Abstract
Introduction. Evidence is consistent with increased screen viewing time among children and adolescents, and anticipation at the age at which children interact with media devices. Incorrect use of technology, as well as overuse, may lead to serious consequences. This study aims to revise scientific international literature and to describe the potential eye risks correlated to screen viewing time in the pediatric age. Materials and Methods. A review of the literature was performed according to the PRISMA 2020 guidelines, using the search terms “media device” and “eye” with the filter “age 0–18”. Results. Analyzing the international literature, we found 26 articles. Pre-myopia, myopia, digital eye strain, and acute acquired comitant esotropia were listed as potential and time-related consequences associated with the incorrect use of media devices among children and adolescents. Discussion. Family education on media device exposure and potential risk for children and adolescents’ sight in case of prolonged digital/screen exposure is required. During pediatric check controls, a dialogue with families on prolonged media device use at a close distance should be undertaken. Pediatricians and ophthalmologists should consider screen viewing time in case of ocular problems.
1. Introduction
Screen viewing time (SVT), or digital/screen exposure, is the total time spent by an individual viewing or using any digital or electronic device, such as televisions, smartphones, tablets, videogames, or computers [].
Evidence is consistent with children starting to use online platforms at an early age in industrialized countries [,,]. In America, a study showed that 96.6% of young children aged 6 months to 4 years used mobile devices, and most began to use them before the age of 1 year []. Evidence suggests a constant use of electronic devices, with even 68% of children under age 3 using screen media daily [].
According to the American Academy of Pediatrics guidelines, children younger than 24 months should not be exposed to media devices and those aged 2 to 5 years should keep their SVT to under 1 h/day [].
Young Italian children are overly exposed to mobile devices. The Italian Paediatric Society recommends no media device exposure in children aged less than 2 years, no more than 2 h daily in those aged 2–5 years, and no more than 4 h/day in older children [].
Nevertheless, media device use in early childhood is still a matter of concern because of the potential risks. According to the literature, unhealthy and excessive media device exposure may lead to physical and neuropsychological impairments, including depression, hostile and aggressive behavior, obesity, musculoskeletal discomfort, and sleep and eye disorders [,,,]. As well as in early childhood, in adolescence prolonged media device use may negatively influence the psychophysical development of the adolescent, such as in learning, sleep, and sight. Moreover, obesity, distraction, addiction, cyberbullying, and Hikikomori phenomena are described in adolescents who use media devices too frequently. The Italian Paediatric Society provides action-oriented recommendations for families and clinicians to avoid negative outcomes [].
This study aims to examine international awareness of the impact of media device exposure on the eye in childhood.
2. Material and Methods
A review of the literature was performed according to the PRISMA guidelines [] on 30 May 2024. An electronic search was undertaken, first using the PubMed database, searching for “media device” and “eye” with the filter “age 0–18”, article language “English”, and publication date of the last ten years. Then, we investigated other database sets, namely Embase, Web of Science, and Scopus. On Embase we used the search terms “media device” AND “eye”, from 2014 to 2024; on Web of Science, the topics “media device” and “eye” were refined by publication years from 2014 to 2024, and limited to infant or child preschool or child or adolescent; and on Scopus, the keywords “media device” and “eye” were limited to adolescent or child or infant, with publication date from 2014 to 2024.
Duplicates were identified and unnecessary copies were excluded. Authors independently evaluated titles and abstracts produced by the literature analysis to limit bias and mistakes. Studies were considered eligible if they met the following inclusion criteria:
- -
- full-length articles or reviews;
- -
- on children and adolescents up to 18 years old;
- -
- reports dealing with media device consequences on the eye;
- -
- English language.
The exclusion criteria were:
- -
- reports including adults (>18 years);
- -
- reports dealing with other themes.
Then, full texts were evaluated for eligibility by the authors. If full-text articles could not be found, an attempt to contact authors was performed to obtain the full text.
According to the PRISMA guidelines, articles not included in the original PubMed search but considered relevant to the report were evaluated. All the authors conducted a 1 h discussion, examining doubts regarding inclusion/exclusion for any report.
