Abstract
Background/Objectives: Although ADHD in adults has become visible and inclusive in recent years in diagnostic manuals, research is still limited regarding the long-term outcomes of patients with this disorder. The main objective of this research was to address the many facets of predictor variables in girls with ADHD facing unplanned pregnancies at young ages in order to improve the management of pre-, peri-, and postnatal complications that may occur, as well as for early psychiatric diagnosis and effective intervention. Methods: PubMed and Web of Science Databases were used to perform literature research, and a total of 27 records were selected and used for data extraction. Results: Related articles have included the persistence of ADHD symptoms comorbid with other disorders among girls with ADHD as a risk factor for teenage pregnancies. Conduct disorders and substance use disorders are the main co-occurrent diagnoses that increase the likelihood for teenage childbirth. Unplanned pregnancies at young ages are associated with unfavorable psychosocial trajectories both for the mother and the child. Conclusions: In this review, we emphasize the importance of predisposing factors for risky sexual behaviors and unplanned pregnancies in cases of girls with ADHD. The topic of the article draws attention to the need for uniform national individualized care of girls with ADHD, the implementation of programs to prevent academic failure and early parenthood as well as addressing comorbid obstetrical and psychiatric conditions, especially in regions where the rate of adolescent births continues to be high.
1. Introduction
Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder frequently diagnosed among pediatric patients, but researchers and clinicians have paid more attention in recent years to symptoms characteristic in adulthood, which are much more difficult to recognize than in the case of children or adolescents due to their polymorphous nature. For a long time, the diagnostic criteria were oriented towards ADHD in children, but the clinical picture manifests differently in adulthood, reflecting the changes in daily activities and responsibilities characteristic of adulthood.
ADHD is characterized by an early onset, and by a combination of hyperactivity, lack of attention, inability to correctly use achieved skills, restlessness, impulsivity, and a high degree of distractibility [1]. These particularities are persistent over time. Recent research demonstrated that in some patients there is a reduction in the severity of symptoms (generally hyperactivity), but in 65% of them the symptoms remain distressing, with 90% of them experiencing dysfunction in adulthood [2]. Although the diagnostic criteria in Diagnostic and Statistical Manual of Mental Disorders (DSM-5) have been modified to be more inclusive of adult symptoms, this disorder is still underdiagnosed and significantly undertreated.
During the transition to adolescence, there are concerns regarding the clinical evolution of a patient with ADHD due to low inhibitory control and poor planning skills. Deficits in emotional self-regulation and at the level of executive functions become exacerbated in adulthood [3]. Although these deficits are not criteria exclusively applicable to patients with ADHD, they are characteristic of this pathology, and their presence is correlated with engagement in risky behaviors that predict negative outcomes in multiple areas of life. Risky sexual behaviors in the case of adolescent girls with ADHD consist of first sexual intercourse at young age, inconstant use of protection, increased risk for sexually transmitted diseases, multiple partners, and unplanned pregnancies before the age of consent [4].
Being one of the most diagnosed mental health disorders of childhood, ADHD is reported to affect 3% to 10% of school-age children, 2–6% of adolescents, and 4–5% in adults [5]. ADHD is diagnosed more frequently among boys than among girls, with the ratio reported in the specialized literature being 2:1, and this proportion tends to equalize in adults [6]. By age group, the prevalence of ADHD is higher among schoolboys than among male adolescents, while the prevalence among girls is lower but more stable over time [7]. Even if the tendency of girls to develop externalizing and rule-breaking behaviors is lower than in the case of boys, the studies that compared groups of teenage girls with ADHD with teenage girls without ADHD demonstrated worse outcomes in education, social relationships, and academic performances for the former [8].
Long-term impairments in young girls need further investigation in future research, since the symptoms of ADHD in adults have received increased attention in recent years with the modification of the diagnostic criteria. Even though the influence of ADHD in early involvement in a pregnancy has been demonstrated, there is still a great need to explore the underlying mechanisms and childhood predictors for impulsive sexual behaviors and failure to used contraception at a young age.
