Abstract
The Latin American Renal Cancer Group (LARCG) was founded in 2013. This is a non-profit collaborative group designed to foster scientific knowledge in all areas of kidney cancer, and to establish international cooperation among well-recognized oncologic institutions. Since its creation, LARCG has reported data from Latin America to the scientific community and has promoted accredited information and advocacy principles for patients, lay people, and medical colleagues. Currently, it consists of 44 centers in 7 Latin American countries and Spain. In this paper, we report our achievements in assistance, teaching, research, and advocacy, and we discuss the successful international collaborations.
Introduction
We created the LARCG (Latin American Renal Cancer Group) in 2013 to address the paucity of renal cell carcinoma (RCC) data in Latin America when compared with North America and Europe and to address the differences between the regions with respect to ethnic composition and health care systems[1]. LARCG is a non-profit collaborative group designed to foster scientific knowledge in all areas of kidney cancer, to produce high-quality scientific information, to establish international cooperation with well-recognized oncological institutions, to report data from Latin America to the scientific community, and to promote accredited information and advocacy principles to patients, lay people, and medical colleagues.
Since its creation, LARCG has grown and incorporated more centers, expanding its activities in several scenarios, in ways unusual for Latin America. In this manuscript, we aimed to report our achievements, divided by subtopics, discussing our future activities.
Creation, Expansion, and Economical Support of the Group and Our Database
The LARCG group was created by urologists, under the guidance of a specific statute. Our board has scientific, ethics, and economic committees. In each participating institution, LARCG is led by a local urologist, who invites other urologists, pathologists, medical oncologists, and radiologists to integrate their institutional departments into LARCG’s branches of pathological anatomy, medical oncology, and imaging, respectively[1].
Soon after our foundation in 2014, we invited selected key opinion leaders from recognized high-quality urologic oncology centers in Central and South America, and Spain. Within a few weeks, 26 centers had joined the group. Retrospectively, we developed a comprehensive encrypted database containing more than 150 variables, with demographic, clinical, and pathological information, therapeutic modalities, and oncological and functional outcomes of 4502 RCC patients from 22 Latin American and 2 Spanish institutions.
In November 2014, we presented the results of our survival analysis of 4238 patients at the plenary session of the Confederación Americana de Urologia meeting in Punta Del Este, Uruguay[1,2]. Between 2014 and 2016, the group expanded to its current composition (44 centers from Argentina, Brazil, Bolivia, Chile, Mexico, Peru, Spain, and Uruguay). At the same time, we developed a bilingual (English/Spanish) website (available at https://larcg.org)[3].
During 2014, data of patients treated since 1980 were retrospectively entered by each participating institution. Subsequently, information was received about patients treated until 2016, resulting in more than 6000 cases.
The inclusion criteria for participation in the LARCG group were first, to accept the invitation, with the commitment to send the required information and the promise to follow our statute rules.
We sought to enhance the quality of our database, removing the repeated cases, searching information for missing values, and starting the development of a free, secure, and encrypted database in the Research Electronic Data Capture (RED Cap) (Vanderbilt University)[4]. Only centers that adhered to these security database policies were accepted.
In the third—and current—phase, launched in 2020, we have received new cases from Chile, and we are also accepting prospective information. Concurrently, we are updating the original database, requiring follow-up information from each center, and encouraging them to include new cases.
The chronological flow presenting the expansion of our database and the diagram of its current structure are represented in Figure 1 and Figure 2, respectively.
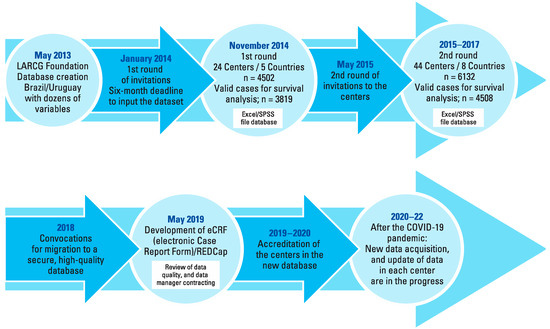
Figure 1.
Chronological diagram for the expansion of the LARCG database.
