Abstract
(1) Background: An asthma exacerbation that is not relieved with medication typically requires an emergency room visit (ERV). The coronavirus disease 2019 (COVID-19) pandemic began in Taiwan in January of 2020. The influence of the COVID-19 pandemic on pediatric ERVs in Taiwan was limited. Our aim was to survey pediatric asthma ERVs in the COVID-19 era; (2) Methods: Data were collected from the health quality database of the Taiwanese National Health Insurance Administration from 2019 to 2021. Air pollution and climatic factors in Taipei were used to evaluate these relationships. Changes in the rates of pediatric asthma ERVs were assessed using logistic regression analysis. Poisson regression was used to evaluate the impact of air pollution and climate change; (3) Results: The rate of pediatric asthma ERVs declined in different areas and at different hospital levels including medical centers, regional and local hospitals. Some air pollutants (particulate matter ≤ 2.5 µm, particulate matter ≤ 10 µm, nitrogen dioxide, and carbon monoxide) reduced during the COVID-19 lockdown. Ozone increased the relative risk (RR) of pediatric asthma ERVs during the COVID-19 period by 1.094 (95% CI: 1.095–1.12) per 1 ppb increase; (4) Conclusions: The rate of pediatric asthma ERVs declined during the COVID-19 pandemic and ozone has harmful effects. Based on these results, the government could reduce the number of pediatric asthma ERVs through healthcare programs, thereby promoting children’s health.
1. Introduction
1.1. Coronavirus Infection since 2019
New respiratory and related diseases in Wuhan City, Hubei Province, China, have been caused by coronavirus infection since December 2019. Most patients have clinical findings of fever, difficulty breathing, and infiltrative lesions in both lungs on chest radiography [1]. Coronavirus disease 2019 (COVID-19) was first identified in Taiwan on 21 January 2020. Patients who meet the clinical and laboratory criteria, and have moderate or severe complications, must be admitted and treated immediately [2].
1.2. Epidemiology of Asthma
Asthma is a chronic airway obstruction caused by many factors. Genetic factors combined with specific environmental factors may result in bronchial wall thickening and respiratory over-responsiveness. Air pollution, daily temperature changes, infections, emotional changes, strenuous exercise, drugs, preservatives, allergic agents, and other factors can cause rapid inflammation of the respiratory tract, induce bronchial constriction, and increased sputum formation [3].
Symptoms of asthma exacerbation include shortness of breath and/or chest tightness. Airflow obstruction increases without immediate treatment, causing increased breathing work and respiratory muscle fatigue, resulting in hypercapnic and hypoxemic respiratory failure due to gas exchange inefficiency. Male patients with asthma, the elderly, and children were less sensitive to the symptoms. As such, an acute asthma attack is a significant public health problem that affects patients and their parents or caregivers and is associated with decreased quality of life, decreased school attendance, emergency room visits (ERVs), and hospitalizations, as well as a higher mortality risk [4]. Based on information in the Taiwanese National Health Insurance database, the prevalence of asthma among adults has been gradually increasing from 2000 to 2011; the prevalence of asthma among adults increased from 7.57% in 2000 to 11.53% in 2011 [5]. However, the overall prevalence of asthma in Taiwan was 9% in 2017 and 2018 [6]. The prevalence of asthma is higher in children; however, the morbidity and mortality rates due to asthma are higher in adults. Childhood asthma is more common in boys than girls, and several environmental factors have been identified. In children, asthma may impair airway development and lead to reduced lung function as an adult [7]. The prevalence of asthma in the United States is 7.7%, with 4.6 million children under the age of 18 years [8], and up to 36% ERVs of asthmatic children under 18 years of age were affected by an asthma attack in the United States in 2016 [9].
Asthma affects approximately 262 million patients worldwide, thus causing about approximately 461,000 deaths in 2019 [8]. Acute asthma attacks are among the most common reasons for ERVs in all age groups and impose a significant burden on healthcare systems. A previous study showed that the proportion of children with asthma aged 6–12 years who were diagnosed by a doctor in Taiwan was 11% between 2008 and 2009, 10.9% between 2010 and 2012, and 9% between 2017 and 2018 [6]. Based on the self-reported questionnaire data from the National Health Interview Survey (NHIS) by the Ministry of Health and Welfare National Health Service in Taiwan in 2017, the overall prevalence of asthma was estimated to be 4.3% in all age groups, including children and adults, which translated into approximately 2 million patients and 318,000 pediatric patients [10]. A total of 9.2% of children < 12 years of age are sent to the emergency room for asthma exacerbations every year, and 23% of people have an asthma attack each year; however, 17% do not follow regular outpatient visits [10]. The five most common causes of asthma in children under 12 years of age are viral infections (56.7%), dust mites (44.5%), sudden temperature changes (42.7%), air pollution (24.6%), and colder food (21.6%) [10].
1.3. Air Pollution and Pediatric Asthma
The respiratory disorders were associated with particulate matter, nitrogen oxides, and sulfur dioxide (SO2) [11,12]. The asthma outcomes in childhood were related to particulate matter ≤ 2.5 µm (PM2.5), nitrogen dioxide (NO2), and ozone in the previous studies [13,14,15,16,17]. Numerous studies have evaluated the effects of PM2.5 and O3 on children with asthma in Taiwan and Hong Kong before 2019 [18,19,20,21]. PM2.5 induces more tissue kallikrein of epithelial cells with mucus hypersecretion and barrier function and causes immunoglobin E, eosinophils to increase [13,14]. Ozone is produced via a photochemical reaction between nitrogen oxides and volatile organic compounds in the troposphere, with motor vehicle emissions being the greatest source [22]. High ozone concentrations can irritate the eyes and nose and cause urgent respiratory distress with impaired lung function [23]. Daily changes in ozone concentrations are positively associated with the incidence of asthma and daily non-accidental mortality [24]. The effects of O3 on asthma risk in Taiwanese schoolchildren have been reported to have an adjusted OR of 1.14 [23]. Ozone is a strong oxidant that causes oxidative damage to the airway cells and induces inflammatory reactions in the airways. Acute ozone exposure in young male children resulted in an increase in sputum neutrophils in 30% of children [25]. Increased ozone induced type 2 inflammation [13]. Controlling ozone pollution is challenging in the United States in 2016, where 90% of the substandard national ambient air quality conditions were caused by ozone, whereas only 10% were caused by particulate matter and other regulated pollutants [24]. Globally, ozone causes premature deaths and several million asthma-related ERVs annually. To combat global ozone pollution, more aggressive reductions in fossil fuel consumption are needed to reduce NO, volatile organic compounds, and greenhouse gas emissions [24]. In Taoyuan, Taiwan, the RR of the ERVs for asthma after ozone exposure was 1.2 [26].
