Abstract
Introduction: Pulmonary diseases are amongst the most common causes of premature death and distressing disorders worldwide. This study aimed to detect the fastidious and routine infectious agents, and their drug resistance patterns in bronchoalveolar lavage (BAL) samples. Methods: A total of 44 BAL samples were collected by bronchoscopy from patients with respiratory disorders hospitalized at 2 teaching hospitals in Ilam, Iran. The samples were cultured on routine bacterial culture media to identify the bacterial agents and calculate the colony count. Antibiotic susceptibility was determined by disk diffusion method according to the CLSI protocol. PCR was used to detect the fastidious bacteria Mycoplasma pneumoniae and Chlamydia pneumoniae using the 16srRNA specific primers and Legionella pneumophila using the mip specific primers. Results: Overall, 100 bacterial isolates were isolated by culture from the 44 BAL samples including: Staphylococcus aureus (24, 31.2%), Streptococcus pyogenes (18, 23.4%), Enterococcus spp. (11, 14.3%), Acinetobacter baumannii (11, 14.3%), Pseudomonas aeruginosa (11, 14.3%), Enterococcus spp. (10, 13%), Micrococcus spp. (5, 6.5%), Staphylococcus epidermidis (5, 6.5%) and Klebsiella pneumoniae (5, 6.5%). PCR detected 4 positive samples (9.1%) for Chlamydia pneumoniae but no positive cases for Mycoplasma pneumoniae and Legionella pneumophila. Acinetobacter baumannii showed the highest resistance rate (81.8%) to aztreonam and ceftazidime. Seventy-five percent of the Staphylococcus aureus isolates were resistant to cefoxitin (MRSA) and 83.3% had the mecA gene. Vancomycin resistance was observed in 27.3% of the Enterococcus species (VRE). Resistance to piperacillin, cefotaxime, ciprofloxacin and imipenem was observed in 54.5%, 45.5%, and 36.4% of the Pseudomonas aeruginosa isolates, respectively. The frequency of organisms isolated from the ICU was higher (46%) than from other wards. Conclusions: The presence of MRSA, cephalosporins-resistant Enterobacteriaceae as well as Pseudomonas aeruginosa and Acinetobacter baumannii resistant against piperacillin, imipenem, cefotaxime, aztreonam and ciprofloxacin amongst different wards, especially the ICU ward of the surveyed hospitals, is a major healthcare concern and it is necessary to wisely scrutinize the preventive strategies for antibiotic resistant infections.
Introduction
Hospitals are the potential centers for the transmission of infectious agents to humans through various routes which can occasionally cause deadly epidemics. All respiratory pathogens are potential causes of nosocomial infections []. Nosocomial infections are becoming increasingly important and pose a serious challenge to healthcare systems worldwide. The emergence of recurrent and emerging diseases, the increase in the number of hospitals, microbial resistance and the need for diverse medical services make the occurrence of infections associated with medical services inevitable. Hospitalized patients are at risk for nosocomial infections. The incidence rate of nosocomial infections among hospitalized patients is estimated to be 7% in developed countries and 10% in developing countries [].
Risk factors for nosocomial infections fall into two main categories: risk factors that are unavoidable (including age and the underlying disorders associated with hospitalization) and those that can be managed and controlled (including the duration of hospitalization, catheter use, broad-spectrum antibiotic application, as well as the application of antiseptic techniques including hand washing by healthcare workers) []. The three most common nosocomial infections are urinary tract, respiratory, and bloodstream infections []. Immuno-compromised patients with underlying medical conditions, and those who have undergone invasive surgery procedures are most prone to respiratory infections [,]. Approximately one-third of nosocomial infections in the intensive care unit (ICU) are associated with respiratory infections, with pneumonia being the most common nosocomial infection in this ward. The incidence rate of pneumonia and the lower respiratory tract bacterial infection can be used as criteria for evaluating the infection prevention measures and nosocomial infection control policies.
Due to the presence of resistant bacteria in various wards, particularly in ICU, repeated susceptibility examination of infection-causing microorganisms to commonly used antibiotics is necessary []. This study therefore aimed to detect the fastidious and routine infectious agents, and their drug resistance patterns in the bronchoalveolar lavage (BAL) samples of patients with respiratory disorders hospitalized at 2 teaching hospitals (Imam Khomeini and Shahid Mostafa Khomeini hospitals) in Ilam, Iran.
Methods
Sample collection and storage
A total of 44 BAL samples (one sample from each patient) were obtained using bronchoscopy from patients admitted to different wards of Shahid Mostafa Khomeini and Imam Khomeini hospitals in Ilam, Iran from September 2014 to August 2015.
The microbiological plates for the BAL sample of each patient were transferred to the microbiology laboratory of Ilam University of Medical Sciences in less than 6 hours, and the isolated colonies were kept at −80 °C for future identification of bacterial agents using microbial culture and PCR, followed by the antibiotic susceptibility testing of the cultured bacteria.
