1. Introduction
Treatment of oral potentially malignant disorders (OPMD) and oral malignant lesions does not simply ends with the complete removal of the affected tissues. Since then, the oral physician plays a key role in terms of secondary prevention, carried out through an appropriate guidance of the patient to a change of lifestyle, and regular post-therapy surveillance. Relapse for head and neck squamous cell carcinoma varies from 16% to 52% [2]. Patients with primary tumor diagnosis also have a higher chance to develop second primary tumors (SPTs), arising further than 2 cm from the primary site and/or 5 years later than primary diagnosis, due to an independent carcinogenesis leading to the onset of a new tumor [1,2]. Aim of the present study was to review retrospectively, from 2003 to 2018, how many patients, firstly diagnosed with an oral malignant neoplasm, experienced a subsequent malignant and/or premalignant disorder, in the form of new OPMD, cancerized OPMD, relapsed cancer or SPT.
2. Methods
Electronic archive of the Oral Medicine Section of University of Turin, Italy was reviewed. Inclusion criteria were the following: patients firstly diagnosed with a malignant neoplasm, who later developed at least one OPMD or another malignant neoplasm. The following data were acquired: histological diagnosis, site of occurrence, new OPMD, relapsed OPMD, SPTs and relapsed cancer.
3. Results
A sample of 79 patients (41 F, 38 M; mean age 67.5 years) was finally examined, associated with 199 histological reports. Figure 1 and Figure 2 show their distribution based on histology and anatomic site.
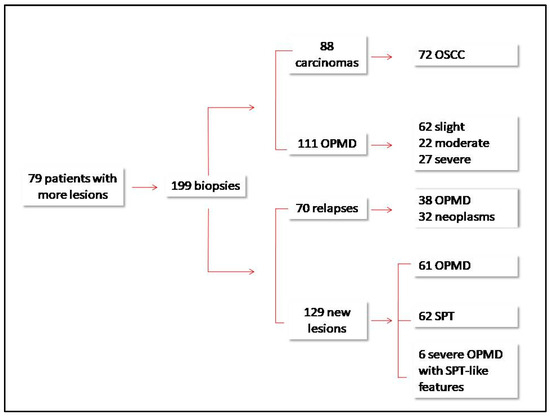
Figure 1.
Flow-chart showing the distribution for type of lesion and new lesions/relapses ratio.
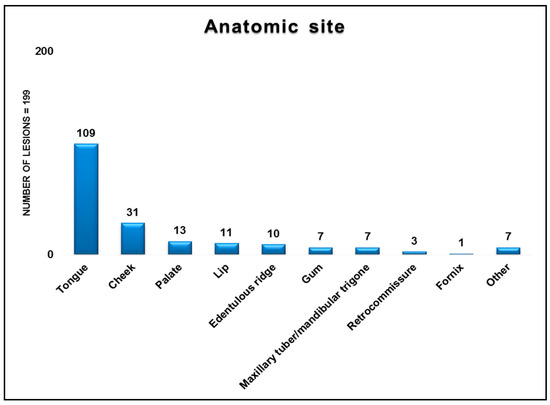
Figure 2.
Distribution of the 199 lesions according to the anatomic site.
Of the 199 lesions detected, 111 (55.8%) were premalignant, whereas 88 (44.2%) where malignant. Seventy-two of the 88 malignancies (81.8%) were diagnosed as oral squamous cell carcinoma (OSCC). Of 199 lesions, 70 could be categorized as relapsed lesions: 38 were diagnosed as OPMD and 32 as neoplasms. Of the remaining 129 new lesions, either detected 2 cm further from the primary site or 5 years after diagnosis, 62 were SPT, 6 severe OPMD with SPT-like features, and 61 OPMD.
4. Discussion
In this case-series, tongue was by far the most affected site for premalignant and malignant recurrent disorders. Rate of oral cancer relapse in our series aligned with that of the most recent literature (36.3% vs. range of 14–52% by Netto and co-workers) [2].
References
- Brands, M.T.; Smeekens, E.A.J.; Takes, R.P.; Kaanders, J.H.A.M.; Verbeek, A.L.M.; Merkx, M.A.W.; Geurts, S.M.E. Time patterns of recurrence and second primary tumors in a large cohort of patients treated for oral cavity cancer. Cancer Med. 2019, 8, 5810–5819. [Google Scholar] [CrossRef] [PubMed]
- Gleber-Netto, F.O.; Braakhuis, B.J.; Triantafyllou, A.; Takes, R.P.; Kelner, N.; Rodrigo, J.P.; Strojan, P.; Vander Poorten, V.; Rapidis, A.D.; Rinaldo, A.; et al. Molecular events in relapsed oral squamous cell carcinoma: Recurrence vs. secondary primary tumor. Oral Oncol. 2015, 51, 738–744. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).