1.4. Other Infection Decline during COVID-19 Pandemic
Infections can induce acute bronchospasms and increase sensitization to environmental air pollutants, which are risk factors for asthma exacerbation in children [27]. A reduction in respiratory pathogens is considered the most important factor in reducing asthma exacerbation. The reasons for the reduction in adult asthma exacerbations are multifactorial, with fewer viral infections resulting from fewer social contacts and the use of monoclonal antibodies in the United States [28]. A decrease in retroviral infection rates has been observed in the United States, and the reduction in infections has the potential to decrease asthma exacerbations [29]. The total number of outpatients and ERVs for influenza-like illnesses in Taiwan is expected to significantly decrease by 2021 [30]. Pediatric ERVs for respiratory disease decreased during the COVID-19 pandemic in Kaohsiung [31]. It may have had fewer asthma exacerbations because of protective measures such as maintaining social distancing, wearing face masks, and frequent hand washing. Residents’ activities decreased after the COVID-19 outbreak. Decreased economic activity and air pollution have health benefits [32]. Lifestyle changes with school closures and stay-at-home orders, as well as restricting eating outside, are measures that reduce air pollution and person-to-person contact.
1.5. The Emergency Room Visits Decline during COVID-19 Pandemic
During the COVID-19 pandemic, the number of ERVs in Taiwan have decreased significantly [33,34]. In the early stages of the pandemic, the number of daily ERVs was significantly reduced and examination times were shortened. Hospitalized patients have benefited from the pandemic, with shorter emergency room stays, faster discharges, lower mortality rates, and fewer readmissions [34].
The government imposed restrictive measures on Taiwan. Pediatric asthma exacerbations decreased during the COVID-19 period compared to the previous 5 years in northern Italy [35]. There are fewer ERVs and hospitalizations of children with asthma in the United States and Canada [29,36]. The reasons for this reduction in asthma ERVs are multifactorial and may include decreased viral infections, restrictive measures, and reduced traffic-related air pollution (TRAP) [35,36]. However, there is a lack of information regarding pediatric asthma ERVs in Taiwan, and this issue requires further study.
This study aimed to determine the impact of the COVID-19 pandemic on ERVs in pediatric patients with asthma in Taiwan. We assessed whether the rate of pediatric asthma ERVs was reduced during the COVID-19 pandemic compared to that in the pre-COVID-19 period. In addition, we examined the influence of different air pollutants on pediatric ERVs for asthma during these two periods. By understanding the possible risk factors for pediatric asthma ERVs during the COVID-19 pandemic, governments can promote children’s health through aggressive policies in the post-COVID-19 era.
2. Materials and Methods
Data were collected from the Taiwanese National Health Insurance Administration and the National Health Insurance database. Pediatric asthma was defined as a patient < 18 years old patients who had an ICD10-CM of J45; had 4 outpatient visits within 1 year; used an asthma medication; and had an Anatomical Therapeutic Chemical classification code of R03AC02, R03AC03, R03AC04, R03AC06, R03AC12, R03AC13, R03AC16, R03AC18, R03BA01, R03BA02, R03BA05, R03BA08, R03AK06, R03AK07, H02AB06, H02AB07, R03DC01, R03DC03, or R03DA05; had an ERVs; or had a hospitalization. The rate of pediatric asthma ERVs was defined as the number of pediatric asthma ERVs divided by the number of pediatric asthma patients, of which it was published every season in the healthcare quality information dataset [37].
We collected data on the rates of pediatric asthma ERVs from the first season of 2019 to the fourth season of 2021. The first season was from January to March, the second season was from April to June, the third season was from July to September, and the fourth season was from October to December. The change in the rate of pediatric asthma ERVs before the COVID-19 pandemic (2019) and during the COVID-19 pandemic (2020–2021) was compared based on the regional distribution and hospital levels (including medical centers, regional and local hospitals). Since the trend of annual pediatric asthma ERVs in Taipei District (including Taipei City and New Taipei City) is relatively close to the trend of pediatric asthma ERVs in Taiwan, Taipei District was selected to study the risk of pediatric asthma ERVs due to air pollution and climate factors. Monthly air pollution data were obtained from the Taiwan Air Quality Monitoring Network of the Ministry of Environmental Protection [38]. The climate factors were collected from the Taipei City Statistical dataset [39]. We used monthly air pollution data from the Wanhua station, located in the Taipei Basin Center. Wanhua Station is located at Fuxing Elementary School (latitude and longitude: 25.04679 and 121.50888, respectively; Google Maps). The values of each air pollutant, including PM2.5, NO2, O3, and climate factor including ambient temperature and relative humidity, were analyzed for correlations. If the p value of the coefficient of the two parameters was < 0.05, indicating a higher correlation, one of the values needed to be excluded. To reduce the likelihood of a multiple collinearity problem, we screened variables by setting the inclusion criteria at |r| < 0.8. Due to the lockdown implemented in the middle of May of 2021, only a half influence of the disease effect was observed. Thus, we selected air pollutants and climatic factors from Taipei from June to July 2021 and compared them with the data from 2019.
The COVID-19 outbreak started in the Wanhua District in May 2021 in Taiwan, and the government implemented a lockdown policy in Taiwan beginning on 15 May 2021, which was in effect until 26 July 2021. We compared the rates of pediatric asthma ERVs between the pre-COVID-19 period (2019) and the COVID-19 pandemic (2020–2021). Air pollution and climatic factors were collected during the pre-COVID period, the COVID-19 pandemic, and COVID-19 pandemic with the lockdown period (second and third seasons of 2021). This study was approved by the Institutional Review Board of Tri-Service General Hospital of TSGHIRB-C202305039.