Bacterial identification using culture
To identify bacterial agents, BAL samples were cultured on blood agar, chocolate agar, McConkey’s agar, mannitol salt agar and gentamicin-containing blood agar (for the isolation of Streptococcus pneumoniae) and incubated at 37 °C for 24 hours. Gram staining, catalase and oxidase tests, as well as the differential tests including sugar fermentation, urease, citratease enzyme production, indole production, coagulase test, etc. were used to identify the bacteria to the species level.
Antibiotic susceptibility testing of the cultured bacteria
Susceptibility against the 15 antibiotics listed below was determined using disk agar diffusion (DAD) method according to CLSI’s guidelines: [] gentamicin (30 µg), cefoxitin (30 µg), imipenem (10 µg), nitrofurantoin (100 µg), aztreonam (30 µg), oxacillin (1 µg), vancomycin (5 µg), piperacillin (10 µg), ciprofloxacin (5 µg), cefotaxime-clavulanic acid (30-10 µg), amikacin (30 µg), ceftriaxone (30 µg), co-trimoxazole (25 µg), cefotaxime (30 µg), ceftazidime (30 µg) (HiMedia, India).
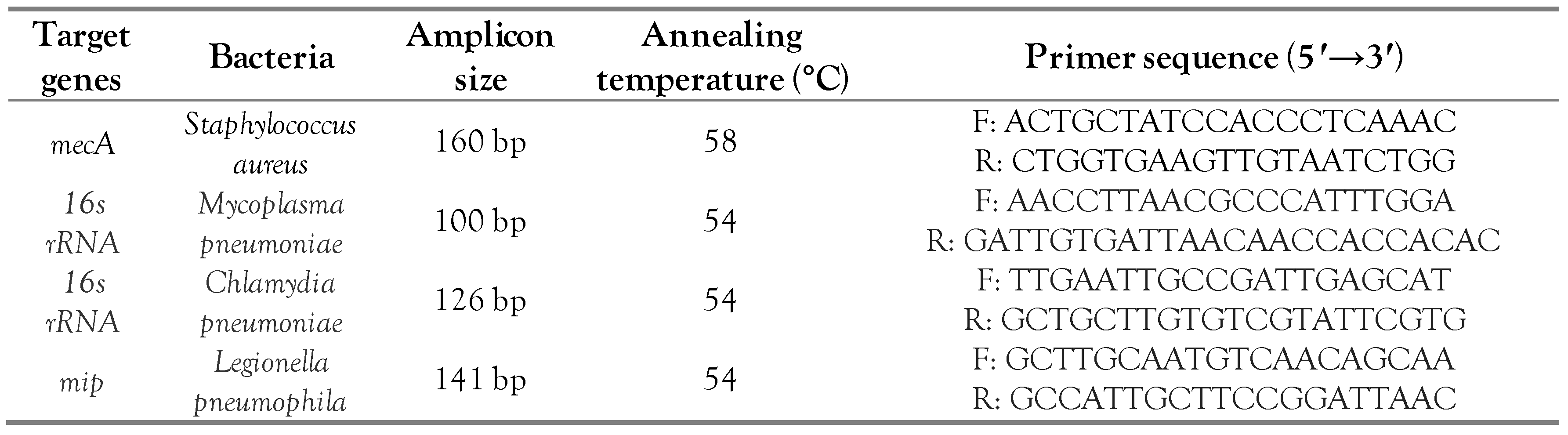
In case of Staphylococcus aureus isolates which showed cefoxitin resistance in the DAD method, PCR using the mecA-specific primers was used to confirm methicillin resistance. For this purpose, DNA of the cefoxitin-resistant S. aureus isolates was extracted by boiling method [], and PCR was carried out as described in the next section (identification of the fastidious bacteria using PCR), except that the annealing temperature was 58 °C here. The mecA-specific primers are shown in Table 1.

Table 1.
Primers used for the identification of methicillin resistant S. aureus isolates as well as fastidious bacteria in the BAL samples.
Identification of the fastidious bacteria using PCR
DNA were extracted from the BAL samples using a standard protocol as mentioned in a previous study []. PCR amplifications were performed in a final volume of 25 μL consisting of 1 μL of the DNA template, 1 μL of each primer, 8 μL of master mix (Taq DNA polymerase Master-mix Red, MgCl2; Amplicon, UK). The total volume was adjusted to 25 μL using distilled deionized water. PCR amplification was performed in a DNA thermal cycler (PeqLab, Germany) and included an initial denaturation step at 95 °C for 4 min; 35 alternating cycles of denaturation at 95 °C for 45 s, annealing at 54 °C for 45 s, and extension at 72 °C for 30 s. A final extension step at 72 °C was followed for 3 min. The results were finally analyzed by electrophoresis. The sequences of the 16srRNA specific primers for the identification of Mycoplasma pneumoniae and Chlamydia pneumoniae and the mip specific primers for the identification of Legionella pneumophila are listed in Table 1.
Statistical analysis
Data were expressed as mean ± standard deviation (SD). Results were compared using Chi square test where appropriate. A p value ≤0.05 was considered as statistically significant.