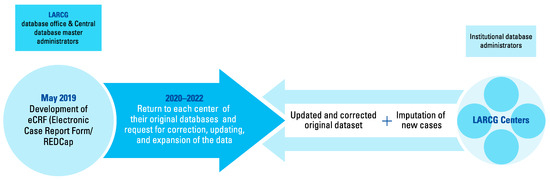
Figure 2.
Flowchart of the current structure of the LARCG database.
In May 2015, we presented our epidemiological data and administrative information at the SWOG fall meeting in San Francisco, California. This was a key event to increase our networking with urologic oncology leaders, resulting in some scientific collaborations[1,5].
Up to 2014, we had no sponsorship from industry, and all efforts to create the LARCG were voluntary (unpaid). In 2016, the LARCG Project was classified as a strategic initiative by the A.C. Camargo Cancer Center (ACCCC), Brazil, and encompassed in a comprehensive project entitled INCITO-INOTE (Instituto Nacional de Ciência e
Tecnologia em Oncogenômica e Inovação Terapêutica) (National Institute for Therapeutic Innovation and Oncogenetics), founded by several official governmental and private Brazilian funding agencies, which support cancer research in that hospital[6].
The funds provided by the INCITO/INOTE project have covered the costs of our basic and translational investigations, as well as the acquisition of immunohistochemistry reagents, biomolecular analyses, and laboratory supplies. Additionally, we received funds from INCITO/INOTE for the maintenance of our website, for the payment of audiovisual resources used during the LARCG annual meetings at American Urological Association meetings[3,7]. These funds also covered travel expenses to bring international speakers to our Brazilian events, promoted by ACCCC. These funds are in place until 2023, when new applications will be made to the official funding agencies.
Other meetings were promoted by the LARCG group. They occurred at Hospital Pasteur (Montevideo, Uruguay) and Hospital Británico (Buenos Aires, Argentina), and an advocacy event took place in Mexico City, funded by Asociación Ale[1]. These meetings were supported by each regional promoter center. The Kidney Cancer Association supported the expenses of the authors D.A. and S.C.Z. at the 17th and the 18th Kidney Cancer Symposiums, respectively[8].
In 2021, the Uruguayan LARCG team established the LARCG Foundation in that country. It is a non-profit virtual organization that received economic resources from the pharmaceutical industry (Roche Company) to cover database maintenance and the data managers’ salaries. This regional foundation receives donations for scientific initiatives through our website[3].
Finally, we reiterate that the LARCG members have received no salaries or professional fees for any of their activities. In collaborative studies among the centers, each center must cover its expenses.
Research
Prognostic factors: clinical markers
In the search of prognostic clinical markers in RCC, we evaluated patients with localized or locally advanced RCC, and patients with metastatic disease, reporting the prognostic factors in patients from Latin America.
In a survival analysis of 5670 patients with non-metastatic disease, using a multiple data imputation method to compensate for the effect of missing values, we demonstrated that the American Society of Anesthesiologists (ASA) classification ≥ 3 and the perirenal fat invasion, aside from other well-known factors, were independent predictors for worse overall survival (OS). Perirenal fat invasion and microvascular invasion were adverse prognostic factors for cancer-specific survival (CSS)[9]. In 2010, we published a study showing that patients with ASA classification ≥ 3 presented more symptomatic tumors, higher nuclear grade, and larger lesions, besides of 10 times more metastasis than ASA 1, and the double those ASA 2. In the multivariable analysis, ASA classification was an independent predictor of OS for the whole cohort, and CSS for the patients with non-metastatic RCC[10].
The ASA classification takes account the comorbidities of the patients, which is not incorporated in the most used performance status classification in oncology. As RCC is a metabolic disease[11], it seems logical that comorbidities could influence the outcomes of RCC patients. Additionally, ASA classification is a classification recognized worldwide that can be validated in many institutions, without the potential biases related to the assistant surgeons.
In a series of 1523 small renal masses, we reported that ASA ≥ 3, bilateral tumors, and extracapsular invasion were adverse independent prognostic factors for disease recurrence and metastases. In this study, patients ≥ 65 had a better 10-year OS if they underwent partial nephrectomy rather than radical nephrectomy[12]. With respect to age, these results are in accordance with those of the Mexican LARCG team, which evaluated 410 patients who underwent surgery. They demonstrated that patients > 75 years presented outcomes similar to those of their younger counterparts[13]. According to these series, we can verify that Latin American countries are progressively increasing their rates of minimally invasive nephron-sparing surgeries, resulting in inherent benefits, such as reduced length of hospital stay, reduced bleeding and transfusion rates, and reduced pain or use of analgesics, as well as an earlier return to daily routine.
