Artificial Intelligence in Public Health: Bridging Today’s Trends with Tomorrow’s Possibilities
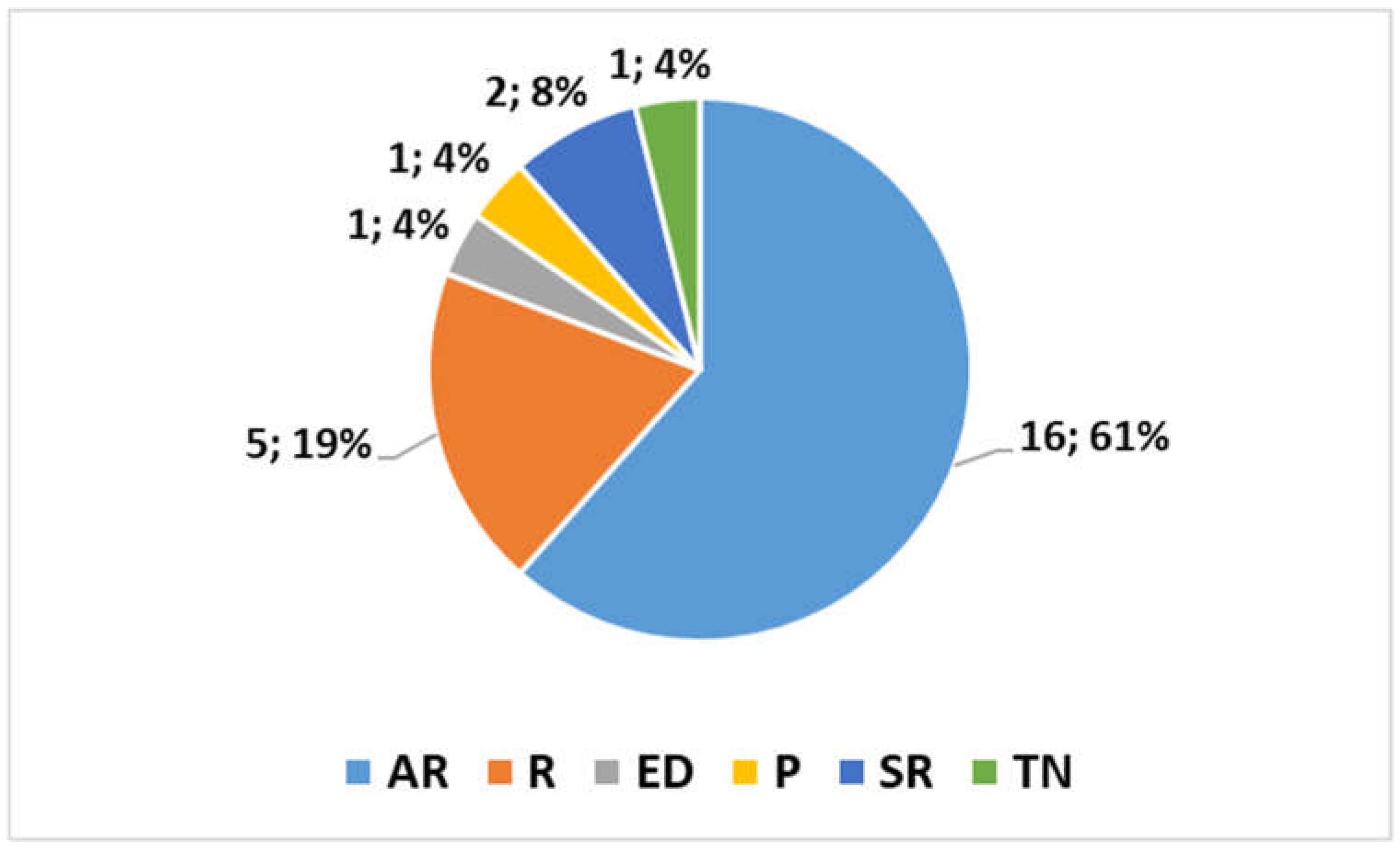
- Contributions of Studies
- Contribution of Review Studies
- Contribution of Other Studies
- Conclusions and message for future work
- Expanding datasets to improve the accuracy and generalizability of AI/ML models across different healthcare populations and settings.
- Developing interdisciplinary frameworks for better integration of AI solutions into clinical contexts, addressing ethical concerns, and ensuring equity.
- Exploring AI’s potential in less-explored areas, such as mental health, long-term disease management, and healthcare logistics.
- Enhancing regulatory frameworks to keep pace with the rapid development of AI/ML technologies, ensuring safe and responsible implementation.
