Abstract
Introduction. Fecaluria and pneumaturia are the patognomonic signs of an abnormal communication between the bladder and the intestinal tract. Therefore, when a history of digestive signs, symptoms or digestive diseases is missing, this borderline pathology leads the patients in the care of urologists. From diagnosis to treatment the management of these cases can be difficult and challenging. Materials and Methods. A 48 year old patient, without any significant medical history, presented to the emergency room for fecaluria, pneumaturia and an episode of haematuria. He had no prior digestive symptoms. The contrast enhanced abdominal and pelvic CT scan revealed a pelvic mass involving the sigmoid colon and the dome and the posterior wall of the bladder. The cystoscopy objectifies a tumor mass involving the right postero-lateral bladder wall, with extravasation of faeces. A biopsy was taken and the frozen section found mainly uncertain inflammatory type tissue. A colonoscopy couldn’t be done because of an impassable obstacle at 15 cm from the anus. Together with general surgeons we decided for en bloc resection of the tumor with partial cystectomy, right ureterocystoneostomy and rectosigmoid resection with mechanic end to end anastomosis. Results. The postoperative period was uneventful. The histopathological examination revealed an abscessed sigmoid diverticulum with vesico-sigmoid fistula and perilesional inflammatory tissue. Two years after the surgery the patient is asymptomatic with a normal function of the right kidney and restored bladder capacity. Conclusions. Being a borderline pathology, patients with fecaluria and pneumaturia and lack of digestive symptoms are referred and managed by the urologists. Despite extensive investigations, even when preoperative biopsies reveal inflammatory tissue the patients should be treated as oncologic cases. A close cooperation with general surgeons for en bloc multiorgan resection within oncologic safety margins is mandatory.
Introduction
Fecaluria and pneumaturia are the patognomonic signs of an abnormal communication between the bladder and the intestinal tract. Therefore, when a history of digestive signs, symptoms or digestive diseases is missing, this borderline pathology leads the patients in the care of urologists. From diagnosis to treatment the management of these cases can be difficult and challenging.
The most common cause of colo-vezical fistulae (CVF) is represented by sigmoid diverticulitis, followed by malignant tumors, Crohn's disease and radiotherapy [1,2,3]. These occur through a peridiverticular abcess fistulization into the bladder and are more common in men than in women (because of the uterus interposition that protects the bladder) [4].
Approximately 65% of CVF may be of diverticular origin [5]. In diverticulitis, CVF incidence is reported to be between 2-4% [6,7]. The treatment of choice in the CVF is surgical, the therapeutic approach requiring multidisciplinary management, by urologists and general surgeons. We present the case of a patient with fecaluria and pneumaturia that was successfully treated in our department.
Materials and Methods
A 48 year old patient, without any significant medical history, presented to the emergency room for fecaluria, pneumaturia and an episode of haematuria. He had no prior digestive symptoms. The clinical examination was within normal limits. The rectal examination revealed a normal prostate. The laboratory workup showed leukocytosis of 17 000 UI/L.
The contrast enhanced abdominal and pelvic CT scan revealed a pelvic mass involving the sigmoid colon and the dome and the posterior wall of the bladder. Cystoscopy was performed and a tumor mass involving the postero-lateral bladder wall was seen, with extravasation of faeces. The biopsy revealed mainly uncertain inflammatory type tissue. The rectal examination under spinal anesthesia showed, after a deep palpation, a pelvic tumor mass. The lower GI endoscopy was inconclusive because the colonoscope could not progress after 15 cm from the anus, due to an impassable obstacle.
