Abstract
Opportunistic fungi are a major cause of morbidity and mortality world-wide, particularly in immunocompromised individuals. Developing new treatments to combat invasive fungal disease is challenging given that fungal and mammalian host cells are eukaryotic, with similar organization and physiology. Even therapies targeting unique fungal cell features have limitations and drug resistance is emerging. New approaches to the development of antifungal drugs are therefore needed urgently. Cryptococcus neoformans, the commonest cause of fungal meningitis worldwide, is an accepted model for studying fungal pathogenicity and driving drug discovery. We recently characterized a phospholipase C (Plc1)-dependent pathway in C. neoformans comprising of sequentially-acting inositol polyphosphate kinases (IPK), which are involved in synthesizing inositol polyphosphates (IP). We also showed that the pathway is essential for fungal cellular function and pathogenicity. The IP products of the pathway are structurally diverse, each consisting of an inositol ring, with phosphate (P) and pyrophosphate (PP) groups covalently attached at different positions. This review focuses on (1) the characterization of the Plc1/IPK pathway in C. neoformans; (2) the identification of PP-IP5 (IP7) as the most crucial IP species for fungal fitness and virulence in a mouse model of fungal infection; and (3) why IPK enzymes represent suitable candidates for drug development.
1. Invasive Fungal Infections: The Clinical Burden
Invasive fungal infections (IFIs) are a major cause of global morbidity and mortality. The majority of IFIs worldwide are caused by Aspergillus spp., Candida spp., Cryptococcus spp., and Pneumocystis jirovecii. However, IFIs caused by emerging fungal pathogens, such as the yeast-like Trichosporon spp., Rhodotorula spp., and the moulds, Scedosporium spp., Fusarium spp., and Zygomycetes spp., are on the rise [1,2,3,4,5]. Due to a lack of international epidemiological and surveillance data, the effect of IFIs on human health is often under-reported [2,6] and consequently the true impact of IFIs on human health is not widely recognized.
Much of the burden of IFIs is on developing countries, which have high incidences of HIV/AIDS. According to a recent UNAIDS Global AIDS Report, 25.8 million people are estimated to be living with HIV in Sub-Saharan Africa, and the region accounts for almost 70% of new HIV infections world-wide [7]. In addition to HIV/AIDs patients, IFIs pose a significant threat to solid organ and hematopoietic stem cell or bone marrow transplant recipients. The US Centers for Disease Control and Prevention (CDC) has developed a list of the 20 most common opportunistic infections affecting immunocompromised individuals. Of these, 5 are caused by fungi [8]. IFIs are also an enormous economic liability to the global health system: a US study found that transplant patients with an IFI stayed in hospital an additional 19 days longer than patients without an IFI, resulting in an excess of ~USD 55,000 for hospital costs/patient [9]. Furthermore, there is a 5-fold increase in the mortality rate of these patients [9].
2. Molecular Targets of Antifungal Drugs and Drug Limitations
As fungi are eukaryotes, the number of selective drug targets is more limited than in the case of prokaryotes. Most marketed drugs (e.g., amphotericin B (AMB), azoles, terbinafine) target the unique fungal plasma membrane sterol, ergosterol, or its biosynthetic pathway, while the echinocandins and 5-flucytosine (5-FC) inhibit the unique cell wall and DNA synthesis, respectively. However, current antifungal therapies have limitations, which compound the adverse public health impact of IFIs. These limitations include an incomplete antifungal spectrum, toxicity, poor bioavailability, poor solubility or stability, and/or high cost. Although well tolerated, the echinochandins are ineffective in treating IFIs caused by Cryptococcus neoformans [10,11,12,13]. Multi-azole resistant Aspergillus fumigatus has been reported [14,15,16,17] and azole and echinocandin resistance has been observed in non-albicans Candida spp. [18,19,20]. Despite this, fluconazole resistance in Candida spp. was the only mention of antifungal drug resistance in the 2014 WHO global surveillance report [21].
For the treatment of meningitis caused by C. neoformans, guidelines issued by the World Health Organization and the Infectious Diseases Society of America, recommend induction therapy with AMB and 5-FC for 2 weeks, followed by maintenance therapy with the azole drug, fluconazole, for 8 weeks [22,23]. In resource limited countries where 5-FC may be frequently unavailable, it is recommended that adults are started on a high-dose fluconazole regime with AMB if the latter is available [22]. However, Day et al. published that AMB and fluconazole combination therapy did not increase patient survival in a Vietnamese cohort and called for greater access to 5-FC; a call echoed by others [24,25,26,27]. Infection relapse can also occur, particularly in patients who are not receiving maintenance therapy or antiretroviral therapy [28]. It is also of great concern that fluconazole-resistant C. neoformans has been reported in Sub-Saharan Africa and South East Asia, regions where the disease burden is the highest [29,30,31,32,33]. It is imperative to develop new drugs to combat these infections. This can be achieved either by repurposing old drugs which are useful in the treatment of other infectious microbes or by developing new classes of antifungal agents. To facilitate the development of new drugs, an understanding of the mechanisms that fungi employ to establish infection and cause disease in the human host is of paramount importance.
3. Cryptococcus neoformans: A Study Model for Virulence and Drug Development
C. neoformans is an opportunistic basidiomycetous yeast pathogen causing serious morbidity and mortality in immunocompromised individuals. Infection is acquired by inhalation of infectious propagules (spores or small desiccated yeast cells) into the lungs and manifests as pneumonia-like symptoms. Yeast cells can further disseminate via the blood and cross the blood brain barrier, resulting in life-threatening meningoencephalitis. Up to one million new cases of cryptococcal meningitis in people living with HIV/AIDs and around 600,000 deaths have been reported to occur annually [34]. Even with access to antiretroviral and antifungal therapy, mortality rates due to cryptococcal meningitis remain at 20%–40% [35,36,37,38]. C. neoformans is also a powerful model for elucidating the mechanisms that fungi use to cause disease: it is a budding yeast that is easy to grow, with minimal nutritional requirements and a defined mating cycle [39,40,41,42]; it produces a suite of virulence traits that are easily measured; and its haploid genome is highly amenable to targeted gene deletion, which can be combined with mating crosses to increase the number of gene deletions within the same genome [43,44]. Furthermore, a number of vertebrate and invertebrate infection models have been developed to address the impact of gene deletion on pathogenesis and virulence and to assess drug efficacy [45,46,47,48,49], also reviewed in [50,51].
C. neoformans virulence is multifactorial and includes the production of capsule, melanin, urease, Sec14-dependent phospholipase B1 (Plb1), the formation of titan cells and high temperature tolerance [52,53,54,55,56,57,58,59,60,61,62]. While some of the C. neoformans virulence determinants are unique, others contribute to virulence in other fungal pathogens, e.g., phospholipase B in Candida albicans [63,64], urease in Coccidioides posadasii [65], melanin and the extracellular polysaccharide (galactosaminogalactan) in Aspergillus fumigatus [66,67]. Production of virulence factors in C. neoformans is regulated by key signaling pathways, including the calcineurin, protein kinase C/mitogen-activated protein kinase (Pkc1/Mpk1), cyclic adenosine monophosphate/protein kinase A (cAMP/Pka1), high osmolarity glycerol (HOG), and Rim101 pathways [68,69,70,71,72,73,74]. Phospholipase C (Plc1)-dependent signalling also contributes to the fitness and virulence of C. neoformans [75], and the next section describes how this pathway was elucidated and characterized in this pathogen.
4. Signaling via Plc1 in C. neoformans: The Role of Inositol 1,4,5-Trisphosphate (IP3)
We established that phosphatidylinositol (PI)-specific phospholipase C1 (Plc1)—the homologue of Plc1 in Saccharomyces cerevisae [76,77,78] and mammalian phospholipase C (PLC-δ) [79] is essential for the virulence of C. neoformans [75]. In a mouse inhalation model, we found that infection with the cryptococcal PLC1 deletion mutant (plc1Δ) was cleared from the lung 14 days post-infection, and that the mutant failed to disseminate to the brain [75]. Furthermore, PLC1 deletion resulted in the attenuation of several key virulence factors: growth at 37 °C, production of melanin (and capsule under some growth conditions) and secretion of phospholipase B1 (Plb1). Given that Plb1 accumulated in the membrane in plc1Δ, we hypothesized that Plc1 also plays a role in releasing membrane-associated Plb1 from its glycosylphosphatidylinositol (GPI) anchor. However, this was not demonstrated directly. plc1Δ also had a cell wall integrity defect and was hyper-susceptible to all antifungal agents used in the treatment of cryptococcosis [75].
To investigate how Plc1 regulates cellular function, we established that recombinant cryptococcal Plc1 preferentially hydrolyses PI-4,5-bisphosphate (PIP2) to produce two signaling molecules, namely, inositol 1,4,5-trisphosphate (IP3) and diacylglycerol (DAG) [80]. In agreement with this finding, the plc1Δ mutant accumulated PIP2 and had reduced IP3 levels, as demonstrated using a radiometric IP3 assay [80]. In addition to Plc1, DAG is produced by the enzyme inositol-phosphorylceramide synthase-1 (Ipc1) and functions as an activator of cryptococcal Pkc1 [81]. Pkc1 acts upstream of the MAP kinase cell wall integrity pathway (Bck1/Mkk2/Mpk1), but also regulates melanization and cell wall homeostasis independently of the MAPK cascade [81,82]. Given the degree of phenotypic similarity between plc1Δ and pkc1Δ, including compromised melanin production and a cell wall integrity defect, and that cell wall perturbing agents fail to activate the Pkc1/Mpk1 pathway in plc1Δ, we deduced that Plc1-derived DAG contributes to Pkc1 activation [75].
In mammalian cells, IP3 derived from PLC-δ interacts with IP3 receptors in the endoplasmic reticulum, causing a release of intracellular calcium and an activation of calcineurin [83,84,85,86]. Fungal homologs of the mammalian IP3 receptor have not been identified, although IP3-mediated calcium release has been demonstrated in hyphal tips of filamentous fungus Neurospora crassa [87]. We observed that plc1Δ and the cryptococcal calcineurin deletion mutant (cna1Δ) shared significant phenotypic similarity under a range of stress conditions, suggesting that Plc1-derived IP3 could activate calcineurin in C. neoformans. However, we demonstrated that the simultaneous inactivation of Plc1 and calcineurin was more detrimental to cryptococcal growth than the inactivation of either calcineurin or Plc1 alone, suggesting that cryptococcal Plc1 activates effectors other than calcineurin. We concluded that Plc1 and the calcineurin pathway function in parallel to regulate a common set of phenotypes, including the ability to grow at 37 °C, cell wall integrity and cell morphology [68,80].
5. Delineating the IP Biosynthesis Pathway in C. neoformans
The cellular fate of Plc1-derived IP3 has been determined in non-pathogenic yeast and mammalian cells. The genomes of these organisms encode kinases, which use ATP to phosphorylate IP3 and other inositol polyphosphates (IP), to generate a structurally diverse family of IP species. Thus, in addition to its role as a secondary messenger, IP3 serves as a precursor for the synthesis of more complex IP. IP species are comprised of a six-carbon myo-inositol ring to which phosphates are covalently attached at various positions by inositol polyphosphate kinases (IPK). There are essentially two types of IP: those with single covalently attached phosphates and those with a mixture of single and diphosphate groups (inositol pyrophosphates, PP-IP). PP-IP contain “high-energy” phosphate bond(s), and are thought to undergo a rapid turnover in eukaryotic cells [88]. The IP biosynthesis pathway has been extensively studied in a model ascomycetous yeast, S. cerevisiae (reviewed in [89,90,91]) and our recent characterization of the pathway in C. neoformans (described forthwith) is the first in a fungal pathogen [80,92,93].