Additionally, to ensure further data were not missed, a second search was undertaken in the PubMed database using the keywords “media device” and “myopia”, “media device” and “digital eye strain”, and “media device” and “acute acquired comitant esotropia”. The same filters of the previous search were used.
3. Results
From PubMed, out of the 102 examined papers, only 4 papers fulfilled the criteria for inclusion in the review [,,,]. As detailed in Figure 1, 98 articles were excluded because they dealt with other themes (94), involved adults (3), or did not provide supporting data (1). From the references of the examined papers, 22 articles were selected and added to the study [,,,,,,,,,,,,,,,,,,,,,]. Regarding the other databases, according to our search strategy and inclusion criteria, we found 4 results in Embase, 61 in Web of Science, and 13 in Scopus. Nevertheless, we did not include them in the review because they were all duplicates of the PubMed results.
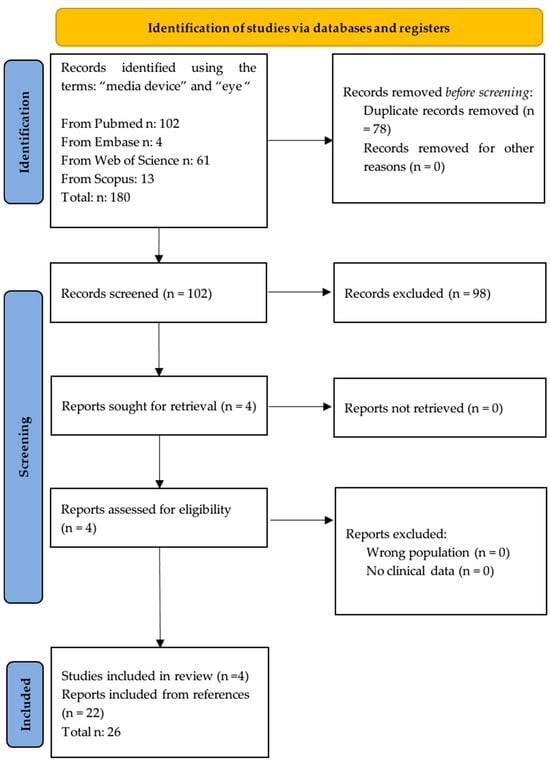
Figure 1.
Flow chart of the selected process.
Analyzing the manuscripts, myopia, digital eye strain, and acute acquired comitant esotropia were the most frequent consequences reported by the literature.
From the second search, we found six results pertaining to myopia, four to digital eye strain, and zero to acute acquired comitant esotropia. Of these, four were already included, one involved either adults or children, and five dealt with other themes [,,,].
3.1. Myopia
From the literature search, 18 reports dealt with the risk of pre-myopia and myopia in childhood and adolescence linked to media device exposure [,,,,,,,,,,,,,,,,,]. Table 1 summarizes the evidence. The evidence suggests that the risk is mainly time-related [,,,,]. Either in childhood or in adolescence, a high use of screen devices is associated with the risk of developing myopia, defined as “a condition in which the spherical equivalent refractive error of an eye is ≤−0.5 D when ocular accommodation is relaxed” [,,,]. Many authors reported media devices as harmful and gave objective proof referring to different types of devices. Many authors reported smartphones and computers being more harmful. In detail, a more myopic spherical equivalent refraction (SER) and a longer axial length (AL) were associated with more time on smartphones and computers, but not on tablets and television [,,]. Computers and smartphones were also linked with an increased risk of myopia compared to television []. Indian reports also correlated refractive deficit with television [,]. Behavioral and modifiable risk factors regarding myopia were evaluated in scientific reports [,,,,,,]. In detail, reduced physical activity and Westernized dietary habits have been associated with media devices [,,,,,,]. A high socio-economic status has also been discussed as a potential risk factor, as students attending private schools were more likely to have access to technology [].

Table 1.
Media device and myopia.
Of note, screen exposure in the postnatal first year, which may be a sensitive period, may lead to later development of myopia in the preschool age [].
Either in childhood or in adolescence, the high use of a screen device is associated with the risk of developing myopia [,]. Childhood and adolescent vision health declined during the COVID-19 period, likely due to increased SVT and online e-learning, an inevitable consequence of lockdown and restrictive measures. In this period, significant increases in myopia and myopic progression were reported [,,,,]. The mean number and time of online classes, as well as the total digital screen exposure duration, were negatively correlated with myopia [].
