Abstract
The aim of this review was to answer the following PICO question: “Do TMJ kinematic parameters (intervention and comparison) show efficacy for assessment of mandibular function (Outcome) both in asymptomatic and TMD subjects? (Population)”. PubMed, Scopus, Web of Science, Embase, Central databases were searched. The inclusion criteria were (1) performed on human, (2) English only, (3) on healthy, symptomatic or surgically altered TMJ, (4) measured dynamic kinematics of mandible or TMJ (5) with six degrees of freedom. To assess the Risk of Bias, the Joanna Briggs Institute tool for non-randomised clinical studies was employed. A pairwise meta-analysis was carried out using STATA v.17.0 (Stata). The heterogeneity was estimated using the Q value and the inconsistency index. Ninety-two articles were included in qualitative synthesis, nine studies in quantitative synthesis. The condylar inclination was significantly increased in female (effect size 0.03°, 95% CI: −0.06, 0.12, p = 0.00). Maximum mouth opening (MMO) was increased significantly in female population in comparison with males (effect size 0.65 millimetres (0.36, 1.66). Incisor displacement at MMO showed higher values for control groups compared with TMD subjects (overall effect size 0.16 millimetres (−0.37, 0.69). Evidence is still needed, considering the great variety of devices and parameters used for arthrokinematics. The present study suggests standardising outcomes, design, and population of the future studies in order to obtain more reliable and repeatable values.
1. Introduction
The temporomandibular joint is a bilateral synovial joint between the temporal bone and the mandible, that function as one unit. Since the TMJ is connected to the mandible, the right and left joints must function together and therefore are not independent of each other. TMJ represents the only mobile joint in the skull. Mandibular stability and movements are essential to perform normal jaw function like biting, chewing, swallowing, and speech [1]. Loss of TMJ function, reduced coordination and pain are factors that determine social dysfunction and discomfort [2].
Temporomandibular disorders (TMD) are a group of heterogeneous clinical situations with multifactorial aetiology which can be related with musculoskeletal pain, joint noise and functional problems. TMD are a significant public health problem, and they represent one of the most common musculoskeletal conditions resulting in pain and disability [3] which mainly affects women. The prevalence of TMD is thought to be greater than 5–12% of the population. Regarding the symptomatology there is a peak occurrence between 20 and 40 years of age [4]. Temporomandibular joint disorders are classified in inflammatory and non-inflammatory pathologies which include disc displacement with reduction, disc displacement without reduction, structural incompatibility, adherence/adhesion, ankylosis, capsulitis, synovitis, retrodiscitis, dislocation, and osteoarthritis [3,5,6,7]. Chronic disc displacement and osteoarthritis are two most frequent TMJ disorders resulting in inflammatory and degenerative process of the joint structures [8]. TMD diagnosis is generally entrusted in physical and clinical examination findings and imaging, and more recently in kinematic analysis which is connected to function.
The treatment of muscle-related pain in TMD commonly consisted of occlusal splint devices, behavioural therapies and other conservative non-pharmacological approaches such as manual therapy, laser therapy, transcutaneous electrical nerve stimulation (TENS) and dry needling. Conservative and physical therapies are recommended for the initial treatment of TMD [9,10,11].
Mandibular kinematics measurements are used for clinical purpose such as study of dynamic occlusion in prosthodontic restorations, orthodontic and gnathological therapies, and for screening of temporomandibular dysfunction [12]. The correlation between TMD and mandibular kinematics has been described in literature: several studies evaluated TMJ function using various parameters such as condylar trajectories, incisal trajectories, mandibular rotation and translation, hinge axis, finite helical axis, intra-articular joint space and mastication cycle data in healthy and affected subjects [13]. However, there is still not enough scientific evidence to establish the physiological and pathological ranges of the kinematic parameters in order to obtain a strong efficacy in using this diagnostic tool.
Mandibular kinematics techniques can be classified in four categories: mechanical linkage systems, magnetic tracking systems, video motion analysis and radiographic tracking [14].
TMD are closely connected to mandibular movement and function, for that reason could be important to have an early and objective diagnosis. Therefore, the aim of this systematic review and meta-analysis is to demonstrate if and which kinematic parameters are useful to diagnose musculoskeletal jaw’s disorders, in order to assess clinical efficacy of this diagnostic tool for treatment planning. The outcome of this study may be useful also to lead future research studies on TMJ kinematic and its correlation to TMD.
2. Materials and Methods
This review followed the guidelines of the preferred reporting items for systematic reviews (PRISMA) [15]. The goal of this meta-analysis was to assess the efficacy of TMJ kinematics parameters for the early diagnosis of TMJ disorders, which is a controversial current clinical topic. The review was registered on the PROSPERO with a registration reference number 313476.
Participants/Population: Patients who are affected by temporomandibular disorders diagnosed according to diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications, in particular myofascial pain, anterior disk displacement with or without joint noises, arthralgia, osteoarthritis and osteoarthrosis for at least three months. No particular limitations about patients age.
Intervention: TMD conservative treatment and non-surgical intervention. There were no restrictions of the duration of intervention.
Comparator (s): Asymptomatic subjects with different types of occlusion. No limitations about subjects age.
Outcome(s): Maximum mouth opening is distance between the incisal edge of the maxillary central incisors to the incisal edge of the mandibular central incisors at the midline when the mouth is open as wide as possible. Incisor displacement at MMO (IP-MMO) is the distance between the incisor point from the medial sagittal plane during maximum mouth opening. Condylar inclination represents the angle of the condyle translating down the condylar eminence as the mandible moves. Horizontal and sagittal angles are decomposition of the mandibular trajectory on the three planes of space.
Time: follow up at 6 mouths.
2.1. Eligibility Criteria
The eligibility criteria were planned considering the following population, intervention, comparison and outcome (PICO) question: “Do TMJ kinematic parameters (intervention and comparison) show efficacy for assessment of mandibular function (Outcome) both in asymptomatic and TMD subjects? (Population)”. We only included studies performed on humans and written in English. Moreover, opinion-based papers, perspectives, conference papers, book chapters, case reports and abstract were excluded. We also considered the cross-references of the included articles and reviews. The studies that met the following criteria: focused on healthy, symptomatic or surgically altered TMJ, measured dynamic kinematic of mandible or TMJ with six degrees of freedom were all included for qualitative and if found eligible quantitative analysis.
2.2. Search Strategy
A search for articles in the following electronic databases was carried out: PubMed, Scopus, Web of Science, Embase, Central. The databases were searched up until 2 January 2022. The key words used were: “temporomandibular joint” OR “TMJ” OR “mandible” OR “temporomandibular joint disorder” OR “TMD” AND “kinematics” OR “jaw motion” OR “motion analysis” OR “biomechanics”. A mix of medical subject headings and free key words were used. Only the studies published in English were included. The articles were manually checked for relevant articles to be included in the review. Once duplicates were removed, titles and abstracts were screened PRISMA flowchart was used to summarise the selection process (Figure 1).
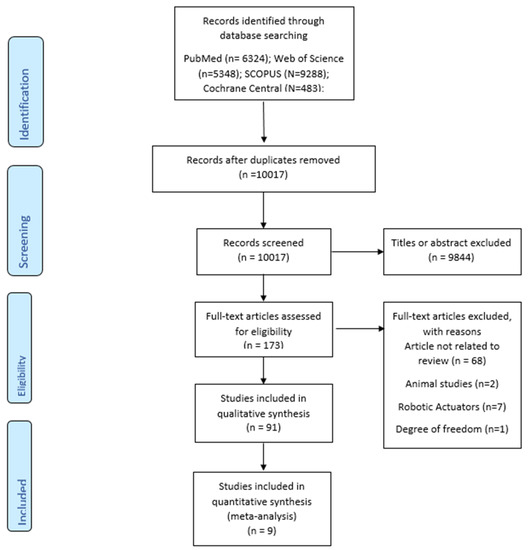
Figure 1.
PRISMA flow chart.
2.3. Selection Process
Search strategy was implemented and tested by three researchers independently (GMT, AS and CG). All articles and abstract which met the selection criteria were included in the review. Three reviewers screened all the titles and abstract independently, those that seemed suitable were included in the full text review. When the information provided in the abstract and title were inadequate to determine eligibility, articles were included in full text review. Any disagreement among the reviewers was resolved by comparison discussion. At least two studies have to be considered to perform the meta-analysis, even if studies can be meaningfully pooled and provided their results are sufficiently ‘similar’ [13].