Using a homology search, we identified a number of putative IPK-encoding genes in the C. neoformans var grubii (wild-type strain H99 [WT], serotype A) genome. These included Arg1 and Arg2 [80], which are most similar to S. cerevisiae Arg82, a dual-specificity kinase phosphorylating Plc1-generated I(1,4,5)P3 to I(1,3,4,5)P4, and I(1,3,4,5)P4 to I(1,3,4,5,6)P5 [94,95], and the putative I(1,3,4,5,6)P5 kinase, Ipk1 [93] (Figure 1). We also identified two putative inositol pyrophosphate synthases, Kcs1 and Vip1 [92], which were predicted to add phosphates to the existing phosphates at positions 5 and 1, respectively, of the inositol ring. Similar to the fission yeast, Schizosaccharomyces pombe [96], Vip1 is referred to as Asp1 in the cryptococcal database.
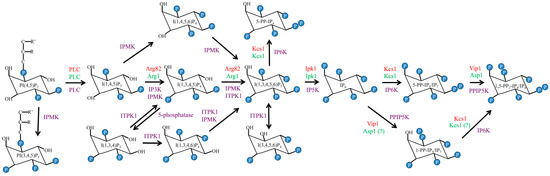
Figure 1.
Comparison of the phospholipase C1/inositol polyphosphate kinase Plc1/IPK pathways in yeast and humans. Enzymes in C. neoformans, S. cerevisiae and humans are marked in green, red and purple, respectively.
To confirm the function and substrate specificity of the IPK enzymes identified in C. neoformans, we determined the IP profiles of the corresponding deletion mutants using strong anion exchange (SAX)-HPLC (summarized in Figure 2 from publications [92,93]). Firstly, we confirmed that Arg1 is the major IP3 kinase in C. neoformans, since the ARG1 deletion mutant (arg1Δ) accumulated IP3 and was deficient in more complex IP species [80,92] (Figure 2B, Table 1). Despite the presence of the conserved IPK amino acid sequence motif, P-x-x-x-D-x-K-x-G [94], the arg2Δ mutant did not accumulate IP3 and was phenotypically identical to WT, demonstrating that Arg1 and Arg2 are not functionally redundant [80]. Although ARG2 most likely arose from ARG1 by gene duplication, its role in cellular function is not apparent [80].
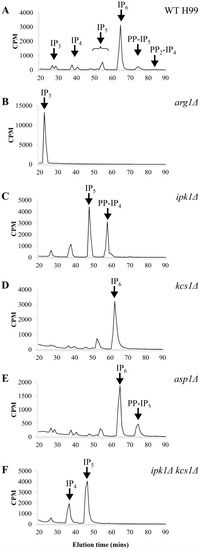
Figure 2.
Comparison of the IP profiles of (A) WT [92,93]; (B) arg1Δ [92]; (C) ipk1Δ [93]; (D) kcs1Δ [92]; (E) asp1Δ [92] and (F) ipk1Δ kcs1Δ [93]. Lysates prepared from [3H]-myo-inositol-labeled cells were subjected to anion-exchange HPLC analysis.

Table 1.
Summary of IP profiles of various strains [80,92,93]. In WT, + indicates that the species is present; in the mutants, multiple + indicates the level of accumulation of a species; − indicates the absence of a species. Note that IP6 is the most abundant IP species in WT (see Figure 2).
HPLC analysis of the IP profiles of the cryptococcal ipk1Δ and kcs1Δ mutants established that Ipk1 and Kcs1 are IP5 and IP6 kinases, respectively (Figure 2C,D) [92,93]. However, in the absence of Ipk1, Kcs1 also functions as an IP5 kinase: IP5 accumulates in the ipk1Δ mutant and a new pyrophosphate species, 5-PP-IP4, is created by Kcs1 via the addition of phosphate to the phosphate at position 5 (Figure 2C,F) [93]. When functional Ipk1 was present, Kcs1 phosphorylated IP6 to create 5-PP-IP5 (IP7). In the absence of Kcs1, PP-IP5 and PP2-IP4 (IP8) were not detected, suggesting that Kcs1 is the main IP6 kinase/PP-IP5 synthase in C. neoformans (Figure 2D, Table 1) [92].
Unlike other IPKs, mammalian and fungal Vip1/Asp1 enzymes have a dual domain structure comprising of an N-terminal kinase and a C-terminal histidine acid phosphatase-like domain. Except for the aspartate residue adjacent to the second histidine in the consensus active site, the key histidine and arginine residues are present in the Vip1 acid phosphatase-like domain [97]. Several studies demonstrate that the C-terminal domain of Vip1 has a negative effect on inositol pyrophosphate output by the N-terminal kinase domain, presumably via direct phosphate hydrolysis [96,97,98,99]. Interestingly, the acid phosphatase-like domain of Vip1 has also been implicated in binding the phospholipid, phosphatidylinositol (3,4,5)-trisphosphate [100]. We established that, similar to other Vip1 enzymes, cryptococcal Asp1 phosphorylates the Kcs1-derived product, 5-PP-IP5, to produce 1,5-PP2-IP4 (Figure 1). This is indicated by the absence of PP2-IP4 in the asp1Δ mutant (Figure 2E, Table 1) [92].
In addition to phosphorylating 5-PP-IP5, Vip1 enzymes also phosphorylate IP6 in vivo and in vitro [97,101]. However, the 1-PP-IP5 product of Vip1 is not easily detectable in vivo, presumably due to its rapid hydrolysis by phosphatases, including the C-terminal domain of the Vip1 protein itself [88,102]. In S. cerevisiae, Vip1-derived PP-IP5 was detectable by HPLC, but only when the polyphosphate phosphatase, Ddp1, and Kcs1 were absent (kcs1Δ ddp1Δ mutant) [101]. Interestingly, the cryptococcal genome does not encode a Ddp1 homolog. However, we did identify a close homolog of S. cerevisiae Siw14, which specifically dephosphorylates Kcs1-derived 5-PP-IP5, to modulate PP-IP metabolism [103].
6. The Contribution of IP/PP-IP Species to Cryptococcal Cellular Function
To determine the contribution of individual IP species to cryptococcal cellular function and virulence, we compared the phenotypic profiles of the entire IPK deletion mutant set [75,80,92,93] (summarized in Table 2). Overall, the mutants could be ranked as follows: plc1Δ > arg1Δ > kcs1Δ > ipk1Δ > asp1Δ, with plc1Δ having the most severe phenotypic defect. Similar to plc1Δ, growth of arg1Δ was compromised at 37 °C [80]. Both mutants exhibited a cell separation defect, enlarged vacuoles (more pronounced in arg1Δ), small capsules and a thickened cell wall. In contrast to arg1Δ, plc1Δ had diminished endocytic activity [80]. The virulence of plc1Δ and arg1Δ was attenuated in Galleria mellonella larvae incubated at the permissive mutant growth temperature of 30 °C. However, larvae infected with the plc1Δ mutant survived longer than those infected with arg1Δ [80].

Table 2.
Phenotypes of cryptococcal IPK mutants (summarized from [75,80,92,93]). * refers to the unpublished data. N/A, the data is not available.
Cell wall integrity and production of urease, melanin and mating filaments was compromised in the plc1Δ, arg1Δ and kcs1Δ mutants [75,80,92]. Defects in cell wall integrity and urease production were also observed in ipk1Δ, but to a lesser extent than in arg1Δ or kcs1Δ [93]. Melanization in plc1Δ, arg1Δ and kcs1Δ was assessed by examining colony color in the presence of the laccase substrate, l-Dopa, over a 3–4 day period. In a more quantitative approach, we assessed laccase activity in ipk1Δ and ipk1Δ kcs1Δ cells following a shift to laccase-inducing conditions (3–6 h in a minimal medium without glucose). Surprisingly, we discovered that laccase activity in these mutants was significantly reduced compared to WT [93], despite WT-like melanization in ipk1 Δ and ipk1 Δ kcs1 Δ. This suggests that the presence of low laccase activity over several days is sufficient to produce WT-like melanization in the mutants.
The virulence of kcs1Δ and ipk1Δ was also compromised: 100% and 80% of mice infected with kcs1Δ and ipk1Δ, respectively, survived the infection over a 50-day time course [93]. In contrast, asp1Δ was phenotypically identical to WT, and just as virulent as WT in mice, suggesting that PP2-IP4 plays a minor role in cryptococcal homeostasis and virulence [92]. In other fungal species, including Schizosaccharomyces pombe, Aspergillus nidulans and Ustilago maydis, Vip1/Asp1 plays a role in polarized growth and the dynamics of the microtubular cytoskeleton [98]. Possible reasons for the varying importance of PP2-IP4 among the different fungal species remain to be elucidated.
Given that asp1Δ (1,5-PP2-IP4-deficient) is as virulent as WT C. neoformans [92], the common phenotypic defects of the plc1Δ, arg1Δ, ipk1Δ and kcs1Δ mutants are likely to be caused by the absence of 5-PP-IP5. We therefore postulated that 5-PP-IP5 is the crucial metabolite responsible for numerous cellular functions in C. neoformans [92]. Interestingly, the ipk1Δ mutant was the least affected by the absence of 5-PP-IP5, exhibiting a more robust phenotype than other 5-PP-IP5-deficient strains [93]. We rationalized that the accumulation of Kcs1-derived 5-PP-IP4 in ipk1Δ contributed to the fitness of this mutant by fulfilling some of the functions of its pyrophosphorylated cousin, 5-PP-IP5 [93].
7. 5-PP-IP5 Plays a Critical Role in Cryptococcal Virulence
A hallmark phenotype of the kcs1Δ mutant is its mucoid appearance and large capsules after being cultured on Sabouraud agar [92]. However, this hyper-encapsulation phenotype was not apparent during the infection of the mouse lung [92]. Similar to plc1Δ, kcs1Δ was avirulent in a mouse inhalation model [92]. However, the kcs1Δ infection differed from that of plc1Δ. As opposed to plc1Δ, which was cleared from the mouse lung 14 days post-infection [92], kcs1Δ established a residual lung infection over a 50 day period that failed to disseminate to the central nervous system [92]. The reduced proliferation of kcs1Δ in the lung tissue may be attributed to its inability to utilize non-glucose carbon sources [92]. Given that the lung is a low glucose environment, this phenotype is likely to have a negative impact on cellular fitness and subsequently on virulence. These metabolic differences suggest that WT, but not kcs1Δ, actively expresses enzymes involved in the utilization of carbon sources other than glucose, (e.g., lactate and fatty acids), which require mitochondrial function. To investigate this further, we performed a high throughput gene expression analysis and showed that our data was supportive of metabolic dysfunction in the absence of PP-IP5. Genes encoding proteins involved in glycolysis were more highly expressed in kcs1Δ than in WT, while the expression of genes encoding enzymes involved in the utilization of alternative carbon sources (citric acid and glyoxylate cycles, gluconeogenesis, and fatty acid β-oxidation) was reduced in kcs1Δ, suggesting that mitochondrial function is suppressed in kcs1Δ [92].
