Highlights
- Postpartum depression has multiple implications, not only on the mother (behavior) but also on the child (mental development).
- Early diagnosis and appropriate therapeutic approach/psychological counseling are key factors for good postpartum depression management.
Highlights
- Postpartum depression has multiple implications, not only on the mother (behavior) but also on the child (mental development).
- Early diagnosis and appropriate therapeutic approach/psychological counseling are key factors for good postpartum depression management.
Abstract
A woman goes through many biological (hormonal, physical), psychological (emotional), and socio-cultural changes during pregnancy. Furthermore, changes also occur in the mother’s familial and interpersonal world after childbirth. While some mothers have positive emotions at birth, such as joy and pleasure, others complain of negative experiences varying from sadness and depression to psychosis. Thus, the risk of depression is higher for women during the postpartum period, having a tendency to decrease in most cases over the first 2 weeks after delivery. Unfortunately, this favorable evolution does not happen in about 1 in 4–7 women, who develops postpartum depression. Postpartum depression has generally the same features as any common depressive episode encountered at any other time in life. However, assessment of depressive symptoms in the parental period implies not only general tools (such as the Depression Scale of the Center for Epidemiological Studies or the Beck Depression Inventory), but also a specific evaluation using the Edinburgh Postnatal Depression Scale. Taking into account all changes that occur during the peripartum period, a multimodal approach for postpartum depression would be recommended, including an appropriate lifestyle (walks, ambient environments), counseling, cognitive-behavioral therapy, and finally antidepressant medication when required. As a conclusion, postpartum depression may range from a mild and reversible episode to a severe and persistent form. Antepartum and postpartum screening, an early diagnosis, and a tailored approach to depression are essential for better results and prognosis related to both mother and child.
Introduction
The diagnosis of depression is generally three times greater in women than in men. In addition, depression seems to affect the person's functioning to a greater extent in women. The World Health Organization (WHO) considers that about a quarter of women suffer from an affective disorder throughout their lives. The vulnerability to depression increases in women mostly during childbearing age (15-44 years), such a disorder often associating with hormonal and psychosocial factors/ imbalances [1]. In women depression may also occur when breast cancer is diagnosed and/ or after breast cancer surgery [2], as well as in close relation with type of birth [3] or after serious complications during cesarean surgery [4].
A vulnerable period for the occurrence of depression in women is the postpartum period, up to 85% of women being placed in circumstances that lead to the experience of different levels of affective disorders during this stage. As an example, the American Academy of Pediatrics (AAP) estimates that more than 400,000 children are born each year to depressed mothers.
Postpartum affective disorders are classified according to their intensity in:
- Postpartum sadness (baby blues or maternity blues), with onset in the first 2 postpartum weeks. Baby Blues is a term used to describe worry, fear, and unhappiness or fatigue, feelings through which many women pass after birth. Baby Blues affects up to 80% of mothers and lasts for 1-2 weeks, having a mild intensity.
- Postpartum depression, which can stretch over a longer period of time, from 1 to 12 months after the birth.
- Puerperal psychosis (in the immediate after-birth period), which presents an acute onset during the first 3- 4 weeks postpartum [5].
Generally, symptoms of affective disorders are for most women transient (postpartum blues), but up to 10- 15% of women may experience persistent symptoms of depression and 0.1-0.2% may develop severe postpartum depression associated with psychosis [6].
Discussions
Postpartum depression is defined as the occurrence of a mild/ moderate non-psychotic depressive episode, with onset from the first postnatal month to 1 year. It is more common in developed countries, raising a major public health problem, due to the negative effects on the mother and the child (especially in terms of the child’s development), but also on the marriage relationship and even social relationships. Postpartum depression is characterized by psychological, physical, and emotional changes that occur in women after birth. Its diagnosis is based on the time interval between birth and onset of the condition, but also on the severity of the depression [7].
Postpartum depression has common features with a depressive episode that occurs at any other time in life: irritability, anxiety, feelings of loneliness, fear of madness, and loss of self. Women with postnatal depression show increased anxiety and are self- perceived as incapacitating and unbearable mothers [8]. Postpartum depression may occur de novo in normally mentally healthy women, or build on the background of small pre-existing psycho-emotional disorders, or continue a prenatal deep sadness (inapetence, loss of interest, trouble sleeping and eating, etc.).