The Chi-square test was used to compare the rates of pediatric asthma ERVs during the COVID-19 and lockdown periods. Student’s t-test was used to compare air pollution and climatic factors before and after COVID-19, or during the lockdown period. The relations between pediatric asthma ERVs and the COVID-19, or the lockdown period, were determined using logistic regression analysis and reported as odds ratios (ORs). A Poisson analysis was performed to determine the relative risk (RR) of air pollution and climatic factors on pediatric asthma ERVs. The mean rates of pediatric asthma ERVs, air pollutant factors, and climatic factors for each season were plotted. Statistical significance was set at p < 0.05. All statistical analyses were performed using SPSS version 21.
3. Results
The annual rate of pediatric asthma ERVs has decreased in the Taipei and Northern, Central, Southern, and Kaohsiung–Pingtung areas of Taiwan. However, there was no significant change in the rate of pediatric asthma ERVs in Eastern Taiwan during the COVID-19 pandemic. The ERV rates of pediatric asthma in different areas are shown in Figure 1. Changes in pediatric asthma ERVs rates are summarized in Table 1.
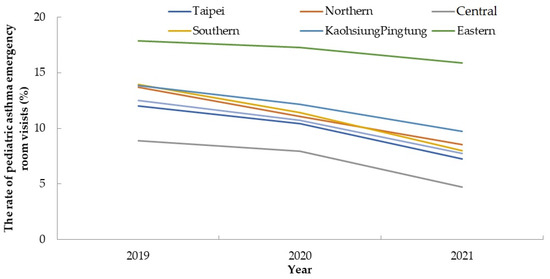
Figure 1.
The rate of pediatric asthma emergency room visits in different areas.

Table 1.
The rate of pediatric asthma emergency room visits during pre-COVID-19 period and COVID-19 period in Taiwan, the rate decline associated with COVID-19 period compared with pre-COVID-19 period using logistic regression.
There was a significant reduction in pediatric asthma ERVs in 2020 and 2021 in medical centers, regional hospitals, and local hospitals compared to the rates in 2019 (pre-COVID-19). The rate of pediatric asthma ERVs ranged from 11.54% to 8.24% in medical centers (OR = 0.688; (95% CI: 0.644–0.735, p < 0.001). The rate of pediatric asthma ERVs ranged from 14.83% to 9.84% in regional hospitals (OR, 0.627; 95% CI: 0.589–0.667, p < 0.001). The rate of pediatric asthma ERVs in local hospitals ranged from 6.76% to 5.58% (OR, 0.815; (95% CI: 0.724–0.917, p < 0.001). The ERV rates of pediatric asthma decreased at different hospital levels (Figure 2).
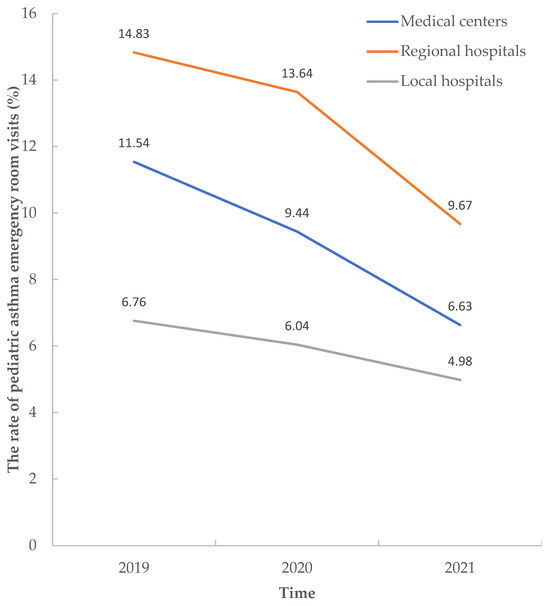
Figure 2.
The rate of pediatric asthma emergency room visits in different hospital levels.
With respect to air pollution in Taipei, the mean PM2.5 was 12.78 ± 2.8 µg/m3, the mean SO2 was 1.77 ± 0.33 ppb, the mean ozone was 26.45 ± 3.69 ppb, the mean NO2 was 18.04 ± 3.12 ppb, the mean air temperature was 24.14 ± 4.24℃, and the mean relative humidity was 75.28 ± 2.57%. The mean air pollutants and climatic factor levels between were not significantly different between the pre-COVID-19 and COVID-19 periods in Taipei.
The greatest air pollutant reduction was particulate matter ≤ 10 µm (PM10), which was 15.95%, followed by around 10% in SO2, CO, and NO2. The increase in O3 concentration was 3.36% (Table 2). Values with a higher Poisson’s correlation (p < 0.05) were excluded (Table 3). The adjusted RR of O3 was 1.094 (95% CI: 1.095–1.12, p < 0.001) per a 1 ppb increase in the COVID-19 era (Table 4). The adjusted RR of PM2.5 was 1.137 (95% CI: 1.042–1.239, p = 0.001) per a 1 µg/m3 increase in the pre-COVID-19 period.

Table 2.
The mean air pollutants and climate factors between pre-COVID-19 and COVID-19 period in Taipei and the rate of seasonal pediatric asthma ERVs.

Table 3.
The correlation between air pollutants and climate factors in Taipei (COVID-19 period).

Table 4.
The relative ratio of pediatric asthma emergency room visits about air pollutants and climate factors in Taipei during COVID-19 period.
4. Discussion
4.1. The Main Finding of This Study
The mean rate of pediatric asthma ERVs has decreased in the past 3 years and the decrease was significant in all regions except for the eastern area. In addition, the rates of pediatric asthma ERVs at medical centers, regional, and local hospitals have decreased significantly. Depending on the period, the mean seasonal rate of pediatric asthma ERVs was the lowest during the COVID-19 lockdown period, followed by the COVID-19 without lockdown period, compared to the pre-COVID-19 period in Taipei. Air pollutants PM2.5, PM10, NO2, and CO decreased significantly during the COVID-19 lockdown period. Ozone was positively associated with pediatric asthma ERVs during the COVID-19 pandemic.