To further understand the pathology of kcs1Δ infection, we compared the immune response in the mouse lung during infection using cytokine profiling [92]. The results showed that kcs1Δ elicited a much weaker cytokine response: lower interferon-gamma (IFN-γ), tumor necrosis factor (TNF), monocyte chemoattractant protein-1 (MCP-1), IL-6 and IL-4, and delayed production of IL-2 and IL-17A, compared to WT [92]. It is known that mannoproteins present in the cryptococcal polysaccharide capsule and cell wall are highly immunogenic [104,105,106,107]. We observed reduced recognition of kcs1Δ by monocytes in vitro, which correlated with diminished mannoprotein exposure at the kcs1Δ surface, as determined by concanavalin A binding [92]. Furthermore, transcription of mannoprotein-encoding genes was reduced in kcs1Δ, as indicated by high throughput gene expression analysis [92]. Taken together, our data suggested that the persistence of a low-grade, asymptomatic kcs1Δ mutant infection is due, in part, to reduced monocyte recruitment to the sites of kcs1Δ infection, and the reduced uptake of kcs1Δ by both lung resident macrophages and monocytes infiltrating from the vasculature [92].
8. The Plc1/IPK Pathway: A Signaling or a Metabolic Pathway?
The Plc1/IPK pathway has the features of both a metabolic and a signaling pathway. On the one hand the Plc1/IPK pathway is an anabolic pathway where sequentially acting kinases use the energy of ATP to synthesize IP and PP-IP of increasing complexity. However, some of the IP products of the pathway have roles in signaling.
8.1. Features of a Metabolic Pathway
In C. neoformans and S. cerevisiae, the Plc1/IPK pathway is constitutively active, maintaining stable levels of each IP species, with IP6 being the most abundant (Figure 2A, Table 1). Furthermore, the role of this pathway in C. neoformans is not limited to the regulation of virulence determinants in response to host-derived stimuli, but includes fungal fitness, as evidenced by the delayed growth of plc1Δ and kcs1Δ under optimal conditions, as well as under conditions of stress [75,92]. In yeast and mammalian cells, biosynthesis of PP-IP5 by Kcs1 is tightly linked to ATP availability [94,108]. Due to the rapid hydrolysis of PP-IP5 by intracellular phosphatases [88], its intracellular concentration is not maintained at the same level following ATP depletion, but drops rapidly. During phosphate deprivation in S. cerevisiae, PP-IP5 levels are decreased in correlation with the reduction in ATP [109,110]. Thus, PP-IP5 appears to serve as an indicator of intracellular energy status, rather than as a classical secondary messenger.
8.2. Features of a Signaling Pathway
A signaling pathway is defined as one which is activated by an extracellular stimulus. The signal is then propagated intracellularly via secondary messengers, which fluctuate in response to a stimulus. The secondary messengers then engage signaling components downstream to elicit physiologically relevant responses. IP/PP-IP can act as secondary messengers. Stimulus-induced changes in IP/PP-IP levels in mammalian and fungal cells have been demonstrated in several instances. Perhaps the best studied example is Plc1-mediated IP3 release in mammalian cells following ligand stimulation, leading to an influx of calcium from the ER and the activation of calcineurin [83,84,85,86]. In the filamentous fungus, Neurospora crassa membrane stretch at the hyphal tip due to growth is thought to activate PLC, triggering IP3 production. IP3 induces calcium release from vesicles localized at the hyphal tip allowing the establishment of a calcium gradient, which is essential for tip expansion [87]. IP3 also triggers calcium release from vacuoles in S. cerevisiae [111], N. crassa [87,112] and C. albicans [113].
In mammalian cells I(3,4,5,6)P4 inhibits Ca2+-activated chloride channels in the plasma membrane. These ion channels are required for salt and fluid secretion from epithelial cells, insulin secretion from pancreatic β-cells, smooth muscle contraction and neurotransmission [114,115,116,117]. The intracellular concentration of I(3,4,5,6)P4 increases during sustained stimulation by phospholipase C agonists [118]. In mammalian cells, I(1,3,4)P3 derived from PLC via I(1,4,5)P3 stimulates the production of I(3,4,5,6)P4 by inositol 1,3,4-triphosphate 5/6 kinase ITPK1 (Figure 1) [119,120]. Chamberlain et al. hypothesized that the function of primordial ITPK1 was to promote the biosynthesis of highly phosphorylated IP species. However, in mammalian cells this function has evolved to accommodate a signaling role for I(3,4,5,6)P4 [120].
PP-IP levels also fluctuate in response to stress: in mammalian cells, hyperosmotic (0.2 M sorbitol), heat (42 °C) and cold (33 °C) stresses triggered an increased production of PP2-IP4 [121,122]. In contrast, neither hyperosmotic nor heat stress caused significant fluctuations in IP/PP-IP levels in S. cerevisiae [121]. However, in S. pombe the IP6 level tripled within minutes of exposure to high salt concentration (0.7 M KCl) [123]. In agreement with the role of IP/PP-IP in stress tolerance, Worley et al. demonstrated that activation of the stress response (by heat and high salt) in S. cerevisiae requires Kcs1 and Vip1-derived PP-IP. These molecules act in parallel with the TORC1 pathway to control the activity of the class I histone deacetylase Rpd3L [124].
Taken together, the data above demonstrates that specific environmental stimuli have an impact on intracellular IP/PP-IP concentration in several experimental models. However, the relative stability of the IP profile in fungal and mammalian cells suggests that the biosynthesis of highly phosphorylated IP is a constitutive process, functioning to maintain cellular function even in the absence of specific extracellular stimuli. In fungal pathogens, including C. neoformans, the dynamic changes in individual IP/PP-IP species that occur in response to various stress conditions require investigation. However, such investigation is hindered by the technical difficulty encountered in separating and quantifying these molecules, and also by the lack of commercially available IP standards.
9. How IP/PP-IP Regulate Cellular Function
IP species, and PP-IP5 in particular, regulate numerous and diverse cellular processes including endocytosis, vesicular trafficking, vacuole formation, autophagy, maintenance of telomere length, apoptosis, cytoskeletal organization, DNA repair and neutrophil-dependent antimicrobial defense (reviewed in [71,89,90,125]). So how do IP achieve this? Do they have specific individual effects on each function or do they function upstream of a pathway, which itself regulates numerous functions? Evidence obtained from yeast and mammalian systems supports both hypotheses, with IP/PP-IP serving as effector molecules to exert allosteric protein regulation (IP and PP-IP), or as phosphate donors to pyrophosphorylate proteins (PP-IP).
In a more recent discovery, PP-IP were shown to allosterically regulate yeast, plant and mammalian proteins containing an SPX domain [126]. SPX domains (135–380 residues) are found in proteins involved in the regulation of phosphate homeostasis, which, in S. cerevisiae, include low-affinity phosphate transporters, components of the vacuolar polyphosphate polymerase complex and the cyclin-dependent kinase inhibitor, Pho81 (reviewed in [127]). In S. cerevisiae, Kcs1-derived PP-IP5 directly stimulates the synthesis of inorganic polyphosphate chains in vacuoles by binding to the SPX-domain of the polyphosphate polymerase complex [126]. The SPX domain of the cyclin-dependent kinase inhibitor, Pho81, is likely to mediate inhibition of CDK Pho85 under phosphate starvation conditions, leading to the activation of the PHO pathway [128]. I(1,4,5,6)P4 is also an allosteric regulator of histone deacetylase class I complexes in mammalian cells [129,130].
As an alternative to allosteric binding, PP-IP were shown to pyrophosphorylate proteins by virtue of their “high energy” pyrophosphate group: the free energy of hydrolysis of the pyrophosphate bond in PP-IP5 is 6.6 Kcal/mol, which is higher than that of ADP [131], while for PP2-IP4 it is estimated to be higher than that of ATP (7.3 Kcal/mol), due to the alleviation of electrostatic and steric constraints [132,133]. Phosphate transfer by PP-IP5 is non-enzymatic, but magnesium-dependent, and requires the target protein to be pre-phosphorylated on serine. Proteins encoding stretches of serines flanked by acidic amino acids or regions containing multiple lysines are good targets for PP-IP5-mediated pyrophosphorylation [133]. It has been shown that casein kinase 2 (CK2) efficiently primes proteins for pyrophosphorylation by PP-IP5 in vitro [134]. In S. cerevisiae, PP-IP5 was shown to suppress the expression of glycolytic genes via pyrophosphorylation of the transcription factor Gcr1 [135]. Similar to other post-translational modifications, PP-IP-mediated pyrophosphorylation represents a unique mode of intracellular communication. It should be kept in mind though that the generation of pyrophosphorylated proteins by PP-IP5 is yet to be observed in vivo. Further exploration of this phenomenon will allow us to distinguish which of the pleiotropic effects of PP-IP5 are conveyed via protein pyrophosphorylation versus allosteric binding.
10. The Plc1/IPK Pathway as a Target for Antifungal Drug Development
Given the significant impact that the loss of PP-IP5 has on cryptococcal virulence in animal models, the Plc1/IPK pathway represents an attractive avenue for antifungal drug development. From a clinical perspective, targeting enzymes upstream of PP-IP5, rather than the PP-IP5 itself, is the only suitable option. While IP and PP-IP have critical roles in regulating diverse cellular processes in the pathogen itself, the same metabolites are produced in the host and play similar essential roles. Targeting fungal-derived IP/PP-IP could therefore have detrimental side effects. Although IP/PP-IP are ubiquitous secondary metabolites in all eukaryotes, the primordial Plc1/IPK pathway, responsible for their production in fungi, has evolved into a more complex one in mammalian cells over millions of years. The absence of redundancy in the fungal pathway, the low homology shared by fungal and mammalian IPK enzymes and the discovery of naturally-occurring inhibitors of these kinases further support their suitability for future drug development. In addition, the cryptococcal mutants, plc1Δ, arg1Δ, ipk1Δ and kcs1Δ, are all hypersusceptible to antifungal agents, suggesting that inhibitors against each of the respective fungal enzymes could act synergistically with marketed antifungal drugs against wild-type pathogens to achieve a more favorable treatment outcome.
Compared to the cryptococcal IP biosynthesis pathway, the mammalian pathway is more complex and includes multiple enzymes with similar catalytic activity. For example, while Arg1 in C. neoformans is the only enzyme able to convert IP3 to IP4, three IP3K isoforms (IP3K-A, IP3K-B and IP3K-C) and the inositol polyphosphate multikinase (IPMK) catalyze this reaction in humans (reviewed in [89,91]) (Figure 1). Similarly, mammals express three isoforms of IP6K, with each having a specialized physiological function (reviewed in [90]).
The human repertoire of IPKs also includes an enzyme, which is structurally and functionally unique to mammalian cells: hITPK1 (inositol 1,3,4-triphosphate 5/6 kinase) mediates the transfer of phosphate between different IP molecules (“intersubstrate” transfer). This mechanism is instrumental in the PLC-dependent increase in I(3,4,5,6)P4 levels: PLC-generated I(1,4,5)P3 is converted to I(1,3,4)P3, which stimulates I(1,3,4,5,6)P5 dephosphorylation by ITPK1 to produce biologically active I(3,4,5,6)P4 (Figure 1) [119,120,136]. Although ITPK1 homologs are present in soybean and Entamoeba histolytica, this mechanism is only functional in mammalian cells. A study by Chamberlain et al. pinpoints structural differences between human and E. histolytica enzymes, potentially responsible for the unique features of hITPK1 [120,137]. Human ITPK1 has no homologs in C. neoformans, C. albicans or A. fumigatus.
