Abstract
Poor youth mental health is an area of global concern. Summer holiday programs may provide environments that support mental health when the structures and supports of school are not available. The aim of this review was to determine the effectiveness of summer holiday programs in improving the mental health, social–emotional well-being, and cognitive (non-academic) outcomes of children and adolescents. Studies of summer holiday programs for school-aged children (5–18 years) were included if they measured any mental, socio-emotional or cognitive (non-academic) outcome. Studies were excluded if they were published prior to 2000, targeted clinical populations or lasted less than five days. Six databases were searched (April 2023). Risk of bias was assessed using the PEDro tool. Study outcomes were grouped according to three main constructs: mental health (psychological well-being, anxiety, depression, distress, and self-perception including self-esteem, self-worth, self-concept, confidence, and competence); social–emotional well-being (behavior and social skills, e.g., communication, bullying, conflict resolution, empathy, and social skills); and cognitive function (memory, selective attention, and executive function). A fourth “other” group captured substance use, personality traits, character skills, and values. Effect sizes were calculated as the standardized mean difference between pre- and post-intervention scores. The synthesis involved a random-effects meta-analysis (presented in forest plots), where possible, with the remaining outcomes narratively synthesized. Twenty-six studies (n = 6812 participants) were included. The results of the meta-analysis suggested that summer programs showed a statistically non-significant trend toward reducing symptoms of anxiety and depression (k = 2 studies, SMD = −0.17, 95% CI −2.94, 2.60), psychological distress (k = 2 studies, SMD −0.46, 95% CI –1.71, 0.79), and no effect on self-esteem (k = 6 studies, SMD = 0.02, 95% CI −0.02, 0.06) or self-worth (k = 3 studies, SMD = 0.05, 95% CI 0.00, 0.11). Narrative syntheses indicated a pattern toward improvements in general mental health, self-perception, social–emotional outcomes, and cognition. Studies were generally small, with a high risk of bias. Summer holiday programs for children and adolescents show trends toward improving mental, social, emotional, and cognitive outcomes. Programs targeting disadvantaged children showed stronger patterns of improvement related to mental health and self-perception than programs targeting the general population. While effect sizes are small to negligible, they consistently indicate improvements. Summer programs present a promising avenue to promote mental health in children; however, further rigorously designed, clearly reported control-group studies are required to more fully understand their effects.
Keywords:
summer camps; children; mental health; anxiety; depression; distress; well-being; cognition 1. Background
A healthy childhood lays the foundation for lifelong health. Mental health, as defined by the World Health Organization, encompasses a state of well-being in which individuals recognize their abilities, can manage normal life stresses, work productively, and contribute to their community [1]. The dual-factor model of mental health suggests that true mental health includes both the absence of mental illness (e.g., symptoms or disorders) and the presence of positive psychological well-being and emphasizes the importance of addressing both negative symptoms and fostering positive aspects such as life satisfaction, happiness, and personal growth [2,3]. Mental health is an important aspect of overall health, and it is critical to healthy social and emotional development, and problem-solving and coping skills [4]. Positive mental health allows children to more fully realize their academic potential [5]. Conversely, mental health disorders such as anxiety and depression reduce children’s quality of life across domains of psychological, physical, and social well-being [6,7].
Poor mental health of children and adolescents is a serious area of concern globally, as depression, anxiety, and behavioral disorders are the leading cause of illness and disability in 10–19-year-olds [8]. The symptoms of poor mental health are not always clearly visible. They may manifest internally, such as through anxiety, depression, and psychological distress; or externally, such as through aggression and hyperactivity. Research indicates that internalizing symptoms are generally more prevalent in children and adolescents than externalizing symptoms [9]. Compared to children with good mental health, children that suffer a mental health condition are six times more likely to suffer a mental health condition in adulthood [10] and go on to earn significantly lower income [11].
Environmental factors play an important role in the mental health of young people [12], and children spend a large proportion of their time in the school environment. School supports the development of positive mental health through consistent engagement in educational activities that positively impact students’ cognitive development [13,14,15]. Participation in classroom learning also requires children to practice executive functions, including memory, selective attention, and inhibitory control [16]. Engagement in enjoyable school-based and extra-curricular activities can be rewarding in and of itself, providing opportunities to learn new skills and achieve mastery in meaningful areas, thus increasing self-worth. Meanwhile, tailored strategies can help enhance a more stable, intrinsic sense of self- acceptance, which is referred to as self-esteem [17]. The social interaction and structured routines of the school day also help children develop social and emotional skills. Teachers can further provide emotional support and set clear expectations and boundaries that help children feel safe, ease anxiety, and develop a sense of belonging [18]. Teachers can also identify students struggling with the social and cognitive demands of schooling, thus allowing for early intervention. School provides opportunities to meet peers and form friendships, thus playing an important role in social development [4,19] that can protect against social maladjustment [20]. Furthermore, schools help children to display more favorable behavior patterns, including more time in physical activity and less time engaged in sedentary behaviors, like recreational screen-use [21,22]. This can positively support children’s mental health [23,24]. For example, decreasing screen use helps to improve sleep habits, supporting, in turn, good mental health [12], while increasing physical activity in children has been shown to reduce anxiety and depression and improve self-esteem and cognitive function [25].
While school holidays offer a reprieve to students and families from the demands of the school term, extended periods of time spent away from the school setting reduces the supports provided by school, the absence of which may negatively impact children’s mental health. Some evidence suggests that negative experiences over the summer holidays (like loneliness or food insecurity) can increase anxiety and negatively influence children’s mental health, with disadvantaged children affected to a greater extent [26,27]. Negative peer-group interactions over summer have been linked with increases in anti-social behaviors (bullying and victimization) [28], while reduced peer contact can reduce children’s enjoyment of, and therefore time spent in, physical activity [29].
Summer programs have proven benefits in a range of other outcomes for children, and it is feasible that some of the beneficial features of summer programs also enhance mental, emotional, and social well-being. Previous reviews of summer programs looking at academic outcomes found improvements in mathematics and reading achievement [30,31,32], while reviews of health outcomes have found moderate reductions in sedentary behavior and small increases in moderate-to-vigorous physical activity [33,34]. To date, no reviews have synthesized the evidence regarding the impact of summer programs on social, emotional, cognitive, and psychological outcomes. Thus, the objective of this systematic review was to determine the effectiveness of summer holiday programs in improving the mental health, social–emotional well-being, and cognitive (non-academic) outcomes of children and adolescents. The review questions were as follows:
- What are the effects of summer holiday programs on children and adolescents’ mental health, well-being, and social–emotional and cognitive function?
- Do the effects differ based on child characteristics (e.g., socioeconomic disadvantage and age)?
- Do the effects differ based on program characteristics (e.g., program content and duration)?
2. Methods
2.1. Protocol and Registration
A systematic review protocol was registered prospectively with PROSPERO (registration number: CRD42023409799) [35] and reported following the PRISMA 2020 guidelines [36].
2.2. Eligibility Criteria
Participants in the included studies were school-aged children (5–18 years) participating in a summer program (intervention) of at least five days’ duration that was exclusively delivered during the summer period (i.e., not including afterschool or other holiday programs). Primary outcomes included any mental health (e.g., psychological well-being, depression, and anxiety), socio-emotional (e.g., social connectedness, sadness, loneliness, appropriate behavior), or cognitive (e.g., working memory and executive function) outcome. Academic outcomes were not included, because they have been the focus of other reviews [30,31]. Studies were excluded if they were published before 2000 or if they targeted clinical populations (e.g., cancer and diabetes), special needs (learning or intellectual disabilities), or gifted/especially talented children. Study designs included both experimental studies with a control group, receiving “summer as usual” or a different summer program, and quasi-experimental (pre-post-intervention measures with no control group). No language limits were set. Full criteria are given in Supplementary File S1.