3.1.1. DES (Digital Eye Strain)
According to the search strategy, seven reports dealt with the risk of digital eye strain (DES) in childhood linked to media device exposure, as reported in Table 2 [,,,,,,]. In the literature, DES or computer vision syndrome is the term used to collectively indicate “dry eyes, impaired vision, near-sightedness, headaches, and eye fatigue” attributed to prolonged usage of desktops, laptops, mobile phones, etc. The main symptoms include blurring, redness, visual disturbance, secretion, inflammation, lacrimation, and dryness. []

Table 2.
Digital eye strain and media device.
Its pathophysiology is multifactorial, with several contributing factors, including reduced contrast level of letters compared to the background of digital screens, screen glare and reflections, wrong distance and angle of viewing digital screens, poor lighting conditions, improper posture during usage, and infrequent blinking of eyes [,]. A reduced blink rate and faster evaporation of the tear film in the case of prolonged media device use may be indicative of DES. [] Additionally, the eye focusing and ocular movements required for better visibility of digital screens place additional demand on an intricate balance between accommodation and convergence mechanisms, thus making people with uncorrected or under-corrected refractive errors increasingly susceptible.
The most used devices, such as mobile phones and smartphones, are consulted within a proximal distance from the eyes. It has been suggested that smartphones affect distance visual acuity when used at a close distance, while there was no significant evidence regarding computer use [,]. After a few weeks wash out from mobile devices, both subjective symptoms and objective signs of the ocular impairment may improve and even disappear []. Outdoor activity as well as living in a rural context have been postulated to represent protective factors in either childhood and adolescence [,].
Compared to conventional light sources, such as incandescent and fluorescent bulbs, computer displays and smartphone screens emit a higher proportion of blue light (380–500 nm), which is associated with DES symptoms. Evidence suggests that longer smartphone use per day can increase the prevalence rates and odds of risk of ocular symptoms, as well as the likelihood of having multiple ocular symptoms [,]. Multivariate analysis revealed that smartphone use, prolonged use of devices, and mobile games are independent risk factors for DES in children [,,,]. Smartphones are the most frequently linked to ocular symptoms but evidence is increasing also regarding video games. This might be explained by the increased mechanical compression exerted by the contracted eyelid muscles during the child’s concentration effort on their plastic cornea []. The effect was particularly of note during the COVID-19 era, due to the prolonged use of media devices [,,].
3.1.2. Acute Acquired Comitant Esotropia
Acute acquired comitant esotropia (AACE) may be defined as an unusual manifestation of esotropia in older children without limitation of eye movement. Although the etiology is still debated, evidence suggests a possible relationship between AACE and excessive smartphone use, as reported in Table 3. The main identified risk factors were the prolonged time spent on media devices and the close reading distance. Authors assumed that excessive near work causes abnormalities in the balance between convergence and divergence, which increases the tonus in the medial rectus muscle, resulting in the development of esotropia [,]. COVID-19 lockdown with school closure and home confinement impacted lifestyle behavior in the young population, including a significant increase in screen time and an increase in the risk of AACE [].

Table 3.
Acute acquired comitant esotropia and media device.
3.1.3. Data Analysis According to Group Age
Considering children aged less than 12 years, and adolescents aged 13 to 18 years, 12 reports were analyzed [,,,,,,,,,,]. Regarding the others, data referred to the pediatric population but without a clear distinction of the results from childhood to adolescence.
In detail, nine studies focused on childhood [,,,,,,,,]. A prolonged screen vision is associated with the risk of developing eye impairment, myopia, and dry eye syndrome []. The duration of computer, smartphone, and video game screen use correlates to irritation, burning sensation, decreased visual acuity, myopia, and dry eye syndrome in several studies [,,,]. Analyzing risk factors correlated with myopic refractive errors, computers and smartphones but not television have been identified in childhood [,]. The first postnatal year represents a sensitive period, as screen exposure in early life can be significantly and positively associated with myopia in childhood [,,]. Myopia prevalence increased with daily exposure duration and total years of exposure [,,]. Screen time exposure correlates with increased myopic spherical equivalent refraction, shorter corneal radius, and higher axial length/corneal radius []. Children spending 3 or more hours daily had a fivefold prevalence of eye impairment []. Myopia prevalence increased in the COVID-19 era, likely due to more screen time [,].