In contrast to mammalian cells, the cryptococcal IP biosynthesis pathway is non-redundant and all three sequentially acting enzymes, Arg1, Ipk1 and Kcs1, are required for the production of PP-IP5. The presence of IPK enzymes in other medically important pathogens, including Candida spp. and Aspergillus spp., supports their exploitation as panfungal drug targets.
11. Structural Studies of IPKs
The three dimensional structures of several IPK enzymes, including Arg82 from S. cerevisiae (Ipk2) [138], the hybrid IP6K/IP3K from E. histolytica [139], IPMKα from Arabidopsis thaliana [140], rat and human IP3K [141,142], and ITPK from E. histolytica and human [120,137] have been solved. Structural comparison and substrate modelling were also used to establish the basis for IPK substrate specificity. IP3K, IPMK and IP6K enzymes share a conserved amino acid motif P-x-x-x-D-x-K-x-G in their inositol binding region (Pfam family PF03770). They are predicted to assume the same overall fold despite their low sequence conservation [138]. The sequence variation allows these enzymes to discriminate between different IP species through a combination of steric exclusion and the requirement for the occupation of specific phosphate binding pockets. Some IPK enzymes contain additional domains or insertions, which have a physiological role. For example, a poly-D loop insertion in yeast Ipk2 was shown to facilitate Ipk2 interaction with the transcription factors, ArgRI and Mcm1 [143]. Thus, yeast Ipk2 (alias ArgRIII/Arg82) performs a unique second function, distinct from IP generation, which is to act as a stabilizer of a transcriptional regulatory complex involved in arginine metabolism [144]. Arg1 in C. neoformans contains a similar polyD/E loop insertion. However, this region is not conserved in the mammalian IPMK enzymes, suggesting that its function is restricted to yeast IPK enzymes.
Additional evidence of drug-exploitable differences in IPK active sites comes from a study performed by Wang et al. [145]. This group found that, in addition to the IP catalytic pocket, the surface of the kinase domain of mammalian PPIP5K (Vip1) contains a second unique substrate binding site with greater flexibility for substrate accommodation. This second site functions to deliver substrate to the catalytic site in a two-step binding process, which is the first of its kind to be described in small molecule kinases.
Differences in the structure of the inositol binding domain in human IP3K and S. cerevisiae Ipk2 were also identified. While the overall conformation is comparable in both enzymes, the inositol-binding domain is smaller in Ipk2 and contains only two of the five α-helices present in IP3K, suggestive of substrate accommodation restrictions in Ipk2 [138]. Taken together, these differential properties of IPK enzymes will potentially allow the development of inhibitors customized specifically for the fungal enzymes.
12. Advances in Identifying IPK Inhibitor Specificity
Pharmacological approaches taken towards understanding the mechanisms of action of IPK enzymes have led to the discovery of several IPK inhibitors that could serve as lead compounds for future drug development. Purine-based IP3K inhibitors were identified as a means to understand how mammalian IP3K regulates intracellular calcium metabolism [146]. Purine-based inhibitors were favored over inositol polyphosphate-based inhibitor analogues because the latter are highly charged and, therefore, unable to be delivered into cells without a carrier. In contrast, the purine-based inhibitors reported by Chang et al. are less negatively charged and thus can more easily penetrate cellular membranes, a property which is essential if these inhibitors are to be used for clinical purposes.
Padmanabhan et al. demonstrated that a purine analogue N2-(m-(trifluoromethyl)benzyl) N6-(p-nitrobenzyl) purine (TNP), selectively inhibits both human IP3K and IP6K enzymes by competing with ATP binding [147]. In vitro, the selectivity of TNP for IP6K was significantly higher than for IP3K (IC50 18 vs. 0.47 µM). This difference is expected to be even more pronounced in vivo due to the relatively low affinity of IP6K for binding ATP. TNP has been used successfully to mimic IP6K (KCS1) deletion in S. cerevisiae: the addition of TNP to wild-type cells caused fragmentation of vacuoles, a typical feature of the kcs1Δ mutant [147,148].
Natural and synthetic plant polyphenolics have also been shown to inhibit all three IP3K isoforms, as well as IPMK in mammalian cells [149], but to varying degrees: the synthetic polyphenol, aurintricarboxylic acid (ATA), was the best inhibitor of all enzymes, while naturally occurring chlorogenic acid (a bioactive ingredient found in coffee) was specific to IPMK [149]. All inhibitors displayed non-competitive inhibition with respect to IP3-binding and a mixed-type inhibition with respect to ATP-binding. Mutagenesis studies showed that both the calmodulin binding and the IP3-binding domains in IP3K interact with the inhibitor. The absence of these domains in IPMK and the presence of a unique insertion in IPMK were found to be important for the selectivity differences observed for IP3K inhibition.
ATA and chlorogenic acid have been reported to have antiproliferative activity [150,151,152]. In addition, derivatives of chlorogenic acid have been described as having antifungal activity against C. neoformans and C. albicans [153]. Examples of other polyphenolic compounds which inhibit IPKs [149] and also have antifungal activity are provided in Table 3. These promising results suggest that polyphenolics, such as chlorogenic acid, have multipurpose functions and could be used in synergy with drugs to treat cancer and/or fungal infections. In summary, these studies provide proof-of-concept that selective inhibitors of fungal IPKs homologues either occur in nature or can be developed.

Table 3.
Examples of natural polyphenolic compounds that inhibit IPKs and also have antifungal activity. MIC: minimum inhibitory concentration; ED50: median effective dose.
13. Conclusions
In summary we have characterized the Plc1/IPK pathway for the first time in a fungal pathogen of great significance to human health, and have demonstrated the important contribution of the pyrophosphate product, PP-IP5, to fungal fitness and pathogenicity in animal infection models. As the technology required to detect and synthesize IP evolves, it will soon be possible to fully elucidate the mechanism of action of PP-IP5 in fungi. The Plc1/IPK pathway in fungi has evolved into a more complex pathway in multi-cellular organisms, providing opportunities for drug development. These drugs could act alone to inhibit IPK enzymes, or synergistically with currently marketed antifungals to reduce side effects and provide more favorable treatment outcomes. By ignoring minimalist primordial pathways such as the Plc1/IPK pathway, and focusing predominantly on the unique aspects of fungi, we could be missing vital opportunities to expand our much needed antifungal armament to combat the predicted rise of IFIs in the future.
Acknowledgments
This work was supported by a National Health and Medical Research Council of Australia project grant (APP1058779) to JD/AS/TC/SL.
Author contributions
All authors co-wrote, proof-read and approved the manuscript for publication.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Brown, G.D.; Denning, D.W.; Gow, N.A.; Levitz, S.M.; Netea, M.G.; White, T.C. Hidden killers: Human fungal infections. Sci. Transl. Med. 2012, 4, 113–165. [Google Scholar] [CrossRef] [PubMed]
- Vallabhaneni, S.; Mody, R.K.; Walker, T.; Chiller, T. The global burden of fungal diseases. Infect. Dis. Clin. N. Am. 2016, 30, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Low, C.Y.; Rotstein, C. Emerging fungal infections in immunocompromised patients. F1000 Med. Rep. 2011, 3, 14. [Google Scholar] [CrossRef] [PubMed]
- Miceli, M.H.; Diaz, J.A.; Lee, S.A. Emerging opportunistic yeast infections. Lancet Infect. Dis. 2011, 11, 142–151. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Diekema, D.J. Rare and emerging opportunistic fungal pathogens: Concern for resistance beyond Candida albicans and Aspergillus fumigatus. J. Clin. Microbiol. 2004, 42, 4419–4431. [Google Scholar] [CrossRef] [PubMed]
- Armstrong-James, D.; Meintjes, G.; Brown, G.D. A neglected epidemic: Fungal infections in HIV/AIDS. Trends Microbiol. 2014, 22, 120–127. [Google Scholar] [CrossRef] [PubMed]
- UNAIDS. Global AIDS Update. Available online: http://www.unaids.org/en/resources/documents/2016/Global-AIDS-update-2016. (Accessed on 1 July 2016).
- CDC. Opportunistic Infections. Available online: http://www.cdc.gov/hiv/basics/livingwithhiv/opportunisticinfections.html (accessed on 10 June 2016).