2.4. Data Collection Process
Data from the included articles were extracted by three independent reviewers and organised into a data sheet using Microsoft Excel 2013 (Microsoft Corp, Remond, WA, USA, https://www.microsoft.com/en-in/, accessed on 10 April 2022). A set of standard variables included was validated by discussing with all the reviewers. The validation was done based on the outcomes included in the previous literature used to assess the TMJ kinematics. The following items were extracted whenever possible: authors, year, country, journal, sponsor, study design, number, mean age and gender of the participants, number of test group, number of control group, TMJ condition, diagnostic tool, kinematic parameters analysed, mean values, number of samples in each group and standard deviation for groups. For each parameter, unit of measurement was specified. Data such as gender, study design, diagnostic tool, different TMD conditions for respective outcomes were used as sub-group analysis.
2.5. Data Items
The results of each study were recorded. Condylar trajectories, incisal trajectories, kinematic hinge axis, finite helical axis, intra-articular space joint, mastication cycle data and bennet angle were the outcomes of the analysed studies. All the outcomes were screened and recorded to assess if a comparison will be possible [16].
The main outcomes of the quantitative synthesis were maximum mouth opening (MMO) (degree and mm), Condylar inclination (degrees), horizontal (degrees) and sagittal angle (degrees) and linear displacement of the interincisal point at maximum mouth opening (IP)-MMO (mm) which are five parameters that represent an index of TMJ movement three-dimensionally. If different units of measure were identified, for the same parameter, we excluded them from quantitative synthesis and reported them in qualitative synthesis.
2.6. Quality and Risk of Bias Assessment
The risk of bias assessment of the included NRTCs was performed by three independent reviewers. The JBI—the Joanna Briggs Institute tool was used to assess the methodological quality of case control studies, cohort studies, cross sectional studies and case series. Each study was assessed according to predefined criteria. The JBI model of evidence-based healthcare conceptualises evidence-based practice as clinical decision-making that considers the best available evidence; the context in which care is delivered; client preference; and the professional judgement of the health professional [17]. The strength of this model is feasibility (setting realistic outcomes by knowing the right intervention and cost effectiveness), appropriateness (establish a best fit model for intervention), meaningfulness (establishing the experience) and effectiveness (scale at which intervention achieves the intended results and outcomes) [18]. The assessment tool was developed using a scored checklist of quality assessment questions. Each question was attributed a score of 1 or 0 based on whether the question in a given paper was clearly addressed or not addressed, respectively. The total scores were summed up. Studies with scores of 0–5, 5–6, and 7–11 points were considered low, moderate, and high-quality studies, respectively. Discussion among reviewers were used to solve any discrepancies in score.
2.7. Outcome Variables
Condylar inclination represents the angle of the condyle translating down the condylar eminence as the mandible moves. In this meta-analysis, the angle is evaluated during protrusive movement of the mandible and is measured in degrees.
The maximum mouth opening (MMO) has been defined as “the greatest distance between the incisal edge of the maxillary central incisors to the incisal edge of the mandibular central incisors at the midline when the mouth is open as wide as possible” [19,20]. MMO can be measured as a linear distance in millimetres or as an angle in degree. This meta-analysis compares MMO measured in millimetres.
Incisor displacement at MMO (IP-MMO) is the distance between the incisor point from the medial sagittal plane during maximum mouth opening, the unit of measure is millimetre.
Horizontal and sagittal angles are the indexes of mandibular movement which could be discomposed in three dimensions of space. These parameters are measures in degrees.
2.8. Measures of Treatment Effect
For continuous outcomes, we pooled data with the mean difference (MD), or standardised mean difference (SMD) if different measures were used to assess the same outcome. If the data are given for each patient, then we used the data to calculate the mean and sd using STATA software v17.0. The mean and sd were collected as mentioned in the published papers and there was no conversion of the values and the units of measure for pairwise comparison. If there were different levels of measure, then we would collect data in categorised form and use it in subgroup analysis.
MMO was analysed using as a reference point the value described by Travell [19] who measured 53 mm for women and 59 mm for men. Condylar inclination varies between 0° and 60°. The greatest frequency is around 40° to 50° [21]. To compare linear incisor displacement at MMO, values reported by Rieder [22], Ferrario [23] and Tsolka [24] were considered as the reference point.
2.9. Synthesis Methods
A meta-analysis was carried out only when there were at least two studies of similar comparisons reporting the same outcomes and unit of measure. A pairwise meta-analysis was carried out using STATA v.17.0 (Stata). The heterogeneity between each study was estimated using the Q value and the inconsistency index (I2 test). If the I2 is ≤50%, it suggests that there is negligible statistical heterogenicity and the fixed effects model will be employed. If the I2 is >50% we explored sources of heterogenicity by subgroup analysis and meta regression. If there was no clinical heterogenicity, the random effects model was used to perform the meta-analysis.
3. Results
3.1. Study Selection and Description
The initial research identified 28619 titles; 10017 remained after duplicates removal. Out of the remaining titles, 184 articles were considered potentially eligible and after a full text revision, verification of inclusion and exclusion criteria was carried out. Sixty-seven studies were excluded because the topic was not related to the review, two were studies on animals, seven on robotic actuators, one did not respect the six degree of freedom and four were systematic reviews. At the end of this stage, 92 were selected for qualitative synthesis. Eventually after outcomes assessment, eight comparative studies were selected for meta-analysis (Flowchart, Figure 1). The PICO assessment and the main findings are reported in Table 1.

Table 1.
PICO assessment and main findings.
3.2. Bias Risk Assessment
JBI Quality sores were collected and reported in an excel table. The JBI tool of the Case control studies ranging from 5 to 9. 7 were considered with moderate risk of bias, 10 studies showed high risk of bias. Cohort studies ranging from 4 to 9. 4 were considered moderate risk of bias, 10 showed high risk of bias. Cross sectional studies ranged from 5 to 7 with moderate quality. Case series studies raged from 1 to 8, all the studies showed high risk of bias.
3.2.1. Qualitative Synthesis
The results of 92 articles were compared to evaluate the kinematic parameters useful to the assessment of TMJ function. Each study considered more than one parameter. A total of 58 studies measured condylar trajectories, 10 incisal trajectories, 8 mastication cycle data, 7 intra-articular joint space, 8 finite helical axis, 15 mandibular rotation and translation, 15 hinge axis and 1 muscular length.
All studies included were non-randomised clinical trials: 17 were case control studies, 14 were cohort studies, 59 were case series and 2 were cross sectional studies, involving a total of 3342 participants, of which 1127 were males and 2030 females, there were 2752 tests and 590 controls subjects. Among participants the following were reported: 813 with TMD, 201 with malocclusion, 204 with surgical intervention, 30 with condyle fracture, 8 with zygomatic fracture, 8 with cerebral palsy, 16 with Trigeminal neuropathic pain and 2062 asymptomatic subjects.
Among the included studies, 43 reported their funding source: 4 received funding from Research institutes, 9 from foundations, 14 from universities and 16 from Grants. The remaining studies did not declare any funding source as reported in the characteristics table (Table S1 in Supplementary Materials).
3.2.2. Quantitative Synthesis
A meta-analysis was performed considering the following outcomes: condylar inclination, maximum mouth opening (MMO), linear incisal displacement at MMO (IP-MMO), and horizontal and sagittal angle, which are mandibular motion indices at maximum opening. For each parameter the mean and standard deviation were recorded. The studies included for quantitative synthesis were Wieckiewicz et al. 2014; Baqaien et al. 2007; Reichender et al. 2013; Ferrario et al. 2005; Gallo et al. 1997; Mapelli 2016; Ugolini 2018; Mapelli 2016; Ugolini 2017.
3.3. Condylar Inclination
In three studies [25,26,27], condylar inclinations were compared between female and male with degrees as unit of measure. All subjects assessed were asymptomatic. Quantitative results show higher values for female with statistically significant difference (95% CI, Overall Effect size in degree 0.03 [−0.06, 0.12], Heterogenicity: T2 = 0.02, I2 = 57,76%, H2 = 2.37, Test of ϴi = ϴj = Q (19) = 45.24, p = 0.00) (Figure 2). Considering the diagnostic tool, axiography shows similar values in males and females, instead ultrasonic tracking technique favours female, however no statistically significant difference was found in term of diagnostic tool. (Figure 3). A subgroup analysis regarding condylar inclination was performed: age analysis shows a negative correlation in adult group, condylar inclination decreased when age increased. The mouth opening analysis demonstrates that there is no correlation between condylar inclination and level of opening (p = 0.65) (Figure 4).
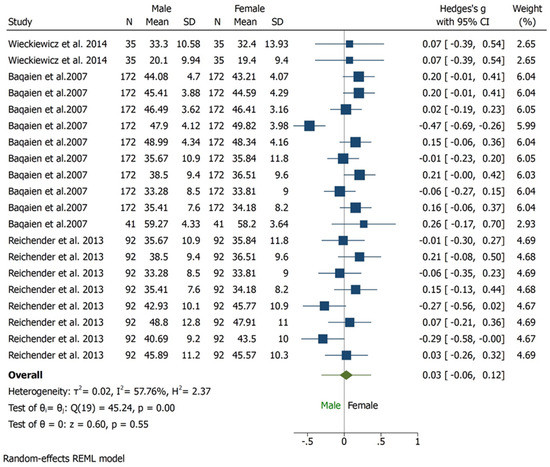
Figure 2.