2. Methods
The core objective of the current research was to highlight the knowledge regarding the underlying mechanisms that increase the likelihood for teenage girls with ADHD to be involved in early pregnancies. PubMed and Web of Science Databases were used to perform a thorough literature search for this review. To guarantee a comprehensive analysis of the pertinent literature, we used a variety of keywords like “ADHD”, “ADHD in girls”, “ADHD in teenagers”, “ADHD and risk for pregnancy”, “ADHD comorbidity”, “obstetrical complications in ADHD or young mothers”, “teenage pregnancy and outcome”, and “mental health”, “risk factors for early pregnancies”, “interventional programmes for unplanned pregnancies”, “psychosocial interventions”, “maternal ADHD”, as well as using “Attention Deficit” and “Hyperkinetic Disorder” instead of ADHD/ADD. The methodology for selecting the articles was performed using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [9].
The selected records were individually analyzed to meet the inclusion criteria of the search in the databases. We selected articles that exposed mediating factors for unplanned pregnancies in girls with ADHD, predictors for risky sexual behaviors in patients with ADHD, risk factors for negative longitudinal trajectory in this category of patients, birth outcomes and obstetrical complications associated with teenage pregnancy, psychosocial intervention for ADHD adolescent parents, and educational programs and current perspectives for teen pregnancy prevention. To ensure that the selected materials were understood and correctly analyzed, we only included reports that were exclusively written in English. Exclusion criteria were as follows: animal or in vitro studies, studies of target groups of patients not including adolescents, case reports, and case series.
Our search parameters generated 250 records in total (Figure 1). A total of 150 papers were eliminated after the titles were screened and duplicates were eliminated. In the screening processes, we excluded 73 papers due to the following: unrelated topics, not published in English, repeated papers, case reports, case series, animal studies, no abstract available, and study protocols not available. In the last phase of the paper inclusion process, 27 studies were selected, fully analyzed, and separated according to the three major factors we aimed to examine: mediators of unplanned pregnancies in girls with ADHD, birth outcomes related to teenage pregnancies, and psychosocial interventions for this category of patients.
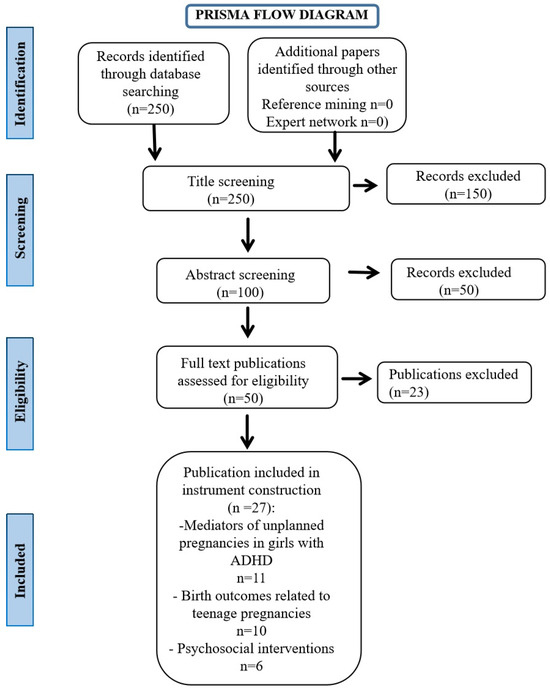
Figure 1.
PRISMA flow diagram.
The goal of the search was to find a large number of papers that addressed the many facets of predictor variables in girls with ADHD facing unplanned pregnancies at young ages, in order to improve the management of pre-, peri-, and postnatal complications that may occur, as well as for early psychiatric diagnosis and effective intervention. There is still a lack of research addressing sex differences in symptom evolution in ADHD patients, with most specialized studies focusing on male dominated samples. Because girls predominantly present the silent form of ADHD with attention deficit and because the prevalence of this disorder is lower than in boys at younger ages, female presentation has been overlooked in past research.
3. Mediating Factors in the Occurrence of Unplanned Pregnancies in Girls with ADHD
More than half of the pregnancies worldwide are unintended or unplanned [10]. The young age of the mother at conception and the presence of mental health disorders or abuse of psychoactive substances are among the most incriminated risk factors for unplanned or unwanted pregnancies [10].