- Menzin, J.; Meyers, J.L.; Friedman, M.; Korn, J.R.; Perfect, J.R.; Langston, A.A.; Danna, R.P.; Papadopoulos, G. The economic costs to United States hospitals of invasive fungal infections in transplant patients. Am. J. Infect. Control 2011, 39, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Abruzzo, G.K.; Flattery, A.M.; Gill, C.J.; Kong, L.; Smith, J.G.; Pikounis, V.B.; Balkovec, J.M.; Bouffard, A.F.; Dropinski, J.F.; Rosen, H.; et al. Evaluation of the echinocandin antifungal MK-0991 (L-743,872): Efficacies in mouse models of disseminated aspergillosis, candidiasis, and cryptococcosis. Antimicrob. Agents Chemother. 1997, 41, 2333–2338. [Google Scholar] [PubMed]
- Bartizal, K.; Gill, C.J.; Abruzzo, G.K.; Flattery, A.M.; Kong, L.; Scott, P.M.; Smith, J.G.; Leighton, C.E.; Bouffard, A.; Dropinski, J.F.; et al. In vitro preclinical evaluation studies with the echinocandin antifungal MK-0991 (L-743,872). Antimicrob. Agents Chemother. 1997, 41, 2326–2332. [Google Scholar] [PubMed]
- Kartsonis, N.A.; Nielsen, J.; Douglas, C.M. Caspofungin: The first in a new class of antifungal agents. Drug Resist. Updates 2003, 6, 197–218. [Google Scholar] [CrossRef]
- Krishnarao, T.V.; Galgiani, J.N. Comparison of the in vitro activities of the echinocandin LY303366, the pneumocandin MK-0991, and fluconazole against Candida species and Cryptococcus neoformans. Antimicrob. Agents Chemother. 1997, 41, 1957–1960. [Google Scholar] [PubMed]
- Howard, S.J.; Cerar, D.; Anderson, M.J.; Albarrag, A.; Fisher, M.C.; Pasqualotto, A.C.; Laverdiere, M.; Arendrup, M.C.; Perlin, D.S.; Denning, D.W. Frequency and evolution of Azole resistance in Aspergillus fumigatus associated with treatment failure. Emerg. Infect. Dis. 2009, 15, 1068–1076. [Google Scholar] [CrossRef] [PubMed]
- Howard, S.J.; Webster, I.; Moore, C.B.; Gardiner, R.E.; Park, S.; Perlin, D.S.; Denning, D.W. Multi-azole resistance in Aspergillus fumigatus. Int. J. Antimicrob. Agents 2006, 28, 450–453. [Google Scholar] [CrossRef] [PubMed]
- Chowdhary, A.; Kathuria, S.; Randhawa, H.S.; Gaur, S.N.; Klaassen, C.H.; Meis, J.F. Isolation of multiple-triazole-resistant Aspergillus fumigatus strains carrying the TR/L98H mutations in the cyp51A gene in India. J. Antimicrob. Chemother. 2012, 67, 362–366. [Google Scholar] [CrossRef] [PubMed]
- Bueid, A.; Howard, S.J.; Moore, C.B.; Richardson, M.D.; Harrison, E.; Bowyer, P.; Denning, D.W. Azole antifungal resistance in Aspergillus fumigatus: 2008 and 2009. J. Antimicrob. Chemother. 2010, 65, 2116–2118. [Google Scholar] [CrossRef] [PubMed]
- Alexander, B.D.; Johnson, M.D.; Pfeiffer, C.D.; Jimenez-Ortigosa, C.; Catania, J.; Booker, R.; Castanheira, M.; Messer, S.A.; Perlin, D.S.; Pfaller, M.A. Increasing echinocandin resistance in Candida glabrata: Clinical failure correlates with presence of FKS mutations and elevated minimum inhibitory concentrations. Clin. Infect. Dis. 2013, 56, 1724–1732. [Google Scholar] [CrossRef] [PubMed]
- Cleveland, A.A.; Farley, M.M.; Harrison, L.H.; Stein, B.; Hollick, R.; Lockhart, S.R.; Magill, S.S.; Derado, G.; Park, B.J.; Chiller, T.M. Changes in incidence and antifungal drug resistance in candidemia: Results from population-based laboratory surveillance in Atlanta and Baltimore, 2008–2011. Clin. Infect. Dis. 2012, 55, 1352–1361. [Google Scholar] [CrossRef] [PubMed]
- Pfaller, M.A.; Rhomberg, P.R.; Messer, S.A.; Jones, R.N.; Castanheira, M. Isavuconazole, micafungin, and 8 comparator antifungal agents’ susceptibility profiles for common and uncommon opportunistic fungi collected in 2013: Temporal analysis of antifungal drug resistance using CLSI species-specific clinical breakpoints and proposed epidemiological cutoff values. Diagn. Microbiol. Infect. Dis. 2015, 82, 303–313. [Google Scholar] [PubMed]
- WHO. Antimicrobial Resistance: Global Report on Surveillance; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- WHO. Rapid Advice: Diagnosis, Prevention and Management of Cryptococcal Disease in HIV-Infected Adults, Adolescents and Children; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Perfect, J.R.; Dismukes, W.E.; Dromer, F.; Goldman, D.L.; Graybill, J.R.; Hamill, R.J.; Harrison, T.S.; Larsen, R.A.; Lortholary, O.; Nguyen, M.H.; et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of America. Clin. Infect. Dis. 2010, 50, 291–322. [Google Scholar] [CrossRef] [PubMed]
- Day, J.N.; Chau, T.T.; Wolbers, M.; Mai, P.P.; Dung, N.T.; Mai, N.H.; Phu, N.H.; Nghia, H.D.; Phong, N.D.; Thai, C.Q.; et al. Combination antifungal therapy for cryptococcal meningitis. N. Engl. J. Med. 2013, 368, 1291–1302. [Google Scholar] [CrossRef] [PubMed]
- Loyse, A.; Dromer, F.; Day, J.; Lortholary, O.; Harrison, T.S. Flucytosine and cryptococcosis: Time to urgently address the worldwide accessibility of a 50-year-old antifungal. J. Antimicrob. Chemother. 2013, 68, 2435–2444. [Google Scholar] [CrossRef] [PubMed]
- Govender, N.P.; Meintjes, G.; Banoo, S. Access to flucytosine for HIV-infected patients with cryptococcal meningitis—An urgent need. S. Afr. Med. J. 2014, 104, 594–595. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sloan, D.; Dlamini, S.; Paul, N.; Dedicoat, M. Treatment of acute cryptococcal meningitis in HIV infected adults, with an emphasis on resource-limited settings. Cochrane Database Syst. Rev. 2008. [Google Scholar] [CrossRef]
- Powderly, W.G. Therapy for cryptococcal meningitis in patients with AIDS. Clin. Infect. Dis. 1992, 14, 54–59. [Google Scholar] [CrossRef]
- Momoff, N.; Parrish, A. Fluconazole-resistant cryptococcal meningitis. S. Afr. Med. J. 2003, 93, 444. [Google Scholar] [PubMed]
- Smith, K.D.; Achan, B.; Hullsiek, K.H.; McDonald, T.R.; Okagaki, L.H.; Alhadab, A.A.; Akampurira, A.; Rhein, J.R.; Meya, D.B.; Boulware, D.R.; et al. Increased antifungal drug resistance in clinical isolates of Cryptococcus neoformans in Uganda. Antimicrob. Agents Chemother. 2015, 59, 7197–7204. [Google Scholar] [CrossRef] [PubMed]
- Bii, C.C.; Makimura, K.; Abe, S.; Taguchi, H.; Mugasia, O.M.; Revathi, G.; Wamae, N.C.; Kamiya, S. Antifungal drug susceptibility of Cryptococcus neoformans from clinical sources in Nairobi, Kenya. Mycoses 2007, 50, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Pfaller, M.A.; Diekema, D.J.; Gibbs, D.L.; Newell, V.A.; Bijie, H.; Dzierzanowska, D.; Klimko, N.N.; Letscher-Bru, V.; Lisalova, M.; Muehlethaler, K.; et al. Results from the ARTEMIS DISK Global Antifungal Surveillance Study, 1997 to 2007: 10.5-year analysis of susceptibilities of noncandidal yeast species to fluconazole and voriconazole determined by CLSI standardized disk diffusion testing. J. Clin. Microbiol. 2009, 47, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Sar, B.; Monchy, D.; Vann, M.; Keo, C.; Sarthou, J.L.; Buisson, Y. Increasing in vitro resistance to fluconazole in Cryptococcus neoformans Cambodian isolates: April 2000 to March 2002. J. Antimicrob. Chemother. 2004, 54, 563–565. [Google Scholar] [CrossRef] [PubMed]
- Park, B.J.; Wannemuehler, K.A.; Marston, B.J.; Govender, N.; Pappas, P.G.; Chiller, T.M. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS 2009, 23, 525–530. [Google Scholar] [CrossRef] [PubMed]
- Lightowler, J.V.; Cooke, G.S.; Mutevedzi, P.; Lessells, R.J.; Newell, M.L.; Dedicoat, M. Treatment of cryptococcal meningitis in KwaZulu-Natal, South Africa. PLoS ONE 2010, 5, e8630. [Google Scholar] [CrossRef] [PubMed]
- Lomes, N.R.; Melhem, M.S.; Szeszs, M.W.; Martins, M.D.; Buccheri, R. Cryptococcosis in non-HIV/non-transplant patients: A Brazilian case series. Med. Mycol. 2016, 54, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Kambugu, A.; Meya, D.B.; Rhein, J.; O‘Brien, M.; Janoff, E.N.; Ronald, A.R.; Kamya, M.R.; Mayanja-Kizza, H.; Sande, M.A.; Bohjanen, P.R.; et al. Outcomes of cryptococcal meningitis in Uganda before and after the availability of highly active antiretroviral therapy. Clin. Infect. Dis. 2008, 46, 1694–1701. [Google Scholar] [CrossRef] [PubMed]
- Brizendine, K.D.; Baddley, J.W.; Pappas, P.G. Predictors of mortality and differences in clinical features among patients with Cryptococcosis according to immune status. PLoS ONE 2013, 8, e60431. [Google Scholar] [CrossRef] [PubMed]
- Bruatto, M.; Vidotto, V.; Maina, A.M. Growth of Cryptococcus neoformans in a thiamine-free medium. Mycopathologia 1992, 119, 129–132. [Google Scholar] [CrossRef] [PubMed]
- Vidotto, V.; Aoki, S.; Campanini, G. A vitamin-free minimal synthetic medium for Cryptococcus neoformans. Mycopathologia 1996, 133, 139–142. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Hull, C.M.; Heitman, J. Sexual reproduction between partners of the same mating type in Cryptococcus neoformans. Nature 2005, 434, 1017–1021. [Google Scholar] [CrossRef] [PubMed]
- Wickes, B.L.; Mayorga, M.E.; Edman, U.; Edman, J.C. Dimorphism and haploid fruiting in Cryptococcus neoformans: Association with the alpha-mating type. Proc. Natl. Acad. Sci. USA 1996, 93, 7327–7331. [Google Scholar] [CrossRef] [PubMed]
- Toffaletti, D.L.; Rude, T.H.; Johnston, S.A.; Durack, D.T.; Perfect, J.R. Gene transfer in Cryptococcus neoformans by use of biolistic delivery of DNA. J. Bacteriol. 1993, 175, 1405–1411. [Google Scholar] [PubMed]
- Hull, C.M.; Heitman, J. Genetics of Cryptococcus neoformans. Annu. Rev. Genet. 2002, 36, 557–615. [Google Scholar] [CrossRef] [PubMed]
- Tenor, J.L.; Oehlers, S.H.; Yang, J.L.; Tobin, D.M.; Perfect, J.R. Live Imaging of Host-Parasite Interactions in a zebrafish infection model reveals cryptococcal determinants of virulence and central nervous system invasion. mBio 2015, 6, e01425–e01415. [Google Scholar] [CrossRef] [PubMed]
