Product Development Studies of Cranberry Seed Oil Nanoemulsion
Abstract
:1. Introduction
2. Materials and Methods
2.1. Drugs and Chemicals
2.2. Analytical Method
2.3. Component Screening
2.4. Construction of Pseudo-Ternary Phase Diagrams
2.5. Formulation Development
2.6. Characterization of Prepared CSO NEs
2.6.1. Thermodynamic Stability
2.6.2. Entrapment Efficiency (EE)
2.6.3. Light Transmittance and pH
2.6.4. Size, Polydispersity Index (PDI), and Surface Charge
2.6.5. Electron Microscopy
2.6.6. Rheology
2.7. Drug Release Study
2.8. Drug Permeation
2.9. Product Stability
2.10. Statistical Analysis
3. Result and Discussion
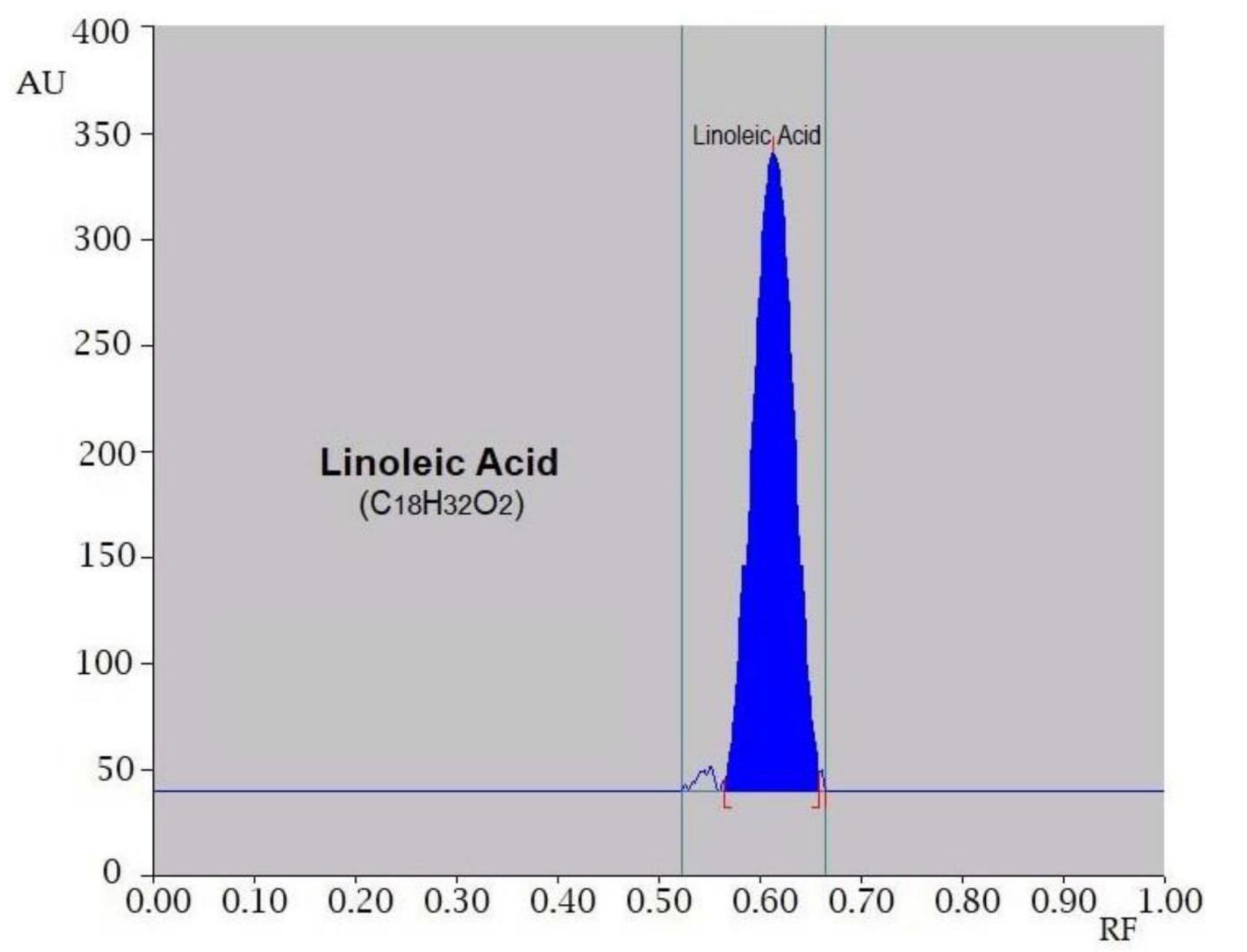
3.1. Analytical Method
3.2. Component Screening
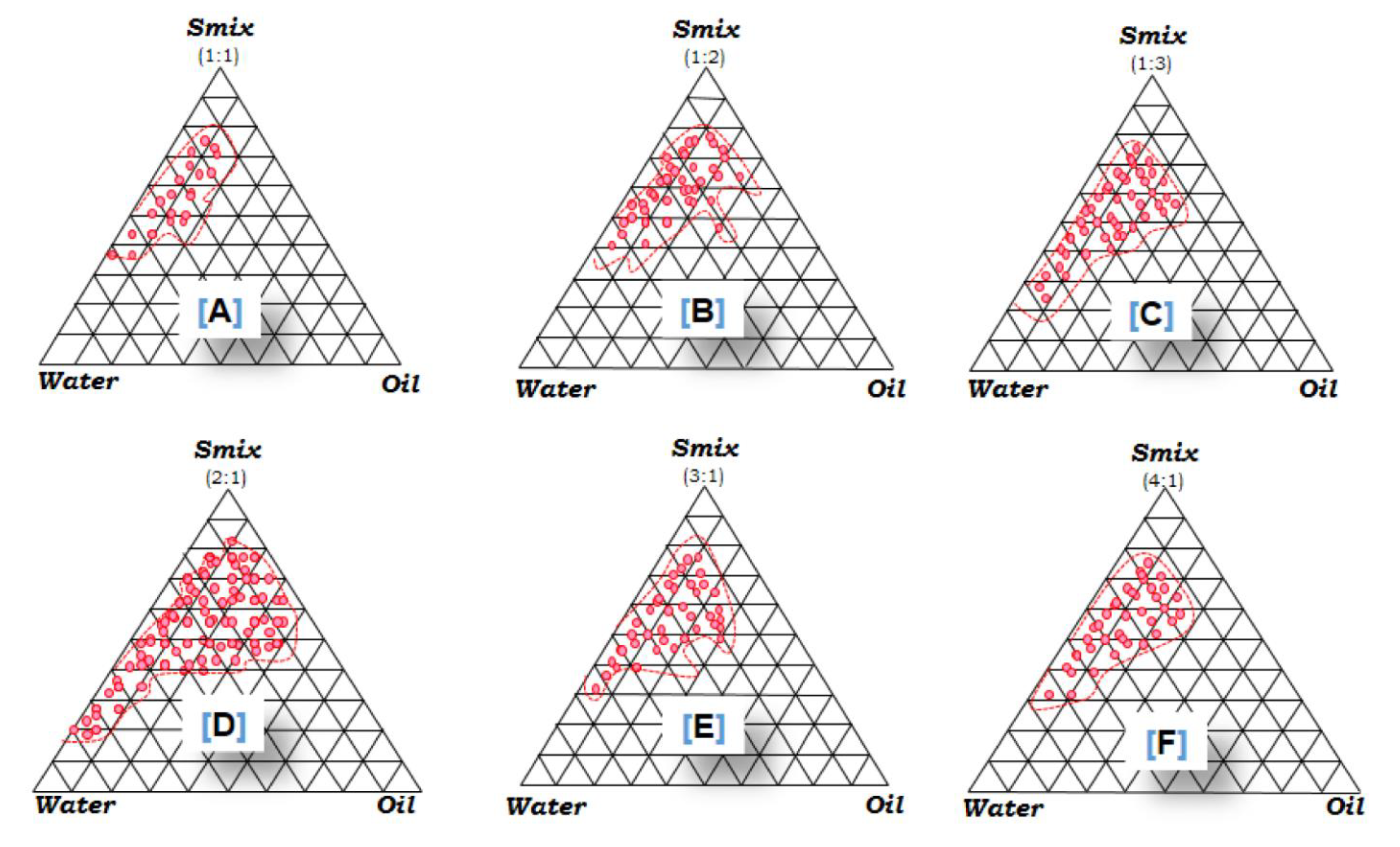
3.3. PPDs
3.4. Formulation Development
3.5. Characterization of Prepared CSO NE
3.5.1. Thermodynamic Stability