2.3. Information Sources and Search Strategy
Six databases were searched for peer-reviewed original articles: Embase, MEDLINE, JBI, PsychINFO (via OVID), ERIC, and Scopus (April 2023). A broad search strategy [37] was developed with an academic librarian, focusing on population and context terms (detailed in Supplementary File S2). Reference lists of included studies were searched using Citationchaser (version 0.0.3, Haddaway, Grainger and Gray 2021), and the corresponding authors of included studies were contacted to identify further relevant studies.
2.4. Selection Process
Search results were imported into Endnote 20 (Clarivate Analytics, Philadelphia, PA, USA), where duplicates were removed before being imported into ASReview [38] (version 1.1.1, ASReview LAB developers, Utrecht, The Netherlands), where the five same relevant studies identified during preliminary searches were used to train the search. Two independent reviewers (EE and BS) completed title and abstract screening, which was stopped once 10% of the total studies were screened and 100 consecutive, irrelevant titles were encountered. Full-text review was then completed using Covidence (Veritas Health Innovation, Melbourne, Australia). Screening was completed by EE and a second independent reviewer (TW or ZR), and disagreements were resolved through discussion.
2.5. Data Collection Process and Data Items
Charting tables were developed by the authorship team and piloted prior to use (example in Supplementary File S3). Fields for data extraction included study features (design, geographical location, and participant number); participant demographics (age, gender, and socioeconomic status); program design (structure, objectives, and environment); findings (measures of effect, certainty, and statistical significance, measurement tool, and timing of evaluation); and implementation outcomes (adverse events and attendance). Data extraction and risk-of-bias assessment were completed in duplicate using Covidence by two independent reviewers (EE, TW, ZW, JG, CS, and AG), with discrepancies resolved through discussion until consensus was reached.
2.6. Study Risk-of-Bias Assessment
Risk-of-bias assessment was completed in duplicate using Covidence by two independent reviewers (EE, TW, ZW, JG, CS, and AG), by employing the PEDro Risk of Bias Tool, recognized for its validity and reliability [39]. The highest possible PEDro score of 10 signifies minimal risk of bias, with categories used to assign studies as low, moderate, and high risk of bias [39]. However, the impracticality of blinding people delivering the program meant that this item was omitted, and the maximum score was revised to nine [40]. The interpretation of scores in this paper was 7–9 (low risk of bias), 5–6 (moderate risk), and 0–4 (high risk of bias).
2.7. Effect Measures and Synthesis Methods
Studies were grouped with the assistance of a behavioral scientist according to three main constructs: mental health, social–emotional well-being, and cognition. Mental health included psychological well-being (e.g., anxiety, depression, distress, well-being) and self-perception (e.g., self-esteem, self-worth, self-concept, confidence, and competence). Social–emotional well-being covered behavior and social skills (e.g., communication, bullying, conflict resolution, empathy, and social skills), while cognitive function included outcomes related to memory, selective attention, and executive function. Outcomes falling outside of these main constructs were presented separately as “other” and included health-related behaviors (substance use), personality traits/character skills, and spirituality/values. Effect sizes were calculated as the standardized mean difference from pre- and post-intervention scores and were interpreted as small (0.2), moderate (0.5), or large (0.8) [41]. Synthesis involved meta-analysis where possible, with the remaining outcomes narratively synthesized. Patterns were examined for each outcome when at least three outcomes were available.
2.8. Meta-Analysis
Meta-analyses were conducted for outcomes with sufficiently homogeneous data from at least two studies. Study authors were contacted for missing data. A random-effects model was used for meta-analyses, considering heterogeneity in study design and outcomes reported. Meta-analyses were conducted using R software (version 4.3.1) with the meta, metafor, and dmetar packages [42,43,44,45,46]. Standardized mean differences and associated confidence intervals were used to indicate the size and precision of the effect estimate, with restricted maximum-likelihood and Knapp–Hartung adjustments [46]. Meta-analysis results were presented using forest plots. Interpretation of results considered the direction, size, and precision of the effect with statistical significance set at p = 0.05. Patterns across studies were also considered. The I2 statistic was used to evaluate statistical heterogeneity, with I2 > 50% indicating substantial heterogeneity [41]. Robustness of results (effect size, statistical significance, and heterogeneity) was explored via a sensitivity analysis, using leave-one-out analyses, and analyses were repeated, excluding studies possessing a high risk of bias. Publication-bias analysis was omitted due to the small study set [47].
2.9. Narrative Synthesis
Where meta-analysis was not possible, a narrative synthesis was conducted according to the synthesis without meta-analysis (SWiM) guidelines [48]. Standardized measures of effect (e.g., odds ratio; mean difference; and standardized mean difference with statistical significance determined by the original study, usually p = 0.05) were used to code outcomes as improved, unchanged, or declined. To indicate the magnitude of intervention effect, a common effect metric was used: SMD (Cohen’s D, Hedges’ g) was prioritized, and when not available, it was calculated from baseline and post-intervention scores or converted from other effect metrics, such as eta-squared [49].
2.10. Certainty of Evidence
The overall evidence for each outcome was graded based on the Oxford Centre for Evidence Based Medicine’s (OCEBM) 2011 Levels of Evidence [50,51]. This approach evaluates an intervention’s effectiveness using a hierarchy of evidence, considering study design, effect size, and consistency of effects across studies. First, studies’ designs and effects were rated on a scale from one (highest) to five (lowest). Then, the evidence for each outcome was graded A–D: Grade A was assigned to outcomes with consistent level 1 studies (randomized controlled trials); Grade B for consistent level 2 studies (non-randomized controlled studies); Grade C for consistent level 3 studies (non-randomized, controlled studies, and for this review, repeat-measure non-controlled studies); and Grade D for inconsistencies in the direction of effect. Grades were adjusted down for high risk of bias and inconsistency between studies and adjusted up for large and consistent effect sizes. A minus sign indicated considerable clinical or statistical heterogeneity (I2 ≥ 50%).
2.11. Deviation from Registered Protocol
There were limited numbers of experimental trials with control groups; therefore, the original inclusion criterion of only experimental controlled study designs was broadened to include quasi-experimental designs (e.g., pre–post-intervention measures with participants acting as their own controls). Subgroup analyses based on child (age and SES) or program (duration and format) characteristics were undertaken narratively.
3. Results
3.1. Study Selection
Database searching yielded 4226 studies, with reference-list searching adding 1014 more. After the removal of duplicates, 4347 titles and abstracts were screened with 181 full texts retrieved. Finally, 26 studies involving 6812 participants were included (Figure 1). A full list of studies excluded at the full-text screening stage and their reason for exclusion is presented in Supplementary File S4.
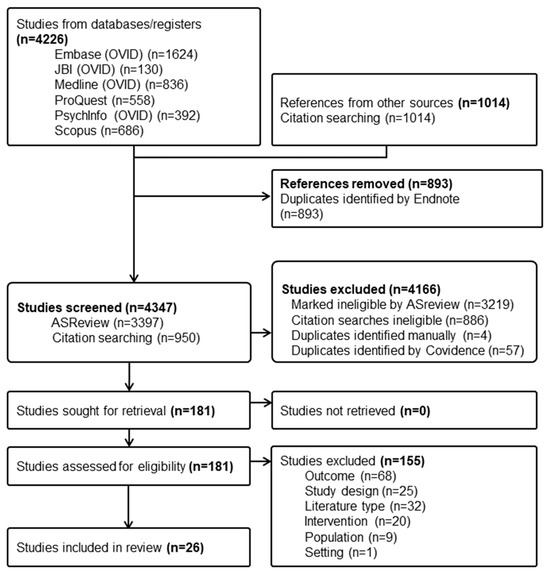
Figure 1.
PRISMA flow diagram of study identification, screening, and inclusion.