- Promoting the development of user-friendly AI tools that clinicians can adopt without disrupting existing workflows.
Conflicts of Interest
References
- Wang, L.; Zhang, Y.; Wang, D.; Tong, X.; Liu, T.; Zhang, S.; Huang, J.; Zhang, L.; Chen, L.; Fan, H.; et al. Artificial Intelligence for COVID-19: A Systematic Review. Front. Med. 2021, 8, 704256. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jemioło, P.; Storman, D.; Orzechowski, P. Artificial Intelligence for COVID-19 Detection in Medical Imaging—Diagnostic Measures and Wasting—A Systematic Umbrella Review. J. Clin. Med. 2022, 11, 2054. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, S.; SeyedAlinaghi, S.; Heydari, M.; Pashaei, Z.; Mirzapour, P.; Karimi, A.; Afsahi, A.M.; Mirghaderi, P.; Mohammadi, P.; Arjmand, G.; et al. Artificial Intelligence in COVID-19 Management: A Systematic Review. J. Comput. Sci. 2023, 19, 554–568. [Google Scholar] [CrossRef]
- Jiang, L.; Wu, Z.; Xu, X.; Zhan, Y.; Jin, X.; Wang, L.; Qiu, Y. Opportunities and challenges of artificial intelligence in the medical field: Current application, emerging problems, and problem-solving strategies. J. Int. Med. Res. 2021, 49, 3000605211000157. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gawande, M.S.; Zade, N.; Kumar, P.; Gundewar, S.; Weerarathna, I.N.; Verma, P. The role of artificial intelligence in pandemic responses: From epidemiological modeling to vaccine development. Mol. Biomed. 2025, 3, 1. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Channa, A.; Popescu, N.; Skibinska, J.; Burget, R. The Rise of Wearable Devices during the COVID-19 Pandemic: A Systematic Review. Sensors 2021, 21, 5787. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alsunaidi, S.J.; Almuhaideb, A.M.; Ibrahim, N.M.; Shaikh, F.S.; Alqudaihi, K.S.; Alhaidari, F.A.; Khan, I.U.; Aslam, N.; Alshahrani, M.S. Applications of Big Data Analytics to Control COVID-19 Pandemic. Sensors 2021, 21, 2282. [Google Scholar] [CrossRef]
- Chang, Z.; Zhan, Z.; Zhao, Z.; You, Z.; Liu, Y.; Yan, Z.; Fu, Y.; Liang, W.; Zhao, L. Application of artificial intelligence in COVID-19 medical area: A systematic review. J. Thorac. Dis. 2021, 13, 7034–7053. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nawaz, F.A.; Khan, A.R.; Boillat, T. AI-enhanced solutions during COVID-19: Current trends and future innovations. Ann. Med. Surg. 2022, 80, 104158. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Artificial Intelligence in Public Health: Current Trends and Future Possibilities. Topic. 2024. Available online: https://www.mdpi.com/topics/C52Z967WA3 (accessed on 20 March 2025).
- Baligh Jahromi, A.; Attarian, K.; Asgary, A.; Wu, J. Advancing Indoor Epidemiological Surveillance: Integrating Real-Time Object Detection and Spatial Analysis for Precise Contact Rate Analysis and Enhanced Public Health Strategies. Int. J. Environ. Res. Public. Health 2024, 21, 1502. [Google Scholar] [CrossRef]
- Yang, Y.; Ning, H.; Liang, B.; Mai, H.; Zhou, J.; Yang, J.; Huang, J. Exploring Factors Influencing Patient Delay Behavior in Oral Cancer: The Development of a Risk Prediction Model in Western China. Healthcare 2024, 12, 2252. [Google Scholar] [CrossRef] [PubMed]
- Jawad, B.N.; Altintas, I.; Eugen-Olsen, J.; Niazi, S.; Mansouri, A.; Rasmussen, L.J.H.; Schultz, M.; Iversen, K.; Normann Holm, N.; Kallemose, T.; et al. Prospective and External Validation of Machine Learning Models for Short- and Long-Term Mortality in Acutely Admitted Patients Using Blood Tests. J. Clin. Med. 2024, 13, 6437. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Xie, H.; Gu, L.; Chen, R.; Chen, S.; Wang, F.; Liu, Y.; Chen, L.; Tang, J. Advancing Mental Health Care: Intelligent Assessments and Automated Generation of Personalized Advice via M.I.N.I and RoBERTa. Appl. Sci. 2024, 14, 9447. [Google Scholar] [CrossRef]
- Kwiatkowska-Miernik, A.; Wasilewski, P.G.; Mruk, B.; Sklinda, K.; Bujko, M.; Walecki, J. Estimating Progression-Free Survival in Patients with Primary High-Grade Glioma Using Machine Learning. J. Clin. Med. 2024, 13, 6172. [Google Scholar] [CrossRef]
- Ganatra, H.A.; Latifi, S.Q.; Baloglu, O. Pediatric Intensive Care Unit Length of Stay Prediction by Machine Learning. Bioengineering 2024, 11, 962. [Google Scholar] [CrossRef]
- Vichare, S.; Nanda, G.; Sundararajan, R. Probabilistic Ensemble Framework for Injury Narrative Classification. AI 2024, 5, 1684–1694. [Google Scholar] [CrossRef]
- Sheehy, L.; Bouchard, S.; Kakkar, A.; El Hakim, R.; Lhoest, J.; Frank, A. Development and Initial Testing of an Artificial Intelligence-Based Virtual Reality Companion for People Living with Dementia in Long-Term Care. J. Clin. Med. 2024, 13, 5574. [Google Scholar] [CrossRef] [PubMed]
- Messova, A.; Pivina, L.; Ygiyeva, D.; Batenova, G.; Dyussupov, A.; Jamedinova, U.; Syzdykbayev, M.; Adilgozhina, S.; Bayanbaev, A. Lessons of the COVID-19 Pandemic for Ambulance Service in Kazakhstan. Healthcare 2024, 12, 1568. [Google Scholar] [CrossRef]
- Guimaraes, G.R.; Figueiredo, R.G.; Silva, C.S.; Arata, V.; Contreras, J.C.Z.; Gomes, C.M.; Tiraboschi, R.B.; Bessa Junior, J. Diagnosis in Bytes: Comparing the Diagnostic Accuracy of Google and ChatGPT 3.5 as an Educational Support Tool. Int. J. Environ. Res. Public. Health 2024, 21, 580. [Google Scholar] [CrossRef]
