Highlights
What are the main findings?
- Nurses play a crucial role in the control and treatment of asthma;
- Identify nurses’ interventions for an asthma surveillance consultation in primary health care units.
What is the implication of the main finding?
- The integration of an asthma nursing consultation in PHC;
- Define the role of nurses as integrated providers of asthma-related care.
Abstract
Bronchial asthma is a chronic pathology and a global public health problem. However, asthma can be controlled and treated for the most part by patients, so the Portuguese General Directorate of Health recommends shared medical appointments in primary health care (PHC). The present study aims to identify the role of PHC nurses in the control and treatment of asthma in adults. Using the MeSH platform, the following descriptors were validated: asthma, nurses, adults. An individual search was carried out in the following databases: CINAHL (ESBSCO host), MEDLINE (Pubmed host), Web of Science, and Scopus. Out of a total of 280 publications, 79 of which were duplicates and 185 publications which did not meet the inclusion criteria, 16 publications remained readable. Of the eligible articles, there were 13 specialist reports, one mixed study, one quasi-experimental study, and one randomized trial. Education was the intervention most identified in the scientific evidence analyzed, and patient assessment, application of an asthma control questionnaire, verification and training of inhalation technique, empowerment for self-management of the disease, support, promotion of seasonal influenza vaccination, and use of written action plans were also identified. The results reveal that, although the scientific evidence on the intervention of these professionals is poorly developed, nurses play a crucial role in the control and treatment of asthma. The scientific evidence analyzed allowed the identification of interventions that can help the organization of a nursing health appointment, providing nurses with a crucial role in the control and treatment of asthma in adults in the context of PHC.
1. Introduction
Bronchial asthma is a chronic pathology that affects all ages, with a worldwide prevalence of 9.1% in children, 11% in adolescents, and 6.6% in adults [1]. Hence, asthma is an important individual and public health problem at a global level, with an estimated 262 million people affected by this disease [2], having a significant impact on patients’ quality of life and healthcare systems [3,4,5]. The prevalence of asthma in Portugal is being studied, with the latest results pointing to a prevalence of 6.8% in 2010 [4].
Globally, it is estimated that 22.5 million disease-adjusted life years (DALYs) are lost annually due to asthma [6]. In Portugal, the number of years of life lived with disability (YLD) due to respiratory diseases is about 5%, with asthma being the main condition responsible for this (3.2%) [4].
Asthma is a respiratory disease usually associated with an organic hyper-response to direct or indirect stimuli, presenting as chronic inflammation of the airways, persisting even when lung function is normal and there are no symptoms, but which can be normalized with medication [5]. It is a pathology characterized by symptoms such as wheezing, paroxysmal dyspnea, a feeling of tightness in the chest, cough, or increased expiratory time, and the intensity of these symptoms may vary over time [3,4,5]. These variations are often triggered by factors such as physical exercise, exposure to irritants or allergens, temperature changes, or respiratory infections [5,7]. Asthma can be controlled and treated in most patients, allowing (i) a reduction in the need for reliever medication, (ii) patients that can lead productive and active lives, (iii) the maintenance of near-normal lung function, and (iv) prevention of exacerbations [5]. In this sense, there is evidence that asthma self-management can reduce the use of health services and school/job absenteeism, thus justifying the need to create specific asthma programs [2,8]. Therefore, in 2018, the Portuguese Directorate-General for Health (DGH) issued the Integrated Care Plan (ICP) for Asthma in Children and Adults (aged 14 years and over), which aims to guide and organize clinical practice to improve results and quality. This ICP also aims to achieve the most effective use of resources, emphasizing activities that are thought to affect the quality of care for this pathology [4].
Despite advances in the knowledge of its pathophysiological mechanisms and the existence of several effective therapeutic options for the control of asthma, the goals of treatment are not always achieved [3,5]. Given the importance of asthma monitoring and control, the DGH recommends primary health care (PHC) consultations, where family health units (FHUs) are in a privileged context to structure a consultation based on the ICP and scientific evidence [4]. In this sense, the present systematic review of the literature (SRL) aims to identify the role of PHC nurses in the control and treatment of asthma in adults.
2. Materials and Methods
The SLR protocol was registered with PROSPERO with the code CRD42023455434, and was guided according to the methodological guidelines proposed by the Joanne Briggs Institute (JBI) [9]. As shown in Table 1, the mnemonic PIO (population, interest, and outcome) was considered when constructing the investigation question [10]: What is the role (I) of the PHC nurse (P) in the control and treatment of asthma in adults (O)?