Out of the included articles, three present results focused on adolescence [,,]. Adolescents with a high exposure to smartphones were found to have higher prevalence rates for ocular symptoms, including inflammation, redness, and lacrimation, and for myopia [,,]. Prolonged daily smartphone use links with a higher risk of multiple ocular symptoms []. It is a matter of speculation whether the increasing prevalence of eye impairment is related to light exposure, alteration in circadian rhythms, or reduced outdoor activity. Evidence suggests both low physical activity and prolonged screen device exposure are significant contributors to sight problems [].
Compared to the pre-pandemic period, in the COVID-19 era, the mean duration of the digital use increased. Multivariate analysis revealed smartphone use, and prolonged use of devices and mobile games, are independent risk factors for dry eye syndrome and digital eye strain [].
4. Discussion
The evidence suggests that media device use may have consequences for the eye’s health, including the risk of pre-myopia, myopia, digital eye strain, and acute acquired comitant esotropia [,,,,,,,,,,,,,,,,,,,,,,,,,].
Viewing distance plays a role if we refer to emerging technologies and devices. The recent sharp increase in the number of children and adolescents spending long periods looking at screens, as well as the availability of technology on laptops or small devices such as pocket-size devices, represent risk factors for eye health [,,,,,]. The literature supports the evidence that media device viewing duration and close distance relate to the risk of myopia, dry eye disease, and acute acquired comitant esotropia [,,,,,]. Small screens and the font size of mobile devices promote a closer viewing distance, leading to ocular fatigue and placing a greater demand on accommodation and vergence than computer screens or printed materials. A reduced blink rate and faster evaporation of the tear film in the case of prolonged media device use may lead to dry eye disease.
AACE in children, especially related to the increased use of electronic devices, may be linked to latent hyperopia and the development of accommodative esotropia. Low fusional divergence, along with increased accommodation and convergence demands from near work, can contribute to the development of esotropia in children with latent hyperopia. Children with low fusional divergence have a reduced ability to relax their convergence and allow the eyes to diverge effectively when looking at distant objects. This can lead to a situation where the eyes remain excessively converged even when they should not be, contributing to strabismus. In children with latent (or uncorrected) hyperopia, the extra effort needed to focus on near objects can trigger excessive convergence. This is further amplified by extended near work, reinforcing the inward deviation of the eyes. Children with weak divergence ability (low fusional divergence) are particularly susceptible to developing esotropia in such circumstances. Essentially, the eye is stuck in an overly converged state because the child cannot easily relax their convergence to compensate for the latent hyperopia, and the demands of near work keep triggering excessive accommodation and convergence. Cycloplegic refraction and measurements of fusional reserves were taken into consideration in the analyzed studies [,]. Cycloplegic refraction eliminates the influence of accommodation, providing a more accurate assessment of the child’s refractive error. It helps determine if optical correction of hyperopia will improve the esotropia. Measuring fusional reserves assesses the dynamic component of the child’s ocular alignment. It can help identify any other underlying vergence issues that may require different treatment strategies.
The small number of studies limits the interpretation of the evidence according to different types of mobile media devices used, even if smartphones and other mobile media devices have been frequently associated with ocular problems [,].
Considering different age groups, we identified evidence in childhood and in adolescence in many cases. In children aged less than 12 years, the evidence suggests an increased risk of poor eye health after the COVID-19 pandemic due to an increased use of media devices likely correlated with an increased time spent on close-distance activities and digital devices [,].
Public health measures should be adopted to avoid the consolidation of these unhealthy behaviors and promote, on the contrary, correct lifestyles. Modifiable factors in the case of excessive screen viewing time include mobile phone use before bedtime, parents’ perception about the child’s habituation to screen time, having a device located in the bedroom, morning mobile screen viewing time, and lack of outdoor play or reading [].