3.5.2. EE
3.5.3. Light Transmittance and pH
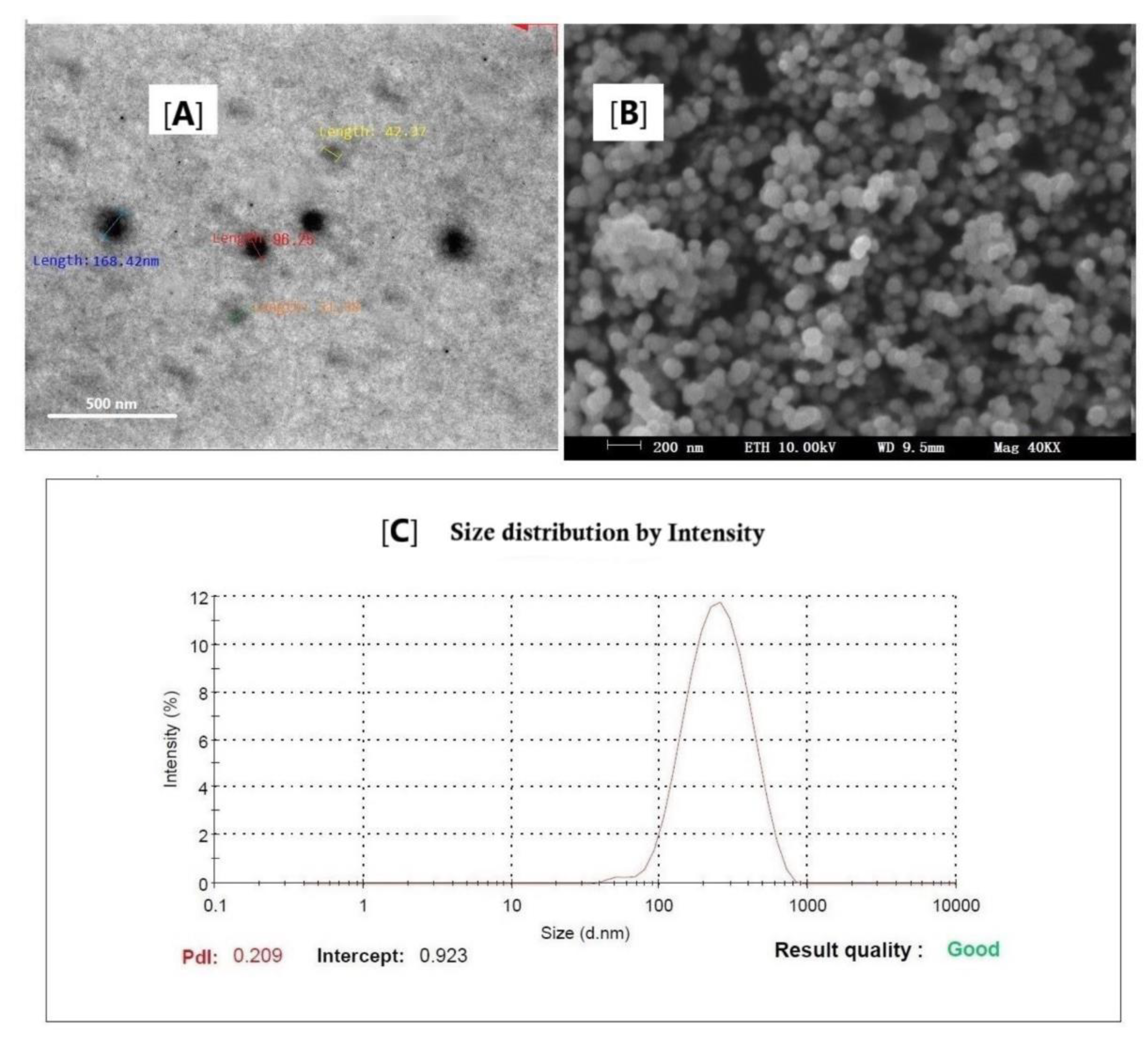
3.5.4. Size, PDI, and Surface Charge
3.5.5. Electron Microscopy
3.5.6. Rheology
3.6. Drug Release Study
3.7. Drug Permeation
3.8. Product Stability
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Agricultural Statistics Service (NASS). Agricultural Statistics Board; Cranberries (Annual reports, Fr Nt 4); Washington, DC, USA, 2001.