- Perfect, J.R.; Lang, S.D.; Durack, D.T. Chronic cryptococcal meningitis: A new experimental model in rabbits. Am. J. Pathol. 1980, 101, 177–194. [Google Scholar] [PubMed]
- Mylonakis, E.; Ausubel, F.M.; Perfect, J.R.; Heitman, J.; Calderwood, S.B. Killing of Caenorhabditis elegans by Cryptococcus neoformans as a model of yeast pathogenesis. Proc. Natl. Acad. Sci. USA 2002, 99, 15675–15680. [Google Scholar] [CrossRef] [PubMed]
- Mylonakis, E.; Moreno, R.; El Khoury, J.B.; Idnurm, A.; Heitman, J.; Calderwood, S.B.; Ausubel, F.M.; Diener, A. Galleria mellonella as a model system to study Cryptococcus neoformans pathogenesis. Infect. Immun. 2005, 73, 3842–3850. [Google Scholar] [CrossRef] [PubMed]
- Wiederhold, N.P.; Najvar, L.K.; Bocanegra, R.; Kirkpatrick, W.R.; Sorrell, T.C.; Patterson, T.F. Limited activity of miltefosine in murine models of cryptococcal meningoencephalitis and disseminated cryptococcosis. Antimicrob. Agents Chemother. 2013, 57, 745–750. [Google Scholar] [CrossRef] [PubMed]
- Carroll, S.F.; Guillot, L.; Qureshi, S.T. Mammalian model hosts of cryptococcal infection. Comp. Med. 2007, 57, 9–17. [Google Scholar] [PubMed]
- Sabiiti, W.; May, R.C.; Pursall, E.R. Experimental models of cryptococcosis. Int. J. Microbiol. 2012, 2012, 626745. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.C.; Kwon-Chung, K.J. Complementation of a capsule-deficient mutation of Cryptococcus neoformans restores its virulence. Mol. Cell. Biol. 1994, 14, 4912–4919. [Google Scholar] [CrossRef] [PubMed]
- Nosanchuk, J.D.; Valadon, P.; Feldmesser, M.; Casadevall, A. Melanization of Cryptococcus neoformans in murine infection. Mol. Cell. Biol. 1999, 19, 745–750. [Google Scholar] [CrossRef] [PubMed]
- Salas, S.D.; Bennett, J.E.; Kwon-Chung, K.J.; Perfect, J.R.; Williamson, P.R. Effect of the laccase gene CNLAC1, on virulence of Cryptococcus neoformans. J. Exp. Med. 1996, 184, 377–386. [Google Scholar] [CrossRef] [PubMed]
- Alspaugh, J.A.; Cavallo, L.M.; Perfect, J.R.; Heitman, J. RAS1 regulates filamentation, mating and growth at high temperature of Cryptococcus neoformans. Mol. Microbiol. 2000, 36, 352–365. [Google Scholar] [CrossRef] [PubMed]
- Chayakulkeeree, M.; Johnston, S.A.; Oei, J.B.; Lev, S.; Williamson, P.R.; Wilson, C.F.; Zuo, X.; Leal, A.L.; Vainstein, M.H.; Meyer, W.; et al. SEC14 is a specific requirement for secretion of phospholipase B1 and pathogenicity of Cryptococcus neoformans. Mol. Microbiol. 2011, 80, 1088–1101. [Google Scholar] [CrossRef] [PubMed]
- Okagaki, L.H.; Strain, A.K.; Nielsen, J.N.; Charlier, C.; Baltes, N.J.; Chretien, F.; Heitman, J.; Dromer, F.; Nielsen, K. Cryptococcal cell morphology affects host cell interactions and pathogenicity. PLoS Pathog. 2010, 6, e1000953. [Google Scholar] [CrossRef]
- Crabtree, J.N.; Okagaki, L.H.; Wiesner, D.L.; Strain, A.K.; Nielsen, J.N.; Nielsen, K. Titan cell production enhances the virulence of Cryptococcus neoformans. Infect. Immun. 2012, 80, 3776–3785. [Google Scholar] [CrossRef] [PubMed]
- Olszewski, M.A.; Noverr, M.C.; Chen, G.H.; Toews, G.B.; Cox, G.M.; Perfect, J.R.; Huffnagle, G.B. Urease expression by Cryptococcus neoformans promotes microvascular sequestration, thereby enhancing central nervous system invasion. Am. J. Pathol. 2004, 164, 1761–1771. [Google Scholar] [CrossRef]
- Idnurm, A.; Reedy, J.L.; Nussbaum, J.C.; Heitman, J. Cryptococcus neoformans virulence gene discovery through insertional mutagenesis. Eukaryot. Cell 2004, 3, 420–429. [Google Scholar] [CrossRef] [PubMed]
- Liu, O.W.; Chun, C.D.; Chow, E.D.; Chen, C.; Madhani, H.D.; Noble, S.M. Systematic genetic analysis of virulence in the human fungal pathogen Cryptococcus neoformans. Cell 2008, 135, 174–188. [Google Scholar] [CrossRef] [PubMed]
- Jung, K.W.; Yang, D.H.; Maeng, S.; Lee, K.T.; So, Y.S.; Hong, J.; Choi, J.; Byun, H.J.; Kim, H.; Bang, S.; et al. Systematic functional profiling of transcription factor networks in Cryptococcus neoformans. Nat. Commun. 2015, 6, 6757. [Google Scholar] [CrossRef] [PubMed]
- Leidich, S.D.; Ibrahim, A.S.; Fu, Y.; Koul, A.; Jessup, C.; Vitullo, J.; Fonzi, W.; Mirbod, F.; Nakashima, S.; Nozawa, Y.; et al. Cloning and disruption of caPLB1, a phospholipase B gene involved in the pathogenicity of Candida albicans. J. Biol. Chem. 1998, 273, 26078–26086. [Google Scholar] [CrossRef] [PubMed]
- Theiss, S.; Ishdorj, G.; Brenot, A.; Kretschmar, M.; Lan, C.Y.; Nichterlein, T.; Hacker, J.; Nigam, S.; Agabian, N.; Kohler, G.A. Inactivation of the phospholipase B gene PLB5 in wild-type Candida albicans reduces cell-associated phospholipase A2 activity and attenuates virulence. Int. J. Med. Microbiol. 2006, 296, 405–420. [Google Scholar] [CrossRef] [PubMed]
- Mirbod-Donovan, F.; Schaller, R.; Hung, C.Y.; Xue, J.; Reichard, U.; Cole, G.T. Urease produced by Coccidioides posadasii contributes to the virulence of this respiratory pathogen. Infect. Immun. 2006, 74, 504–515. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gresnigt, M.S.; Bozza, S.; Becker, K.L.; Joosten, L.A.; Abdollahi-Roodsaz, S.; van der Berg, W.B.; Dinarello, C.A.; Netea, M.G.; Fontaine, T.; De Luca, A.; et al. A polysaccharide virulence factor from Aspergillus fumigatus elicits anti-inflammatory effects through induction of Interleukin-1 receptor antagonist. PLoS Pathog. 2014, 10, e1003936. [Google Scholar] [CrossRef] [PubMed]
- Jahn, B.; Koch, A.; Schmidt, A.; Wanner, G.; Gehringer, H.; Bhakdi, S.; Brakhage, A.A. Isolation and characterization of a pigmentless-conidium mutant of Aspergillus fumigatus with altered conidial surface and reduced virulence. Infect. Immun. 1997, 65, 5110–5117. [Google Scholar] [PubMed]
- Odom, A.; Muir, S.; Lim, E.; Toffaletti, D.L.; Perfect, J.; Heitman, J. Calcineurin is required for virulence of Cryptococcus neoformans. EMBO J. 1997, 16, 2576–2589. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, C.A.; Alspaugh, J.A.; Yue, C.; Harashima, T.; Cox, G.M.; Perfect, J.R.; Heitman, J. Cyclic AMP-dependent protein kinase controls virulence of the fungal pathogen Cryptococcus neoformans. Mol. Cell. Biol. 2001, 21, 3179–3191. [Google Scholar] [CrossRef] [PubMed]
- Bahn, Y.S.; Kojima, K.; Cox, G.M.; Heitman, J. Specialization of the HOG pathway and its impact on differentiation and virulence of Cryptococcus neoformans. Mol. Biol. Cell 2005, 16, 2285–2300. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, A.; Kim, S.; Snyder, S.H. Inositol pyrophosphates as mammalian cell signals. Sci. Signal. 2011, 4, re1. [Google Scholar] [CrossRef] [PubMed]
- O’Meara, T.R.; Norton, D.; Price, M.S.; Hay, C.; Clements, M.F.; Nichols, C.B.; Alspaugh, J.A. Interaction of Cryptococcus neoformans Rim101 and protein kinase A regulates capsule. PLoS Pathog. 2010, 6, e1000776. [Google Scholar] [CrossRef] [PubMed]
- Kozubowski, L.; Lee, S.C.; Heitman, J. Signalling pathways in the pathogenesis of Cryptococcus. Cell. Microbiol. 2009, 11, 370–380. [Google Scholar] [CrossRef] [PubMed]
- Gerik, K.J.; Bhimireddy, S.R.; Ryerse, J.S.; Specht, C.A.; Lodge, J.K. PKC1 is essential for protection against both oxidative and nitrosative stresses, cell integrity, and normal manifestation of virulence factors in the pathogenic fungus Cryptococcus neoformans. Eukaryot. Cell 2008, 7, 1685–1698. [Google Scholar] [CrossRef] [PubMed]
- Chayakulkeeree, M.; Sorrell, T.C.; Siafakas, A.R.; Wilson, C.F.; Pantarat, N.; Gerik, K.J.; Boadle, R.; Djordjevic, J.T. Role and mechanism of phosphatidylinositol-specific phospholipase C in survival and virulence of Cryptococcus neoformans. Mol. Microbiol. 2008, 69, 809–826. [Google Scholar] [PubMed]
- Flick, J.S.; Thorner, J. Genetic and biochemical characterization of a phosphatidylinositol-specific phospholipase C in Saccharomyces cerevisiae. Mol. Cell. Biol. 1993, 13, 5861–5876. [Google Scholar] [CrossRef] [PubMed]
- Yoko-o, T.; Matsui, Y.; Yagisawa, H.; Nojima, H.; Uno, I.; Toh-e, A. The putative phosphoinositide-specific phospholipase C gene, PLC1, of the yeast Saccharomyces cerevisiae is important for cell growth. Proc. Natl. Acad. Sci. USA 1993, 90, 1804–1808. [Google Scholar] [CrossRef] [PubMed]
- Payne, W.E.; Fitzgerald-Hayes, M. A mutation in PLC1, a candidate phosphoinositide-specific phospholipase C gene from Saccharomyces cerevisiae, causes aberrant mitotic chromosome segregation. Mol. Cell. Biol. 1993, 13, 4351–4364. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hofmann, S.L.; Majerus, P.W. Identification and properties of two distinct phosphatidylinositol-specific phospholipase C enzymes from sheep seminal vesicular glands. J. Biol. Chem. 1982, 257, 6461–6469. [Google Scholar] [PubMed]
- Lev, S.; Desmarini, D.; Li, C.; Chayakulkeeree, M.; Traven, A.; Sorrell, T.C.; Djordjevic, J.T. Phospholipase C of Cryptococcus neoformans regulates homeostasis and virulence by providing inositol trisphosphate as a substrate for Arg1 kinase. Infect. Immun. 2013, 81, 1245–1255. [Google Scholar] [CrossRef] [PubMed]
- Heung, L.J.; Luberto, C.; Plowden, A.; Hannun, Y.A.; Del Poeta, M. The sphingolipid pathway regulates Pkc1 through the formation of diacylglycerol in Cryptococcus neoformans. J. Biol. Chem. 2004, 279, 21144–21153. [Google Scholar] [CrossRef] [PubMed]
- Gerik, K.J.; Donlin, M.J.; Soto, C.E.; Banks, A.M.; Banks, I.R.; Maligie, M.A.; Selitrennikoff, C.P.; Lodge, J.K. Cell wall integrity is dependent on the PKC1 signal transduction pathway in Cryptococcus neoformans. Mol. Microbiol. 2005, 58, 393–408. [Google Scholar] [CrossRef] [PubMed]