- Ciarmiello, A.; Giovannini, E.; Tutino, F.; Yosifov, N.; Milano, A.; Florimonte, L.; Bonatto, E.; Bareggi, C.; Dellavedova, L.; Castello, A.; et al. Does FDG PET-Based Radiomics Have an Added Value for Prediction of Overall Survival in Non-Small Cell Lung Cancer? J. Clin. Med. 2024, 13, 2613. [Google Scholar] [CrossRef]
- Saeed, Z.; Bouhali, O.; Ji, J.X.; Hammoud, R.; Al-Hammadi, N.; Aouadi, S.; Torfeh, T. Cancerous and Non-Cancerous MRI Classification Using Dual DCNN Approach. Bioengineering 2024, 11, 410. [Google Scholar] [CrossRef] [PubMed]
- Miyagi, Y.; Tada, K.; Yasuhi, I.; Tsumura, K.; Maegawa, Y.; Tanaka, N.; Mizunoe, T.; Emoto, I.; Maeda, K.; Kawakami, K.; et al. A Novel Method for Determining Fibrin/Fibrinogen Degradation Products and Fibrinogen Threshold Criteria via Artificial Intelligence in Massive Hemorrhage during Delivery with Hematuria. J. Clin. Med. 2024, 13, 1826. [Google Scholar] [CrossRef] [PubMed]
- Bhimavarapu, U.; Chintalapudi, N.; Battineni, G. Brain Tumor Detection and Categorization with Segmentation of Improved Unsupervised Clustering Approach and Machine Learning Classifier. Bioengineering 2024, 11, 266. [Google Scholar] [CrossRef] [PubMed]
- Jungwirth, D.; Haluza, D. Artificial Intelligence and Public Health: An Exploratory Study. Int. J. Environ. Res. Public. Health 2023, 20, 4541. [Google Scholar] [CrossRef] [PubMed]
- He, T.; Liu, H.; Zhang, Z.; Li, C.; Zhou, Y. Research on the Application of Artificial Intelligence in Public Health Management: Leveraging Artificial Intelligence to Improve COVID-19 CT Image Diagnosis. Int. J. Environ. Res. Public. Health 2023, 20, 1158. [Google Scholar] [CrossRef]
- Giansanti, D. AI in Cytopathology: A Narrative Umbrella Review on Innovations, Challenges, and Future Directions. J. Clin. Med. 2024, 13, 6745. [Google Scholar] [CrossRef]
- Michelutti, L.; Tel, A.; Zeppieri, M.; Ius, T.; Agosti, E.; Sembronio, S.; Robiony, M. Generative Adversarial Networks (GANs) in the Field of Head and Neck Surgery: Current Evidence and Prospects for the Future—A Systematic Review. J. Clin. Med. 2024, 13, 3556. [Google Scholar] [CrossRef]
- Lepri, G.; Oddi, F.; Gulino, R.A.; Giansanti, D. Reimagining Radiology: A Comprehensive Overview of Reviews at the Intersection of Mobile and Domiciliary Radiology over the Last Five Years. Bioengineering 2024, 11, 216. [Google Scholar] [CrossRef]
- Kim, H.-K. The Effects of Artificial Intelligence Chatbots on Women’s Health: A Systematic Review and Meta-Analysis. Healthcare 2024, 12, 534. [Google Scholar] [CrossRef]
- Gala, D.; Makaryus, A.N. The Utility of Language Models in Cardiology: A Narrative Review of the Benefits and Concerns of ChatGPT-4. Int. J. Environ. Res. Public Health 2023, 20, 6438. [Google Scholar] [CrossRef]
- Giansanti, D. The Artificial Intelligence in Teledermatology: A Narrative Review on Opportunities, Perspectives, and Bottlenecks. Int. J. Environ. Res. Public Health 2023, 20, 5810. [Google Scholar] [CrossRef] [PubMed]
- Hui, V.; Constantino, R.E.; Lee, Y.J. Harnessing Machine Learning in Tackling Domestic Violence—An Integrative Review. Int. J. Environ. Res. Public Health 2023, 20, 4984. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, A.A.A. Machine Learning for Predicting Neutron Effective Dose. Appl. Sci. 2024, 14, 5740. [Google Scholar] [CrossRef]
- Pasini, A.; Amendola, S. A Neural Modelling Tool for Non-Linear Influence Analyses and Perspectives of Applications in Medical Research. Appl. Sci. 2024, 14, 2148. [Google Scholar] [CrossRef]
- Giansanti, D. Artificial Intelligence in Public Health: Current Trends and Future Possibilities. Int. J. Environ. Res. Public Health 2022, 19, 11907. [Google Scholar] [CrossRef]
| Study | Focus | Brief Summary | Contribution |
|---|---|---|---|
| [11] | Indoor transmission of respiratory diseases and real-time contact rate analysis | This study addresses the increasing concern about airborne diseases spreading in indoor spaces, particularly in settings like offices, schools, and hospitals. It introduces an advanced software tool powered by YOLOv8, a state-of-the-art deep learning model, to accurately detect and track individuals from video streams. The tool uses dynamic circular buffer zones and a 2D projective transformation to overlay digital coordinates of the physical environment, visualizing heatmaps of spatial contact patterns and quantifying contact events. This method provides a more precise and automated alternative to traditional manual contact tracing and counting techniques. | This study introduces a transformative shift in public health surveillance by integrating real-time tracking and AI to model disease transmission more accurately and efficiently. The system’s ability to offer precise, dynamic tracking within enclosed spaces will significantly enhance epidemiological studies, improve the management of disease outbreaks, and provide public health officials with a robust tool to develop non-pharmaceutical interventions based on real-time, spatially detailed data. |
