Abstract
Background/Objectives: The high prevalence of benign paroxysmal positional vertigo (BPPV) poses a considerable burden on healthcare systems, with an estimated annual cost of 2 billion dollars per year in the United States. The results of previous network meta-analyses (NMAs) have been inconclusive regarding the efficacy of different treatment strategies for managing BPPV. This study aimed to provide updated evidence of the comparative efficacy and safety of different treatment strategies in patients with BPPV. Methods: The present study was divided into two subgroups. The first part was the posterior canal BPPV, and the second was the horizontal canal BPPV. This frequentist model-based NMA included randomized controlled trials (RCTs) of treatments for BPPV, either in the posterior or horizontal canal. Results: This NMA of 82 RCTs revealed that, regarding posterior canal BPPV, most maneuvers plus postmaneuver rehabilitation/self-treatments were ranked superior to the traditional maneuver with/without medication in terms of the resolution rate. Among them, the modified Epley maneuver + self-treatment at home [odds ratio (OR) = 33.70, 95% confidence intervals (95%CIs) = 6.45–176.13] was ranked to be associated with the highest resolution rate. Regarding horizontal canal BPPV, only the Gufoni maneuver was associated with a significantly better resolution rate (OR = 4.40, 95%CIs = 1.13–17.12) and a higher transition/conversion rate (OR = 3.55, 95%CIs = 1.20–10.57) than that of sham/control groups. Conclusions: This study provides evidence that treatment strategies consisting of maneuvers in combination with postmaneuver rehabilitation/self-treatment may be preferred for managing BPPV affecting the posterior canal. However, no effective treatment strategy for horizontal canal involvement has been identified.
1. Introduction
Benign paroxysmal positional vertigo (BPPV) is a prevalent peripheral vestibular disease that presents with positional vertigo and nystagmus, accounting for 17–42% of vertigo cases [1]. The high prevalence of BPPV poses a considerable burden on healthcare systems, with an estimated annual cost of 2 billion dollars per year in the United States [2]. Despite various treatments for BPPV [2], the high recurrence rate remains a challenge, with approximately 22.1% of the patients experiencing at least one recurrence and 70% experiencing another episode within a year [3]. Therefore, an unmet clinical need remains for an effective BPPV treatment with a low risk of recurrence.
The detached otolith from the semicircular canals would result in endolymphatic turbulence, leading to symptoms of BPPV. Among the three semicircular canals, the most common type of otolith detachment is posterior semicircular canal BPPV, accounting for 60–90%, followed by horizontal semicircular canal BPPV [4]. Several treatment strategies, either maneuvers or medications, have been developed to manage detached otoliths in various canals. However, the efficacies of these treatment strategies vary widely. In addition, along with repositioning the detached otolith, some patients experienced transition events (so-called conversion in some articles), defined as otolith transitioning (or conversion) to another canal during the procedure [5]. Therefore, the efficacy and safety of these treatments remain unclear.
Several network meta-analyses (NMAs) have investigated the efficacy of various treatment strategies for managing BPPV [6,7] and noticed that traditional maneuvers showed comparable efficacy in managing posterior canal BPPV [6], while only the Epley and Semont maneuvers demonstrated effectiveness in long-term follow-up [7]. Finally, Si and colleagues recently published another NMA of 22 randomized controlled trials (RCTs) and demonstrated that most maneuvers had a higher response rate than controls [8]. The NMA has the advantage of allowing multiple efficacy comparisons between individual treatment strategies for a specific disease [9]. Nevertheless, methodological issues regarding these two NMAs have been raised. Specifically, in the NMA by Liu et al., the authors pooled all different traditional maneuvers into one heterogeneous group, such that they could only conclude that the Epley maneuver was similar to the Semont maneuver in efficacy [6]. As addressed in several RCTs, different maneuvers plus postmaneuver rehabilitation/self-treatment exert different efficacies and safety in BPPV management [10,11,12]. In contrast, in the NMA by Li et al. [7], the authors mainly focused on the therapeutic efficacy, either short- or long-term, but seldom focused on safety and acceptability (i.e., recurrence, transition/conversion, and dropout) related to BPPV treatment. As previously mentioned, recurrence and high transition/conversion rates are clinically relevant and important issues in BPPV management. Furthermore, the two aforementioned NMAs mainly addressed BPPV with posterior canal involvement but not those with horizontal canal involvement. As previously mentioned, the management of horizontal canal BPPV differs from that of the posterior canal [2]. Therefore, a more comprehensive NMA is needed for clinicians to serve as a guide in clinical practice.
Based on the framework of our previous publication [13,14,15], this study aimed to comprehensively compare the efficacy and safety of different treatment strategies in patients with BPPV, either in posterior canal or horizontal canal involvement.
2. Methods
2.1. General Guidelines Applied in the Present Study
The present study adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (2020) (Table S1) [16] and the A MeaSurement Tool to Assess Systematic Reviews 2 guidelines [17]. This study was registered in the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42023407395).
2.2. Search Strategy and Selection Criteria
We conducted a systematic search of PubMed, Embase, ScienceDirect, ProQuest, Web of Science, ClinicalKey, Cochrane CENTRAL, and ClinicalTrials.gov (the detailed search strategy is shown in Table S2). The initial date of the literature search was 11 March 2023, and the final update search was performed on 23 August 2025. Language restrictions were not imposed. In addition to these database searches, we manually searched for potentially eligible articles cited in reviews and pairwise meta-analyses [6,7,18,19,20,21,22,23,24,25].
2.3. Inclusion and Exclusion Criteria
The present study was divided into two subgroups for analysis. The first part was the posterior canal BPPV, and the second was the horizontal canal BPPV. The patients, intervention, comparator, outcome, and study of the present study included the following: (1) patients with BPPV, either the posterior or horizontal canal involvement; (2) intervention: any active pharmacologic, nonpharmacologic, or maneuver intervention; (3) comparator: sham control, placebo control, active control, or waiting list; (4) outcome: resolution rate, changes in dizziness severity, recurrence rate, transition/conversion rate, and dropout rate; and (5) study: RCTs.
The inclusion criteria were as follows: (1) RCTs, (2) human participants, and (3) patients diagnosed with BPPV, either the posterior or horizontal canal involvement. Studies were excluded if they (1) were not clinical trials, (2) were not RCTs, (3) did not report the target outcomes of interest, or (4) were not specific to patients with BPPV. When the same set of data was used in multiple studies, we included only the most informative study with the largest sample size. If a study did not address the treatment or maneuver used, the study was excluded.
2.4. Data Extraction
Two authors independently screened the studies for inclusion, extracted relevant data from the manuscripts, and assessed the risk of bias in the included studies. Disagreement between the two authors was adjudicated by the corresponding author. If the manuscript lacked relevant data, the corresponding authors or coauthors were contacted to obtain the original data. We followed the research process used in previous NMAs [26,27,28,29,30,31].
2.5. Outcomes
As the primary aim of treatment is the resolution of BPPV [2], we chose the resolution of BPPV as our primary outcome. BPPV resolution was defined as the absence of symptoms, nystagmus, or negative results for the Dix–Hallpike test, depending on the definition in the recruited studies. For example, if one study provided results of BPPV resolution of two definitions, we would choose the “absence of nystagmus” because this definition is a more objective one than that of “absence of symptoms.” In addition, since BPPV is a highly recurrent disease and the quality of life is associated with truly resolved disease, we chose the final outcome in the last follow-up in the recruited studies. The secondary outcome was a change in dizziness severity. The safety profile included the transition/conversion and recurrence rates. The transition/conversion rate was defined as the proportion of transitions (or conversions) to another BPPV canal during treatment. Recurrence was defined as recurrent symptoms or nystagmus after resolution. Acceptability was calculated using the dropout rate. The dropout rate was defined as the proportion of participants who left the study before the end of the trial for any reason.
2.6. Cochrane Risk of Bias Tool
Two authors independently evaluated the risk of bias (interrater reliability = 0.86) for each domain using the Cochrane Risk-of-Bias tool [32].
2.7. Statistical Analysis
Statistical analyses were performed using STATA version 16.0 (StataCorp LLC, College Station, TX, USA). For continuous data, we estimated the standardized mean difference (SMD). Summary odds ratios (OR) were calculated for categorical data. SMD and OR were estimated with the corresponding 95% confidence intervals (95%CIs). For categorical data, we applied a 0.5 zero-cell correction to the meta-analysis procedure. However, we did not apply such a correction for studies with 0 in both the intervention and control arms because bias might be increased [33]. We used the frequentist NMA model to compare effect sizes between studies with the same intervention. All comparisons were made using a two-tailed test, where p < 0.05 was considered statistically significant. Heterogeneity among the included studies was evaluated using the tau statistic, the estimated standard deviation of the effects across the included studies.
For the analytical procedure, we employed a mixed comparison using a generalized linear mixed model to analyze direct and indirect comparisons among the NMA. Specifically, indirect comparisons were made by assuming transitivity; we assumed that the hitherto unknown difference between treatments A and B could be determined from the known differences between treatments A and C and between treatments B and C, where C was the third treatment. Subsequently, to compare multiple treatment arms, we combined the direct and indirect evidence obtained from the included studies. We use the mvmeta command in STATA (StataCorp, College Station, TX, USA) [34]. The restricted maximum likelihood method was used to evaluate between-study variance. To increase the clinical applicability of our findings, we calculated the surface under the cumulative ranking curve (SUCRA) to rank the relative superiority of individual treatments compared with others [35].
We evaluated the inconsistencies using a loop-specific approach, node-splitting method, and design-by-treatment model. The quality of evidence was evaluated using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) tools [36]. We evaluated the GRADE ratings to evaluate the certainty of the evidence.
3. Results
After the initial screening procedure, 150 articles were selected for full-text review (Figure 1). Overall, 68 articles were excluded for various reasons (Figure 1 and Table S3), leaving 82 for final inclusion in the NMA (Table S4) [2,5,6,7,10,11,12,16,18,19,20,21,22,23,24,25,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171]. The overall network structure of the treatment arms is shown in Figure 2A,B. The treatment arm definition was listed in Table S5.
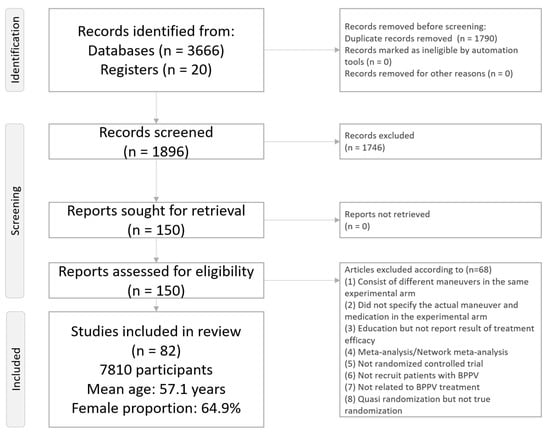
Figure 1.
Flowchart of the network meta-analysis procedure (PRISMA2020 Flowchart).
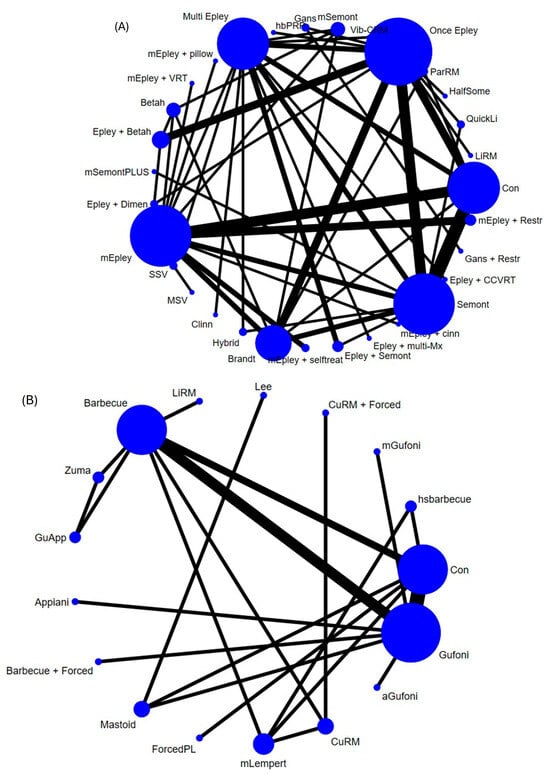
Figure 2.