In an Argentinian series of 293 patients, the concomitant invasion of perirenal fat and renal sinus invasion was associated with an unfavorable setting for pT3a tumors. This is associated with higher mortality rates, venous involvement, and metastatic progression[14]. This study suggests a need for a subdivision of T3 stage, indicating that the concomitant fat and venous invasion present an ominous prognosis in comparison with any of these factors in isolation[15].
Recently, the Uruguayan LARCG team, in collaboration with several recognized global experts in RCC, published their prognostic score in 530 de novo metastatic patients. It was a unique database, since 511 patients underwent nephrectomy, probably consisting of those in the more favorable risk group. In this series, the ASA classification ≥ 3, perirenal fat invasion, and more than 2 metastatic lesions were associated with poor 5-year OS and CSS. The authors presented a prognostic score, ranging from 0 to 3 points, being: 0 point: favorable group; 1 point: intermediary group; and 2 or 3 points: unfavorable group, which achieved the following median survivals: not reached, 33 months, and 14 months, respectively. In this population, patients with bone metastases, particularly those with non-vertebral lesions had better OS. These data deserve further investigation[16].
Validating the ASA classification, perirenal fat invasion, and bone metastases as prognostic factors in other populations would be interesting and valuable, in order to extend resources in these areas.
Immunochemistry markers
A project called LARCG 001 was launched, encompassing the analyses of several potential immunohistochemical (IHC) markers associated with “endocrine kidney enzymes” and with chromatin remodeling genes. We demonstrated that the low IHC expression of erythropoietin (EPO) was an independent adverse prognostic factor for OS and disease-free survival (DFS) in 220 patients with localized or locally advanced RCC (all histological types included)[17]. Furthermore, the lack of renin (REN) expression was an independent prognostic factor for DFS, with almost 3 times more recurrences than those expressing REN. This study analyzed 498 patients with non-metastatic clear cell RCC (ccRCC), in collaboration with the University of California Davis (UCD)[18]. In both studies, low expression of EPO or REN was associated with unfavorable pathological features, such as higher TNM stages, higher nuclear grades, and larger lesions. The area of renal endocrine markers in RCC has been insufficiently studied enough and could open a new route of research. We are currently analyzing the concomitant expression of REN, EPO, and cathepsin D, an alternative renin-angiotensin pathway activator, in more than 700 patients (data not published).
Motivated by the new era of check-point inhibitors in RCC, we investigated the prognostic role of the IHC expression of the check-point markers (PD-L1 and PD-1) in collaboration with Lee Moffitt Cancer Center (Tampa, FL). In a series of 1017 patients with non-metastatic ccRCC (follow-up data available in 738 cases), the higher expression of these markers was associated with higher tumor stages, intratumoral necrosis, and lymph-vascular invasion. In a multivariable analysis, the expression of PD-L1 was associated with double the cancer-specific mortality compared with PD-L1-negative cases. We hypothesized that this marker could aid in stratifying high-risk patients for adjuvant treatment or selecting candidates for immunotherapy[19].
Regarding chromatin remodeling genes, our previous studies revealed that BAP-1 and PBRM-1 were strong predictors of unfavorable outcomes in localized or locally advanced ccRCC. In a conjugated analysis of 441 patients with non-metastatic ccRCC, the concomitant low expression of BAP-1 and PBRM-1 was associated with higher mortality rates and double the number of recurrences when compared with patients presenting both or only one of the markers expressed[20]. Additionally, in 2019, we reported that the low IHC expression of BAP-1 and PBRM-1 in 124 metastatic samples was an unfavorable feature for patients who underwent metastasectomy. In this study, the low expression of BAP-1 was independently associated with 60% higher mortality and 93% more recurrences. On the other hand, the isolated PRBM-1 immunostaining status did not influence the outcomes in the multivariate analysis[21].