Until now, teenage pregnancies in ADHD girls have not been complexly explored in research data, because the majority of the studies investigating this topic have relied on self-measuring instruments. Such investigations do not allow generalization to larger cohorts. The update of the diagnostic criteria applicable to adults in DSM-5 has recently brought the evolution of ADHD in young adults to the attention of researchers. The problem of unplanned pregnancies in young women and teenagers with ADHD brings about psychosocial concerns such as additional mental health disorders for the mother, child maltreatment and developmental disorders, or the need for social assistance.
The rate of unplanned pregnancies in girls with ADHD compared to those without ADHD is reported by studies as varying between 42 and 45% [10]. Also, in the case of boys, the presence of this diagnosis is associated with an increased probability of early parenthood (25%) [11]. Starting from these worrying statistics, we consider the knowledge and research of the factors that could mediate the relationship between persistent ADHD symptoms and early pregnancy of great importance.
ADHD is described as a disorder of executive functions, such as response inhibition, working memory, or deficits in executive control. Research on the neuropsychology of ADHD children found a pattern of cognitive deficiencies associated with prefrontal executive function impairments: inattention, difficulties in self-regulation, deficiencies in inhibitory responses, restlessness or hyperactivity, and in certain situations, lack of interest. Executive functions reported to be deficient in ADHD patients are response inhibition, vigilance, working memory, and planning [12]. The same authors suggest that ADHD patients have difficulty delaying gratification, preferring small, immediate rewards over delayed but more consistent ones. Considering the deficits in organization, planning, flexibility, inhibition, and control of motor actions that characterize executive functions, it is possible to explain the impulsiveness of girls with ADHD in engaging in risky sexual behaviors, neglecting the use of contraceptives and experimenting with multiple sexual partners.
In 75% of cases, ADHD co-occurs with one or more psychiatric illnesses. Three concurrent medical conditions are typically present in ADHD patients [13]. This indicates that ADHD is not a minor ailment, but rather a disorder that is frequently misdiagnosed in individuals who have already sought treatment for more complicated issues that may not respond to therapy. Thus, it can be concluded that ADHD in patients whose symptomatology does not remit or is not treated in time leads to the chronicity of comorbid disorders. The presence of one or more mental health disorders is often the rule and not the exception for adolescents with ADHD. Children with the most severe disruptive behaviors generally present with the coexistence of ADHD and conduct disorder, with the comorbidity prevalence reported to be between 35% and 50% in these children [14]. They show the onset of symptoms at a much younger age, engage in more aggressive behaviors, and develop serious delinquency, resulting in greater dysfunction in adulthood. Impulsivity is the component of ADHD that usually increases over time, generating additional symptoms of conduct disorder. By inhibiting self-regulation processes, the ADHD patient is constantly irritable and is involved in impulsive behaviors based on extreme sensation-seeking. They change jobs frequently and start new relationships impulsively. The tendency toward destructive behaviors and the continuous need to be continuously stimulated determine an increased predisposition for these patients to be involved in car accidents, delinquent acts, unbalanced family relationships, and early parenthood (unintended pregnancies before the age of 18) [8].
In light of these findings, the presence of comorbid conduct disorder should be examined as a mediator in the relationship between childhood ADHD and early pregnancy.
Behavioral under-control is associated not only with the persistence of ADHD symptoms but also with drugs/alcohol abuse. Unwanted pregnancies at a young age are correlated with a deviant pattern of behaviors, such as delinquency and the abuse of psychoactive substances. Comorbidity rates among people with ADHD who have a history of addiction or dependence on psychostimulants range from 25% to 55%, according to studies that have examined the existence of this condition [15]. Taking into account the prevalence rate in the overall population (15–18%), we can conclude that having ADHD doubles a person’s risk of developing psychoactive substance misuse [15]. These individuals have a higher propensity to begin abusing drugs at a young age, using many drugs at once, and remaining in treatment programs that combine medication and psychotherapy for longer periods of time. When compared to the control group, adolescents with ADHD start abusing drugs and alcohol at a younger age, and this trend continues until around the age of 40. This fact is possibly associated with the loss of hope for symptom relief. According to specialized studies, there is no predilection for a certain psychoactive substance, and adults with ADHD use all types of drugs. In our current psychiatric evaluation of adolescent girls who chronically use psychoactive substances, we detected repeated sexual behaviors with unknown partners in order to obtain drugs. This demonstrates another factor that predicts sexual risk-taking, early or unwanted pregnancies, and other psychosocial concerns.