A laparotomy was performed by a mixed team of general and urologic surgeons. A wide median pubo-supraombilical incision was made and a tumor was found at the level of the sigmoid colon with bladder and right pelvic ureter invasion. Because the malignant nature could not be ruled out, together with the general surgeons an oncologic intervention was decided and performed: partial cystectomy en bloc with segmental right ureterectomy and rectosigmoid resection. The team of urologists started with the partial cystectomy, then dissected and resected the distal segment of the right ureter. Afterwards the general surgeons carried on with a radical rectosigmoid resection (high ligation of the inferior mesenteric artery and inferior mesenteric vein). The reconstruction of the urinary and gastro-intestinal tracts consisted of: a reimplantation of the right ureter using the split – cuff nipple technique with an autostatic ”JJ” stent, a double layered cystorrhaphy, and an end to end colo-rectal anastomosis with circular GI stapler.
Results
The postoperative course was uneventful. The patient resumed normal bowel function on the 3rd day. The Folley catheter was removed on the 10th day and the patient was discharged on the 11th day. The histopathological examination revealed an abscessed sigmoid diverticulum with vesico-sigmoid fistula and perilesional inflammatory tissue. Suffering a short initial period of polakiuria due to the partial cystectomy, two years after the surgery the patient is asymptomatic with a normal function of the right kidney and restored bladder capacity.
Discussions
CVF is the most common type of fistula that is associated with colonic diverticulitis. But it is also quite frequent in digestive tumors located at the level of the sigmoid colon or the rectum. Pneumaturia and fecaluria are the most common presentation symptoms [3] and are considered to be pathognomonic for the diagnosis of CVF.
Although urethrocistoscopy and colonoscopy rarely allow direct visualization of the fistula [8] they are important in excluding the malignant etiology and in obtaining a biopsy for histopathological confirmation. In our case, a preoperative diagnosis could not be established, as the colonoscopy could not be continued because of anatomical considerations [8].
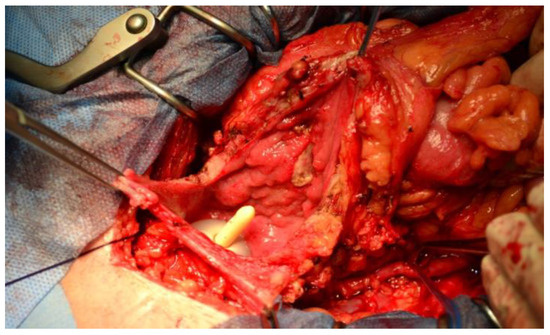
Image 1 .
Partial cystectomy en bloc with rectosigmoid resection.
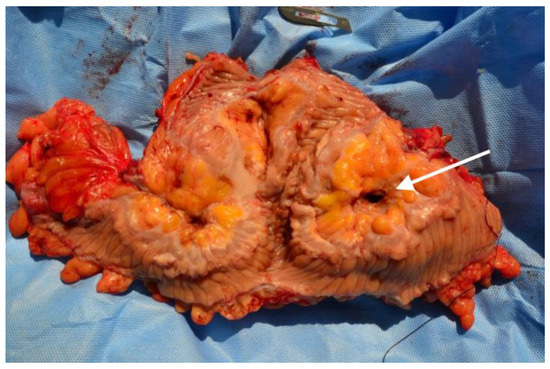
Image 2 .
Opperative specimen with identified CVF.
A preoperative diagnosis of certainty, confirming of infirming a malignant etiology is important in establishing the surgical management. Oncologic interventions with radical resections can bring additional morbidity compared to segmental non-radical resections that do not require lymphadenectomy. Until proven otherwise, the suspicion of a malignant lesion associated colo-vesical fistula should remain high, as a non-oncologic approach can lead to dissemination and seeding of the peritoneal cavity. Moreover, the absence of lymphadenectomy results in an incorrect and incomplete staging of the patient. In these uncertain cases, a joint effort between urologists and oncologic surgeons is essential.
The histopathological report is the only one which can diagnose malignancy. If neoplasia is confirmed the surgical treatment should be tailored according to the type of the tumor. A digestive origin implies performing a partial cystectomy with en bloc rectosigmoid resection, while a bladder invasive tumor (rarely encountered) requires radical cystectomy with appropriate colic resection (according to the degree of the invasion), urinary tract diversion and ilio-obturator limph node dissection. In our case, although the CT scan and the macroscopic intraoperative aspect were suggestive of malignancy, the pathologic examination did not confirm the presence of malignant cells. So the patient did not require an oncologic follow-up.