Depression is also more common in people/ women with risk factors. Certain hormonal, biological, and psychosocial factors are considered risk factors for postpartum affective disorders. In postpartum depression, extreme feelings such as sadness and anxiety predominate, making the mother feel unable to care for her, her family, and especially her child [9]. Regarding postpartum depression, hormonal factors are represented by the decrease of estrogen, progesterone, and cortisol concentration in blood, changes that occur in the first 48 hours after delivery. Affected/ susceptible women may be abnormally sensitive to hormonal variations, and may develop symptoms of depression. Recent data indicate that premenstrual dysphoric syndrome is a risk factor for postpartum major depressive disorder [10]. It is well known that during pregnancy, estrogen and progesterone blood levels are 10 times higher than usual. Their sudden drop after delivery appears to be related to postpartum depression, this association being not yet fully understood. Postpartum and even perinatal (including both postpartum and prenatal) depression has also been associated with low levels of oxytocin [11].
Recent studies indicate that there are complex associations between immunity and depression. One such study, starting from the observation that postpartum depression is more common than depression during pregnancy, was performed on a sample of 51 women. During the study, mood and anxiety level were assessed, as well as 23 cytokines, 5 times during pregnancy and postpartum. An increase in pro- inflammatory markers occurs during the peripartum period in patients with depressive or anxious symptoms. The results indicate, in mentally ill women, increased activation of the immune response occurring towards the end of pregnancy [12]. Another study performed at Brazil State Maternity from 2015 to 2017 on a sample of 168 patients, with 40 women with hypertensive disorders of pregnancy (HDP) and 126 normotensive ones, found that women diagnosed with HDP had more depressive symptoms than their normotensive counterparts [13].
The first pregnancy is at increased risk of peripartum depression, which is explained at least in part by the mother's lack of experience. A decrease in the incidence of parental depression has been reported in couples who attended parenting courses before the birth of the first child [14].
Besides clinical symptoms and laboratory data (although the term postpartum depression officially entered the medical literature in 1950), so far only 17 imaging studies of the brain have been performed to investigate postpartum depression [15].
Psychological risk factors are associated with a history of personal depression, anxiety or depression in pregnancy, low social support, or recent negative impact events such as a family member death, financial difficulties, or partner violence. Also, women with a history of postpartum depression or psychosis have a recurrence risk of up to 90% [16].
Biological vulnerability is associated with a personal history of depression, family history of behavioral disorders, or depression during pregnancy, these women having a higher risk of developing postpartum depression. Apparently, there is no conclusive association between obstetrical factors and the risk of postpartum depression.
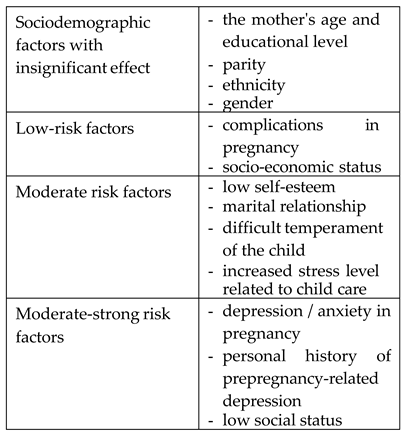
Risk factors are classified based on their effects, as shown in Table 1.

Table 1.
Risk factors classification for postpartum depression.
Postpartum depression is diagnosed when at least 5 of the following symptoms (and at least one of the first two) are present, with a duration of at least 2 weeks [17].
- Depressive mood, sadness, feelings of despair and inner void, associated with a state of severe anxiety;
- Loss of interest in daily activities;
- Changes in appetite and weight (usually decreasing);
- Changes in sleep (usually insomnia);
- Changes in attitude and speech (restlessness, apathy);
- Extreme fatigue or lack of energy;
- Feelings of futility or guilt;
- Difficulties in maintaining concentration or decision making;
- Suicidal thoughts.
Depressive symptoms in the perinatal period can be measured using specific instruments such as the Edinburgh Postnatal Depression Scale (EPDS), and/ or general tools such as the Depression Scale of the Center for Epidemiological Studies (CES-D) or the Beck Depression Inventory scale [6]. The Edinburgh Postnatal Depression Scale (EPDS) contains 10 questions for assessing the risk of depression during and after pregnancy, with a score between 0 and 3. Scores higher than 13 correspond to high level of symptoms [7]. The EPDS not only assesses the risk of postpartum depression, but also correlates with breastfeeding, the effects on the father, the type of birth, and its influence on the mental condition, especially in association with other predictive scales. Using this assessment instrument and a breastfeeding self-efficacy scale, a cohort study of 83 patients demonstrated that postpartum depression is a major risk factor for discontinuation of breastfeeding [18].