| [12] | Delayed medical treatment behavior in oral cancer patients in Western China and machine learning for prediction | This research investigates the social, economic, and health factors contributing to delays in seeking medical treatment among oral cancer patients in Western China. A combination of logistic regression and machine learning models (such as nearest neighbors, SVM, and random forest) is applied to identify key risk factors and predict the likelihood of delayed treatment. This study compares the behavior of patients before and after the lifting of COVID-19 restrictions, offering insights into the pandemic’s impact on medical delays. | This study provides a unique and large-scale analysis of delayed treatment behavior, with a focus on how family dynamics, social support, and external factors like the pandemic influence patients’ decision-making. By developing a predictive model, it offers valuable insights into healthcare policies and early intervention strategies, especially in regions with limited healthcare access. It underscores the importance of social support, highlighting the role of family structures in reducing treatment delays and potentially improving outcomes. |
| [13] | Short- and long-term mortality prediction in emergency department patients using clinical data | This study focuses on creating predictive models for mortality risks in patients admitted to emergency departments (EDs) by using minimal, routine clinical data—specifically, blood biochemistry results from a single admission sample. This study uses datasets from several large Danish hospitals, applying machine learning models to predict patient mortality within 10, 30, 90, and 365 days post-admission. The goal is to enhance patient triage and prioritization, particularly in settings where timely decisions can save lives. | The contribution lies in proving that routine biochemistry tests, often performed at admission, can be leveraged to accurately predict both short-term and long-term mortality. This study proposes a simplified yet highly effective tool for mortality prediction, which could become an integral part of emergency care workflows, helping clinicians make better decisions regarding patient management and resource allocation in EDs. |
| [14] | AI-assisted mental health evaluation and personalized medical advice generation | This paper proposes an integrated AI system that combines finite state machines, semantic matching algorithms, and medical knowledge graphs to improve mental health assessments. By automating the collection of patient data and conducting preliminary evaluations, the tool optimizes decision-making. It then generates personalized medical advice based on deep learning techniques such as RoBERTa for semantic matching, ensuring accuracy in recommending treatment options. | This study showcases how AI can significantly improve mental healthcare by streamlining the assessment process and providing personalized advice. The integration of AI-driven diagnostics with medical knowledge graphs leads to more accurate recommendations, ensuring efficient use of medical resources. The findings have the potential to reduce the diagnostic burden on mental health professionals and provide a personalized care experience for patients. |
| [15] | Radiomics and AI in predicting progression-free survival in high-grade glioma patients | This study explores the use of radiomics (the extraction of quantitative features from medical images) combined with AI algorithms to predict progression-free survival (PFS) in patients with high-grade gliomas, a type of brain cancer. The research focuses on preoperative MRI scans, analyzing 109 radiomic features along with clinical factors like age, sex, and tumor location to develop predictive models. | This research contributes to personalized oncology by demonstrating how AI models, when integrated with radiomic features, can provide accurate predictions of progression-free survival in glioma patients. These insights can assist in stratifying patients based on their risk of tumor recurrence, potentially guiding tailored treatment plans. The study emphasizes the importance of early prediction in managing high-grade gliomas and improving patient outcomes through more individualized treatment strategies. |
| [16] | Machine learning for predicting length of stay in pediatric intensive care units (PICU) | This study investigates the application of machine learning models to predict the length of stay (LOS) in pediatric intensive care units (PICUs). This research uses data from over 100 North American PICUs, applying algorithms such as support vector machine, Gradient Boosting, and Recurrent Neural Networks (RNNs) to predict patient outcomes at various thresholds (24, 36, 48 h, etc.). The primary goal is to improve resource management and optimize staffing within PICUs. | This study highlights how machine learning can outperform traditional methods of predicting PICU LOS, with models like Gradient Boosting and RNNs achieving higher accuracy and balanced performance. These models provide critical insights that can be used to better allocate resources, optimize staffing, and improve patient care. The findings suggest that further refinement of machine learning models could enhance their applicability in clinical settings, improving operational efficiency in pediatric intensive care units. |