Results
Demographic and clinical information of the hospitalized patients
In this study, out of the 44 BAL samples (from 44 patients), 42 (95.5%) were collected from Mostafa Khomeini Hospital and 2 (4.5%) from Imam Khomeini Hospital. A total of 15 samples (out of the 44 BAL samples; 34.1%) were from the ICU ward, 2 samples (4.5%) from the cardiac care unit (CCU) ward, and 27 samples from other wards. In this study, 32 patients (72.7%) out of the 44 patients were male and 12 (27.3%) were female with an age range of 18-90 years old. The length of hospital stay was one week for 6 patients (13.6%), less than one week for 27 patients (61.4%) and more than one week for 11 patients (25%). Thirty-five patients (79.5%) were smokers and 9 (20.5%) were non-smokers.
Frequency of the microorganisms isolated from BAL culture
In this study, 100 bacterial isolates were isolated by culture out of the 44 BAL samples which, in the order of frequency, included: Staphylococcus aureus(24, 24%), Streptococcus pyogenes (18, 18%), Enterococcus spp. (11, 11%), Acinetobacter baumannii (11, 11%), Pseudomonas aeruginosa (11, 11%), Enterobacter spp. (10, 10%), Micrococcus spp. (5, 5%), Staphylococcus epidermidis (5, 5%) and Klebsiella pneumoniae (5, 5%).
The highest frequencies of the isolated bacteria were respectively found in the ICU (46, 46%), male internal ward (34, 34%), female internal ward (16, 16%), and CCU (4, 4%). The most frequently isolated bacteria from each ward and their frequency is shown in Figure 1. No significant association was found between the frequency of the isolated bacteria and the wards (p=0.127).
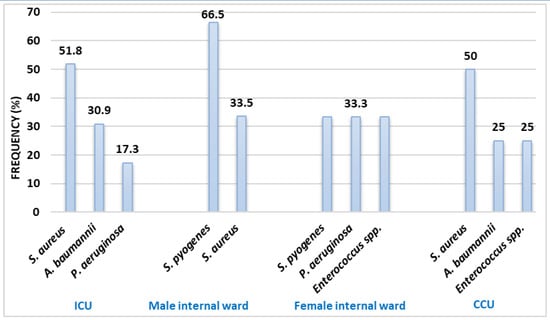
Figure 1.
Frequency distribution of the most frequently isolated bacteria from BAL cultures based on hospital wards. CCU—cardiac care unit; ICU—intensive care unit.
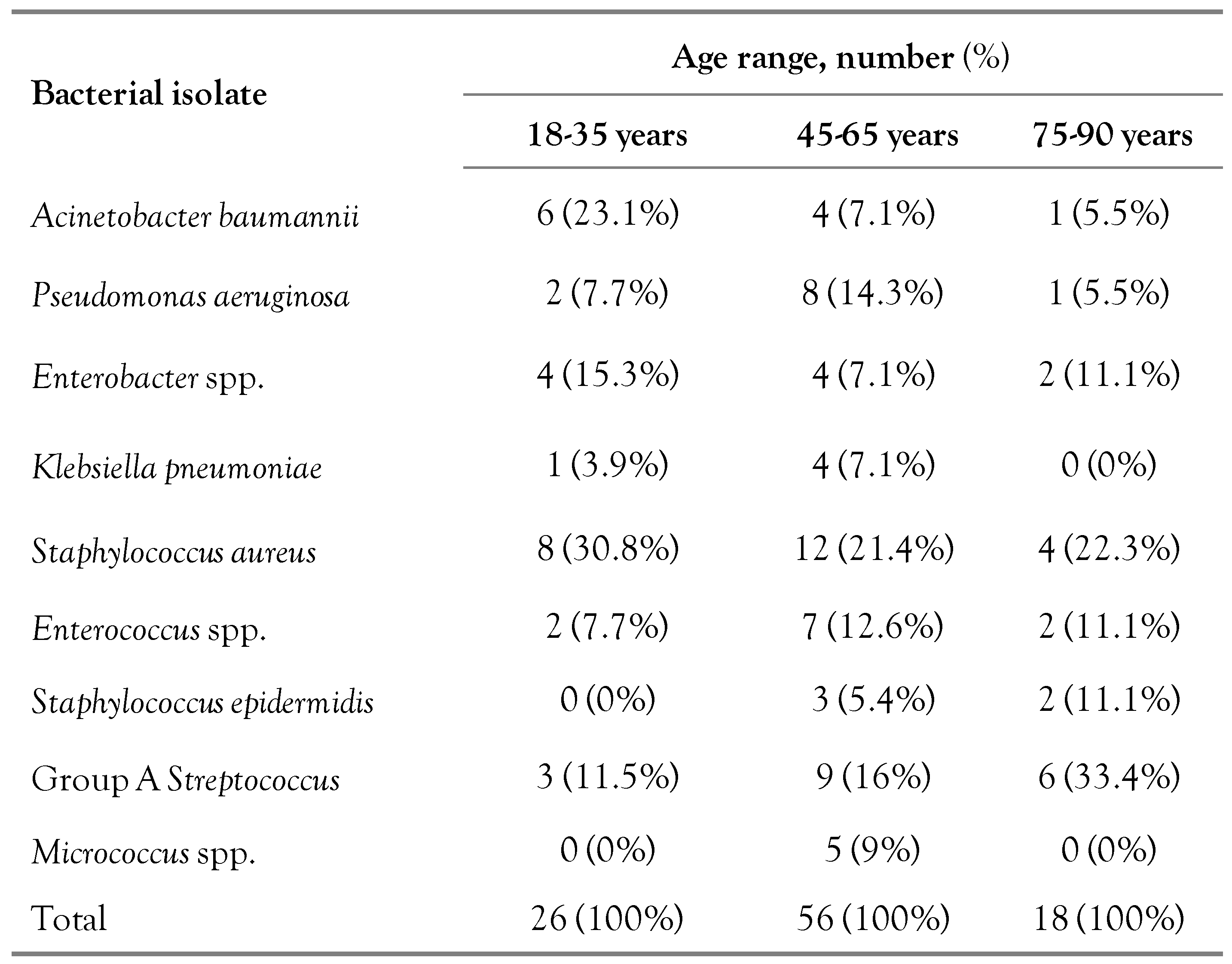
Frequency of the bacteria isolated from BAL culture based on patients’ age range is shown in Table 2. Frequency of Acinetobacter baumannii was significantly higher in patients with an age range of 18-35 years old (p=0.015). No significant association was found between the frequencies of other bacteria with any age ranges.