It is known that ADHD is a neurodevelopmental disorder with genetic determinism but with a strong educational influence. The pattern of educational attitude of the parents of children with ADHD can influence premature sexual activity. A meta-analysis that assessed the relationship between the parental monitoring of adolescents’ social activities and relationships and early sexual behaviors concluded that positive sexual decision making was influenced by supportive and constant parental monitoring [16]. The parental enforcement of rules and firm guidance were correlated with delaying starting sexual activities, the use of condoms and contraceptives, and positive outcomes of long-term health trajectories. Neglectful parenting, insufficient family support, and unstructured parental bonding increase the risk of externalizing problems in teenagers. Thus, low quality of an educational family system can be another explanatory mechanism for risky sexual behaviors and early pregnancies.
In the case of adolescents with ADHD, family life is also affected given the increased hereditary risk of this disorder. Adults with ADHD are at risk of having a negatively impacted parent–child relationship [17]. Financial resources are often at a low level due to lower academic performance compared to people with the same cognitive abilities. Many adults with ADHD experience feelings of loneliness and isolation due to social difficulties and shame caused by failures, and their mental and physical well-being is at a lower level, even in the presence of an increased IQ. Lower educational achievements, regardless their intellectual potential; failure in finish their educational programs; unstable job positions as a result of experiencing continuous boredom; and conflicts with colleagues determines poor family functioning and failure to reach their full potential. The bidirectional relationship between school dropout/academic failure and involvement in risky sexual behaviors and early pregnancies represents a vast future research topic.
The above-mentioned mediating factors have been investigated in recent studies, and these consistent results across diverse population cohorts demonstrate the link between ADHD symptoms and risk-taking behavior. A summary of these studies and their conclusions regarding the mediating factors in the occurrence of unplanned pregnancies and risky sexual behaviors is listed in Table 1:

Table 1.
Mediating factors in the occurrence of unplanned pregnancies or risky sexual behaviors.
4. Birth Outcomes Related to Teenage Pregnancies
Teenage pregnancy represents a complex interplay of health, social, and policy factors, presenting unique challenges for adolescent mothers and their children [26]. Comprehensive research on these various risks, as well as evidence-based mitigation techniques, appear to be lacking at the moment. In addition to highlighting evidence-based strategies to lessen their impact, this narrative synthesis examines these complex risks. Wong et al. found that teenage mothers are at serious risk for obstetric complications [27]. Low birth weight (LBW) and preterm birth (PTB) are among the complications that adolescents are biologically more likely to experience. Lower Apgar scores and other compromised health indicators are common in newborns born to teenage mothers, highlighting the importance of effective prenatal care.
These results are consistent with the broader literature, indicating that detrimental neonatal outcomes are largely caused by biological immaturity and limited access to prenatal care. Teenage mothers are more likely to undergo obstructed labor and have limited pelvic development, which increases the likelihood of complications during childbirth. The health of the mother and the baby is at risk due to conditions like anemia and preeclampsia, which are more prevalent in teenage mothers [28].
Education on dietary and health requirements during pregnancy as well as focused prenatal care are necessary to address these issues. The rate of adolescent births is a crucial measure of reproductive health on a global scale. In 2000, there were 64 out of every 1000 births among women aged 15 to 19 worldwide; by 2023, that number had dropped to 41 out of every 1000, according to the World Health Organization (WHO) [29]. However, regional disparities persist. High rates of adolescent births frequently point to structural problems like lack of access to reproductive health and educational resources, socioeconomic disparities, and cultural norms that encourage early marriage and parenthood. Complex behaviors that represent the core of ADHD impulsivity can be correlated to the differences and increase in teenage pregnancies in some regions (“In the WHO African Region, estimations were 97 per 1000 adolescent in 2023 compared to 13.1 per 1000 adolescent girls in the European Region”) [29].