Lifestyle, including low outdoor activity, Westernized dietary habits, and urban setting, should be considered when referring to risk factors for myopia and dry eye syndrome in minors exposed to media devices [,,,,,].
In line with the Italian Society’s recommendations, we suggest that families’ education about the correct use of media devices is fundamental to protecting minors’ sight. Parents should be educated regarding media device exposure in childhood, modulating it based on clinical evidence and scientific recommendation, limiting especially the use at a close distance. There should be no media device use in children less than 2 years of age, during meals, before bedtime, or as a limited pacifier. Children should use media devices in the presence of a caregiver to supervise both contents and physical posture [].
Regarding adolescents, the literature reveals an association between the high use of screen devices, reduced levels of physical activity, and the risk of myopia []. So, as well as in childhood, sports and physical activity should be promoted among adolescents. In adolescence, as well, rules and limits should be discussed to prevent ocular problems because the increased use of smartphones may result in problems such as dry eye disease, eye irritation, decreased visual acuity, and macular degeneration [,].
The connection between myopia and outdoor activity has become a significant area of research in recent years [,,,,]. The evidence suggests that spending less time outdoors is a key risk factor for the development and progression of myopia []. On the contrary, exposure to natural light may play a protective role. Studies have shown that children who spend more time outdoors, where they are exposed to brighter light, tend to have a lower risk of myopia compared to those who spend more time indoors. The main potential mechanisms involved in the protective effect of time spent outdoors against myopia include exposure to elevated levels and shorter wavelengths of light (daylight), and increased dopamine and vitamin D levels. Vitamin D synthesis, as well as the concentration and release of dopamine influenced by outdoor time, may play a role in inhibiting myopic development, thereby promoting eye growth [,,,]. So, interventions should be aimed at increasing daily light exposure and outdoor activities [,]. Spending time outdoors may also encourage activities like focusing on distant objects, which may help eye health, even if the relationship with myopia remains controversial []. In a cross-sectional study of children, more time spent in outdoor sport and activity was associated with lower myopia risk, but there was no similar effect for indoor sports and activity. This suggests that spending time outdoors, rather than physical activity, was protective for eye health [].
A simple but scientific dialogue with families on media device use should be undertaken during check controls. The evidence suggests that the parents with higher levels of risk perception and more parental mediation were more likely to mediate their child’s eye care behavior. Moreover, minors whose parents had a lower mediation and spent a prolonged period online were at higher risk for a prolonged SVT [].
Pediatric ophthalmologists are now constantly facing disorders related to the use of electronic devices, particularly if they are used at a close distance. So, the level of parents’ awareness of the potential risks should be considered, and the short and long-term consequences of the incorrect use of the devices should be explained [,,]. Then, recommendations to contain the problem should be shared, including adequate lighting, avoiding prolonged use and display use at night, the distance from the device, and limiting near-use for text and message-sharing activities [,]. In the case of reduced visual acuity and without refractive errors in cycloplegia or ocular pathologies, a wash-out period from the devices must be recommended, followed by a follow-up control. In case of concomitant refractive error, an ophthalmologic correction is required. In case of diplopia, orthoptic and neurological evaluations are prescribed to avoid other possible concomitant systemic pathologies.
A limitation of this research is that the reviewed studies were conducted among different populations of different ages, so the results are not generalizable to all of the pediatric population. Further studies are required to better define the risks according to age groups, ethnicity, demographic, and social characteristics in order to strengthened the evidence regarding media device effects on eye health.
5. Conclusions
Pre-myopia, myopia, digital eye strain, and acute acquired comitant esotropia are potential time-related short- and long-term outcomes associated with incorrect use of media devices among children and adolescents. Raising awareness among parents and policymakers should be considered key to mitigating and avoiding consequences for children’s and adolescents’ sight. We suggest allocating time during a pediatric routine healthcare visit and promptly referring minors to ophthalmologists in case of ocular symptoms.