Pediatric asthma exacerbations decreased during the COVID-19 period in Northern Italy compared with the historical data [35]. In Canada, during the COVID-19 period, there were reductions in hospitalization (RR = 0.21), ERVs (RR = 0.35), and outpatient visits (RR = 0.61) in children and young adults with asthma [36]. The results of our study are similar and likely reflect the strict hygiene and social distancing measures adopted in 2020 during the COVID-19 pandemic. In addition, pediatric healthcare searches for serious outbreaks have decreased during the coronavirus pandemic. The decreasing trend in pediatric asthma ERVs was greater during the lockdown period (Figure 3). There were fewer ERVs which may indicate that the number of asthma attacks could be reduced or that asthma patients did not want to visit the emergency department with the potential risk of exposure to COVID-19. This was likely the result of a combination of related restriction measures. PM2.5, PM10, NO2, and CO levels decreased during the lockdown period, supporting the influence of restrictive measures. Several studies have shown that social distancing and increased hygiene measures reduce the diffusion of respiratory pathogens and decrease the incidence of respiratory tract infections. Additionally, adherence to asthma treatment increased during the lockdown period [40,41].
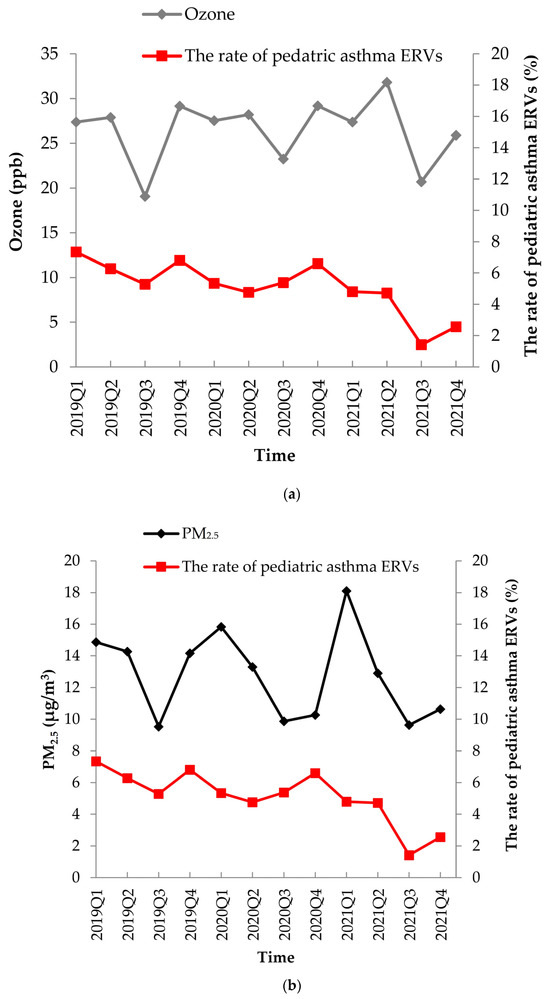
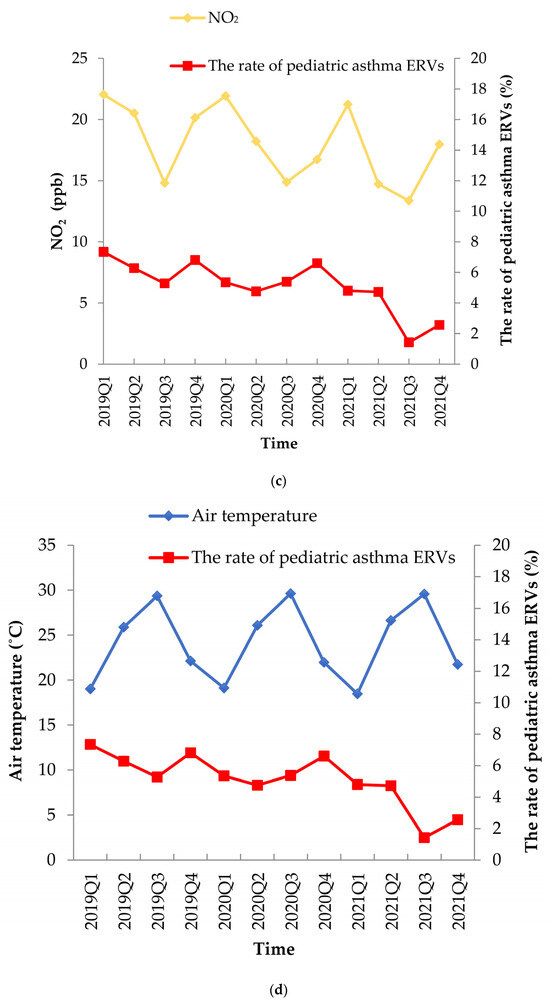
Figure 3.
The air pollution (a) ozone, (b) PM2.5, (c) nitrogen dioxide, (d) air temperature, and the rate of pediatric asthma ERVs change from 2019 to 2021.
4.2. The Change in Air Pollution
The results show a clear decline in NO2 short-term levels and the annual average throughout Europe [42]. The rate of pediatric asthma ERVs was reduced, with the most in Southern Taiwan (OR = 0.68), and this reduction was related to improvements in air pollutant levels. Between 2019 and 2021 in Tainan, the air quality index (summed up by O3, PM2.5, PM10, CO, SO2, and NO2) [38] was decreased from 73 to 66, the PM2.5 decreased from 22.2 to 19.9 µg/m3, NO2 decreased from 11.18 to 10.29 ppb, and O3 decreased from 31.49 to 29.89 ppb [38]. There were no significant changes in the pediatric asthma ERVs in Eastern Taiwan. A potential reason for this finding is that there are fewer clinics in Eastern Taiwan, resulting in fewer patients being sent to the emergency department and lower air pollutant levels.
Between 2019 and 2021 in Hualien, the PM2.5 decreased from 8.5 to 7.8 µg/m3, NO2 decreased from 6.08 to 4.95 ppb, and O3 decreased from 29.49 to 27.07 ppb. The decrease in PM2.5 is likely due to fewer industrial factories, and the decrease in NO2 may be due to less residents and less transportation. We compared air pollutant levels in Taipei between the pre-COVID-19 and COVID-19 eras and found no significant decreases, but there were declining trends in PM2.5, PM10, and NO2 (Table 2). There was a significant decrease in air pollutant levels in Taipei during the lockdown period (Table 5). There was no significant reduction in pediatric asthma ERVs to local hospitals in 2020 compared to 2019, which is likely because, during the initial COVID-19 outbreak, patients were admitted to higher-level hospitals.

Table 5.
The mean air pollutants and climate factors between pre-COVID-19 period and lockdown period in Taipei.