Table 2.
Frequency of the bacteria isolated from BAL culture based on the patients’ age range.
Frequency of the isolated bacteria based on the smoking status, gender, duration of hospital stay, are shown in Supplementary Table S1, Supplementary Table S2, and Supplementary Table S3, respectively. No significant association was found between the frequency of the isolated bacteria and the smoking status, gender, and duration of hospital stay (p=0.286, 0.701, and 0.462, respectively).
Antibiotic resistance patterns of the bacteria isolated from BAL using the DAD method
The antibiotic resistance pattern of bacteria isolated from BAL culture are shown in Figure 2. No resistance was found neither against nitrofurantoin and piperacillin among Enterobacter spp. nor against cefotaxime, imipenem, gentamicin, amikacin, ceftriaxone, nitrofurantoin, piperacillin among K. pneumoniae isolates.
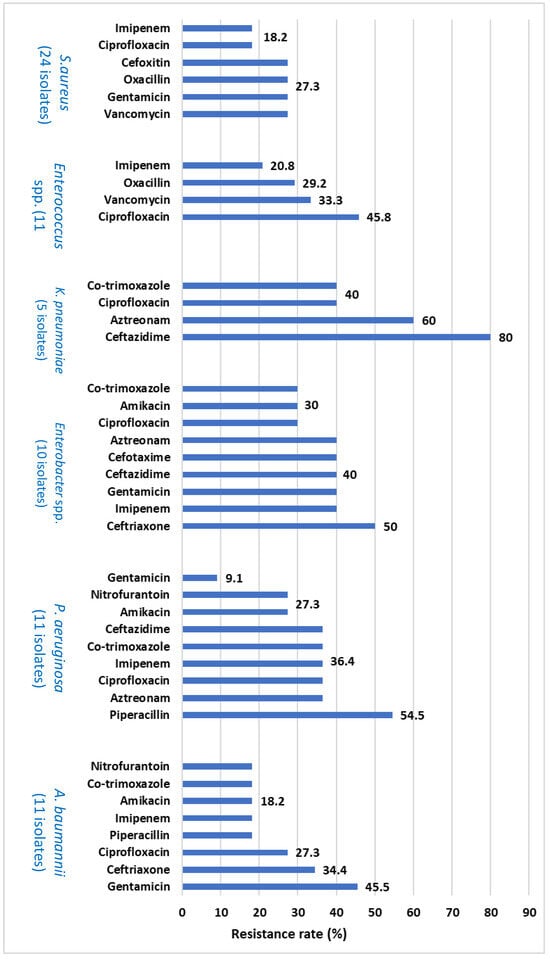
Figure 2.
Antibiotic resistance pattern of bacteria isolated from BAL culture.
The antibiotic resistance pattern of bacteria isolated from BAL culture are shown in Figure 2. No resistance was found neither against nitrofurantoin and piperacillin among Enterobacter spp. nor against cefotaxime, imipenem, gentamicin, amikacin, ceftriaxone, nitrofurantoin, piperacillin among K. pneumoniae isolates.
Among the 24 S. aureus isolated by culture, 18 (75%) were resistant to cefoxitin and detected as methicillin-resistant S. aureus (MRSA) and 3 out of the 11 Enterococcus isolates (27.3%) were resistant to vancomycin and detected as vancomycin-resistant enterococci (VRE) in disk diffusion method.
The total rate of resistance among all bacterial isolates was 57.5% to cefoxitin, 56.8% to aztreonam and ceftazidime, 48.6% to cefotaxime, 37.5% to vancomycin, 35.1% to ceftriaxone, 33.8% to ciprofloxacin, 32.5% to gentamicin, 29.7% to co-trimoxazole, 27.5% to oxacillin, 24.7% to imipenem, amikacin and piperacillin, 16.2% to nitrofurantoin, and finally 6.9% to cefotaxime-clavulanic acid.