In a retrospective review of 662 patients with primary or metastatic ccRCC, the low expression of SETD-2, another chromatin remodeling gene, was associated with higher cancer mortality and recurrence[22]. Finally, the negative expression of ezrin, an epithelial-mesenchymal transition marker, was associated with poor survival rates in a series of 567 patients with localized or locally advanced ccRCC[23].
Intending to conclude the LARCG 001 project, we will analyze the IHC expression of PTEN, and we need to validate the nitric oxide synthase 3 (NOS-3) expression. In a limited series of 110 patients with diverse RCC histologies, high expression of NOS-3 was associated with unfavorable pathological features worse, OS in univariate analysis (58.1% versus 79.4%; P = 0.033)[24].
Translational research: international collaboration groups
Regarding translational research, we developed a patient-derived xenograft (PDX) project performed in immunodeficient mice at ACCCC in collaboration with UCD. We were able to reproduce the anatomo-pathological and genetic features of the original tumors in 27% of the cases. A more intense gene expression was evidenced, probably due to the intratumoral heterogeneity or the immunodeficiency in the animal models. The most impressive was the resemblance of venous thrombus in 5 consecutive generations originated from one animal[25]. These PDX models can be an opportunity for testing future drugs or planning adjuvant treatment in patients with advanced disease. Once this technique is standardized, we can deliver it in other LARCG centers in the future.
Recently, ACCCC (São Paulo), Hospital Pasteur (Montevideo), and Hospital Italiano (Buenos Aires) sent more than 1500 DNA aliquots from RCC patients, and 700 DNA aliquots from healthy control samples, in collaboration with the continuation of the Genome Wide Association Study project from the American National Cancer Institute (NCI), part of the National institutes of Health. This international multicenter collaborative research encompasses the most recognized institutions in the RCC scenario around the world[26]. In this study, there were dedicated funds to each LARCG participating institutions provided by the NCI to this project.
In support of continuing medical education and best practices, there was cooperation between LARCG and the Latin American Cooperative Oncology Group (LACOG), promoting expert meetings in 2019 that resulted in 2 manuscripts with recommendations for the best surgical and systemic management[27,28]. An update meeting was held in the second half of 2022.
Multicentric prospective studies
LARCG has developed a multicenter prospective study, led by Hospital Italiano from Buenos Aires. They are investigating the 10-year outcomes of patients in active surveillance with small renal masses, including those who refused surgical or percutaneous treatments. This trial was initiated in 2018, and currently has more than 140 enrolled patients[3].
Teaching
One of the LARCG scopes is to offer the opportunity for international observerships in worldwide recognized institutions to young colleagues (urologists or medical oncologists). Since 2017, there has been an agreement (Residents & Young Doctors Rotation Program) between the LARCG and the Department of Medical Oncology and Therapeutics Research from City of Hope Comprehensive Cancer Center, in Duarte, headed by Professor Sumanta Kumar Pal[29]. Yearly, 4 young colleagues (2 urologists and 2 medical oncologists) from ACCCC and other LARCG centers are selected for a 2-month rotation program at the City of Hope. The COVID-19 pandemic interrupted the program in 2020.
According to this agreement, the travel expenses are supported by the Californian Cancer Center. During this period, the observers can participate in clinic activities, become familiar with the routine of clinical trials, participate on tumor boards, participate in inpatient visits, and collaborate on the preparation of scientific manuscripts. This is a unique opportunity to get world class knowledge in RCC and in the clinical management of urological malignancies. Six Brazilian and 2 Argentinian young professionals have benefited from this program. We hope to promote similar educational initiatives for our members in the future.
Advocacy
In Latin American, oncology patients are not commonly well-informed about treatments and their implications. However, in the face of regional socioeconomic limitations and disparities, some educational and advocacy initiatives are necessary.
As a result, the International Kidney Cancer Coalition (IKCC) contacted the LARCG to foster advocacy with kidney cancer patients in Latin America between 2017 and 2018[30]. Immediately, we organized several meetings in Mexico, involving patients, associations, medical experts, the press, and lawyers. They debated aspects of the inequities in health assistance and the limited access to some medications or procedures. There was an exchange of information among 48 RCC patients’ organizations from all continents.