Depression can affect not only women but also men when they become parents, and this psycho-social factor can induce/ increase in turn the postpartum depression of the mother. Men may feel sadness, fatigue, anxiety, and perceive changes in their usual habits. Symptoms are similar to those seen in postpartum women, or to depression in general. A risk category for fathers with depression is young men and those who face financial or couple problems. Sometimes called paternal depression, this affection can have the same effects on the child and the couple's relationship as postpartum depression. One study conducted on a sample of 298 spouses of pregnant women who gave birth by caesarean section to Zonguldak Maternity (the data being collected using Edinburgh Postnatal Depression Scale) showed that more than one-third of fathers were at risk for postpartum depression. The study concluded that the risk of postpartum depression is high for fathers having a female newborn, or having a spouse with postpartum depression.
Noting that in the UK about 92,000 women give birth annually via elective cesarean section, a study was conducted (between 2015 and 2016 at Wales Hospital University] to determine the prevalence of depression and anxiety using specific assessment questionnaires and the Edinburgh Scale. Women with prenatal anxiety who gave birth by elective cesarean section showed ongoing symptoms more than a year after delivery [19].
Another cohort study performed at 2 and 6 months postpartum included 513 questionnaires reporting on three scales: the Karitane Parenting Confidence Scale (KPCS), the Edinburgh Postnatal Depression Scale (EPDS), and the Parental Stress Scale (PSS). This study demonstrated that KPCS scores at 2 months postpartum were the strongest predictors for both maternal and parental stress, symptoms that generally involved the underlying symptoms of postpartum depression [20].
Postpartum depression acts on both the mother and the child. The child may show a delay in developing mental and behavioral abilities, such that an early therapeutic approach toward postpartum depression is recommended. This strategy has been associated with a better prognosis, therapeutic options being carefully adapted to the severity of the disease. Failure or inappropriate treatment can lead to a deterioration of the relationship between the mother and child or between mother and her partner. It may also increase the risk of morbidity in both the mother and child [21].
Although several studies have sought ways to prevent postpartum depression, no specific factor for triggering postpartum depression has been identified. As a consequence, therapeutic options for postpartum depression are multiple and typically include some form of a multimodal therapy, as presented below.
Cognitive-behavioral therapy
When applied by a trained counselor, studies have shown that symptoms of postpartum depression decrease after the first session and show significant relief after six sessions [22].
Antidepressant medication
The use of antidepressants that have no adverse effects on the child are recommended so as to avoid the need to stop breastfeeding. Whether or not breastfeeding, treatment with serotonin reuptake inhibitors (SSRI) is recommended, due to the fact that this class of drugs is highly effectiveand presents mininimal side effects for women with postnatal depression [23].
Women treated with valproic acid or carbamazepine should avoid breastfeeding as these medications can cause liver toxicity in the baby. Also, breast-feeding should be avoided in premature or hepatically impaired children due to the difficulty of metabolizing these agents contained in mother’s milk [24].
Antidepressant medication used to treat postpartum depression can also treat symptoms such as insomnia, inappetence, and exhaustion but may not bring relief from negative thought patterns that cause/ maintain depression. For this reason, the Canadian Mental Health Organization recommends combining medication with psychological counseling [25].
Other recommendations that have proven useful for postpartum depression are walking or moderate exercise, family or friends visits, ambient lighting, and a balanced diet with avoidance of coffee and alcohol consumption. Daily exercise and avoiding overwork, good sleep, and rest have documented benefits. Interacting with others who also suffer from the problem is recommended, along with music therapy. Aromatherapy may help prevent the occurrence of postpartum depression and may also be an adjuvant treatment for it [26].
High cholesterol levels during postpartum may contribute to protecting the mother's psychological state [27]. Finally, there is no link between HIV-positive pregnant women receiving antiretroviral therapy and postpartum depression [28].
Conclusions
Perinatal mental illness, including pospartum depression, is generally under-diagnosed. Postpartum depression may range from a mild and reversible episode (with a tendency to decrease in most cases over the first 2 weeks after delivery) to severe and persistent forms that require adequate/ multimodal therapeutic support.Healthcare professionals should regularly evaluate women during antepartum and postpartum periods, using general and specific tools (Depression Scale of the Center for Epidemiological Studies, the Beck Depression Inventory, the Edinburgh Postnatal Depression Scale). Women who are at high-risk for developing postpartum depression should be identified and carefully monitored. An early diagnosis of postpartum depression allows a precoce and tailored approach for the condition, both of which are essential for optimal results related to mental and physical evolution of mother and child(s).