Forest plot for condylar inclination outcome.
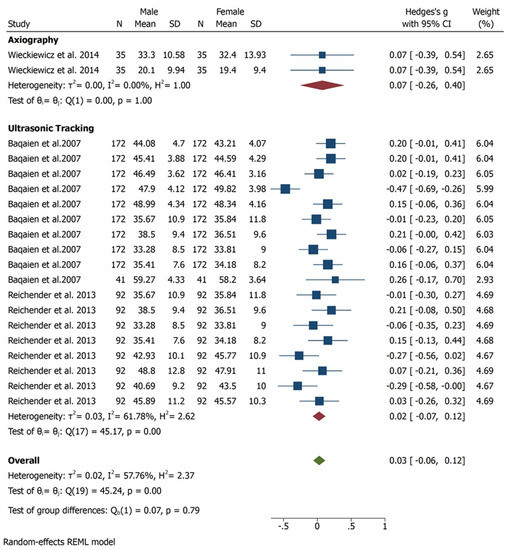
Figure 3.
Forest plot for different method employed to estimate the condylar inclination.
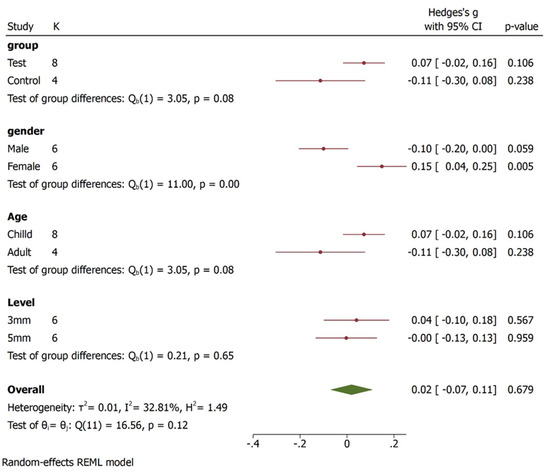
Figure 4.
Condylar inclination subgroup analysis forest plot displays the study labels (id), the number of studies within each group (K), the plot of effect sizes and their CIs (plot), the values of effect sizes and their CIs (esci), and the p-values (p-value) of the corresponding significance tests. The between-group homogeneity test based on the Qb is reported for each subgroup analysis. For example, for subgroup analysis based on variable “Group”, there are two groups “test” and “control”. The test investigates whether the overall effect sizes corresponding to these two groups are the same. The results of this test are identical to those we would have obtained if we had specified subgroup (Group).
3.4. Maximum Mouth Opening
Regarding MMO, three studies [27,28,29] were used to perform meta-analysis. The studies included MMO outcome, the unit of measure reported was in millimetre (mm). Male and female were compared: the overall effect size was 0.65 mm (−0.36, 1.66) with 95% CI, heterogeneity is I2 = 90.12% which indicates the studies were highly heterogeneous in characteristics. The pooled effect has passed the line of no effect, hence there exists statistically significant difference between the male and female groups in MMO outcome. The results were favouring females who showed higher values of MMO (Figure 5). Since the heterogeneity is very high, the results should be interpreted with caution and more studies are required to reach a meaningful interpretation.
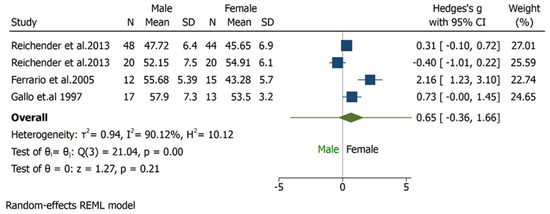
Figure 5.
Forest plot for MMO outcome. The overall effect size was 0.65 (−0.36, 1.66). The highest weight was 27.01% with sample size N = 48 in males and N = 44 in females. The heterogeneity is I2 = 90.12% which indicates, the studies were found to be highly heterogeneous in characteristics. The pooled effect has passed the line of no effect, hence there exists statistically significant difference between the studies in MMO outcome favouring females.
The subgroup analysis shows that there is significant difference between the type of studies (case control and cohort studies) included and MMO outcome (Figure 6). Children and adult did not have significant values although the effect size varied. The Galbraith Plot for MMO shows the heterogeneity of the analysed studies: two studies were identified as outlier (Figure 7). There is a publication bias in MMO outcome as illustrated from funnel plot (Figure 8).
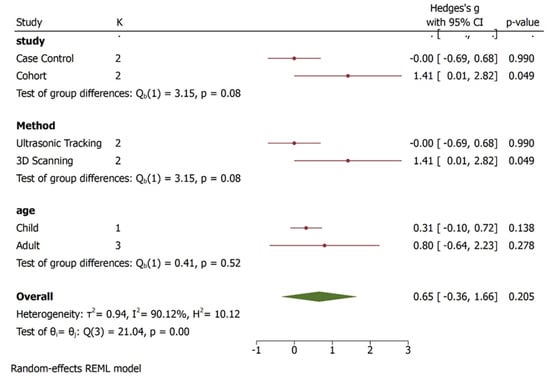
Figure 6.
Subgroup analysis for MMO outcomes. The overall effect size was 0.65 (−0.36, 1.66). There is statistical significance between the type of studies included and its impact of results in MMO outcome. In addition, the method employed to record MMO outcome was statistically significant. Children and adult did not have significant values although the effect size varied i.e., child 0.31 (−1.10, 0.72) and adult 0.80 (−0.64, 2.23).
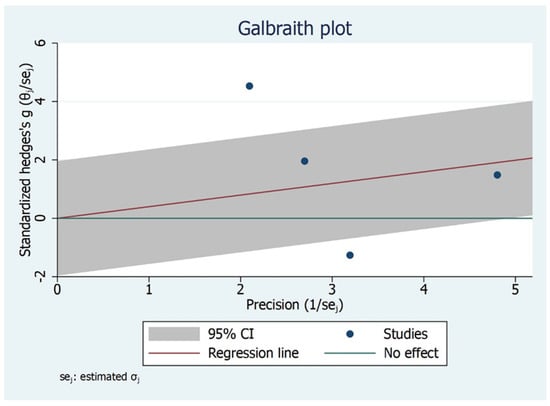
Figure 7.
Galbraith Plot for MMO Outcome illustrating heterogeneity of the studies and detecting potential outliers. Two studies identified as an outlier.
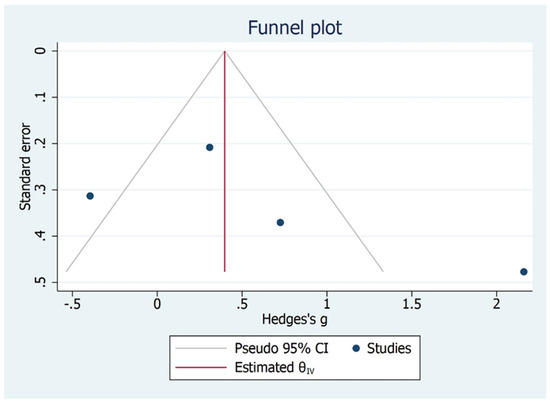
Figure 8.
Publication bias for MMO outcome.
3.5. IP-MMO
The linear incisor displacement at MMO was analysed in two studies [30,31]. As for MMO, the unit of measure reported was millimetre. The comparison between TMD subjects and control group (asymptomatic) showed no significantly higher values for control asymptomatic subjects than TMD subjects (p = 0.05), the overall effect size being 0.16 mm (−0.37, 0.69) (95% CI) (Figure 9, Figure 10 and Figure 11).
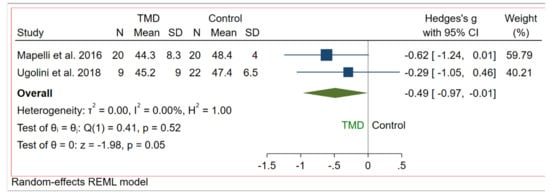
Figure 9.
Forest plot for IP-MMO outcome.
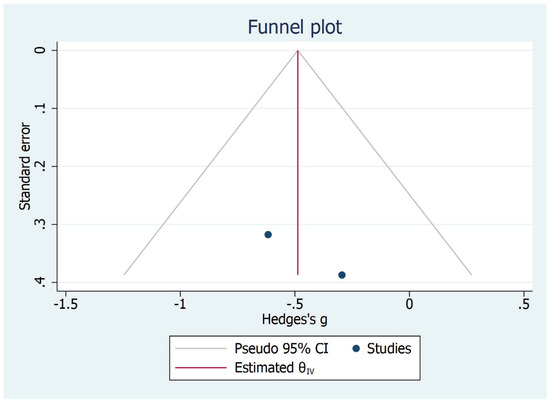
Figure 10.