Adolescent pregnancies are both a cause and an effect of socioeconomic disadvantage from a social standpoint. According to Laurenzi et al., adolescents from low-income neighborhoods usually face structural obstacles to healthcare and education [30]. Dropping out of school frequently occurs before becoming pregnant, which restricts opportunities and prolongs poverty cycles. The vulnerability of teenage mothers is increased by mental health issues, such as elevated rates of ADHD. Often, social stigma and insufficient social support networks exacerbate these psychological burdens.
This group of patients may be discouraged from seeking necessary services due to the stigma attached to adolescent motherhood and the impaired inhibition processes that are typical of ADHD teenagers. SmithBattle emphasizes the value of community-based initiatives that normalize adolescent motherhood, build resilience, and offer strong support networks [31]. By increasing access to healthcare, education, and other support networks, these partnerships play a critical role in mitigating the long-term socioeconomic effects of adolescent pregnancy. To address these disparities, interventions that take into account the unique needs and challenges that these patient categories face must be culturally sensitive. Community-based health education initiatives that are culturally sensitive have shown promise in reaching at-risk groups and promoting the use of contraceptives [32].
5. Proposed Measures to Address the Medical and Social Determinants of Health
These interrelated hazards underscore the pressing necessity for coordinated measures that concurrently address the medical and social determinants of health. For example, increasing prenatal care access can lower obstetric risks and psychosocial programs can improve mental health and facilitate reintegration into school. Policymakers, medical professionals, and community organizations must work together to break the cycle of disadvantage and ensure that adolescent mothers and their children have healthier futures.
School-based health programs that provide comprehensive sex education, free contraceptives, and counseling services are examples of promising interventions. Furthermore, mentorship programs that pair adolescent mothers with exemplary role models have proven successful in fostering healthy parenting habits and lessening feelings of loneliness. The primary aim of interventions should be facilitating access to monitoring and counseling services that address the prevention of recurrent pregnancies, which worsen the health and financial difficulties faced by adolescent mothers. Additionally, the revolution in digital health opens up new avenues for intervention. Teenage mothers can now receive critical health information, remote consultations, and continuous support through mobile health apps and telemedicine, which effectively overcome logistical and geographic obstacles to healthcare access.
Mental health specialists can adopt evidence-based approaches to prevent teenage pregnancy and promote sexual health. In Table 2, we include some key recommendations [33,34,35]:

Table 2.
Proposed interventions for addressing medical and social determinants of health.
Given its widespread implications, teenage pregnancy represents a pressing public health concern that requires a collective response. Effective interventions must target both obstetric risks through improved prenatal care and social determinants by enhancing education, mental health support, and access to contraception. Healthcare providers must collaborate to design programs that acknowledge the unique experiences of adolescent mothers, ultimately disrupting cycles of poverty and poor health.
6. Limitations
Our review has several limitations. Firstly, pertinent research published in other databases or in languages other than English may not have been included in our PubMed-only, English-language literature search. Furthermore, relevant research that utilized different terminologies or concentrated on related but different issues would have been excluded as a result of the usage of certain keywords. We believe that multicentric prospective studies are crucial for developing uniform and useful clinical guidelines, because the information provided may be biased by our local hospital resources and our national clinical guidelines.
7. Conclusions
The mechanisms underlying the impulsive sexual behaviors to which girls diagnosed with ADHD are exposed are far from being clarified. The negative associations for school achievements, the presence of comorbidities, overly flexible parenting styles (e.g., excessively adaptable parenting approaches or inconsistency in the application of intrafamilial rules), and the predisposition toward drug use are only some of the factors that mediate the relationship between the persistence of ADHD symptoms in young girls and unwanted pregnancies. There is evidence to indicate the negative effects of an unwanted pregnancy on offspring development and adjustment. Further research is needed in order to monitor and detail these negative effects on different developmental stages but also on the potential physical/somatic diseases of these children as a result of teenage pregnancies.