Conflicts of Interest
The authors declare that there are no conflicts of interest to be disclosed for this article.
References
- Chung, F.F.; Wan, G.H.; Kuo, S.C.; Lin, K.C.; Liu, H.E. Mother-infant interaction quality and sense of parenting competence at six months postpartum for first-time mothers in Taiwan: A multiple time series design. BMC Pregnancy Childbirth. 2018, 18, 365. [Google Scholar] [CrossRef]
- Kristensen, I.H.; Simonsen, M.; Trillingsgaard, T.; Pontoppidan, M.; Kronborg, H. First-time mothers' confidence mood and stress in the first months postpartum. A cohort study. Sex Reprod Healthc. 2018, 17, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Janssen, A.B.; Savory, K.A.; Garay, S.M.; Sumption, L.; Watkins, W.; Garcia-Martin, I.; Savory, N.A.; Ridgway, A.; Isles, A.R.; Penketh, R.; Jones, I.R.; John, R.M. Persistence of anxiety symptoms after elective caesarean delivery. B J Psych Open. 2018, 4, 354–360. [Google Scholar] [CrossRef] [PubMed]
- Kianpour, M.; Moshirenia, F.; Kheirabadi, G.; Asghari, G.; Dehghani, A.; Dehghani-tafti, A. The Effects of Inhalation Aromatherapy with Rose and Lavender at Week 38 and Postpartum Period on Postpartum Depression in High-risk Women Referred to Selected Health Centers of Yazd, Iran in 2015. Iranian Journal of Nursing and Midwifery Research 2018, 23, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Diaconu, C.; Balaceanu, A.; Bartos, D. Venous thromboembolism in pregnant woman – a challenge for the clinician. Central European Journal of Medicine. 2013, 8, 548–552. [Google Scholar] [CrossRef]
- Scăunașu, R.V.; Voiculescu, Ș.; Popescu, B.; Popa, R.; Bălălău, D.O.; Răducu, L.; Cozma, C.N.; Jecan, C.R. Depression and breast cancer; postoperative short- term implications. J Mind Med Sci. 2018, 5, 82–84. [Google Scholar] [CrossRef]
- Pleș, L.; Sima, R.M.; Carp, D.; Alexăndroaia, C.; Bălălău, D.O.; Stănescu, A.D.; Olaru, O.G. The psychosocial impact of vaginal delivery and cesarean section in primiparous women. J Mind Med Sci. 2018, 5, 70–74. [Google Scholar] [CrossRef]
- Buttner, M.M.; Mott, S.L.; Pearlstein, T.; Stuart, S.; Zlotnick, C.; O'Hara, M.W. Examination of premenstrual symptoms as a risk factor for depression in postpartum women. Arch Womens Ment Health. 2013, 16, 219–225. [Google Scholar] [CrossRef]
- Strapasson, M.R.; Ferreira, C.F.; Ramos, J.G.L. Associations between postpartum depression and hypertensive disorders of pregnancy. Int J Gynaecol Obstet. 2018. [CrossRef]
- Scaunasu, R.V.; Burcoș, T.; Voiculescu, Ș.; Popescu, B.; Bertesteanu, Ș.V.; Bălălău, O.D.; Bacalbasa, N. , Bălălău Cristian. Conservative surgery of breast cancer in women; psychological benefits. J Mind Med Sci. 2016, 3, 13–18. [Google Scholar] [CrossRef]
- Sarna, A.; Singh, R.J.; Duggal, M.; et al. The prevalence and determinants of depression among HIV-positive perinatal women receiving antiretroviral therapy in India. Arch Womens Ment Health. 2018. [CrossRef] [PubMed]
- Noonan, M.; Doody, O.; Jomeen, J.; O'Regan, A.; Galvin, R. Family physicians perceived role in perinatal mental health: An integrative review. BMC Fam Pract. 2018, 19, 154. [Google Scholar] [CrossRef]
- Balalau, D.O.; Sima, R.M.; Bacalbașa, N.; Pleș, L.; Stănescu, A.D. Emergency peripartum hysterectomy, physical and mental consequences: A 6-year study. J Mind Med Sci. 2016, 3, 65–70. [Google Scholar] [CrossRef]
- Rowland, D.L.; Motofei, I.G.; Popa, F.; Constantin, V.D.; Vasilache, A.; Păunică, I.; Bălălău, C.; Păunică, G.P.; Banu, P.; Păunică, S. The postfinasteride syndrome; an overview. J Mind Med Sci. 2016, 3, 99–107. [Google Scholar] [CrossRef]