| [17] | Ensemble machine learning models for injury prediction | This study analyzes the use of ensemble machine learning (ML) models to predict injury codes from the National Electronic Injury Surveillance System (NEISS) dataset. Four ensemble models were tested: random forest (RF) + logistic regression (LR), K-Nearest Neighbor (KNN) + RF, LR + KNN, and a combined LR + RF + KNN approach. The KNN + LR ensemble model achieved 90.47% accuracy for the top injury code, while the combined KNN + LR + RF model excelled with 99.50% accuracy for predicting the top two injury codes. | This study demonstrates how ensemble ML models, particularly the probabilistic framework, can enhance the accuracy of unstructured narrative classification, especially when dealing with imbalanced data. The findings underscore the potential of these models to improve decision-making in public health, especially in injury classification systems. |
| [18] | Virtual companion for people with dementia in long-term care | This study focuses on developing a virtual companion for people living with dementia (PLWD) in long-term care (LTC). The system, delivered via a head-mounted virtual reality display, initially prompted conversation and reminiscence, and later used advanced AI to allow more nuanced interactions. Testing showed that while the system faced challenges in early stages, the improved AI in later stages led to more meaningful interactions. Despite some issues like speech recognition and display weight, the system was found to be enjoyable for many users. | This research illustrates the application of virtual reality and AI to provide an engaging, socially interactive tool for PLWD in LTC, promoting meaningful conversations and reducing loneliness. It lays the groundwork for future enhancements, emphasizing the need for innovations in both hardware and software to improve user experience. |
| [19] | Impact of COVID-19 on emergency medical services in Kazakhstan | This retrospective study examines the structure and frequency of ambulance calls in Kazakhstan from 2019 to 2023, focusing on changes during and after the COVID-19 pandemic. The analysis found significant fluctuations in urgency category IV calls, with decreases during the pandemic due to quarantine restrictions and a subsequent increase in the post-pandemic period. | The research provides valuable insights into the dynamics of EMS call volumes in response to the COVID-19 pandemic. It highlights the shifts in healthcare service demand and the long-term impact on emergency medical systems, particularly in less urgent cases. This study offers critical data for improving future emergency healthcare responses during pandemics. |
| [20] | Comparison of diagnostic accuracy between Google and ChatGPT 3.5 for urological conditions | This study compares the diagnostic accuracy of two freely available platforms, Google and ChatGPT 3.5, for identifying urological pathologies. A sample of 60 clinical cases was used to assess each platform’s performance. ChatGPT 3.5 showed superior accuracy, especially for common urological conditions, while Google was less reliable, particularly for rare disorders. | The findings highlight the increasing role of AI platforms in medical diagnosis, showing that ChatGPT 3.5 outperformed Google in providing accurate diagnoses, particularly in common urological conditions. This research sets the stage for exploring the use of AI tools in clinical practice, though further improvements are necessary for rare condition diagnosis. |
| [21] | Radiomics and machine learning for predicting survival in NSCLC patients | This retrospective study investigates the use of radiomics and machine learning to predict survival in non-small cell lung cancer (NSCLC) patients using FDG PET/CT imaging. It evaluates a radiomic model, incorporating tumor stage, SUVmax, and selected radiomic features like NGTDM coarseness, and compares it with a traditional survival model based only on tumor stage and SUVmax. | This study demonstrates that integrating radiomic features with traditional clinical data can offer similar predictive power for survival in NSCLC patients. While the radiomic model’s accuracy was comparable to traditional methods, the findings suggest a potential for more precise, personalized prognostic models in the future. |
| [22] | Deep learning for brain tumor detection in MRI scans | This research introduces a novel dual deep convolutional neural network (DCNN) model designed for classifying brain tumor MRI scans. By using two deep learning models (InceptionV3 and DenseNet121) for feature extraction, this study achieves high performance in classifying brain tumors as cancerous or non-cancerous. It compares this dual DCNN approach against other popular deep learning architectures, showing superior performance. | This study presents a highly effective AI model for brain tumor detection, outperforming traditional deep learning methods in terms of accuracy, precision, and recall. This approach highlights the potential for deep learning models to revolutionize early cancer detection through automated analysis of medical images, which could greatly enhance diagnostic efficiency and outcomes. |