3.2. Study Characteristics
Included studies are summarized in Table 1. A summary of program and participant characteristics is presented in Table 2 (thematic coding is described in Supplementary File S5). Three studies were randomized controlled trials (RCTs) (k = 2 cluster RCTs [52,53], k = 1 individual RCT) [54], three were non-randomized controlled trials [55,56,57], and the remaining studies were within-subject, repeated-measures of groups all receiving an intervention (k = 2 studies had three groups [58,59], k = 1 study had two groups [60], and k = 17 studies had a single intervention group [61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76]). Sixty-two percent of the studies were from the United States (k = 16), with two studies from India and single studies from Australia, Canada, Italy, Japan, Spain, Switzerland, Turkey, and the United Kingdom. Ten of the eleven interventions that targeted children disadvantaged by low family SES or race were conducted in the US [52,59,63,68,69,70,71,74,75], with the remaining study conducted in Spain [64]. In 42% of studies (11/26 studies), program attendance was funded on behalf of the participants (e.g., trial funding, community organization, and scholarships) [52,53,54,58,62,64,68,69,71,73,75]; in two cases, the participants paid in full [55,72], and in another three studies, participants paid part of the fees with scholarships or third-party funding paying the gap [67,70,76]. Only 38% of studies (10/26) reported attendance levels, and most of these (k = 7) reported high attendance (categorized as ≥66% of the sessions) [54,63,65,69,70,71,73]. One study reported moderate attendance (51–65% of the sessions) [67], one reported low attendance (≤50% of the sessions) [77], and another reported different low-to-high attendance levels across three different sites [52]. One study reported no adverse events [73], while all other studies did not mention adverse events. Thus, no studies described experiencing adverse events.

Table 1.
Characteristics of included studies.

Table 2.
Summary of participant and program characteristics.
A diverse range of outcomes were reported across the studies, and a brief definition of each broad construct is provided here for readers unfamiliar with this literature. First, “mental health” is used here to describe critical components of psychological well-being, encompassing symptoms of anxiety, depression, and psychological distress, as well as items related to self-perception, including self-esteem (the overall sense of value or worth) and self-worth (value derived from specific achievements or attributes) [78,79,80]. “Social–emotional” outcomes relate to one’s ability to comprehend and regulate emotions, form and sustain healthy relationships, and effectively interact within social contexts. This includes key social skills, such as communication, cooperation, assertion, problem-solving, responsibility, and self-control [81]. “Cognitive” outcomes measure mental processes involved in gaining knowledge and understanding, and they encompass a range of cognitive functions, including memory, attention, executive function, and decision-making [82].
3.3. Program Characteristics
Most interventions were day camps (k = 15) [52,54,56,59,61,62,63,65,66,67,68,69,71,74,75], five were residential (overnight) camps [55,58,70,72,76], and one studied both day-camp and residential formats [73]. Two were delivered at home [53,77]. School was the most common setting for interventions (k = 10 [52,54,55,59,61,62,63,67,74,75]), followed by private organizations (k = 4 studies), including yoga training centers [60], outdoor recreational settings [70], or summer camp [76] facilities or horse-riding schools [72]. Two studies included a diverse range of camps run by different providers [56,73], and one was run by a church-based community group [58]. Partnerships were sometimes formed to share settings, resources, and facilities across sites between schools and community-based organizations, like homeless shelters [68] or local councils partnering with a local urban farm business [69]. Five studies did not specify the setting [57,64,65,66,71].
Just over a third of interventions (k = 10) ran between one and two weeks from start to finish [54,57,58,60,64,65,66,70,72,76]. Single studies lasted for three [71], four [61], or five weeks [75] each. Five studies lasted for six weeks [62,63,67,69,74]. Four studies had ranges of duration (either by allowing participants to select how many sessions they attended or using a research design that contrasted shorter- vs. longer-duration interventions). For these studies, the minimum duration started at 1–5 weeks and went to a maximum of 4–6 weeks [55,59,68,73]. The longest intervention was eight weeks [52]. Three studies did not report the duration of interventions [53,56,77].
Regarding attendance, all but the two home-based programs [53,77] involved daily attendance of 4–5 days per week. Regarding contact hours, ten studies conducted programs using full-day schedules (≥7 h) [55,58,60,63,65,69,70,72,74,76], while four studies each ran their programs during the usual school hours [52,67,68,71] or a half-day schedule [54,61,66,75]. Two home-based programs [53,77] conducted intermittent group sessions, and two others conducted daily sessions lasting approximately two hours (one focusing on building specific conflict resolution skills [62] and another delivering counselling within an existing camp program [59]).
The content of interventions was primarily based around general enrichment (recreation, sports, and play-based programs), with some also targeted toward addressing specific mental health and well-being factors (e.g., overall mental health [53,68,74], stress reduction [59], development of social skills [62,64,77], or reduction in risk behaviors [53,54,66]). Some programs solely targeted physical health [55,75] (e.g., physical activity and weight control), while others combined physical and mental health components [52,76]. Two broad studies covering multiple sites and programs did not report the program content [56,73].
3.4. Participant Characteristics
Studies were categorized into school levels based on the age range of their participants. Primary-school children (kindergarten/reception to grade six, aged from five to 11 years) were targeted in ten studies [52,62,63,65,66,67,68,70,73,77]. Six studies focused on middle-school students (grades 7–9, aged 12–14) [53,58,60,64,72,76]. Three studies focused on high-school aged students (grades 10–12, ages 15 and older) [54,59,69], and seven studies included children across all three age categories [55,57,61,71,74,75].
4. Meta-Analysis
Figure 2 presents the meta-analysis results for each construct, and Supplementary File S6 provides the full results, along with sensitivity analyses.
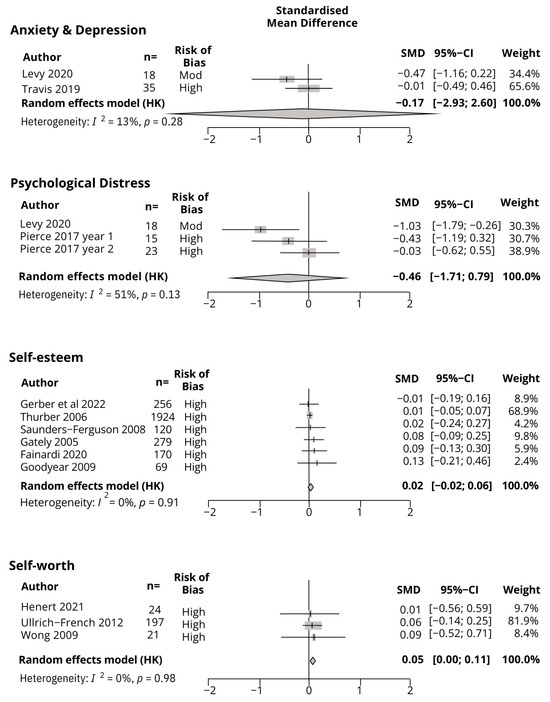
Figure 2.
Meta-analysis results for anxiety and depression, distress, and self-esteem and self-worth.
4.1. Mental Health
A meta-analysis was conducted on combined anxiety and depression scores (n = 53) [59,74] (one study reported only the aggregate anxiety and depression scores [74]; thus, anxiety and depression scores had to be combined). The result indicated that summer programs had a small but statistically non-significant effect in reducing symptoms of anxiety and depression (SMD = −0.17, 95% CI −2.94, 2.60, p = 0.0.58, I2 = 13%). Both studies showed a trend toward improvement. Certainty of evidence: Grade C.
A meta-analysis was conducted on psychological distress in two studies (n = 56 participants) [59,69]. The result indicated that summer programs had a small/moderate but statistically non-significant effect in reducing symptoms of psychological distress (SMD −0.46, 95%CI –1.71, 0.79, p = 0.26, I2 = 51%). A sensitivity analysis identified Levy et al. (2020) [59] as an influential case, and when omitted from the analysis, the effect size reduced to small and remained statistically non-significant. All studies showed a trend toward an improvement. Certainty of evidence: Grade C.