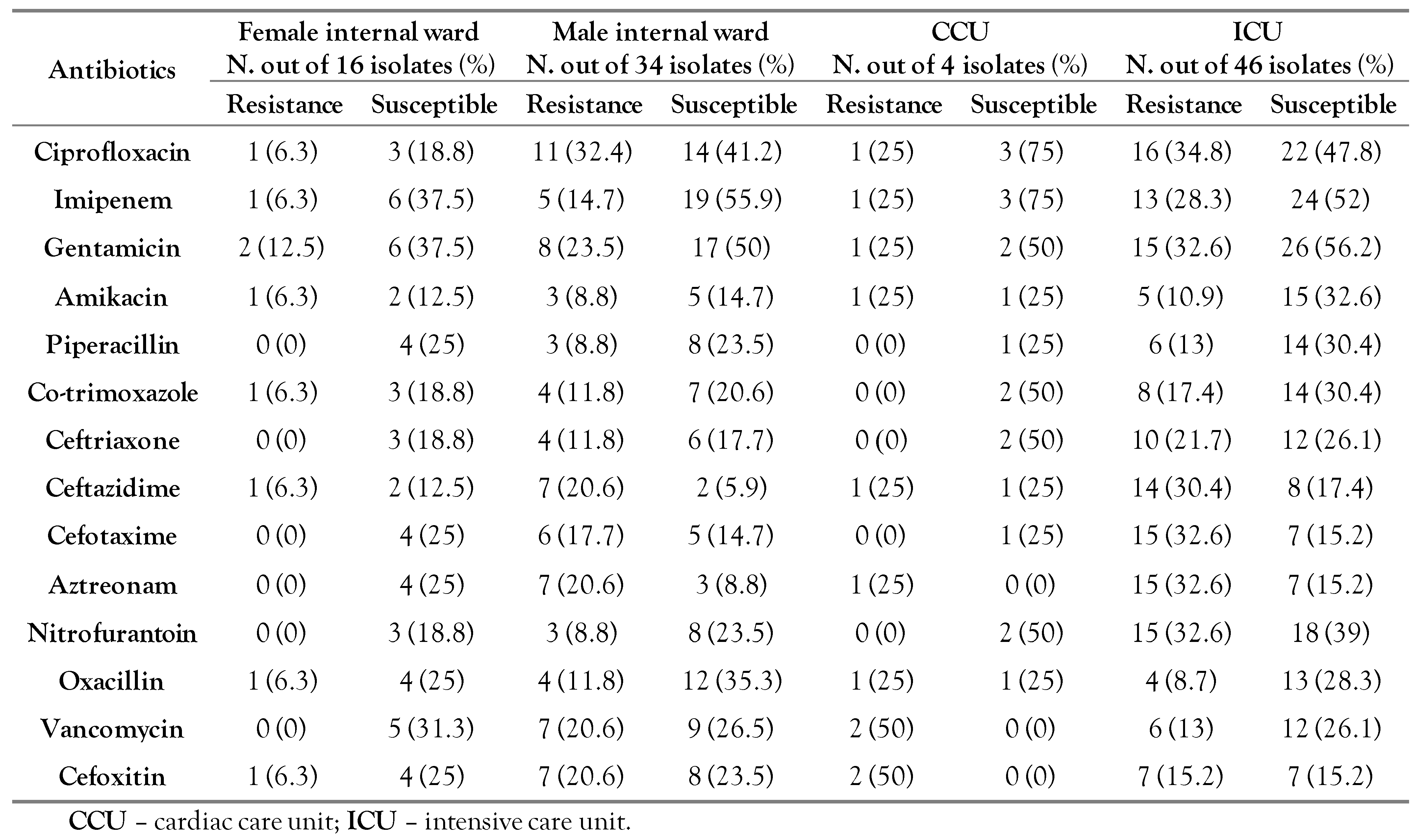
The antibiotic resistance patterns of the isolated bacteria among different hospital wards are shown in Table 3.

Table 3.
Antibiotic resistance patterns of the isolated bacteria among different hospital wards.
PCR detection of fastidious bacteria in the BAL sample
PCR results showed negative results for Mycoplasma pneumoniae using the 16 srRNA-specific primers and also for Legionella pneumophila using the mip-specific primers. However, 4 samples (9.1%) were positive for Chlamydia pneumoniae using the 16 srRNA-specific primers. The frequency of Chlamydia pneumoniae was significantly higher among patients with an age range of 45-65 years (p=0.036). Methicillin resistance (possessing the mecA gene) was detected as 83.3% in PCR, whilst it was found as 75% in the DAD method. Moreover, 2 S. aureus isolates (8%) were not resistant to cefoxitin despite having the mecA gene. On the other hand, 4 isolates (16.7%) lacked the mecA gene while being resistant to cefoxitin.