Network structure of the primary outcome: resolution rate (A) regarding the posterior and (B) horizontal canal involvement. This is the overall network structure of the present network meta-analysis for the primary outcome of resolution. The lines between nodes represent direct comparisons in various trials, and the size of each circle is proportional to the number of participants receiving each specific treatment. The thickness of the lines is proportional to the number of trials connected to the network.
These 82 RCTs included a total of 7810 participants (6299 participants with posterior canal BPPV and 1511 with horizontal canal BPPV). The mean age was 56.35 years (25–75% interquartile: 52.175–60.95 years), and 64.9% of the participants were women (25–75% interquartile: 58.0–72.9%). The mean study duration was 2.5 weeks (25–75% interquartile range: 1.0–4.75 weeks).
3.1. Subgroup Part of the Posterior Canal BPPV
3.1.1. Primary Outcome: Resolution Rate
The main results revealed that the maneuvers plus postmaneuver rehabilitation/self-treatment (modified Epley maneuver + self-treatment at home [mEpley + selftreat], multiple Epley maneuvers + vestibular rehabilitation training [mEpley + VRT], and modified Epley maneuver with postmaneuver restriction [mEpley + Restr]), modern technology-assisted reposition (multi-step vertigo treatment and rehabilitation chair [MSV]), and simply traditional maneuver with/without medication [particle repositioning maneuver (ParRM), modified multiple Epley maneuver (mEpley), Epley maneuver then Semont maneuver (Epley + Semont), Epley maneuver + Betahistine (Epley + Betah), Semont maneuver (Semont), Epley maneuver once (Once Epley), and multiple Epley maneuvers (Multi Epley)] were associated with a significantly better resolution rate in posterior canal BPPV involvement than that of the sham/control groups (Table S13, and Figure 2A and Figure 3A). According to the SUCRA results, mEpley + selftreat yielded the highest resolution rate among all the interventions (Table S6A).
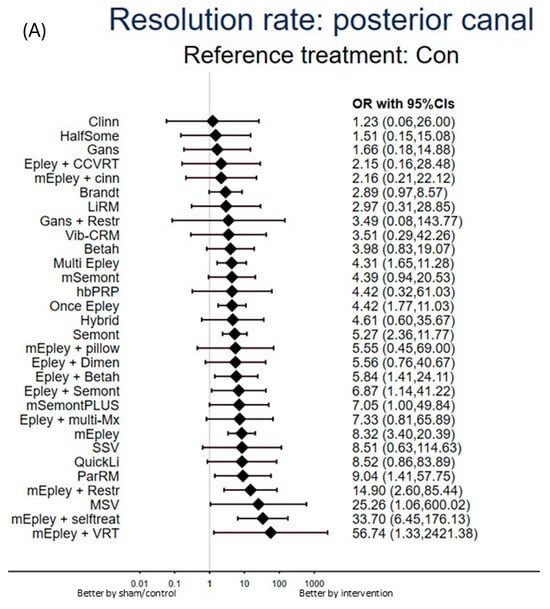
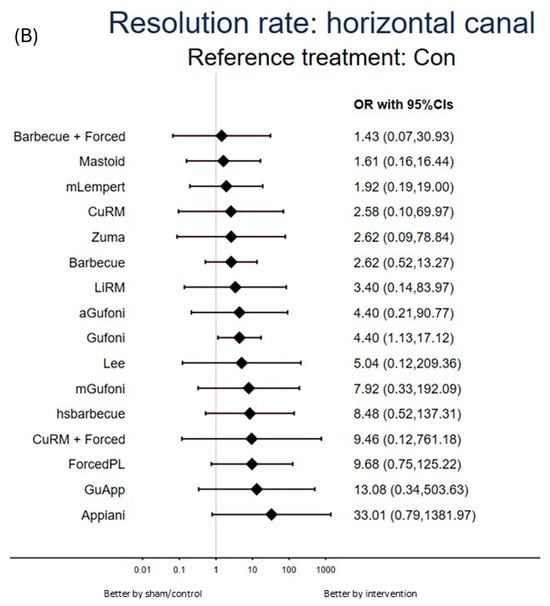
Figure 3.
Forest plot of primary outcome: resolution rate (A) regarding the posterior and (B) horizontal canal involvement. When the effect size was >1 (presented as the odds ratio), the specified treatment yielded a better resolution rate in benign paroxysmal positional vertigo (BPPV) management than that of the sham/control groups (A) regarding the posterior or (B) horizontal canal BPPV involvement. Abbreviation: 95%CIs: 95% confidence intervals; aGufoni: Accelerated Gufoni maneuver; Appiani: Appiani maneuver; Barbecue + Forced: Barbecue maneuver + forced prolonged position; Barbecue: Multiple barbecue repositioning maneuver; Betah: Betahistine; BPPV: benign paroxysmal positional vertigo; Brandt: Brandt–Daroff exercise; CCVRT: Cawthorne–Cooksey vestibular exercises; Clinn: Cinnarizine; Con: Placebo/Sham; CuRM + Forced: Cupulolith repositioning maneuver + Forced prolonged position; CuRM: Cupulolith repositioning maneuver; Dimen: dimenhydrinate; Epley + Betah: Epley maneuver + Betahistine; Epley + CCVRT: Epley Maneuver plus Cawthorne–Cooksey vestibular exercise; Epley + Danhong: Epley maneuver then Danhong injection; Epley + Dimen: Epley maneuver + Dimenhydrinate; Epley + Gingko: Epley maneuver + Gingko biloba; Epley + HUS: Epley maneuver + head-up sleep; Epley + multi-Mx: Epley maneuver + Betahistine + Flunarizine + Ginkgo biloba; Epley + Semont: Epley maneuver then Semont maneuver; Epley + Trim: Epley maneuver + Trimetazidine; ForcedPL: Forced prolonged liberatory maneuver; Gans + Restr: Gans repositioning maneuver with postmaneuver restriction; Gans: Gans repositioning maneuver; Ginkgo: Chinese herb + Ginkgo; GuApp: Gufoni–Appiani maneuver; Gufoni: Gufoni maneuver; HalfSome: Half Somersault Maneuver; hbPRP: Home-based particle repositioning procedure; hsbarbecue: high-speed barbecue maneuver; Hybrid: Hybrid maneuver (Semont + Epley); Lee: Lee maneuver; LiRM: Multiple Li quick repositioning maneuver; Mastoid: Mastoid oscillation; mEpley + Brandt: modified Epley maneuver + Brandt–Daroff exercises; mEpley + cinn: modified Epley maneuver plus cinnarizine; mEpley + head: modified Epley maneuver with augmented head movement; mEpley + pillow: modified Epley maneuver with pillow under the shoulders; mEpley + Restr: modified Epley maneuver with postmaneuver restriction; mEpley + selftreat: modified Epley maneuver + self-treatment at home; mEpley + Shop: modified Epley maneuver + shopping exercise; mEpley + VRT: Multiple Epley maneuver + vestibular stimulated exercise training; mEpley: Modified Epley maneuver; mGufoni: modified Gufoni maneuver; mLempert: modified Lempert maneuver; mSemont: Modified Semont maneuver; mSemontPLUS: Multiple Semont maneuver PLUS; MSV: Multi-step vertigo treatment and rehabilitation chair; Multi Epley: Multiple Epley maneuver; NMA: network meta-analysis; Once Epley: Epley maneuver once; OR: odds ratio; ParRM: Particle Repositioning Maneuver; Polyph: Polyphenol compound; QuickLi: Quick Liberatory Rotation; RCT: randomized controlled trial; Restr: Postural restriction; Semont: Semont maneuver; SMD: standardized mean difference; SSV: Simple-step vertigo treatment and rehabilitation chair; SUCRA: surface under the cumulative ranking curve; Vib-CRM: Vibration-assisted canalith repositioning maneuver; VRT: Vestibular rehabilitation training; Zuma: Zuma-e-Maia maneuver.
3.1.2. Secondary Outcome: Changes in Dizziness Severity
The main result of the NMA revealed that only the Epley maneuver, rather than the Danhong injection (Epley + Danhong), was associated with a significantly better improvement in dizziness severity than that of the sham/control groups (Table S7A, and Figures S1A and S2A). According to the SUCRA results, Epley + Danhong yielded the largest decrease in dizziness severity among all interventions (Table S6B).
3.1.3. Safety Profile: Recurrence Rate
The main results revealed that the maneuvers plus postmaneuver rehabilitation (mEpley + VRT, mEpley + Restr, modified Epley maneuver + shopping exercise [mEpley + Shop]), simply traditional maneuver (modified Epley maneuver + Brandt–Daroff exercises [mEpley + Brandt], Epley + Semont, ParRM, mEpley, modified Semont maneuver [mSemont], Brandt–Daroff exercise [Brandt], Gans repositioning maneuver [Gans], Once Epley, and Semont), and simple medication (Betahistine [Betah]) were associated with a significantly lower recurrence rate in the posterior canal BPPV involvement than that of the sham/control groups (Table S7B, and Figures S1B and S2B). According to the SUCRA results, Gans’ repositioning maneuver with postmaneuver restriction (Gans + Restr) yielded the lowest recurrence rate among all interventions, followed by mEpley + VRT (Table S6C).
3.1.4. Safety Profile: Transition/Conversion Rate
The main results revealed that none of the investigated treatments were associated with significantly different transition/conversion rates in the posterior canal BPPV involvement compared with that of the sham/control groups (Tables S6D and S7C, and Figures S1C and S2C).
3.1.5. Acceptability with Respect to the Dropout Rate
The main result of the NMA revealed that only the Once Epley was associated with significantly lower dropout rates than that of the sham/control groups (Table S7D, and Figures S1D and S2D). According to the SUCRA results, the mEpley + selftreat yielded the lowest dropout rate among all interventions (Table S6E).
3.2. Subgroup Part of Horizontal Canal BPPV
3.2.1. Primary Outcome: Resolution Rate
The main results revealed that only the Gufoni maneuver (Gufoni) was associated with a significantly better resolution rate in the horizontal canal BPPV involvement than that of the sham/control groups (Table S14, and Figure 2B and Figure 3B). According to the SUCRA results, the Appiani maneuver (Appiani) yielded the highest resolution rate among all interventions (Table S6F).
3.2.2. Secondary Outcome: Changes in Dizziness Severity
NMA of changes in dizziness severity regarding the horizontal canal was not performed because few RCTs provided such information.
3.2.3. Safety Profile: Recurrence Rate
The main results revealed that none of the investigated treatments were associated with significantly different recurrence rates of BPPV with horizontal canal involvement compared with those of the sham/control groups (Tables S6G and S7E, and Figures S1E and S2E).
3.2.4. Safety Profile: Transition/Conversion Rate
The main results revealed that only the Gufoni was associated with a significantly higher transition/conversion rate in the horizontal canal BPPV involvement than that of the sham/control groups (Table S7F, and Figures S1F and S2F). According to the SUCRA results, the modified Gufoni maneuver (mGufoni) was associated with the least transition/conversion rate among the investigated treatments (Table S6H).
3.2.5. Acceptability with Respect to the Dropout Rate
The main results revealed that none of the investigated treatments were associated with significantly different dropout rates in the horizontal canal BPPV involvement compared with that of the sham/control groups (Tables S6I and S7G, and Figures S1G and S2G).