A narrative synthesis was conducted on mental health data from four studies (n = 714) [52,54,58,65]. Two studies measured general mental health and found either a small improvement [65] or no change [54]. Two measured a positive/negative affect: one found improvements [52], and the other (which investigated various settings, curricula, and facilitation strategies across three different intervention programs) also measured life satisfaction and found mixed results for all outcomes [58]. Overall, there was a trend toward improvements in general mental health. Certainty of evidence: Grade C-.
4.2. Self-Perception
A meta-analysis was conducted for self-esteem, based on six studies (total n = 2818) [55,56,65,66,72,73]. The results indicated that summer programs had no effect on self-esteem (SMD = 0.02, 95%CI −0.02, 0.06, p = 0.21, I2 = 0%). Five of the six studies showed a trend toward improvement; however, effect sizes were negligible. The effect of summer programs on self-esteem is negligible. Certainty of evidence: Grade C.
A meta-analysis was conducted for self-worth, based on three studies (n = 424 participants) [67,75,76]. The results indicated that summer programs had no effect on self-worth (SMD = 0.05, 95%CI 0.00, 0.11, p = 0.05, I2 = 0%). The direction of effect was consistent across studies; however, the effect sizes were negligible. Overall, the effect of summer programs on self-worth is negligible. Certainty of evidence: Grade C.
A narrative synthesis was conducted on self-perception-related outcome measures from nine studies [61,63,67,70,72,73,74,75,76]. These included self-concept, self-perception, self-efficacy (competence and confidence), physical appearance, and identity. For self-concept, three studies found improvements [70,76], with one also finding improvements in racial identity [63]. Two found improvements in general, sport, or social competence [61,74], and two more studies found improvements in self-perceptions [73,75]. Two studies found no change in physical appearance and self-acceptance [67,72]. Overall, there was a general trend toward improvements in self-perception. Certainty of evidence: Grade C-.
4.3. Social–Emotional Well-Being
A narrative synthesis was conducted on social–emotional outcomes from fourteen studies (n = 4771 participants) [54,58,61,62,63,64,66,67,68,71,73,74,76,77]. For emotional and behavioral outcomes, an improvement was found in self-control [71], but no change was found in externalizing behaviors [71] or behavioral conduct [76]. Mixed findings were also found when teachers simultaneously rated children’s behaviors as deteriorating while parents rated them as improved [68]. Regarding communication skills, a single study was available that was suggestive of an overall improvement [77]. For pro-social behaviors, improvements were seen in empathy [64], social skills [63,73], social acceptance [76], social competence [67], relationships and coping with problems [66], and aspects of conflict resolution [62]. Other studies found no effect on connection, caring [74], social competence, or belonging [61]. One study had mixed results for social skills across intervention groups that received different curriculum and facilitation strategies [58]. A final study looked at bullying and found improvements in victimization, but no change in perpetration [54]. There was an overall trend toward improvements in social–emotional well-being across the heterogeneous measures of social–emotional well-being. Certainty of evidence: Grade C-.
4.4. Cognition
A narrative synthesis was conducted on cognitive outcomes, including memory [57,60] and executive function [58] (n = 274). All three studies found improvements, with effects ranging from small to large. Certainty of evidence: Grade C.
4.5. Other Outcomes
The remaining outcomes included health-related behaviors (substance use, k = 2 RCTs), personal attributes, and character skills (k = 3 studies) and values (k = 2 studies). For substance use, findings were conflicting, with one finding a small improvement [53] and the other reporting worsening [54]. For personal attributes and character skills, one study each found improvements in physical and thinking skills (related to awareness and enjoyment of the environment) [73] and altruism [56], while two other studies found no changes in “horsemanship attributes” (which included responsibility and motivation) [72] or mindfulness [69]. Certainty of evidence: Grade D-.
5. Subgroup Analysis
Subgroup analyses were performed using count-based methods considering participant characteristics (disadvantage and age) and program features (duration, format, content, funding, and daily contact hours) for each outcome category. The results are detailed in Supplementary File S7.
5.1. Participant Characteristics
A subgroup analysis based on disadvantage was conducted on all 26 studies. Studies that reported outcomes exclusively disadvantaged populations (i.e., low SES or racial minority, n = 18 outcomes) were compared to those from populations not identified as disadvantaged (i.e., mixed SES groups, SES/race not reported, n = 25 outcomes). Disadvantaged children showed more improvements in self-perception, with a trend toward improvements in mental health. Non-disadvantaged studies showed clearer improvements in social–emotional outcomes. A subgroup analysis based on participant age was conducted according to broad school categories (described previously, detailed in Supplementary File S5): primary school (n = 15 outcomes), middle school (n = 13 outcomes), and high school (n = 6 outcomes). There were no clear patterns based on children’s age.
5.2. Program Characteristics
A subgroup analysis was conducted based on format (residential vs. day programs), excluding studies where formats were mixed [73] or not reported [57,60,64]. Home-based programs [53,65,77] were also excluded due to the small number of heterogenous studies preventing meaningful grouping. Residential programs (n = 9 outcomes) targeted weight loss in obese children [55,76], programs for disadvantaged youth [58,70], and those attending a horse-riding camp. Day programs (n = 24 outcomes) [52,54,56,58,61,62,63,66,67,68,69,71,74,75] were much more varied. Day programs showed a clearer pattern of improvement for mental health and social–emotional outcomes. Self-perception improved across both formats.
A subgroup analysis was conducted based on content, comparing studies that had a curriculum with a specific mental, emotional, or social well-being content (n = 18 outcomes) [52,53,54,59,62,64,66,68,69,74,76,77] versus programs that did not (n = 25 outcomes) [55,57,58,60,61,63,65,67,70,72,73,74,75]. Specific programs showed stronger patterns of improvement in social–emotional well-being and self-perception, while non-specific curriculums favored mental health and cognitive improvements.
A subgroup analysis was conducted based on daily contact hours: half day or less (n = 10 outcomes) [53,54,56,61,66,75,77] versus school day or longer programs (n = 24 outcomes) [52,55,58,59,62,63,65,67,68,69,70,71,72,74,76]. Social–emotional and self-perception outcomes improved across both groups, with clearer patterns of improvement in shorter day programs.
A subgroup analysis was conducted based on program duration, comparing programs lasting less than three weeks (n = 18 outcomes) [54,58,64,65,66,70,71,72,76] to programs that ran for three weeks or more (n = 14 outcomes) [52,61,62,67,68,69,74,75]. Studies that did not specify a duration [53,56,77] or that had a range of attendance durations that crossed this cut-off [55,59,73] were omitted from the analysis. There were no clear patterns when comparing shorter- vs. longer-duration programs. Only short programs studied cognitive outcomes, and all demonstrated improvements.
A subgroup analysis was conducted based on the funding model for children’s attendance. Studies where children’s attendance was funded in part or full by the child’s family (n = 8 outcomes) [55,67,70,72,76] was compared to programs where children’s attendance was externally funded (e.g., by the research trial, n = 18 outcomes) [52,53,54,58,62,64,69,73,75]. Family-funded programs appeared to have clearer social–emotional improvements than programs for which students did not pay.
6. Risk of Bias
A majority of studies (k = 22) lacked a comparison group and therefore were considered high risk of bias [52,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,77]. Three were deemed moderate [53,74,75], and one study had a low risk of bias [76]. The items of most concern involved the lack of concealed allocation to treatment arms (achieved by one study [53]) and blinding of the participants [53,76] or evaluators to which study arm the participant was in [74,76], achieved by just two studies each. Self-esteem and self-worth only included studies designated as high risk of bias. The small number of low- or moderate-risk-of-bias studies meant that sensitivity analyses based on risk of bias were not possible. The results for the PEDro risk-of-bias assessment are presented in Supplementary File S7.