Discussion
The issue of nosocomial infections is one of the adverse effects of patient care, and has gained official attention in the fourth century AD with the establishment of hospitals. Prolonged hospital stay, as well as the use of invasive maintenance and monitoring devices in the ICU ward are amongst the main contributing factors to the increased risk of nosocomial infections, which in turn increase the morbidity and mortality rates among hospitalized patients as well as impose financial burden on the healthcare system [,] Considering the increasing number of patients admitted to the ICU ward and the use of high doses of antibiotics administered to the patients in this ward, it seems that the prevalence of antibiotic resistant pathogens is expanding in this particular ward throughout the world. The average length of hospital stay for patients with nosocomial pneumonia is one to two weeks longer than that in other patients [].
The most common nosocomial infections threatening patients admitted to the ICU ward are respiratory associated infections.
In this study, out of the 44 BAL samples cultured, 100 isolates, including 37 Gram-negative and 63 Gram-positive bacteria were identified. The most frequent bacterial isolates included S. aureus (24, 24%), S. pyogenes (18, 18%), A. baumannii, Pseudomonas and Enterococcus spp. (11, 11% each), Enterobacter spp. (10, 10%), and K. pneumoniae (5, 5%), respectively.
In a study in Italy, Acinetobacter baumannii (18.6%), Staphylococcus aureus (15.2%), Pseudomonas aeruginosa (14.2%), and Klebsiella pneumoniae (10.9%) were the most common microorganisms isolated from the lower respiratory tract infections among hospitalized patients []. In another study in Taiwan, Pseudomonas aeruginosa (1574 isolates), Klebsiella pneumoniae (1226), Acinetobacter baumannii (627) and Escherichia coli (476) accounted for 73.1% of 5342 Gram-negative respiratory pathogens []. In a study conducted in Iran, the most prevalent isolated bacteria from BAL samples were as follows: M. tuberculosis (25%), P. aeruginosa (15%), and S. aureus (14%) []. In another study in Iran, A. baumannii was the most prevalent organism (37%) isolated from hospital-acquired pneumonia, followed by S. aureus (27.8%), P. aeruginosa (24.1%), and E. coli (11.1%) []. These results were consistent with our study. In the ICU ward, some factors such as reduced consciousness level, connection to the endotracheal tube, and mechanical ventilation increase the risk of pneumonia in patients.
In our study, the highest frequency of bacteria (56%) was found in patients with a mean age of 45-65 years and the most common bacterium isolated from this age group was S. aureus (21.4%). In a study conducted in China on 3370 cases of elderly patients, the rate of nosocomial infection was reported as 3.3% (80 among 2413 patients), pneumonia was the most common nosocomial infection and S. aureus and P. aeruginosa were the most commonly isolated Gram positive and Gram negative bacteria, respectively. It was concluded in this study that the improvement of the nutritional status of the elderly patients is effective in reducing the risks of nosocomial infections among these patients [].
In this study, it was observed that there was no significant relationship between smoking and the frequency of bacteria isolated from the BAL samples (p=0.286). It is suspected that apart from smoking, factors such as air dust in Ilam, could be predisposing factors for respiratory infections.
In a study in Arak in 2005, no significant relationship was found between smoking and lower respiratory tract infections [], which is consistent with the present study. On the other hand, a review article has shown direct associations between smoking and the increased risk of many infections including respiratory infections [].
A. baumannii isolated in the mentioned study in Arak showed the highest resistance to ceftazidime (81.8%) aztreonam (63.6%), cefotaxime (45.5%), respectively. Resistance to betalactams in A. baumannii can be attributed to the horizontal transfer of resistance genes and the differential expression of intrinsic genes. In a study in 2021 in Iran, all the Gram negative nosocomial bacteria, including A. baumannii were susceptible to colistin; however, the highest rate of resistance among these Gram negative bacteria was observed for levofloxacin, cefotaxime, and ceftriaxone, respectively. On the other hand, S. aureus isolates showed a high rate of resistance to penicillin (93%), levofloxacin, azithromycin and cefoxitin (80% each) [].
The low gentamicin resistance in our study, which contradicts with the results of studies from other parts of the world, but is consistent with some studies in Iran [], might be due to a decrease in the use of gentamicin and a predilection for the third-generation cephalosporins and quinolones in recent years for the treatment of infections in Iran. In our study, the highest prevalence of MRSA was in the ICU ward, which could be due to the long-term hospitalization of patients, multiple comorbidities, the overuse of antibiotics, invasive treatment methods and the transfer of colonized patients from one hospital to another. These factors increase the risk of bacterial colonization and thus lead to the emergence of resistant strains.
Among Gram-positive bacteria, the highest and lowest resistance rates were associated to cefoxitin (71.4%) and oxacillin (61.9%), respectively. Resistance to cefotaxime was significantly higher in the ICU ward of the hospitals (p=0.011).