- Putney, J.W., Jr. Formation and actions of calcium-mobilizing messenger, inositol 1,4,5-trisphosphate. Am. J. Physiol. 1987, 252, 149–157. [Google Scholar]
- Putney, J.W., Jr.; Aub, D.L.; Taylor, C.W.; Merritt, J.E. Formation and biological action of inositol 1,4,5-trisphosphate. Fed. Proc. 1986, 45, 2634–2638. [Google Scholar] [PubMed]
- Hogan, P.G.; Chen, L.; Nardone, J.; Rao, A. Transcriptional regulation by calcium, calcineurin, and NFAT. Genes Dev. 2003, 17, 2205–2232. [Google Scholar] [CrossRef] [PubMed]
- Jayaraman, T.; Marks, A.R. Calcineurin is downstream of the inositol 1,4,5-trisphosphate receptor in the apoptotic and cell growth pathways. J. Biol. Chem. 2000, 275, 6417–6420. [Google Scholar] [CrossRef] [PubMed]
- Silverman-Gavrila, L.B.; Lew, R.R. An IP3-activated Ca2+ channel regulates fungal tip growth. J. Cell Sci. 2002, 115, 5013–5025. [Google Scholar] [CrossRef] [PubMed]
- Menniti, F.S.; Miller, R.N.; Putney, J.W., Jr.; Shears, S.B. Turnover of inositol polyphosphate pyrophosphates in pancreatoma cells. J. Biol. Chem. 1993, 268, 3850–3856. [Google Scholar] [PubMed]
- Tsui, M.M.; York, J.D. Roles of inositol phosphates and inositol pyrophosphates in development, cell signaling and nuclear processes. Adv. Enzyme Regul. 2010, 50, 324–337. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M.S.; Livermore, T.M.; Saiardi, A. Inositol pyrophosphates: Between signalling and metabolism. Biochem. J. 2013, 452, 369–379. [Google Scholar] [CrossRef] [PubMed]
- Alcazar-Roman, A.R.; Wente, S.R. Inositol polyphosphates: A new frontier for regulating gene expression. Chromosoma 2008, 117, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Lev, S.; Li, C.; Desmarini, D.; Saiardi, A.; Fewings, N.L.; Schibeci, S.D.; Sharma, R.; Sorrell, T.C.; Djordjevic, J.T. Fungal inositol pyrophosphate IP7 is crucial for metabolic adaptation to the host environment and pathogenicity. mBio 2015, 6, e00531–e00515. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Lev, S.; Saiardi, A.; Desmarini, D.; Sorrell, T.C.; Djordjevic, J.T. Identification of a major IP5 kinase in Cryptococcus neoformans confirms that PP-IP5/IP7, not IP6, is essential for virulence. Sci. Rep. 2016, 6, 23927. [Google Scholar] [CrossRef] [PubMed]
- Saiardi, A.; Erdjument-Bromage, H.; Snowman, A.M.; Tempst, P.; Snyder, S.H. Synthesis of diphosphoinositol pentakisphosphate by a newly identified family of higher inositol polyphosphate kinases. Curr. Biol. 1999, 9, 1323–1326. [Google Scholar] [CrossRef]
- Odom, A.R.; Stahlberg, A.; Wente, S.R.; York, J.D. A role for nuclear inositol 1,4,5-trisphosphate kinase in transcriptional control. Science 2000, 287, 2026–2029. [Google Scholar] [CrossRef] [PubMed]
- Pohlmann, J.; Fleig, U. Asp1, a conserved 1/3 inositol polyphosphate kinase, regulates the dimorphic switch in Schizosaccharomyces pombe. Mol. Cell. Biol. 2010, 30, 4535–4547. [Google Scholar] [CrossRef] [PubMed]
- Fridy, P.C.; Otto, J.C.; Dollins, D.E.; York, J.D. Cloning and characterization of two human VIP1-like inositol hexakisphosphate and diphosphoinositol pentakisphosphate kinases. J. Biol. Chem. 2007, 282, 30754–30762. [Google Scholar] [CrossRef] [PubMed]
- Pohlmann, J.; Risse, C.; Seidel, C.; Pohlmann, T.; Jakopec, V.; Walla, E.; Ramrath, P.; Takeshita, N.; Baumann, S.; Feldbrugge, M.; et al. The Vip1 inositol polyphosphate kinase family regulates polarized growth and modulates the microtubule cytoskeleton in fungi. PLoS Genet. 2014, 10, e1004586. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Nair, V.S.; Holland, A.A.; Capolicchio, S.; Jessen, H.J.; Johnson, M.K.; Shears, S.B. Asp1 from Schizosaccharomyces pombe binds a [2Fe-2S](2+) cluster which inhibits inositol pyrophosphate 1-phosphatase activity. Biochemistry 2015, 54, 6462–6474. [Google Scholar] [CrossRef] [PubMed]
- Gokhale, N.A.; Zaremba, A.; Shears, S.B. Receptor-dependent compartmentalization of PPIP5K1, a kinase with a cryptic polyphosphoinositide binding domain. Biochem. J. 2011, 434, 415–426. [Google Scholar] [CrossRef] [PubMed]
- Mulugu, S.; Bai, W.; Fridy, P.C.; Bastidas, R.J.; Otto, J.C.; Dollins, D.E.; Haystead, T.A.; Ribeiro, A.A.; York, J.D. A conserved family of enzymes that phosphorylate inositol hexakisphosphate. Science 2007, 316, 106–109. [Google Scholar] [CrossRef] [PubMed]
- Glennon, M.C.; Shears, S.B. Turnover of inositol pentakisphosphates, inositol hexakisphosphate and diphosphoinositol polyphosphates in primary cultured hepatocytes. Biochem. J. 1993, 293, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Steidle, E.A.; Chong, L.S.; Wu, M.; Crooke, E.; Fiedler, D.; Resnick, A.C.; Rolfes, R.J. A novel inositol pyrophosphate phosphatase in Saccharomyces cerevisiae: Siw14 protein selectively cleaves the beta-phosphate from 5-diphosphoinositol pentakisphosphate (5PP-IP5). J. Biol. Chem. 2016, 291, 6772–6783. [Google Scholar] [CrossRef] [PubMed]
- Pietrella, D.; Cherniak, R.; Strappini, C.; Perito, S.; Mosci, P.; Bistoni, F.; Vecchiarelli, A. Role of mannoprotein in induction and regulation of immunity to Cryptococcus neoformans. Infect. Immun. 2001, 69, 2808–2814. [Google Scholar] [CrossRef] [PubMed]
- Delfino, D.; Cianci, L.; Migliardo, M.; Mancuso, G.; Cusumano, V.; Corradini, C.; Teti, G. Tumor necrosis factor-inducing activities of Cryptococcus neoformans components. Infect. Immun. 1996, 64, 5199–5204. [Google Scholar] [PubMed]
- Levitz, S.M.; Specht, C.A. The molecular basis for the immunogenicity of Cryptococcus neoformans mannoproteins. FEMS Yeast Res. 2006, 6, 513–524. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Nong, S.H.; Mansour, M.K.; Specht, C.A.; Levitz, S.M. Purification and characterization of a second immunoreactive mannoprotein from Cryptococcus neoformans that stimulates T-cell responses. Infect. Immun. 2002, 70, 5485–5493. [Google Scholar] [CrossRef] [PubMed]
- Voglmaier, S.M.; Bembenek, M.E.; Kaplin, A.I.; Dorman, G.; Olszewski, J.D.; Prestwich, G.D.; Snyder, S.H. Purified inositol hexakisphosphate kinase is an ATP synthase: Diphosphoinositol pentakisphosphate as a high-energy phosphate donor. Proc. Natl. Acad. Sci. USA 1996, 93, 4305–4310. [Google Scholar] [CrossRef] [PubMed]
- Lonetti, A.; Szijgyarto, Z.; Bosch, D.; Loss, O.; Azevedo, C.; Saiardi, A. Identification of an evolutionarily conserved family of inorganic polyphosphate endopolyphosphatases. J. Biol. Chem. 2011, 286, 31966–31974. [Google Scholar] [CrossRef] [PubMed]
- Boer, V.M.; Crutchfield, C.A.; Bradley, P.H.; Botstein, D.; Rabinowitz, J.D. Growth-limiting intracellular metabolites in yeast growing under diverse nutrient limitations. Mol. Biol. Cell 2010, 21, 198–211. [Google Scholar] [CrossRef] [PubMed]
- Belde, P.J.; Vossen, J.H.; Borst-Pauwels, G.W.; Theuvenet, A.P. Inositol 1,4,5-trisphosphate releases Ca2+ from vacuolar membrane vesicles of Saccharomyces cerevisiae. FEBS Lett. 1993, 323, 113–118. [Google Scholar] [CrossRef]
- Cornelius, G.; Gebauer, G.; Techel, D. Inositol trisphosphate induces calcium release from Neurospora crassa vacuoles. Biochem. Biophys. Res. Commun. 1989, 162, 852–856. [Google Scholar] [CrossRef]
- Calvert, C.M.; Sanders, D. Inositol trisphosphate-dependent and -independent Ca2+ mobilization pathways at the vacuolar membrane of Candida albicans. J. Biol. Chem. 1995, 270, 7272–7280. [Google Scholar] [PubMed]
- Ho, M.W.; Yang, X.; Carew, M.A.; Zhang, T.; Hua, L.; Kwon, Y.U.; Chung, S.K.; Adelt, S.; Vogel, G.; Riley, A.M.; et al. Regulation of Ins(3,4,5,6)P(4) signaling by a reversible kinase/phosphatase. Curr. Biol. 2002, 12, 477–482. [Google Scholar] [CrossRef]
- Xie, W.; Kaetzel, M.A.; Bruzik, K.S.; Dedman, J.R.; Shears, S.B.; Nelson, D.J. Inositol 3,4,5,6-tetrakisphosphate inhibits the calmodulin-dependent protein kinase II-activated chloride conductance in T84 colonic epithelial cells. J. Biol. Chem. 1996, 271, 14092–14097. [Google Scholar] [PubMed]
- Renstrom, E.; Ivarsson, R.; Shears, S.B. Inositol 3,4,5,6-tetrakisphosphate inhibits insulin granule acidification and fusogenic potential. J. Biol. Chem. 2002, 277, 26717–26720. [Google Scholar] [CrossRef] [PubMed]
- Ismailov, I.I.; Fuller, C.M.; Berdiev, B.K.; Shlyonsky, V.G.; Benos, D.J.; Barrett, K.E. A biologic function for an “orphan” messenger: d-myo-inositol 3,4,5,6-tetrakisphosphate selectively blocks epithelial calcium-activated chloride channels. Proc. Natl. Acad. Sci. USA 1996, 93, 10505–10509. [Google Scholar] [CrossRef] [PubMed]
- Vajanaphanich, M.; Schultz, C.; Rudolf, M.T.; Wasserman, M.; Enyedi, P.; Craxton, A.; Shears, S.B.; Tsien, R.Y.; Barrett, K.E.; Traynor-Kaplan, A. Long-term uncoupling of chloride secretion from intracellular calcium levels by Ins(3,4,5,6)P4. Nature 1994, 371, 711–714. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Rudolf, M.; Carew, M.A.; Yoshida, M.; Nerreter, V.; Riley, A.M.; Chung, S.K.; Bruzik, K.S.; Potter, B.V.; Schultz, C.; et al. Inositol 1,3,4-trisphosphate acts in vivo as a specific regulator of cellular signaling by inositol 3,4,5,6-tetrakisphosphate. J. Biol. Chem. 1999, 274, 18973–18980. [Google Scholar] [CrossRef] [PubMed]
- Chamberlain, P.P.; Qian, X.; Stiles, A.R.; Cho, J.; Jones, D.H.; Lesley, S.A.; Grabau, E.A.; Shears, S.B.; Spraggon, G. Integration of inositol phosphate signaling pathways via human ITPK1. J. Biol. Chem. 2007, 282, 28117–28125. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.; Mollapour, E.; Shears, S.B. Signal transduction during environmental stress: InsP8 operates within highly restricted contexts. Cell. Signal. 2005, 17, 1533–1541. [Google Scholar] [CrossRef] [PubMed]