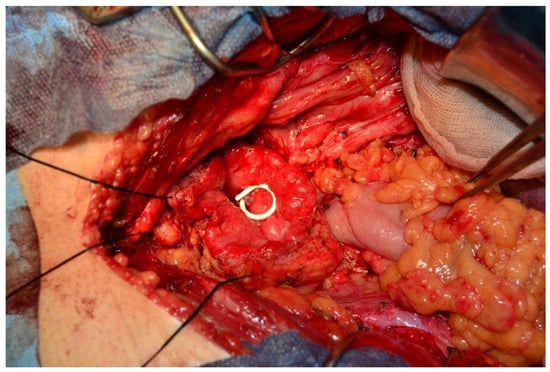
Image 3 .
Right ureterocystoneostomy with autostatic "JJ" stent.
Conclusions
Being a borderline pathology, patients with fecaluria and pneumaturia and lack of digestive symptoms are referred and managed by the urologists. Despite extensive investigations, even when preoperative biopsies reveal inflammatory tissue the patients should be treated as oncologic cases. A close cooperation with general surgeons for en bloc multiorgan resection within oncologic safety margins is mandatory. Sigmoid-vesical fistulas should be considered neoplasia until proven otherwise, the treatment of choice in our view is partial cystectomy with recto-sigmoid resection with oncologic safety limits. In case of malignancy, en bloc resection is of outmost importance to avoid dissemination and peritoneal cavity seeding.
References
- Walker, K.G.; Anderson, J.H.; Iskander, N.; McKee, R.F.; Finlay, I.G. Colonic resection for colovesical fistula: 5-year follow-up. Colorectal Dis 2002, 4, 270–274. [Google Scholar] [PubMed]
- Driver, C.P.; Anderson, D.N.; Findlay, K.; Keenan, R.A.; Davidson, A.I. Vesico-colic fistulae in the Grampian region: presentation, assessment, management and outcome. J R Coll Surg Edinb 1997, 42, 182–185. [Google Scholar] [PubMed]
- McBeath, R.B.; Schiff Jr, M.; Allen, V.; Bottaccini, M.R.; Miller, J.I.; Ehreth, J.T. A 12-year experience with enterovesical fistulas. Urology 1994, 44, 661–5. [Google Scholar] [CrossRef] [PubMed]
- Floch, M.H.; Bina, I. The natural history of divertiulitis: fact and theory. J. Clin. Gastroenterol. 2004, 38, 52–57. [Google Scholar]
- Woods, R.J.; Lavery, I.C.; Fazio, V.W.; Jagelman, D.G.; Weakley, F.L. Internal fistulas indiverticular disease. Dis Colon Rectum 1988, 31, 591–596. [Google Scholar] [PubMed]
- Melchior, S.; Cudovic, D.; Jones, J.; Thomas, C.; Gillitzer, R.; Thuroff, J. Diagnosis and surgical management of colovesical fistulas due to sigmoid diverticulitis. J Urol 2009, 182, 978–982. [Google Scholar] [PubMed]
- Najjar, S.F.; Jamal, M.K.; Savas, J.F.; Miller, T.A. The spectrum of colovesical fistula and diagnostic paradigm. Am J Surg 2004, 188, 617–621. [Google Scholar] [PubMed]
- Vasilevsky, C.A.; Belliveau, P.; Trudel, J.L.; Stein, B.L.; Gordon, P.H. Fistulas complicating diverticulitis. Int J Colorectal Dis 1998, 13, 57–60. [Google Scholar] [PubMed]
© 2015 by the author. 2015 C Gingu, A Dick, I Ianiotescu, C Baston, M Crasneanu, A Andresanu, L Domnisor, V Brasoveanu, A Martiniuc, I Sinescu