One result to be noted in this study was that there were some variations in the percentage of methicillin resistance as reported by the DAD method and the molecular detection of the mecA gene. For instance, 83.3% of the S. aureus isolates were detected to have the mecA gene using PCR, whilst only 75% were found to be cefoxitin resistant by the DAD method. Moreover, 2 S. aureus isolates (8%) were susceptible to cefoxitin despite having the mecA gene. In addition, 4 isolates (16.7%) lacked the mecA gene while being resistant to cefoxitin. These results indicate that the presence of the mecA gene is not 100 percent associated with its phenotypic expression and that resistance to methicillin (cefoxitin) is not 100 percent related to the presence of the mecA gene as also reported by other studies [,,] This shows that other methicillin resistance mechanisms, including the presence of some other genes, or the over-expression of betalactamase enzymes might contribute to methicillin resistance among staphylococcal isolates [].
PCR results showed negative results for M. pneumoniae and L. pneumophila among the BAL samples. The low rate of Mycoplasma detection in our study, compared to other studies in Iran or other parts of the world, may be related to differences in the detection method since using serological tests, along PCR and culture, increases the sensitivity for the detection of this microorganism. [,] In the study by Ieven et al., adhesin P1-associated primers showed a higher sensitivity compared to the 16S rRNA primers, which might be due to the presence of multiple copies of this adhesin in M. pneumoniae [].
The lack of L. pneumophila detection in the present study might be due to the fact that this organism is a facultative intracellular bacterium and will only be found in the alveolar space and lower respiratory tract secretions after multiplication within macrophages and their rupture. The use of antibiotics in patients can inhibit the bacterial growth followed by their clearance by the immune system. This can, thus, interfere with the detection of bacteria using different methods, including PCR.
This study presented some limitations including financial resources which restricted the sample collection to two hospitals, and limited the range of routinely un-culturable bacteria detected in the BAL samples. In addition, access to different wards of the hospital and the patients’ clinical documentations was not freely possible, which impaired a comprehensive study on the association between the prevalence of the isolated bacteria and different aspects of the patients’ disease status.
Conclusions
This study aimed to detect the bacterial infectious agents and their drug resistance patterns in bronchoalveolar lavage (BAL) samples of hospitalized patients in 2 hospitals in Iran.
Due to the presence of MRSA, cephalosporin-resistant Enterobacteriaceae as well as Pseudomonas aeruginosa and Acinetobacter baumannii resistant against piperacillin, imipenem, cefotaxime, aztreonam and ciprofloxacin amongst different wards of the hospitals, especially the ICU ward, it is necessary to update the antimicrobial susceptibility patterns of nosocomial microorganisms and to wisely scrutinize the infectious prevention strategies among infection centers.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/doi/s1.
Author Contributions
IP conceptualized the study design, ZT collected and analyzed the data, PA prepared the manuscript. NS, SG, EGPK contributed in the study design. BSK helped in drafting the manuscript. All authors read and approved the final version of the manuscript.
Funding
This research was financially supported by the Ilam University of Medical Sciences. The funder was not involved in the study design; collection, management, analysis, and interpretation of data; writing of the report; and the decision to submit the report for publication.
Acknowledgments
The authors would like to thank the laboratory staff of Shahid Mostafa Khomeini and Imam Khomeini hospitals in Ilam, Iran for their collaboration in data collection of this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Flanders, S.A.; Collard, H.R.; Saint, S. Nosocomial pneumonia: State of the science. Am J Infect Control. 2006, 34, 84–93. [Google Scholar] [CrossRef]
- Pezhman, B.; Fatemeh, R.; Amir, R.; Mahboobeh, R.; Mohammad, F. Nosocomial infections in an Iranian educational hospital: An evaluation study of the Iranian nosocomial infection surveillance system. BMC Infect Dis. 2021, 21, 1256. [Google Scholar] [CrossRef] [PubMed]
- Auerbach, P.S. Wilderness Medicine E-Book: Expert Consult Premium Edition-Enhanced Online Features. Elsevier Health Sciences, 2011. [Google Scholar]
- Berenholtz, S.M.; Pronovost, P.J.; Lipsett, P.A.; et al. Eliminating catheter-related bloodstream infections in the intensive care unit. Crit Care Med. 2004, 32, 2014–2020. [Google Scholar] [CrossRef] [PubMed]
- American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005, 171, 388–416. [Google Scholar] [CrossRef] [PubMed]