| [23] | Artificial intelligence for early detection of hemorrhage and organ dysfunction during delivery | This study leverages machine learning to establish numerical criteria for identifying organ dysfunction in cases of massive hemorrhage during delivery. The research uses a dataset of 107 deliveries with >2000 mL blood loss from nine national perinatal centers in Japan. By analyzing coagulation factors like fibrinogen and FDP, this study identifies thresholds for predicting hematuria development, which can indicate organ dysfunction. It applies six different machine learning methods, with the support vector machine being the most effective in determining the relevant clinical criteria. | This study presents a novel AI-driven method to detect organ dysfunction in massive hemorrhage cases during delivery. By providing more precise numerical thresholds and combining machine learning with clinical coagulation data, the method could significantly improve the early identification of severe complications in obstetric care, leading to quicker interventions and better patient outcomes. |
| [24] | Advanced Fuzzy C-Means segmentation for MRI brain tumor detection | This research focuses on improving the Fuzzy C-Means (FCM) segmentation algorithm for MRI images to enhance brain tumor classification. This study integrates feature selection based on tumor shape, texture, and color, which reduces complexity and increases classification accuracy. It then uses the Extreme Learning Machine (ELM) classifier to segment and categorize brain tumors. The performance of this enhanced model is compared with existing methods, and it consistently demonstrates superior accuracy, particularly in detecting gliomas. | The improved FCM-based model delivers better performance for tumor classification in MRI scans, with notable improvements in accuracy, precision, and recall. This algorithm can play a pivotal role in medical imaging for early and accurate brain tumor detection, offering clinicians more reliable tools for diagnosis. Additionally, the model’s success in glioma detection has the potential to be a breakthrough in clinical practice for more precise brain tumor identification. |
| [25] | Exploring AI’s role in public health research and scientific authorship | This study explores the potential of GPT-3, an advanced AI model, to support public health research by generating relevant text blocks and summarizing scientific articles. The research specifically tests GPT-3’s capacity to provide plausible answers on public health issues. Despite some fabricated content, it demonstrates the potential for AI to assist researchers in compiling and analyzing large amounts of data. It also discusses the implications of using AI as a scientific contributor in research publications while adhering to the principles of scientific integrity. | This study highlights the potential of AI to assist in public health research by summarizing the literature and generating scientific content. However, it also raises critical questions about the credibility of AI-generated information and its appropriate role in authorship. This research emphasizes the importance of establishing guidelines for AI’s involvement in scientific research, ensuring that its contributions are valid and adhere to ethical standards. |
| [26] | AI-powered COVID-19 CT image diagnosis and lesion segmentation | This study presents a deep learning-based method for accurately segmenting lesions from CT images of COVID-19 patients. The proposed solution, DLShelper, corrects rough initial labels of lesions by analyzing pixel distribution in infected and healthy areas. By improving segmentation accuracy, the system aids in diagnosing COVID-19 and grading the severity of lung lesions. The approach is tested on a public dataset of CT images and has been shown to significantly improve segmentation and diagnosis accuracy, benefiting medical staff with better diagnostic support. | The DLShelper tool offers a promising AI-driven solution for diagnosing COVID-19 through enhanced lesion segmentation and severity grading. It assists clinicians by providing more accurate and detailed diagnostic information, improving decision-making during the diagnosis process. The tool’s effectiveness in handling CT images can be adapted for other diagnostic applications, paving the way for more advanced, AI-powered diagnostic systems in healthcare. |
| Study/Type | Focus | Brief Summary | Contribution |
|---|---|---|---|