Table 1.
Mnemonic used in this study.
The literature search was carried out based on the descriptors validated in the Medical subject heading platform (MeSH). Considering CINAHL (ESBSCO host), MEDLINE (Pubmed host), Web of Science, and Scopus, we searched for full-text articles in Portuguese, Spanish, and English. To create the search expression, the Boolean operators “AND” and “NOT” were used: asthma AND “nurse* role” NOT child*.
The present study did not consider a specific time frame, as the historical milestones of nurses’ involvement in the consultation of asthma patients remain unknown. The inclusion and exclusion criteria adopted are presented in Table 2. Duplicate publications, and studies that did not address the theme relevant to the objective of this study and that used methods other than those selected were excluded.

Table 2.
Inclusion and exclusion criteria.
The searches were conducted on 18 November 2023. Both the research and the review of the articles were carried out by at least two independent reviewers.
Through the search of scientific databases, 280 articles were obtained, of which 71 duplicates were excluded. The process of identification and selection of articles took place in two stages. The first stage consisted of screening the titles and abstracts according to the inclusion and exclusion criteria. Upon this screening, 162 were rejected due to their failure to meet the previously established inclusion criteria. Subsequently, the articles resulting from this first analysis were fully evaluated. The full and critical reading of the articles was evaluated, taking into account the process of evaluation and interpretation of the evidence, as well as its validity and relevance, following the methodology proposed by the JBI appraisal tools [11]. These tools were applied by two independent reviewers, and articles were included, or excluded, if both had the same opinion. If there was a difference of opinion between both reviewers regarding the quality of the article, a third reviewer would be asked to assess the quality using the same methodology. Figure 1 presents a diagram according to Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [12], which shows the total number of references returned by the search and those excluded at each step. After the selection and evaluation process, 16 registries were integrated into the present study.
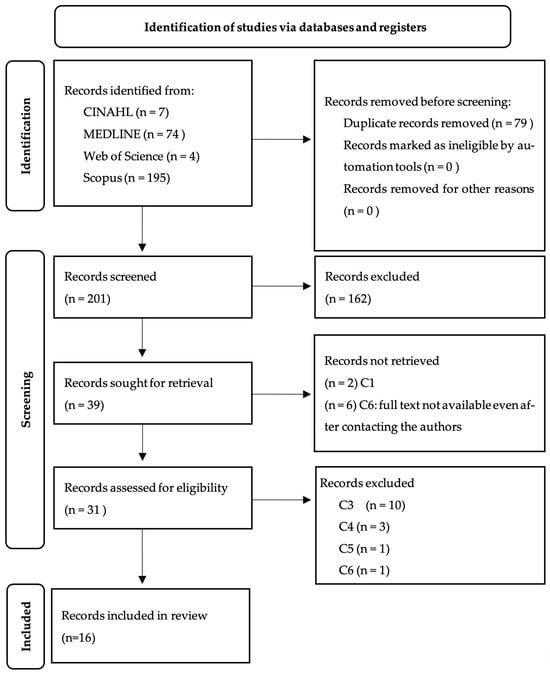
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analysis diagram.
The articles included in the review were summarized and presented in a table prepared by the authors.
3. Results
Of the selected articles, 13 specialist reports were identified, of which eight were published in the United Kingdom (UK) and five in the United States of America (USA). We also identified a mixed descriptive study conducted in the United Kingdom, a quasi-experimental study developed in Jordan, and finally, a randomized experimental study developed in Turkey. Table 3 shows the objectives and participants involved in each study, the level of evidence, the nursing interventions that can be performed in the context of asthma consultations in PHC, and the results in regard to the control and treatment of this pathology.

Table 3.
Presentation of the studies included in the review.
4. Discussion
Through this RSL, it was possible to identify that the scientific evidence relating to the intervention of nurses in asthma consultations is poorly developed, with only three primary research studies identified and the remaining articles considered specialists’ reports. It is possible to verify that most of the expert reports came from the UK. It is possible that these data are due to the higher prevalence of asthma in this country (17.6%) compared to other European countries [29].
The evidence gathered from the articles analyzed allowed us to identify that nurses play a crucial role in the control and treatment of asthma [13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28], as there is substantial evidence that supports systematic follow-up or structured consultations on asthma by nurses [13,14,15,19,25,28].