Publication Bias for IP-MMO outcome.
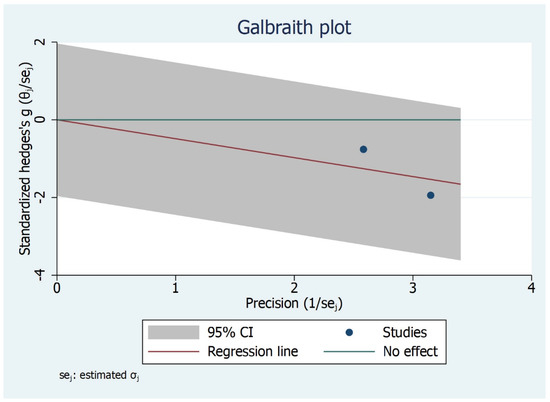
Figure 11.
Galbraith plot for IP-MMO outcome.
3.6. Horizontal Angle
The horizontal angle was analysed in two studies [30,31] and reported in degrees. Treatment group was compared to control group: subjects who were surgically treated showed lower values than the controls. However, no statistically significant difference was found in terms of angle variation between the two groups (CI 95%, I2 = 0%, H2 = 1.00, p = 0.56). As for IP-MMO, the overall effect size was 0.16 (−0.37, 0.69) (Figure 12, Figure 13 and Figure 14).
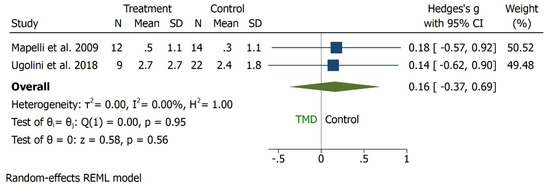
Figure 12.
Forest plot for horizontal angle outcome.
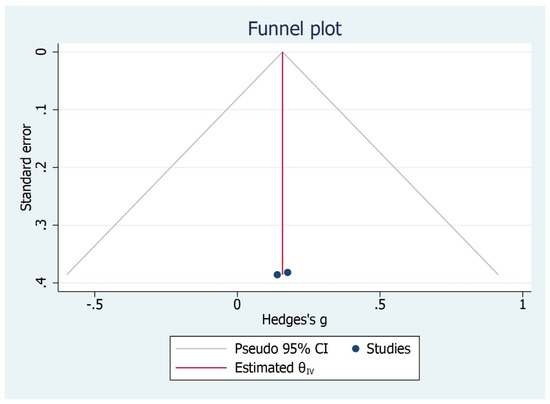
Figure 13.
Publication bias for horizontal angle outcome.
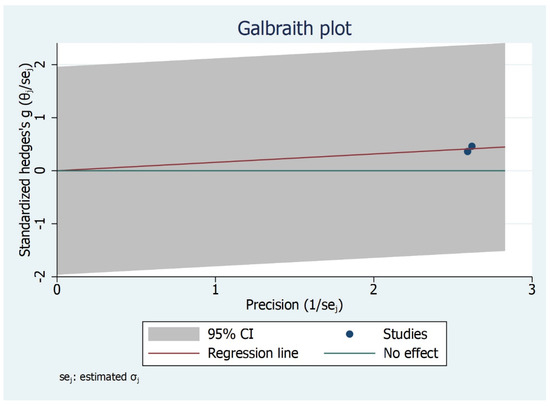
Figure 14.
Galbraith plot for horizontal angle outcome.
3.7. Sagittal Angle
The sagittal angle was assessed in three studies [30,31,32] and reported in degrees. TMD subjects were compared to asymptomatic ones: there was no statistically significant difference between the two groups in sagittal angle outcome favouring TMD which showed lower values (CI 95%, I2 = 78.89%, H2 = 4.74, p = 0.85). The overall effect size was −0.09 degrees [−0.99, 0.82] (Figure 15, Figure 16 and Figure 17).
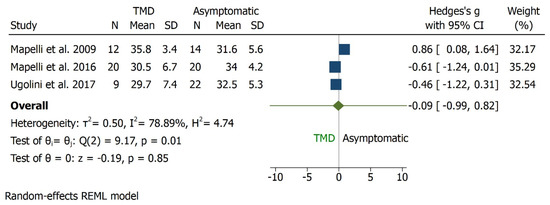
Figure 15.
Forrest plot for sagittal angle outcome.
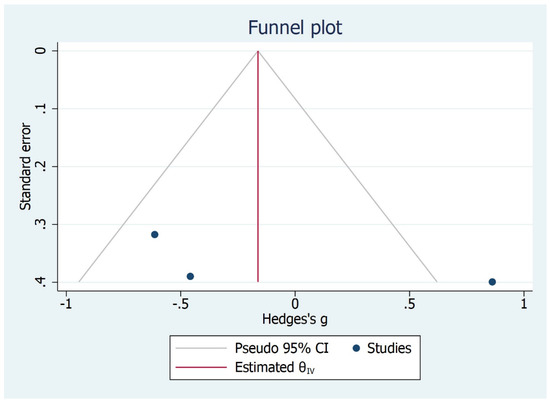
Figure 16.
Funnel plot for sagittal angle outcome.
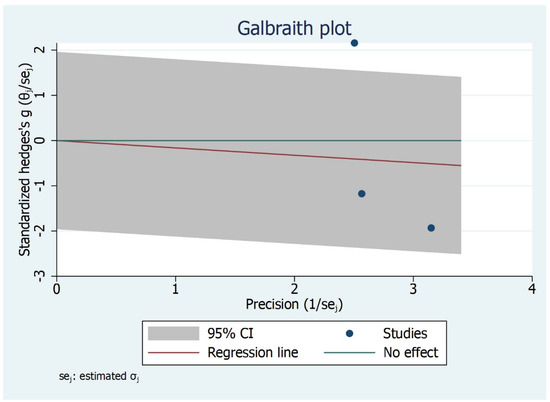
Figure 17.
Galbraith plot for Sagittal angle outcome.
4. Discussion
Mandibular kinematics plays an important role in the evaluation of temporomandibular function. This aspect affects many oral health areas which are connected with the occlusal balance [33] such as prosthodontics, orthodontics and gnathology. The assessment of mandibular movement through condylar rotations and translation represents a cornerstone for TMD diagnosis, in terms of identification and classifying the degree of severity [34]. The quantification of mandibular movements allows both static and dynamic analysis of TMJ, that helps in making informed decisions in clinical setting. This review highlights the use of many arthrokinematic parameters but the absence of an effective gold standard of reference that can help in clinical practice.
Several studies aimed to measure kinematic parameters in order to identify specific values for asymptomatic, TMD [35,36] or surgically treated [37,38,39] subjects, using different diagnostic tools. Therefore, we aimed to determine the efficacy of kinematic in mandibular function assessment in different categories of subjects. A meta-analysis was performed in order to compare the outcome of several studies: only parameters reported with the same unit of measure was analysed. In our review, it was feasible to report few kinematics outcomes such as maximum mouth opening (MMO), horizontal angle, IP-MMO, condylar inclination, sagittal angle, and coronal angle.
Based on the qualitative analysis, we found that very few studies analyse the same parameters with the same units of measure. For example, Condylar inclination was assessed in several papers which considered the angle during opening, laterotrusion and protrusion but only four studies compared the angle during mandible protrusion [24,25,26,40] and among that, only three studies [24,25,26] evaluated condylar inclination during 5 mm of protrusion, involving 380 participants: 171 males and 209 females. Condylar inclination was higher in females than males and in younger than older subjects. Although is important to point out that the three studies included in the meta-analysis showed high risk of bias.
MMO was measured in eleven studies [26,27,39,41,42,43,44,45]; among these, eight studies reported MMO in millimetres and eventually only three [26,27,28] studies were included in the meta-analysis because of homogeneity of the participants (189 of which 97 were males and 92 females). Moreover, in this case the studies included showed high risk of bias, so the results must be evaluated with caution.
Linear incisor displacement at MMO (IP-MMO) was reported in four studies [29,30,36,38]. Eventually two [29,30] studies were included in the meta-analysis because of the comparability of the subjects (total participants are 71 of which 17 were male and 54 females) with high risk of bias. The results of the meta-analysis indicate that females display significantly higher values of condylar inclination and maximum mouth opening than males. This means that, the MMO and condylar inclination among females is more pronounced than males in TMD. Asymptomatic subjects present increased values regarding IP-MMO and horizontal angle than exposed (surgically treated subjects or with malocclusion) or suffering from TMD.