4.3. The Effect of Air Pollution in COVID-19 Period
There were 5275 COVID-19 patients in Taipei City and 7196 COVID-19 patients in New Taipei City during 2021. The majority of COVID-19 cases were in the Taipei metropolitan area, accounting for 76.5% (12,471/16,302) of cases in Taiwan [43]. We selected the Taipei metropolitan area to analyze the risk of pediatric asthma ERVs due to the severe COVID-19 pandemic and a similar rate of pediatric asthma ERVs in Taiwan [37]. Studies have reported that PM2.5, PM10, NO, NO2, and O3 reduce airway defense and induce inflammation and oxidative stress in the airways, which can easily trigger asthma exacerbation [13,14,15,16,17,22].
The cumulative risk of O3 on asthma exacerbation increased by 18.9% for 2 weeks [44]. Our results showed that ozone increased the risk of pediatric asthma ERVs, and there was a 9.4% increased risk of pediatric asthma ERVs for every 1 ppb increase in ozone. Our results showed a mildly increasing trend in the mean ozone level, as compared with the decreasing trends of the other air pollutants (Table 2). Possible reasons for the increase in ozone are the empowered photochemical reactions of increased global temperature [45], the development of the semiconductor industry [26], and the use of negative ion air purifiers and ozone machines for reducing pathogens during the COVID-19 pandemic in urban regions. The inverse effect showed the ozone levels and the number of ERVs exhibited a negative correlation in Korea [46]. A study found that PM2.5 and PM10 may have played important roles in severe pediatric respiratory events requiring ERVs in Kaohsiung during the COVID-19 pandemic [45]. Our results show that ozone increased the risk of pediatric asthma ERVs in Taipei, Taiwan. Since Kaohsiung City is an industrial production area in Taiwan, there are higher levels of air pollutants (2020; mean PM2.5 20.1 µg/m3, PM10 39.8 µg/m3, NO2 12.55 ppb, and O3 30.88 ppb), as compared to Taipei city that is an urban area where air pollution is primarily due to cars and residents (2020; mean PM2.5 12.6 µg/m3, PM10 23.6 µg/m3, NO2 15.69 ppb, and O3 29.98 ppb) [38]. The lower rate of childhood asthma exacerbations in a previous study paralleled the reduced TRAP levels observed during the pandemic. Possible reasons of reduction in O3, NO2, and PM10 during lockdowns have been widely studied in many locations worldwide. The reasons for this reduction are complex and include meteorological conditions. Although most previous studies have confirmed the decrease in NO2 during lockdowns, the decrease in PM10 and PM2.5 is less obvious and is often related to wind conditions. The past study found the lockdown response to COVID-19 has resulted in an unprecedented reduction in global economic activity and associated air pollutant levels, especially land transportation decline [32]. Fossil-fuel combustion was positively correlated with vehicular traffic in an urban context, where it showed decreased concentrations during the lockdown period [35]. Our study found a significant reduction in PM, NO2, and CO levels during the lockdown period, which potentially reduced the pediatric asthma ERVs.
The unscheduled asthma visits were reduced during COVID-19. It was potentially associated with reduced viral upper respiratory tract infections [47]; higher relative humidity increases pollen levels, increasing pediatric asthma exacerbations [48]. A relative humidity level of >60% in Taiwan resulted in more allergic diseases. Cumulative ambient exposure over 0–3 days to PM2.5 (odds ratio (OR) 1.01, per 6.2 µg/m3) and NO2 (OR 1.021 per 7.7 ppb) concentrations were associated with ERVs for COVID-19 [49]. Atmospheric PM2.5 concentrations are significantly associated with a greater risk of asthma exacerbation [13,14,15,16,17,50]. The short-term lag effect of PM2.5 was a 1.2-fold RR with a 2-day lag in pediatric asthma ED visits [20]. Our study found similar findings in the pre-COVID-19 period; however, PM concentration was not associated with pediatric asthma ERVs, since there was a decrease in the lockdown period due to the COVID-19 epidemic in Taipei. This can be explained by the complex formation chemistry in urban areas, mainly non-traffic sources combined with natural, anthropogenic, primary and secondary sources. In addition, the mean monthly PM2.5 decreased to below 10 µg/m3 during the lockdown period, reducing the number of pediatric ERVs for asthma. The potential reason for this was a reduction in winter wind pollution from mainland China during the COVID-19 pandemic because of factory closures and restrictive measures for citizens [45].
In this national retrospective cross-sectional study, we found that pediatric asthma ERVs were affected by the COVID-19 pandemic during 2020–2021, a major environmental trigger of ozone compared with PM2.5 before the COVID-19 period in urban areas. Restrictive measures implemented during the lockdown period significantly reduced air pollution, which potentially positively affected the incidence of pediatric asthma ERVs. The restrictive measures of public health interventions for COVID-19 reduced influenza virus infection [51], and lockdown measures such as school closures, stay-at-home orders, working at home, and protective measures (including social distancing, wearing masks, and increasing hand hygiene) have dictated changes in lifestyle, behavioral, and social habits, which are reflected in the reduced transmission of respiratory pathogens and reductions in anthropogenic atmospheric emissions [35]. Our study highlights the potential role of reduced exposure to air pollution with a slightly anomalous pattern of pediatric asthma ERVs in 2020–2021.
4.4. The Preventive Policy in Post-COVID-19 Era
The air pollutant at risk of pediatric asthma ERVs in Taiwan during the COVID-19 era was ozone. Carbon-containing masks reduce the effects of ozone on the respiratory tract. Residents were encouraged to use public transportation, drive electric cars or motorcycles, and ride bicycles to reduce TRAP. Other measures for reducing asthma attacks were promoted, such as using dehumidifiers to reduce the relative humidity to <50%, avoiding cold food, using non-negative ion air purifiers, avoiding smoking and second-hand smoke, regularly cleaning houses to reduce mite growth, regular outpatient follow ups, and adherence to controller medications.