| [27]/R | Artificial intelligence in cytopathology | This umbrella review delves into the integration of artificial intelligence (AI) into the field of cytopathology, highlighting its potential to improve diagnostic accuracy and operational efficiency. This study examines 21 review articles to identify key trends, opportunities, challenges, and best practices for AI adoption in cytopathology. It emphasizes the importance of validation processes, integration with existing clinical workflows, and addressing ethical issues such as algorithmic bias and data privacy. | This review contributes by offering an extensive analysis of the current landscape of AI in cytopathology, revealing how AI can automate diagnostic processes, reduce errors, and improve patient outcomes. It highlights critical challenges, such as high implementation costs, the need for empirical data on diagnostic accuracy, and the integration of AI with existing clinical systems. This review also provides a roadmap for future AI development in cytopathology, informed by advancements in related fields like histopathology and radiology. |
| [28]/SR | Generative Adversarial Networks (GANs) in head and neck surgery | The review explores the application of Generative Adversarial Networks (GANs) in the field of head and neck surgery. GANs are a class of AI algorithms capable of generating new data from existing data. This review examines how GANs are being used in diagnostic imaging and treatment planning in craniofacial surgery, particularly for conditions such as craniosynostosis, chronic sinusitis, and various bone defects. The review assesses 9 studies out of 700, summarizing 8 key applications of GANs in the head and neck region. | This study highlights the emerging role of GANs in improving diagnostic accuracy and treatment outcomes in head and neck surgery. It identifies several practical applications of GANs, including the enhancement of diagnostic imaging, surgical planning, and post-operative prediction. The review emphasizes GANs as a transformative tool in personalized healthcare, providing a more precise and data-driven approach to treating head and neck pathologies, including oncological cases. |
| [29]/R | Mobile and domiciliary radiology with AI integration | This review investigates the growing integration of mobile radiology and AI technologies in healthcare, particularly focusing on how these innovations have transformed domiciliary (home-based) radiology services. This study assesses 21 recent publications to analyze the effectiveness of mobile X-ray equipment, AI-enhanced diagnostic tools, and telemedicine applications, with a focus on the post-COVID-19 era. Notably, it explores how mobile mammography units have become essential for breast cancer screening in underserved populations. | The contribution of this review is in examining how AI, mobile radiology, and telemedicine technologies can significantly improve access to diagnostic services in rural and underserved areas. It also discusses the potential of AI in enhancing pediatric radiology and the broader implications for healthcare equity. The review offers insights into the future of domiciliary radiology, suggesting the importance of multi-domain technology assessment and regulatory frameworks for the responsible integration of these technologies. |
| [30]/SR | AI chatbots in women’s health | This systematic review and meta-analysis explores the use of AI-powered chatbots in improving health outcomes for women, specifically focusing on mental health (e.g., anxiety, depression), health behaviors (e.g., cancer self-care), and preconception care. By analyzing 10 studies published between 2019 and 2023, this review assesses the effectiveness of chatbot interventions in various health domains, including reproductive health, eating disorders, and relationship management. | This study underscores the positive impact AI chatbots can have on women’s health by providing accessible, digital therapeutic interventions. This review provides evidence that chatbots can improve mental health outcomes and health behaviors among women, offering a cost-effective and scalable solution for addressing issues such as anxiety, depression, and self-care practices. It emphasizes that chatbots could become a critical tool in healthcare interventions, especially for women in remote or underserved areas. |
| [31]/R | AI and language models in cardiology | This review examines the integration of generative AI, such as ChatGPT-4, and other language models in cardiology. It focuses on how AI can assist in diagnosing heart disease, recommending treatment plans, and improving physician efficiency through administrative task automation. It discusses the challenges associated with AI, such as outdated information, high costs, and the potential loss of human empathy in patient care. | This study explores the role of AI in revolutionizing cardiology by improving diagnostic accuracy, treatment planning, and operational efficiency. It highlights both the benefits of AI tools—such as enhancing physician decision-making and reducing administrative burdens—and the challenges, such as maintaining up-to-date knowledge and ensuring equitable access to these technologies. This review calls for comprehensive training for healthcare professionals and careful integration of AI into medical practices to ensure patient-centered care. |