However, several limitations existed; therefore, the results should be interpreted with caution. First, the large panel of the existing arthrokinematics parameters and units of measure adopted by the different studies, which make difficult to compare clinical data. Second, modifications in head posture and reference point could affect the movement path of the mandible. In the absence of standardisation, this may give rise to a considerable variability. Third, heterogeneities among studies were often observed, which may be caused by differences in study populations and the high number of diagnostic tools that could be used for each study’ purpose. Fourth, the study design: most studies are case series with a higher risk of bias in data interpretation.
This meta-analysis shows that TMJ kinematic parameters are useful for mandibular function assessment in clinical practice, but studies included demonstrated that there is a need for data standardisation and establish a gold standard as a reference point. The current studies have heterogeneity in terms of outcomes and variables included. To improve the methods of strategies, the authors suggest carrying out future well-designed case-control studies to improve the level of evidence. Finally, it would be good if future studies compared the various diagnostic methods using the same parameters and units of measurement in order to be able to compare more data more reliably.
5. Conclusions
We concluded that, there is high heterogeneity among the majority of the outcomes except condylar inclination. Considering this factor, the interpretation should be done with caution and take a meaning full message that, the kinematic parameters are an important and useful tool for TMJ evaluation, both to evaluate function and dysfunction. There is a need of well-designed case-control or cohort studies that can add further evidence. The present review suggests standardising outcomes, study design, type of diagnostic devices used to assess the kinametics and population selection in the future studies. This would improve and add reliable and repeatable values.
6. Recommendations
- A well-designed case-control studies would be beneficial in order to increase the level of evidence on the clinical significance of kinematics;
- The literature in the present review demonstrated varying diagnostic tools and measurements for different outcomes. It would be beneficial if the different diagnostic tools are used along with a standard of care;
- The present review highlighted different outcome measures and it would benefit if the case-control studies with MMO outcome as standard method would be measured along with the different outcomes which can have similar dimensions or unit of measurement;
- There are varying groups compared in the studies highlighted within this review. Comparing the groups that include, the TMD and the pre-surgical, post-surgical would bridge the gap in the evidence;
- Majority of studies included in this review lack sample size calculations. Therefore, it is highly recommended to use appropriate sample size calculations for respective studies.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/bioengineering9070269/s1, Table S1: Characteristic Table [46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113].
Author Contributions
The authors confirm contribution toward study conception and design: A.S., S.K., M.D.F., G.M.T.; Data collection: A.S.; Analysis and interpretation of results: A.S., S.K., M.D.F., G.M.T., P.M.R., F.F., F.A., A.M., C.G.; Draft manuscript preparation: A.S., S.K., M.D.F., G.M.T., P.M.R., F.F., F.A., A.M., C.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data is from previous published studies. Hence, not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Okeson, J.P. Management of Temporomandibular Disorders and Occlusion, 7th ed.; Elsevier: Mosby, MO, USA; Louis, MO, USA, 2012. [Google Scholar]
- Reisine, S.T.; Weber, J. The effects of temporomandibular joint disorders on patients’ quality of life. Community Dent. Health 1989, 6, 257–270. [Google Scholar] [PubMed]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations of the international RDC/TMD consortium network and orofacial pain special interest group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Steinkeler, A. Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent. Clin. N. Am. 2013, 57, 465–479. [Google Scholar] [CrossRef] [PubMed]
- Peck, C.C.; Goulet, J.-P.; Lobbezoo, F.; Schiffman, E.L.; Alstergren, P.; Anderson, G.C.; de Leeuw, R.; Jensen, R.; Michelotti, A.; Ohrbach, R.; et al. Expanding the taxonomy of the diagnostic criteria for temporomandibular disorders. J. Oral Rehabil. 2014, 41, 2e23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koolstra, J.H. Dynamics of the human masticatory system. Crit. Rev. Oral Biol. Med. 2002, 13, 366e76. [Google Scholar] [CrossRef] [Green Version]
- Soboleva, U.; Laurina, L.; Slaidina, A. Jaw tracking devices-historical review of methods development, Part II. Stomatologija 2005, 7, 72–76. [Google Scholar]
- De Bont, L.G.; Stegenga, B. Pathology of temporomandibular joint internal derangement and osteoarthritis. Int. J. Oral Maxillofac. Surg. 1993, 22, 71–74. [Google Scholar] [CrossRef]
- Ferrillo, M.; Ammendolia, A.; Paduano, S.; Calafiore, D.; Marotta, N.; Migliario, M.; Fortunato, L.; Giudice, A.; Michelotti, A.; De Sire, A. Efficacy of rehabilitation on reducing pain in muscle-related temporomandibular disorders: A systematic review and meta-analysis of randomized controlled trials. J. Back Musculoskelet. Rehabil. in press. 2022, 1–16. [Google Scholar] [CrossRef]
- Deregibus, A.; Ferrillo, M.; Piancino, M.; Domini, M.; De Sire, A.; Castroflorio, T. Are occlusal splints effective in reducing myofascial pain in patients with muscle-related temporomandibular disorders? A randomized-controlled trial. Turk. J. Phys. Med. Rehabil. 2021, 67, 32–40. [Google Scholar] [CrossRef]
- De Sire, A.; Marotta, M.; Ferrillo, M.; Agostini, F.; Sconza, C.; Lippi, L.; Respizzi, S.; Giudice, A.; Invernizzi, M.; Ammendolia, A. Oxygen-Ozone Therapy for Reducing Pro-Inflammatory Cytokines Serum Levels in Musculoskeletal and Temporomandibular Disorders: A Comprehensive Review. Int. J. Mol. Sci. 2022, 23, 2528. [Google Scholar] [CrossRef]
- Bando, E.; Nishigawa, K.; Nakano, M.; Takeuchi, H.; Shigemoto, S.; Okura, K.; Satsuma, T.; Yamamoto, T. Currentstatus of researches on jaw movement and occlusion for clinical applications. Jpn. Dent. Sci. Rev. 2009, 45, 83–97. [Google Scholar] [CrossRef] [Green Version]
- Chen, C.-C.; Lin, C.-C.; Hsieh, H.-P.; Fu, Y.-C.; Chen, Y.-J.; Lu, T.-W. In vivo three-dimensional mandibular kinematics and functional point trajectories during temporomandibular activities using 3d fluoroscopy. Dentomaxillofacial Radiol. 2021, 50, 20190464. [Google Scholar] [CrossRef] [PubMed]
- Woodford, S.C.; Robinson, D.L.; Mehl, A.; Lee, P.V.S.; Ackland, D.C. Measurement of normal and pathological mandibular and temporomandibular joint kinematics: A systematic review. J. Biomech. 2020, 111, 109994. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematics review and meta-analyses: The PRISMA statement. BMJ Br. Med. J. 2009, 339, 332–336. [Google Scholar] [CrossRef] [Green Version]
- Ryan, R.; Cochrane Consumers and Communication Review Group. Cochrane Consumers and Communication Group: Meta-analysis. Available online: http://cccrg.cochrane.org (accessed on 10 December 2016).