3.3. Risk of Bias, Inconsistency, Heterogeneity, and Publication Bias
We found that 68.5% (393/574 items), 13.1% (75/574 items), and 18.4% (106/574 items) of the included studies had low, unclear, and high risks of bias, respectively. Vague reporting of the blindness of the participants/investigator contributed to the risk of bias (Figure S3A,B). Funnel plots of publication bias across the included studies (Figure S4A–D) revealed general symmetry, and the results of the Egger’s test indicated no significant publication bias among the articles included in the NMA. The present study did not exhibit inconsistency, whether local (assessed using the loop-specific approach and node-splitting method) or global (assessed using the design-by-treatment method) (Tables S8–S10). There had been no significant heterogeneity detected in the tau values (Table S11). The GRADE rating revealed that the quality of evidence for most comparisons in the present study ranged from low to medium (Table S12).
4. Discussion
To the best of our knowledge, this is the first comprehensive NMA, from both efficacy and safety, addressing different treatment strategies for BPPV management in different semicircular canal involvement. Regarding the posterior canal involving BPPV, the present study noticed a trend that, among those treatments achieving statistical significance, maneuvers plus postmaneuver rehabilitation/self-treatment was ranked as relatively superior to modern technology-assisted repositioning or simply traditional maneuvers, with/without medication in resolution rate. Regarding the horizontal canal involving the BPPV, only the Gufoni maneuver was associated with a significantly better resolution rate and a higher transition/conversion rate than that of the sham/control groups. In addition, most investigated treatments were associated with acceptability, similar to those of the sham/control groups.
Unlike previous NMAs, our present study addressed both the efficacy and safety of different treatment strategies for managing BPPV [6,7]. Unlike the overt simplification of treatment arms in the study by Liu et al. [6], the present study not only divided the treatment into Epley versus Semont maneuvers but also different strategies of the aforementioned maneuvers; hence, the clinicians could distinguish between the different efficacies and safety of the others. Therefore, our study provided additional clinically relevant information to clinicians compared with the previous NMA by Liu et al. [6], which concluded similar efficacy of different traditional maneuvers for managing posterior canal BPPV. Similarly, in the NMA by Li et al. [7], the authors overtly emphasized the efficacy but did not mention any information regarding safety and acceptability (i.e., recurrence, transition/conversion, and dropout rate) related to BPPV treatment. Finally, although Si and the colleagues separated different maneuvers individually and found that most maneuvers had higher response rate than controls [8], they failed to clarify (1) the additional benefits related to postmaneuver rehabilitation and (2) the potentially different efficacy of treatment in BPPV related to different semicircular canals involvement, which two factors were believed to affect the efficacy of different maneuvers in BPPV management. Our present study explored the superiority of various BPPV management strategies in different aspects, including efficacy (i.e., resolution rate and changes in dizziness severity in different semicircular canals), BPPV (i.e., posterior canal BPPV versus horizontal canal BPPV), safety profile (i.e., recurrence and transition/conversion rates), and acceptability (i.e., dropout rate), which would provide more comprehensive information to clinicians than that of the previous NMAs. Based on an additional analysis regarding safety and acceptability compared with the previous NMA by Li et al. [7], our study provided additional evidence to support the superiority of maneuvers plus postmaneuver rehabilitation/self-treatment owing to their preferable efficacy, safety, and acceptability.
Based on the aforementioned advantages, the present study provided evidence that, among the treatments achieving statistical significance, the treatments of maneuvers plus postmaneuver rehabilitation/self-treatment were superior in both efficacy (i.e., good resolution rate) and safety (i.e., low recurrence rate) compared with the treatments of simple traditional maneuver, with/without medication in posterior canal-involved BPPV. Specifically, those treatments of maneuvers plus postmaneuver rehabilitation/self-treatment had a favorable SUCRA ranking in comparison with those simple traditional maneuvers. The SUCRA, just as its name suggests, “surface under the cumulative ranking curve” [35], was calculated based on the surface area under the ranking curve. It could represent the properties of ranking. In our primary outcome, resolution rate, we set the direction as “the smaller SUCRA, the better resolution rate”. In contrast to the results of previous NMAs [6,7], our study supports the rationale for the application of postmaneuver care in patients with posterior canal BPPV involvement. There have been concerns about overt interventions related to postmaneuver care in BPPV management because of the cost and uncertainty of patient compliance [2]. However, as mentioned in most guidelines and review articles, BPPV is a highly recurrent tendency disorder [2]. Among the investigated patients with BPPV, approximately 70% of recurred patients would encounter a recurrence within 1 year despite receiving satisfactory management [3]. Therefore, acute treatment in clinics or outpatient departments is not sufficient for the long-term prognosis of patients with BPPV. Postmaneuver care, either rehabilitation or self-treatment, would be beneficial for such situations by improving adequate posture, movement, fall prevention, and self-remedy/treatment in physiological aspects [61] and self-control ability and quality of life in psychological/emotional aspects [129]. According to previous reports, abnormal posture, fall-induced head trauma, migraine, Meniere’s disease, and anxiety/stress might be associated with the etiology of BPPV [1,172]. Dealing with the aforementioned events via vestibular rehabilitation or self-treatment on the basis of treatment toward the etiology of BPPV would have extra merits regarding the prevention of recurrence. For example, regular vestibular rehabilitation or self-treatment on the basis of migraine preventive medication might reduce the recurrence rate of BPPV. However, because most maneuvers applied for BPPV management are manually operated by humans, there might be potential interoperator differences between different research teams. This interoperator difference might theoretically influence the resolution rate of each maneuver, and these differences could be supported by the wide 95%CIs of some treatment arms in the present study. In addition, since the evidence of these treatments of maneuvers plus postmaneuver rehabilitation/self-treatment was based on relatively few RCTs [11,12,44,46,53,61,81,129,140,143,155], this might limit the application of this evidence to different types of patients with BPPV. According to the overall evidence, the treatment of maneuvers plus postmaneuver rehabilitation/self-treatment could be considered the preferred treatment in posterior-canal BPPV management.
The number of clinical studies on horizontal canal BPPV would be relatively fewer than those on posterior canal BPPV because the prevalence of horizontal canal BPPV is lower than that of posterior canal BPPV (5–30% vs. 60–90%) [173]. Regarding the management of horizontal canal BPPV involvement, only the Gufoni maneuver was associated with a significantly better resolution rate but a higher transition/conversion rate than that of the sham/control groups. Those effective maneuvers for posterior canal BPPV are not suitable for the horizontal canal [1]. Several newly developed maneuvers, such as the Barbecue repositioning, accelerated Gufoni, Li quick repositioning, and Gufoni–Appiani maneuvers, provide relatively good therapeutic effects but are accompanied by adverse events [2]. To be specific, the transition/conversion is common in the management of horizontal canal BPPV [5]. Currently, there is insufficient evidence to prove that any maneuver or treatment is superior for safely managing BPPV with horizontal canal involvement. In addition, since the audiovestibular dysfunction might be associated with various etiologies [174,175,176,177,178], treatment strategies should be designed individually. Furthermore, to strengthen the evidence, we applied GRADE to rate the certainty of evidence in our NMA [36]. Through GRADE rating, we noticed that the evidence of most comparisons fell within moderate certainty. Finally, along with the new application of image tools in the diagnosis of BPPV, the resolution rate would be improved based on those new tools [179].
5. Strengths and Limitations
The proposed NMA method offers several advantages. First, we provided information not only on efficacy but also on safety, yielding additional information to clinicians. Second, through exhaustive efforts, we made multiple comparisons between different maneuvers and treatments, but did not overtly simplify them into simple groups. Therefore, based on our updated NMA, clinicians can identify the beneficial trends of additive postmaneuver vestibular rehabilitation or self-treatment in BPPV management. Third, we included only RCTs to increase the reliability of the present study. Finally, based on methodological merits, the present study provides information about the superiority of different individual treatments in BPPV management; hence, clinicians can benefit from the information in this study and make relevant comparisons in different clinical situations.
The present study had some limitations that need to be addressed. First, although we did not detect any “statistical heterogeneity” through tau evaluation in our NMA, there was still potential “clinical heterogeneity” that existed in our study. Specifically, some analyses in our study might be limited by potential heterogeneity between studies with respect to participant characteristics, such as differences in diagnostic criteria, operator expertise, and trial duration. Second, some comparisons might have included small sample sizes or study numbers, which may have resulted in less robust quantitative findings. In addition, most evidence regarding postmaneuver rehabilitation or self-treatment came from outpatient department settings. Therefore, the findings of superiority of postmaneuver rehabilitation or self-treatment might not be suitable for those subjects in emergency department settings. Third, since the outcomes of recurrence and transition/conversion might be inconsistently reported across trials, this issue might impose potential heterogeneity among our NMA. Finally, most RCTs in the current NMA had relatively short study durations (mean: 2.5 weeks). Therefore, little is known about the long-term prognosis. Further studies with longer durations are warranted.
6. Conclusions
The present study demonstrated that, regarding the posterior canal BPPV involvement, the treatment strategies with maneuvers plus postmaneuver rehabilitation/self-treatment might be considered the treatment of choice in BPPV management when considering their efficacy and safety. In addition, most investigated treatments were associated with acceptability, similar to those of the sham/control groups. Regarding the horizontal canal involved in BPPV, there are no satisfactory treatment strategies when considering both efficacy and safety. Because of the limitations of the short study duration, we recommend that future RCTs be conducted with a longer follow-up duration to determine the long-term prognosis related to the treatment of maneuvers plus postmaneuver rehabilitation/self-treatment.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/ohbm6020023/s1. Figure S1: network structure; Figure S2: forest plot; Figure S3: risk of bias; Figure S4: funnel plot and Egger regression; Table S1: PRISMA checklist; Table S2: keyword list; Table S3: excluded study list; Table S4: included study list; Table S5: treatment node definition; Table S6: SUCRA list; Table S7: league table; Table S8: design-by-treatment and loop inconsistency test; Table S9: side-splitting inconsistency test; Table S10: between study deviation; Table S11: heterogeneity; Table S12: GRADE rating.