Of the interventions identified in this review, the largest consensus was on the education of individuals with asthma [13,14,16,17,18,19,20,21,22,23,24,25,26,27,28]. In this sense, the following topics that nurses should address in an asthma-related consultation stand out: (i) general information about asthma [14,28], (ii) medication regimen [16,17,19,20,22,23,27,28], (iii) environmental control [17,18,28], (iv) prevention and management of exacerbations [19,21,23,25,28], (v) self-management of the disease [19,20,21,22,25], (vi) when to seek out health services [22,25], (vii) understanding the treatment plan [19,23], (viii) breathing exercises [16,23], (ix) use of PEF devices [23,24] and (x) inhalation technique [13,14,15,17,21,23,25,26,27,28].
Given the importance of the correct use of medication for asthma management, the articles analyzed reinforce that the role of nurses should go beyond simple education, and also include the verification and training of inhalation technique [13,14,15,16,17,21,22,23,25,26,27,28]. Therefore, the evaluation of the need to use an expansion chamber in the administration of inhaled medication was also pointed out as a role of the nurse when verifying the inhalation technique [15,16,21]. It is important to emphasize that, for the satisfactory efficacy of medication, it is necessary not only to verify the inhalation technique but also to promote adherence to the therapeutic regimen [13,21,22,27].
Several studies analyzed show the importance of the role of nurses in empowering individuals with asthma to self-manage the disease [13,21,22,23,25,27], corroborating the B2 criterion of the Regulation of the Competence Profile of General Care Nurses [30] and the application of Orem’s self-care theory in patients with asthma [31]. It was also found to be useful to involve the family in their care [17,18,23,28] and/or home visits [28]. For self-management of the disease by individuals with asthma, it is essential to use written action plans carried out jointly between the health team and the patient [14,16,19,21,22,25]. This evidence is in line with what is recommended by the DGH [4] and by the Global Initiative for Asthma (GINA) [5].
Both DGH [4] and GINA [5] advocate the use of an asthma control assessment scale, such as the Asthma Control Test (ACT) [32]. This fact is corroborated by this study [13,14,21]. The ACT has a higher sensitivity than the Asthma Control Questionnaire-7 (ACQ-7) when evaluating the asthma control criteria recommended by the GINA [33], making it a good option for application in asthma consultations [34].
The results also reveal that the peak expiratory flow (PEF) was pointed out by the analyzed articles as being important for the evaluation of people with asthma [13,14,17,20,23,24]. This is an intervention that can be performed by nurses, following the most recent recommendations of the GINA [34]. The assessment of vital signs is also the role of nurses and is useful in the assessment of people with asthma, especially body mass index (BMI), blood pressure (BP), heart rate (HR) and, in case of exacerbation, peripheral blood oxygen saturation (SpO2) [17,20,23] interventions are also recommended by the DGH [4].
Another role evidenced by the articles analyzed was the establishment of a supportive therapeutic relationship between nurses and asthma patients [13,22,25,27,28]. In this sense, one SRL identified communication, trust, and follow-up over time as essential elements of support for people with asthma [35]. Regular support from health professionals for people with asthma reduces the need for them to use health services and improves their quality of life [36], with communication and effective interpersonal relationships being key competencies of nurses [30].
Furthermore, only one of the articles analyzed referred to the importance of seasonal influenza vaccination [19], despite the recommendations of the DGH [4] and GINA [5] regarding this vaccine for people with asthma, as well as several other studies [37,38].
In addition to the surveillance consultation, nurses also play an important role in the management of asthma-related emergencies [20,23]. In this sense, the following interventions, which should be performed by nurses in consultations for acute illnesses related to asthma complications, were identified: (i) assessment of vital signs [17,20,23], (ii) evaluation of PEF [13,14,17,20,23,24], (iii) oxygen administration [23], (iv) administration of medication prescribed by the physician [20,23], and (v) patient education on crisis management and relapse prevention [19,20,21,22,23,25,28].
Finally, the studies analyzed also show that integrating the role of the nurse with the role of the physician in the management of asthma results in significant benefits for asthma patients [13,17,19,23,25], in addition to better cost-effectiveness for the health system [22,25], which is corroborated by an SRL carried out by Htay and Whitehead [39].