7. Discussion
This systematic review aimed to determine the effectiveness of summer holiday programs in improving the mental health, social–emotional well-being, and cognitive (non-academic) outcomes of children and adolescents. It included 26 trials, involving a total of 6812 children. The results revealed that previous studies have measured a wide variety of different mental, social, and cognitive outcomes, though the evidence base for any particular outcome is quite small. The results from the meta-analysis revealed that, while the directions of effects were generally favorable, effect sizes were small and not statistically significant for mental health outcomes (anxiety/depression and distress) and negligible for self-perception outcomes (self-esteem and self-worth). The results from the narrative synthesis indicated trends toward improvements in general measures of mental health, self-perception, social–emotional well-being, and cognition. Disadvantaged populations showed greater improvement in mental health and self-perception compared to non-disadvantaged populations.
First, we can explore how these programs compare to mental health-promotion programs in other settings. A review of systematic reviews (without meta-analysis) of mental health-promotion interventions for children (up to the age of nineteen) found that school-based interventions improved broad constructs of general mental health but did not change problematic behaviors, such as delinquency, conduct disorder, or school non-attendance [83]. More recently, a meta-analysis of school-based interventions that specifically targeted stress, anxiety, and depression found moderate (d = 0.62) improvements in depressive symptoms and no change in anxiety [84]. Targeted programs showed larger effects than universal programs. The effects found in our review are in the same direction as the reviews of school-based interventions, but they are smaller in size. This is most likely because summer program interventions are much shorter than school-based interventions, which can continue for a year or more [85]. Also, the studies included in our review were small and likely underpowered to reveal changes.
It is also important to consider that, in the context of the summer holidays, a lack of deterioration in outcomes may, in fact, indicate a positive finding. A vast majority of the included studies were pre- or post-intervention design, and while there were inconsistencies in the size of the effects across the outcomes, the directions of effects were almost never in the direction of deterioration. These findings should be overlaid on observational research that suggests that numerous outcomes decline during the summer holidays [86]; negative experiences over summer, like social isolation, hunger, and decreased physical activity, can have unfavorable consequences for children’s mental well-being, particularly for disadvantaged children [26]. Thus, a lack of decline may indicate that the summer programs actually did have a protective effect for children’s mental well-being. However, until there are high-quality studies with control group design, this uncertainty will remain unanswered.
The subgroup analysis based on participant characteristics suggested greater improvement in mental health and self-perception in disadvantaged populations compared to non-disadvantaged populations. This may be because children and adolescents from disadvantaged backgrounds are more likely to suffer from poor mental health [87] and, therefore, have more scope to improve over the course of the intervention than children already scoring well at baseline. This was the case for Thurber and colleagues [73] in their study of over five thousand children attending one of 80 accredited summer camps across the United States (n = 3395 completed both baseline and immediate post-camp measures). They found that children with the lowest scores pre-camp made the greatest gains over the course of the summer program. This could reflect a sharper contrast between the out-of-school environments typically experienced by disadvantaged children compared to non-disadvantaged children and, therefore, the greater relative benefits gained from being within the supportive networks and environments of summer programs.
The subgroup analysis based on program characteristics suggested a somewhat surprising pattern. While targeted programs appeared better at improving social–emotional outcomes than general programs, the reverse was the case for mental health and cognitive outcomes, where general programs seemed more effective. When we explored this finding further, we found that the targeted programs tended to recruit populations living with a greater number of risk factors for mental health issues [88], such as children living with mentally ill parents [66] or in homeless shelters [68], as well as disadvantaged populations (racial minority and low socioeconomic status). Taken together, our findings could indicate that social–emotional outcomes are more amenable to the interventions offered, while mental health outcomes are harder to change in the face of persistent structural barriers outside the scope of the summer program. Conversely, our findings may highlight the value of play and physical activity in enhancing youth mental health, as the general programs frequently focused on sports, outdoor recreation, yoga, and increasing physical activity.
It is important to acknowledge the study’s strengths and limitations. Importantly, this is the first review to explore the effect of summer programs on children’s mental, emotional, or social well-being. This review used rigorous systematic review methodology, including a highly comprehensive search strategy, and used a meta-analysis to synthesize data. It also considered a wide range of mental, emotional, and social outcomes. However, the review has a number of limitations, mostly related to the current state of the evidence base on this topic. The majority of included studies had small sample sizes and were rated as having a high risk of bias. Less than a quarter of the studies used a controlled design, which seems particularly prudent here, where previous observational studies have demonstrated clear time effects. While many outcomes were measured, there were inconsistencies in the use and reporting of validated outcome measures, with some studies using self-designed questionnaires. The majority of the studies were from the United States, limiting the generalizability to other contexts. While this limits our ability to draw strong conclusions from these data, there are still valuable insights to be gleaned on the role that summer holiday programs could play in improving the mental health of young people.
There are several important implications from this review. First, it builds on our understanding of how summer programs can impact children’s health in a holistic sense. Summer programs have demonstrated effectiveness in improving academic outcomes including reading, writing [31], and mathematics [89], and physical health outcomes, including reducing sedentary behavior by increasing moderate-to-vigorous physical activity [55,90,91]. The current review highlights the quality and design issues of studies of summer programs targeting mental–emotional well-being. The same rigor that has been used to investigate health and academic outcomes should be adopted in future studies to explore the effect that summer programs have on mental and emotional well-being outcomes. Further research using rigorously designed and conducted RCTs is needed to test the effectiveness of specific mental health interventions delivered within (or as) summer holiday programs. Due to a lack of data on the mental health challenges children face and their “natural” trajectory over summer, control-group data will be vital to further help us understand the role that summer programs play in children’s overall mental health and well-being. Future intervention studies should clearly describe the components and structure of their interventions and use consistent, validated outcome measures to detect changes in mental, social, and emotional outcomes so that the most effective program structure and content can be identified.
Summer programs may form part of a broader mental health-promotion strategy. Summer programs could complement school-based interventions by providing further small gains, or at least preventing regression, during a potentially high-risk time for declines. This could lead to cumulative effects when interventions in school and summer settings are run side by side [89]. But in order to improve mental health outcomes for entire populations, interventions need to be delivered at scale in real-world settings, a task that has proven exceptionally difficult thus far [85]. Taking an implementation science approach to future research is necessary and involves designing or adapting programs into potentially suitable large-scale delivery models.
There are policy implications for these findings. Ensuring equitable access to mental health interventions is crucial so that the populations in need (e.g., disadvantaged families, those living with a greater number of risk factors for mental health disorders) are able to access them. Some have highlighted the need for greater cross-disciplinary collaboration in the design and implementation of trials, as such cross-disciplinary collaboration is currently hindered by existing policies and practices related to training, trial funding, and publishing [85]. Addressing these barriers requires concerted efforts to foster collaboration across various disciplines, ensuring comprehensive and inclusive mental health interventions.
8. Conclusions
The evidence base is affected by studies with a high risk of bias and clinical heterogeneity. Included studies generally show trends toward improvement, though often with small effect sizes. Disadvantaged children exhibited more significant improvements in self-perception and a trend toward better mental health. Future research on summer programs should incorporate validated measures of anxiety, depression, and psychological distress, utilizing high-quality, rigorously designed trials with clearly reported intervention components. Given the demonstrated improvements in academic and physical health outcomes, summer programs present a promising intervention strategy to mitigate health declines, especially in disadvantaged populations, during a potentially high-risk period.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/children11080887/s1. File S1: Inclusion-exclusion criteria; File S2: Search strategy; File S3: Example data extraction form; File S4: Reasons for exclusion table; File S5: Thematic Coding of Study and Program Characteristics; File S6: Mental Health Meta analysis with sensitivity; File S7: Mental health subgroup analyses.