Author Contributions
Conceptualization, C.-S.C., C.-S.L., Y.-C.W., B.S., K.-P.S., Y.-K.T., T.-Y.C. and Y.-W.C.; data curation, J.-J.C., B.-Y.Z. and B.-S.Z.; writing—original draft preparation, J.-J.C., B.-Y.Z. and B.-S.Z.; writing—review and editing, C.-S.C., C.-S.L., Y.-C.W., B.S., K.-P.S., Y.-K.T., T.-Y.C. and Y.-W.C.; supervision, C.-W.H., Y.-L.S. and P.-T.T.; project administration, C.-W.H., Y.-L.S. and P.-T.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviation
3min delayed Epley: Epley Maneuver with 3-min interval between head positions; 95%CIs: 95% confidence intervals; aGufoni: Accelerated Gufoni maneuver; Appiani: Appiani maneuver; Barbecue + Forced: Barbecue maneuver + forced prolonged position; Barbecue: Multiple barbecue repositioning maneuver; Betah: Betahistine; BPPV: benign paroxysmal positional vertigo; Brandt: Brandt–Daroff exercise; CCVRT: Cawthorne–Cooksey vestibular exercises; Clinn: Cinnarizine; Con: Placebo/Sham; CuRM + Forced: Cupulolith repositioning maneuver + Forced prolonged position; CuRM: Cupulolith repositioning maneuver; Dimen: dimenhydrinate; Epley + Betah: Epley maneuver + Betahistine; Epley + CCVRT: Epley Maneuver plus Cawthorne–Cooksey vestibular exercise; Epley + Danhong: Epley maneuver then Danhong injection; Epley + Dimen: Epley maneuver + Dimenhydrinate; Epley + Gingko: Epley maneuver + Gingko biloba; Epley + HUS: Epley maneuver + head-up sleep; Epley + multi-Mx: Epley maneuver + Betahistine + Flunarizine + Ginkgo biloba; Epley + Semont: Epley maneuver then Semont maneuver; Epley + Trim: Epley maneuver + Trimetazidine; ForcedPL: Forced prolonged liberatory maneuver; Gans + Restr: Gans repositioning maneuver with postmaneuver restriction; Gans: Gans repositioning maneuver; Ginkgo: Chinese herb + Ginkgo; GuApp: Gufoni–Appiani maneuver; Gufoni: Gufoni maneuver; HalfSome: Half Somersault Maneuver; hbPRP: Home-based particle repositioning procedure; hsbarbecue: high-speed barbecue maneuver; Hybrid: Hybrid maneuver (Semont + Epley); Lee: Lee maneuver; LiRM: Multiple Li quick repositioning maneuver; Mastoid: Mastoid oscillation; mEpley + Brandt: modified Epley maneuver + Brandt–Daroff exercises; mEpley + cinn: modified Epley maneuver plus cinnarizine; mEpley + head: modified Epley maneuver with augmented head movement; mEpley + pillow: modified Epley maneuver with pillow under the shoulders; mEpley + Restr: modified Epley maneuver with postmaneuver restriction; mEpley + selftreat: modified Epley maneuver + self-treatment at home; mEpley + Shop: modified Epley maneuver + shopping exercise; mEpley + VRT: Multiple Epley maneuver + vestibular stimulated exercise training; mEpley: Modified Epley maneuver; mGufoni: modified Gufoni maneuver; mLempert: modified Lempert maneuver; mSemont: Modified Semont maneuver; mSemontPLUS: Multiple Semont maneuver PLUS; MSV: Multi-step vertigo treatment and rehabilitation chair; Multi Epley: Multiple Epley maneuver; NMA: network meta-analysis; Once Epley: Epley maneuver once; OR: odds ratio; ParRM: Particle Repositioning Maneuver; Polyph: Polyphenol compound; QuickLi: Quick Liberatory Rotation; RCT: randomized controlled trial; Restr: Postural restriction; Semont: Semont maneuver; SMD: standardized mean difference; SSV: Simple-step vertigo treatment and rehabilitation chair; SUCRA: surface under the cumulative ranking curve; Vib-CRM: Vibration-assisted canalith repositioning maneuver; VRT: Vestibular rehabilitation training; Zuma: Zuma-e-Maia maneuver.
References
- You, P.; Instrum, R.; Parnes, L. Benign paroxysmal positional vertigo. Laryngoscope Investig. Otolaryngol. 2019, 4, 116–123. [Google Scholar] [CrossRef]
- Bhattacharyya, N.; Gubbels, S.P.; Schwartz, S.R.; Edlow, J.A.; El-Kashlan, H.; Fife, T.; Holmberg, J.M.; Mahoney, K.; Hollingsworth, D.B.; Roberts, R.; et al. Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo (Update). Otolaryngol. Head. Neck Surg. 2017, 156, S1–S47. [Google Scholar] [CrossRef]
- Kong, T.H.; Song, M.H.; Shim, D.B. Recurrence Rate and Risk Factors of Recurrence in Benign Paroxysmal Positional Vertigo: A Single-Center Long-Term Prospective Study With a Large Cohort. Ear Hear. 2022, 43, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Kim, J.S. Benign paroxysmal positional vertigo. J. Clin. Neurol. 2010, 6, 51–63. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Oh, S.Y.; Lee, S.H.; Kang, J.H.; Kim, D.U.; Jeong, S.H.; Choi, K.D.; Moon, I.S.; Kim, B.K.; Oh, H.J.; et al. Randomized clinical trial for apogeotropic horizontal canal benign paroxysmal positional vertigo. Neurology 2012, 78, 159–166. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, W.; Zhang, A.B.; Bai, X.; Zhang, S. Epley and Semont maneuvers for posterior canal benign paroxysmal positional vertigo: A network meta-analysis. Laryngoscope 2016, 126, 951–955. [Google Scholar] [CrossRef]
- Li, D.; Cheng, D.; Yang, W.; Chen, T.; Zhang, D.; Ren, J.; Zhao, Y. Current Therapies in Patients With Posterior Semicircular Canal BPPV, a Systematic Review and Network Meta-analysis. Otol. Neurotol. 2022, 43, 421–428. [Google Scholar] [CrossRef]
- Si, N.; Liu, M.; Chang, W. Effect of different maneuvers of repositioning on benign paroxysmal vertigo: A network meta-analysis. BMC Neurol. 2025, 25, 109. [Google Scholar] [CrossRef]
- Higgins, J.P.; Welton, N.J. Network meta-analysis: A norm for comparative effectiveness? Lancet 2015, 386, 628–630. [Google Scholar] [CrossRef]
- Strupp, M.; Goldschagg, N.; Vinck, A.S.; Bayer, O.; Vandenbroeck, S.; Salerni, L.; Hennig, A.; Obrist, D.; Mandala, M. BPPV: Comparison of the SemontPLUS With the Semont Maneuver: A Prospective Randomized Trial. Front. Neurol. 2021, 12, 652573. [Google Scholar] [CrossRef]
- You, J.; Yu, D.; Yin, S.; Feng, Y.; Tan, J.; Song, Q.; Chen, B. Complementary self-treatment for posterior canal benign paroxysmal positional vertigo. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2014, 28, 693–696. [Google Scholar]
- Ribeiro, K.M.; Ferreira, L.M.; Freitas, R.V.; Silva, C.N.; Deshpande, N.; Guerra, R.O. "Positive to Negative" Dix-Hallpike test and Benign Paroxysmal Positional Vertigo recurrence in elderly undergoing Canalith Repositioning Maneuver and Vestibular Rehabilitation. Int. Arch. Otorhinolaryngol. 2016, 20, 344–352. [Google Scholar] [CrossRef]
- Hsu, C.W.; Zeng, B.S.; Liang, C.S.; Zeng, B.Y.; Hung, C.M.; Stubbs, B.; Chen, Y.W.; Lei, W.T.; Chen, J.J.; Chen, P.H.; et al. The Preventive Effects of GLP-1 Receptor Agonists and SGLT2 Inhibitors on Cancer Metastasis: A Network Meta-Analysis of 67 Randomized Controlled Trials. Int. J. Mol. Sci. 2025, 26, 8202. [Google Scholar] [CrossRef]
- Hung, C.M.; Zeng, B.Y.; Hsu, C.W.; Chen, P.H.; Sun, C.K.; Carvalho, A.F.; Stubbs, B.; Chen, Y.W.; Chen, T.Y.; Lei, W.T.; et al. The different colorectal tumor risk related to GLP-1 receptor agonists and SGLT2 inhibitors use: A network meta-analysis of 68 randomized controlled trials. Int. J. Surg. 2025. online ahead of print. [Google Scholar] [CrossRef]
- Chen, J.J.; Hsu, C.W.; Hung, C.M.; Liang, C.S.; Su, K.P.; Carvalho, A.F.; Stubbs, B.; Chen, Y.W.; Chen, T.Y.; Lei, W.T.; et al. Risk of Hearing Loss in Patients Treated with Exendin-4 Derivatives: A Network Meta-Analysis of Glucagon-like Peptide-1 Receptor Agonists and Sodium-Glucose Cotransporter 2 Inhibitors. Pharmaceuticals 2025, 18, 735. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef]
- Sharif, S.; Khoujah, D.; Greer, A.; Naples, J.G.; Upadhye, S.; Edlow, J.A. Vestibular suppressants for benign paroxysmal positional vertigo: A systematic review and meta-analysis of randomized controlled trials. Acad. Emerg. Med. 2023, 30, 541–551. [Google Scholar] [CrossRef]
- Yang, Z.; Li, J.; Zhu, Z.; He, J.; Wei, X.; Xie, M. Effect of vitamin D supplementation on benign paroxysmal positional vertigo recurrence: A meta-analysis. Sci. Prog. 2021, 104, 368504211024569. [Google Scholar] [CrossRef]
- Zhang, X.; Qian, X.; Lu, L.; Chen, J.; Liu, J.; Lin, C.; Gao, X. Effects of Semont maneuver on benign paroxysmal positional vertigo: A meta-analysis. Acta Otolaryngol. 2017, 137, 63–70. [Google Scholar] [CrossRef]
- Hilton, M.P.; Pinder, D.K. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst. Rev. 2014, 2014, CD003162. [Google Scholar] [CrossRef] [PubMed]
- Hunt, W.T.; Zimmermann, E.F.; Hilton, M.P. Modifications of the Epley (canalith repositioning) manoeuvre for posterior canal benign paroxysmal positional vertigo (BPPV). Cochrane Database Syst. Rev. 2012, 2012, CD008675. [Google Scholar] [CrossRef] [PubMed]
- Abdulovski, S.; Klokker, M. Repositioning Chairs in the Diagnosis and Treatment of Benign Paroxysmal Positional Vertigo—A Systematic Review. J. Int. Adv. Otol. 2021, 17, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Kerber, K.A. Benign paroxysmal positional vertigo: Opportunities squandered. Ann. N. Y. Acad. Sci. 2015, 1343, 106–112. [Google Scholar] [CrossRef]
- Brehmer, D. Self-treatment of benign paroxysmal positional vertigo with DizzyFix, a new dynamic visual device. Expert. Rev. Med. Devices 2010, 7, 605–609. [Google Scholar] [CrossRef]
- Tseng, P.T.; Yang, C.P.; Su, K.P.; Chen, T.Y.; Wu, Y.C.; Tu, Y.K.; Lin, P.Y.; Stubbs, B.; Carvalho, A.F.; Matsuoka, Y.J.; et al. The association between melatonin and episodic migraine: A pilot network meta-analysis of randomized controlled trials to compare the prophylactic effects with exogenous melatonin supplementation and pharmacotherapy. J. Pineal Res. 2020, 69, e12663. [Google Scholar] [CrossRef]
- Tseng, P.T.; Chen, Y.W.; Zeng, B.Y.; Zeng, B.S.; Hung, C.M.; Sun, C.K.; Cheng, Y.S.; Stubbs, B.; Carvalho, A.F.; Brunoni, A.R.; et al. The beneficial effect on cognition of noninvasive brain stimulation intervention in patients with dementia: A network meta-analysis of randomized controlled trials. Alzheimers Res. Ther. 2023, 15, 20. [Google Scholar] [CrossRef]