- Thyagarajan, P. Evaluation and Optimization of Cranberry Seed Oil Extraction Methods. Master’s Thesis, McGill University, Montréal, QC, Canada, 2012. [Google Scholar]
- Yu, L.L.; Zhou, K.K.; Parry, J. Antioxidant properties of cold-pressed black caraway, carrot, cranberry and hemp seed oils. Food Chem. 2005, 91, 723–729. [Google Scholar] [CrossRef]
- Connor, W.E. Importance of n-3 fatty acids in health and disease. Am. J. Clin. Nutr. 2000, 71, 171S–175S. [Google Scholar] [CrossRef] [PubMed]
- Aronson, W.J.; Glaspy, J.A.; Reddy, S.T.; Reese, D.; Heber, D.; Bagga, D. Modulation of omega-3/omega-6 polyunsaturated ratios with dietary fish oils in men with prostate cancer. Urology 2001, 58, 283–288. [Google Scholar] [CrossRef]
- Parry, J.; Su, L.; Luther, M.; Zhou, K.; Yurawecz, M.P.; Whittaker, P.; Yo, L. Fatty acid composition and antioxidant properties of cold-pressed marionberry, boysenberry, red raspberry and blueberry seed oils. J. Agric. Food Chem. 2005, 53, 566–573. [Google Scholar] [CrossRef] [PubMed]
- Bushman, B.S.; Phillips, B.; Isbell, T.; Ou, B.; Crane, J.M.; Knapp, S.J. Chemical composition of cranberry (Rubus spp.) seeds and oils and their antioxidant potential. J. Agric. Food Chem. 2004, 52, 7982–7987. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Yu, H.; Ma, Q.; Shen, S.; Das, U.N. Linoleic acid suppresses colorectal cancer cell growth by inducing oxidant stress and mitochondrial dysfunction. Lipids Health Dis. 2010, 9, E106. [Google Scholar] [CrossRef] [Green Version]
- Bilia, A.R.; Guccione, C.; Isacchi, B.; Righeschi, C.; Firenzuoli, F.; Bergonzi, M.C. Essential oils loaded in nanosystems: A developing strategy for a successful therapeutic approach. Evid. Based Complement. Altern. Med. 2014, 2014, E651593. [Google Scholar] [CrossRef] [Green Version]
- Shakeel, F.; Alamer, M.M.; Alam, P.; Alshetaili, A.; Haq, N.; Alanazi, F.K.; Alshehri, S.; Ghoneim, M.M.; Alsarra, I.A. Hepatoprotective effects of bioflavonoid luteolin using self-nanoemulsifying drug delivery system. Molecules 2021, 26, E7479. [Google Scholar] [CrossRef]
- Shakeel, F.; Salem-Bekhit, M.M.; Haq, N.; Alshehri, S. Nanoemulsification improves the pharmaceutical properties and bioactivities of niaouli essential oil (Melaleuca quinquenervia L.). Molecules 2021, 26, E4750. [Google Scholar] [CrossRef]
- Shakeel, F.; Alam, P.; Ali, A.; Alqarni, M.H.; Alshetaili, A.; Ghoneim, M.M.; Alshehri, S.; Ali, A. Investigating antiarthritic potential of nanostructured clove oil (Syzygium aromaticum) in FCA-induced arthritic rats: Pharmaceutical action and delivery strategies. Molecules 2021, 26, E7327. [Google Scholar] [CrossRef]