LARCG has contributed to the dissemination of information to lay people about kidney cancer risk factors, symptoms, and treatments. The group’s other task is to demystify clinical trials in this population, clarifying for them that participation in a clinical trial may be an opportunity to collaborate with scientific development and to receive the best available therapeutic options. Meetings have also occurred in São Paulo and Lisbon, and a recent report was published regarding these meetings[31].
Additionally, we published a study revealing that uninsured patients with metastatic disease in Brazil receive fewer second- or third-line therapies, or even receive less effective therapies in comparison with insured or private patients. This was based on a survey using a commercial database with more than 4000 patients[32]. In other evaluation with 273 patients with metastatic disease at a tertiary center, we demonstrated that uninsured patients have more advanced disease, worse performance status, and are less likely than insured patients to undergo nephrectomy or systemic therapies[33].
Since 2017, IKCC has promoted the annual World Kidney Cancer Day (WKCD), with awareness campaigns, surveys, educational brochures, and websites in 14 languages. Each year, the WKCD promotes provocative debates for questions associated with the daily life of the patients, many of which are underreported. LARCG has actively participated in the WKCD, and launched the 2019 campaign in Latin America. Again in June, the IKCC and LARCG joined together again for the 2022 WKCD, whose theme was “We must discuss therapeutic options”[34].
Conclusion
LARCG was intended to enhance knowledge of and promote information about RCC. In few years, we have furthered the support, research, teaching, and advocacy for professionals and patients involved with this malignancy. Expanding our network and establishing further collaborations will result in our partners maintaining higher levels of education and technical proficiency, and will benefit Latin American patients affected by kidney malignancies. Clinical trial development is in our future sights.
Conflicts of Interest
None declared.
Abbreviations
| ACCCC A.C. Camargo Cancer Center |
| ASA American Society of Anesthesiologists |
| ccRCC clear cell RCC |
| EPO erythropoietin |
| IHC immunohistochemical |
| LARCG Latin American Renal Cancer Group |
| OS overall survival |
| RCC renal cell carcinoma |
| REN renin |
References
- Zequi, S.C.; Clavijo, D.A. The creation, development and diffusion of the LARCG Latin American renal cancer group. Int. Braz. J. Urol. 2017, 43, 3–6. [Google Scholar] [CrossRef] [PubMed][Green Version]
- XXXIII Congreso CAU, XIX Congreso SIUP, IX Congreso Uruguayo de Urologia, Jornadas Rioplantenses de Urologia. CAU - Confederación Americana de Urología. Available online: https://caunet.org/e-posters-cau-2014/ (accessed on 4 June 2022).
- Latin American Renal Cancer Group Website. Available online: https://larcg.org (accessed on 29 May 2022).
- Research Electronic Data Capture Website. Available online: https://redcapbrasil.com.br (accessed on 29 May 2022).
- Southwest Oncology Group (SWOG) Website. Available online: https://www.swog.org/news-events/swog-meetings (accessed on 10 May 2015).
- Martins, V.R. INCT de oncogenômica e inovação terapêutica. Available online: https://seminarioinct.cgee.org.br/inct-de-oncogenomica-e-inovacao-terapeutica/ (accessed on 27 May 2012).
- American Urological Association Annual Meeting Website. Available online: https://www.auanet.org/annualmeeting (accessed on 20 May 2022).
- Eighteenth International Kidney Cancer Symposium. Kidney Cancer Association (KCA) Meetings. Available online: https://www.kcameetings.org/wp-content/uploads/2020/06/IKCS-2019-Program-Book.pdf (accessed on 4 June 2022).