- Tseng, P.T.; Zeng, B.S.; Hung, C.M.; Liang, C.S.; Stubbs, B.; Carvalho, A.F.; Brunoni, A.R.; Su, K.P.; Tu, Y.K.; Wu, Y.C.; et al. Assessment of Noninvasive Brain Stimulation Interventions for Negative Symptoms of Schizophrenia: A Systematic Review and Network Meta-analysis. JAMA Psychiatry 2022, 79, 770–779. [Google Scholar] [CrossRef]
- Yang, B.; Tseng, P.T.; Hu, X.; Zeng, B.Y.; Chang, J.P.; Liu, Y.; Chu, W.J.; Zhang, S.S.; Zhou, Z.L.; Chu, C.S.; et al. Comparative efficacy of omega-3 polyunsaturated fatty acids on major cardiovascular events: A network meta-analysis of randomized controlled trials. Prog. Lipid Res. 2022, 88, 101196. [Google Scholar] [CrossRef]
- Tseng, P.T.; Zeng, B.S.; Suen, M.W.; Wu, Y.C.; Correll, C.U.; Zeng, B.Y.; Kuo, J.S.; Chen, Y.W.; Chen, T.Y.; Tu, Y.K.; et al. Efficacy and acceptability of anti-inflammatory eicosapentaenoic acid for cognitive function in Alzheimer’s dementia: A network meta-analysis of randomized, placebo-controlled trials with omega-3 fatty acids and FDA-approved pharmacotherapy. Brain Behav. Immun. 2023, 111, 352–364. [Google Scholar] [CrossRef]
- Chen, J.J.; Zeng, B.S.; Su, K.P.; Wu, Y.C.; Tu, Y.K.; Stubbs, B.; Chen, T.Y.; Zeng, B.Y.; Chen, Y.W.; Hsu, C.W.; et al. Network Meta-analysis of Different Treatments for Vestibular Migraine. CNS Drugs 2023, 37, 837–847. [Google Scholar] [CrossRef]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.0.2; The Cochrane Collaboration: London, UK, 2009. [Google Scholar]
- Brockhaus, A.C.; Bender, R.; Skipka, G. The Peto odds ratio viewed as a new effect measure. Stat. Med. 2014, 33, 4861–4874. [Google Scholar] [CrossRef]
- White, I.R. Network meta-analysis. Stata, J. 2015, 15, 951–985. [Google Scholar] [CrossRef]
- Salanti, G.; Ades, A.E.; Ioannidis, J.P. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: An overview and tutorial. J. Clin. Epidemiol. 2011, 64, 163–171. [Google Scholar] [CrossRef]
- Puhan, M.A.; Schunemann, H.J.; Murad, M.H.; Li, T.; Brignardello-Petersen, R.; Singh, J.A.; Kessels, A.G.; Guyatt, G.H.; Group, G.W. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ 2014, 349, g5630. [Google Scholar] [CrossRef]
- Acar, B.; Karasen, R.M.; Buran, Y. Efficacy of medical therapy in the prevention of residual dizziness after successful repositioning maneuvers for Benign Paroxysmal Positional Vertigo (BPPV). B-ENT 2015, 11, 117–121. [Google Scholar]
- Agarwal, K.; Bronstein, A.M.; Faldon, M.E.; Mandala, M.; Murray, K.; Silove, Y. Visual dependence and BPPV. J. Neurol. 2012, 259, 1117–1124. [Google Scholar] [CrossRef] [PubMed]
- Amor-Dorado, J.C.; Barreira-Fernandez, M.P.; Aran-Gonzalez, I.; Casariego-Vales, E.; Llorca, J.; Gonzalez-Gay, M.A. Particle repositioning maneuver versus Brandt-Daroff exercise for treatment of unilateral idiopathic BPPV of the posterior semicircular canal: A randomized prospective clinical trial with short- and long-term outcome. Otol. Neurotol. 2012, 33, 1401–1407. [Google Scholar] [CrossRef] [PubMed]
- Anastasopoulos, D.; Lempert, T.; Gianna, C.; Gresty, M.A.; Bronstein, A.M. Horizontal otolith-ocular responses to lateral translation in benign paroxysmal positional vertigo. Acta Otolaryngol. 1997, 117, 468–471. [Google Scholar] [CrossRef]
- Andera, L.; Azeredo, W.J.; Greene, J.S.; Sun, H.; Walter, J. Optimizing Testing for BPPV - The Loaded Dix-Hallpike. J. Int. Adv. Otol. 2020, 16, 171–175. [Google Scholar] [CrossRef]
- Angeli, S.I.; Hawley, R.; Gomez, O. Systematic approach to benign paroxysmal positional vertigo in the elderly. Otolaryngol. Head. Neck Surg. 2003, 128, 719–725. [Google Scholar] [CrossRef]
- Asawavichianginda, S.; Isipradit, P.; Snidvongs, K.; Supiyaphun, P. Canalith repositioning for benign paroxysmal positional vertigo: A randomized, controlled trial. Ear Nose Throat J. 2000, 79, 732–734, 736–737. [Google Scholar] [CrossRef]
- Badawy, W.M.; Gad El-Mawla, E.K.; Chedid, A.E.; Mustafa, A.H. Effect of a hybrid maneuver in treating posterior canal benign paroxysmal positional vertigo. J. Am. Acad. Audiol. 2015, 26, 138–144. [Google Scholar] [CrossRef]
- Balatsouras, D.G.; Korres, S.G. Subjective benign paroxysmal positional vertigo. Otolaryngol. Head Neck Surg. 2012, 146, 98–103. [Google Scholar] [CrossRef]
- Balikci, H.H.; Ozbay, I. Effects of postural restriction after modified Epley maneuver on recurrence of benign paroxysmal positional vertigo. Auris Nasus Larynx 2014, 41, 428–431. [Google Scholar] [CrossRef] [PubMed]
- Ballve, J.L.; Carrillo-Munoz, R.; Rando-Matos, Y.; Villar, I.; Cunillera, O.; Almeda, J.; Rodero, E.; Monteverde, X.; Rubio, C.; Moreno, N.; et al. Effectiveness of the Epley manoeuvre in posterior canal benign paroxysmal positional vertigo: A randomised clinical trial in primary care. Br. J. Gen. Pract. 2019, 69, e52–e60. [Google Scholar] [CrossRef] [PubMed]
- Bech, M.W.; Staffe, A.T.; Hougaard, D.D. A mechanical rotation chair provides superior diagnostics of benign paroxysmal positional vertigo. Front. Neurol. 2023, 14, 1040701. [Google Scholar] [CrossRef]
- Bigelow, R.T.; Carey, J.P. Randomized controlled trial in support of vitamin D and calcium supplementation for BPPV. Neurology 2020, 95, 371–372. [Google Scholar] [CrossRef]
- Brignardello-Petersen, R.; Izcovich, A.; Rochwerg, B.; Florez, I.D.; Hazlewood, G.; Alhazanni, W.; Yepes-Nunez, J.; Santesso, N.; Guyatt, G.H.; Schunemann, H.J.; et al. GRADE approach to drawing conclusions from a network meta-analysis using a partially contextualised framework. BMJ 2020, 371, m3907. [Google Scholar] [CrossRef] [PubMed]
- Bromwich, M.A.; Parnes, L.S. The DizzyFix: Initial results of a new dynamic visual device for the home treatment of benign paroxysmal positional vertigo. J. Otolaryngol. Head. Neck Surg. 2008, 37, 380–387. [Google Scholar]
- Bruintjes, T.D.; Companjen, J.; van der Zaag-Loonen, H.J.; van Benthem, P.P. A randomised sham-controlled trial to assess the long-term effect of the Epley manoeuvre for treatment of posterior canal benign paroxysmal positional vertigo. Clin. Otolaryngol. 2014, 39, 39–44. [Google Scholar] [CrossRef]
- Cakir, B.O.; Ercan, I.; Cakir, Z.A.; Turgut, S. Efficacy of postural restriction in treating benign paroxysmal positional vertigo. Arch. Otolaryngol. Head. Neck Surg. 2006, 132, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Califano, L.; Capparuccia, P.G.; Di Maria, D.; Melillo, M.G.; Villari, D. Treatment of benign paroxysmal positional vertigo of posterior semicircular canal by "Quick Liberatory Rotation Manoeuvre". Acta Otorhinolaryngol. Ital. 2003, 23, 161–167. [Google Scholar]
- Carrillo Munoz, R.; Ballve Moreno, J.L.; Villar Balboa, I.; Rando Matos, Y.; Cunillera Puertolas, O.; Almeda Ortega, J.; Vertigo Study Group in Florida Primary, C. A single Epley manoeuvre can improve self-perceptions of disability (quality of life) in patients with pc-BPPV: A randomised controlled trial in primary care. Aten. Primaria 2021, 53, 102077. [Google Scholar] [CrossRef] [PubMed]
- Casani, A.P.; Nacci, A.; Dallan, I.; Panicucci, E.; Gufoni, M.; Sellari-Franceschini, S. Horizontal semicircular canal benign paroxysmal positional vertigo: Effectiveness of two different methods of treatment. Audiol. Neurootol. 2011, 16, 175–184. [Google Scholar] [CrossRef]
- Casani, A.P.; Navari, E.; Albera, R.; Agus, G.; Asprella Libonati, G.; Chiarella, G.; Lombardo, N.; Marcelli, V.; Ralli, G.; Scotto di Santillo, L.; et al. Approach to residual dizziness after successfully treated benign paroxysmal positional vertigo: Effect of a polyphenol compound supplementation. Clin. Pharmacol. 2019, 11, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Celis-Aguilar, E.; Mayoral-Flores, H.O.; Torrontegui-Zazueta, L.A.; Medina-Cabrera, C.A.; Leon-Leyva, I.C.; Dehesa-Lopez, E. Effectiveness of Brandt Daroff, Semont and Epley maneuvers in the treatment of Benign Paroxysmal Positional Vertigo: A Randomized Controlled Clinical Trial. Indian. J. Otolaryngol. Head Neck Surg. 2022, 74, 314–321. [Google Scholar] [CrossRef]
- Cetin, Y.S.; Cagac, A.; Duzenli, U.; Bozan, N.; Elasan, S. Residual Dizziness in Elderly Patients after Benign Paroxysmal Positional Vertigo. ORL J. Otorhinolaryngol. Relat. Spec. 2022, 84, 122–129. [Google Scholar] [CrossRef]
- Cetin, Y.S.; Ozmen, O.A.; Demir, U.L.; Kasapoglu, F.; Basut, O.; Coskun, H. Comparison of the effectiveness of Brandt-Daroff Vestibular training and Epley Canalith repositioning maneuver in benign Paroxysmal positional vertigo long term result: A randomized prospective clinical trial. Pak. J. Med. Sci. 2018, 34, 558–563. [Google Scholar] [CrossRef]
- Chang, W.C.; Yang, Y.R.; Hsu, L.C.; Chern, C.M.; Wang, R.Y. Balance improvement in patients with benign paroxysmal positional vertigo. Clin. Rehabil. 2008, 22, 338–347. [Google Scholar] [CrossRef]
- Chen, Y.; Zhuang, J.; Zhang, L.; Li, Y.; Jin, Z.; Zhao, Z.; Zhao, Y.; Zhou, H. Short-term efficacy of Semont maneuver for benign paroxysmal positional vertigo: A double-blind randomized trial. Otol. Neurotol. 2012, 33, 1127–1130. [Google Scholar] [CrossRef]
- Choi, S.Y.; Cho, J.W.; Choi, J.H.; Oh, E.H.; Choi, K.D. Effect of the Epley Maneuver and Brandt-Daroff Exercise on Benign Paroxysmal Positional Vertigo Involving the Posterior Semicircular Canal Cupulolithiasis: A Randomized Clinical Trial. Front. Neurol. 2020, 11, 603541. [Google Scholar] [CrossRef]
- Cohen, H.S.; Jerabek, J. Efficacy of treatments for posterior canal benign paroxysmal positional vertigo. Laryngoscope 1999, 109, 584–590. [Google Scholar] [CrossRef]
- Cohen, H.S.; Kimball, K.T. Treatment variations on the Epley maneuver for benign paroxysmal positional vertigo. Am. J. Otolaryngol. 2004, 25, 33–37. [Google Scholar] [CrossRef]
- Cohen, H.S.; Kimball, K.T. Effectiveness of treatments for benign paroxysmal positional vertigo of the posterior canal. Otol. Neurotol. 2005, 26, 1034–1040. [Google Scholar] [CrossRef] [PubMed]
- Cohen, H.S.; Sangi-Haghpeykar, H. Canalith repositioning variations for benign paroxysmal positional vertigo. Otolaryngol. Head. Neck Surg. 2010, 143, 405–412. [Google Scholar] [CrossRef]