Author Contributions
E.B. coordinated the study; E.B. and M.F. conceived the study, S.C. and M.I. carried out the literature research, E.B. and M.I. were responsible of the pediatric content of the manuscript, S.C. and M.F. dedicated to the ophthalmologist aspects, and R.H. participated in its design. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported also by the Italian Ministry of Health with “current Research funds”.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| SVT | Screen viewing time |
| DES | Digital eye strain |
| AACE | Acute acquired comitant esotropia |
| SER | myopic spherical equivalent refraction |
| AL | axial length |
References
- Barber, S.E.; Kelly, B.; Collings, P.J.; Nagy, L.; Bywater, T.; Wright, J. Prevalence, Trajectories, and Determinants of Television Viewing Time in an Ethnically Diverse Sample of Young Children from the UK. Int. J. Behav. Nutr. Phys. Act. 2016, 14, 88. [Google Scholar] [CrossRef] [PubMed]
- Kabali, H.K.; Irigoyen, M.M.; Nunez-Davis, R.; Budacki, J.G.; Mohanty, S.H.; Leister, K.P.; Bonner, R.L., Jr. Exposure and Use of Mobile Media Devices by Young Children. Pediatrics 2015, 136, 1044–1050. [Google Scholar] [CrossRef] [PubMed]
- Duch, H.; Fisher, E.M.; Ensari, I.; Harrington, A. Screen time use in children under 3 years old: A systematic review of correlates. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 102. [Google Scholar] [CrossRef] [PubMed]
- Council on Communications and Media. Media and Young Minds. Pediatrics 2016, 138, e20162591. [Google Scholar] [CrossRef]
- Bozzola, E.; Spina, G.; Ruggiero, M.; Memo, L.; Agostiniani, R.; Bozzola, M.; Corsello, G.; Villani, A. Media devices in pre-school children: The recommendations of the Italian pediatric society. Ital. J. Pediatr. 2018, 44, 69. [Google Scholar] [CrossRef]
- Toumbourau, J.W. Developmental trajectories of Internalising Behaviours in the prediction of adolescent depressive symptoms. Aust. J. Psicol. 2011, 63, 214–223. [Google Scholar] [CrossRef]
- Hinkley, T.; Verbestel, V.; Ahrens, W.; Lissner, L.; Molnár, D.; Moreno, L.A.; Pigeot, I.; Pohlabeln, H.; Reisch, L.A.; Russo, P.; et al. Early childhood electronic media use as a predictor of poorer well-being: A Prospective cohort study. JAMA Pediatr. 2014, 168, 485–489. [Google Scholar] [CrossRef]
- Chiang, H.Y.; Liu, C.H. Exploration of the associations of touch-screen tablet computer usage and musculoskeletal discomfort. Work. 2016, 53, 917–925. [Google Scholar] [CrossRef]
- Cain, N.; Gradisar, M. Electronic media use and sleep in school-aged children and adolescents: A review. Sleep. Med. 2010, 11, 735–742. [Google Scholar] [CrossRef]
- Bozzola, E.; Spina, G.; Ruggiero, M.; Vecchio, D.; Caruso, C.; Bozzola, M.; Staiano, A.M.; Agostiniani, R.; Del Vecchio, A.; Banderali, G.; et al. Media use during adolescence: The recommendations of the Italian Pediatric Society. Ital. J. Pediatr. 2019, 45, 149. [Google Scholar] [CrossRef]
- Jones, E.; LibGuides, M. Creating a PRISMA Flow Diagram; PRISMA: San Francisco, CA, USA, 2020. [Google Scholar]
- Trovato Battagliola, E.; Mangiantini, P.; D’Andrea, M.; Malvasi, M.; Loffredo, L.; Scalinci, S.Z.; Comberiati, A.M.; Migliorini, R.; Pacella, E. Effect of COVID-19 lockdown on refractive errors in Italian children aged 5-12 years: A multi-center retrospective study. Eur. J. Ophthalmol. 2023, 33, 112–122. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bhattacharya, S.; Heidler, P.; Saleem, S.M.; Marzo, R.R. Let There Be Light-Digital Eye Strain (DES) in Children as a Shadow Pandemic in the Era of COVID-19: A Mini Review. Front. Public. Health 2022, 10, 945082. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Foreman, J.; Salim, A.T.; Praveen, A.; Fonseka, D.; Ting, D.S.W.; Guang He, M.; Bourne, R.R.A.; Crowston, J.; Wong, T.Y.; Dirani, M. Association between digital smart device use and myopia: A systematic review and meta-analysis. Lancet Digit. Health 2021, 3, e806–e818. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.W.; Tsai, A.; Jonas, J.B.; Ohno-Matsui, K.; Chen, J.; Ang, M.; Ting, D.S.W. Digital Screen Time During the COVID-19 Pandemic: Risk for a Further Myopia Boom? Am. J. Ophthalmol. 2021, 223, 333–337. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Harrington, S.C.; Stack, J.; O’Dwyer, V. Risk factors associated with myopia in schoolchildren in Ireland. Br. J. Ophthalmol. 2019, 103, 1803–1809. [Google Scholar] [CrossRef] [PubMed]
- Hansen, M.H.; Laigaard, P.P.; Olsen, E.M.; Skovgaard, A.M.; Larsen, M.; Kessel, L.; Munch, I.C. Low physical activity and higher use of screen devices are associated with myopia at the age of 16-17 years in the CCC2000 Eye Study. Acta Ophthalmol. 2020, 98, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Enthoven, C.A.; Tideman, J.W.L.; Polling, J.R.; Yang-Huang, J.; Raat, H.; Klaver, C.C.W. The impact of computer use on myopia development in childhood: The Generation R study. Prev. Med. 2020, 132, 105988. [Google Scholar] [CrossRef] [PubMed]
- Harrington, S.; O’Dwyer, V. The association between time spent on screens and reading with myopia, premyopia and ocular biometric and anthropometric measures in 6- to 7-year-old schoolchildren in Ireland. Ophthalmic Physiol. Opt. 2023, 43, 505–516. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Ye, S.; Xi, W.; Zhang, X. Electronic devices and myopic refraction among children aged 6-14 years in urban areas of Tianjin, China. Ophthalmic Physiol. Opt. 2019, 39, 282–293. [Google Scholar] [CrossRef] [PubMed]
- Terasaki, H.; Yamashita, T.; Yoshihara, N.; Kii, Y.; Sakamoto, T. Association of lifestyle and body structure to ocular axial length in Japanese elementary school children. BMC Ophthalmol. 2017, 17, 123. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Guan, H.; Yu, N.N.; Wang, H.; Boswell, M.; Shi, Y.; Rozelle, S.; Congdon, N. Impact of various types of near work and time spent outdoors at different times of day on visual acuity and refractive error among Chinese school-going children. PLoS ONE 2019, 14, e0215827. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, J.; Li, B.; Sun, Y.; Chen, Q.; Dang, J. Adolescent Vision Health During the Outbreak of COVID-19: Association Between Digital Screen Use and Myopia Progression. Front. Pediatr. 2021, 9, 662984. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Saxena, R.; Vashist, P.; Tandon, R.; Pandey, R.M.; Bhardawaj, A.; Menon, V.; Mani, K. Prevalence of myopia and its risk factors in urban school children in Delhi: The North India Myopia Study (NIM Study). PLoS ONE 2015, 10, e0117349. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Singh, N.K.; James, R.M.; Yadav, A.; Kumar, R.; Asthana, S.; Labani, S. Prevalence of Myopia and Associated Risk Factors in Schoolchildren in North India. Optom. Vis. Sci. 2019, 96, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.Y.; Huang, L.H.; Schmid, K.L.; Li, C.G.; Chen, J.Y.; He, G.H.; Liu, L.; Ruan, Z.L.; Chen, W.Q. Associations Between Screen Exposure in Early Life and Myopia amongst Chinese Preschoolers. Int. J. Environ. Res. Public Health 2020, 17, 1056. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chang, P.; Zhang, B.; Lin, L.; Chen, R.; Chen, S.; Zhao, Y.; Qu, J. Comparison of Myopic Progression before, during, and after COVID-19 Lockdown. Ophthalmology 2021, 128, 1655–1657. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alvarez-Peregrina, C.; Martinez-Perez, C.; Villa-Collar, C.; Andreu-Vázquez, C.; Ruiz-Pomeda, A.; Sánchez-Tena, M.