- Pesesse, X.; Choi, K.; Zhang, T.; Shears, S.B. Signaling by higher inositol polyphosphates. Synthesis of bisdiphosphoinositol tetrakisphosphate (“InsP8”) is selectively activated by hyperosmotic stress. J. Biol. Chem. 2004, 279, 43378–43381. [Google Scholar] [CrossRef] [PubMed]
- Ongusaha, P.P.; Hughes, P.J.; Davey, J.; Michell, R.H. Inositol hexakisphosphate in Schizosaccharomyces pombe: Synthesis from Ins(1,4,5)P3 and osmotic regulation. Biochem. J. 1998, 335, 671–679. [Google Scholar] [CrossRef] [PubMed]
- Worley, J.; Luo, X.; Capaldi, A.P. Inositol pyrophosphates regulate cell growth and the environmental stress response by activating the HDAC Rpd3L. Cell Rep. 2013, 3, 1476–1482. [Google Scholar] [CrossRef] [PubMed]
- York, J.D. Regulation of nuclear processes by inositol polyphosphates. Biochim. Biophys. Acta 2006, 1761, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Wild, R.; Gerasimaite, R.; Jung, J.Y.; Truffault, V.; Pavlovic, I.; Schmidt, A.; Saiardi, A.; Jessen, H.J.; Poirier, Y.; Hothorn, M.; et al. Control of eukaryotic phosphate homeostasis by inositol polyphosphate sensor domains. Science 2016, 352, 986–990. [Google Scholar] [CrossRef] [PubMed]
- Secco, D.; Wang, C.; Shou, H.; Whelan, J. Phosphate homeostasis in the yeast Saccharomyces cerevisiae, the key role of the SPX domain-containing proteins. FEBS Lett. 2012, 586, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Mulugu, S.; York, J.D.; O’Shea, E.K. Regulation of a cyclin-CDK-CDK inhibitor complex by inositol pyrophosphates. Science 2007, 316, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Millard, C.J.; Watson, P.J.; Celardo, I.; Gordiyenko, Y.; Cowley, S.M.; Robinson, C.V.; Fairall, L.; Schwabe, J.W. Class I HDACs share a common mechanism of regulation by inositol phosphates. Mol. Cell. 2013, 51, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Watson, P.J.; Fairall, L.; Santos, G.M.; Schwabe, J.W. Structure of HDAC3 bound to co-repressor and inositol tetraphosphate. Nature 2012, 481, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Stephens, L.; Radenberg, T.; Thiel, U.; Vogel, G.; Khoo, K.H.; Dell, A.; Jackson, T.R.; Hawkins, P.T.; Mayr, G.W. The detection, purification, structural characterization, and metabolism of diphosphoinositol pentakisphosphate(s) and bisdiphosphoinositol tetrakisphosphate(s). J. Biol. Chem. 1993, 268, 4009–4015. [Google Scholar] [PubMed]
- Laussmann, T.; Eujen, R.; Weisshuhn, C.M.; Thiel, U.; Vogel, G. Structures of diphospho-myo-inositol pentakisphosphate and bisdiphospho-myo-inositol tetrakisphosphate from Dictyostelium resolved by NMR analysis. Biochem. J. 1996, 315, 715–720. [Google Scholar] [CrossRef] [PubMed]
- Saiardi, A.; Bhandari, R.; Resnick, A.C.; Snowman, A.M.; Snyder, S.H. Phosphorylation of proteins by inositol pyrophosphates. Science 2004, 306, 2101–2105. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, R.; Saiardi, A.; Ahmadibeni, Y.; Snowman, A.M.; Resnick, A.C.; Kristiansen, T.Z.; Molina, H.; Pandey, A.; Werner, J.K., Jr.; Juluri, K.R.; et al. Protein pyrophosphorylation by inositol pyrophosphates is a posttranslational event. Proc. Natl. Acad. Sci. USA 2007, 104, 15305–15310. [Google Scholar] [CrossRef] [PubMed]
- Szijgyarto, Z.; Garedew, A.; Azevedo, C.; Saiardi, A. Influence of inositol pyrophosphates on cellular energy dynamics. Science 2011, 334, 802–805. [Google Scholar] [CrossRef] [PubMed]
- Saiardi, A.; Cockcroft, S. Human ITPK1: A reversible inositol phosphate kinase/phosphatase that links receptor-dependent phospholipase C to Ca2+-activated chloride channels. Sci. Signal. 2008, 1, pe5. [Google Scholar] [CrossRef] [PubMed]
- Miller, G.J.; Wilson, M.P.; Majerus, P.W.; Hurley, J.H. Specificity determinants in inositol polyphosphate synthesis: Crystal structure of inositol 1,3,4-trisphosphate 5/6-kinase. Mol. Cell 2005, 18, 201–212. [Google Scholar] [CrossRef] [PubMed]
- Holmes, W.; Jogl, G. Crystal structure of inositol phosphate multikinase 2 and implications for substrate specificity. J. Biol. Chem. 2006, 281, 38109–38116. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; DeRose, E.F.; London, R.E.; Shears, S.B. IP6K structure and the molecular determinants of catalytic specificity in an inositol phosphate kinase family. Nat. Commun. 2014, 5, 4178. [Google Scholar] [CrossRef] [PubMed]
- Endo-Streeter, S.; Tsui, M.K.; Odom, A.R.; Block, J.; York, J.D. Structural studies and protein engineering of inositol phosphate multikinase. J. Biol. Chem. 2012, 287, 35360–35369. [Google Scholar] [CrossRef] [PubMed]
- Miller, G.J.; Hurley, J.H. Crystal structure of the catalytic core of inositol 1,4,5-trisphosphate 3-kinase. Mol. Cell 2004, 15, 703–711. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, B.; Schell, M.J.; Letcher, A.J.; Veprintsev, D.B.; Irvine, R.F.; Williams, R.L. Structure of a human inositol 1,4,5-trisphosphate 3-kinase: Substrate binding reveals why it is not a phosphoinositide 3-kinase. Mol. Cell 2004, 15, 689–701. [Google Scholar] [CrossRef] [PubMed]
- El Bakkoury, M.; Dubois, E.; Messenguy, F. Recruitment of the yeast MADS-box proteins, ArgRI and Mcm1 by the pleiotropic factor ArgRIII is required for their stability. Mol. Microbiol. 2000, 35, 15–31. [Google Scholar] [CrossRef] [PubMed]
- Messenguy, F.; Dubois, E. Genetic evidence for a role for MCM1 in the regulation of arginine metabolism in Saccharomyces cerevisiae. Mol. Cell. Biol. 1993, 13, 2586–2592. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Godage, H.Y.; Riley, A.M.; Weaver, J.D.; Shears, S.B.; Potter, B.V. Synthetic inositol phosphate analogs reveal that PPIP5K2 has a surface-mounted substrate capture site that is a target for drug discovery. Chem. Biol. 2014, 21, 689–699. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.T.; Choi, G.; Bae, Y.S.; Burdett, M.; Moon, H.S.; Lee, J.W.; Gray, N.S.; Schultz, P.G.; Meijer, L.; Chung, S.K.; et al. Purine-based inhibitors of inositol-1,4,5-trisphosphate-3-kinase. Chembiochem 2002, 3, 897–901. [Google Scholar] [CrossRef]
- Padmanabhan, U.; Dollins, D.E.; Fridy, P.C.; York, J.D.; Downes, C.P. Characterization of a selective inhibitor of inositol hexakisphosphate kinases: Use in defining biological roles and metabolic relationships of inositol pyrophosphates. J. Biol. Chem. 2009, 284, 10571–10582. [Google Scholar] [CrossRef] [PubMed]
- Dubois, E.; Scherens, B.; Vierendeels, F.; Ho, M.M.; Messenguy, F.; Shears, S.B. In Saccharomyces cerevisiae, the inositol polyphosphate kinase activity of Kcs1p is required for resistance to salt stress, cell wall integrity, and vacuolar morphogenesis. J. Biol. Chem. 2002, 277, 23755–23763. [Google Scholar] [CrossRef] [PubMed]
- Mayr, G.W.; Windhorst, S.; Hillemeier, K. Antiproliferative plant and synthetic polyphenolics are specific inhibitors of vertebrate inositol-1,4,5-trisphosphate 3-kinases and inositol polyphosphate multikinase. J. Biol. Chem. 2005, 280, 13229–13240. [Google Scholar] [CrossRef] [PubMed]
- Fraifeld, V.; Seidman, R.; Sagi, O.; Muradian, K.; Wolfson, M. Aurintricarboxylic acid decreases proliferative potential of SKOV3 and MCF7 human carcinoma cells. Anticancer Res. 2001, 21, 1975–1978. [Google Scholar] [PubMed]
- Mori, H.; Kawabata, K.; Matsunaga, K.; Ushida, J.; Fujii, K.; Hara, A.; Tanaka, T.; Murai, H. Chemopreventive effects of coffee bean and rice constituents on colorectal carcinogenesis. Biofactors 2000, 12, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Benezra, M.; Ben-Sasson, S.A.; Regan, J.; Chang, M.; Bar-Shavit, R.; Vlodavsky, I. Antiproliferative activity to vascular smooth muscle cells and receptor binding of heparin-mimicking polyaromatic anionic compounds. Arterioscler. Thromb. 1994, 14, 1992–1999. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.M.; Kully, M.; Khan, J.K.; Hattori, M.; Daneshtalab, M. Synthesis of chlorogenic acid derivatives with promising antifungal activity. Bioorg. Med. Chem. 2007, 15, 6830–6833. [Google Scholar] [CrossRef] [PubMed]
- Mellon, J.E.; Dowd, M.K.; Beltz, S.B.; Moore, G.G. Growth inhibitory effects of gossypol and related compounds on fungal cotton root pathogens. Lett. Appl. Microbiol. 2014, 59, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Sung, S.W.; Lee, D.G. Antifungal action of chlorogenic acid against pathogenic fungi, mediated by membrane disruption. Pure Appl. Chem. 2010, 82, 219–226. [Google Scholar] [CrossRef]
- Da Silva, C.R.; de Andrade Neto, J.B.; de Sousa Campos, R.; Figueiredo, N.S.; Sampaio, L.S.; Magalhaes, H.I.; Cavalcanti, B.C.; Gaspar, D.M.; de Andrade, G.M.; Lima, I.S.; et al. Synergistic effect of the flavonoid catechin, quercetin, or epigallocatechin gallate with fluconazole induces apoptosis in Candida tropicalis resistant to fluconazole. Antimicrob. Agents Chemother. 2014, 58, 1468–1478. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.J.; Guo, X.; Dawuti, G.; Aibai, S. Antifungal activity of ellagic acid in vitro and in vivo. Phytother. Res. 2015, 29, 1019–1025. [Google Scholar] [CrossRef] [PubMed]
- Rezusta, A.; Lopez-Chicon, P.; Paz-Cristobal, M.P.; Alemany-Ribes, M.; Royo-Diez, D.; Agut, M.; Semino, C.; Nonell, S.; Revillo, M.J.; Aspiroz, C.; et al. In vitro fungicidal photodynamic effect of hypericin on Candida species. Photochem. Photobiol. 2012, 88, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Paz-Cristobal, M.P.; Gilaberte, Y.; Alejandre, C.; Pardo, J.; Revillo, M.J.; Rezusta, A. In vitro fungicidal photodynamic effect of hypericin on Trichophyton spp. Mycopathologia 2014, 178, 221–225. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license ( http://creativecommons.org/licenses/by/4.0/).