- Correia, F.; Castelhano, L.; Cavilhas, P.; Escada, P. Lateral semicircular canal-BPPV: Prospective randomized study on the efficacy of four repositioning maneuvers. Acta Otorrinolaringol. Esp. (Engl. Ed.) 2022, 73, 27–34. [Google Scholar] [CrossRef] [PubMed]
- De Stefano, A.; Dispenza, F.; Citraro, L.; Petrucci, A.G.; Di Giovanni, P.; Kulamarva, G.; Mathur, N.; Croce, A. Are postural restrictions necessary for management of posterior canal benign paroxysmal positional vertigo? Ann. Otol. Rhinol. Laryngol. 2011, 120, 460–464. [Google Scholar] [CrossRef] [PubMed]
- Deng, W.; Yang, C.; Xiong, M.; Fu, X.; Lai, H.; Huang, W. Danhong enhances recovery from residual dizziness after successful repositioning treatment in patients with benign paroxysmal positional vertigo. Am. J. Otolaryngol. 2014, 35, 753–757. [Google Scholar] [CrossRef]
- Dispenza, F.; Kulamarva, G.; De Stefano, A. Comparison of repositioning maneuvers for benign paroxysmal positional vertigo of posterior semicircular canal: Advantages of hybrid maneuver. Am. J. Otolaryngol. 2012, 33, 528–532. [Google Scholar] [CrossRef]
- Dlugaiczyk, J.; Thiemer, M.; Neubert, C.; Schorn, B.A.; Schick, B. The aVOR App Increases Medical Students’ Competence in Treating Benign Paroxysmal Positional Vertigo (BPPV). Otol. Neurotol. 2018, 39, e401–e406. [Google Scholar] [CrossRef] [PubMed]
- Franco-Gutierrez, V.; Perez-Guillen, V.; Gil-Aguilar, M.T.; Franco-Gutierrez, R.; Alvarez-Zapico, M.J.; Garcia-Zamora, E.; Perez-Vazquez, P. Comparative Analysis of the Efficiency of Two Treatment Protocols for Posterior Canal Benign Paroxysmal Positional Vertigo. Acta Otorrinolaringol. Esp. (Engl. Ed.) 2022, 73, 69–76. [Google Scholar] [CrossRef]
- Froehling, D.A.; Bowen, J.M.; Mohr, D.N.; Brey, R.H.; Beatty, C.W.; Wollan, P.C.; Silverstein, M.D. The canalith repositioning procedure for the treatment of benign paroxysmal positional vertigo: A randomized controlled trial. Mayo Clin. Proc. 2000, 75, 695–700. [Google Scholar] [CrossRef]
- Gan, Z.; Zhou, S.; Yang, H.; He, F.; Wei, D.; Bai, Y.; Wang, Y.; Wang, Y.; Fu, W.; Han, J. Self-Treatment of Posterior Canal Benign Paroxysmal Positional Vertigo: A Preliminary Study. Front. Med. 2021, 8, 654637. [Google Scholar] [CrossRef]
- Giardino, D.; Musazzi, M.; Perez Akly, M.; Cherchi, M.; Yacovino, D.A. A comparative study of two methods for treatment of benign paroxysmal positional vertigo in the emergency department. J. Otol. 2021, 16, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Guneri, E.A.; Kustutan, O. The effects of betahistine in addition to epley maneuver in posterior canal benign paroxysmal positional vertigo. Otolaryngol. Head Neck Surg. 2012, 146, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Han, K.; Lee, J.; Shin, J.E.; Kim, C.H. Treatment Efficacy of Forced Prolonged Position After Cupulolith Repositioning Maneuver in Apogeotropic HSCC BPPV. Ear Nose Throat J. 2021, 103, NP234–NP240. [Google Scholar] [CrossRef]
- Helminski, J.O.; Janssen, I.; Kotaspouikis, D.; Kovacs, K.; Sheldon, P.; McQueen, K.; Hain, T.C. Strategies to prevent recurrence of benign paroxysmal positional vertigo. Arch. Otolaryngol. Head Neck Surg. 2005, 131, 344–348. [Google Scholar] [CrossRef]
- Herdman, S.J.; Tusa, R.J.; Zee, D.S.; Proctor, L.R.; Mattox, D.E. Single treatment approaches to benign paroxysmal positional vertigo. Arch. Otolaryngol. Head Neck Surg. 1993, 119, 450–454. [Google Scholar] [CrossRef]
- Heydari, M.; Ahadi, M.; Jalaei, B.; Maarefvand, M.; Talebi, H. The Additional Effect of Vestibular Rehabilitation Therapy on Residual Dizziness After Successful Modified Epley Procedure for Posterior Canal Benign Paroxysmal Positional Vertigo. Am. J. Audiol. 2021, 30, 535–543. [Google Scholar] [CrossRef]
- Horinaka, A.; Kitahara, T.; Shiozaki, T.; Ito, T.; Wada, Y.; Yamanaka, T.; Nario, K. Head-Up Sleep May Cure Patients With Intractable Benign Paroxysmal Positional Vertigo: A six-Month Randomized Trial. Laryngoscope Investig. Otolaryngol. 2019, 4, 353–358. [Google Scholar] [CrossRef]
- Hwang, M.; Kim, S.H.; Kang, K.W.; Lee, D.; Lee, S.Y.; Kim, M.K.; Lee, S.H. Canalith repositioning in apogeotropic horizontal canal benign paroxysmal positional vertigo: Do we need faster maneuvering? J. Neurol. Sci. 2015, 358, 183–187. [Google Scholar] [CrossRef]
- Imai, T.; Okumura, T.; Sato, T.; Takeda, N.; Ohta, Y.; Okazaki, S.; Inohara, H. Effects of Interval Time of the Epley Maneuver on Immediate Reduction of Positional Nystagmus: A Randomized, Controlled, Non-blinded Clinical Trial. Front. Neurol. 2019, 10, 304. [Google Scholar] [CrossRef]
- Isaradisaikul, S.K.; Chowsilpa, S.; Hanprasertpong, C.; Rithirangsriroj, T. Single Cycle Versus Multiple Cycles of Canalith Repositioning Procedure for Treatment of Posterior Canal Benign Paroxysmal Positional Vertigo: A Randomized Controlled Trial. Otol. Neurotol. 2021, 42, 121–128. [Google Scholar] [CrossRef]
- Jaffar, M.; Ghous, M.; Ayaz, M.; Khan, A.A.; Akbar, A.; Haleem, F. Effects of Half-Somersault and Brandt-Daroff exercise on dizziness, fear of fall and quality of life in patients with posterior canal benign paroxysmal positional vertigo: A randomised control trial. J. Pak. Med. Assoc. 2023, 73, 139–142. [Google Scholar] [CrossRef]
- Jalali, M.M.; Gerami, H.; Saberi, A.; Razaghi, S. The Impact of Betahistine versus Dimenhydrinate in the Resolution of Residual Dizziness in Patients with Benign Paroxysmal Positional Vertigo: A Randomized Clinical Trial. Ann. Otol. Rhinol. Laryngol. 2020, 129, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Janssens, J.P.; Metzger, M.; Sforza, E. Impact of volume targeting on efficacy of bi-level non-invasive ventilation and sleep in obesity-hypoventilation. Respir. Med. 2009, 103, 165–172. [Google Scholar] [CrossRef]
- Jeon, E.J.; Lee, D.H.; Park, J.M.; Oh, J.H.; Seo, J.H. The efficacy of a modified Dix-Hallpike test with a pillow under shoulders. J. Vestib. Res. 2019, 29, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.H.; Kim, J.S.; Kim, H.J.; Choi, J.Y.; Koo, J.W.; Choi, K.D.; Park, J.Y.; Lee, S.H.; Choi, S.Y.; Oh, S.Y.; et al. Prevention of benign paroxysmal positional vertigo with vitamin D supplementation: A randomized trial. Neurology 2020, 95, e1117–e1125. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.J.; Koo, J.W.; Kim, C.S.; Kim, J.S.; Song, J.J. Anxiolytics reduce residual dizziness after successful canalith repositioning maneuvers in benign paroxysmal positional vertigo. Acta Otolaryngol. 2012, 132, 277–284. [Google Scholar] [CrossRef]
- Karan, A.; Alptekin, H.K.; Capan, N.; Diracoglu, D.; Saral, I.; Aydin, S.; Aksoy, C. The efficacy of vestibular electrical stimulation on patients with unilateral vestibular pathologies. Turk. J. Phys. Med. Rehabil. 2017, 63, 149–154. [Google Scholar] [CrossRef]
- Karanjai, S.; Saha, A.K. Evaluation of vestibular exercises in the management of benign paroxysmal positional vertigo. Indian J. Otolaryngol. Head Neck Surg. 2010, 62, 202–207. [Google Scholar] [CrossRef]
- Kaur, J.; Shamanna, K. Management of Benign Paroxysmal Positional Vertigo: A Comparative Study between Epleys Manouvre and Betahistine. Int. Tinnitus J. 2017, 21, 30–34. [Google Scholar] [CrossRef]
- Kerber, K.A.; Damschroder, L.; McLaughlin, T.; Brown, D.L.; Burke, J.F.; Telian, S.A.; Tsodikov, A.; Fagerlin, A.; An, L.C.; Morgenstern, L.B.; et al. Implementation of Evidence-Based Practice for Benign Paroxysmal Positional Vertigo in the Emergency Department: A Stepped-Wedge Randomized Trial. Ann. Emerg. Med. 2020, 75, 459–470. [Google Scholar] [CrossRef]
- Khaftari, M.D.; Ahadi, M.; Maarefvand, M.; Jalaei, B. The Efficacy of the Half Somersault Maneuver in Comparison to the Epley Maneuver in Patients with Benign Paroxysmal Positional Vertigo. J. Int. Adv. Otol. 2021, 17, 417–421. [Google Scholar] [CrossRef]
- Kim, H.A.; Park, S.W.; Kim, J.; Kang, B.G.; Lee, J.; Han, B.I.; Seok, J.I.; Chung, E.J.; Kim, J.; Lee, H. Efficacy of mastoid oscillation and the Gufoni maneuver for treating apogeotropic horizontal benign positional vertigo: A randomized controlled study. J. Neurol. 2017, 264, 848–855. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Kim, J.S.; Choi, K.D.; Choi, S.Y.; Lee, S.H.; Jung, I.; Park, J.H. Effect of Self-treatment of Recurrent Benign Paroxysmal Positional Vertigo: A Randomized Clinical Trial. JAMA Neurol. 2023, 80, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Oh, S.Y.; Lee, S.H.; Kang, J.H.; Kim, D.U.; Jeong, S.H.; Choi, K.D.; Moon, I.S.; Kim, B.K.; Kim, H.J. Randomized clinical trial for geotropic horizontal canal benign paroxysmal positional vertigo. Neurology 2012, 79, 700–707. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.B.; Lee, H.S.; Ban, J.H. Vestibular suppressants after canalith repositioning in benign paroxysmal positional vertigo. Laryngoscope 2014, 124, 2400–2403. [Google Scholar] [CrossRef]
- Kitahara, T.; Horinaka, A.; Shiozaki, T.; Ito, T.; Wada, Y.; Yamanaka, T.; Nario, K. Combination of head-up sleep and vertical recognition training may cure intractable motion-evoked dizziness with unknown origin. Acta Otolaryngol. 2020, 140, 467–472. [Google Scholar] [CrossRef] [PubMed]
- Kong, T.H.; Song, M.H.; Kang, J.W.; Shim, D.B. Double-blind randomized controlled trial on efficacy of cupulolith repositioning maneuver for treatment of apogeotropic horizontal canal benign paroxysmal positional vertigo. Acta Otolaryngol. 2020, 140, 473–478. [Google Scholar] [CrossRef]
- Kulcu, D.G.; Yanik, B.; Boynukalin, S.; Kurtais, Y. Efficacy of a home-based exercise program on benign paroxysmal positional vertigo compared with betahistine. J. Otolaryngol. Head Neck Surg. 2008, 37, 373–379. [Google Scholar]