The causal pathways that can explain risky sexual behaviors and unplanned pregnancies in ADHD girls take shape in this research, but there is still a gap in identifying long-term effects and health outcomes in this category of patients.
Author Contributions
Conceptualization, A.M.B. and N.G.; methodology, F.R.; software, A.M.B.; validation, F.R., A.M.B. and N.G.; formal analysis, F.R.; investigation, A.M.B.; resources, N.G.; data curation, F.R., A.M.B. and N.G.; writing—original draft preparation, A.M.B. and N.G.; writing—review and editing, F.R.; visualization, A.M.B.; supervision, N.G.; project administration, F.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Sibley, M.H.; Arnold, L.E.; Swanson, J.M.; Hechtman, L.T.; Kennedy, T.M.; Owens, E.; Molina, B.S.G.; Jensen, P.S.; Hinshaw, S.P.; Roy, A.; et al. Variable patterns of remission from ADHD in the multimodal treatment study of ADHD. Am. J. Psychiatry 2022, 179, 142–151. [Google Scholar] [CrossRef] [PubMed]
- Krieger, V.; Amador-Campos, J.A.; Guàrdia-Olmos, J. Executive functions, Personality traits and ADHD symptoms in adolescents: A mediation analysis. PLoS ONE 2020, 15, e0232470. [Google Scholar] [CrossRef] [PubMed]
- Meinzer, M.C.; LeMoine, K.A.; Howard, A.L.; Stehli, A.; Arnold, L.E.; Hechtman, L.; Hinshaw, S.P.; Molina, B.S.G.; Murray, D.W.; Sibley, M.H.; et al. Childhood ADHD and Involvement in Early Pregnancy: Mechanisms of Risk. J. Atten. Disord. 2020, 24, 1955–1965. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, K.; Pietrzak, R.H.; El-Gabalawy, R.; Mackenzie, C.S.; Sareen, J. Prevalence of psychiatric disorders in US older adults: Findings from a nationally representative survey. World Psychiatry 2015, 14, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Hinshaw, S.P.; Nguyen, P.T.; O’Grady, S.M.; Rosenthal, E.A. Annual Research Review: Attention-deficit/hyperactivity disorder in girls and women: Underrepresentation, longitudinal processes, and key directions. J. Child Psychol. Psychiatry 2022, 63, 484–496. [Google Scholar] [CrossRef]
- Ghanizadeh, A.; Salehi, A.; Moeini, S.R. Clinical Presentation of Attention-Deficit Hyperactivity Disorder Symptoms in Terms of Gender and Chronological Age. Int. J. Community Based Nurs. Midwifery 2019, 7, 241–246. [Google Scholar] [CrossRef]
- Owens, E.B.; Zalecki, C.; Gillette, P.; Hinshaw, S.P. Girls with Childhood ADHD as Adults: Cross-Domain Outcomes by Diagnostic Persistence. J. Consult. Clin. Psychol. 2017, 85, 723–736. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Enthoven, C.A.; Hanan, E.l.; Marroun, H.E.; Koopman-Verhoeff, M.E.; Jansen, W.; Lambregtse-van den Berg, M.P.; Sondeijker, F.; Hillegers, M.H.J.; Bijma, H.H.; Jansen, P.W. Clustering of characteristics associated with unplanned pregnancies: The generation R study. BMC Public Health 2022, 22, 1957. [Google Scholar] [CrossRef] [PubMed]
- Owens, E.B.; Hinshaw, S.P. Adolescent Mediators of Unplanned Pregnancy among Women with and without Childhood ADHD. J. Clin. Child Adolesc. Psychol. 2019, 49, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Halse, M.; Steinsbekk, S.; Hammar, Å.; Wichstrøm, L. Longitudinal relations between impaired executive function and symptoms of psychiatric disorders in childhood. J. Child Psychol. Psychiatry 2022, 63, 1574–1582. [Google Scholar] [CrossRef] [PubMed]