- De Sousa Marcial, S.P.; Carneiro, G.; Leite, E.A. Lipid-based nanoparticles as drug delivery system for paclitaxel in breast cancer treatment. J. Nanopart. Res. 2017, 19, E340. [Google Scholar] [CrossRef]
- Garcia, C.R.; Malik, M.H.; Biswas, S.; Tam, V.H.; Rumbaugh, K.P.; Li, W.; Liu, X. Nanoemulsion delivery system for enhanced efficacy of antimicrobials and essential oils. Biomater. Sci. 2022, 10, 633–653. [Google Scholar] [CrossRef] [PubMed]
- Barradas, T.N.; Silva, H.G.D.H. Nanoemulsions of essential oils to improve solubility, stability, and permeability: A review. Environ. Chem. Lett. 2021, 19, 1153–1171. [Google Scholar] [CrossRef]
- Fallen, H.; Jemaa, M.B.; Neves, M.A.; Isoda, H.; Nakajima, M. Formulation, physicochemical characterization, and anti-E. coli activity of food-grade nanoemulsions incorporating clove, cinnamon, and lavender essential oils. Food Chem. 2021, 359, E129963. [Google Scholar] [CrossRef] [PubMed]
- Cossetin, L.F.; Garlet, Q.I.; Velho, M.C.; Gundel, S.; Ourique, A.F.; Heinzmann, B.M.; Monteiro, S.G. Development of nanoemulsions containing Lavandula dentata or Myristica fragrans essential oils: Influence of temperature and storage period on physical-chemical properties and chemical stability. Ind. Crops Prod. 2021, 160, E113115. [Google Scholar] [CrossRef]
- Qadir, A.; Faiyazuddin, M.; Hussain, M.T.; Alshammari, T.M.; Shakeel, F. Critical steps and energetics involved in a successful development of a stable nanoemulsion. J. Mol. Liq. 2016, 214, 7–18. [Google Scholar] [CrossRef]
- Shafiq, S.; Shakeel, F.; Talegaonkar, S.; Ahmad, F.J.; Khar, R.K.; Ali, M. Development and bioavailability assessment of ramipril nanoemulsion formulation. Eur. J. Pharm. Biopharm. 2007, 66, 227–243. [Google Scholar] [CrossRef]
- Schmidts, T.; Nocker, P.; Lavi, G.; Kuhlmann, J.; Czermak, P.; Runkel, F. Development of an alternative, time and cost saving method of creating pseudoternary diagrams using the example of microemulsion. Coll. Surf. A. 2009, 340, 187–192. [Google Scholar] [CrossRef]
- Ricaurte, L.; de Jesús Perea-Flores, M.; Martinez, A.; Quintanilla-Carvajal, M.X. Production of high-oleic palm oil nanoemulsions by high-shear homogenization (microfluidization). Innov. Food Sci. Emerg. Technol. 2016, 35, 75–85. [Google Scholar] [CrossRef]
- Müller, R.H.; Mäder, K.; Gohla, S. Solid lipid nanoparticles (SLN) for controlled drug delivery—A review of the state of the art. Eur. J. Pharm. Biopharm. 2000, 50, 161–177. [Google Scholar] [CrossRef]