- Lee, D.H.; Park, J.Y.; Kim, T.H.; Shin, J.E.; Kim, C.H. New Therapeutic Maneuver for Horizontal Semicircular Canal Cupulolithiasis: A Prospective Randomized Trial. J. Clin. Med. 2022, 11, 4136. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Jeon, E.J.; Lee, D.H.; Seo, J.H. Therapeutic Efficacy of the Modified Epley Maneuver With a Pillow Under the Shoulders. Clin. Exp. Otorhinolaryngol. 2020, 13, 376–380. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Lee, D.H.; Noh, H.; Shin, J.E.; Kim, C.H. Immediate and short-term effects of Gufoni and Appiani liberatory maneuver for treatment of ageotropic horizontal canal benign paroxysmal positional vertigo: A prospective randomized trial. Laryngoscope Investig. Otolaryngol. 2021, 6, 832–838. [Google Scholar] [CrossRef]
- Lee, J.D.; Shim, D.B.; Park, H.J.; Song, C.I.; Kim, M.B.; Kim, C.H.; Byun, J.Y.; Hong, S.K.; Kim, T.S.; Park, K.H.; et al. A multicenter randomized double-blind study: Comparison of the Epley, Semont, and sham maneuvers for the treatment of posterior canal benign paroxysmal positional vertigo. Audiol. Neurootol. 2014, 19, 336–341. [Google Scholar] [CrossRef]
- Li, J.; Tian, S.; Zou, S. Efficacy of the Li maneuver in treating posterior canal benign paroxysmal positional vertigo. Acta Otolaryngol. 2017, 137, 588–592. [Google Scholar] [CrossRef]
- Li, J.; Zou, S.; Tian, S. A prospective randomized controlled study of Li quick repositioning maneuver for geotropic horizontal canal BPPV. Acta Otolaryngol. 2018, 138, 779–784. [Google Scholar] [CrossRef] [PubMed]
- Macias, J.D.; Ellensohn, A.; Massingale, S.; Gerkin, R. Vibration with the canalith repositioning maneuver: A prospective randomized study to determine efficacy. Laryngoscope 2004, 114, 1011–1014. [Google Scholar] [CrossRef]
- Mancera Sanchez, J.; Hernaiz Leonardo, J.C.; Ishiwara Niembro, J.K.; Lesser, J.C. Therapeutic Effect of the Correction of Vitamin D Deficiency in Patients with Benign Paroxysmal Positional Vertigo. A Randomized Clinical Trial. Int. Arch. Otorhinolaryngol. 2022, 26, e666–e670. [Google Scholar] [CrossRef]
- Mandala, M.; Califano, L.; Casani, A.P.; Faralli, M.; Marcelli, V.; Neri, G.; Pecci, R.; Scasso, F.; Scotto di Santillo, L.; Vannucchi, P.; et al. Double-Blind Randomized Trial on the Efficacy of the Forced Prolonged Position for Treatment of Lateral Canal Benign Paroxysmal Positional Vertigo. Laryngoscope 2021, 131, E1296–E1300. [Google Scholar] [CrossRef]
- Mandala, M.; Pepponi, E.; Santoro, G.P.; Cambi, J.; Casani, A.; Faralli, M.; Giannoni, B.; Gufoni, M.; Marcelli, V.; Trabalzini, F.; et al. Double-blind randomized trial on the efficacy of the Gufoni maneuver for treatment of lateral canal BPPV. Laryngoscope 2013, 123, 1782–1786. [Google Scholar] [CrossRef]
- Mandala, M.; Santoro, G.P.; Asprella Libonati, G.; Casani, A.P.; Faralli, M.; Giannoni, B.; Gufoni, M.; Marcelli, V.; Marchetti, P.; Pepponi, E.; et al. Double-blind randomized trial on short-term efficacy of the Semont maneuver for the treatment of posterior canal benign paroxysmal positional vertigo. J. Neurol. 2012, 259, 882–885. [Google Scholar] [CrossRef]
- Martens, C.; Goplen, F.K.; Aasen, T.; Gjestad, R.; Nordfalk, K.F.; Nordahl, S.H.G. Treatment of horizontal canal BPPV-a randomized sham-controlled trial comparing two therapeutic maneuvers of different speeds. Laryngoscope Investig. Otolaryngol. 2020, 5, 750–757. [Google Scholar] [CrossRef] [PubMed]
- Maslovara, S.; Soldo, S.B.; Puksec, M.; Balaban, B.; Penavic, I.P. Benign paroxysmal positional vertigo (BPPV): Influence of pharmacotherapy and rehabilitation therapy on patients’ recovery rate and life quality. NeuroRehabilitation 2012, 31, 435–441. [Google Scholar] [CrossRef]
- Meurer, W.J.; Johnson, P.; Brown, D.; Tsodikov, A.; Rowell, B.; Fagerlin, A.; Telian, S.A.; Damschroder, L.; An, L.C.; Morgenstern, L.B.; et al. An Educational Intervention for Acute Dizziness Care: A Randomized, Vignette-based Study. Otol. Neurotol. 2019, 40, e830–e838. [Google Scholar] [CrossRef] [PubMed]
- Morales-Olavarria, C.; Sarria-Echegaray, P.; Til-Perez, G.; Carnevale, C. Role of Intratympanic Dexamethasone for Intractable Posterior Canal Benign Paroxysmal Positional Vertigo. Int. Tinnitus J. 2021, 25, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Munoz, J.E.; Miklea, J.T.; Howard, M.; Springate, R.; Kaczorowski, J. Canalith repositioning maneuver for benign paroxysmal positional vertigo: Randomized controlled trial in family practice. Can. Fam. Physician Med. De Fam. Can. 2007, 53, 1048–1053. [Google Scholar]
- Oh, S.Y.; Kim, J.S.; Choi, K.D.; Park, J.Y.; Jeong, S.H.; Lee, S.H.; Lee, H.S.; Yang, T.H.; Kim, H.J. Switch to Semont maneuver is no better than repetition of Epley maneuver in treating refractory BPPV. J. Neurol. 2017, 264, 1892–1898. [Google Scholar] [CrossRef]
- Organ, B.; Liu, H.; Bromwich, M. An iPhone-assisted particle repositioning maneuver for benign paroxysmal positional vertigo (BPPV): A prospective randomized study. J. Am. Board. Fam. Med. 2015, 28, 118–120. [Google Scholar] [CrossRef]
- Patino, J.E.P.; Moreno, J.L.B.; Matos, Y.R.; Ortega, J.A.; Puertolas, O.C.; Munoz, R.C.; Balboa, I.V.; Compta, X.G.; Agudelo, O.L.A.; Munoz, S.C.; et al. Effectiveness of a training intervention to improve the management of vertigo in primary care: A multicentre cluster-randomised trial, VERTAP. Trials 2022, 23, 608. [Google Scholar] [CrossRef]
- Perez-Guillen, V.; Franco-Gutierrez, V.; Aguilar, M.T.G.; Zamora, E.G.; Perez-Vazquez, P. Can Benign Paroxysmal Positional Vertigo Be Treated in a One Session? Otol. Neurotol. 2020, 41, e727–e734. [Google Scholar] [CrossRef]
- Piromchai, P.; Eamudomkarn, N.; Srirompotong, S.; Ratanaanekchai, T.; Yimtae, K. The Efficacy of a Home Treatment Program Combined With Office-Based Canalith Repositioning Procedure for Benign Paroxysmal Positional Vertigo-A Randomized Controlled Trial. Otol. Neurotol. 2019, 40, 951–956. [Google Scholar] [CrossRef]
- Pollak, L.; Gilad, R.; Michael, T. Unilateral mimicking bilateral BPPV- a forgotten entity? Characteristics of a large cohort of patients, comparison with posterior canal BPPV and clinical implications. J. Otol. 2021, 16, 252–257. [Google Scholar] [CrossRef]
- Pollak, L.; Michael, T. Bilateral Posterior Canal Benign Paroxysmal Positional Vertigo Tends to Reoccur. Otol. Neurotol. 2019, 40, 946–950. [Google Scholar] [CrossRef]
- Qi, H.; Wang, B.; Yu, W.; Zheng, Z.; Yang, J. Clinical efficacy and quality of life evaluation of BPPV by different reduction methods. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2016, 30, 392–395. [Google Scholar]
- Ranju, R.L.; Lepcha, A.; Mammen, M.D.; Vasanthan, L.T.; Augustine, A.M.; Philip, A. An Effective Home-Based Particle Repositioning Procedure for Posterior Canal Benign Paroxysmal Positional Vertigo (BPPV). Indian. J. Otolaryngol. Head Neck Surg. 2022, 74, 516–523. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, K.M.; Freitas, R.V.; Ferreira, L.M.; Deshpande, N.; Guerra, R.O. Effects of balance Vestibular Rehabilitation Therapy in elderly with Benign Paroxysmal Positional Vertigo: A randomized controlled trial. Disabil. Rehabil. 2017, 39, 1198–1206. [Google Scholar] [CrossRef]
- Roberts, R.A.; Gans, R.E.; DeBoodt, J.L.; Lister, J.J. Treatment of benign paroxysmal positional vertigo: Necessity of postmaneuver patient restrictions. J. Am. Acad. Audiol. 2005, 16, 357–366. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, D.L.; Ledesma, A.L.L.; Pires de Oliveira, C.A.; Bahmad, F., Jr. Effect of Vestibular Exercises Associated With Repositioning Maneuvers in Patients With Benign Paroxysmal Positional Vertigo: A Randomized Controlled Clinical Trial. Otol. Neurotol. 2019, 40, e824–e829. [Google Scholar] [CrossRef]
- Saberi, A.; Nemati, S.; Sabnan, S.; Mollahoseini, F.; Kazemnejad, E. A safe-repositioning maneuver for the management of benign paroxysmal positional vertigo: Gans vs. Epley maneuver; a randomized comparative clinical trial. Eur. Arch. Otorhinolaryngol. 2017, 274, 2973–2979. [Google Scholar] [CrossRef]
- Sacco, R.R.; Burmeister, D.B.; Rupp, V.A.; Greenberg, M.R. Management of benign paroxysmal positional vertigo: A randomized controlled trial. J. Emerg. Med. 2014, 46, 575–581. [Google Scholar] [CrossRef]
- Saeedi, M.; Khosravi, M.H.; Bayatpoor, M.E. Comparing the Effects of Epley Maneuver and Cinnarizine on Benign Positional Paroxysmal Vertigo; A Randomized Clinical Trial. Galen. Med. J. 2019, 8, e866. [Google Scholar] [CrossRef]
- Salvinelli, F.; Casale, M.; Trivelli, M.; D’Ascanio, L.; Firrisi, L.; Lamanna, F.; Greco, F.; Costantino, S. Benign paroxysmal positional vertigo: A comparative prospective study on the efficacy of Semont’s maneuver and no treatment strategy. La Clin. Ter. 2003, 154, 7–11. [Google Scholar]
- Salvinelli, F.; Trivelli, M.; Casale, M.; Firrisi, L.; Di Peco, V.; D’Ascanio, L.; Greco, F.; Miele, A.; Petitti, T.; Bernabei, R. Treatment of benign positional vertigo in the elderly: A randomized trial. Laryngoscope 2004, 114, 827–831. [Google Scholar] [CrossRef]
- Sammartino, G.; Mariniello, M.; Scaravilli, M.S. Benign paroxysmal positional vertigo following closed sinus floor elevation procedure: Mallet osteotomes vs. screwable osteotomes. A triple blind randomized controlled trial. Clin. Oral. Implants Res. 2011, 22, 669–672. [Google Scholar] [CrossRef] [PubMed]
- Sayin, I.; Koc, R.H.; Temirbekov, D.; Gunes, S.; Cirak, M.; Yazici, Z.M. Betahistine add-on therapy for treatment of subjects with posterior benign paroxysmal positional vertigo: A randomized controlled trial. Braz. J. Otorhinolaryngol. 2022, 88, 421–426. [Google Scholar] [CrossRef] [PubMed]
- Schuricht, A.; Hougaard, D.D. Is a Mechanical Rotational Chair Superior to Manual Treatment Maneuvers on an Examination Bed in the Treatment of Benign Paroxysmal Positional Vertigo? Otol. Neurotol. 2022, 43, e235–e242. [Google Scholar] [CrossRef] [PubMed]
- Se To, P.L.; Singh, D.K.A.; Whitney, S.L. Effects of customized vestibular rehabilitation plus canalith repositioning maneuver on gait and balance in adults with Benign Paroxysmal Positional Vertigo: A Randomized Controlled Trial. J. Vestib. Res. 2022, 32, 79–86. [Google Scholar] [CrossRef]
- Shan, X.; Peng, X.; Wang, E. Efficacy of computer-controlled repositioning procedure for benign paroxysmal positional vertigo. Laryngoscope 2015, 125, 715–719. [Google Scholar] [CrossRef] [PubMed]