4.1. Limitations of the Study
One of the biggest risks when conducting an SRL is the definition of the research strategy [9,10]. In this sense, several free searches were carried out to improve the search terms and Boolean operators that were used, maintaining a balance between the sensitivity and relevance of the results. Different databases were used to minimize the risk of losing relevant information. Another limitation of the present study was the linguistic restriction to Portuguese, English, and Spanish, excluding studies published in other languages. In addition, the scientific evidence of most of the selected articles is limited, with only three studies and 13 expert reports found. Further studies evaluating the effectiveness of nursing interventions for controlling asthma are recommended. Of equal relevance would be assessing the knowledge and perception of Portuguese nurses about the performance of this role in asthma control.
4.2. Implications for Clinical Practice
As most of the studies analyzed support the role of nurses as integrated providers of asthma-related care, and this practice is not yet common in Portuguese PHC, this SRL has several implications for practice. The integration of an asthma nursing consultation in PHC (i) helps to alleviate the burden currently placed on physicians, (ii) increases accessibility for patients, (iii) has positive implications for the cost of health care, as it appears that multidisciplinary asthma management helps to reduce costs and improve the efficiency of the health care system, (iii) improves asthma control, and (iv) empowers patients to better manage their disease.
5. Conclusions
This study revealed that PHC nurses play a crucial role in the management and treatment of asthma in adults. Data analysis allowed us to find nursing interventions for asthma control, highlighted in several reports, standards, and studies. Thus, the contribution of this study makes it possible to organize a regular surveillance nursing consultation in PHC units. The role of nurses is also highlighted in (i) the assessment of the patient, including BMI, vital signs, and PEF; (ii) the assessment of asthma control by a questionnaire, such as the ACT; (iii) the verification and training of the inhalation technique, including assessment of the need for the use of expander chamber devices; (iv) in the education of the patient and their family, (v) in the evaluation and promotion of adherence to the management of the therapeutic regimen, (vi) empowering people with asthma to self-manage the disease, (vii) support for the person with asthma through a therapeutic relationship of trust and support in the event of any doubts or the need for care, (viii) promoting adherence to seasonal influenza vaccination, and (ix) the use of written action plans to be drawn up jointly by nurses, doctors, and patients, and delivered to the patient at the end of consultations. On the other hand, the role of nurses in acute asthma-related illness consultations are described as (i) assessment of vital signs and PEF, (ii) administration of oxygen and other medication prescribed by the physician, and (iii) patient education on crisis management and relapse prevention. Multidisciplinary asthma management programs in PHC show both health gains for patients and cost-effectiveness for health services.
Author Contributions
Conceptualization, P.A.-S., J.B., N.S., F.A., M.A. and J.M.; methodology, P.A.-S. and J.M.; validation, P.A.-S., J.B., N.S., F.A., M.A. and J.M.; formal analysis, P.A.-S., J.B., N.S., F.A., M.A. and J.M.; writing—original draft preparation, P.A.-S. and J.M..; writing—review and editing, P.A.-S., J.B., N.S., F.A., M.A. and J.M.; visualization, P.A.-S., J.B., N.S., F.A., M.A. and J.M.; supervision, J.M; project administration, P.A.-S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Rutter, C.; Silverwood, R.; Fernández, V.P.; Pearce, N.; Strachan, D.; Mortimer, K.; Lesosky, M.; Asher, I.; Ellwood, P.; Chiang, C.-Y.; et al. The Global Burden of Asthma. In The Global Asthma Report 2022; International Union Against Tuberculosis and Lung Disease: Paris, France, 2022; pp. 20–23. [Google Scholar] [CrossRef]
- The Global Asthma Network. The Global Asthma Report 2022; International Union Against Tuberculosis and Lung Disease: Paris, France, 2022. [Google Scholar] [CrossRef]
- Costa, R. Introdução. In Guia Prático de Gestão da Asma nos Cuidados de Saúde Primários; Alves, L., Sousa, J.C., Costa, R., Cruz, A.M., Gonçalves, C., Maricoto, T., Pina, N., Prudente, M., Ramires, J., Silva, E., et al., Eds.; Springer Healthcare Ibérica S.L.: Algés, Portugal, 2020; p. 4. [Google Scholar]
- Direção-Geral da Saúde. Processo Assistencial Integrado da Asma na Criança e no Adulto. Available online: https://www.dgs.pt/directrizes-da-dgs/normas-e-circulares-normativas/norma-n-0122018-de-12062018-pdf.aspx (accessed on 15 December 2023).