Á. Impact of COVID-19 Home Confinement in Children’s Refractive Errors. Int. J. Environ. Res. Public Health 2021, 18, 5347. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, W.; Zhu, L.; Zheng, S.; Ji, Y.; Xiang, Y.; Lv, B.; Xiong, L.; Li, Z.; Yi, S.; Huang, H.; et al. Survey on the Progression of Myopia in Children and Adolescents in Chongqing During COVID-19 Pandemic. Front. Public Health 2021, 9, 646770. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- McCrann, S.; Loughman, J.; Butler, J.S.; Paudel, N.; Flitcroft, D.I. Smartphone use as a possible risk factor for myopia. Clin. Exp. Optom. 2021, 104, 35–41. [Google Scholar] [CrossRef]
- Moon, J.H.; Kim, K.W.; Moon, N.J. Smartphone use is a risk factor for pediatric dry eye disease according to region and age: A case control study. BMC Ophthalmol. 2016, 16, 188. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, J.; Hwang, Y.; Kang, S.; Kim, M.; Kim, T.S.; Kim, J.; Seo, J.; Ahn, H.; Yoon, S.; Yun, J.P.; et al. Association between Exposure to Smartphones and Ocular Health in Adolescents. Ophthalmic Epidemiol. 2016, 23, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Mohan, A.; Sen, P.; Shah, C.; Jain, E.; Jain, S. Prevalence and risk factor assessment of digital eye strain among children using online e-learning during the COVID-19 pandemic: Digital eye strain among kids (DESK study-1). Indian. J. Ophthalmol. 2021, 69, 140–144. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mohan, A.; Sen, P.; Shah, C.; Datt, K.; Jain, E. Binocular Accommodation and Vergence Dysfunction in Children Attending Online Classes During the COVID-19 Pandemic: Digital Eye Strain in Kids (DESK) Study-2. J. Pediatr. Ophthalmol. Strabismus 2021, 58, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Mohan, A.; Sen, P.; Mujumdar, D.; Shah, C.; Jain, E. Series of cases of acute acquired comitant esotropia in children associated with excessive online classes on smartphone during COVID-19 pandemic; digital eye strain among kids (DESK) study-3. Strabismus 2021, 29, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Rechichi, C.; De Mojà, G.; Aragona, P. Video Game Vision Syndrome: A New Clinical Picture in Children? J. Pediatr. Ophthalmol. Strabismus 2017, 54, 346–355. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.S.; Park, S.W.; Heo, H.B.M.C. Acute acquired comitant esotropia related to excessive Smartphone use. Ophthalmol. 2016, 16, 37. [Google Scholar] [CrossRef] [PubMed]
- Flitcroft, D.I.; He, M.; Jonas, J.B.; Jong, M.; Naidoo, K.; Ohno-Matsui, K.; Rahi, J.; Resnikoff, S.; Vitale, S.; Yannuzzi, L. IMI—Defining and Classifying Myopia: A Proposed Set of Standards for Clinical and Epidemiologic Studies. Investig. Ophthalmol. Vis. Sci. 2019, 60, M20–M30. [Google Scholar] [CrossRef]
- Jain, S.; Shrivastava, S.; Mathur, A.; Pathak, D.; Pathak, A. Prevalence and Determinants of Excessive Screen Viewing Time in Children Aged 3-15 Years and Its Effects on Physical Activity, Sleep, Eye Symptoms and Headache. Int. J. Environ. Res. Public Health 2023, 20, 3449. [Google Scholar] [CrossRef]
- Zhang, J.; Deng, G. Protective effects of increased outdoor time against myopia: A review. J. Int. Med. Res. 2020, 48, 300060519893866. [Google Scholar] [CrossRef]
- French, A.N.; Ashby, R.S.; Morgan, I.G.; Rose, K.A. Time outdoors and the prevention of myopia. Exp. Eye Res. 2013, 114, 58–68. [Google Scholar] [CrossRef]
- Lingham, G.; Mackey, D.A.; Lucas, R.; Yazar, S. How does spending time outdoors protect against myopia? A review. Br. J. Ophthalmol. 2020, 104, 593–599. [Google Scholar] [CrossRef]
- Read, S.A.; Collins, M.J.; Vincent, S.J. Light Exposure and Eye Growth in Childhood. Investig. Ophthalmol. Vis. Sci. 2015, 56, 6779–6787. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).