- Chen, Y.H.; Huang, J.P.; Au, H.K.; Chen, Y.H. High risk of depression, anxiety, and poor quality of life among experienced fathers, but not mothers: A prospective longitudinal study. J Affect Disord. 2018, 242, 39–47. [Google Scholar] [CrossRef]
- Nagle, U.; Farrelly, M. Women's views and experiences of having their mental health needs considered in the perinatal period. Midwifery. 2018, 66, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Maleki, A.; Faghihzadeh, S.; Niroomand, S. The relationship between paternal prenatal depressive symptoms with postnatal depression: The PATH model. Psychiatry Res. 2018, 269, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Motofei, I.G.; Rowland, D.L.; Baconi, D.L.; Georgescu, S.R.; Paunica, S.; Constantin, V.D.; Balalau, D.; Paunica, I.; Balalau, C.; Baston, C.; Sinescu, I. Therapeutic considerations related to finasteride administration in male androgenic alopecia and benign prostatic hyperplasia. Farmacia. 2017, 65, 660–666. [Google Scholar]
- Georgescu, S.R.; Tampa, M.; Paunica, S.; Balalau, C.; Constantin, V.; Paunica, G.; Motofei, I. Distribution of post-finasteride syndrome in men with androgenic alopecia. J Investig Dermatol. 2015, 135, S40. [Google Scholar]
- Johnson, J.E.; Wiltsey-Stirman, S.; Sikorskii, A.; Miller, T.; King, A.; Blume, J.L.; Pham, X.; Moore Simas, T.A.; Poleshuck, E.; Weinberg, R.; Zlotnick, C. Protocol for the ROSE sustainment (ROSES) study, a sequential multiple assignment randomized trial to determine the minimum necessary intervention to maintain a postpartum depression prevention program in prenatal clinics serving low-income women. Implement Sci. 2018, 13, 115. [Google Scholar] [CrossRef]
- Balalau, C.; Voiculescu, S.; Motofei, I.; Scaunasu, R.V.; Negrei, C. Low dose tamoxifen as treatment of benign breast proliferative lesions. Farmacia. 2015, 63, 371–375. [Google Scholar]
- Gallaher, K.G.H.; Slyepchenko, A.; Frey, B.N.; Urstad, K.; Dørheim, S.K. The Role of Circadian Rhythms in Postpartum Sleep and Mood. Sleep Med Clin. 2018, 13, 359–374. [Google Scholar] [CrossRef] [PubMed]
- McEvoy, K.; Payne, J.L.; Osborne, L.M. Neuroactive Steroids and Perinatal Depression: A Review of Recent Literature. Curr Psychiatry Rep. 2018, 20, 78. [Google Scholar] [CrossRef] [PubMed]
- Silverman, M.E.; Smith, L.; Lichtenstein, P.; Reichenberg, A.; Sandin, S. The association between body mass index and postpartum depression: A population-based study. J Affect Disord. 2018, 240, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Treut, L.L.; Poinso, F.; Grandgeorge, P.; Jouve, E.; Dugnat, M.; Sparrow, J.; Guivarch, J. Infant psychomotor development in cases of maternal postpartum depression: Observation of a mother and baby unit. Ment Illn. 2018, 10, 7267. [Google Scholar] [CrossRef]
- Khalifa, D.S.; Glavin, K.; Bjertness, E.; Lien, L. Course of depression symptoms between 3 and 8 months after delivery using two screening tools (EPDS and HSCL-10) on a sample of Sudanese women in Khartoum state. BMC Pregnancy Childbirth. 2018, 18, 324. [Google Scholar] [CrossRef]
- Drozd, F.; Haga, S.M.; Valla, L.; Slinning, K. Latent trajectory classes of postpartum depressive symptoms: A regional population-based longitudinal study. J Affect Disord. 2018, 241, 29–36. [Google Scholar] [CrossRef]
- Shorey, S.; Chee, C.Y.I.; Ng, E.D.; Chan, Y.H.; Tam, W.W.S.; Chong, Y.S. Prevalence and incidence of postpartum depression among healthy mothers: A systematic review and meta-analysis. J Psychiatr Res. 2018, 104, 235–248. [Google Scholar] [CrossRef]
© 2018 by the authors. 2018 Anca Daniela Stanescu, Denisa Oana Balalau, Liana Ples, Stana Paunica, Cristian Balalau