- Pearson, A.; Wiechula, R.; Court, A.; Lockwood, C. The JBI model of evidence-based healthcare. Int. J. Evid. Based Healthc. 2005, 3, 207–215. [Google Scholar]
- Placko, G.; Bellot-Samson, V.; Brunet, S.; Guyot, L.; Richard, O.; Cheynet, F.; Chossegros, C.; Ouaknine, M. Normal mouth opening in the adult French population. Rev. Stomatol. Chir. Maxillofac. 2005, 106, 267–271. [Google Scholar] [CrossRef]
- Travell, J. Temporomandibular joint dysfunction. Temporomandibular joint pain referred from muscles of the head and neck. J. Prosthet. Dent. 1960, 10, 745–763. [Google Scholar] [CrossRef]
- Visscher, C.M.; Huddleston Slater, J.J.R.; Lobbezoo, F.; Naeije, M. Kinematics of the human mandible for different head postures. J. Oral Rehabil. 2000, 27, 299–305. [Google Scholar] [CrossRef]
- Rieder, C.E. Maximum mandibular opening in patients with and without a history of temporomandibular dysfunction. J. Prosthet. Dent. 1978, 39, 441–446. [Google Scholar] [CrossRef]
- Ferrario, V.F.; Sforza, C.; Miani, A.; D’Addona, A.; Tartaglia, G. Statistical evaluation of some mandibular reference positions in normal young people. Int. J. Prosthodont. 1992, 5, 158–165. [Google Scholar]
- Tsolka, P.; Fenlon, M.R.; McCullock, A.J.; Preiskel, H.W. A controlled clinical, electromyographic, and kinesiographic assessment of craniomandibular disorders in women. J. Orofac. Pain 1994, 8, 80–89. [Google Scholar] [PubMed]
- Wieckiewicz, M.; Zietek, M.; Nowakowska, D.; Wieckiewicz, W. Comparison of selected kinematic facebows applied to mandibular tracing. Biomed. Res. Int. 2014, 2014, 818694. [Google Scholar] [CrossRef] [PubMed]
- Baqaien, M.A.; Al-Salti, F.M.; Muessig, D. Changes in condylar path inclination during maximum protrusion between the ages of 6 and 12 years. J. Oral Rehabil. 2007, 34, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Reicheneder, C.; Kardari, Z.; Proff, P.; Fanghaenel, J.; Faltermeier, A.; Römer, P. Correlation of condylar kinematics in children with gender, facial type and weight. Ann. Anat. 2013, 195, 243–247. [Google Scholar] [CrossRef]
- Ferrario, V.F.; Sforza, C.; Lovecchio, N.; Mian, F. Quantification of translational and gliding components in human temporomandibular joint during mouth opening. Arch. Oral Biol. 2005, 50, 507–515. [Google Scholar] [CrossRef]
- Gallo, L.M.; Airoldi, G.B.; Airoldi, R.L.; Palla, S. Description of mandibular finite helical axis pathways in asymptomatic subjects. J. Dent. Res. 1997, 76, 704–713. [Google Scholar] [CrossRef]
- Mapelli, A.; Machado, B.C.Z.; Garcia, D.M.; Rodrigues Da Silva, M.A.M.; Sforza, C.; DeFelicio, C.M. Three-dimensional analysis of jaw kinematic alterations in patients with chronic TMD—Disc displacement with reduction. J. Oral Rehabil. 2016, 43, 824–832. [Google Scholar] [CrossRef]
- Ugolini, A.; Mapelli, A.; Segu, M.; Zago, M.; Codari, M.; Sforza, C. Three dimensional mandibular motion in skeletal Class III patients. CRANIO J. Craniomandib. Sleep Pract. 2018, 36, 113–120. [Google Scholar] [CrossRef]
- Mapelli, A.; Galante, D.; Lovecchio, N.; Sforza, C.; Ferrario, V.F. Translation and rotation movements of the mandible during mouth opening and closing. Clin. Anat. 2009, 22, 311–318. [Google Scholar] [CrossRef]
- Tamaki, K.; Celar, A.G.; Beyrer, S.; Aoki, H. Reproduction of excursive tooth contact in an articulator with computerized axiography data. J. Prosthet. Dent. 1997, 78, 373–378. [Google Scholar] [CrossRef]
- Leissner, O.; Maulén-Yáñez, M.; Meeder-Bella, W.; León-Morales, C.; Vergara-Bruna, E.; González-Arriagada, W.A. Assessment of mandibular kinematics values and its relevance for the diagnosis of temporomandibular joint disorders. J. Dent. Sci. 2021, 16, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Jordan, Z.; Lockwood, C.; Munn, Z.; Aromataris, E. The updated Joanna Briggs Institute model of evidence-based healthcare. JBI Evid. Implement. 2019, 17, 58–71. [Google Scholar] [CrossRef] [PubMed]
- Leader, J.K.; Boston, J.R.; Rudy, T.E.; Greco, C.M.; Zaki, H.S. Relation of jaw sounds and kinematics visualized and quantified using 3-D computer animation. Med. Eng. Phys. 2003, 25, 191–200. [Google Scholar] [CrossRef]
- De Felicio, C.M.; Mapelli, A.; Sidequersky, F.V.; Tartaglia, G.M.; Sforza, C. Mandibular kinematics and masticatory muscles EMG in patients with short lasting TMD of mild-moderate severity. J. Electromyogr. Kinesiol. 2013, 23, 627–633. [Google Scholar] [CrossRef]
- Sforza, C.; Ugolini, A.; Rocchetta, D.; Galante, D.; Mapelli, A.; Giannì, A.B. Mandibular kinematics after orthognathic surgical treatment. A pilot study. Br. J. Oral Maxillofac. Surg. 2010, 48, 110–114. [Google Scholar] [CrossRef]
- Ugolini, A.; Mapelli, A.; Segu, M.; Galante, D.; Sidequersky, F.V.; Sforza, C. Kinematic analysis of mandibular motion before and after orthognathic surgery for skeletal Class III malocclusion: A pilot study. CRANIO J. Craniomandib. Sleep Pract. 2017, 35, 94–100. [Google Scholar] [CrossRef]
- Linsen, S.S.; Schön, A.; Mercuri, L.G.; Teschke, M. Unilateral, Alloplastic Temporomandibular Joint Reconstruction, Biomechanically What Happens to the Contralateral Joint? A Prospective Cohort Study. J. Oral Maxillofac. Surg. 2021, 79, 2016–2029. [Google Scholar] [CrossRef]
- Hüe, O. Condylar paths during protrusion in edentulous patients: Analysis with electronic axiography. J. Prosthodont. 2011, 20, 294–298. [Google Scholar] [CrossRef]
- Ko, E.W.-C.; Huang, C.S.; Lo, L.-J.; Chen, Y.-R. Longitudinal observation of mandibular motion pattern in patients with skeletal class III malocclusion subsequent to orthognathic surgery. J. Oral Maxillofac. Surg. 2012, 70, e158–e168. [Google Scholar]
- Linsen, S.S.; Wolf, M.; Mussig, D. Long-term outcomes of mandibular kinematics following class II malocclusion therapy with removable functional appliance therapy. CRANIO J. Craniomandib. Sleep Pract. 2016, 34, 363–370. [Google Scholar] [CrossRef]
- Coutant, J.-C.; Mesnard, M.; Morlier, J.; Ballu, A.; Cid, M. Discrimination of objective kinematic characters in temporomandibular joint displacements. Arch. Oral Biol. 2008, 53, 453–461. [Google Scholar] [CrossRef] [PubMed]
- Lemoine, J.J.; Xia, J.J.; Gateno, J.; Liebschner, M.A.K. Radiographic analysis for jaw motion normalization. J. Oral Maxillofac. Surg. 2005, 63, 961–967. [Google Scholar] [CrossRef] [PubMed]
- Sforza, C.; Ugolini, A.; Sozzi, D.; Galante, D.; Mapelli, A.; Bozzetti, A. Threedimensional mandibular motion after closed and open reduction of unilateral mandibular condylar process fractures. J. Cranio-Maxillofacial Surg. 2011, 39, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Bernhardt, O.; Küppers, N.; Rosin, M.; Meyer, G. Comparative tests of arbitrary and kinematic transverse horizontal axis recordings of mandibular movements, J. Prosthet. Dent. 2003, 89, 175–179. [Google Scholar] [CrossRef]
- Ghodsi, S.; Rasaeipour, S. Revising average condylar inclinations using electronic pantograph assessment: A cross-sectional study. Dent. Hypotheses. 2018, 9, 84–89. [Google Scholar]
- Hirai, S.; Ogawa, T.; Shigeta, Y.; Ando, E.; Hirabayashi, R.; Ikawa, T.; Kasama, S.; Fukushima, S.; Matsuka, Y. Characteristics of mandibular movements in patients with square mandible. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2009, 108, e75–e81. [Google Scholar] [CrossRef]
- Sadat-Khonsari, R.; Fenske, C.; Kahl-Nieke, B.; Kirsch, I.; Jüde, H.D. Mandibular instantaneous centers of rotation in patients with and without temporomandibular dysfunction. J. Orofac. Orthop. 2003, 64, 256–264. [Google Scholar] [CrossRef]
- Sadat-Khonsari, R.; Fenske, C.; Kahl-Nieke, B.; Kirsch, I.; Jüde, H.D. The helical axis of the mandible during the opening and closing movement of the mouth. J. Orofac. Orthop. 2003, 64, 178–185. [Google Scholar] [CrossRef]