5. Conclusions
This study demonstrates a reduction in pediatric asthma ERVs during the COVID-19 pandemic in Taiwan. Although decreased outside activity resulted in decreased air pollutants in the lockdown period, air pollutant levels did not change during 2020–2021. Ozone significantly increased the risk of pediatric asthma ERVs, without significant ozone elevation in the COVID-19 era. This research provides important information regarding PM2.5 reduction to a level that can reduce pediatric asthma ERVs, and ozone is still associated with health risks in childhood. An aggressive policy is needed to control the amount of air pollution and reduce ozone to decrease pediatric asthma ERVs, maintain national health, and protect the living environment to improve quality of life.
6. Limitations
This study has some limitations. First, the dataset did not contain the sex and age of the children. Children younger than six years are more sensitive to air pollution than those older than six years [51]. Second, detailed daily pediatric asthma treatments were not examined in this study, and air pollutants may have influenced the short-term frequency of asthma attacks. As seasonal pediatric asthma ERVs are supported by the government, we used seasonal data to survey these relationships during the COVID-19 period. Third, influenza infection decreased in a previous study [52]; however, a direct relationship between influenza infection and ERVs in pediatric asthma is lacking. The analysis should be adjusted for influenza if detailed data are available. The correlation between these two conditions should be investigated in the future. Fourth, the rate of smoking and second-hand smoke exposure were marked by juniors (2.2% cigarettes and 3.9% electronic cigarettes) and seniors (7.2% cigarettes and 8.8% electronic cigarettes) in high school by 2021 in Taiwan [53], which may increase pediatric asthma attacks and ERVs [17]. Registered studies are required to investigate the effects of smoking. Fifth, we used air pollution to assess the risk of pediatric asthma ERVs in Taipei; different areas may have different levels of pollution.
Author Contributions
Conceptualization, Y.-L.C., C.-G.C. and C.-A.C.; methodology, Y.-Y.L. and P.-W.C.; software, C.-C.C.; validation, Y.-L.C. and C.-G.C.; formal analysis, C.-A.C.; investigation, Y.-Y.L. and P.-W.C.; resources, C.-C.C., C.-G.C. and C.-A.C.; data curation, Y.-Y.L. and P.-W.C.; writing—original draft preparation, Y.-L.C., C.-G.C. and C.-A.C.; writing—review and editing, Y.-L.C., C.-G.C. and C.-A.C.; visualization, Y.-Y.L. and P.-W.C.; supervision, C.-C.C.; project administration, C.-C.C.; funding acquisition, C.-G.C. and C.-A.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Tri-Service General Hospital (protocol code C202305039, 27 May 2023).
Informed Consent Statement
Informed consent was not applicable for the data.
Data Availability Statement
The datasets used in the current study are available from the correspondence.
Acknowledgments
The authors are thankful for the support of TYAFGH-E-112042 and TYAFGH-E-113048 for this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Hui, D.S.; IAzhar, E.; Madani, T.A.; Ntoumi, F.; Kock, R.; Dar, O.; Ippolito, G.; Mchugh, T.D.; Memish, Z.A.; Drosten, C.; et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—The latest 2019 novel coronavirus outbreak in Wuhan, China. Int. J. Infect. Dis. 2020, 91, 264–266. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus Disease 2019 (COVID-19) in Taiwan. 2023. Available online: https://www.cdc.gov.tw/en/Disease/SubIndex/ (accessed on 1 September 2023).
- Postma, D.S.; Kerkhof, M.; Boezen, H.M.; Koppelman, G.H. Asthma and chronic obstructive pulmonary disease: Common genes, common environments? Am. J. Respir. Crit. Care Med. 2011, 183, 1588–1594. [Google Scholar] [CrossRef]
- World Health Organization. Global Surveillance, Prevention and Control of Chronic Respiratory Diseases: A Comprehensive Approach; World Health Organization: Geneva, Switzerland, 2007; Available online: http://www.who.int/gard/publications/GARDBook2007.pdf (accessed on 1 September 2023).
- Ma, Y.C.; Lin, C.C.; Yang, S.Y.; Chen, H.J.; Li, T.C.; Lin, J.G. Time Trend Analysis of the Prevalence and Incidence of Diagnosed Asthma and Traditional Chinese Medicine Use among Adults in Taiwan from 2000 to 2011: A Population-Based Study. PLoS ONE 2015, 10, e0140318. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.Y.; Lin, C.W.; Lee, J.; Chen, P.S.; Tsai, H.J.; Wang, J.Y. Decreasing ten-year (2008–2018) trends of the prevalence of childhood asthma and air pollution in southern Taiwan. World Allergy Organ. J. 2021, 14, 100538. [Google Scholar] [CrossRef] [PubMed]
- Gushue, C.; Miller, R.; Sheikh, S.; Allen, E.D.; Tobias, J.D.; Hayes, D., Jr.; Tumin, D. Gaps in health insurance coverage and emergency department use among children with asthma. J. Asthma 2019, 56, 1070–1078. [Google Scholar] [CrossRef] [PubMed]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Dharmage, S.C.; Perret, J.L.; Custovic, A. Epidemiology of Asthma in Children and Adults. Front. Pediatr. 2019, 7, 246. [Google Scholar] [CrossRef]
- National Health Interview Survey in Taiwan in 2017. Available online: https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=364&pid=13636 (accessed on 1 September 2023).