- Faiyazuddin, M.; Akhtar, N.; Akhter, J.; Suri, S.; Shakeel, F.; Shafiq, S.; Mustafa, G. Production, characterization, in vitro and ex vivo studies of babchi oil-encapsulated nanostructured solid lipid carriers produced by a hot aqueous titration method. Pharmazie 2010, 65, 348–355. [Google Scholar] [PubMed]
- Jain, S.; Kaur, A.; Puri, R.; Utreja, P.; Jain, A.; Bhide, M.; Ratnam, R.; Singh, V.; Patil, A.S.; Jayaraman, N.; et al. Poly propyl ether imine (PETIM) dendrimer: A novel non-toxic dendrimer for sustained drug delivery. Eur. J. Med. Chem. 2010, 45, 4997–5005. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, C.; Mehnert, W.; Lucks, J.S.; Müller, R.H. Solid lipid nanoparticles (SLN) for controlled drug delivery. I. Production, characterization and sterilization. J. Control. Release 1994, 30, 83–96. [Google Scholar] [CrossRef]
- Kosa, D.; Peto, A.; Fenyvesi, F.; Varadi, J.; Vecsernyes, M.; Gonda, S.; Vasas, G.; Feher, P.; Bacskay, I.; Ujhelyi, Z. Formulation of novel liquid crystal (LC) formulations with skin-permeation-enhancing abilities of Plantago lanceolate (PL) extract and their assessment on HaCaT cells. Molecules 2021, 26, E1023. [Google Scholar] [CrossRef]
- Theochari, I.; Mitsou, E.; Nikolic, I.; Ilic, T.; Dobricic, V.; Plesta, V.; Savic, S.; Xenakis, A.; Papadimitriou, V. Colloidal nanodispersions for the topical delivery of ibuprofen: Structure, dynamics and bioperformances. J. Mol. Liq. 2021, 334, E116021. [Google Scholar] [CrossRef]
- Osborne, D.W.; Musakhanian, J. Skin penetration and permeation properties of Transcutol®-neat or diluted mixtures. AAPS PharmSciTech. 2018, 19, 3512–3533. [Google Scholar] [CrossRef]
- Nurhidayati, L.G.; Nugroho, B.H.; Indrati, O. In vitro permeation test of diclofenac sodium nanoemulsion with combination Tween 80 and Transcutol. Curr. Trends Biotechnol. Pharm. 2020, 14, S48. [Google Scholar]
| Component | Phasic Area ± SD (mm2) |
|---|---|
| Tween 20 | 77.11 ± 2.40 |
| Tween 80 | 94.63 ± 1.91 |
| Labrasol * | 143.12 ± 4.17 |
| PEG-200 | 97.08 ± 4.26 |
| Capryol-90 | 81.74 ± 3.11 |
| Carbitol * | 73.45 ± 4.09 |
| Ethanol | 35.22 ± 1.84 |
| Cremophor EL | 42.16 ± 2.39 |
| Labrafac | 28.78 ± 3.54 |
| Formulation Matrix | Composition (%) of Selected Nanoemulsion | Smix Ratio | ||
|---|---|---|---|---|
| Oil (CSO) | Smix | Water | ||
| CNE1 | 10 | 40 | 50 | 1:1 |
| CNE2 | 10 | 44 | 46 | 1:2 |
| CNE3 | 10 | 38 | 52 | 1:3 |
| CNE4 | 10 | 39 | 51 | 2:1 |
| CNE5 | 10 | 41 | 49 | 3:1 |
| CNE6 | 10 | 42 | 48 | 4:1 |
| Formulation Code | Mean Diameter (nm) | Polydispersity Index (PDI) | Zeta Potential (−mV) | Mean Viscosity (cps) | Entrapment Efficiency (%) | Drug Release (%) |
|---|---|---|---|---|---|---|