- Jalalpour, S.; Kermanshahi, R.K.; Nouhi, A.S.; Esfahani, H.Z. Surveying the frequency of β-lactamase enzyme and antibiotic sensitivity pattern in isolated pathogen bacteria from low and high hospital contact surfaces. Pejouhandeh. 2010, 15, 77–82. [Google Scholar]
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Fifth Informational Supplement. M100S25; CLSI: Wayne, PA, USA, 2021. [Google Scholar]
- Asadollahi, P.; Jabalameli, F.; Beigverdi, R.; Emaneini, M. Assessment of disinfectant and antibiotic susceptibility patterns and multi-locus variable number tandem repeat analysis of Staphylococcus epidermidis isolated from blood cultures. Iran J Microbiol. 2018, 10, 90–97. [Google Scholar]
- Marsh, R.L.; Kaestli, M.; Chang, A.B.; et al. The microbiota in bronchoalveolar lavage from young children with chronic lung disease includes taxa present in both the oropharynx and nasopharynx. Microbiome. 2016, 4, 37. [Google Scholar] [CrossRef]
- Kollef, M.H.; Torres, A.; Shorr, A.F.; Martin-Loeches, I.; Micek, S.T. Nosocomial infection. Crit Care Med. 2021, 49, 169–187. [Google Scholar] [CrossRef]
- de la Varga-Martínez, O.; Gómez-Sánchez, E.; Muñoz, M.F.; et al. Impact of nosocomial infections on patient mortality following cardiac surgery. J Clin Anesth. 2021, 69, 110104. [Google Scholar] [CrossRef]
- Unal, S.; Garcia-Rodriguez, J.A. Activity of meropenem and comparators against Pseudomonas aeruginosa and Acinetobacter spp. isolated in the MYSTIC Program, 2002-2004. Diagn Microbiol Infect Dis. 2005, 53, 265–271. [Google Scholar] [CrossRef]
- Santella, B.; Serretiello, E.; De Filippis, A.; et al. Lower respiratory tract pathogens and their antimicrobial susceptibility pattern: A 5-year study. Antibiotics 2021, 10, 851. [Google Scholar] [CrossRef]
- Kuo, S.C.; Liu, C.E.; Lu, P.L.; et al. Activity of ceftolozane-tazobactam against Gram-negative pathogens isolated from lower respiratory tract infections in the Asia-Pacific region: SMART 2015-2016. Int J Antimicrob Agents. 2020, 55, 105883. [Google Scholar] [CrossRef] [PubMed]
- Imani Fooladi, A.; Parvizi, E.; Soltanpour, M.; Ahmadi, A. Study of prevalence and antimicrobial susceptibility pattern of polybacterial pneumonia. Tehran Univ Med J. 2015, 73, 632–638. [Google Scholar]
- Mazloomirad, F.; Hasanzadeh, S.; Sharifi, A.; Nikbakht, G.; Roustaei, N.; Khoramrooz, S.S. Identification and detection of pathogenic bacteria from patients with hospital-acquired pneumonia in southwestern Iran; evaluation of biofilm production and molecular typing of bacterial isolates. BMC Pulm Med. 2021, 21, 408. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Ren, L.; Zou, J. Risk factors and prevention strategies of nosocomial infection in geriatric patients. Can J Infect Dis Med Microbiol. 2019, 2019, 6417959. [Google Scholar] [CrossRef]
- Mohammad Shafiei, P.; Baserisalehi, M.; Mobasherizade, S. Investigating the antibiotic resistance prevalence and phenotypic and genotypic evaluation of AcrAB-OprM efflux pump in multidrug-resistant in clinical isolates of Moraxella catarrhalis in Kazerun City, Iran. Iran J Med Microbiol. 2020, 14, 388–407. [Google Scholar] [CrossRef]
- Jiang, C.; Chen, Q.; Xie, M. Smoking increases the risk of infectious diseases: A narrative review. Tob Induc Dis. 2020, 18, 60. [Google Scholar] [CrossRef]
- Keivanfar, M.; Zibanejad, N.; Rahimi, H.; Babaei, S.; Emadoleslami, M.S.; Reisi, M. Treatment protocol of ventilator-associated pneumonia based on microbial susceptibility in pediatric intensive care unit, Isfahan, Iran. Int J Pediatr. 2020, 8, 12039–12051. [Google Scholar]
- Broekema, N.M.; Van, T.T.; Monson, T.A.; Marshall, S.A.; Warshauer, D.M. Comparison of cefoxitin and oxacillin disk diffusion methods for detection of mecA-mediated resistance in Staphylococcus aureus in a large-scale study. J Clin Microbiol. 2009, 47, 217–219. [Google Scholar] [CrossRef]
- Uddin, M.; Ahn, J. Associations between resistance phenotype and gene expression in response to serial exposure to oxacillin and ciprofloxacin in Staphylococcus aureus. Lett Appl Microbiol. 2017, 65, 462–468. [Google Scholar] [CrossRef]
- Naccache, S.N.; Callan, K.; Burnham, C.A.; et al. Evaluation of oxacillin and cefoxitin disk diffusion and microbroth dilution methods for detecting mecA-mediated β-lactam resistance in contemporary Staphylococcus epidermidis isolates. J Clin Microbiol. 2019, 57, e00961–19. [Google Scholar] [CrossRef]
- Peacock, S.J.; Paterson, G.K. Mechanisms of methicillin resistance in Staphylococcus aureus. Annu Rev Biochem. 2015, 84, 577–601. [Google Scholar] [CrossRef]
- Tang, M.; Wang, D.; Tong, X.; et al. Comparison of different detection methods for Mycoplasma pneumoniae infection in children with community-acquired pneumonia. BMC Pediatr. 2021, 21, 90. [Google Scholar] [CrossRef]
- Ieven, M.; Ursi, D.; Van Bever, H.; Quint, W.; Niesters, H.; Goossens, H. Detection of Mycoplasma pneumoniae by two polymerase chain reactions and role of M. pneumoniaein acute respiratory tract infections in pediatric patients. J Infect Dis. 1996, 173, 1445–1452. [Google Scholar] [CrossRef]
© GERMS 2022.