- Kiseri, B.; Dayan, Ç.; Yildiz, M.; Sülün, T. The correlation between direction and amount of retrusive movement and condyle position and joint space. CRANIO J. Craniomandib. Sleep Pract. 2018, 36, 250–256. [Google Scholar] [CrossRef]
- Ko, E.W.-C.; Alazizi, A.I.; Lin, C.-H. Three-dimensional surgical changes of mandibular proximal segments affect outcome of jaw motion analysis. J. Oral Maxillofac. Surg. 2015, 73, 971–984. [Google Scholar]
- Kordaß, B.; Bernhardt, O.; Ratzmann, A.; Hugger, S.; Hugger, A. Standard and limit values of mandibular condylar and incisal movement capacity. Int. J. Comput. Dent. 2014, 17, 9–20. [Google Scholar] [PubMed]
- Ratzmann, A.; Mundt, T.; Schwahn, C.; Langforth, G.; Hützen, D.; Gedrange, T.; Kordaß, B. Comparative clinical investigation of horizontal condylar inclination using the JMA electronic recording system and a protrusive wax record for setting articulators. Int. J. Comput. Dent. 2007, 10, 265–284. [Google Scholar] [PubMed]
- Schwestka-Polly, R.; Kubein-Meesenburg, D.; Nagerl, H.; Fanghanel, J.; Miehe, B. Alteration of the functional condition of the mandible during clinical treatment. Ann. Anat. 1999, 181, 45–50. [Google Scholar] [CrossRef]
- Stiesch-Scholz, M.; Demling, A.; Rossbach, A. Reproducibility of jaw movements in patients with craniomandibular disorders. J. Oral Rehabil. 2006, 33, 807–812. [Google Scholar] [CrossRef] [PubMed]
- Teng, T.T.-Y.; Ko, E.W.-C.; Huang, C.S.; Chen, Y.-R. The Effect of early physiotherapy on the recovery of mandibular function after orthognathic surgery for Class III correction: Part I - Jaw-motion analysis. J. Cranio-Maxillofacial Surg. 2015, 43, 131–137. [Google Scholar] [CrossRef]
- Wang, D.; Fu, H.; Zeng, R.; Yang, X. Changes of mandibular movement tracings after the correction of mandibular protrusion by bilateral sagittal split ramus osteotomy. J. Oral Maxillofac. Surg. 2009, 67, 2238–2244. [Google Scholar] [CrossRef]
- Yen, C.-I.; Chou, P.-Y.; Chen, C.-H.; Chen, T.-Y.; Chen, C.-T.; Lin, W.-Y.; Lee, M.-Y. Kinematic, Kinetic and surface electromyography analysis following zygomatic fracture reconstruction. J. Med. Biol. Eng. 2017, 37, 468–473. [Google Scholar] [CrossRef]
- Baeyens, J.P.; Gilomen, H.; Erdmann, B.; Clijsen, R.; Cabri, J.; Vissers, D. In vivo measurement of the 3D kinematics of the temporomandibular joint using miniaturized electromagnetic trackers: Technical report. Med. Biol. Eng. Comput. 2013, 51, 479–484. [Google Scholar] [CrossRef]
- Baltali, E.; Zhao, K.D.; Koff, M.F.; Durmus, E.; An, K.-N.; Keller, E.E. A method for quantifying condylar motion in patients with osteoarthritis using an electromagnetic tracking device and computed tomography imaging. J. Oral Maxillofac. Surg. 2008, 66, 848–857. [Google Scholar] [CrossRef]
- Keller, E.E.; Baltali, E.; Liang, X.; Zhao, K.; Huebner, M.; An, K.-N. Temporomandibular custom hemijoint replacement prosthesis: Prospective clinical and kinematic study. J. Oral Maxillofac. Surg. 2012, 70, 276–288. [Google Scholar] [CrossRef]
- Minami, I.; Wirianski, A.; Harakawa, R.; Wakabayashi, N.; Murray, G.M. The three-axial gyroscope sensor detects the turning point between opening and closing phases of chewing. Clin. Exp. Dent. Res. 2018, 4, 249–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamamoto, T.; Nishigawa, K.; Bando, E.; Hosoki, M. Effect of different head positions on the jaw closing point during tapping movements. J. Oral Rehabil. 2009, 36, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.R.; Han, J.J.; Kim, D.-S.; Yi, W.-J.; Hwang, S.J. Evaluation of intraarticular distance narrowing during tem-poromandibular joint movement in patients with facial asymmetry using 3-dimensional computed tomography image and tracking camera system. J. Cranio-Maxillofacial Surg. 2015, 43, 342–348. [Google Scholar] [CrossRef]
- Ettlin, D.A.; Mang, H.; Colombo, V.; Palla, S.; Gallo, L.M. Stereometric assessment of TMJ space variation by occlusal splints. J. Dent. Res. 2008, 87, 877–881. [Google Scholar] [CrossRef] [PubMed]
- Fushima, K.; Gallo, L.M.; Krebs, M.; Palla, S. Analysis of the TMJ intraarticular space variation: A non-invasive insight during mastication. Med. Eng. Phys. 2003, 25, 181–190. [Google Scholar] [CrossRef]
- Gallo, L.M.; Gössi, D.B.; Colombo, V.; Palla, S. Relationship between kinematic center and TMJ anatomy and function. J. Dent. Res. 2008, 87, 726–730. [Google Scholar] [CrossRef]
- Goto, T.K.; Langenbach, G.E.J.; Hannam, A.G. Length changes in the human masseter muscle after jaw movement. Anat. Rec. 2001, 262, 293–300. [Google Scholar] [CrossRef]
- Hayasaki, H.; Saitoh, I.; Iwase, Y.; Inada, E.; Hasegawa, H.; Tokutomi, J.; Matsumoto, Y.; Yamasaki, Y. Movement of the instantaneous center of rotation and the position of the lateral excursion center during lateral excursion. CRANIO J. Craniomandib. Sleep Pract. 2008, 26, 253–262. [Google Scholar]
- Kim, D.-S.; Choi, S.-C.; Lee, S.-S.; Heo, M.-S.; Huh, K.-H.; Hwang, S.-J.; Kim, S.-H.; Yi, W.-J. Principal direction of inertia for 3D trajectories from patientspecific TMJ movement. Comput. Biol. Med. 2013, 43, 169–175. [Google Scholar] [CrossRef]
- Kim, S.-G.; Kim, D.-S.; Choi, S.-C.; Lee, S.-S.; Heo, M.-S.; Huh, K.-H.; Hwang, S.-J.; Yi, W.-J. The relationship between three-dimensional principal rotations and mandibular deviation. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2010, 110, 52–60. [Google Scholar] [CrossRef]
- Kubota, N.; Hayasaki, H.; Saitoh, I.; Iwase, Y.; Maruyama, T.; Inada, E.; Hasegawa, H.; Yamada, C.; Takemoto, Y.; Matsumoto, Y.; et al. Jaw motion during gum-chewing in children with primary dentition. CRANIO J. Craniomandib. Sleep Pract. 2010, 28, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Wojczynska, A.; Gallo, L.M.; Bredell, M.; Leiggener, C.S. Alterations of mandibular movement patterns after total joint replacement: A case series of long-term outcomes in patients with total alloplastic temporomandibular joint reconstructions. Int. J. Oral Maxillofac. Surg. 2019, 48, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Yashiro, K.; Iwata, A.; Takada, K.; Murakami, S.; Uchiyama, Y.; Furukawa, S. Temporomandibular joint articulations on working side during chewing in adult females with cross-bite and mandibular asymmetry. J. Oral Rehabil. 2015, 42, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Yashiro, K.; Yamamoto, K.; Takada, K.; Murakami, S.; Uchiyama, Y.; Furukawa, S. Influence of balancing-side occlusal interference on smoothness of working-side condylar movement and intra-articular space in chewing efforts. J. Oral Rehabil. 2015, 42, 10–17. [Google Scholar] [CrossRef]
- Zaugg, B.; Hämmerle, C.H.F.; Palla, S.; Gallo, L.M. Implant-supported mandibular splinting affects temporomandibular joint biomechanics. Clin. Oral Implants Res. 2012, 23, 897–901. [Google Scholar] [CrossRef]
- Abbink, J.H.; Van Der Bilt, A.; Bosman, F.; Van Der Glas, H.W. Speed-dependent control of cyclic open-close movements of the human jaw with an externalforce counteracting closing. J. Dent. Res. 1999, 78, 878–886. [Google Scholar] [CrossRef]
- Amhamed, M.; Whittle, T.; Maulina, T.; Gal, J.; Akhter, R.; Murray, G.M. Effect of experimental anterior temporalis muscle pain on jaw movements. J. Oral Rehabil. 2016, 43, 889–899. [Google Scholar] [CrossRef]
- Bhaskaracharya, M.; Memon, S.M.; Whittle, T.; Murray, G.M. Jaw movements in patients with a history of pain: An exploratory study. J. Oral Rehabil. 2015, 42, 18–26. [Google Scholar] [CrossRef]
- Buschang, P.H.; Throckmorton, G.S.; Travers, K.H.; Hayasaki, H. Incisor and mandibular condylar movements of young adult females during maximum protrusion and lateratrusion of the jaw. Arch. Oral Biol. 2001, 46, 39–48. [Google Scholar] [CrossRef]