Author Contributions
E.E. conceptualized the study, designed the data collection instruments, collected (ran searches, conducted study screening and data extraction) data, carried out the analyses, and drafted the initial manuscript. B.S. contributed to study selection, assisted analyses, and critically reviewed the revised manuscript. C.S. assisted with study screening, data extraction, analyses, and data synthesis and reviewed the manuscript. C.M. and T.O. supervised the study, assisted with the conceptualization and design of the review, and critically reviewed the manuscript. R.V. and A.M. assisted with the design of the study and critically reviewed and revised the manuscript. M.R. and K.B. assisted with the conceptualization and design of the study and revised the manuscript for important intellectual content. A.G., J.G., T.W. and Z.R. contributed significantly to the data acquisition process (study screening and data extraction), assisted in analysis and data synthesis, and assisted it the revision of the document. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work, including accuracy and integrity. All authors have read and agreed to the published version of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The funding of the authorship team is as follows (funding bodies supporting the authorship team had no role in this review): Carol Maher received an Investigator Grant from the Medical Research Future Fund (MRF1193862). Emily Eglitis is supported by an RTP grant. There was no specific support for this review.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets analyzed in this review are derived from publicly available sources. All data can be accessed through the original publications.
Acknowledgments
The authors acknowledge the assistance of Scott Dale, Academic Librarian, University of South Australia, for advice in the development of the search strategy; and Rachel Curtis (Behavioural Scientist) for assistance in grouping outcomes into appropriate categories.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organisation. Mental Health. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response (accessed on 16 July 2024).
- Keyes, C.L. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J. Consult. Clin. Psychol. 2005, 73, 539. [Google Scholar] [CrossRef] [PubMed]
- Suldo, S.M.; Shaffer, E.J. Looking Beyond Psychopathology: The Dual-Factor Model of Mental Health in Youth. Sch. Psychol. Rev. 2008, 37, 52–68. [Google Scholar] [CrossRef]
- National Scientific Council on the Developing Child. Establishing a Level Foundation for Life: Mental Health Begins in Early Childhood; Harvard University, Center on the Developing Child: Cambridge, MA, USA, 2012. [Google Scholar]
- O’Connor, M.; Cloney, D.; Kvalsvig, A.; Goldfeld, S. Positive Mental Health and Academic Achievement in Elementary School: New Evidence from a Matching Analysis. Educ. Res. 2019, 48, 205–216. [Google Scholar] [CrossRef]
- Jonsson, U.; Alaie, I.; Löfgren Wilteus, A.; Zander, E.; Marschik, P.B.; Coghill, D.; Bölte, S. Annual Research Review: Quality of life and childhood mental and behavioural disorders—A critical review of the research. J. Child Psychol. Psychiatry 2017, 58, 439–469. [Google Scholar] [CrossRef] [PubMed]
- Celebre, A.; Stewart, S.L.; Theall, L.; Lapshina, N. An examination of correlates of quality of life in children and youth with mental health issues. Front. Psychiatry 2021, 12, 709516. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Mental Health of Adolescents. Available online: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health/ (accessed on 11 April 2024).
- Costello, E.J.; Egger, H.; Angold, A. 10-Year Research Update Review: The Epidemiology of Child and Adolescent Psychiatric Disorders: I. Methods and Public Health Burden. J. Am. Acad. Child Adolesc. Psychiatry 2005, 44, 972–986. [Google Scholar] [CrossRef] [PubMed]
- Copeland, W.E.; Wolke, D.; Shanahan, L.; Costello, E.J. Adult Functional Outcomes of Common Childhood Psychiatric Problems: A Prospective, Longitudinal Study. JAMA Psychiatry 2015, 72, 892–899. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, N.; Abdulghani, E.A.; Alonso, J.; Bromet, E.; Bruffaerts, R.; Caldas-de-Almeida, J.M.; Chiu, W.T.; de Girolamo, G.; de Graaf, R.; Fayyad, J.; et al. Early-Life Mental Disorders and Adult Household Income in the World Mental Health Surveys. Biol. Psychiatry 2012, 72, 228–237. [Google Scholar] [CrossRef] [PubMed]
- Basu, S.; Banerjee, B. Impact of environmental factors on mental health of children and adolescents: A systematic review. Child. Youth Serv. Rev. 2020, 119, 105515. [Google Scholar] [CrossRef]
- Cortés Pascual, A.; Moyano Muñoz, N.; Quílez Robres, A. The relationship between executive functions and academic performance in primary education: Review and meta-analysis. Front. Psychol. 2019, 10, 449759. [Google Scholar] [CrossRef]
- Sankalaite, S.; Huizinga, M.; Dewandeleer, J.; Xu, C.; de Vries, N.; Hens, E.; Baeyens, D. Strengthening executive function and self-regulation through teacher-student interaction in preschool and primary school children: A systematic review. Front. Psychol. 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, J.A.; Goodrich, J.M.; Morris, B.M.; Osborne, C.M.; Lonigan, C.J. Relations between executive functions and academic outcomes in elementary school children: A meta-analysis. Psychol. Bull. 2021, 147, 329. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, L. Executive Function in Education: From Theory to Practice; Guilford Publications: New York, NY, USA, 2018. [Google Scholar]
- El-Daw, B.; Hammoud, H. The effect of building up self-esteem training on students’ social and academic skills 2014. Procedia-Soc. Behav. Sci. 2015, 190, 146–155. [Google Scholar] [CrossRef]
- Eijgenraam, L. Why Children Need Boundaries: How Clear Rules and Healthy Habits Will Help Your Children Thrive; Floris Books: Stourbridge, UK, 2020. [Google Scholar]
- Domitrovich, C.E.; Durlak, J.A.; Staley, K.C.; Weissberg, R.P. Social-Emotional Competence: An Essential Factor for Promoting Positive Adjustment and Reducing Risk in School Children. Child Dev. 2017, 88, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Waldrip, A.M.; Malcolm, K.T.; Jensen-Campbell, L.A. With a little help from your friends: The importance of high-quality friendships on early adolescent adjustment. Soc. Dev. 2008, 17, 832–852. [Google Scholar] [CrossRef]
- Baranowski, T.; O’Connor, T.; Johnston, C.; Hughes, S.; Moreno, J.; Chen, T.-A.; Meltzer, L.; Baranowski, J. School year versus summer differences in child weight gain: A narrative review. Child. Obes. 2014, 10, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Brazendale, K.; Beets, M.W.; Weaver, R.G.; Pate, R.R.; Turner-McGrievy, G.M.; Kaczynski, A.T.; Chandler, J.L.; Bohnert, A.; von Hippel, P.T. Understanding differences between summer vs. school obesogenic behaviors of children: The structured days hypothesis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Alonzo, R.; Hussain, J.; Stranges, S.; Anderson, K.K. Interplay between social media use, sleep quality, and mental health in youth: A systematic review. Sleep Med. Rev. 2021, 56, 101414. [Google Scholar] [CrossRef] [PubMed]
- Biddle, S.J.; Asare, M. Physical activity and mental health in children and adolescents: A review of reviews. Br. J. Sports Med. 2011, 45, 886–895. [Google Scholar] [CrossRef] [PubMed]