- Solberg, B.S.; Halmoy, A.; Engeland, A.; Igland, J.; Haavik, J.; Klungsoyr, K. Gender differences in psychiatric comorbidity: A population-based study of 40 000 adults with attention deficit hyperactivity disorder. Acta Psychiatr. Scand. 2018, 137, 176–186. [Google Scholar] [CrossRef] [PubMed]
- Sonuga-Barke, E.J.S.; Becker, S.P.; Bölte, S.; Castellanos, F.S.; Franke, B.; Newcorn, J.H.; Nigg, J.T.; Rohde, L.A.; Simonoff, E. Annual Research Review: Perspectives on progress in ADHD science—From characterization to cause. J. Child Psychol. Psychiatry 2023, 64, 506–532. [Google Scholar] [CrossRef] [PubMed]
- Choi, W.S.; Woo, Y.S.; Wang, S.M.; Lim, H.K.; Bahk, W.M. The prevalence of psychiatric comorbidities in adult ADHD compared with non-ADHD populations: A systematic literature review. PLoS ONE 2022, 17, e0277175. [Google Scholar] [CrossRef]
- Dittus, P.J.; Michael, S.L.; Becasen, J.S.; Gloppen, K.M.; McCarthy, K.; Guilamo-Ramos, V. Parental Monitoring and Its Associations With Adolescent Sexual Risk Behavior: A Meta-analysis. Pediatrics 2015, 136, e1587–e1599. [Google Scholar] [CrossRef]
- Montejo, J.E.; Durán, M.; Martínez, M.; Hilari, A.; Roncalli, N.; Vilaregut, A.; Corrales, M.; Nogueira, M.; Casas, M.; Linares, J.L.; et al. Family Functioning and Parental Bonding During Childhood in Adults Diagnosed With ADHD. J. Atten. Disord. 2019, 23, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Isaksson, J.; Stickley, A.; Koposov, R.; Ruchkin, V. The danger of being inattentive—ADHD symptoms and risky sexual behaviour in Russian adolescents. Eur. Psychiatry 2018, 47, 42–48. [Google Scholar] [CrossRef]
- Flory, K.; Molina, B.S.G.; Pelham, W.E.; Gnagy, E.; Smith, B. Childhood ADHD Predicts Risky Sexual Behavior in Young Adulthood. J. Clin. Child Adolesc. Psychol. 2006, 35, 571–577. [Google Scholar] [CrossRef]
- Bachanas, P.J.; Morris, M.K.; Lewis-Gess, J.K.; Sarett-Cuasay, E.J.; Sirl, K.; Ries, J.K.; Sawyer, M.K. Predictors of risky sexual behavior in African American adolescent girls: Implications for prevention interventions. J. Pediatr. Psychol. 2002, 27, 519–530. [Google Scholar] [CrossRef]
- Sarver, D.E.; McCart, M.R.; Sheidow, A.J.; Letourneau, E.J. ADHD and risky sexual behavior in adolescents: Conduct problems and substance use as mediators of risk. J. Child Psychol. Psychiatry 2014, 55, 1345–1353. [Google Scholar] [CrossRef] [PubMed]
- Hua, M.H.; Huang, K.L.; Hsu, J.W.; Bai, Y.M.; Su, T.P.; Tsai, S.J.; Li, C.T.; Lin, W.C.; Chen, T.J.; Chen, M.H. Early Pregnancy Risk Among Adolescents With ADHD: A Nationwide Longitudinal Study. J. Atten. Disord. 2021, 25, 1199–1206. [Google Scholar] [CrossRef] [PubMed]
- Hosain, G.M.M.; Berenson, A.B.; Tennen, H.; Bauer, L.O.; Wu, Z.H. Attention deficit hyperactivity symptoms and risky sexual behavior in young adult women. J. Womens Health 2012, 21, 463–468. [Google Scholar] [CrossRef]
