [CrossRef]
- Kulshrestha, V.; Dhillan, R.; Sood, M. Unusual Presentation of a Profunda Femoris Pseudoaneurysm Following Osteosynthesis of Proximal Femur Fracture. J. Mar. Med. Soc. 2020, 22, 87. [Google Scholar] [CrossRef]
- Harvey, L.S.; Langdon, S.; Lao, D.J.; Jim, J.; Lund, E.A.; Busel, G.A. Femoral Artery Pseudoaneurysm from Heterotopic Ossification after Fixation of Intertrochanteric Hip Fracture: A Case Report. J. Orthop. Case Rep. 2024, 14, 67–72. [Google Scholar] [CrossRef]
- Kulkarni, S.L.; Daragad, M.; R, R.; Manoj, N. A Rare Case of Pseudoaneurysm of Profunda Femoris Artery Following Surgical Fixation of an Intertrochanteric Fracture. J. Orthop. Case Rep. 2025, 15, 174–178. [Google Scholar] [CrossRef]
- Patel, P.V.; Patel, J.S.; Parmar, S.C. Pseudoaneurysm of the Profunda Femoris Artery Following Hip Surgery. Int. Surg. J. 2023, 10, 1103–1105. [Google Scholar] [CrossRef]
- Čičak, S.; Kocur, J.; Farkaš, V.; Čičak, P.; Ištvanić, S.; Lovrić, M.; Perić, M.; Koruga, N.; Ištvanić, T. Delayed Deep Femoral Artery Injury Secondary to Migrated Lesser Trochanter Fragment After Intertrochanteric Fracture Fixation: A Case Report and Updated Literature Review. Geriatr. Orthop. Surg. Rehabil. 2025, 16, 21514593251351188. [Google Scholar] [CrossRef]
- Gong, J.; Liu, P.; Cai, M. Imaging Evaluation of the Safe Region for Distal Locking Screw of Proximal Femoral Nail Anti-Rotation in Patients with Proximal Femoral Fracture. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2017, 23, 719–724. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Montoli, C.; Pasquali, C.; Paiusco, E.; Pellecchia, V.; Vulcano, E. Lesser Trochanter Migration Following Intramedullary Fixation of an Intertrochanteric Femur Fracture. Case Rep. Orthop. 2016, 2016, 9348032. [Google Scholar] [CrossRef] [PubMed]
- Valli, F.; Teli, M.G.; Innocenti, M.; Vercelli, R.; Prestamburgo, D. Profunda Femoris Artery Pseudoaneurysm Following Revision for Femoral Shaft Fracture Nonunion. World J. Orthop. 2013, 4, 154–156. [Google Scholar] [CrossRef] [PubMed]
- Craxford, S.; Gale, M.; Lammin, K. Arterial Injury to the Profunda Femoris Artery Following Internal Fixation of a Neck of Femur Fracture with a Compression Hip Screw. Case Rep. Orthop. 2013, 2013, 181293. [Google Scholar] [CrossRef]
- Sun, Q.; Fan, G.; Li, X.; Gong, J.; Ge, W.; Cai, M. Relationship Between Femur and Femoral Arteries for Identifying Risk Factors for Vascular Injury. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2017, 23, 1733–1740. [Google Scholar] [CrossRef]
- Kim, B.-S.; Kim, S.-T.; Shin, S.; Yu, C.G. Delayed Pseudoaneurysm of Deep Femoral Artery Caused by Migration of Lesser Trochanter, Subsequent to an Intertrochanteric Fracture Surgery—A Case Report. J. Musculoskelet. Trauma 2021, 34, 76–79. [Google Scholar] [CrossRef]
- Jain, V.T.; Katariya, J.; Archik, S. Pseudoaneurysm of Profunda Femoris Artery: A Rare Complication after Intramedullary Fixation for an Intertrochanteric Femur Fracture. Int. J. Res. Orthop. 2019, 5, 969–973. [Google Scholar] [CrossRef]
- A Platform for Scientific Journals and Research Publications. Available online: https://ecronicon.net/assets/ecor/pdf/ECOR-14-01048.pdf (accessed on 18 September 2025).
- Cho, H.M.; Heo, H.; Jung, M.C. Iatrogenic Injury to the Descending Branch of the Lateral Circumflex Femoral Artery during Intertrochanteric Fracture Fixation: A Case Report of Guide Pin-Related Vascular Complication. Acta Orthop. Traumatol. Turc. 2025, 59, 237–240. [Google Scholar] [CrossRef]
- Beckett, N.C.; Haglin, J.; Van Schuyver, P.; Spangehl, M.J.; Kalani, M.A.; Lyons, M.K.; Bathini, A.R.; Bingham, J.S. Traumatic Disruption of Profunda Femoris Artery Branch Following Treatment of an Intertrochanteric Hip Fracture With a Cephalomedullary Nail. Case Rep. Orthop. 2024, 2024, 5590091. [Google Scholar] [CrossRef]
- Huh, S.H.; Cho, H.-M.; Park, J. Injury of the Ascending Branch of the Lateral Femoral Circumflex Artery Caused by a Spike of the Displaced Lesser Trochanter in an Intertrochanteric Femoral Fracture: A Case Report. J. Korean Fract. Soc. 2021, 34, 71. [Google Scholar] [CrossRef]
- Castelli, V.; Faustino, C.B.; Fioranelli, A.; Volpiani, G.; Park, J.H.; Santos, V.P.; Wolosker, N. Pseudoaneurysm and Arteriovenous Fistula of the Deep Femoral Artery after Complete Rupture of the Vastus Medialis Muscle: Endovascular Treatment. J. Vasc. Bras. 2022, 21, e20190001. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).