- Sherman, D.; Massoud, E.A. Treatment outcomes of benign paroxysmal positional vertigo. J. Otolaryngol. 2001, 30, 295–299. [Google Scholar] [CrossRef]
- Simoceli, L.; Bittar, R.S.; Greters, M.E. Posture restrictions do not interfere in the results of canalith repositioning maneuver. Braz. J. Otorhinolaryngol. 2005, 71, 55–59. [Google Scholar] [CrossRef]
- Sinsamutpadung, C.; Kulthaveesup, A. Comparison of outcomes of the Epley and Semont maneuvers in posterior canal BPPV: A randomized controlled trial. Laryngoscope Investig. Otolaryngol. 2021, 6, 866–871. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.M.; Marroney, N.; Beattie, J.; Newdick, A.; Tahtis, V.; Burgess, C.; Marsden, J.; Seemungal, B.M. A mixed methods randomised feasibility trial investigating the management of benign paroxysmal positional vertigo in acute traumatic brain injury. Pilot Feasibility Stud. 2020, 6, 130. [Google Scholar] [CrossRef] [PubMed]
- Song, M.H.; Kong, T.H.; Shim, D.B. Optimal reassessment time for treatment response in posterior canal benign paroxysmal positional vertigo. Laryngoscope 2020, 130, 496–499. [Google Scholar] [CrossRef] [PubMed]
- Sridhar, S.; Panda, N.; Raghunathan, M. Efficacy of particle repositioning maneuver in BPPV: A prospective study. Am. J. Otolaryngol. 2003, 24, 355–360. [Google Scholar] [CrossRef]
- Steenerson, R.L.; Cronin, G.W. Comparison of the canalith repositioning procedure and vestibular habituation training in forty patients with benign paroxysmal positional vertigo. Otolaryngol. Head Neck Surg. 1996, 114, 61–64. [Google Scholar] [CrossRef]
- Sugita-Kitajima, A.; Sato, S.; Mikami, K.; Mukaide, M.; Koizuka, I. Does vertigo disappear only by rolling over? Rehabilitation for benign paroxysmal positional vertigo. Acta Otolaryngol. 2010, 130, 84–88. [Google Scholar] [CrossRef]
- Sun, L.B.; Zheng, Z.Y.; Wang, B.Q.; Yu, W.Y.; Yang, J.; Guo, W.J.; Ren, H.J. Curative effect analysis of the vestibular rehabilitation training on residual dizziness after successful canalith repositioning maneuvers in patients with benign paroxysmal positional vertigo. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2017, 31, 897–900. [Google Scholar] [CrossRef]
- Sundararajan, I.; Rangachari, V.; Sumathi, V.; Kumar, K. Epley’s manoeuvre versus Epley’s manoeuvre plus labyrinthine sedative as management of benign paroxysmal positional vertigo: Prospective, randomised study. J. Laryngol. Otol. 2011, 125, 572–575. [Google Scholar] [CrossRef]
- Tabanfar, R.; Chan, H.H.L.; Lin, V.; Le, T.; Irish, J.C. Development and face validation of a Virtual Reality Epley Maneuver System (VREMS) for home Epley treatment of benign paroxysmal positional vertigo: A randomized, controlled trial. Am. J. Otolaryngol. 2018, 39, 184–191. [Google Scholar] [CrossRef]
- Tacalan, E.; Inal, H.S.; Senturk, M.N.; Mengi, E.; Alemdaroglu-Gurbuz, I. Effectiveness of the Epley maneuver versus Cawthorne-Cooksey vestibular exercises in the treatment of posterior semicircular canal benign paroxysmal positional vertigo (BPPV): A randomized controlled trial. J. Bodyw. Mov. Ther. 2021, 28, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.; Yu, D.; Feng, Y.; Song, Q.; You, J.; Shi, H.; Yin, S. Comparative study of the efficacy of the canalith repositioning procedure versus the vertigo treatment and rehabilitation chair. Acta Otolaryngol. 2014, 134, 704–708. [Google Scholar] [CrossRef] [PubMed]
- Tanimoto, H.; Doi, K.; Katata, K.; Nibu, K.I. Self-treatment for benign paroxysmal positional vertigo of the posterior semicircular canal. Neurology 2005, 65, 1299–1300. [Google Scholar] [CrossRef] [PubMed]
- Testa, D.; Castaldo, G.; De Santis, C.; Trusio, A.; Motta, G. Treatment of horizontal canal benign paroxysmal positional vertigo: A new rehabilitation technique. ScientificWorldJournal 2012, 2012, 160475. [Google Scholar] [CrossRef]
- Tian, L.; Sheng, H.B.; Wang, J.; Luo, X.; Yu, J.; Jia, X.H.; Cheng, X.; Han, Z.; Chi, F.L. Comparative Study on the Roles of the Number of Accelerations and Rotation Angle in the Treatment Maneuvers for Posterior Semicircular Canal Benign Paroxysmal Positional Vertigo. ORL J. Otorhinolaryngol. Relat. Spec. 2016, 78, 36–45. [Google Scholar] [CrossRef]
- Toupet, M.; Ferrary, E.; Bozorg Grayeli, A. Effect of repositioning maneuver type and postmaneuver restrictions on vertigo and dizziness in benign positional paroxysmal vertigo. ScientificWorldJournal 2012, 2012, 162123. [Google Scholar] [CrossRef]
- Uz, U.; Uz, D.; Akdal, G.; Celik, O. Efficacy of Epley Maneuver on Quality of Life of Elderly Patients with Subjective BPPV. J. Int. Adv. Otol. 2019, 15, 420–424. [Google Scholar] [CrossRef]
- Vaz, D.P.; Gazzola, J.M.; Lanca, S.M.; Dorigueto, R.S.; Kasse, C.A. Clinical and functional aspects of body balance in elderly subjects with benign paroxysmal positional vertigo. Braz. J. Otorhinolaryngol. 2013, 79, 150–157. [Google Scholar] [CrossRef]
- von Brevern, M.; Seelig, T.; Radtke, A.; Tiel-Wilck, K.; Neuhauser, H.; Lempert, T. Short-term efficacy of Epley’s manoeuvre: A double-blind randomised trial. J. Neurol. Neurosurg. Psychiatry 2006, 77, 980–982. [Google Scholar] [CrossRef]
- Wang, T.; An, F.; Xie, C.; Chen, J.; Zhu, C.; Wang, Y. The treatment of benign positional paroxysmal vertigo of posterior semicircular canal by Epley maneuver combined with Semont maneuver. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2014, 28, 1469–1471. [Google Scholar]
- Wolf, M.; Hertanu, T.; Novikov, I.; Kronenberg, J. Epley’s manoeuvre for benign paroxysmal positional vertigo: A prospective study. Clin. Otolaryngol. Allied Sci. 1999, 24, 43–46. [Google Scholar] [CrossRef]
- Wu, F.; Xing, Y.Z.; Bi, W.; Liu, J.X. The value of lean nystagmus and sitting to supine positioning nystagmus in the diagnosis of horizontal semicircular canal benign paroxysmal positional vertigo. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2019, 33, 106–109. [Google Scholar] [CrossRef]
- Wu, P.X.; Liu, J.P.; Wang, W.Q.; Li, H.W. Intervention strategies for residual dizziness after successful repositioning maneuvers in benign paroxysmal positional vertigo: A single center randomized controlled trial. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2021, 56, 41–46. [Google Scholar] [CrossRef]
- Xu, Y.; Fu, M.; Zhang, N. Efficacy of different treatment on residual symptoms aftercanalith repositioning procedure in patients withbenign paroxysmal positional vertigo. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2016, 30, 1146–1149. [Google Scholar] [CrossRef]
- Yimtae, K.; Srirompotong, S.; Srirompotong, S.; Sae-Seaw, P. A randomized trial of the canalith repositioning procedure. Laryngoscope 2003, 113, 828–832. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Zhao, F. The effect of combination of Brandt-Daroff training and otolith reposition instrument pair in benign paroxysmal positional vertigo. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2021, 35, 598–601. [Google Scholar] [CrossRef]
- Zhang, H.; Geng, M.; Yan, B.; Lu, X. Epley’s manoeuvre versus Epley’s manoeuvre plus labyrinthine sedative in the management of benign paroxysmal positional vertigo: Prospective, randomised study. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2012, 26, 750–752. [Google Scholar]
- Zhang, Y.X.; Wu, C.L.; Xiao, G.R.; Zhong, F.F. Comparison of three types of self-treatments for posterior canal benign paroxysmal positional vertigo: Modified Epley maneuver, modified Semont maneuver and Brandt-Daroff maneuver. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2012, 47, 799–803. [Google Scholar]
- Zou, S.Z.; Li, J.R.; Tian, S.Y.; Ju, J.; Jia, M.Y. A randomized controlled trial on short-term efficacy of the modified Semont maneuver for the treatment of posterior canal benign paroxysmal positional vertigo. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2017, 31, 1468–1472. [Google Scholar] [CrossRef]
- Chen, Z.J.; Chang, C.H.; Hu, L.Y.; Tu, M.S.; Lu, T.; Chen, P.M.; Shen, C.C. Increased risk of benign paroxysmal positional vertigo in patients with anxiety disorders: A nationwide population-based retrospective cohort study. BMC Psychiatry 2016, 16, 238. [Google Scholar] [CrossRef]
- Hu, Y.; Lu, Y.; Wang, S.; Quan, X.; Ren, Y.; Rong, K.; Pan, S.; Lu, X.; Chen, L.; Tian, C.; et al. Global research trends in benign paroxysmal positional vertigo: A bibliometric analysis. Front. Neurol. 2023, 14, 1204038. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.J.; Hsu, C.W.; Stubbs, B.; Chen, T.Y.; Liang, C.S.; Chen, Y.W.; Zeng, B.Y.; Tseng, P.T. Audiovestibular Dysfunction in Hyper-IgE Syndrome: A Systematic Review of Characteristics, Pathophysiology, Diagnosis, and Management. Int. J. Mol. Sci. 2025, 26, 9932. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.J.; Hsu, C.W.; Chen, T.Y.; Liang, C.S.; Chen, Y.W.; Zeng, B.Y.; Tseng, P.T. Audiovestibular Dysfunction in Patients with Hashimoto’s Disease: A Systematic Review. Int. J. Mol. Sci. 2025, 26, 4703. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.J.; Hsu, C.W.; Chen, Y.W.; Chen, T.Y.; Zeng, B.S.; Tseng, P.T. Audiological Features in Patients with Rheumatoid Arthritis: A Systematic Review. Int. J. Mol. Sci. 2024, 25, 13290. [Google Scholar] [CrossRef]
- Chen, J.J.; Hsu, C.W.; Chen, Y.W.; Chen, T.Y.; Zeng, B.Y.; Tseng, P.T. Audiovestibular Dysfunction Related to Anti-Phospholipid Syndrome: A Systematic Review. Diagnostics 2024, 14, 2522. [Google Scholar] [CrossRef]
- Chen, J.J.; Hsu, C.W.; Chen, Y.W.; Chen, T.Y.; Zeng, B.S.; Tseng, P.T. Audiovestibular Dysfunction in Systemic Lupus Erythematosus Patients: A Systematic Review. Diagnostics 2024, 14, 1670. [Google Scholar] [CrossRef]
- Chen, J.J.; Lui, C.C.; Chen, T.Y.; Tseng, P.T.; Hung, C.M. The Tyndall Effect in High-Resolution Computed Tomography of Semicircular Canalolithiasis with Benign Paroxysmal Positional Vertigo. Diagnostics 2022, 12, 1000. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).