- Zequi, S.C.; Mourão, T.C.; Oliveira, M.M.; Curado, M.P.; Gueglio, G.; da Costa, W.H.; et al. Predictors of survival outcomes in non-metastatic renal cell carcinoma in Latin America and Spain: a multicentric analysis. Kidney Cancer. 2019, 3, 253–261. [Google Scholar] [CrossRef]
- de Cássio Zequi, S.; de Campos, E.C.; Guimarães, G.C.; Bachega, W., Jr.; da Fonseca, F.P.; Lopes, A. The use of the American Society of Anesthesiology Classification as a prognostic factor in patients with renal cell carcinoma. Urol. Int. 2010, 84, 67–72. [Google Scholar] [CrossRef]
- Linehan, W.M.; Srinivasan, R.; Schmidt, L.S. The genetic basis of kidney cancer: a metabolic disease. Nat. Rev. Urol. 2010, 7, 277–285. [Google Scholar] [CrossRef] [PubMed]
- Mourão, T.C.; Abreu, D.; Carvalhal, G.F.; Gueglio, G.; da Costa, W.H.; Calsavara, V.F.; et al. Small renal masses in Latin-American population: characteristics and prognostic factors for survival, recurrence and metastasis - a multi-institutional study from LARCG database. BMC Urol. 2020, 20, 85. [Google Scholar] [CrossRef] [PubMed]
- Garza-Gangemi, A.M.; Castillejos-Molina, R.A.; Gueglio, G.; Tobia Gonzalez, I.P.; Jurado, A.M.; Meza-Montoya, L.; et al.; Latin American Renal Cancer Group (LARCG) Characteristics and surgical outcomes in very elderly patients (≥75 years) with renal cell carcinoma: data from the Latin American Renal Cancer Group. Rev. Investig. Clin. 2020, 72. [Google Scholar] [CrossRef]
- García Marchiñena, P.; Tobia, I.; Abreu, D.; de Cássio Zequi, S.; Jurado, A.; Gueglio, G.; en representación del grupo Latin American Renal Cancer (LARCG Group). Prognostic value of perirenal and/or sinus fat infiltration in patients with pT3a renal cell carcinoma: A multicentre cohort study. LARCG Group. Actas Urol Esp. (Engl Ed) 2019, 43, 495–502. [Google Scholar] [CrossRef]
- da Costa, W.H.; Moniz, R.R.; da Cunha, I.W.; Fonseca, F.P.; Guimaraes, G.C.; de Cássio Zequi, S. Impact of renal vein invasion and fat invasion in pT3a renal cell carcinoma. BJU Int. 2012, 109, 544–548. [Google Scholar] [CrossRef]
- Abreu, D.; Carvalhal, G.; Gueglio, G.; Tobia, I.; Garcia, P.; Zuñiga, A.; et al. Prognostic factors in de novo metastatic renal cell carcinoma: A Report from the Latin American Renal Cancer Group. JCO Glob. Oncol. 2021, 7, 671–685. [Google Scholar] [CrossRef]
- Ferreira, D.B.; da Costa, W.H.; Clavijo, D.A.; Decia, R.; Cunha, I.W.; Schultz, L.; et al. Tissue expression of erythropoietin predicts survival rates in clear cell renal cell carcinoma. Kidney Cancer. 2017, 1, 143–149. [Google Scholar] [CrossRef]
- de Almeida EPaula, F.; Bezerra, S.M.; da Cunha, I.W.; Munhoz, G.C.; Abreu, D.; Lara, P.N., Jr.; et, a.l. Immunohistochemical expression of renin is a prognostic factor for recurrence in nonmetastatic renal cell carcinoma. Urol. Oncol. 2019, 37, 947–954. [Google Scholar] [CrossRef]
- Chipollini, J.; da Costa, W.H.; Werneck da Cunha, I.; de Almeida EPaula, F.; Guilherme OSalles, P.; Azizi, M.; et al. Prognostic value of PD-L1 expression for surgically treated localized renal cell carcinoma: implications for risk stratification and adjuvant therapies. Ther. Adv. Urol. 2019, 11, 1756287219882600. [Google Scholar] [CrossRef]
- da Costa, W.H.; da Cunha, I.W.; Fares, A.F.; Bezerra, S.M.; Shultz, L.; Clavijo, D.A.; et al. Prognostic impact of concomitant loss of PBRM1 and BAP1 protein expression in early stages of clear cell renal cell carcinoma. Urol. Oncol. 2018, 36, 243.e1–243.e8. [Google Scholar] [CrossRef] [PubMed]
- da Costa, W.H.; Fares, A.F.; Bezerra, S.M.; Morini, M.A.; de Toledo Benigno, L.A.; Clavijo, D.A.; et al. Loss of BAP1 expression in metastatic tumor tissue is an event of poor prognosis in patients with metastatic clear cell renal cell carcinoma. Urol. Oncol. 2019, 37, 78–85. [Google Scholar] [CrossRef]