| [32]/R | AI in teledermatology | This review discusses the role of AI in advancing teledermatology, particularly in diagnosing skin conditions remotely through telemedicine platforms. It evaluates the integration of AI in eHealth and mHealth for self-care, quality control, and patient management in dermatology. This study also addresses the challenges of app validation, standardization, cybersecurity, and the need for legal and regulatory frameworks. | This study highlights the potential of AI to improve the quality of care in dermatology by facilitating remote diagnosis and patient monitoring. It identifies key benefits such as increased accessibility, reduced healthcare costs, and improved efficiency in diagnosis. However, this review also emphasizes the need for enhanced app design, better cybersecurity measures, and standardized protocols for AI applications in teledermatology. It suggests that regulatory frameworks and position statements from scientific societies are critical to ensuring responsible implementation. |
| [33]/R | Machine learning in domestic violence detection | This review explores the use of machine learning (ML) algorithms in detecting and predicting domestic violence (DV) through the analysis of digital data, including social media, surveys, and health records. The study reviews 22 articles and identifies key applications of both supervised and unsupervised ML methods, focusing on their ability to classify, predict, and explore patterns associated with DV. | The contribution of this review lies in demonstrating the potential of machine learning techniques to identify early signs of domestic violence by analyzing digital text data. It provides insights into the algorithms used in this field, such as random forests and support vector machines, and discusses the challenges, including data quality, algorithmic bias, and the need for extensive data preparation. The review encourages further development of ML models specifically designed for DV detection, which could significantly enhance early intervention efforts. |
| Study/Type | Focus | Brief Summary | Contribution |
|---|---|---|---|
| [34]/TN | Machine learning for effective dose calculation | This study explores the use of machine learning (ML) algorithms to predict organ doses and effective dose conversion coefficients (DCCs) for various anthropomorphic phantoms. Traditionally, Monte Carlo methods are used for these calculations, which are time-consuming and require expertise. By compiling a comprehensive dataset from Monte Carlo studies, the authors train ML models (XGB, GB, and Extra Trees regressor) to predict the effective dose. This study evaluates the ML models’ performance using error metrics and compares them with ICRP values. | This study highlights the potential of ML techniques to predict effective doses efficiently, offering a solution to the traditional Monte Carlo method’s limitations. The ML models demonstrated good accuracy at mid-range neutron energies, providing a faster alternative for dose prediction, especially in scenarios requiring quick results. Additionally, this study suggests improvements in data representation and the inclusion of larger datasets to enhance model accuracy, thereby contributing to personalized dosimetry in radiation protection. |
| [35]/P | Neural network models for causal variable analysis in medical and climatic studies | This paper presents a neural network-based method to analyze non-linear systems, focusing on small datasets. The authors propose a strategy to identify the roles (linear, non-linear, or threshold) of causal variables in predicting the behavior of a target variable. They apply this method to climate studies and medical research, particularly cancer studies. The approach allows for predictions about future scenarios based on causal variables. | This paper introduces a complementary approach to deep learning by focusing on understanding causal relationships within datasets. The methodology has applications in medical research, particularly in cancer studies, by helping identify important causal variables and predicting future trends. The approach’s utility in small datasets makes it valuable for medical studies with limited data, and its potential to influence research on cancer treatment is a key contribution. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giansanti, D.; Costantini, G. Artificial Intelligence in Public Health: Bridging Today’s Trends with Tomorrow’s Possibilities. Bioengineering 2025, 12, 559. https://doi.org/10.3390/bioengineering12060559
Giansanti D, Costantini G. Artificial Intelligence in Public Health: Bridging Today’s Trends with Tomorrow’s Possibilities. Bioengineering. 2025; 12(6):559. https://doi.org/10.3390/bioengineering12060559
Chicago/Turabian StyleGiansanti, Daniele, and Giovanni Costantini. 2025. "Artificial Intelligence in Public Health: Bridging Today’s Trends with Tomorrow’s Possibilities" Bioengineering 12, no. 6: 559. https://doi.org/10.3390/bioengineering12060559
APA StyleGiansanti, D., & Costantini, G. (2025). Artificial Intelligence in Public Health: Bridging Today’s Trends with Tomorrow’s Possibilities. Bioengineering, 12(6), 559. https://doi.org/10.3390/bioengineering12060559