- Biddle, S.J.H.; Ciaccioni, S.; Thomas, G.; Vergeer, I. Physical activity and mental health in children and adolescents: An updated review of reviews and an analysis of causality. Psychol. Sport Exerc. 2019, 42, 146–155. [Google Scholar] [CrossRef]
- Morgan, K.; Melendez-Torres, G.; Bond, A.; Hawkins, J.; Hewitt, G.; Murphy, S.; Moore, G. Socio-Economic Inequalities in Adolescent Summer Holiday Experiences, and Mental Wellbeing on Return to School: Analysis of the School Health Research Network/Health Behaviour in School-Aged Children Survey in Wales. Int. J. Environ. Res. Public Health 2019, 16, 1107. [Google Scholar] [CrossRef] [PubMed]
- Kromydas, T.; Campbell, M.; Chambers, S.; Boon, M.H.; Pearce, A.; Wells, V.; Craig, P. The effect of school summer holidays on inequalities in children and young people’s mental health and cognitive ability in the UK using data from the millennium cohort study. BMC Public Health 2022, 22, 154. [Google Scholar] [CrossRef] [PubMed]
- Rulison, K.L.; Gest, S.D.; Loken, E.; Welsh, J.A. Rejection, feeling bad, and being hurt: Using multilevel modeling to clarify the link between peer group aggression and adjustment. J. Adolesc. 2010, 33, 787–800. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.F.; Conway, T.L.; Cain, K.L.; Geremia, C.M.; Bonilla, E.; Spoon, C. Race/ethnic variations in school-year versus summer differences in adolescent physical activity. Prev. Med. 2019, 129, 105795. [Google Scholar] [CrossRef]
- Cooper, H.; Charlton, K.; Valentine, J.C.; Muhlenbruck, L.; Borman, G.D. Making the most of summer school: A meta-analytic and narrative review. Monogr. Soc. Res. Child Dev. 2000, 65, 1–127. [Google Scholar] [CrossRef]
- Dujardin, E.; Ecalle, J.; Gomes, C.; Magnan, A. Summer Reading Program: A Systematic Literature Review. Soc. Educ. Res. 2022, 4, 108–121. [Google Scholar] [CrossRef]
- Lynch, K.; An, L.; Mancenido, Z. The Impact of Summer Programs on Student Mathematics Achievement: A Meta-Analysis. Rev. Educ. Res. 2022, 93, 275–315. [Google Scholar] [CrossRef]
- Wilson, C.; Sibthorp, J.; Brusseau, T.A. Increasing Physical Activity and Enjoyment Through Goal-Setting at Summer Camp. J. Park Recreat. Adm. 2017, 35, 24–36. [Google Scholar] [CrossRef]
- Brazendale, K.; Beets, M.W.; Weaver, R.G.; Turner-McGrievy, G.M.; Moore, J.B.; Huberty, J.L.; Ward, D.S. Turn up the healthy eating and activity time (HEAT): Physical activity outcomes from a 4-year non-randomized controlled trial in summer day camps. Prev. Med. Rep. 2020, 17, 101053. [Google Scholar] [CrossRef]
- Eglitis, E.; Maher, C.; Virgara, R.; Watson, A.; Olds, T.; Richardson, M.; Singh, B.; Rix, Z.; Wilkinson, T. Effect of Summer Holiday Programs on Children’s Mental Health and Wellbeing: Protocol for a Systematic Review. PROSPERO: International Prospective Register of Systematic Reviews. [CRD42023409799]. National Institute for Health and Care Research. 2023. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023409799 (accessed on 21 March 2023).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, n71. [Google Scholar] [CrossRef]
- Eglitis, E.; Simpson, C.; Singh, B.; Olds, T.; Virgara, R.; Machell, A.; Richardson, M.; Grant, A.; Gray, J.; Wilkinson, T.; et al. Effect of summer holiday programs on children’s mental health and wellbeing (MEDLINE). searchRxiv 2023. [Google Scholar] [CrossRef]
- Oude Wolcherink, M.J.; Pouwels, X.G.L.V.; van Dijk, S.H.B.; Doggen, C.J.M.; Koffijberg, H. Can artificial intelligence separate the wheat from the chaff in systematic reviews of health economic articles? Expert Rev. Pharmacoecon. Outcomes Res. 2023, 23, 1049–1056. [Google Scholar] [CrossRef] [PubMed]
- De Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Cashin, A.G.; McAuley, J.H. Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J. Physiother. 2020, 66, 59. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; L. Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef]
- Harrer, M.; Cuijpers, P.; Furukawa, T.; Daniel, D.E. dmetar: Companion R Package for The Guide ‘Doing Meta-Analysis in R’; R Core Team: Vienna, Austria, 2019. [Google Scholar]
- R Core Team R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2018. Available online: https://www.R-project.org/ (accessed on 1 July 2023).
- Balduzzi, S.; Rücker, G.; Schwarzer, G. How to perform a meta-analysis with {R}: A practical tutorial. Evid. -Based Ment. Health 2019, 22, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Harrer, M.; Cuijpers, P.; Furukawa, T.A.; Ebert, D.D. Doing Meta-Analysis with R: A Hands-On Guide, 1st ed.; Chapman & Hall/CRC Press: Boca Raton, FL, USA; London, UK, 2021. [Google Scholar]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 6.4; Cochrane: London, UK, 2023. [Google Scholar]
- Campbell, M.; McKenzie, J.E.; Sowden, A.; Katikireddi, S.V.; Brennan, S.E.; Ellis, S.; Hartmann-Boyce, J.; Ryan, R.; Shepperd, S.; Thomas, J.; et al. Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ 2020, 368, l6890. [Google Scholar] [CrossRef] [PubMed]
- Wilson, D.B. Practical Meta-Analysis Effect Size Calculator; Version 2023.11.27; George Mason University: Fairfax, VI, USA, 2023; Available online: https://www.campbellcollaboration.org/escalc/ (accessed on 1 April 2023).
- OCEBM Levels of Evidence Working Group. The Oxford 2011 Levels of Evidence. Oxford Centre for Evidence-Based Medicine. 2011. Available online: http://www.cebm.net/index.aspx?o=5653 (accessed on 25 January 2023).
- Phillips, B.; Ball, C.; Sackett, D.; Badenoch, D.; Straus, S.; Haynes, B.; Dawes, M.; Howick, J. Oxford Centre for Evidence-Based Medicine: Levels of Evidence (March 2009). Available online: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009 (accessed on 25 January 2024).
- Hopkins, L.C.; Holloman, C.; Melnyk, B.; Fristad, M.; Goodway, J.D.; Kennel, J.A.; Eneli, I.; Gunther, C. Participation in structured programming may prevent unhealthy weight gain during the summer in school-aged children from low-income neighbourhoods: Feasibility, fidelity and preliminary efficacy findings from the Camp NERF study. Public Health Nutr. 2019, 22, 1100–1112. [Google Scholar] [CrossRef] [PubMed]
- Werch, C.E.; Carlson, J.M.; Pappas, D.M.; Edgemon, P.; DiClemente, C.C. Effects of a brief alcohol preventive intervention for youth attending school sports physical examinations. Subst. Use Misuse 2000, 35, 421–432. [Google Scholar] [CrossRef]
- Exner-Cortens, D.; Wolfe, D.; Crooks, C.V.; Chiodo, D. A preliminary randomized controlled evaluation of a universal healthy relationships promotion program for youth. Can. J. Sch. Psychol. 2020, 35, 3–22. [Google Scholar] [CrossRef]
- Gately, P.; Cooke, C.; Barth, J.H.; Bewick, B.M.; Radley, D.; Hill, A.J. Children’s Residential Weight-Loss Programs Can Work: A Prospective Cohort Study of Short-Term Outcomes for Overweight and Obese Children. Pediatrics 2005, 116, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Gerber, Y.; Gentaz, E.; Malsert, J. The effects of Swiss summer camp on the development of socio-emotional abilities in children. PLoS ONE 2022, 17, e0276665. [Google Scholar] [CrossRef] [PubMed]
- Manjunath, N.K.; Telles, S. Spatial and verbal memory test scores following yoga and fine arts camps for school children. Indian J. Physiol. Pharmacol. 2004, 48, 353–356. [Google Scholar] [PubMed]
- Smith, B.H.; Kim, H.; Esat, G.; Izuno-Garcia, A.K.; Meinert, A.; Banks Hawthorne, D.; Vazquez, M.; Gonzalez, J. Comparing Three Overnight Summer Camp Experiences for Marginalized Middle School Students: Negative, Neutral, and Positive Results. J. Exp. Educ. 2022, 45, 136–156. [Google Scholar] [CrossRef]