- Santos, V.E.; da Costa, W.H.; Bezerra, S.M.; da Cunha, I.W.; Nobre, J.Q.C.; Brazão, E.S., Jr.; et, a.l. Prognostic impact of loss of SETD2 in clear cell renal cell carcinoma. Clin. Genitourin. Cancer. 2021, 19, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.V.O.; da Costa, W.H.; Matushita, M.A.M.; Meduna, R.R.; Brazao, E.S.; Bezerra, S.M.; et al. Immunohistochemical negative expression of ezrin predicts poor prognosis in clear cell renal cell carcinoma. Urol. Oncol. 2020, 38, 75.e1–75.e7. [Google Scholar] [CrossRef]
- Cássio Zequi, S.d.; Fregnani, J.H.; Favaretto, R.L.; Costa, W.H.; Madeira Campos, R.S.; Fonseca, F.P.; et al. The impact of immunohistochemical expression of nitric oxide synthases on clinical and pathological features of renal cell carcinoma. World J. Urol. 2013, 31, 1197–1203. [Google Scholar] [CrossRef] [PubMed]
- Beserra, A.O.; Estevan, E.C.; Bezerra, S.M.; Torrezan, G.T.; Ikegami, A.; Dellê, H.; et al. Patient-derived renal cell carcinoma xenografts capture tumor genetic profiles and aggressive behaviors. Kidney Cancer. 2022, 6, 11–22. [Google Scholar] [CrossRef]
- Scelo, G.; Purdue, M.P.; Brown, K.M.; Johansson, M.; Wang, Z.; Eckel-Passow, J.E.; et al. Genome-wide association study identifies multiple risk loci for renal cell carcinoma. Nat. Commun. 2017, 8, 15724. [Google Scholar] [CrossRef]
- de Cássio Zequi, S.; da Costa, W.H.; Korkes, F.; Dos Reis, R.B.; Busato, W.F.S.; Matheus, W.E.; et al. Renal cell cancer treatment: an expert panel recommendation from the Latin American cooperative group-genitourinary and the Latin American renal cancer group: focus on surgery. Ther. Adv. Urol. 2019, 11, 1756287219872324. [Google Scholar] [CrossRef]
- Soares, A.; Monteiro, F.S.M.; Maluf, F.C.; Bastos, D.A.; Jardim, D.L.; Sasse, A.D.; et al. Advanced renal cell carcinoma (RCC) management: an expert panel recommendation from the Latin American Cooperative Oncology Group (LACOG) and the Latin American Renal Cancer Group (LARCG). J. Cancer Res. Clin. Oncol. 2020, 146, 1829–1845. [Google Scholar] [CrossRef] [PubMed]
- City of Hope Comprehensive Cancer Center Website. Available online: https://www.cityofhope.org/academics (accessed on 30 May 2022).
- The International Kidney Cancer Coalition (IKCC) Website. Available online: https://ikcc.org (accessed on 30 May 2022).
- Herrera-Caceres, J.O.; Ajaj, R.; Leão, R.; Barello, S.; Rodriguez-Covarrubias, F.; Zequi, S.C.; et al. Patient-centered care can be improved by joint meetings between cancer patient group leaders and health care providers. Patient Educ. Couns. 2022, 105, 786–787. [Google Scholar] [CrossRef] [PubMed]
- Bergerot, P.G.; Bergerot, C.D.; Dizman, N.; Zequi, S.; Fay, A.; Dara, Y.; et al. Assessment of treatment patterns for metastatic renal cell carcinoma in Brazil. J. Glob. Oncol. 2018, 4, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Leite, L.M.; Bergerot, P.G.; Dettino, A.L.A.; RJAJúnior Zequi, S.C.; Formiga, M.N.D.C. Influence of treatment access on survival of metastatic renal cell carcinoma in Brazilian cancer center. Int. Braz. J. Urol. 2021, 47, 566–573, World Kidney Cancer Day 2022. The International Kidney Cancer Coalition (IKCC). Available online: https://www.worldkidneycancerday.org (accessed on 28 May 2022). [Google Scholar] [CrossRef] [PubMed]
- World Kidney Cancer Day 2022. The International Kidney Cancer Coalition (IKCC). Available online: https://www.worldkidneycancerday.org (accessed on 28 May 2022).
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2023 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.