- Liu, H.Y.; Bartonova, A.; Schindler, M.; Sharma, M.; Behera, S.N.; Katiyar, K.; Dikshit, O. Respiratory Disease in Relation to Outdoor Air Pollution in Kanpur, India. Arch. Environ. Occup. Health 2013, 68, 204–217. [Google Scholar] [CrossRef]
- Khatri, S.B.; Newman, C.; Hammel, J.P.; Dey, T.; Van Laere, J.J.; Ross, K.A.; Rose, J.A.; Anderson, T.; Mukerjee, S.; Smith, L.; et al. Associations of Air Pollution and Pediatric Asthma in Cleveland, Ohio. Sci. World J. 2021, 2021, 8881390. [Google Scholar] [CrossRef]
- Altman, M.C.; Kattan, M.; O’Connor, G.T.; Murphy, R.C.; Whalen, E.; LeBeau, P.; Calatroni, A.; Gill, M.A.; Gruchalla, R.S.; Liu, A.H.; et al. Relationships of outdoor air pollutants to non-viral asthma exacerbations and airway inflammatory responses in urban children and adolescents: A population-based study. Lancet Planet. Health 2019, 144, 935–944. [Google Scholar] [CrossRef]
- Dunea, D.; Iordache, S.; Liu, H.Y.; Bøhler, T.; Pohoata, A.; Radulescu, C. Quantifying the impact of PM2.5 and associated heavy metals on respiratory health of children near metallurgical facilities. Environ. Sci. Pollut. Res. 2016, 15, 15395–15406. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.-Y.; Dunea, D.; Iordache, S.; Pohoata, A. A Review of Airborne Particulate Matter Effects on Young Children’s Respiratory Symptoms and Diseases. Atmosphere 2018, 9, 150. [Google Scholar] [CrossRef]
- Holst, G.J.; Pedersen, C.B.; Thygesen, M.; Brandt, J.; Geels, C.; Bønløkke, J.H.; Sigsgaard, T. Air pollution and family related determinants of asthma onset and persistent wheezing in children: Nationwide case-control study. BMJ 2020, 370, m2791. [Google Scholar] [CrossRef]
- Tiotiu, A.I.; Novakova, P.; Nedeva, D.; Chong-Neto, H.J.; Novakova, S.; Steiropoulos, P.; Kowal, K. Impact of Air Pollution on Asthma Outcomes. Int. J. Environ. Res. Public Health 2020, 17, 6212. [Google Scholar] [CrossRef]
- Hsu, S.-C.; Chang, J.-W.; Lee, C.-L.; Huang, W.-C.; Hsu, Y.-P.; Liu, C.-T.; Jean, S.-S.; Huang, S.-K.; Hsu, C.-W. Differential time-lag effects of ambient PM2.5 and PM2.5-PAHs on asthma emergency department visits. Environ. Sci. Pollut. Res. Int. 2020, 27, 43117–43124. [Google Scholar] [CrossRef] [PubMed]
- Zafirah, Y.; Lin, Y.K.; Andhikaputra, G.; Deng, L.W.; Sung, F.C.; Wang, Y.C. Mortality and morbidity of asthma and chronic obstructive pulmonary disease associated with ambient environment in metropolitans in Taiwan. PLoS ONE 2021, 16, e0253814. [Google Scholar] [CrossRef]
- Lee, S.L.; Wong, W.H.; Lau, Y.L. Association between air pollution and asthma admission among children in Hong Kong. Clin. Exp. Allergy 2006, 36, 1138–1146. [Google Scholar] [CrossRef]
- Fan, J.; Li, S.; Fan, C.; Bai, Z.; Yang, K. The impact of PM2.5 on asthma emergency department visits: A systematic review and meta-analysis. Environ. Sci. Pollut. Res. Int. 2016, 23, 843–850. [Google Scholar] [CrossRef]
- Guarnieri, M.; Balmes, J.R. Outdoor air pollution and asthma. Lancet 2014, 383, 1581–1592. [Google Scholar] [CrossRef]
- Hwang, B.F.; Lee, Y.L.; Lin, Y.C.; Jaakkola, J.J.; Guo, Y.L. Traffic related air pollution as a determinant of asthma among Taiwanese school children. Thorax 2005, 60, 467–473. [Google Scholar] [CrossRef]
- Zhang, J.J.; Wei, Y.; Fang, Z. Ozone Pollution: A Major Health Hazard Worldwide. Front. Immunol. 2019, 10, 2518. [Google Scholar] [CrossRef] [PubMed]
- Mumby, S.; Chung, K.F.; Adcock, I.M. Transcriptional Effects of Ozone and Impact on Airway Inflammation. Front. Immunol. 2019, 10, 1610. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.-G.; Yen, S.-Y.; Hsiao, C.-C.; Lin, Y.-Y.; Chang, Y.-H.; Chen, Y.-H.; Cheng, C.-A. Short-Term Exposure Effect of Ambient Fine Particulate Matter, Ozone and Cold Temperature on Emergency Room Visits for Asthma Patients. Toxics 2023, 11, 94. [Google Scholar] [CrossRef]
- Dondi, A.; Calamelli, E.; Piccinno, V.; Ricci, G.; Corsini, I.; Biagi, C.; Lanari, M. Acute Asthma in the Pediatric Emergency Department: Infections Are the Main Triggers of Exacerbations. Biomed. Res. Int. 2017, 2017, 9687061. [Google Scholar] [CrossRef]
- Moore, W.C.; Ledford, D.K.; Carstens, D.D.; Ambrose, C.S. Impact of the COVID-19 Pandemic on Incidence of Asthma Exacerbations and Hospitalizations in US Subspecialist-Treated Patients with Severe Asthma: Results from the CHRONICLE Study. J. Asthma Allergy 2022, 15, 1195–1203. [Google Scholar] [CrossRef] [PubMed]
- Taquechel, K.; Diwadkar, A.R.; Sayed, S.; Dudley, J.W.; Grundmeier, R.W.; Kenyon, C.C.; Henrickson, S.E.; Himes, B.E.; Hill, D.A. Pediatric Asthma Health Care Utilization, Viral Testing, and Air Pollution Changes During the COVID-19 Pandemic. J. Allergy Clin. Immunol. Pract. 2020, 8, 3378–3387.e11. [Google Scholar] [CrossRef]
- Taiwan Centers of Diseases Control. Taiwan Influenza News. 2023. Available online: https://www.cdc.gov.tw/File/Get/SziwknOOrnO1NW9GQEyRSA (accessed on 1 September 2023).