- Buschang, P.H.; Hayasaki, H.; Throckmorton, G.S. Quantification of human chewing-cycle kinematics. Arch. Oral Biol. 2000, 45, 461–474. [Google Scholar] [CrossRef]
- Calixtre, L.B.; Nakagawa, T.H.; Alburquerque-Sendin, F.; da Silva Gruninger, B.L.; de Sena Rosa, L.R.; Oliveira, A.B. Inter- and intra-rater reliability of 3D kinematics during maximum mouth opening of asymptomatic subjects. J. Biomech. 2017, 64, 245–252. [Google Scholar] [CrossRef] [PubMed]
- C´atic, A.; Naeije, M. Location of the hinge axis and the kinematic centre in asymptomatic and clicking temporo-mandibular joints. J. Oral Rehabil. 1999, 26, 661–665. [Google Scholar] [CrossRef] [PubMed]
- Crane, E.A.; Rothman, E.D.; Childers, D.; Gerstner, G.E. Analysis of temporal variation in human masticatory cycles during gum chewing. Arch. Oral Biol. 2013, 58, 1464–1474. [Google Scholar] [CrossRef] [PubMed]
- Gallo, L.M.; Fushima, K.; Palla, S. Mandibular helical axis pathways during mastication. J. Dent. Res. 2000, 79, 1566–1572. [Google Scholar] [CrossRef] [PubMed]
- Gallo, L.M.; Brasi, M.; Ernst, B.; Palla, S. Relevance of mandibular helical axis analysis in functional and dysfunctional TMJs. J. Biomech. 2006, 39, 1716–1725. [Google Scholar] [CrossRef]
- Gerstner, G.E.; Lafia, C.; Lin, D. Predicting masticatory jaw movements from chin movements using multivariate linear methods. J. Biomech. 2005, 38, 1991–1999. [Google Scholar] [CrossRef]
- Hayashi, K.; Reich, B.; Delong, R.; Lee, S.-P.; Mizoguchi, I. A novel statistical model for mandibular helical axis analysis. J. Oral Rehabil. 2009, 36, 102–109. [Google Scholar] [CrossRef]
- Hayashi, K.; Hayashi, M.; Reich, B.; Lee, S.-P.; Sachdeva, A.U.C.; Mizoguchi, I. Functional data analysis of mandibular movement using third-degree b-spline basis functions and self-modeling regression. Orthod. Waves. 2012, 71, 17–25. [Google Scholar] [CrossRef]
- Leader, J.K.; Boston, J.R.; Rudy, T.E.; Greco, C.M.; Zaki, H.S. Use of sound and jaw movement patterns to characterize patients with temporomandibulardisorders. Annu. Int. Conf IEEE Eng. Med. Biol. Proc. 1997, 4, 1729–1732. [Google Scholar]
- Lewis, R.P.; Buschang, P.H.; Throckmorton, G.S. Sex differences in mandibular movements during opening and closing. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 294–303. [Google Scholar] [CrossRef]
- Lobbezoo, F.; Zwijnenburg, A.J.; Naeije, M. Functional subdivision of the human masseter and temporalis muscles as shown by the condylar movement response to electrical muscle stimulation. J. Oral Rehabil. 2000, 27, 887–892. [Google Scholar] [CrossRef]
- Naeije, M. Local kinematic and anthropometric factors related to the maximum mouth opening in healthy individuals. J. Oral Rehabil. 2002, 29, 534–539. [Google Scholar] [CrossRef]
- Naeije, M.; Hofman, N. Biomechanics of the human temporomandibular joint during chewing. J. Dent. Res. 2003, 82, 528–531. [Google Scholar] [CrossRef] [PubMed]
- Ostry, D.J.; Vatikiotis-Bateson, E.; Gribble, P.L. An examination of the degrees of freedom of human jaw motion in speech and mastication. J. Speech Lang. Hear. Res. 1997, 40, 1341–1351. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, T.; Koyano, K.; Umemoto, G. Inclination of the occlusal plane and occlusal guidance as contributing factors in mastication. J. Dent. 1998, 26, 641–647. [Google Scholar] [CrossRef]
- Remijn, L.; Groen, B.E.; Speyer, R.; van Limbeek, J.; Vermaire, J.A.; van den Engel-Hoek, L.; Nijhuis-van der Sanden, M.W.G. Can mastication in children with cerebral palsy be analyzed by clinical observation, dynamic ultrasound and 3D kinematics? J. Electromyogr. Kinesiol. 2017, 32, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Sforza, C.; Tartaglia, G.M.; Lovecchio, N.; Ugolini, A.; Monteverdi, R.; Giannì, A.B.; Ferrario, V.F. Mandibular movements at maximum mouth opening and EMG activity of masticatory and neck muscles in patients rehabilitated after a mandibular condyle fracture. J. Cranio-Maxillofacial Surg. 2009, 37, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Shiller, D.M.; Ostry, D.J.; Gribble, P.L. Effects of gravitational load on jaw movements in speech. J. Neurosci. 1999, 19, 9073–9080. [Google Scholar] [CrossRef]
- Shiller, D.M.; Ostry, D.J.; Gribble, P.L.; Laboissière, R. Compensation for the effects of head acceleration on jaw movement in speech. J. Neurosci. 2001, 21, 6447–6456. [Google Scholar] [CrossRef] [Green Version]
- Siegler, S.; Hayes, R.; Nicolella, D.; Fielding, A. A technique to investigate the three-dimensional kinesiology of the human temporomandibular joint. J. Prosthet. Dent. 1991, 65, 833–839. [Google Scholar] [CrossRef]
- Slater, J.; Visscher, C.M.; Lobbezoo, F.; Naeije, M. The intra-articular distance within the TMJ during free and loaded closing movements. J. Dent. Res. 1999, 78, 1815–1820. [Google Scholar] [CrossRef] [PubMed]
- Tomonari, H.; Kwon, S.; Kuninori, T.; Miyawaki, S. Differences between the chewing and non-chewing sides of the mandibular first molars and condyles in the closing phase during chewing in normal subjects. Arch. Oral Biol. 2017, 81, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Travers, K.H.; Buschang, P.H.; Hayasaki, H.; Throckmorton, G.S. Associations between incisor and mandibular condylar movements during maximum mouth opening in humans. Arch. Oral Biol. 2000, 45, 267–275. [Google Scholar] [CrossRef]
- Zhao, N.N.; Whittle, T.; Murray, G.M.; Peck, C.C. The effects of capsaicin induced intraoral mucosal pain on jaw movements in humans. J. Oral Facial Pain Headache. 2012, 26, 277–287. [Google Scholar]
- Dos Santos, D.M.; Lucareli, P.R.; Borges Barbosa, B.R.; Alves de Azevedo, L.M.; Leonardis, M.N.; Fonseca, F.F.; de Carvalho, L.S.; Gonzalez, T.D.O.; Politti, F.; Biasotto-Gonzalez, D.A. Reproducibility of a three-dimensional jaw model during opening and lateral excursion tests. Gait Posture. 2019, 73, 529–530. [Google Scholar]
- Dos Santos, D.M.; Politti, F.; de Azevedo, L.M.A.; de Cassia das Neves Martins, R.; Ricci, F.C.; Masuda, K.S.Y.; Muramoto do Nascimento, E.M.; Spinato, I.L.; de Paula Gomes, C.A.F.; Biasotto-Gonzalez, D.A. Association between convergence insufficiency and temporomandibular disorder cross-sectional study. Clin. Oral Investigations. 2021, 25, 851–858. [Google Scholar] [CrossRef]
- Ernst, M.; Schenkenberger, A.E.; Domin, M.; Kordass, B.; Lotze, M. Effects of centric mandibular splint therapy on orofacial pain and cerebral activation patterns. Clin. Oral Investigations. 2020, 24, 2005–2013. [Google Scholar] [CrossRef]
- Choi, D.D.; Vandenberg, K.; Smith, D.; Davis, C.; McCain, J.P. Is Temporomandibular Joint Arthroscopy Effective in Managing Pediatric Temporomandibular Joint Disorders in the Short- and Long-Term? J. Oral Maxillofac Surg. 2020, 78, 44–51. [Google Scholar] [CrossRef]
- Feng, Y.; Shu, J.; Liu, Y.; Zheng, T.; Shao, B.; Liu, Z. Biomechanical analysis of temporomandibular joints during mandibular pro-trusion and retraction motions: A 3d finite element simulation. Comput. Methods Programs Biomed. 2021, 208, 106299. [Google Scholar] [CrossRef]
- Shu, J.; Ma, H.; Jia, L.; Fang, H.; Chong, D.Y.R.; Zheng, T.; Yao, J.; Liu, Z. Biomechanical behaviour of temporomandibular joints during opening and closing of the mouth: A 3D finite element analysis. Int. J. Numer. Methods Biomed. Eng. 2020, 8, e3373. [Google Scholar] [CrossRef]
- Shu, J.; Ma, H.; Xiong, X.; Shao, B.; Zheng, T.; Liu, Y.; Liu, Z. Mathematical analysis of the condylar trajectories in asymptomatic subjects during mandibular motions. Med. Biol. Eng. Comput. 2021, 59, 901–911. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).