- Levy, I.; Travis, R. The Critical Cycle of Mixtape Creation: Reducing Stress via Three Different Group Counseling Styles. J. Spec. Group Work. 2020, 45, 307–330. [Google Scholar] [CrossRef]
- Pradhan, B.; Nagendra, H.R. Effect of yoga relaxation techniques on performance of digit-letter substitution task by teenagers. Int. J. Yoga 2009, 2, 30–34. [Google Scholar]
- Anderson-Butcher, D.; Iachini, A.L.; Riley, A.; Wade-Mdivanian, R.; Davis, J.; Amorose, A.J. Exploring the impact of a summer sport-based youth development program. Eval. Program Plan. 2013, 37, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Ay, S.C.; Keskin, H.K.; Akilli, M. Examining the effects of negotiation and peer mediation on students’ conflict resolution and problem-solving skills. Int. J. Instr. 2019, 12, 717–730. [Google Scholar] [CrossRef]
- Bethea, S.L. The Impact of Oakland Freedom School’s Summer Youth Program on the Psychosocial Development of African American Youth. J. Black Psychol. 2012, 38, 442–454. [Google Scholar] [CrossRef]
- de los Pinos, C.C.; Soto, A.G.; Conty, J.L.M.; Serrano, R.C. Summer Camp: Enhancing Empathy Through Positive Behavior and Social and Emotional Learning. J. Exp. Educ. 2020, 43, 105382592092338–105382592092415. [Google Scholar] [CrossRef]
- Fainardi, V.; Fasola, S.; Mastrorilli, C.; Volta, E.; La Grutta, S.; Vanelli, M. A two-week summer program promoting physical activity: Quality of life assessment in Italian children. Psychol. Health Med. 2020, 26, 444–456. [Google Scholar] [CrossRef] [PubMed]
- Goodyear, M.; Cuff, R.; Maybery, D.; Reupert, A. CHAMPS: A peer support program for children of parents with a mental illness. AeJAMH Aust. e-J. Adv. Ment. Health 2009, 8, 296–304. [Google Scholar] [CrossRef]
- Henert, S.; Jacobs, J.; Wahl-Alexander, Z. Let’s play! Exploring the impact of summer day camp participation on the physical and psychosocial experiences of diverse urban youth. Child Adolesc. Soc. Work. J. 2021, 38, 381–391. [Google Scholar] [CrossRef]
- Nabors, L.; Proescher, E.; DeSilva, M. School-based mental health prevention activities for homeless and at-risk youth. Child Youth Care Forum 2001, 30, 3–18. [Google Scholar] [CrossRef]
- Pierce, B.A.; Bowden, B.; McCullagh, M.; Diehl, A.; Chissell, Z.; Rodriguez, R.; Berman, B.; Adamo, C.R.D. A Summer Health Program for African-American High School Students in Baltimore, Maryland: Community Partnership for Integrative Health. Explore 2017, 13, 186–197. [Google Scholar] [CrossRef] [PubMed]
- Readdick, C.A.; Schaller, G.R. Summer camp and self-esteem of school-age inner-city children. Percept. Mot. Ski. 2005, 101, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Riley, A.; Anderson-Butcher, D.; Logan, J.A.R.; Newman, T.J.; Davis, J. Staff Practices and Social Skill Outcomes in a Sport-Based Youth Program. J. Appl. Sport Psychol. 2016, 29, 59–74. [Google Scholar] [CrossRef]
- Saunders-Ferguson, K.; Barnett, R.V.; Culen, G.; Tenbroeck, S. Self-esteem assessment of adolescents involved in horsemanship activities. J. Ext. 2008, 46, 8. [Google Scholar]
- Thurber, C.A.; Scanlin, M.M.; Scheuler, L.; Henderson, K.A. Youth Development Outcomes of the Camp Experience: Evidence for Multidimensional Growth. J. Youth Adolesc. 2006, 36, 241–254. [Google Scholar] [CrossRef]
- Travis, R., Jr.; Gann, E.; Crooke, A.H.; Jenkins, S.M. Hip hop, empowerment, and therapeutic beat-making: Potential solutions for summer learning loss, depression, and anxiety in youth. J. Hum. Behav. Soc. Environ. 2019, 29, 744–765. [Google Scholar] [CrossRef]
- Ullrich-French, S.; McDonough, M.H.; Smith, A.L. Social Connection and Psychological Outcomes in a Physical Activity-Based Youth Development Setting. Res. Q. Exerc. Sport 2012, 83, 431–441. [Google Scholar] [CrossRef] [PubMed]
- Wong, W.W.; Abrams, S.H.; Mikhail, C.; Terrazas, N.L.; Wilson, T.A.; Arceo, D.; Mrowczynski, P.K.; King, K.L.; Stansel, A.D.; Albright, A.N.; et al. An innovative summer camp program improves weight and self-esteem in obese children. J. Pediatr. Gastroenterol. Nutr. 2009, 49, 493–497. [Google Scholar] [CrossRef] [PubMed]
- Fujieda, S. A practical study of the social skills training at home for elementary school children during summer and winter vacation. Jpn. J. Couns. Sci. 2011, 44, 313–322. [Google Scholar]
- Ryff, C.D.; Keyes, C.L.M. The structure of psychological well-being revisited. J. Personal. Soc. Psychol. 1995, 69, 719. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Andrews, G.; Colpe, L.J.; Hiripi, E.; Mroczek, D.K.; Normand, S.-L.; Walters, E.E.; Zaslavsky, A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef] [PubMed]
- Harter, S. The Construction of the Self: A Developmental Perspective; Guilford Press: New York, NY, USA, 1999. [Google Scholar]
- Gresham, F.M. Social skills assessment and intervention for children and youth. Camb. J. Educ. 2016, 46, 319–332. [Google Scholar] [CrossRef]
- Diamond, A. Executive functions. Annu. Rev. Psychol. 2013, 64, 135–168. [Google Scholar] [CrossRef] [PubMed]
- Tennant, R.; Goens, C.; Barlow, J.; Day, C.; Stewart-Brown, S. A systematic review of reviews of interventions to promote mental health and prevent mental health problems in children and young people. J. Public Ment. Health 2007, 6, 25–32. [Google Scholar] [CrossRef]
- Feiss, R.; Dolinger, S.B.; Merritt, M.; Reiche, E.; Martin, K.; Yanes, J.A.; Thomas, C.M.; Pangelinan, M. A systematic review and meta-analysis of school-based stress, anxiety, and depression prevention programs for adolescents. J. Youth Adolesc. 2019, 48, 1668–1685. [Google Scholar] [CrossRef]
- O’Reilly, M.; Svirydzenka, N.; Adams, S.; Dogra, N. Review of mental health promotion interventions in schools. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 647–662. [Google Scholar] [CrossRef]
- Eglitis, E.; Miatke, A.; Virgara, R.; Machell, A.; Olds, T.; Richardson, M.; Maher, C. Children’s Health, Wellbeing and Academic Outcomes over the Summer Holidays: A Scoping Review. Children 2024, 11, 287. [Google Scholar] [CrossRef] [PubMed]
- Reiss, F. Socioeconomic inequalities and mental health problems in children and adolescents: A systematic review. Soc. Sci. Med. 2013, 90, 24–31. [Google Scholar] [CrossRef] [PubMed]
- National Research Council (US) and Institute of Medicine (US) Committee on the Prevention of Mental Disorders; Substance Abuse Among Children, Youth; Young Adults: Research Advances; Promising Interventions. Preventing Mental, Emotional, and Behavioral Disorders among Young People: Progress and Possibilities; National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Lynch, K.; Kim, J.S. Effects of a summer mathematics intervention for low-income children: A randomized experiment. Educ. Eval. Policy Anal. 2017, 39, 31–53. [Google Scholar] [CrossRef]
- Dugger, R.; Brazendale, K.; Hunt, E.T.; Moore, J.B.; Turner-McGrievy, G.; Vogler, K.; Beets, M.W.; Armstrong, B.; Weaver, R.G. The impact of summer programming on the obesogenic behaviors of children: Behavioral outcomes from a quasi-experimental pilot trial. Pilot Feasibility Stud. 2020, 6, 1–15. [Google Scholar] [CrossRef]
- D’Haese, S.; Van Dyck, D.; De Bourdeaudhuij, I.; Deforche, B.; Cardon, G. Organizing “Play Streets” during school vacations can increase physical activity and decrease sedentary time in children. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 1–9. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).