- Global Initiative for Asthma. Global Stategy for Asthma Management and Prevention (2023 Update). Available online: https://ginasthma.org/wp-content/uploads/2023/07/GINA-2023-Full-report-23_07_06-WMS.pdf (accessed on 15 December 2023).
- Wang, Z.; Li, Y.; Gao, Y.; Fu, Y.; Lin, J.; Lei, X.; Zheng, J.; Jiang, M. Global, regional, and national burden of asthma and its attributable risk factors from 1990 to 2019: A systematic analysis for the Global Burden of Disease Study 2019. Respir. Res. 2023, 24, 169. [Google Scholar] [CrossRef] [PubMed]
- Buelo, A.; McLean, S.; Julious, S.; Flores-Kim, J.; Bush, A.; Henderson, J.; Paton, J.Y.; Sheikh, A.; Shields, M.; Pinnock, H. At-risk children with asthma (ARC): A systematic review. Thorax 2018, 73, 813–824. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Therapeutic Patient Education: An Introductory Guide; WHO Regional Office for Europe: Copenhagen, Denmark, 2023; Available online: https://iris.who.int/bitstream/handle/10665/372743/9789289060219-eng.pdf?sequence=12 (accessed on 15 December 2023).
- Aromataris, E.; Munn, Z. (Eds.) JBI Manual for Evidence Synthesis. JBI. 2020. Available online: https://synthesismanual.jbi.global (accessed on 15 December 2023).
- Vilelas, J. Investigação-O Processo de Construção do Conhecimento, 3rd ed.; Edições Sílabo: Lisboa, Portugal, 2022. [Google Scholar]
- Munn, Z.; Stone, J.C.; Aromataris, E.; Klugar, M.; Sears, K.; Leonardi-Bee, J.; Barker, T.H. Assessing the risk of bias of quantitative analytical studies: Introducing the vision for critical appraisal within JBI systematic reviews. JBI Evid. Synth. 2023, 21, 467–471. Available online: https://journals.lww.com/jbisrir/fulltext/2023/03000/assessing_the_risk_of_bias_of_quantitative.2.aspx (accessed on 15 December 2023). [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Robertson, R.; Osman, L.M.; Douglas, J.G. Adult asthma review in general practice: Nurses’ perception of their role. Fam. Pract. 1997, 14, 227–232. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Barnes, G.R. The nurse’s role in asthma management. Semin. Respir. Crit. Care Med. 1998, 19, 593–601. [Google Scholar] [CrossRef]
- Coakley, A.L. Helping patients to master correct inhaler techniques: Nursing role. Br. J. Nurs. 2001, 10, 424–432. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S.; White, J. Bronchodilators: Implications for nursing practice. Nurs. Stand. 2001, 15, 45–52; quiz 54–56. [Google Scholar] [CrossRef] [PubMed]
- Brooks, E.G.; Hayden, M.L. Exercise-induced asthma. Nurs. Clin. N. Am. 2003, 38, 689–696. [Google Scholar] [CrossRef]
- Huss, K.; Travis, P.; Huss, R.W. General principles of asthma management: Environmental control. Nurs. Clin. N. Am. 2003, 38, 609–620. [Google Scholar] [CrossRef]
- Kallenbach, A.; Ludwig-Beymer, P.; Welsh, C.; Norris, J.; Giloth, B. Process improvement for asthma: An integrated approach. J. Nurs. Care Qual. 2003, 18, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, E.G. Management of asthma emergencies. Nurs. Clin. N. Am. 2003, 38, 713–724. [Google Scholar] [CrossRef] [PubMed]
- McAllister, J. An overview of the current asthma disease management guidance. Br. J. Nurs. 2004, 13, 512–517. [Google Scholar] [CrossRef] [PubMed]
- Newell, K. Concordance with asthma medication: The nurse’s role. Nurs. Stand. 2006, 20, 31–33. [Google Scholar] [CrossRef] [PubMed]
- Sims, J.M. An overview of asthma. Dimens. Crit. Care Nurs. 2006, 25, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Booker, R. Peak expiratory flow measurement. Nurs. Stand. 2007, 21, 42–43. [Google Scholar] [CrossRef]
- Mendes, A. Providing meaningful support to patients with asthma. Br. J. Community Nurs. 2015, 20, 516. [Google Scholar] [CrossRef] [PubMed]