- Seppä, S.; Halt, A.H.; Nordström, T.; Hurtig, T. Efects of Symptoms of Attention-Defcit/Hyperactivity Disorder (ADHD) and Oppositional Defiant Disorder (ODD) on Academic Performance and Educational Attainment. Child Psychiatry Hum. Dev. 2023. [Google Scholar] [CrossRef] [PubMed]
- Skoglund, C.; Kopp Kallner, H.; Skalkidou, A.; Wikström, A.K.; Lundin, C.; Hesselman, S.; Wikman, A.; Sundström Poromaa, I. Association of Attention-Deficit/Hyperactivity Disorder With Teenage Birth Among Women and Girls in Sweden. JAMA Netw. Open. 2019, 2, e1912463. [Google Scholar] [CrossRef]
- Amjad, S.; Adesunkanmi, M.; Twynstra, J.; Seabrook, J.A.; Ospina, M.B. Social Determinants of Health and Adverse Outcomes in Adolescent Pregnancies. Semin. Reprod. Med. 2022, 40, 116–123. [Google Scholar] [CrossRef]
- Wong, S.P.W.; Twynstra, J.; Gilliland, J.A.; Cook, J.L.; Seabrook, J.A. Risk factors and birth outcomes associated with teenage pregnancy: A Canadian sample. J. Pediatr. Adolesc. Gynecol. 2020, 33, 153–159. [Google Scholar] [CrossRef]
- Pinho-Pompeu, M.; Surita, F.G.; Pastore, D.A.; Moraes Paulino, D.S.; Pinto E Silva, J.L. Anemia in pregnant adolescents: Impact of treatment on perinatal outcomes. J. Matern.-Fetal Neonatal Med. 2017, 30, 1158–1162. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Adolescent Birth Rate (per 1000 Females Aged 15–19 Years). 2023. Available online: https://platform.who.int/data/maternal-newborn-child-adolescent-ageing/indicator-explorer-new/MCA/adolescent-birth-rate-(per-1-000-females-aged-15-19-years (accessed on 1 November 2024).
- Laurenzi, C.A.; Gordon, S.; Abrahams, N.; du Toit, S.; Bradshaw, M.; Brand, A.; Melendez-Torres, G.J.; Tomlinson, M.; Ross, D.A.; Servili, C.; et al. Psychosocial interventions targeting mental health in pregnant adolescents and adolescent parents: A systematic review. Reprod. Health 2020, 17, 65. [Google Scholar] [CrossRef] [PubMed]
- SmithBattle, L. Reducing the stigmatization of teen mothers. MCN Am. J. Matern./Child. Nurs. 2013, 38, 235–241; quiz 242–243. [Google Scholar] [CrossRef] [PubMed]
- Manet, H.; Doucet, M.-H.; Bangoura, C.; Dioubaté, N.; El Ayadi, A.M.; Sidikiba, S.; Millimouno, T.M.; Delamou, A. Factors facilitating the use of contraceptive methods among urban adolescents and youth in Guinea: A qualitative study. Reprod. Health 2023, 20, 89. [Google Scholar] [CrossRef]
- Yang, Z.; Gaydos, L.M. Reasons for and Challenges of Recent Increases in Teen Birth Rates: A Study of Family Planning Service Policies and Demographic Changes at the State Level. J. Adolesc. Health 2010, 46, 517–524. [Google Scholar] [CrossRef] [PubMed]
- Diabelková, J.; Rimárová, K.; Dorko, E.; Urdzík, P.; Houžvičková, A.; Argalášová, L’. Adolescent Pregnancy Outcomes and Risk Factors. Int. J. Environ. Res. Public Health 2023, 20, 4113. [Google Scholar] [CrossRef]
- Ponsford, R.; Bragg, S.; Meiksin, R.; Tilouche, N.; Van Dyck, L.; Sturges, J.; Allen, E.; Elbourne, D.; Hadley, A.; Lohan, M.; et al. Feasibility and acceptability of a whole-school social-marketing intervention to prevent unintended teenage pregnancies and promote sexual health: Evidence for progression from a pilot to a phase III randomised trial in English secondary schools. Pilot Feasibility Stud. 2022, 8, 52. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).