| CNE1 | 229.4 ± 11.6 | 0.357 ± 0.090 | 28.63 ± 4.19 | 94.76 ± 6.24 | 61.79 ± 5.07 | 69.28 ± 3.31 |
| CNE2 | 187.3 ± 9.2 | 0.282 ± 0.076 | 9.08 ± 4.31 | 100.39 ± 9.51 | 68.44 ± 7.12 | 72.13 ± 5.29 |
| CNE3 | 166.5 ± 10.1 | 0.196 ± 0.077 | 19.52 ± 3.18 | 118.06 ± 5.93 | 71.52 ± 5.33 | 83.06 ± 7.91 |
| CNE4 | 109.7 ± 4.3 | 0.172 ± 0.031 | 34.21 ± 2.70 | 141.26 ± 5.34 | 80.29 ± 4.92 | 89.16 ± 8.14 |
| CNE5 | 154.6 ± 8.7 | 0.148 ± 0.013 | 23.35 ± 3.47 | 291.25 ± 8.74 | 69.25 ± 7.29 | 78.41 ± 4.65 |
| CNE6 | 250.7 ± 10.6 | 0.308 ± 0.091 | 9.55 ± 1.86 | 283.57 ± 10.29 | 70.42 ± 6.55 | 74.50 ± 4.31 |
| Formulation Code | Flux (Jss) ± SD (mg/cm2/h) | Permeability Constant (Kp) ± SD (cm/h × 10−2) | Enhancement Ratio (Er) | p-Value † |
|---|---|---|---|---|
| Neat CSO | 18.33 ± 0.19 | 0.175 ± 0.09 | - | - |
| CNE1 | 25.58 ± 0.12 | 0.213 ± 0.06 | 1.21 | <0.05 |
| CNE2 | 37.92 ± 0.09 | 0.377 ± 0.09 | 2.15 | <0.05 |
| CNE3 | 41.83 ± 0.11 | 0.431 ± 0.04 | 2.46 | >0.01 |
| CNE4 | 46.71 ± 0.07 | 0.529 ± 0.03 | 3.02 | <0.01 |
| CNE5 | 35.24 ± 0.13 | 0.407 ± 0.05 | 2.32 | >0.01 |
| CNE6 | 32.51 ± 0.10 | 0.380 ± 0.07 | 2.17 | <0.05 |
| Formulation Matrix | Sampling (Day First) | Sampling (after Three Months) | ||
|---|---|---|---|---|
| RTP (25 °C (±2)) | Stability Chamber (40 °C (±2)/65%RH (±5)) | |||
| PMD (nm) | ZP (−mV) | PMD (nm) | ZP (−mV) | |
| CNE1 | 230.1 ± 10.2 | 28.6 ± 5.2 | 261.9 ± 11.5 | 30.7 ± 6.1 |
| CNE2 | 187.6 ± 8.1 | 9.1 ± 4.3 | 193.2 ± 7.6 | 11.3 ± 5.4 |
| CNE3 | 166.8 ± 4.3 | 19.6 ± 3.3 | 178.3 ± 5.5 | 22.3 ± 6.3 |
| CNE4 | 110.5 ± 3.2 | 34.4 ± 2.7 | 115.2 ± 7.2 | 35.2 ± 3.6 |
| CNE5 | 156.4 ± 8.2 | 23.6 ± 4.7 | 164.8 ± 6.1 | 25.8 ± 6.2 |
| CNE6 | 253.3 ± 11.1 | 10.4 ± 3.8 | 270.4 ± 7.9 | 12.3 ± 3.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahdi, W.A.; Alam, P.; Alshetaili, A.; Alshehri, S.; Ghoneim, M.M.; Shakeel, F. Product Development Studies of Cranberry Seed Oil Nanoemulsion. Processes 2022, 10, 393. https://doi.org/10.3390/pr10020393
Mahdi WA, Alam P, Alshetaili A, Alshehri S, Ghoneim MM, Shakeel F. Product Development Studies of Cranberry Seed Oil Nanoemulsion. Processes. 2022; 10(2):393. https://doi.org/10.3390/pr10020393
Chicago/Turabian StyleMahdi, Wael A., Prawez Alam, Abdullah Alshetaili, Sultan Alshehri, Mohammed M. Ghoneim, and Faiyaz Shakeel. 2022. "Product Development Studies of Cranberry Seed Oil Nanoemulsion" Processes 10, no. 2: 393. https://doi.org/10.3390/pr10020393
APA StyleMahdi, W. A., Alam, P., Alshetaili, A., Alshehri, S., Ghoneim, M. M., & Shakeel, F. (2022). Product Development Studies of Cranberry Seed Oil Nanoemulsion. Processes, 10(2), 393. https://doi.org/10.3390/pr10020393