- Al-Kalaldeh, M.; El-Rahman, M.A.; El-Ata, A. Effectiveness of Nurse-Driven Inhaler Education on Inhaler Proficiency and Compliance Among Obstructive Lung Disease Patients: A Quasi-Experimental Study. Can. J. Nurs. Res. 2016, 48, 48–55. [Google Scholar] [CrossRef]
- Scullion, J. The Nurse Practitioners’ Perspective on Inhaler Education in Asthma and Chronic Obstructive Pulmonary Disease. Can. Respir. J. 2018, 2018, 2525319. [Google Scholar] [CrossRef]
- Şanlıtürk, D.; Ayaz-Alkaya, S. The effect of a nurse-led home visit program on the care burden of caregivers of adults with asthma: A randomized controlled trial. Public Health Nurs. 2023, 40, 895–902. [Google Scholar] [CrossRef]
- Wecker, H.; Tizek, L.; Ziehfreund, S.; Kain, A.; Traidl-Hoffmann, C.; Zimmermann, G.S.; Scala, E.; Elberling, J.; Doll, A.; Boffa, M.J.; et al. Impact of asthma in Europe: A comparison of web search data in 21 European countries. World Allergy Organ. J. 2023, 16, 100805. [Google Scholar] [CrossRef]
- Regulamento N.o 190/2015. Diário da República Série II: N.o79/2015. 2015. Available online: https://diariodarepublica.pt/dr/detalhe/regulamento/190-2015-67058782 (accessed on 4 January 2024).
- Yip, J.Y.C. Theory-Based Advanced Nursing Practice: A Practice Update on the Application of Orem’s Self-Care Deficit Nursing Theory. SAGE Open Nurs. 2021, 7, 237796082110119. [Google Scholar] [CrossRef] [PubMed]
- Nathan, R.A.; Sorkness, C.A.; Kosinski, M.; Schatz, M.; Li, J.T.; Marcus, P.; Murray, J.J.; Pendergraft, T.B. Development of the asthma control test: A survey for assessing asthma control. J. Allergy Clin. Immunol. 2004, 113, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Korn, S.; Both, J.; Jung, M.; Hübner, M.; Taube, C.; Buhl, R. Prospective evaluation of current asthma control using ACQ and ACT compared with GINA criteria. Ann. Allergy Asthma Immunol. 2011, 107, 474–479.e2. [Google Scholar] [CrossRef] [PubMed]
- Levy, M.L.; Bacharier, L.B.; Bateman, E.; Boulet, L.-P.; Brightling, C.; Buhl, R.; Brusselle, G.; Cruz, A.A.; Drazen, J.M.; Duijts, L.; et al. Key recommendations for primary care from the 2022 Global Initiative for Asthma (GINA) update. NPJ Prim. Care Respir. Med. 2023, 33, 7. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, S.; McCarthy, V.J.; Savage, E. Self-management support preferences of people with asthma or chronic obstructive pulmonary disease: A systematic review and meta-synthesis of qualitative studies. Chronic Illn. 2021, 17, 283–305. [Google Scholar] [CrossRef] [PubMed]
- Hodkinson, A.; Bower, P.; Grigoroglou, C.; Zghebi, S.S.; Pinnock, H.; Kontopantelis, E.; Panagioti, M. Self-management interventions to reduce healthcare use and improve quality of life among patients with asthma: Systematic review and network meta-analysis. BMJ 2020, m2521. [Google Scholar] [CrossRef]
- Martínez-Baz, I.; Navascués, A.; Casado, I.; Portillo, M.E.; Guevara, M.; Gómez-Ibáñez, C.; Burgui, C.; Ezpeleta, C.; Castilla, J. Effect of influenza vaccination in patients with asthma. CMAJ 2021, 193, E1120–E1128. [Google Scholar] [CrossRef]
- Vasileiou, E.; Sheikh, A.; Butler, C.C.; Robertson, C.; Kavanagh, K.; Englishby, T.; Lone, N.I.; Von Wissmann, B.; McMenamin, J.; Ritchie, L.D.; et al. Seasonal Influenza Vaccine Effectiveness in People with Asthma: A National Test-Negative Design Case-Control Study. Clin. Infect. Dis. 2020, 71, e94–e104. [Google Scholar] [CrossRef]
- Htay, M.; Whitehead, D. The effectiveness of the role of advanced nurse practitioners compared to physician-led or usual care: A systematic review. Int. J. Nurs. Stud. Adv. 2021, 3, 100034. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).