- Lin, C.F.; Huang, Y.H.; Cheng, C.Y.; Wu, K.H.; Tang, K.S.; Chiu, I.M. Public Health Interventions for the COVID-19 Pandemic Reduce Respiratory Tract Infection-Related Visits at Pediatric Emergency Departments in Taiwan. Front. Public Health 2020, 8, 604089. [Google Scholar] [CrossRef]
- Venter, Z.S.; Aunan, K.; Chowdhury, S.; Lelieveld, J. Air pollution declines during COVID-19 lockdowns mitigate the global health burden. Environ. Res. 2021, 192, 110403. [Google Scholar] [CrossRef]
- Chen, J.Y.; Chang, F.Y.; Lin, C.S.; Wang, C.H.; Tsai, S.H.; Lee, C.C.; Chen, S.J. Impact of the COVID-19 Pandemic on the Loading and Quality of an Emergency Department in Taiwan: Enlightenment from a Low-Risk Country in a Public Health Crisis. J. Clin. Med. 2021, 10, 1150. [Google Scholar] [CrossRef]
- Chang, H.M.; Chang, C.C.; Lin, P.Y.; Lee, Y.C.; Huang, H.H.; Yen, D.H. The impact of COVID-19 epidemic on emergency department visits of older patients in Taiwan. BMC Geriatr. 2023, 23, 490. [Google Scholar] [CrossRef]
- Dondi, A.; Betti, L.; Carbone, C.; Dormi, A.; Paglione, M.; Rinaldi, M.; Gualtieri, M.; Scotto, F.; Poluzzi, V.; Fabi, M.; et al. Understanding the environmental factors related to the decrease in Pediatric Emergency Department referrals for acute asthma during the SARS-CoV-2 pandemic. Pediatr. Pulmonol. 2022, 57, 66–74. [Google Scholar] [CrossRef]
- To, T.; Zhang, K.; Terebessy, E.; Zhu, J.; Licskai, C. Healthcare utilization in Canadian children and young adults with asthma during the COVID-19 pandemic. PLoS ONE 2023, 18, e0280362. [Google Scholar] [CrossRef] [PubMed]
- National Health Insurance. Administration Medical Quality Indicator Information Hospital Total Professional Medical Service Quality Report. 2023. Available online: https://www.nhi.gov.tw/Content_List.aspx?n=9ABC74CDF4F839F6&topn=23C660CAACAA159D (accessed on 1 September 2023).
- Ministry of Environment. Taiwan Air Quality Monitoring Network. 2023. Available online: https://www.moenv.gov.tw/Page/686030BBD5DFC8DD (accessed on 1 September 2023).
- Taipei City Statistical Database Query System Climatic Data. 2023. Available online: https://tsis.dbas.gov.taipei/statis/webMain.aspx?k=tpemain (accessed on 1 September 2023).
- Golan-Tripto, I.; Arwas, N.; Maimon, M.S.; Bari, R.; Aviram, M.; Gatt, D.; Goldbart, A. The effect of the COVID-19 lockdown on children with asthma-related symptoms: A tertiary care center experience. Pediatr. Pulmonol. 2021, 56, 2825–2832. [Google Scholar] [CrossRef] [PubMed]
- Groff, D.; Sun, A.; Ssentongo, A.E.; Ba, D.M.; Parsons, N.; Poudel, G.R.; Lekoubou, A.; Oh, J.S.; Ericson, J.E.; Ssentongo, P.; et al. Short-term and Long-term Rates of Postacute Sequelae of SARS-CoV-2 Infection: A Systematic Review. JAMA Netw. Open 2021, 4, e2128568. [Google Scholar] [CrossRef]
- Bartoňová, A.; Colette, A.; Zhang, H.; Fons, J.; Liu, H.-Y.; Brzezina, J.; Chantreux, A.; Couvidat, F.; Guerreiro, C.; Guevara, M.; et al. ETC/ATNI Report 2021/16: The COVID-19 Pandemic and Environmental Stressors in Europe: Synergies and Interplays. Available online: https://www.eionet.europa.eu/etcs/etc-atni/products/etc-atni-reports/etc-atni-report-16-2021-the-covid-19-pandemic-and-environmental-stressors-in-europe-synergies-and-interplays (accessed on 16 December 2023).
- Taiwan Centers of Disease Control. Infectious Disease Surveillance-Annual Report. 2023. Available online: https://www.cdc.gov.tw/Report/YearList/HalSp-frR_CAVqSn9SWzeQ (accessed on 1 September 2023).
- Ma, Y.; Zhao, H.; Su, Y. Ozone Pollution and Acute Exacerbation of Asthma in Residents of China: An Ecological Study. J. Asthma Allergy 2023, 16, 951–960. [Google Scholar] [CrossRef]
- Cheng, C.Y.; Tseng, Y.L.; Huang, K.C.; Chiu, I.M.; Pan, H.Y.; Cheng, F.J. Association between Ambient Air Pollution and Emergency Room Visits for Pediatric Respiratory Diseases: The Impact of COVID-19 Pandemic. Toxics 2022, 10, 247. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Lee, M. Low-to-moderate atmospheric ozone levels are negatively correlated with hospital visits by asthma patients. Medicine 2022, 101, e31737. [Google Scholar] [CrossRef]
- Stout, S.; Murphy, H.; Pandya, A.; Yeh, H.W.; Portnoy, J. The effect of coronavirus disease 2019 on asthma visits. Ann. Allergy Asthma Immunol. 2022, 128, 594–595. [Google Scholar] [CrossRef]
- Taylor, P.E.; Jacobson, K.W.; House, J.M.; Glovsky, M.M. Links between Pollen, Atopy and the Asthma Epidemic. Int. Arch. Allergy Immunol. 2007, 144, 162–170. [Google Scholar] [CrossRef]
- Poniedziałek, B.; Rzymski, P.; Zarębska-Michaluk, D.; Rogalska, M.; Rorat, M.; Czupryna, P.; Kozielewicz, D.; Hawro, M.; Kowalska, J.; Jaroszewicz, J.; et al. Short-term exposure to ambient air pollution and individual emergency department visits for COVID-19: A case-crossover study in Canada. Thorax 2023, 78, 459–466. [Google Scholar]
- Liu, Q.; Xu, C.; Ji, G.; Liu, H.; Shao, W.; Zhang, C.; Gu, A.; Zhao, P. Effect of exposure to ambient PM2.5 pollution on the risk of respiratory tract diseases: A meta-analysis of cohort studies. J. Biomed. Res. 2017, 31, 130–142. [Google Scholar] [PubMed]
- Kuo, C.Y.; Chan, C.K.; Wu, C.Y.; Phan, D.V.; Chan, C.L. The Short-Term Effects of Ambient Air Pollutants on Childhood Asthma Hospitalization in Taiwan: A National Study. Int. J. Environ. Res. Public Health 2019, 16, 203. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Wang, Y.; Shen, C.; Luo, J.; Yu, W. Decreased Incidence of Influenza During the COVID-19 Pandemic. Int. J. Gen. Med. 2022, 15, 2957–2962. [Google Scholar] [CrossRef] [PubMed]
- Health Promotion Administration. Global Youth Tobacco Survey. Available online: https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=1725&pid=9931 (accessed on 1 September 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).